Abstract
Purpose
Subjective tinnitus is a common symptom with potentially negative impact on quality of life. More research is required to gain a deeper understanding of the disease and its clinical presentation. To estimate the incidence of tinnitus and to describe patient-related characteristics such as lifestyle factors and comorbidities.
Patients and methods
Using the Clinical Practice Research Datalink, we calculated incidence rates of first-time diagnosed tinnitus in an adult population between 2000 and 2016. We stratified incidence rates by sex, age, and year of diagnosis. Additionally, we performed a 1:1 matched case-control study comparing body mass index, lifestyle factors and selected comorbidities between patients with incident tinnitus and tinnitus-free controls.
Results
We identified 109 783 adults with a first-time diagnosis of tinnitus between 2000 and 2016, yielding an overall age-standardized incidence rate of 25.0 new tinnitus cases per 10,000 person-years (95% CI: 24.6–25.5). There was a steady increase in tinnitus incidence throughout the study period. Approximately 80% of tinnitus cases were diagnosed at age 40 years or older. We observed the highest incidence rate in individuals aged 60–69 years (41.2 per 10,000 person-years, 95% CI: 40.7–41.7). Smokers and alcohol drinkers were at lower risk of being diagnosed with tinnitus compared with non-smokers and non-drinkers, respectively. The occurrence of tinnitus was strongly associated with a recent diagnosis of several otological and vestibular disorders as well as head and neck disorders.
Conclusion
The present observational study found an increasing incidence of tinnitus over time, emphasizing the continuously growing health burden. The findings on patient characteristics, lifestyle factors, and selected comorbidities contribute to a better understanding of risk factors for tinnitus.
Keywords: case-control study, clinical practice research datalink, lifestyle factors, incidence rates, tinnitus
Introduction
Patients suffering from subjective tinnitus experience a perception of sound in the absence of an external source. It is a symptom audible only to the patient, and not to the examiner.1–3 The nature of tinnitus varies and is described as ringing, buzzing, clicking, hissing, roaring, humming, or pulsations. The manifestation differs considerably in severity, ranging from mild to very bothersome.4,5 A severe, persistent form commonly introduces comorbidities such as sleep disturbance, anxiety or depression, and as a consequence substantially affect the patients’ quality of life.6–9
Tinnitus is a frequent symptom in the developed world. Nevertheless, there is no universal definition, and as a result epidemiological studies report a wide range of prevalences extending from 5.1% to 42.7%.10 In the United Kingdom (UK), a large observational study reported an incidence rate of 5.4 cases of clinically significant tinnitus per 10,000 person-years,11 and another study estimated the annual healthcare burden of tinnitus-related costs to be £750 million in the National Health Service (NHS).12 A similar study in the Netherlands attributed €1.9 billion of direct health care costs to tinnitus, whereas the total cost of illness (health care costs, productivity losses, and out-of-pocket costs) was considerably higher amounting to €6.8 billion.13
The pathophysiology of tinnitus is not fully understood,14 however, there has been remarkable progress in recent years. Results from animal studies, mainly in rodents, complemented by imaging studies in humans suggest various underlying mechanisms affecting auditory and non- auditory brain areas, as well as the interaction between the auditory and the somatosensory structures.15,16 Based on these pathophysiological concepts, various therapeutic compounds (mostly approved for other indications) were tested in tinnitus patients. Despite this substantial effort, clear evidence for an effective pharmacological treatment is still lacking.16–18 The difficulty to demonstrate replicable significant clinical benefit may be explained by the heterogeneity of tinnitus (in terms of perception, distress, concomitant comorbidities and risk factors, as well as the underlying etiology).19–21 Thus, to date guidelines do not recommend any specific drug therapy.2,15
More research is required to gain a deeper understanding of the disease and a better characterization of affected patients, including lifestyle factors and common comorbidities
In this population-based study, we estimate the incidence of tinnitus recorded by general practitioners (GPs) in the UK from January 2000 to December 2016, and describe patient-related characteristics with respect to demography, lifestyle factors and comorbidities compared with persons without tinnitus.
Materials and methods
Data source
We used primary care data derived from the Clinical Practice Research Datalink (CPRD) obtained under license from the UK Medicines and Healthcare products Regulatory Agency (MHRA). The CPRD is an anonymized database created in 1987 that contains ongoing medical records from over 11 million patients provided by approximately 700 GP practices throughout the UK.22 Recorded data include patients’ demographics, lifestyle factors, diagnoses, signs and symptoms, treatments, test results, and referrals to secondary care.22–24 CPRD patients represent the general UK population with respect to sex, age and ethnicity.22 Several studies have reported on the high quality and validity of the database.23,25,26 The Independent Scientific Advisory Committee (ISAC) for Medicines and Healthcare products Regulatory Agency database research (MHRA) approved the study (protocol number: 18_024R) and the study protocol was available to the journal and reviewers.
Study design and study population
We established two separate study populations. First, we conducted a retrospective cohort study to quantify incidence rates (IRs) of first-time diagnosed tinnitus. Therefore, we included all adult patients who were present in the CPRD population between 2000 and 2016 and who had a minimum active history in the CPRD of 3 years prior to cohort entry. We excluded patients if they had a recorded diagnosis for malignant cancer or HIV/AIDS prior to cohort entry.
Second, we conducted a separate case-control study, for which we identified all patients in the CPRD with a first-time Read code for tinnitus at the age of 18 years or older between January 1st, 2000 and December 31st, 2016 (cases). Like in the cohort study, we excluded all patients with less than three years of recorded history in the CPRD prior to the date of the first tinnitus diagnosis (index date) to minimize outcome misclassification be including prevalent tinnitus cases. In addition, we again excluded patients with any record of malignancy or HIV/AIDS prior to the index date, as these patients may receive specialized care and often suffer from various additional comorbidities.
We matched each tinnitus case to a randomly selected control patient who did not have a recorded diagnosis for tinnitus in the CPRD medical record. Cases and controls were matched on sex, age, general practice, years of history in the CPRD, and calendar time and we applied the same exclusion criteria to controls as we did to cases.
Statistical analysis
In the cohort analysis, we calculated crude and age-standardized IRs (ASR) of first-time diagnosed tinnitus in the CPRD population by dividing the total number of incident tinnitus diagnoses by the person-years (PY) at risk overall as well as stratified by age, sex, and year of diagnosis. We assessed PY at risk by summing-up person-time between cohort entry and the end of follow-up, which was defined as the earliest out of the day of a first-time diagnosis of tinnitus diagnosis, death, leaving the practice, or December 31st, 2016. Age-standardization was performed using the European Standard Population published in 2013 by Eurostat, the Statistical Office of the European Union.27
In the case-control analysis we conducted conditional logistic regression analyses to calculate odds ratios (ORs) with 95% confidence intervals (CIs) for the following exposure groups: BMI (<18.5, 25.0–29.9, ≥30.0, and 30.0–34.9, 35.0–39.9, ≥40 kg m−2, unknown, compared to normal BMI [18.5–24.9 kg m−2]), smoking (ex-smokers, current smokers, unknown smoking status compared to non-smokers) and alcohol consumption (ex-drinkers, current drinkers subdivided in units per week, unknown status, compared to non-drinkers). Furthermore, we investigated the association between tinnitus and selected comorbidities (systemic somatic diseases and neurological/psychological disorders, otological and vestibular disorders, and head and neck disorders) overall as well as stratified by sex. For otological or vestibular disorders as well as for head and neck disorders, we also considered the amount of time between the last record of the respective condition and the index date (≤30, 31–360 days or >360 days prior to (including) the index date). All covariates were assessed prior to the index date.
We adjusted all OR for smoking, alcohol consumption, and BMI. We did not adjust for any other comorbidities due to the descriptive nature of this analysis.
For confidentiality reasons, we do not provide the number of patients in categories containing less than five patients.
We performed all analyses using SAS 9.4 software (SAS Institute, Cary, North Carolina, USA). Statistical significance was set at the alpha level of 0.05.
