Abstract
Syphilis rates and trends vary by population subgroup. Among men who have sex with men (MSM), rates of primary and secondary (P&S) syphilis are high throughout the United States (228.8 per 100,000 in 2013). P&S syphilis among women is much less common (0.9 per 100,000 in 2013) and occurs in isolated outbreaks plus in a few counties with persistent low levels of infection. Congenital syphilis trends closely follow P&S trends among women. These trends have implications for prevention. Routine screening among MSM can prevent tertiary syphilis, but despite interventions, rates of infection continue to rise among MSM and will soon approach those last seen in 1982 (estimate: 340.7 per 100,000). Control of syphilis among women is possible and important because it often leads to congenital syphilis. Outbreaks among heterosexuals can be halted by intensive screening, treatment, and partner notification.
Keywords: Syphilis, congenital syphilis, epidemiology, prevention, surveillance, men who have sex with men
In 2012, syphilis in the United States reached a 13-year high (in adults) and an all-time low (in newborns).1 Case reports of primary and secondary (P&S) syphilis in adults have increased every year between 2000 and 2012, from 5,979 to 15,667. At the same time, congenital syphilis reports decreased from 580 to 322, the lowest number of reported cases since the case definition was changed in 1988. The divergent trends in adult and congenital syphilis exemplify the complex epidemiology of syphilis in the United States.
Syphilis trends are often quite different in population subgroups. Rates of P&S syphilis were rising among men who have sex with men (MSM) even before the syphilis elimination plan was drafted in 1999,2 but trends among MSM were difficult to detect because they were hidden by continuing decreases in rates among heterosexuals.3 Syphilis case report data at the national level did not include sex-of-sex-partner information until 2005 and that variable is still incompletely reported from some areas. Ironically, trends in syphilis among heterosexuals are now easily missed because they are hidden by the very large number of cases occurring among MSM. Increases in syphilis among women are important because they are followed by increases in congenital syphilis. Local trends can be hidden when data from all areas of the country are combined in one summary trend. Small areas can have big outbreaks that are obscured in national data because trends are dominated by numbers from large cities. Obscured outbreaks are a problem because diagnosing, treating, and preventing syphilis involve decisions based on the local epidemiology.4
In this paper we examine trends in P&S syphilis in key subgroups. We estimate trends among MSM since 1963 using an approach based on the male:female rate ratio.5 We look at trends since 2003 among women, and the relationship of trends in women to trends in congenital syphilis. Finally, we look at county level data to see how national and county trends differ. These findings, and a review of the literature, help inform priorities for syphilis control efforts.
Methods
We analyzed P&S syphilis case data reported to CDC during 1963–2013, and congenital syphilis case data reported during 1995–2012. Reports have included sex of cases since 1963, and both sex and age of cases since 1983. County of residence of cases has been available since 2003. We also reviewed the literature on syphilis epidemiology in the United States using the PubMed search terms “syphilis United States,” focusing on reports from the past 10 years and on reports from the 1969–1982 syphilis epidemic among MSM.
In adults, syphilis is reported by stage at the time of diagnosis.1 Traditionally, syphilis trends are described using cases detected during the primary and secondary stages (P&S). These most accurately reflect recent infection and are less susceptible to changes in screening rates because (presumably) cases are detected due to signs and symptoms. Latent syphilis cases have no signs or symptoms, and are classified as early latent when there is specific evidence that the infection was acquired within the year before diagnosis, and late latent if there is no such evidence. P&S represents only about one-quarter of syphilis diagnoses because it does not include the infections detected in the latent stages.1 We limited our epidemiologic analysis here to P&S syphilis case reports, as they most likely represent recently acquired infections.
