Abstract
The aim of this study was to determine whether patients whose treatment is consistent with the 3-hour rule have better outcomes than patients whose treatment is not consistent with the 3-hour rule.
This is a retrospective review of the records of 581 patients. The authors compared the outcomes of 397 patients whose therapy was consistent with the 3-hour rule to the outcomes of 184 patients whose therapy was not consistent with the rule for at least one 7-day period during the stay on an inpatient rehabilitation facility.
Patients whose care was consistent with the rule did not have more improvement in function or shorter length of stay than patients whose care was not consistent with the 3-hour rule.
There is not good evidence to support the 3-hour rule as a determinant of the care that a patient at an IRF needs to achieve a good outcome.
Keywords: inpatient rehabilitation facilities, outcomes, three -hour rule
1. Introduction
An inpatient rehabilitation facility (IRF) is eligible for payment as an IRF under the Center for Medicare and Medicaid Services (CMS) prospective payment system if it complies with a number of regulations set forth by CMS. Sixty percent of patients admitted to the unit must have 1 of 13 conditions: stroke, spinal cord injury, congenital deformity, amputation, major multiple trauma, fracture of the hip, brain injury, burns, active polyarthritis, systemic vasculitis with joint involvement, specified neurologic conditions, severe or advanced osteoarthritis, knee or hip replacement (if bilateral, body mass index >50, or age 85). This is known as the 60% rule. The patients must be offered an intensive multidisciplinary rehabilitation program. They should attend 3 hours of therapy in 5 of 7 consecutive days. They may attend 15 hours (900 minutes) of therapy in 7 days if there is a reason (such as low endurance) why they cannot attend therapy 3 hours per day in 5 of 7 days (3-hour requirement). The therapies included in the rule are physical therapy (PT), occupational therapy (OT), speech and language pathology (SLP), and orthotic and prosthetic services. The patient must be cared for by nurses with specialized training or experience in rehabilitation services and must be seen by a physician with specialized training in rehabilitation at least 3 times per week. The patient must have a case manager or social worker. There must be an interdisciplinary team conference led by the physician at least once a week. At the time of admission, there must be the expectation that the patient can benefit from therapy. There must be daily notes and team conference notes that provide evidence that the patient's level of function is improving.[1,2]
The 3-hour requirement was based upon the recommendation of consultants to the Health Care Financing Administration.[3] The requirement was not based upon objective evidence that 3 hours per day of therapy is necessary or sufficient to promote good outcomes on an IRF. Two studies have evaluated the benefit of this regulation. Wang et al reviewed the outcomes of 360 patients who had rehabilitation after cerebrovascular accident. They reported that patients who received 3 hours per day of therapy had better outcomes than patients who received <3 hours per day of therapy.[3] Johnston and Miller compared 426 patients admitted to an IRF in 1982 before the 3-hour rule went into effect and 501 patients in 1983 after the rule went into effect. They reported that therapy time per patient increased by 0.55 hour per day in 1983. The increased therapy time did not result in improvement in function or reduction in length of stay (LOS).[4] Foley et al[5] reviewed the literature pertaining to time of therapy provided on an IRF and concluded that there is not sufficient evidence to support a regulation that requires 3 hours per day of therapy 5 days per week or 900 minutes of therapy per week in patients who cannot tolerate 3 hours of therapy in a day.
The 3-hour requirement applies to all patients regardless of age, admitting diagnosis, functional level, or comorbidities. It does not take into account the need for other services such as mental health professionals, physicians, wound care, nutrition, and registered nurses that may not be available or readily available at skilled nursing facilities or with in-home care. The rule has been used by third-party payors to deny previous authorization for an admission to an IRF. The rule has been used by third-party payors and recovery audit contractors to deny payment for care at an IRF.
The intent of this study is to evaluate whether patients at the Medical Center who received therapy that was consistent with the 3-hour rule had better outcomes than patients in the same program who in at least one 7-day period attended <900 minutes of therapy. The purpose of the article is to try to answer two questions. Is 900 minutes per week of therapy a threshold that needs to be passed to provide high quality rehabilitation? Can patients who do not meet the CMS guideline for therapy hours make as much progress as patients who do meet the CMS guideline for therapy hours? A purpose of the study was to help to determine whether it makes sense to use the 3-hour rule as a requirement for every patient's admission to an IRF or payment to an IRF.