Results
Characteristics of the study population
We identified 109,783 adults with a first-time recorded Read code for tinnitus between January 2000 and December 2016. There was a similar number of males and females. The mean age was 54.7 years (standard deviation [SD] ±15.9), though women were slightly older than men at the time of diagnosis (55.7 [SD ±16.5] and 53.6 [SD ±15.2] years, respectively). Approximately two thirds of the tinnitus cases were between 40 and 69 years of age at first recording of tinnitus (Table 1).
Table 1.
Distribution of patient characteristics and lifestyle factors in patients with tinnitus and their matched controls
| Tinnitus cases (%) | Tinnitus-free controls (%) | OR crude (95% CI) | OR adjusteda (95% CI) | |
|---|---|---|---|---|
| Sex | ||||
| Male | 53,874 (49.1) | 53,874 (49.1) | NA | NA |
| Female | 55,909 (50.9) | 55,909 (50.9) | NA | NA |
| Age (years) | ||||
| <20 | 1097 (1.0) | 1100 (1.0) | NA | NA |
| 20–29 | 7118 (6.5) | 7109 (6.5) | NA | NA |
| 30–39 | 11,757 (10.7) | 11,757 (10.7) | NA | NA |
| 40–49 | 19,454 (17.7) | 19,476 (17.7) | NA | NA |
| 50–59 | 26,247 (23.9) | 26,233 (23.9) | NA | NA |
| 60–69 | 24,097 (22.0) | 24,122 (22.0) | NA | NA |
| 70–79 | 13,860 (12.6) | 13,823 (12.6) | NA | NA |
| ≥80 | 6153 (5.6) | 6163 (5.6) | NA | NA |
| BMI (kg/m2) | ||||
| 12.0–18.4 | 1561 (1.4) | 1634 (1.5) | 0.88 (0.82–0.95) | 0.91 (0.84–0.97) |
| 18.5–24.9 | 36,055 (32.8) | 33,901 (30.9) | 1.00 (reference) | 1.00 (reference) |
| 25.0–29.9 | 36,138 (32.9) | 32,981 (30.0) | 1.04 (1.02–1.06) | 1.02 (1.00–1.04) |
| 30.0–60.0 | 21,853 (19.9) | 22,157 (20.2) | 0.94 (0.91–0.96) | 0.91 (0.89–0,94) |
| 30.0–34.9 | 14,876 (13.6) | 14,847 (13.5) | 0.95 (0.93–0.96) | 0.93 (0.90–0.96) |
| 35.0–39.9 | 4794 (4.4) | 4917 (4.5) | 0.93 (0.89–0.97) | 0.90 (0.86–0.94) |
| 40.0–60.0 | 2183 (2.0) | 2393 (2.2) | 0.87 (0.82–0.92) | 0.83 (0.79–0.89) |
| Unknown | 14,176 (12.9) | 19,110 (17.4) | 0.64 (0.62–0.66) | 0.78 (0.75–0.80) |
| Smoking status | ||||
| Non-smoker | 53,513 (48.7) | 50,517 (46.0) | 1.00 (reference) | 1.00 (reference) |
| Ex-smoker | 32,952 (30.0) | 29,321 (26.7) | 1.08 (1.06–1.10) | 1.08 (1.06–1.10) |
| Current smoker | 18,334 (16.7) | 21,904 (20.0) | 0.78 (0.76–0.79) | 0.78 (0.76–0.80) |
| Unknown | 4984 (4.5) | 8041 (7.3) | 0.51 (0.49–0.53) | 0.68 (0.65–0.71) |
| Alcohol consumption | ||||
| Non-drinker | 17,399 (15.9) | 16,062 (14.6) | 1.00 (reference) | 1.00 (reference) |
| Ex-drinker | 2308 (2.1) | 2005 (1.8) | 1.07 (1.00–1.14) | 1.09 (1.03–1.17) |
| Current drinker (units/week) | ||||
| 1–9 | 29,403 (26.8) | 27,743 (25.3) | 0.97 (0.95–1.00) | 0.96 (0.93–0.98) |
| 10–19 | 12,159 (11.1) | 11,971 (10.9) | 0.93 (0.89–0.96) | 0.91 (0.88–0.94) |
| ≥20 | 9132 (8.3) | 9462 (8.6) | 0.87 (0.84–0.90) | 0.88 (0.84–0.91) |
| unknown | 28,443 (25.9) | 27,281 (24.9) | 0.95 (0.93–0.98) | 0.95 (0.92–0.98) |
| Unknown | 10,939 (10.0) | 15,259 (13.9) | 0.59 (0.57–0.62) | 0.74 (0.71–0.77) |
Notes: aAdjusted for BMI category, smoking status, alcohol consumption.
Abbreviations: BMI, body mass index; CI, confidence interval; NA, not applicable; OR, odds ratio.
Incidence rates (IRs)
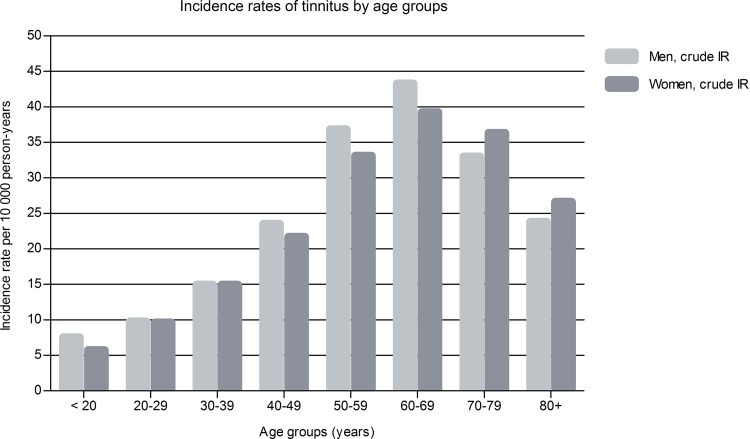
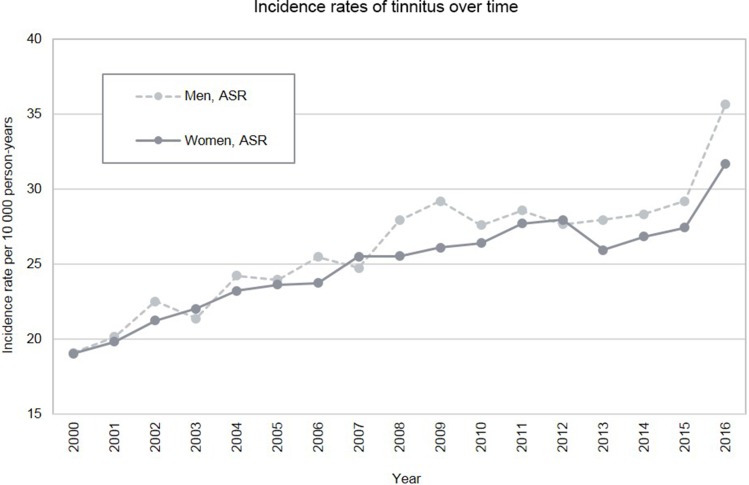
Age-standardized IR (ASR) of first time GP-recorded tinnitus was 25.0 per 10,000 PY (95% CI: 24.6–25.5), and rates were similar for men (ASR of 25.7, 95% CI: 25.0–26.4) and women (ASR 24.7, 95% CI: 24.0–25.3 per 10,000 PY). The IRs increased with age and were highest in the age group 60–69 years (41.2 per 10,000 PY, 95% CI: 40.7–41.7, Figure 1). During the course of the study period, we found a steady increase in the incidence of tinnitus, which was similar in men and women (Figure 2) as well as in younger and older adults (<30 years and ≥30 years of age; data not shown). IRs stratified by sex, age group, and year of diagnosis (age-standardised and crude incidence rates) are provided in the Table S1.
Figure 1.
Age- and sex-specific crude incidence rates (IRs) of tinnitus first-time diagnoses in the United Kingdom from 2000 to 2016.
Figure 2.
Sex-specific and age-standardised incidence rates (ASRs) of tinnitus first-time diagnoses in the United Kingdom from 2000 to 2016.
Note: Standard population from Eurostat.27
Table S1.