Congenital syphilis is more difficult to diagnose because maternal antibody crosses the placenta and not all infants who have antibody are truly infected with Treponema pallidum. Untreated congenital syphilis is a debilitating infection, so the consequences of over-treatment are small compared to the risk of under-treatment. In 1988 the surveillance case definition was changed to be highly-sensitive, but not specific, in order to not miss cases. Briefly, a case is considered to be congenital syphilis if a mother has inadequately treated syphilis at delivery, or if the child has specific evidence of syphilis.1
The true extent of syphilis among MSM has been difficult to monitor because national case report data did not include sex-of-sex-partner information until 2005 and reports are still incomplete in some areas. An earlier paper estimated the number of cases that were MSM in 2000–2003 using the male:female case ratio of P&S, and assuming there were no MSM with syphilis in 1998.5 We used a similar approach, using the male:female rate ratio and assuming there were no MSM with syphilis in 1994, the year with the lowest male:female rate ratio (1.1236). Using the formula, [(male:female rate ratio - 1.1236) / male:female rate ratio], we calculated the proportion of male cases that were MSM, and that proportion was used to estimate the number of cases that were MSM. We then estimated the rate of syphilis among MSM by assuming that 3.9% of men were MSM, based on several studies that asked men about same-sex contact within the past 5 years.6
Results
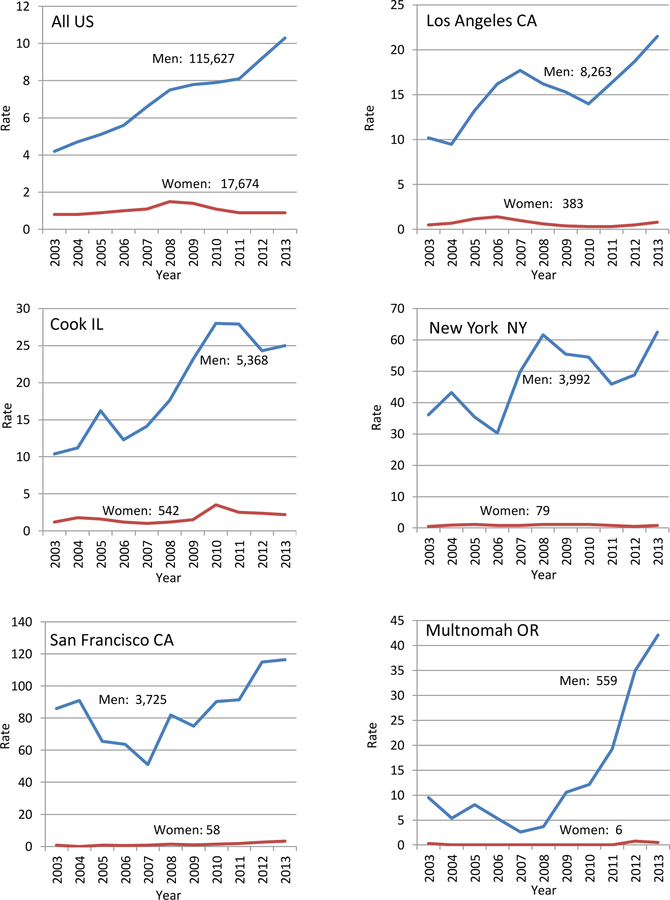
Primary and secondary syphilis rates in the United States have varied considerably since 1963 (Figure 1a). The male:female rate ratio has been rapidly increasing since 2000, reaching the highest level ever recorded (11) in 2013. Using the male:female rate ratio, the estimated percent of male cases that were MSM was: 25.1 in 2000, 78.2 in 2008, and 89.7 in 2013 (Figure 1b). Assuming 3.9% of men were MSM6 every year, the rate of P&S syphilis for MSM (per 100,000 MSM) was: 15.8 in 2000, 146.5 in 2008, and 228.8 in 2013 (Figure 1c). In 2013, the rate for MSM was 243 times the rate for women (0.94 per 100,000 women) and 214 times the rate for heterosexual men (1.07 per 100,000 heterosexual men). During 1963–2013, we estimate that syphilis among MSM peaked at 15,820 cases in 1982. Assuming that 3.9% of men were MSM in 1982, then the rate of infection was 340.7 per 100,000 or about 1.5 times the rate in 2013 (228.8 per 100,000).
1a.
Primary and secondary syphilis cases per 100,000 population, by sex, and the male:female rate ratio, United States, 1963–2013.
1 b.
Estimated cases of Primary and Secondary Syphilis among men who have sex with men (MSM), men who have sex with women only (MSW), and women, United States, 1963–2013.
1 c.

Estimated annual rate of primary and secondary syphilis among men who have sex with men (MSM), men who have sex with women only (MSW), and women, United States, 1963–2013. The curves for MSW and women overlap.