2. Methods
Data were collected retrospectively from records maintained by the quality improvement team of the Department of Physical Medicine and Rehabilitation. The authors reviewed the records of all patients admitted to an IRF between September 1, 2013 and December 31, 2015. Patients on the unit for <1 week were excluded from the study. Patients who were transferred to acute medical surgical services were excluded from the study. The authors noted which patients had treatment schedules that were consistent with the 3-hour rule for every 7-day period on the unit (consistent group) and which patients had treatment schedules that were not consistent with the 3-hour rule for at least one 7-day period, while on the unit (not consistent group). The IRF offers PT, OT, and SLP to all patients Monday to Saturday. Patients who missed therapy time, or who are thought to need extra help are offered therapy time on Sunday. The most common reason that patients’ schedules were not consistent with the 3-hour rule was patients wanting to rest rather than attend therapy. Great efforts were made to ensure that each patient was offered therapy time consistent with the rule. The authors recorded the number of minutes of therapy per day of each patient in the study. They recorded the age, sex, admitting diagnosis, admission score on the Functional Independence Measure (FIM), change in FIM score, discharge FIM score, LOS, place of discharge (home, subacute care, or assisted living), and comorbidity tier of each patient. The FIM is an instrument with 18 items that evaluate a patient's mobility, activities of daily living, communication, and cognitive function. Each item is scored from 1 to 7. The minimum score is 18 and the maximum score is 126. CMS requires that each patient admitted to an IRF have a FIM score at the time of admission and at the time of discharge. Two-sample t test was used to compare total change in FIM and change in FIM per day in the consistent and non- consistent groups. Contingency tables and Pearson χ2 test were used to evaluate the relationship between whether a patient was in the consistent or nonconsistent group and whether the patient was discharged to home. Two-sample t test evaluated the number of minutes per day of therapy in the consistent and non- consistent groups. Two-sample t test evaluated the relationship between sex and change in function. A linear regression analysis looked at the relationships between minutes of therapy per day and total change in FIM and change in FIM/day. A regression analysis looked at relationship between minutes of therapy/day and LOS. Mann–Whitney test was used to evaluate whether there was a difference in LOS between the patients in the consistent and nonconsistent group. Mann–Whitney test was also used to look at the relationship between minutes of therapy per day and whether or not the patients were discharged to home. Fisher exact test was used to evaluate the comorbidity tiers of the patients. Multiple linear regression analysis evaluated improvement in FIM score as a function of age, sex, admission FIM score, comorbidity tier, admitting diagnosis, and whether the patient was in the consistent or nonconsistent group.
Most patients in the consistent group are reported to have <180 minutes per day of therapy. Patients may be considered consistent with the rule if they receive 900 minutes of therapy in a 7-day period. Patients may be considered consistent with the rule if they receive 180 minutes of therapy 5 days and <180 per day minutes of therapy during the other 2 days of a 7-day period. The study was approved by the IRB of the Albany Medical College.
3. Results
There were 581 patients in the study (Table 1). The therapy hours of 397 patients met the requirements of the 3-hour rule during each 7-day period that they were at the IRF. The records of 184 patients showed at least one week when they did not have 900 minutes of therapy. The patients in the consistent group had an average of 154.0 minutes of therapy per day and the patients in the nonconsistent group had an average of 137.5 minutes per day of therapy. Patients with stroke were more likely to be in the consistent group. Patients with joint replacement and patients who came to the IRF after complex medical/surgical care were less likely to be in the consistent group (Table 2). There were no significant differences between the consistent and notconsistent groups in age, sex, admission FIM score (Table 1.), or comorbidity score. The patients in the consistent group did not have better outcomes in terms of discharge FIM score, change in FIM score, LOS, or discharge to home (Table 1). Regression analysis looked at the relationship between minutes of therapy per day and improvement in FIM and improvement in FIM per day. Regression analysis did not show that more minutes of therapy/day were associated with a greater improvement in FIM (Fig. 1) or in FIM/day (Fig. 2). Regression analysis did not show that more minutes per day were associated with reduced LOS (Fig. 3). Actually, patients with fewer minutes per day had more improvement in FIM/day (P = .02) and shorter LOS (P > .001). For both of these equations, the r2 is small (1.6% for FIM/day and 5.4% LOS) indicating that most of the variation is likely related to other factors. Each patient admitted to an IRF is assigned to a comorbidity group 0–3.[6] Fisher exact test showed that there were no significant differences between the consistent group and the nonconsistent group in terms of the percentage of patients in any of the comorbidity tiers.