Incidence rates of tinnitus diagnosed in the UK between 2000 and 2016
| Number of PY at risk | Number of tinnitus patients | crude IR per 10,000 PY (95% CI) | ASRa per 10,000 PY (95% CI) | |
|---|---|---|---|---|
| Overall | 4,52,48,312 | 1,09,783 | 24.3 (24.1–24.4) | 25.0 (24.6–25.5) |
| By sex | ||||
| Men | 2,18,41,921 | 53,874 | 24.7 (24.5–24.9) | 25.7 (25.0–26.4) |
| Women | 2,34,06,391 | 55,909 | 23.9 (23.7–24.1) | 24.7 (24.0–25.3) |
| By age (years) | ||||
| <20 | 16,50,985 | 1,097 | 6.6 (6.3–7.0) | NA |
| 20–29 | 73,48,559 | 7,118 | 9.7 (9.5–9.9) | NA |
| 30–39 | 78,78,802 | 11,757 | 14.9 (14.7–15.2) | NA |
| 40–49 | 86,20,883 | 19,454 | 22.6 (22.3–22.9) | NA |
| 50–59 | 75,16,334 | 26,247 | 34.9 (34.5–35.3) | NA |
| 60–69 | 58,51,960 | 24,097 | 41.2 (40.7–41.7) | NA |
| 70–79 | 39,82,409 | 13,860 | 34.8 (34.2–35.4) | NA |
| ≥80 | 23,98,378 | 6,153 | 25.7 (25.0–26.3) | NA |
| By year of diagnosis | ||||
| 2000 | 25,43,654 | 4,646 | 18.3 (17.7–18.8) | 19.1 (17.4–20.9) |
| 2001 | 26,44,954 | 5,049 | 19.1 (18.6–19.6) | 18.3 (16.7–20.0) |
| 2002 | 27,28,728 | 5,671 | 20.8 (20.2–21.3) | 20.0 (18.3–21.6) |
| 2003 | 28,20,513 | 5,821 | 20.6 (20.1–21.2) | 19.8 (18.2–21.5) |
| 2004 | 29,14,236 | 6,541 | 22.4 (21.9–23.0) | 21.6 (19.9–23.3) |
| 2005 | 29,73,188 | 6,713 | 22.6 (22.0–23.1) | 21.9 (20.2–23.5) |
| 2006 | 30,16,968 | 7,028 | 23.3 (22.8–23.8) | 22.6 (20.9–24.3) |
| 2007 | 30,27,173 | 7,276 | 24.0 (23.5–24.6) | 23.4 (21.6–25.1) |
| 2008 | 30,47,487 | 7,775 | 25.5 (25.0–26.1) | 24.7 (23.0–26.5) |
| 2009 | 30,26,926 | 8,060 | 26.6 (26.1–27.2) | 26.0 (24.2–27.9) |
| 2010 | 29,78,185 | 7,754 | 26.0 (25.5–26.6) | 25.4 (23.6–27.3) |
| 2011 | 29,04,131 | 7,903 | 27.2 (26.6–27.8) | 26.4 (24.5–28.2) |
| 2012 | 28,15,439 | 7,591 | 27.0 (26.4–27.6) | 26.1 (24.2–28.0) |
| 2013 | 25,98,517 | 6,858 | 26.4 (25.8–27.0) | 25.4 (23.5–27.4) |
| 2014 | 22,81,051 | 6,190 | 27.1 (26.5–27.8) | 26.0 (23.9–28.1) |
| 2015 | 18,33,974 | 5,171 | 28.2 (27.4–29.0) | 26.9 (24.6–29.3) |
| 2016 | 10,93,189 | 3,736 | 34.2 (33.1–35.3) | 32.2 (28.8–35.6) |
Note: aStandard population from Eurostat.27
Abbreviations: ASR, age-standardised incidence rates; CI, confidence interval; IR, incidence rate; PY, person-years.
Lifestyle factors
We observed an adjusted ORs for diagnosed tinnitus of 0.91 (95% CI: 0.89–0.94) in obese patients (BMI ≥30.0 kg/m2), and an adjusted ORs of 0.91 (95% CI: 0.84–0.97) in underweight patients (BMI <18.5 kg/m2), when compared to individuals of normal weight.
Compared with non-smokers, current smokers were at a reduced risk of being diagnosed with tinnitus (adj. OR 0.78, 95% CI: 0.76–0.80). Overall, current alcohol drinkers had a minimally decreased risk compared to non-drinkers. However, the effect became stronger with increasing levels of alcohol consumption (in consumed units of alcohol per week, Table 1).
Comorbidities
Internal diseases and neurological/psychological disorders
We observed an increased risk of being diagnosed with tinnitus in patients with insomnia (adj. OR 1.45, 95% CI: 1.41–1.49), anxiety (adj. OR 1.39, 95% CI: 1.35–1.42), and depression (adj. OR 1.31, 95% CI: 1.28–1.34). We found a decreased risk of being diagnosed with tinnitus in patients with dementia (adj. OR 0.43, 95% CI: 0.37–0.50), Parkinson’s disease (adj. OR 0.63, 95% CI: 0.54–0.74), and schizophrenia (adj. OR 0.76, 95% CI: 0.69–0.85). No association was found between tinnitus and seizures/epilepsy or multiple sclerosis.
Cardiovascular comorbidities (arrhythmia, hypertension, myocardial infarction, congestive heart failure, and stroke/transient ischemic attack) did not reveal any meaningfully increased or decreased ORs. Diabetes mellitus revealed a decreased adjusted OR of 0.85 (95% CI: 0.83–0.89), whereas other metabolic diseases (hyperlipidemia, hypothyroidism, and hyperthyroidism) were not associated with the risk of being diagnosed with tinnitus.
Irritable bowel syndrome and fibromyalgia were statistically significantly associated with the risk of being diagnosed with tinnitus (adj. ORs 1.56, 95% CI: 1.51–1.61, and 1.54, 95% CI: 1.42–1.67), whereas ORs for asthma, COPD, and rheumatoid arthritis were not associated (Table 2).
Table 2.
Distribution of comorbidities in patients with tinnitus and their matched controls: internal diseases and neurological/psychological disorders
| Tinnitus cases (%) | Tinnitus-free controls (%) | OR crude (95% CI) | OR adjusteda (95% CI) | |
|---|---|---|---|---|
| Neurological/psychological disorders | ||||
| Insomnia | 14,944 (13.6) | 11,043 (10.1) | 1.46 (1.42–1.50) | 1.45 (1.41–1.49) |
| Anxiety | 22,872 (20.8) | 17,839 (16.3) | 1.39 (1.36–1.42) | 1.39 (1.35–1.42) |
| Depression | 22,421 (20.4) | 18,363 (16.7) | 1.30 (1.27–1.33) | 1.31 (1.28–1.34) |
| Seizure/Epilepsy | 2393 (2.2) | 2366 (2.2) | 1.01 (0.96–1.07) | 1.01 (0.96–1.08) |
| Multiple Sclerosis | 324 (0.3) | 369 (0.3) | 0.88 (0.76–1.02) | 0.89 (0.76–1.03) |
| Schizophrenia | 623 (0.6) | 831 (0.8) | 0.75 (0.67–0.83) | 0.76 (0.69–0.85) |
| Parkinson Disease | 256 (0.2) | 411 (0.4) | 0.62 (0.53–0.73) | 0.63 (0.54–0.74) |
| Dementia | 282 (0.3) | 660 (0.6) | 0.42 (0.36–0.48) | 0.42 (0.37–0.49) |
| Cardiovascular disorders | ||||
| Arrhythmia | 6374 (5.8) | 5304 (4.8) | 1.23 (1.18–1.28) | 1.19 (1.14–1.24) |
| Hypertension | 25,988 (23.7) | 25,609 (23.3) | 1.02 (1.00–1.05) | 0.98 (0.96–1.00) |
| Myocardial infarction | 2935 (2.7) | 2974 (2.7) | 0.99 (0.94–1.04) | 0.95 (0.90–1.00) |
| Congestive heart failure | 1505 (1.4) | 1593 (1.5) | 0.94 (0.88–1.01) | 0.92 (0.85–0.99) |
| Stroke/TIA | 3385 (3.1) | 3735 (3.4) | 0.90 (0.86–0.94) | 0.88 (0.84–0.93) |
| Metabolic disorders | ||||
| Hyperlipidemia | 12,081 (11.0) | 10,595 (9.7) | 1.18 (1.15–1.22) | 1.14 (1.11–1.18) |
| Hypothyroidism | 6225 (5.7) | 5500 (5.0) | 1.15 (1.10–1.19) | 1.13 (1.08–1.17) |
| Hyperthyroidism | 1523 (1.4) | 1363 (1.2) | 1.12 (1.04–1.21) | 1.11 (1.03–1.20) |
| Diabetes mellitus | 6915 (6.3) | 7626 (7.0) | 0.90 (0.87–0.93) | 0.85 (0.83–0.89) |
| Other disorders | ||||
| Irritable bowel syndrome | 11,008 (10.0) | 7288 (6.6) | 1.59 (1.54–1.65) | 1.56 (1.51–1.61) |
| Fibromyalgia | 1588 (1.5) | 1053 (1.0) | 1.54 (1.42–1.67) | 1.53 (1.41–1.66) |
| Asthma | 16,630 (15.2) | 14,842 (13.5) | 1.15 (1.12–1.18) | 1.11 (1.08–1.14) |
| Rheumatoid Arthritis | 1479 (1.4) | 1336 (1.2) | 1.11 (1.03–1.20) | 1.10 (1.02–1.19) |
| COPD | 2848 (2.6) | 3062 (2.8) | 0.93 (0.88–0.98) | 0.95 (0.90–1.00) |
Notes: Comorbidities listed according to their odds ratios in decreasing order. aAdjusted for BMI category, smoking status, alcohol consumption.