Those estimated rates were calculated using data for all ages combined because national syphilis data were not available by both age and sex until 1983. They underestimate the rates for sexually active MSM because the denominators include males of all ages, and many males in some age groups are unlikely to be sexually active. Restricting our analysis to men aged 15 and older, the rates (per 100,000 MSM) were 20.6 in 2000, 180.9 in 2008, and 282.2 in 2013. Further restricting to men ages 15–54, the rates for MSM were 23.0 in 2000, 255.5 in 2008, and 404.7 in 2013.
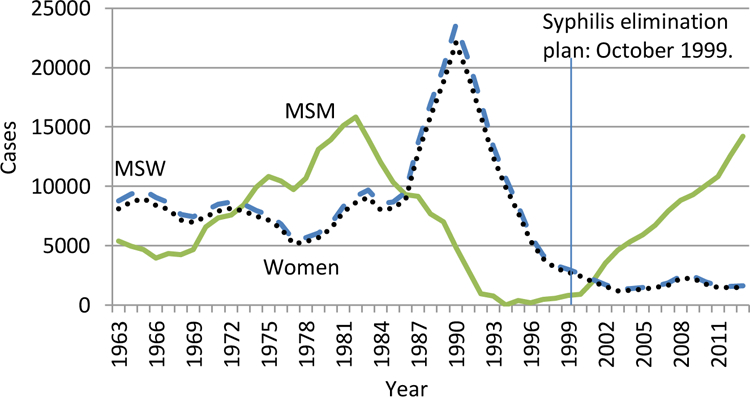
Trends in congenital syphilis mirror trends in P&S among women. (Figure 2) The risk of congenital syphilis is very high when women have syphilis. Since 1995, there has been, on average, one case of congenital syphilis for every 4.5 women with P&S syphilis. As P&S syphilis among women decreased from 7,779 cases in 1995 to 1,458 cases in 2012, the number of congenital syphilis cases also fell from 1,863 to 322.
2.

Women with primary and secondary syphilis and cases of congenital syphilis, by year, United States, 1995–2012.
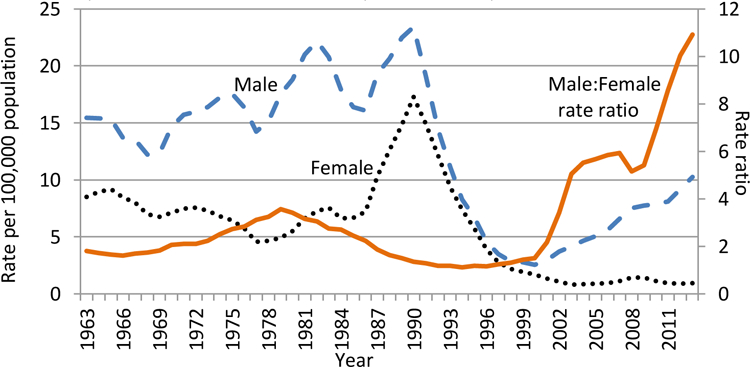
The rate of P&S syphilis also varied by geographic location. Between 2003 and 2013, every state, and the District of Columbia, had an increase in cases among men for the most recent 5 years (2009–2013) compared to the first 5 years (2003–2007), and 31 areas also had slight increases among women. Despite this apparent uniform increase in cases among men across states, different counties had vastly different experience with P&S syphilis. Of 3142 counties in the US, 2123 (67.6%) reported no P&S syphilis in 2012. Half of reported P&S syphilis in the US came from 27 counties, which contained 19.6% of the U.S. population in 2012. Among US counties, 436 (13.9%) averaged at least 2 cases of P&S per year for the 10-year period ending in 2012, and only 47 counties (1.5%) averaged at least 1 case per week during that time.
Trends for the four counties that reported the most P&S syphilis cases between 2003 and 2013 varied considerably from each other, and from national trends (Figure 3). These counties (Los Angeles, Cook, New York, and San Francisco) have had large increases in rates of P&S syphilis among MSM, as demonstrated by the high rates among men and the relatively low rates among women. Although these counties all show an increase among men during this interval, the timing of the increases was quite different. For example, in San Francisco, rates decreased during 2005–2007 then increased, whereas the opposite occurred in Los Angeles. Many other counties have had later increases in syphilis among MSM. For example, in Multnomah County, the increase began in 2009 and continued through 2013.