Table 1.
Patient demographics.
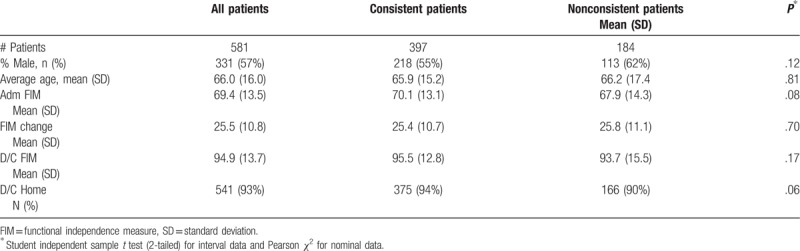
Table 2.
Diagnostic groups.
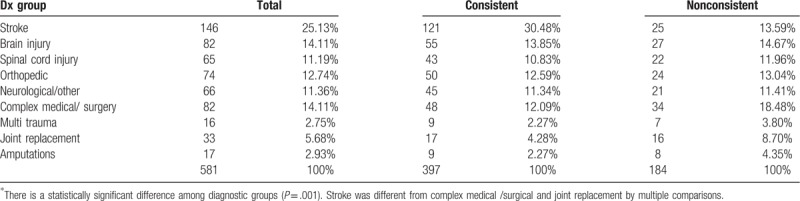
Figure 1.
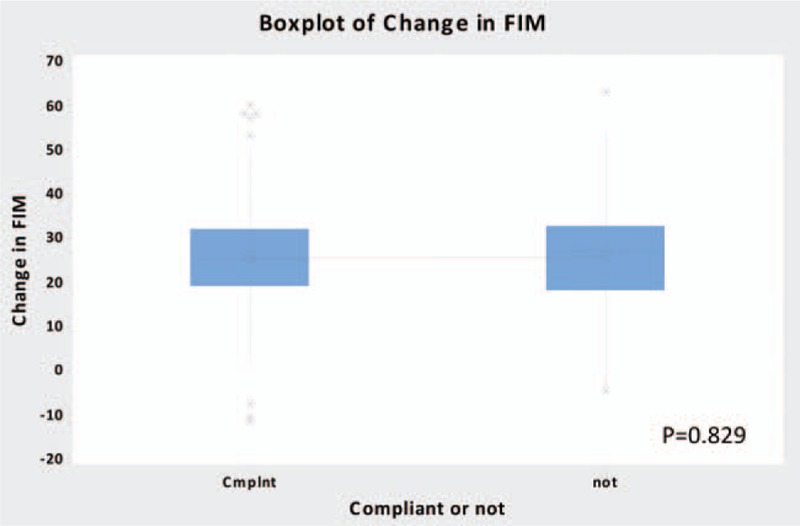
Boxplot change in FIM. FIM = functional independence measure.
Figure 2.
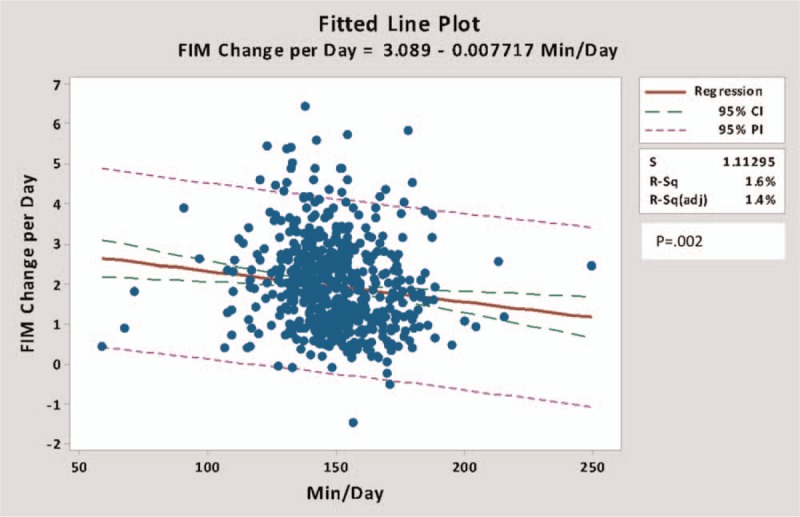
Regression analysis FIM change per day versus minute per day. FIM = functional independence measure.