Abbreviations: CI, confidence interval; COPD, Chronic obstructive pulmonary disease; OR, odds ratio; TIA, transient ischemic attack.
Stratification by sex did not reveal meaningful effect modification for the risk of tinnitus in association with mental health and other comorbidities (Table S2).
Table S2.
Distribution of patient characteristics and lifestyle factors in patients with tinnitus and their matched controls, stratified by sex
| Men (n=53,874) | Women (n=55,909) | |||||||
|---|---|---|---|---|---|---|---|---|
| Tinnitus cases (%) | Tinnitus-free controls (%) | OR crude (95% CI) |
OR adjusteda (95% CI) |
Tinnitus cases (%) | Tinnitus-free controls (%) | OR crude (95% CI) |
OR adjusteda (95% CI) |
|
| Neurological/psychological disorders | ||||||||
| Insomnia | 5942 (11.0) | 4175 (7.8) | 1.51 (1.45–1.58) | 1.49 (1.43–1.56) | 9002 (16.1) | 6868 (12.3) | 1.42 (1.37–1.48) | 1.42 (1.37–1.47) |
| Anxiety | 8806 (16.4) | 6880 (12.8) | 1.35 (1.31–1.40) | 1.35 (1.30–1.40) | 14,066 (25.2) | 10,959 (19.6) | 1.41 (1.37–1.45) | 1.41 (1.37–1.46) |
| Depression | 8143 (15.1) | 6390 (11.9) | 1.34 (1.29–1.39) | 1.33 (1.28–1.38) | 14,278 (25.5) | 11,973 (21.4) | 1.28 (1.24–1.32) | 1.30 (1.26–1.34) |
| Seizure/Epilepsy | 1231 (2.3) | 1267 (2.4) | 0.97 (0.90–1.05) | 0.98 (0.90–1.06) | 1162 (2.1) | 1099 (2.0) | 1.06 (0.97–1.15) | 1.06 (0.97–1.15) |
| Multiple Sclerosis | 98 (0.2) | 126 (0.2) | 0.78 (0.60–1.01) | 0.79 (0.60–1.03) | 226 (0.4) | 243 (0.4) | 0.93 (0.78–1.12) | 0.94 (0.78–1.12) |
| Schizophrenia | 333 (0.6) | 402 (0.8) | 0.83 (0.71–0.96) | 0.84 (0.72–0.98) | 290 (0.5) | 429 (0.8) | 0.67 (0.58–0.78) | 0.70 (0.60–0.81) |
| Parkinson Disease | 124 (0.2) | 228 (0.4) | 0.54 (0.44–0.68) | 0.54 (0.44–0.68) | 132 (0.2) | 183 (0.3) | 0.72 (0.58–0.90) | 0.74 (0.59–0.92) |
| Dementia | 106 (0.2) | 207 (0.4) | 0.50 (0.40–0.64) | 0.51 (0.41–0.65) | 176 (0.3) | 453 (0.8) | 0.38 (0.32–0.45) | 0.38 (0.32–0.46) |
| Cardiovascular disorders | ||||||||
| Arrhythmia | 3111 (5.8) | 2632 (4.9) | 1.21 (1.14–1.28) | 1.16 (1.09–1.22) | 3263 (5.8) | 2672 (4.8) | 1.25 (1.18–1.32) | 1.22 (1.16–1.29) |
| Hypertension | 12,176 (22.6) | 11,907 (22.1) | 1.04 (1.00–1.07) | 0.98 (0.94–1.01) | 13,812 (24.7) | 13,702 (24.5) | 1.01 (0.98–1.05) | 0.98 (0.95–1.01) |
| Myocardial infarction | 2120 (3.9) | 2121 (3.9) | 1.00 (0.94–1.07) | 0.96 (0.90–1.02) | 815 (1.5) | 853 (1.5) | 0.95 (0.86–1.05) | 0.92 (0.84–1.02) |
| Congestive heart failure | 766 (1.4) | 828 (1.5) | 0.92 (0.83–1.02) | 0.89 (0.80–0.98) | 739 (1.3) | 765 (1.4) | 0.96 (0.87–1.07) | 0.95 (0.86–1.06) |
| Stroke/TIA | 1703 (3.2) | 1906 (3.5) | 0.89 (0.83–0.95) | 0.86 (0.81–0.93) | 1682 (3.0) | 1829 (3.3) | 0.91 (0.85–0.98) | 0.90 (0.84–0.97) |
| Metabolic disorders | ||||||||
| Hyperlipidemia | 6238 (11.6) | 5445 (10.1) | 1.19 (1.14–1.24) | 1.13 (1.09–1.18) | 5843 (10.5) | 5150 (9.2) | 1.18 (1.13–1.23) | 1.16 (1.11–1.21) |
| Hypothyroidism | 1074 (2.0) | 899 (1.7) | 1.20 (1.10–1.31) | 1.16 (1.06–1.27) | 5151 (9.2) | 4601 (8.2) | 1.14 (1.09–1.18) | 1.12 (1.07–1.17) |
| Hyperthyroidism | 312 (0.6) | 285 (0.5) | 1.10 (0.93–1.29) | 1.04 (0.89–1.23) | 1211 (2.2) | 1078 (1.9) | 1.13 (1.04–1.22) | 1.13 (1.04–1.23) |
| Diabetes mellitus | 3839 (7.1) | 4280 (7.9) | 0.88 (0.84–0.93) | 0.83 (0.79–0.87) | 3076 (5.5) | 3346 (6.0) | 0.91 (0.87–0.96) | 0.88 (0.84–0.93) |
| Other disorders | ||||||||
| Irritable bowel syndrome | 3405 (6.3) | 2028 (3.8) | 1.74 (1.64–1.84) | 1.66 (1.57–1.76) | 7603 (13.6) | 5260 (9.4) | 1.53 (1.48–1.59) | 1.51 (1.46–1.57) |
| Fibromyalgia | 388 (0.7) | 262 (0.5) | 1.50 (1.28–1.76) | 1.50 (1.27–1.76) | 1200 (2.2) | 791 (1.4) | 1.55 (1.41–1.70) | 1.54 (1.40–1.68) |
| Asthma | 7577 (14.1) | 6743 (12.5) | 1.15 (1.11–1.19) | 1.09 (1.05–1.13) | 9053 (16.2) | 8099 (14.5) | 1.15 (1.11–1.18) | 1.12 (1.09–1.16) |
| Rheumatoid Arthritis | 475 (0.9) | 413 (0.8) | 1.15 (1.01–1.32) | 1.13 (0.99–1.29) | 1004 (1.8) | 923 (1.7) | 1.09 (1.00–1.19) | 1.09 (0.99–1.19) |
| COPD | 1535 (2.9) | 1576 (2.9) | 0.97 (0.90–1.05) | 0.99 (0.91–1.06) | 1313 (2.4) | 1486 (2.7) | 0.88 (0.81–0.95) | 0.91 (0.84–0.98) |
Notes: aAdjusted for BMI category, smoking status, alcohol consumption. Comorbidities listed according to their odds ratios in decreasing order
Abbreviations: CI, confidence interval; COPD, Chronic obstructive pulmonary disease; OR, odds ratio; TIA, transient ischemic attack.