3.
Rates of primary and secondary among men and women, per 100,000, in the United States and select U.S. counties, 2003–2013 (with total number of cases). Scale varies.
Some counties have had high rates of P&S syphilis among women (Figure 4). Most often, these counties have had sharp increases followed by decreases. Perhaps the most striking example is Jefferson County, TX, where there was no reported P&S syphilis among women in 2003 or 2004, 140 cases during 2008–2009, and 2 cases in 2013. Jefferson County, AL, had a more gradual increase and then decreased, going from 3 cases in 2003 to 236 during 2006–2008, before falling back to 3 cases in 2013. Some of these counties have had heterosexual epidemics in the midst of increases among MSM. For example, in Jefferson County, AL, the male:female rate ratio was 2 or less in 2004–2008, but was 17.4 in 2013. Baltimore (city), MD has had high (though gradually decreasing) rates among women and high (recently increasing) rates among men.
4.
Rates of primary and secondary among men and women, per 100,000, in select U.S. counties, 2003–2013 (with total number of cases). Scale varies.
Discussion
Syphilis among MSM is on the rise across the United States. In many places, rates have been increasing dramatically since 2000, shortly after the advent of HAART was announced at the HIV/AIDS conference in Vancouver in 1996. Our analysis allowed us to estimate the number of syphilis cases, and case rates, for MSM. When we examined historic data, we were surprised to see that rates among MSM were much higher in the 1970’s than they were in 2013. According to our estimates, the previous epidemic among MSM began rising just before the time of the Stonewall riot (June of 1969) and reached a peak 15 years later in 1982. Papers written at the time reported that syphilis was an increasing problem among MSM, though there were no good estimates of the size of the MSM population to allow estimation of rates.7 The increase between 1967 and 1979 was accompanied by a 351% increase in cases among white males reported by public clinics, and the male-to-female case ratio doubled, from 1.5 to 3.8 Dramatic decreases in syphilis during the early years of the AIDS epidemic were thought to be due to a combination of behavior change among MSM and deaths of the persons at highest risk for syphilis.9 The previous MSM syphilis epidemic happened many years ago. However, if recent trends go unchecked, rates will soon surpass the peak that occurred in 1982.
Our estimates certainly contain errors due to the assumptions that 3.9% of all men are MSM and that no MSM acquired syphilis in 1998, however, reasonable changes in these assumptions would have little effect on the estimates. Other investigators have recently collected information on sex-of-sex-partners of persons with syphilis, and their estimated rates are similar to ours. Analyses of 2008 P&S syphilis data from 27 states found 89.3% of the 6,176 male cases reported sex-of-sex-partner information, and 76.7% of male cases were classified as MSM.10 In this paper, we estimated that 78.2% of all male P&S syphilis cases were MSM for the entire United States in 2008. Analysis of data from 39 states and Washington DC in 2008, found sex partner information was available for 86.5% and estimated that the rate of syphilis (per 100,000) was 154 for MSM and 2.2 for other men.6 A study from New York City in 2008, estimated rates for 18–64 year-old MSM to be 707 per 100,000 MSM, 147 times the rate for MSW (4.8).11 Our corresponding 2008 estimates for 15–54 year old men in the United States were 255.5 for MSM and 2.9 for MSW. By 2013 these estimated rates had changed to 404.7 for MSM and 1.9 for MSW, a MSM:MSW rate ratio of 213. While these methods varied, all estimated rates of P&S syphilis for MSM were over 70 times the rates for heterosexual males, and the disparity has since increased.