Figure 3.
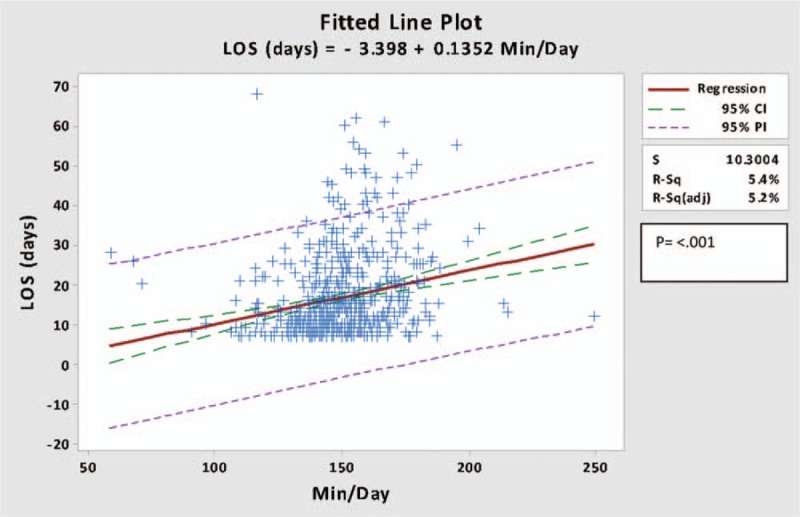
Regression analysis LOS (days) versus minute per day. LOS = length of stay.
Multiple linear regression analysis did not find a significant relationship between improvement in FIM and comorbidity tier or being consistent with the 3-hour requirement (P = 0.546) or sex (P = 0.302). Improvement in FIM correlated with age (P < 0.001) and with admission FIM score (P < 0.001). The coefficient of age at admission was −0.1105 change in FIM/year of age. Thus, for every 10 years of age, there was a 1.1 point less improvement in FIM score. The coefficient of admission FIM score was −0.3259 change in FIM/unit FIM on admission. For every 10-point increase in FIM score improvement in FIM was reduced by 3.26 points. The only diagnosis with a significant relationship to improvement in FIM was total joint replacement (P = .029). Patients in the joint replacement group had significantly more improvement than patients in the other 8 diagnostic groups.
A regression analysis of FIM change per day versus minutes per day showed that patients in orthopedic, joint replacement, and complex medical/surgical group had a trend to have more positive change in FIM per minute per day than did the patients in the stroke group but results did not reach significance (Fig. 4).
Figure 4.
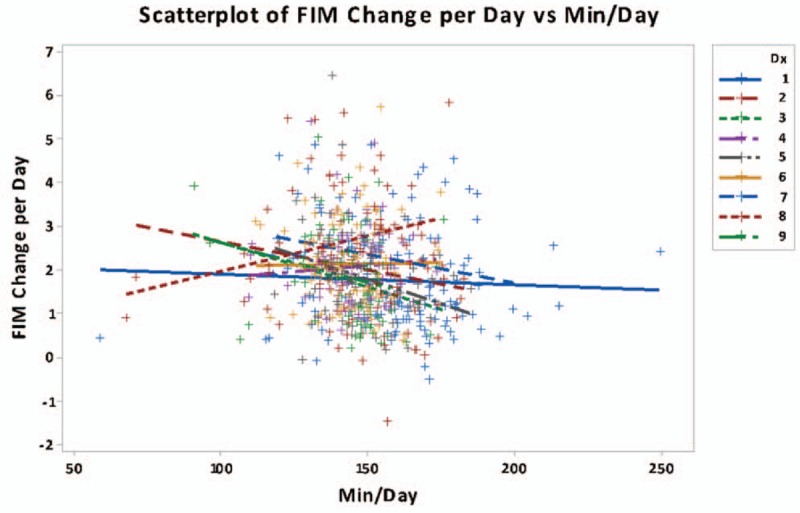
Scatterplot of FIM change per day versus minute per day. FIM = functional independence measure.