Otological and vestibular disorders
Having a medical history of various otological or vestibular disorders was associated with a higher risk of being diagnosed with tinnitus. All inner ear conditions evaluated were found positively associated with tinnitus. This included common conditions such as ear infections (labyrinthitis, otitis media, or otitis externa) and cerumen, as well as rarer conditions such as sensorineural or conductive hearing loss, acute vestibular neuritis or benign positional vertigo. These observed associations were stronger when the comorbidities were closer in time to the index date (Table 3, stratified by sex in Table S3). The association was strongest with sensorineural hearing loss (adj. OR 161.70, 95% CI: 60.56–431.73) followed by acute vestibular neuritis (adj. OR 34.14, 95% CI: 4. 79–243.60), otitis media (adj. OR 22.82, 95% CI: 17.23–30.22), labyrinthitis (adj. OR 20.19, 95% CI: 12.88–31.65), conductive hearing loss (adj. OR 19.51, 95% CI: 6.07–62.74), benign positional vertigo (adj. OR 12.94, 95% CI: 9.24–18.11), cerumen (adj. OR 11.56, 95% CI: 10.41–13.83), and otitis externa (adj. OR 9.87, 95% CI: 8.52–11.43).
Table 3.
Distribution of comorbidities in patients with tinnitus and their matched controls: otological and vestibular disorders
| Tinnitus cases (%) | Tinnitus-free controls (%) | OR crude (95% CI) |
OR adjusteda (95% CI) |
|
|---|---|---|---|---|
| Sensorineural Hearing Loss | ||||
| ≤30 days prior to (includigng) the ID | 618 (0.6) | < 5b (0.0) | 156.99 (58.81–419.08) | 161.70 (60.56–431.73) |
| 31 to 360 days prior to the ID | 179 (0.2) | 60 (0.1) | 3.18 (2.36–4.28) | 3.10 (2.29–4.18) |
| >360 days prior to the ID | 1142 (1.0) | 701 (0.6) | 1.68 (1.53–1.85) | 1.68 (1.53–1.85) |
| Acute vestibular neuronitis | ||||
| ≤30 days prior to (includigng) the ID | 37 (0.0) | < 5b (0.0) | 36.15 (5.07–257.83) | 34.14 (4.79–243.60) |
| 31 to 360 days prior to the ID | 68 (0.1) | 27 (0.0) | 2.58 (1.64–4.05) | 2.37 (1.50–3.73) |
| >360 days prior to the ID | 390 (0.4) | 236 (0.2) | 1.66 (1.41–1.95) | 1.63 (1.39–1.92) |
| Otitis media | ||||
| ≤30 days prior to (includigng) the ID | 1114 (1.0) | 51 (0.1) | 22.91 (17.30–30.32) | 22.82 (17.23–30.22) |
| 31 to 360 days prior to the ID | 1753 (1.6) | 489 (0.5) | 3.82 (3.45–4.23) | 3.81 (3.44–4.22) |
| >360 days prior to the ID | 11,552 (10.5) | 9483 (8.6) | 1.33 (1.29–1.37) | 1.31 (1.27–1.36) |
| Labyrinthitis | ||||
| ≤30 days prior to (includigng) the ID | 408 (0.4) | 20 (0.0) | 20.90 (13.34–32.73) | 20.19 (12.88–31.65) |
| 31 to 360 days prior to the ID | 867 (0.8) | 277 (0.3) | 3.26 (2.85–3.74) | 3.19 (2.78–3.66) |
| >360 days prior to the ID | 4338 (4.0) | 3014 (2.8) | 1.49 (1.42–1.57) | 1.46 (1.40–1.54) |
| Conductive Hearing Loss | ||||
| ≤30 days prior to (includigng) the ID | 52 (0.1) | < 5b (0.0) | 17.32 (5.41–55.42) | 19.51 (6.07–62.74) |
| 31 to 360 days prior to the ID | 29 (0.0) | < 5b (0.0) | 7.25 (2.55–20.62) | 7.23 (2.53–20.67) |
| >360 days prior to the ID | 290 (0.3) | 229 (0.2) | 1.27 (1.07–1.51) | 1.25 (1.05–1.48) |
| Benign positional vertigo | ||||
| ≤30 days prior to (includigng) the ID | 462 (0.4) | 37 (0.0) | 13.11 (9.37–18.34) | 12.94 (9.24–18.11) |
| 31 to 360 days prior to the ID | 960 (0.9) | 398 (0.4) | 2.56 (2.28–2.89) | 2.48 (2.20–2.80) |
| >360 days prior to the ID | 3488 (3.2) | 2294 (2.1) | 1.60 (1.51–1.69) | 1.56 (1.48–1.65) |
| Cerumen | ||||
| ≤30 days prior to (includigng) the ID | 4249 (3.9) | 407 (0.4) | 11.74 (10.58–13.04) | 11.56 (10.41–12.83) |
| 31 to 360 days prior to the ID | 6680 (6.1) | 3512 (3.2) | 2.17 (2.07–2.26) | 2.12 (2.03–2.21) |
| >360 days prior to the ID | 14,702 (13.4) | 14,513 (13.2) | 1.13 (1.10–1.16) | 1.11 (1.08–1.14) |
| Otitis externa | ||||
| ≤30 days prior to (includigng) the ID | 1875 (1.7) | 203 (0.2) | 9.88 (8.54–11.44) | 9.87 (8.52–11.43) |
| 31 to 360 days prior to the ID | 3575 (3.3) | 1506 (1.4) | 2.55 (2.40–2.71) | 2.54 (2.39–2.70) |
| >360 days prior to the ID | 13,171 (12.0) | 11,085 (10.1) | 1.28 (1.24–1.31) | 1.26 (1.23–1.30) |
Notes: aAdjusted for BMI category, smoking status, alcohol consumption. bFor confidentiality reasons, we do not provide the number of patients in categories containing less than five patients.
Abbreviations: CI, confidence interval; ID, index date; NA, not available; OR, odds ratio.
Table S3.