True rates of syphilis are even higher than these estimates for P&S. Because only one quarter to one third of syphilis is diagnosed in the P&S stages,1 the rate of any syphilis infection is likely to be three or four times higher than the 404.7 estimate for 15–54 year old MSM. This rate is high enough to be listed as a percentage (1.2–1.6) rather than as per 100,000 (1,200–1600). The rates of syphilis would be higher still for other subgroups of MSM. Our data did not allow estimation of syphilis among MSM by race, however, syphilis rates have been increasing the most among all young black men.1 Between 2004 and 2008, syphilis diagnoses increased among young black men in 70% of large metropolitan areas and HIV among black MSM increased in 85% of areas.12 Using reported data from 27 states in 2008, the rate for MSM aged 25–34 was 1.8 times the rate of all MSM (over age 12), and the rate for black MSM was estimated to be 2.3 times the rate for all MSM in the US.6 In New York City, the rate of P&S for 18–64 year old MSM was 0.7% but the rate for MSM aged 18–29 was 1.4% and the rate for black MSM was 2.4%.11
Rates of syphilis have been particularly high among HIV-infected MSM. In California, during 2002–2006, 52.7% of MSM diagnosed with P&S syphilis had HIV co-infection.13 A study in Seattle estimated 4% of HIV-infected MSM acquired syphilis in 2011.14 One study used remnant sera from men with P&S syphilis diagnosed in Atlanta, San Francisco, and Los Angeles and tested for evidence of recent seroconversion and the estimated that 10.5% of MSM with P&S syphilis had recently acquired HIV.15 If MSM with syphilis are not already infected with HIV, chances are very high that they will acquire it. A study of men diagnosed with early syphilis in Florida in 2003 found 21.5% were reported with new HIV infection by the end of 2011.16
Some MSM acquire syphilis repeatedly. In California, 300 (10%) of 3,000 MSM with P&S reported between 2002 and 2006 had a repeat early syphilis infection reported within 2 years.13 In South Florida in 2008, 10% of all persons diagnosed with early syphilis had a previous syphilis diagnosis between 2000 and 2008.17 In San Diego, between 2004 and 2007, 11.7% of MSM with early syphilis had another syphilis diagnosis within 2 years.18 This concentration of syphilis and HIV among MSM may be increasing. In Baltimore, during 2007–2011, of 460 MSM with early syphilis, 20% had syphilis more than once, and 86% of those with repeat diagnoses had HIV by the time of their latest syphilis diagnosis.19 Our analysis did not consider repeat infections, therefore, the number of individuals infected with syphilis might be fewer than the number of reported infections. Identification of persons repeatedly infected with syphilis might help control transmission in specific populations.20
Controlling syphilis among MSM has been challenging. We found no papers in the literature that described interventions that successfully decreased syphilis rates among MSM. In the 1970’s there were calls for gay-friendly services to decrease stigma,7, 21, 22 and screening in bars and bathhouses found some infections.23, 24 However, investigators noted that “the population is very large, and our efforts must be viewed more as surveillance than as control programs.”23 Screening can help limit progression to disease. Monthly syphilis screening was recommended for MSM at high risk, but there was no indication of how many men were tested.24 The prevalence of stigma has decreased somewhat since the 1970’s, but it remains an important issue.25 In the current MSM epidemic, high screening coverage for HIV-infected MSM can be achieved by routinely testing for syphilis whenever a viral load or CD4 test is done.26, 27 However, many HIV clinics have not established routine testing, and their screening rates remain low.28–30 It is more difficult to screen MSM who are not receiving routine health care. In San Francisco, a survey of high-risk MSM in 2012 found 37.5% reported they had been screened within the previous 3 to 6 months.31
Although most syphilis is now occurring among MSM, most serious complications of syphilis are still related to syphilis among women because of the link to congenital syphilis. For adults, the morbidity caused by infection with Treponema pallidum has changed considerably in the antibiotic era. In the 1930’s the death rate from syphilis among adults in the United States was 16 per 100,00032 which approximates the diagnosis rate in 2012 (16.0 for all ages, all stages)1 and the diagnosis rate for HIV in 2011 (15.8 for all ages).33 Nowadays, syphilis rarely kills an adult,34 though up to 1–2% may develop symptomatic early neurosyphilis.35, 36 In contrast, the likelihood of transmission during pregnancy and the consequences of congenital infection have not changed; 66.5% of women with untreated syphilis will have an adverse outcome of pregnancy, including 25.6% who will have a stillbirth.37 Thus, compared with disease in adults, the relative importance of congenital infection is higher than in the past.
Congenital syphilis is partly controlled by routine serologic screening of all pregnant women during their first prenatal visit, which is widely recommended.4, 38 Universal screening can detect and cure many, but not all, infections because some women acquire infection after the initial test, some who are detected are not treated, and some women do not seek care until late in pregnancy.39 In communities in which the risk for congenital syphilis is high, serologic testing and a sexual history should also be obtained at 28 weeks’ gestation and at delivery.5 This approach requires that providers know when the risk is high, and even in an area where three tests were required by law, only 9% of pregnant women were tested three times.40 Clearly, the most effective way to prevent transmission during pregnancy is to prevent infection in women.