4. Discussion
The staff of the IRF made every effort to make sure that each patient was offered and scheduled for an adequate and intensive program of therapy. The difference in the therapy time of the patients in the consistent and not consistent groups was 18.5 minutes/day. This study like the study of Johnston and Miller[4] did not find 3 hours per day or 900 minutes per week of therapy to be a threshold necessary or associated with improvement in function. Multiple linear regression analysis showed that age, admission FIM score, and the diagnosis of total joint replacement were significantly related to improvement in FIM. Younger age is associated with better outcomes from illness and from IRF.[7] There is a ceiling effect on improvement in FIM.[8] When patients reach an adequate level of function, they are discharged to home. Therefore, properly selected patients at a lower level of function may make more improvement than patients admitted with a higher FIM score. Total joint replacement is a procedure with a very high rate of good outcomes.[9]
Regression analysis showed that patients in nonconsistent group had shorter LOS and more improvement in FIM/day. The R2 was small indicating that the variation was likely due to factors other than therapy time. There was a higher percent of patients in the non-consistent group who went to IRF after total joint replacement (8.7 vs 4.3). There was a trend (P = .08) for the patients in the nonconsistent group to have a lower admission FIM score (67.9 vs 70.1). These factors likely contributed to the difference in outcomes between the consistent and nonconsistent groups.
There were more patients in the consistent group than non- consistent group with a diagnosis of stroke (30.5% vs 13.6%). There were significantly more patients in the consistent group with stroke compared to complex medical/surgical and joint replacement (P = .001) (Table 2). There was a trend for patients in the stroke group to have less FIM change per day versus minutes per day than patients in those 2 groups (Fig. 4). This also likely contributed to the difference in outcome between the consistent and nonconsistent groups.
The literature is consistent with the idea that exercise is good medicine. Exercise is important in improving strength, endurance, coordination, and the ability to perform functional tasks.[10] Wade and de Jong[11] report that there are no studies that indicate the minimum amount of therapy time necessary to help a patient or the maximum amount of time beyond which therapy is not helpful. Keith, PhD,[12] reviewed the literature of treatment strength in rehabilitation and reported that evidence for a direct relationship between treatment intensity and outcome is mixed. There are studies that show that increased therapy time leads to reduced LOS and improved level of function. Roach et al reviewed the records of 177 patients admitted to an acute care hospital with orthopedic problems that impaired the patients’ ability to walk. They found a significant relationship between minutes of PT and functional status at discharge.[13] Kirk-Sanchez and Roach[14] reviewed the records of 116 patients admitted to an IRF after orthopedic surgery. They found that increased therapy time was related to improved level of function at time of discharge. DiSotto-Monastero et al reported the results of increasing therapy services at an IRF from five days per week to 7 days per week. The study population was 3500 patients admitted with a diverse set of problems. LOS was reduced from 20.3 days to 19.3 days, but there was no change in improvement in function.[15] Hughes et al[16] compared patients who received 5 day per week and patients who received 7 day per week therapy after total joint replacement and found reduced LOS in the 7 day per week group. Rapoport and Judd-Van Eerd[17] reported that patients at a community hospital with stroke and orthopedic problems had shorter LOS if they had therapy 7 days per week than if they had therapy 5 days per week. Qu et al[18] discussed data available in the National Spinal Cord Injury data base (SCI). Review of the records of 1974 patients admitted 2000 to 2004 showed a significant relationship between therapy time and improvement in function. Dumas et al[19] reviewed the records of 80 children and adolescents admitted to an IRF with traumatic brain injury (TBI) and found a significant relationship between the amount of therapy provided and improvement in function. Slade et al randomly assigned 141 patients with neurologic problems to a usual care group and an enhanced therapy group. Patients in both groups made the same amount of improvement in function as measured by the Barthel's Index, but the patients in the enhanced therapy group had a significantly shorter LOS.[20] Spivak et al[21] reviewed the records of 95 patients admitted to an IRF with TBI and found a significant relationship between the amount of therapy provided and improvement in function. Peiris et al randomly assigned 996 patients admitted to 2 IRFs in Australia, to groups that received therapy 5 days per week and 7 days per week. The patients in the 7 day per week therapy group made significantly more improvement in function and had significantly shorter LOS.[22] Cifu et al[23] reviewed records of 491 patients admitted to IRFs participating in the Model TBI System and reported that increased therapy time was significantly related to improved motor function but not to improved cognitive function or LOS.
