Abstract
Large-cell calcifying Sertoli cell tumor is a very rare neoplasm of the testis with less than 100 reported cases. It is associated with some genetic syndromes, and it has some features that help to distinguish benign and malign cases. An 11-year-old boy presented with testicular lesions in both testicles. He underwent right radical orchiectomy in another institution and was referred to our hospital for further treatment. The lesions were reported as large-cell calcifying Sertoli cell tumors in our institution. There were multiple hyperechoic lesions with calcifications in the left testis and lesions showed vascularization on Doppler. Sonographic features of these lesions were also suggestive of benign large-cell calcifying Sertoli cell tumor. The lesions were stabile during follow-up. The ultrasonographic appearance of large-cell calcifying Sertoli cell tumor is descriptive and, together with clinical findings, allows differential diagnosis. It can direct patient management, with a more conservative approach. We report a child with large-cell calcifying Sertoli cell tumor who could have been saved from extensive surgery, such as radical orchiectomy, if the tumor had been diagnosed correctly with sonography.
Keywords: large-cell calcifying, Sertoli cell tumor, ultrasonography, testis, testicular tumor
Case report
An eleven-year-old boy reported to another hospital with right-sided scrotal pain two months earlier. He had palpitations, pallor and weakness episodes approximately once a month since he was about 2 years old. These episodes occurred mainly when he was hungry and were relieved with the elevation of his legs or some food intake. Cardiological and neurological investigations were unrevealing, and his symptoms disappeared around the age of 7. He suffered from urolithiasis with the stones removed via the urethral route and a double J stent was placed. During his follow-up, bilateral testicular enlargement was noticed, and ultrasonography revealed multiple hyperechoic lesions in both testicles. He underwent right orchiectomy in another hospital. The histopathological examination revealed Sertoli cell tumors. Due to the need for further investigation and follow-up, he was referred to our institution with his tissue blocks.
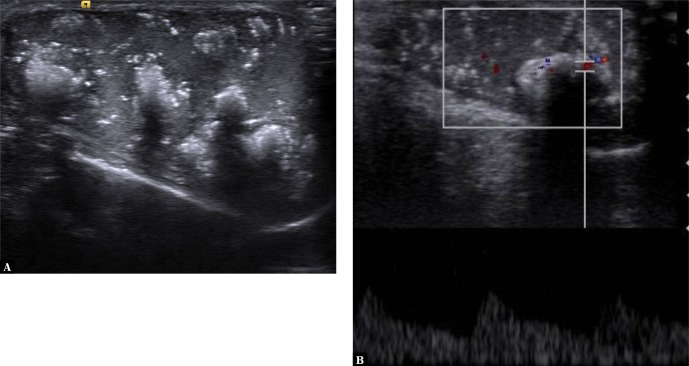
We observed multiple hyperechoic, partially calcified lesions with acoustic shadowing in the left testis (Fig. 1A). All lesions were smaller than 1 cm in diameter and had peripheral vascularization in color and spectral Doppler (Fig. 1B). These lesions were also consistent with large-cell calcifying Sertoli cell tumor (LCCSCT). Indeed, the pathology specimens re-evaluated in our institution were diagnosed as LCCSCT (Fig. 2, Fig. 3).
Fig. 1.
Longitudinal sonogram of the left testis shows multiple diffuse hyperechoic masses with acoustic shadowing. B. Spectral Doppler image shows increased vascularity in the periphery of one of the calcified lesions
Fig. 2.
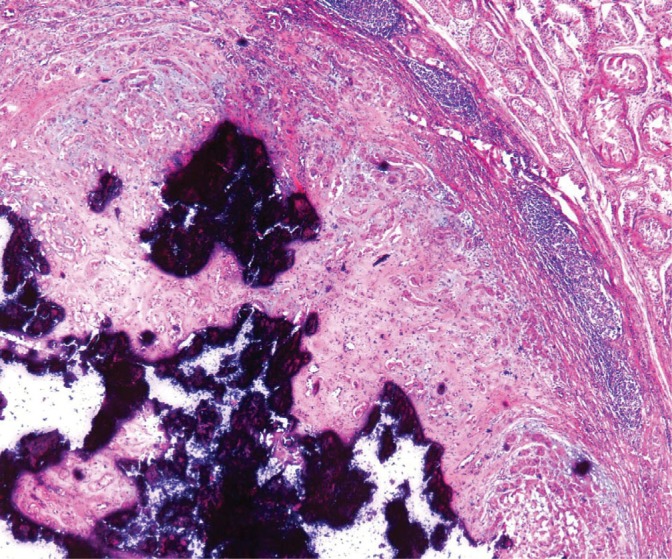
One of the nodules of LCCSCT in the resected testis of the patient (H-E ×40)
Fig. 3.