Outbreaks of syphilis among women have often been stopped by an intensive public health response. An outbreak among American Indians in Arizona during 2007–2009 involved 69 women and 6 congenital cases (including 2 stillbirths).41 Rates gradually decreased after educating providers and the public, increasing screening in clinics and targeted venues, and emphasizing notifying and treating sex partners. The epidemic in Jefferson County, AL lasted longer, with a small increase in 2004 followed by larger increases during 2005–2006. After clinic hours were increased, partner notification interviews were expanded, and community education campaign was conducted,42 rates decreased slightly during 2007–2008 followed by a sustained decline in 2009–2011. Some areas, like Baltimore continue to have high rates of P&S syphilis among women, whereas other areas (like Jefferson, TX or Jefferson, AL) have had high rates of syphilis among women in the past, but now have lower rates. The near elimination of syphilis among women in some areas suggests it might be possible in others. Determining why syphilis rates declined among women in some areas may help reduce rates in areas where they remain high. The rate of P&S among women in the United States, 0.9 per 100,000, is still about twice the level considered the target for successful syphilis elimination.2
Syphilis in the United States is on the rise in some subgroups but not in others. Most syphilis cases, by far, are occurring among MSM who comprise a relatively small percentage of the population. Screening can identify most of these infections before they progress to tertiary syphilis, and thus prevent most complications. Routine, opt-out syphilis testing added to HIV viral load testing has increased screening in some clinics to 87% and identified many infections where it was implemented, yet screening in other clinics is still risk-based and much less successful (22%).27 Additional approaches are needed to reach MSM who are not routinely receiving medical care. The epidemic of 1967–1982 suggests rates among MSM may continue to increase. Congenital syphilis is less common than ever, but is devastating when it occurs. The most effective way to prevent congenital syphilis is to prevent syphilis among women.
Expert commentary & five-year view
Current increases in P&S syphilis among MSM are reminiscent of increases that started in 1969. Rates of P&S syphilis may have climbed even higher, were they not interrupted in 1982 by the AIDS epidemic. Unless effective interventions are identified and implemented to prevent syphilis among MSM, the current increases in P&S syphilis will likely continue. In contrast, P&S syphilis among heterosexuals has been occurring at low rates in most of the US since the late 1990’s, with the exception of occasional outbreaks. Many heterosexual outbreaks have been controlled by intensive interventions. One consequence of heterosexual syphilis—congenital syphilis—has rates that mirror rates of P&S syphilis among women, suggesting we could reduce rates of congenital syphilis even further by intensifying interventions that prevent syphilis among women.
Key issues.
Rates of primary and secondary (P&S) syphilis among men who have sex with men (MSM) greatly exceed the rates of P&S syphilis among women and heterosexual men, and have been rising across the U.S. since the late 1990’s.
If rates of P&S syphilis among MSM continue to increase they will soon reach levels last seen in 1982, at the beginning of the AIDS epidemic.
In contrast, national rates of P&S syphilis among heterosexuals are currently low, although local rates vary.
When heterosexual outbreaks occur, congenital infections soon follow.
Congenital syphilis can be prevented by intensive interventions that have been successful in stopping outbreaks among heterosexuals.
Efforts to control syphilis in the United States should be targeted to the at-risk populations. Partner notification is currently more effective in heterosexual epidemics, while routine screening effectively identifies many infections among MSM.
References
- 1.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2012 Atlanta: U.S. Department of Health and Human Services; 2013, pp 79–80. [Google Scholar]
- 2.Centers for Disease Control and Prevention. The national plan to eliminate syphilis from the United States. 1999 Available at http://www.cdc.gov/stopsyphilis/Plan.pdf.