There are also studies that show no significant relationship between increased therapy time and improved outcome. Ruff et al assigned patients admitted to an IRF after stroke to groups that received therapy 6 days per week and 7 days per week. There was no difference in improvement in function or LOS.[24] Horn et al[25] reviewed the records of 2130 patients in the Model Traumatic Brain Injury System and found that the number of minutes of therapy provided contributed minimally to the outcome of the patient. Heinemann et al reviewed the records of 140 patients with TBI and 106 patients with SCI. The study did not show a significant relationship between the time spent with therapy and improvement in function.[26] Keren et al[27] collected data from 50 patients admitted to an IRF after stroke and found no significant relationship between therapy minutes and improved function.
There are many differences between the IRF at the institution where this study took place and subacute units. Appropriate physicians and diagnostic technologies for any unresolved medical issues or new problems are available on site. This level of physician care is generally not available at a subacute rehabilitation unit. An IRF has a higher ratio of nurses to patients and a higher ratio of registered nurses to total nurses than does a subacute rehabilitation unit.[28] Studies have shown that patient outcomes are improved by increased ratios of nurses to patients and increased ratio of registered nurses to patients.[29] Evaluation and counseling by psychiatrists, psychologists, and clinical nurse specialists to help the patient understand or change behaviors that cause the patient to refuse therapy may be more available at the IRF than a subacute unit.
Different patients may have varying needs for different members of the rehabilitation team. For many patients, the amount of time spent in gym with PT and OT is the most important factor in their recovery. Other patients’ improvement may depend upon the availability of a comprehensive medical staff to manage complicated problems. Some patients need nurses with great expertise in management of skin care, bowel and bladder problems, or behavioral issues. Some patients may need counseling. It is easy to document the amount of time that a patient spends with PT, OT, and SLP. It is very difficult to quantify the value of the physician and nursing services that are more available at an IRF than at a subacute rehabilitation unit.
Decisions as to where patients go for post-acute care are often determined in large part by the 60% rule and the 3-hour rule. The 60% rule is a regulation-based entirely upon opinion.[30] There have been only 3 studies evaluating the 3-hour rule. Neither this study nor the study of Johnston and Miller[4] found that patients whose treatments are consistent with the 3-hour rule have better outcomes than patients who receive a little less therapy time than is required by the rule. Wang et al[3] found that patients whose treatments were consistent with the 3-hour regulation had better outcomes than patients whose therapy was not consistent with the rule. This study and the study of Johnston and Miller[4] included all admissions to an IRF. The study of Wang et al included only patients with stroke. This possibly accounts for the different conclusions. The patients in the study of Wang and colleagues received an average of 34 minutes per day of SLP. Patients with stroke are more likely than patients in other diagnostic groups such as hip fracture or amputation to require speech therapy so the groups are not exactly comparable.
The courts have ruled that it is not appropriate for a patient to be denied access to an IRF based on the requirement for 3 hours per day of therapy. In the case of Hooper versus Sullivan, a federal court judge ruled that carriers cannot deny admission to an IRF based upon the 3-hour. Admission to an IRF should be considered necessary if the patient receives a coordinated program of multiple services at a level that cannot be provided at home or in a skilled nursing facility. On February 23,2018 CMS informed Medicare contractors that they cannot deny reimbursement based upon any threshold of therapy time.[31]
The main conclusion of the study and the review of the literature are in agreement with the ruling in the federal court district of Connecticut. There is not sufficient evidence to support 3 hours per day of therapy as a criterion for admission or continued stay on an IRF. Each patient needs to be evaluated based on diagnosis, level of function, age, comorbidities, and need for medical, and nursing services that might not be available at a lower level of care. The study highlights the fact that the 3-hour rule applies the same requirement for treatment to patients with very different problems.
A limitation of this study is that it is a retrospective study and it was performed at 1 IRF. Ethical and regulatory issues will make randomized prospective studies of different therapy times difficult to perform. Medical complexity was controlled for using the comorbidity tiers developed by CMS for IRF. The study also uses admission FIM. Shih et al[32] have shown that admission FIM score is as good or better than comorbidity indices for predicting medical stability. A study with a more concentrated focus on the need for therapy time by patients receiving 2 therapies as opposed to 3 therapies would be helpful. A study concentrated on therapy time needed by patients with different diagnosis would be helpful.