Distribution of comorbidities in patients with tinnitus and their matched controls, stratified by sex: otological and vestibular disorders
| Men (n=53,874) | Women (n=55,909) | |||||||
|---|---|---|---|---|---|---|---|---|
| Tinnitus cases (%) | Tinnitus-free controls (%) | OR crude (95% CI) | OR adjusteda (95% CI) | Tinnitus cases (%) | Tinnitus-free controls (%) | OR crude (95% CI) | OR adjusteda (95% CI) | |
| Sensorineural Hearing Loss | ||||||||
| ≤30 days prior to (includigng) the ID | 330 (0.6) | <5b (0.0) | 166.11 (41.47–665.34) | 171.24 (42.74–686.06) | 288 (0.5) | <5b (0.0) | 148.37 (36.97–595.42) | 153.01 (38.12–614.15) |
| 31 to 360 days prior to the ID | 85 (0.2) | 31 (0.1) | 2.94 (1.93–4.49) | 2.84 (1.86–4.35) | 94 (0.2) | 29 (0.1) | 3.42 (2.24–5.21) | 3.36 (2.20–5.13) |
| >360 days prior to the ID | 565 (1.1) | 380 (0.7) | 1.52 (1.33–1.73) | 1.52 (1.33–1.74) | 577 (1.0) | 321 (0.6) | 1.88 (1.64–2.16) | 1.88 (1.63–2.16) |
| Acute vestibular neuronitis | ||||||||
| ≤30 days prior to (includigng) the ID | 18 (0.0) | <5b (0.0) | 17.98 (2.40–134.54) | 17.90 (2.38–134.45) | 19 (0.0) | 0 (0.0) | NA | NA |
| 31 to 360 days prior to the ID | 23 (0.0) | 5 (0.0) | 4.60 (1.75–12.10) | 3.95 (1.50–10.46) | 45 (0.1) | 22 (0.0) | 2.10 (1.25–3.52) | 1.98 (1.17–3.34) |
| >360 days prior to the ID | 123 (0.2) | 78 (0.1) | 1.58 (1.19–2.09) | 1.49 (1.12–1.99) | 267 (0.5) | 158 (0.3) | 1.70 (1.39–2.07) | 1.69 (1.39–2.07) |
| Otitis media | ||||||||
| ≤30 days prior to (includigng) the ID | 548 (1.0) | 13 (0.0) | 44.05 (25.41–76.36) | 43.55 (25.11–75.54) | 566 (1.0) | 38 (0.1) | 15.74 (11.33–21.86) | 15.76 (11.34–21.91) |
| 31 to 360 days prior to the ID | 784 (1.5) | 201 (0.4) | 4.12 (3.52–4.82) | 4.09 (3.49–4.79) | 969 (1.7) | 288 (0.5) | 3.62 (3.17–4.14) | 3.62 (3.17–4.14) |
| >360 days prior to the ID | 5171 (9.6) | 4391 (8.2) | 1.27 (1.21–1.33) | 1.24 (1.19–1.30) | 6381 (11.4) | 5092 (9.1) | 1.38 (1.32–1.44) | 1.37 (1.32–1.43) |
| Labyrinthitis | ||||||||
| ≤30 days prior to (includigng) the ID | 155 (0.3) | 5 (0.0) | 31.29 (12.84–76.23) | 29.62 (12.14–72.28) | 253 (0.5) | 15 (0.0) | 17.46 (10.37–29.40) | 17.05 (10.11–28.73) |
| 31 to 360 days prior to the ID | 298 (0.6) | 89 (0.2) | 3.47 (2.73–4.40) | 3.43 (2.69–4.36) | 569 (1.0) | 188 (0.3) | 3.16 (2.68–3.74) | 3.07 (2.60–3.64) |
| >360 days prior to the ID | 1453 (2.7) | 992 (1.8) | 1.51 (1.39–1.64) | 1.47 (1.35–1.59) | 2885 (5.2) | 2022 (3.6) | 1.49 (1.40–1.58) | 1.46 (1.38–1.55) |
| Conductive Hearing Loss | ||||||||
| ≤30 days prior to (includigng) the ID | 19 (0.0) | <5b (0.0) | 18.97 (2.54–141.51) | 21.20 (2.81–159.97) | 33 (0.1) | <5b (0.0) | 16.49 (3.96–68.68) | 18.60 (4.45–77.82) |
| 31 to 360 days prior to the ID | 13 (0.0) | <5b (0.0) | 6.50 (1.47–28.80) | 6.95 (1.55–31.13) | 16 (0.0) | <5b (0.0) | 8.00 (1.84–34.79) | 7.62 (1.75–33.25) |
| >360 days prior to the ID | 127 (0.2) | 112 (0.2) | 1.13 (0.88–1.46) | 1.10 (0.85–1.43) | 163 (0.3) | 117 (0.2) | 1.40 (1.10–1.77) | 1.39 (1.09–1.76) |
| Benign positional vertigo | ||||||||
| ≤30 days prior to (includigng) the ID | 146 (0.3) | 12 (0.0) | 12.61 (6.99–22.74) | 11.95 (6.61–21.60) | 316 (0.6) | 25 (0.0) | 13.32 (8.86–20.03) | 13.33 (8.86–20.06) |
| 31 to 360 days prior to the ID | 344 (0.6) | 124 (0.2) | 2.92 (2.37–3.60) | 2.80 (2.27–3.46) | 616 (1.1) | 274 (0.5) | 2.39 (2.07–2.77) | 2.33 (2.01–2.69) |
| >360 days prior to the ID | 1189 (2.2) | 725 (1.4) | 1.70 (1.55–1.87) | 1.65 (1.50–1.82) | 2299 (4.1) | 1569 (2.8) | 1.54 (1.44–1.65) | 1.52 (1.42–1.63) |
| Cerumen | ||||||||
| ≤30 days prior to (includigng) the ID | 2502 (4.6) | 237 (0.4) | 11.83 (10.32–13.56) | 11.58 (10.10–13.29) | 1747 (3.1) | 170 (0.3) | 11.57 (9.84–13.61) | 11.50 (9.77–13.53) |
| 31 to 360 days prior to the ID | 3737 (6.9) | 2037 (3.8) | 2.11 (1.99–2.24) | 2.06 (1.94–2.18) | 2943 (5.3) | 1475 (2.6) | 2.23 (2.09–2.38) | 2.19 (2.05–2.34) |
| >360 days prior to the ID | 7841 (14.6) | 8009 (14.9) | 1.10 (1.06–1.14) | 1.07 (1.04–1.11) | 6861 (12.3) | 6504 (11.6) | 1.16 (1.12–1.21) | 1.15 (1.11–1.20) |
| Otitis externa | ||||||||
| ≤30 days prior to (includigng) the ID | 970 (1.8) | 96 (0.2) | 10.81 (8.74–13.36) | 10.71 (8.65–13.25) | 905 (1.6) | 107 (0.2) | 9.03 (7.38–11.06) | 9.10 (7.43–11.15) |
| 31 to 360 days prior to the ID | 1713 (3.2) | 717 (1.3) | 2.56 (2.34–2.80) | 2.56 (2.34–2.80) | 1862 (3.3) | 789 (1.4) | 2.54 (2.33–2.76) | 2.53 (2.32–2.75) |
| >360 days prior to the ID | 6353 (11.8) | 5585 (10.4) | 1.22 (1.17–1.27) | 1.20 (1.15–1.25) | 6818 (12.2) | 5500 (9.8) | 1.34 (1.29–1.39) | 1.33 (1.28–1.38) |
Notes: aAdjusted for BMI category, smoking status, alcohol consumption. bFor confidentiality reasons, we do not provide the number of patients in categories containing less than five patients.
Abbreviations: CI, confidence interval; ID, index date; NA, not available; OR, odds ratio.
Head and neck disorders
Similarly, tinnitus patients were more likely to have a prior diagnosis of head and neck disorders compared with controls. Risk estimates were particularly increased if these diagnoses were recorded within one month before the ID. We found elevated ORs for tinnitus in patients with tension-type headache (adj. OR 11.71, 95% CI: 5.92–23.19), concussion (adj. OR 8.45, 95% CI: 2.54–28.05), temporomandibular joint disorders (adj. OR 6.63, 95% CI: 3.98–11.06), whiplash (adj. OR 5.39, 95% CI: 3.11–9.34), cervicalgia (adj. OR 5.04, 95% CI: 4.33–5.86), migraine (adj. OR 4.38, 95% CI: 3.43–5.60), or cranial nerve disorders (adj. OR 4.33, 95% CI: 2.69–6.98; Table 4, stratified by sex in Table S4).
Table 4.