- 3.Centers for Disease Control and Prevention. Primary and secondary syphilis—United States, 1999. MMWR 2001;50:113–117. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2010, MMWR 2010;59(no.RR-12) pp. 26–36. [Google Scholar]
- 5.Heffelfinger JD, Swint EB, Berman SM, Weinstock HS. Trends in primary and secondary syphilis among men who have sex with men in the United States. Am J Public Health 2007;97:1076–1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Purcell DW, Johnson CH, Lansky A, et al. Estimating the population size of men who have sex with men in the United States to obtain HIV and syphilis rates. Open AIDS J 2012;6(Suppl1:M6)98–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Darrow WW, Barrett D, Jay K, Young A. The gay report on sexually transmitted diseases. AJPH 1981;71:1004–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fichtner RR, Aral SO, Blount JH, Zaidi AA, Reynolds GH, Darrow WW. Syphilis in the United States: 1967–1979. Sex Transm Dis 1983;10:77–80. [DOI] [PubMed] [Google Scholar]
- 9.Chesson HW, Dee TS, Aral SO. AIDS mortality may have contributed to the decline in syphilis rates in the United States in the 1990s. Sex Transm Dis 2003;30:419–424. [DOI] [PubMed] [Google Scholar]
- 10.Su JR, Beltrami JF, Zaidi AA, Weinstock HS. Primary and secondary syphilis among black and Hispanic men who have sex with men: case report data from 27 states. Ann Intern Med 2011;155:145–151. [DOI] [PubMed] [Google Scholar]
- 11.Pathela P, Braunstein SL, Schillinger JA, Shepard C, Sweeney M, Blank S. Men who have sex with men have a 140-fold higher risk for newly diagnosed HIV and syphilis compared with heterosexual men in New York City. J Acquir Immune Defic Syndr 2011;58:408–416. [DOI] [PubMed] [Google Scholar]
- 12.Torrone EA, Bertolli J, Li J, et al. Increased HIV and primary and sexondary syphilis diagnoses among young men—United States, 2004–2008. J Acquir Immune Defic Syndr 2011;58:328–335. [DOI] [PubMed] [Google Scholar]
- 13.Cohen SE, Chew Ng RA, Katz KA, Bernstein KT, et al. Repeat syphilis among men who have sex with men in California, 2002–2006: implications for syphilis elimination efforts. Am J Public Helath 2012;102:No.1,e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kerani RP, Golden MR. 2011. King county sexually transmitted diseases epidemiology report p 28 http://www.kingcounty.gov/healthservices/health/communicable/std/statistics.aspx Accessed April 7, 2014.
- 15.Buchacz K, Klausner JD, Kerndt PR, et al. HIV incidence among men diagnosed with early syphilis in Atlanta, San Francisco, and Los Angeles, 2004 to 2005. J Acquir Immune Defic Syndr 2008;47:234–240. [PubMed] [Google Scholar]
- 16.Peterman TA, Newman DR, Maddox L, Schmitt K, Shiver S. High risk for HIV following syphilis diagnosis among men in Florida 2000–2011. Pub Health Rep 2014;129:164–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brewer TH, Peterman TA, Newman DR, Schmitt K. Reinfections during the Florida syphilis epidemic, 2000–2008. Sex Transm Dis 2011;38:12–17. [DOI] [PubMed] [Google Scholar]
- 18.Katz KA, Lee MA, Gray T, Marcus JL, Pierce EF. Repeat syphilis among men who have sex with men—San Diego County, 2004–2009. Sex Transm Dis 2011;38:349–352. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Notes from the field. Repeat syphilis infection and HIV coinfection among men who have sex with men—Baltimore, Maryland, 2010–2011. Morbid Mortal Weekly Rep 2013;62:649–650. [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenberg D, Moseley K, Kahn R, et al. Networks of persons with syphilis and at risk for syphilis in Louisiana: evidence of core transmitters. Sex Transm Dis 1999;26:108–114. [DOI] [PubMed] [Google Scholar]
- 21.Henderson RH. Improving sexually transmitted disease health services for gays: a national prospective. Sex Transm Dis 1977;4:58–62. [DOI] [PubMed] [Google Scholar]
- 22.Ritchey MG, Leff AM. Venereal disease control among homosexuals: an outreach program. JAMA 1975;232:509–510. [PubMed] [Google Scholar]
- 23.Merino HI, Judson FN, Bennett D, Schaffnit TR. Screening for gonorrhea and syphilis in gay bathhouses in Denver and Los Angeles. Pub Health Rep 1979;94:376–379. [PMC free article] [PubMed] [Google Scholar]