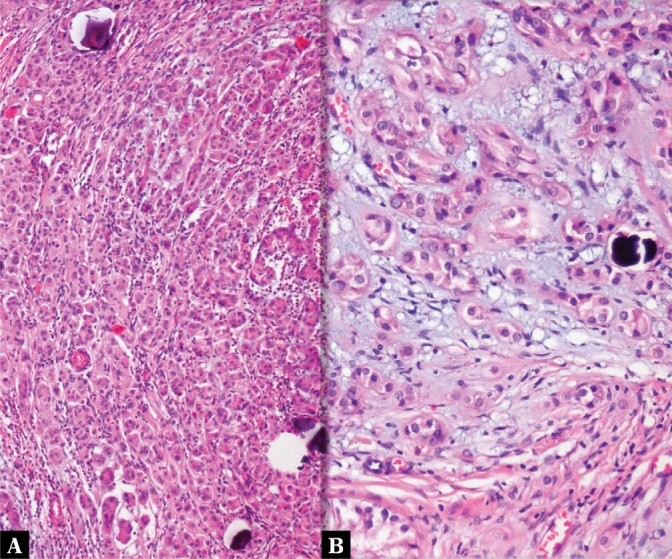
Tumors were composed of cords and solid tubules of large eosinophilic cells within myxoid stroma and areas of calcification (A: H–E × 100; B: H–E ×200)
The patient was explored for the stigmata of Carney complex or Peutz-Jeghers syndrome. He had no signs of endocrinological dysfunction except for increased levels of basal insulin-like growth factor (IGF-1) and urinary cortisol. He was prepubertal and had no gynecomastia or abnormal skin pigmentation on physical examination. His echocardiography was normal. The pituitary gland was normal in MRI. Abdominal imaging was normal except for mild hydronephrosis in the right kidney and minimal wall thickening in the right ureter, possibly related to the history of urolithiasis. No adrenal mass was found. Alphafetoprotein was 1.34 and within normal limits. One year before, he developed swelling in the hard palate which was removed surgically and evaluated histologically as papilloma.
The patient did not meet the diagnostic criteria for Carney complex. Due to the benign course in the overwhelming majority of LCCSCTs, no intervention was planned, and the patient was placed on regular follow-up. The lesions were stable at six- and eighteen-month follow-up after the surgery.
Discussion
Sex cord stromal tumors constitute 4% of testicular neoplasms, and pure Sertoli cell tumors account for less than 1% of testicular tumors. Apart from the classic and malignant forms, the WHO classification of male genital organs from 2016 distinguishes two subtypes: intratubular large-cell hyalinizing tumor and large-cell calcifying tumor(1). Since it was first described by Proppe and Scully(2), less than 100 cases of LCCSCT have been reported. LCCSCT is commonly seen in young patients, with the mean age of 16 years at presentation (3). Sixty percent of these cases were sporadic, while the rest was associated with clinical syndromes. Carney complex and Peutz-Jeghers syndrome are most commonly associated with endocrine disorders. Carney complex is a genetic abnormality which is associated with cardiac myxomas, skin pigmentation, endocrine hyperactivity, and neoplasms. Sudden death can occur secondary to myxoma. More than a half of the cases have autosomal dominant inheritance, but sporadic cases can occur through de novo mutation. Our patient had increased insulin-like growth factor levels beside LCCSCT. A patient must exhibit two major criteria or one major and one supplemental one to diagnose Carney complex. Although increased IGF levels can be associated with Carney complex, it is not one of the diagnostic or supplemental criteria. Our patient had only one major criterion (LCCSCT), and therefore he did not meet the diagnostic criteria for Carney syndrome.
LCCSCT may be multicentric and bilateral, especially if it is associated with Carney complex. Benign tumors are commonly seen in younger patients and tend to be multifocal or bilateral and smaller than 4 cm. About 17% of the reported LCCSCTs were malignant, and all of them unilateral and unifocal. Malignant LCCSCTs tend to occur in older patients (mean age 39 vs 19 years)(3). Only one of the reported malignant LCCSCT cases concerned a child(4). It was a boy with a single lesion in the left testis without prominent calcifications. Except for one patient, all of the LCCSCTs associated with Carney complex were benign(5). Malignancy should be suspected if the lesion is larger than 4 cm, or when there are more than three mitoses per 10 high power fields, extratesticular growth, necrosis, hemorrhage, significant nuclear atypia and angiolymphatic invasion. Malignant tumors can metastasize to retroperitoneal lymph nodes or, less commonly, to the lungs, liver, and bones(6).