Distribution of comorbidities in patients with tinnitus and their matched controls: head and neck disorders
| Tinnitus cases (%) | Tinnitus-free controls (%) | OR crude (95% CI) | OR adjusteda (95% CI) | |
|---|---|---|---|---|
| Tension-type headache | ||||
| ≤30 days prior to (includigng) the ID | 104 (0.1) | 9 (0.0) | 11.72 (5.93–23.17) | 11.71 (5.92–23.19) |
| 31 to 360 days prior to the ID | 359 (0.3) | 145 (0.1) | 2.53 (2.09–3.07) | 2.52 (2.07–3.06) |
| >360 days prior to the ID | 3331 (3.0) | 2176 (2.0) | 1.58 (1.49–1.67) | 1.54 (1.46–1.63) |
| Concussion | ||||
| ≤30 days prior to (includigng) the ID | 25 (0.0) | <5b (0.0) | 8.31 (2.51–27.47) | 8.45 (2.54–28.05) |
| 31 to 360 days prior to the ID | 39 (0.0) | 19 (0.0) | 2.05 (1.19–3.55) | 2.10 (1.21–3.66) |
| >360 days prior to the ID | 539 (0.5) | 497 (0.5) | 1.09 (0.96–1.23) | 1.09 (0.96–1.23) |
| Temporomandibular joint disorders | ||||
| ≤30 days prior to (includigng) the ID | 115 (0.1) | 17 (0.0) | 6.84 (4.11–11.38) | 6.63 (3.98–11.06) |
| 31 to 360 days prior to the ID | 308 (0.3) | 144 (0.1) | 2.17 (1.78–2.64) | 2.09 (1.71–2.56) |
| >360 days prior to the ID | 2323 (2.1) | 1501 (1.4) | 1.58 (1.48–1.68) | 1.54 (1.44–1.64) |
| Whiplash | ||||
| ≤30 days prior to (includigng) the ID | 86 (0.1) | 15 (0.0) | 5.80 (3.35–10.04) | 5.39 (3.11–9.34) |
| 31 to 360 days prior to the ID | 345 (0.3) | 232 (0.2) | 1.51 (1.27–1.78) | 1.48 (1.25–1.75) |
| >360 days prior to the ID | 4517 (4.1) | 3778 (3.4) | 1.21 (1.16–1.27) | 1.20 (1.15–1.25) |
| Cervicalgia | ||||
| ≤30 days prior to (includigng) the ID | 985 (0.9) | 210 (0.2) | 5.17 (4.45–6.01) | 5.04 (4.33–5.86) |
| 31 to 360 days prior to the ID | 3000 (2.7) | 1740 (1.6) | 1.89 (1.78–2.01) | 1.82 (1.72–1.94) |
| >360 days prior to the ID | 18,075 (16.5) | 13,399 (12.2) | 1.50 (1.46–1.54) | 1.47 (1.44–1.51) |
| Migraine | ||||
| ≤30 days prior to (includigng) the ID | 346 (0.3) | 80 (0.1) | 4.54 (3.56–5.79) | 4.38 (3.43–5.60) |
| 31 to 360 days prior to the ID | 1045 (1.0) | 603 (0.6) | 1.83 (1.65–2.02) | 1.77 (1.59–1.95) |
| >360 days prior to the ID | 9519 (8.7) | 7160 (6.5) | 1.39 (1.35–1.44) | 1.37 (1.32–1.41) |
| Cranial nerve disorders | ||||
| ≤30 days prior to (includigng) the ID | 90 (0.1) | 21 (0.0) | 4.32 (2.69–6.95) | 4.33 (2.69–6.98) |
| 31 to 360 days prior to the ID | 342 (0.3) | 177 (0.2) | 1.95 (1.63–2.35) | 1.90 (1.58–2.29) |
| >360 days prior to the ID | 2286 (2.1) | 1772 (1.6) | 1.30 (1.22–1.39) | 1.30 (1.22–1.39) |
Notes: aAdjusted for BMI category, smoking status, alcohol consumption. bFor confidentiality reasons, we do not provide the number of patients in categories containing less than five patients.
Abbreviations: CI, confidence interval; ID, index date; NA, not available; OR, odds ratio.
Table S4.
Distribution of comorbidities in patients with tinnitus and their matched controls, stratified by sex: head and neck disorders
| Men (n=53,874) | Women (n=55,909) | |||||||
|---|---|---|---|---|---|---|---|---|
| Tinnitus cases (%) | Tinnitus-free controls (%) | OR crude (95% CI) | OR adjusteda (95% CI) | Tinnitus cases (%) | Tinnitus-free controls (%) | OR crude (95% CI) | OR adjusteda (95% CI) | |
| Tension-type headache | ||||||||
| ≤30 days prior to (includigng) the ID | 38 (0.1) | 0 (0.0) | NA | NA | 66 (0.1) | 9 (0.0) | 7.47 (3.72–14.99) | 7.55 (3.76–15.18) |
| 31 to 360 days prior to the ID | 117 (0.2) | 48 (0.1) | 2.47 (1.77–3.46) | 2.38 (1.70–3.35) | 242 (0.4) | 97 (0.2) | 2.56 (2.02–3.24) | 2.57 (2.03–3.26) |
| >360 days prior to the ID | 1143 (2.1) | 708 (1.3) | 1.64 (1.49–1.81) | 1.57 (1.43–1.73) | 2188 (3.9) | 1468 (2.6) | 1.54 (1.44–1.65) | 1.52 (1.42–1.63) |
| Concussion | ||||||||
| ≤30 days prior to (includigng) the ID | 14 (0.0) | <5b (0.0) | 14.00 (1.84–106.41) | 13.36 (1.74–102.45) | 11 (0.0) | <5b (0.0) | 5.50 (1.22–24.80) | 5.98 (1.32–27.08) |
| 31 to 360 days prior to the ID | 15 (0.0) | 7 (0.0) | 2.14 (0.87–5.26) | 2.31 (0.93–5.75) | 24 (0.0) | 12 (0.0) | 2.00 (1.00–4.00) | 2.00 (1.00–4.01) |
| >360 days prior to the ID | 332 (0.6) | 324 (0.6) | 1.03 (0.88–1.20) | 1.02 (0.88–1.20) | 207 (0.4) | 173 (0.3) | 1.20 (0.98–1.47) | 1.21 (0.99–1.49) |
| Temporomandibular joint disorders | ||||||||
| ≤30 days prior to (includigng) the ID | 38 (0.1) | 7 (0.0) | 5.43 (2.42–12.15) | 5.27 (2.34–11.85) | 77 (0.1) | 10 (0.0) | 7.81 (4.05–15.10) | 7.59 (3.92–14.70) |
| 31 to 360 days prior to the ID | 106 (0.2) | 38 (0.1) | 2.80 (1.93–4.06) | 2.73 (1.88–3.97) | 202 (0.4) | 106 (0.2) | 1.93 (1.53–2.45) | 1.86 (1.47–2.36) |
| >360 days prior to the ID | 696 (1.3) | 413 (0.8) | 1.70 (1.51–1.93) | 1.64 (1.44–1.85) | 1627 (2.9) | 1088 (2.0) | 1.53 (1.41–1.65) | 1.50 (1.39–1.62) |
| Whiplash | ||||||||
| ≤30 days prior to (includigng) the ID | 44 (0.1) | 7 (0.0) | 6.44 (2.90–14.30) | 5.77 (2.59–12.86) | 42 (0.1) | 8 (0.0) | 5.27 (2.47–11.22) | 5.12 (2.40–10.92) |
| 31 to 360 days prior to the ID | 160 (0.3) | 112 (0.2) | 1.45 (1.13–1.84) | 1.41 (1.10–1.81) | 185 (0.3) | 120 (0.2) | 1.56 (1.24–1.97) | 1.54 (1.22–1.94) |
| >360 days prior to the ID | 2144 (4.0) | 1724 (3.2) | 1.26 (1.18–1.35) | 1.25 (1.17–1.33) | 2373 (4.2) | 2054 (3.7) | 1.17 (1.10–1.25) | 1.16 (1.09–1.23) |
| Cervicalgia | ||||||||
| ≤30 days prior to (includigng) the ID | 425 (0.8) | 81 (0.2) | 5.57 (4.39–7.07) | 5.41 (4.26–6.88) | 560 (1.0) | 129 (0.2) | 4.90 (4.03–5.95) | 4.80 (3.94–5.83) |
| 31 to 360 days prior to the ID | 1184 (2.2) | 674 (1.3) | 1.90 (1.72–2.09) | 1.81 (1.64–2.00) | 1816 (3.3) | 1066 (1.9) | 1.88 (1.74–2.03) | 1.83 (1.69–1.98) |
| >360 days prior to the ID | 7533 (14.0) | 5411 (10.0) | 1.53 (1.47–1.59) | 1.49 (1.43–1.55) | 10,542 (18.9) | 7988 (14.3) | 1.48 (1.43–1.53) | 1.46 (1.41–1.51) |
| Migraine | ||||||||
| ≤30 days prior to (includigng) the ID | 103 (0.2) | 17 (0.0) | 6.16 (3.69–10.30) | 5.73 (3.42–9.60) | 243 (0.4) | 63 (0.1) | 4.09 (3.10–5.39) | 3.98 (3.01–5.26) |
| 31 to 360 days prior to the ID | 246 (0.5) | 134 (0.3) | 1.87 (1.51–2.31) | 1.77 (1.43–2.19) | 799 (1.4) | 469 (0.8) | 1.81 (1.62–2.04) | 1.76 (1.57–1.98) |
| >360 days prior to the ID | 2821 (5.2) | 1988 (3.7) | 1.45 (1.37–1.54) | 1.41 (1.33–1.49) | 6698 (12.0) | 5172 (9.3) | 1.37 (1.32–1.42) | 1.35 (1.30–1.40) |
| Cranial nerve disorders | ||||||||
| ≤30 days prior to (includigng) the ID | 33 (0.1) | 10 (0.0) | 3.30 (1.63–6.70) | 3.43 (1.68–6.99) | 57 (0.1) | 11 (0.0) | 5.23 (2.74–9.98) | 5.14 (2.69–9.83) |
| 31 to 360 days prior to the ID | 122 (0.2) | 53 (0.1) | 2.36 (1.70– 3.28) | 2.26 (1.62–3.14) | 220 (0.4) | 124 (0.2) | 1.78 (1.43–2.23) | 1.75 (1.40–2.19) |
| >360 days prior to the ID | 874 (1.6) | 722 (1.3) | 1.22 (1.10– 1.35) | 1.21 (1.09–1.33) | 1412 (2.5) | 1050 (1.9) | 1.36 (1.26–1.48) | 1.37 (1.26–1.48) |
Notes: aAdjusted for BMI category, smoking status, alcohol consumption. bFor confidentiality reasons, we do not provide the number of patients in categories containing less than five patients.