- 24.Bolan RK. Sexually transmitted diseases in homosexuals: focusing the attack. Sex Transm Dis 1981;8:293–297. [PubMed] [Google Scholar]
- 25.Glick SN, Golden MR. Persistence of racial differences in attitudes toward homosexuality in the United States. J Acquir Immune Defic Syndr 2010;55:516–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cohen CE, Winston A, Asboe D, et al. Increasing detection of asymptomatic syphilis in HIV patients. Sex Transm Infect 2005;81:217–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guy R, El-Hayek C, Fairley CK, et al. Opt-out and opt-in testing increases syphilis screening of HIV-positive men who have sex with men in Australia. PLoS One 2013:8(8):e71436. doi: 10.1371/journal.pone.0071436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hoover KW, Butler M, Workowski K, et al. STD screening of HIV-infected MSM in HIV clinics. Sex Transm Dis 2010;37:771–776. [DOI] [PubMed] [Google Scholar]
- 29.Zou H, Fairley CK, Guy R, Chen MY. The efficacy of clinic-based interventions aimed at increasing screening for bacterial sexually transmitted infections among men who have sex with men: a systematic review. Sex Transm Dis 2012;39:382–387. [DOI] [PubMed] [Google Scholar]
- 30.Blair JM, Fagan JL, Frazier EL, et al. Behavioral and Clinical Characteristics of Persons Receiving Medical Care for HIV Infection — Medical Monitoring Project, United States, 2009. MMWR 2014;63(No. SS-5):p1. [PubMed] [Google Scholar]
- 31.Katz KA, Raymond HF, Bernstein KT, Klausner JD. Knowledge, attitudes and practices regarding syphilis screening among men who have sex with men in San Francisco. Sex Transm Dis 2013;40:318–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moore JE. An Evaluation of public-health measures for the control of syphilis: an epidemiological study. Lancet 1951. 699–711. [DOI] [PubMed]
- 33.Centers for Disease Control and Prevention. HIV Surveillance Report, 2011; vol. 23 http://www.cdc.gov/hiv/pdf/statistics_2011_HIV_Surveillance_Report_vol_23.pdf Page18 Published February 2013. Accessed July 24, 2014. [Google Scholar]
- 34.McElligott KA. Mortality from sexually transmitted diseases in reproductive-aged women: United States, 1999–2010. Am J Public Health 2014;104:e101–e105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention. Symptomatic early neurosyphilis among HIV-positive men who have sex with men—four cities, United States, January 2002–June 2004. MMWR 2007;56:625–628. [PMC free article] [PubMed] [Google Scholar]
- 36.Taylor MM, Aynalem G, Olea LM, He P, Smith LV, Kerndt PR. A consequence of the syphilis epidemic among men who have sex with men (MSM): neurosyphilis in Los Angeles, 2001–2004. Sex Transm Dis 2008;35:430–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gomez GB, Kamb ML, Newman LM, Mark J, Broutet N, Hawkes SJ. Untreated maternal syphilis and adverse outcomes of pregnancy: a systematic review and meta-analysis. Bull World Health Organ 2013;91:217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wolfe T, Shelton E, Sessions C, Miller T. Screening for syphilis infection in pregnant women: evidence for the U.S. Preventive Services Task Force reaffirmation recommendation statement. Ann Intern Med 2009;150:710–716. [DOI] [PubMed] [Google Scholar]
- 39.Taylor MM, Mickey T, Browne K, Kenney K, England B, Blasini-Alcivar L. Opportunities for the prevention of congenital syphilis in Maricopa County, Arizona. Sex Transm Dis 2008;35:341–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Trepka MJ, Bloom SA, Zhang G, Kim S, Nobles RE. Inadequate syphilis screening among women with prenatal care in a community with a high syphilis incidence. Sex Transm Dis 2006;33:670–674. [DOI] [PubMed] [Google Scholar]
- 41.Centers for Disease Control and Prevention. Syphilis outbreak among American Indians—Arizona, 2007–2009. MMWR 2010;59:158–161. [PMC free article] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention. Primary and secondary syphilis—Jefferson County, Alabama, 2002–2007. MMWR 2009;58:463–467. [PubMed] [Google Scholar]