Ultrasound plays a crucial role in the differential diagnosis of testicular lesions(7). LCCSCTs are characterized by partially calcified, regularly round hyperechoic intratesticular lesions with acoustic shadowing and vascularity in ultrasonography, as in our case(3). Due to artifacts caused by prominent calcifications, it can be hard to evaluate the internal vasculature of the lesions. The presence of multiple calcified lesions with similar echogenicity and vascularization suggests LCCSCT. Leydig cell hyperplasia is their main radiological differential diagnosis. Clinical features and laboratory tests are helpful in distinguishing them from Leydig cell hyperplasia(8). Even though some of the germ-cell tumors may calcify, heterogeneity and presence of cystic parts are helpful to differentiate(9). LCCSCT is one of the entities in which ultrasound can suggest a diagnosis with significant accuracy due to its distinctive sonographic features, which may spare the need for a histopathologic examination.
The treatment of malignant cases is radical orchiectomy. But its rarity has prohibited the establishment of standard treatment for benign cases despite reported various radical or partial orchiectomy/tumorectomies. The confirmation of the benign nature of the lesion with intraoperative frozen section analysis has been recommended if organ-sparing surgery is planned(10). It was not possible to perform partial orchiectomy in our case due to multiple tumors. However, because of the absence of reported malignant LCCSCT in bilateral cases, regular clinical and ultrasonographic follow-up may be preferred in the case of distinctive sonographic appearance in order to avoid complications of the surgery and lifelong hormone replacement treatment. If ultrasound had been conducted at the initial presentation and helped establish the diagnosis of LCCSCT, a biopsy would have been performed to confirm the diagnosis and follow-up rather than radical orchiectomy could have been recommended. The lesions of the other testis were stabile during the follow-up period.
Conclusion
Characteristic sonographic features in LCCSCT can suggest the diagnosis before invasive procedures. Patients need to be investigated for the presence of commonly associated clinical syndromes that may imply an increased risk for the possible development of other malignancies.
Footnotes
Conflict of interest
Authors do not report any financial or personal connections with other persons or organizations, which might negatively affect the contents of this publication and/or claim authorship rights to this publication.
References
- 1.Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE: WHO Classification of Tumours of the Urinary System and Male Genital Organs. International Agency for Research on Cancer, Lyon 2016.
- 2.Proppe KH, Scully RE: Large-cell calcifying Sertoli cell tumor of the testis. Am J Clin Pathol 1980; 74: 607–619. [DOI] [PubMed] [Google Scholar]
- 3.Shin SL, Outwater EK: Benign large cell calcifying Sertoli cell tumor of the testis in a prepubescent patient. AJR Am J Roentgenol 2007; 189: W65–W66. [DOI] [PubMed] [Google Scholar]
- 4.Li G, Lee MS, Kraft KH, Heider A: Prepubertal malignant large cell calcifying Sertoli cell tumor of the testis. Urology 2018; 117: 145–149. [DOI] [PubMed] [Google Scholar]
- 5.Kratzer SS, Ulbright TM, Talerman A, Srigley JR, Roth LM, Wahle GR et al.: Large cell calcifying Sertoli cell tumor of the testis: contrasting features of six malignant and six benign tumors and a review of the literature. Am J Surg Pathol 1997; 21: 1271–1280. [DOI] [PubMed] [Google Scholar]
- 6.De Raeve H, Schoonooghe P, Wibowo R, Van Marck E, Goossens A: Malignant large cell calcifying Sertoli cell tumor of the testis. Pathol Res Pract 2003; 199: 113–117. [DOI] [PubMed] [Google Scholar]
- 7.Tyloch JF, Wieczorek AP: Standards for scrotal ultrasonography. J Ultrason 2016; 16: 391–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carucci LR, Tirkes AT, Pretorius ES, Genega EM, Weinstein SP: Testicular Leydig’s cell hyperplasia: MR imaging and sonographic findings. AJR Am J Roentgenol 2003; 180: 501–503. [DOI] [PubMed] [Google Scholar]
- 9.Coursey Moreno C, Small WC, Camacho JC, Master V, Kokabi N, Lewis M et al.: Testicular tumors: what radiologists need to know – differential diagnosis, staging, and management. Radiographics 2015; 35: 400–415. [DOI] [PubMed] [Google Scholar]
- 10.Kałużny A, Matuszewski M, Wojtylak S, Krajka K, Cichy W, Pławski A et al.: Organ-sparing surgery of the bilateral testicular large cell calcifying Sertoli cell tumor in patient with atypical Peutz–Jeghers syndrome. Int Urol Nephrol 2012; 44: 1045–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]