Author contributions
Conceptualization: George P Forrest.
Formal analysis: George P Forrest.
Investigation: George P Forrest, Alycia Horn, Mina Kodsi.
Methodology: George P Forrest.
Project administration: George P Forrest.
Software: Mina Kodsi, Joshua Smith.
Writing – original draft: George P Forrest, Joshua Smith.
Writing – review & editing: George P Forrest, Mina Kodsi.
George P Forrest orcid: 0000-0002-3648-417X.
Footnotes
Abbreviations: CMS = Center for Medicare and Medicaid Services, FIM = functional independence measure, IRF = inpatient rehabilitation facility, LOS = length of stay, OT = occupational therapy, PT = physical therapy, SCI = Spinal cord injury, SLP = speech and language pathology, TBI = traumatic brain injury.
How to cite this article: Forrest G, Reppel A, Kodsi M, Smith J. Inpatient rehabilitation facilities. Medicine. 2019;98:37(e17096).
There is no funding for this paper.
There are no conflicts of interest of any kind
No author received any money or remuneration of any kind relates to this paper.
I have no disclosures. There has been no financial support of any kind for this project or paper.
The authors report no conflicts of interests.
References
- [1].Medicare Benefit Policy Manual Chapter 1 section 110 retrieved from https://www.cms.gov/regulations-and-guidance/guidance/manuals/downloads/bp102c01pdf Accessed on December 9, 2018. [Google Scholar]
- [2].Medicare Learning Network retrieved at https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/Inpatient_Rehab_Fact_Sheet Accessed August 20, 2018. [Google Scholar]
- [3].Wang H, Camicia M, Terdiman J, et al. Daily treatment time and functional gains of stroke patients during inpatient rehabilitation. PM&R 2013;5:122–8. [DOI] [PubMed] [Google Scholar]
- [4].Johnston MV, Miller LS. Cost effectiveness of the Medicare three-hour regulation. Arch Phys Med Rehabil 1986;67:581–5. [PubMed] [Google Scholar]
- [5].Foley N, Pereira S, Salter K, et al. Are recommendations regarding inpatient therapy intensity following acute stroke really evidenced based? Top Stroke Rehabil 2012;19:96–102. [DOI] [PubMed] [Google Scholar]
- [6].CMS Rehabilitation facility tier comorbidity updates 2016. Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/InpatientRehabFacPPS/Downloads/2016-06-16-IRF-Tier-Comorbidity.pdf Accessed December 12, 2018. [Google Scholar]
- [7].Everink IH, van Haastregt JC, van Hoof SJ, et al. Factors influencing discharge after inpatient rehabilitation of older patients: a systematic review. BMC Geriatr 2016;16: doi:1186/s12877-016-0187-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Forrest G, Deike D. The impact of inpatient rehabilitation on outcome for patients with cancer. J Community Support Oncology 2018;16:e138–44. [Google Scholar]
- [9].DeJong G, Tian W, Smout RJ, et al. Long-term outcomes of joint replacement rehabilitation patients discharged from skilled nursing and inpatient rehabilitation facilities. Arch Phys Med Rehabil 2009;90:1306–16. [DOI] [PubMed] [Google Scholar]
- [10].CDC Physical Activity Basics retrieved at https://www.cdc.gov/physicalactivity/basics/pa-health/accessed 8/208/20/2018. [Google Scholar]
- [11].Wade DT, de Jong BA. Recent advances in rehabilitation. BMJ 2000;320:1385–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Keith RA. Treatment strength in rehabilitation. Arch Phys Med Rehabil 1997;78:1298–304. [DOI] [PubMed] [Google Scholar]
- [13].Roach KE, Ally D, Finnerty B, et al. The relationship between the duration of physical therapy services in the acute care setting and change in functional status with lower-extremity orthopedic problems. Phys Ther 1998;78:19–24. [DOI] [PubMed] [Google Scholar]
- [14].Kirk-Sanchez NJ, Roach KE. Relationship between duration of therapy services in a comprehensive rehabilitation program and mobility at discharge in patients with orthopedic problems. Phys Ther 2011;81:888–95. [PubMed] [Google Scholar]
- [15].DiSotto-Monastero M, Chen X, Fish S, et al. Efficacy of 7 days per week inpatient admissions and rehabilitation therapy. Arch Phys Med Rehabil 2012;93:2165–9. [DOI] [PubMed] [Google Scholar]
- [16].Hughes K, Kuffner L, Dean B. Effect of weekend physical therapy on postoperative length of stay following total hip and total knee arthroplasty. Physiother Can 1993;45:245–9. [PubMed] [Google Scholar]
- [17].Rapoport J, Judd-Van Eerd M. Impact of physical therapy weekend coverage on length of stay in an acute care community hospital. Phys Ther 1989;69:32–7. [DOI] [PubMed] [Google Scholar]
- [18].Qu H, Shewchuk RM, Yu-ying C, et al. Evaluating quality of acute rehabilitation care for patients with spinal cord injury: an extended Donabedian model. Qual Manag Health Care 2010;19:47–61. [DOI] [PubMed] [Google Scholar]
- [19].Dumas HM, Haley SM, Carey TM, et al. The relationship between functional mobility and the intensity of physical therapy intervention in children with traumatic brain injury. Pediatr Phys Ther 2004;16:157–64. [DOI] [PubMed] [Google Scholar]
- [20].Slade A, Tennant A, Chamberlain A. A randomized controlled trial to determine the effect of intensity of therapy upon length of stay in a neurological rehabilitation setting. J Rehabil Med 2002;34:260–6. [DOI] [PubMed] [Google Scholar]
- [21].Spivak G, Spettell CM, Ellis DW, et al. Effects of intensity of treatment and length of stay on rehabilitation outcomes. Brain Inj 1992;5:419–34. [DOI] [PubMed] [Google Scholar]
- [22].Peiris CL, Sheilds N, Brusco NK, et al. Additional Saturday rehabilitation improves functional independence and quality of life and reduces length of stay: a randomized controlled trial. BMC Med 2013;11:198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Cifu DX, Kreutzer JS, Kolakowsky-Hayner SA, et al. The relationship between therapy intensity and rehabilitative outcomes after traumatic brain injury: a multicenter analysis. Arch Phys Med Rehabil 2003;84:1441–8. [DOI] [PubMed] [Google Scholar]
- [24].Ruff RM, Yarnell S, Marinos JM. Are stroke patients discharged sooner if in-patient rehabilitation services are provided seven v six days per week? Am J Phys Med Rehabil 1999;78:143–6. [DOI] [PubMed] [Google Scholar]
- [25].Horn SD, Corrigan JD, Beaulieu CL, et al. TBI patient, injury, therapy, and ancillary treatments associated with outcomes at discharge and 9 months post discharge. Arch Phys Med Rehabil 2015;968 suppl:S304–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Heineman AW, Hamilton B, Linacre JM, et al. Functional status and therapeutic intensity during inpatient rehabilitation. Am J of Phys Med and Rehabil 1995;74:315–26. [DOI] [PubMed] [Google Scholar]
- [27].Keren O, Motin M, Heinemann AW, et al. Relationship between rehabilitation therapies and outcome of stroke patients in Israel: a preliminary study. Isr Med Assoc J 2004;6:736–41. [PubMed] [Google Scholar]
- [28].Jung HY, Li Q, Rahman M, et al. Medicare Advantage enrollee's use of nursing homes: trends and nursing home characteristics. Am J of Man Care 2018;24:e349–256. [PMC free article] [PubMed] [Google Scholar]
- [29].Nelson A, Powell-Cope G, Palacios P, et al. Nurse staffing and patient outcomes in inpatient rehabilitation settings. Rehabil Nurs 2007;32:179–202. [DOI] [PubMed] [Google Scholar]
- [30].Reinstein L. The history of the 75-percent rule: three decades past and an uncertain future. PM&R 2014;6:973–5. [DOI] [PubMed] [Google Scholar]
- [31].Medicare Advocacy retrieved at Http://Www.Medicareadvocacy.Org/Cms-Clarifies-3-Hour-Rule-Should-Not-Preclude-Medicare-Covered-Inpatient-Rehabilitation-Hospital-Care Accessed on 12/11/201830. [Google Scholar]
- [32].Shih SL, Zafonte R, Bates DW, et al. Functional status outperforms comorbidities as a predictor of 30-day acute care readmissions in the inpatient rehabilitation population. J of Am Med Dir Assoc 2016;17:921–6. [DOI] [PubMed] [Google Scholar]