Abbreviations: CI, confidence interval; ID, index date; NA, not available; OR, odds ratio.
Discussion
In this large case-control analysis, we assessed incidence rates of GP-recorded tinnitus in the UK over time, and we characterized life style parameters as well a large range of comorbidities in tinnitus patients. The direct comparison of tinnitus cases with a randomly selected, matched sample of tinnitus-free patients allowed us to characterize which factors were more and which less frequently observed in tinnitus patients compared to controls, without any claim that such observed association are necessarily causal.
Incidence rates
Between 2000 and 2016, we calculated an overall crude IR of GP-reported tinnitus of 24.3 cases per 10,000 PY. IRs for men and women were comparable, which is consistent with results of previously published studies although there is no general consensus in the field.4,11,28–30
We observed that IRs increased with age, were highest between age 60–69 years, and decreased subsequently thereafter. This pattern has been reported by others.4,11,28 It is hypothesized that, with increasing age, the importance of tinnitus in a patient’s overall health burden declines, and the ability to cope with symptoms grows.28,31 Another theory is that tinnitus may be associated with cardiovascular disease, and that patients with cardiovascular diseases are more likely to die, whereby those who survive are less likely to develop tinnitus.28 However, we did not find a marked increase in tinnitus risk associated with previous cardiovascular diseases, and exploring cardiovascular mortality was not the goal of this study.
We observed a substantial rise in the annual IRs during the study period from 18.3 per 10,000 PY in 2000 to 34.2 per 10,000 PY in 2016. Over the past two decades, other studies also reported increases in rates of hearing disorders including tinnitus in adolescents and young adults, possibly due to higher exposure to loud music in bars, concerts, discotheques and from personal electronic devices.32–34 However, our analysis yielded no difference between young adults below 30 years of age and older adults with respect to the pattern of IRs over time. Other explanations for the rise in tinnitus incidence include more demanding health expectations, and a higher awareness of symptoms over time.11,35
The precise IRs reported in the literature vary due to differences in study periods, regions, and case definitions. We included all patients with GP-reported tinnitus, whereas other authors exclusively focused on i) clinically significant tinnitus defined by Martinez et al,11 ii) self-reported tinnitus symptoms lasting for at least five minutes4 or iii) self-reported tinnitus symptoms in the last year of at least moderate severity or leading to sleep disorders.28,36 These differences likely explain the higher IRs observed in our study.
Lifestyle factors
We found that obese patients were not at increased risk of developing tinnitus, as did three previous cross-sectional studies37–39 and a cohort study.36 On the contrary, our data suggest a slightly lower risk in obese as well as in underweight patients, though the ORs were very close to the null.
We observed an inverse association between current smoking and tinnitus. The same was found in a cross-sectional study using the UK Biobank resource for persistent tinnitus, but not for transient tinnitus.39 An Italian study published in 2015 reported a comparable trend, but due to the small study population the results did not meet statistical significance.40 In contrast, other studies have reported an increased risk of being diagnosed with tinnitus among smokers.34,36,41,42 A variety of possible causes of tinnitus as well as differences in the study designs and respective study populations may contribute to these contradictory results.15
Current alcohol consumption was also inversely related to tinnitus, which is consistent with the findings of several other studies.29,36,40 It has been hypothesized that alcohol exerts a favorable effect on microvascular health in the cochlea.29 Another explanation is that tinnitus is underreported in patients with unhealthy lifestyles who may be more likely to suffer from more pressing health-related problems and may not discuss tinnitus with their GP.
Comorbidities
Our analyses yielded a statistically significant association between prevalent anxiety, depression, and insomnia, and the risk of developing tinnitus. It is well known that these disorders have a negative impact on quality of life and on severity of tinnitus,7–9 and they are also often a consequence of bothersome tinnitus.5,7,34,43 Some studies have also found that anxiety and depression can precede tinnitus,34,44,45 and parallels in pathophysiology have been noted.8,9,46 In this study, however, we were careful to establish that the depression-related disorders occurred before the tinnitus diagnosis. It has previously been suggested that tinnitus is associated with greater mental health burden in women than in men.47 A prior cross-sectional study further reported a statistically significantly increased risk of suicide attempts in women with severe tinnitus, but not in men.48 The absence of any meaningful effect modification by sex for the association of the risk of tinnitus and mental health and other comorbidities may thus reflect that women with mental health diseases are not per se at an increased risk of developing tinnitus compared to men; however, they may suffer more distress from co-existing tinnitus and mental health diseases. Further research is needed to evaluate this potential association.
Our finding of decreased ORs, especially in patients with a diagnosis of dementia, Parkinson’s disease or schizophrenia, could be explained by underreporting due to more serious health-related problems or due to difficulties in communication.
Impairment of the auditory system seems to be an important underlying mechanism of tinnitus.14,29 It is assumed that hearing impairment may induce tinnitus by initiating changes on a cellular and structural level in the brain This involves changes within the central auditory system as well as within non-auditory systems.14 Our results showed that hearing loss, in particular sensorineural hearing loss, and ear infections were highly associated with tinnitus. Previous studies also found this association, and they have also shown that concomitantly occurring hearing loss may be considered a predictor for tinnitus severity.28,49
Another proposed mechanism of somatosensory system-related tinnitus involves pathological processes of musculoskeletal structures of the head and neck,4,28,50–54 such as functional disorders of the cervical spine or neck and the temporomandibular joint.37,55–58 Changes in the neuronal activity of the dorsal cochlear nucleus or between somatosensory and auditory systems seem to play an important role in this subtype of tinnitus.59 A meta-analysis of eight cross-sectional studies in patients with temporomandibular joint disorders identified tinnitus as a common symptom in over 50% of patients.58 The results of our study were similar, with a large proportion of tinnitus occurring in patients suffering from tension headaches, migraine, cervicalgia, whiplash, concussion, or cranial nerve disorders.
The highest rate of tinnitus among patients with otological and vestibular disorders as well as head and neck disorders, occurred shortly after the recording of the respective disorder which supports the possibility of a causal association.
Study limitations
When interpreting the results of this study, we took several limitations into account. First, tinnitus is usually a subjective phenomenon, and the diagnosis is based on self-reporting. Case validation is difficult without uniformly followed standardized procedures60 and the availability of questionnaires or referral letters. To our knowledge, the tinnitus diagnosis has not been validated in the CPRD, as this is virtually impossible, since tinnitus is a self-diagnosed condition that cannot be confirmed as yet with objective diagnostic procedures; thus, there is likely to be some case misclassification in this study. However, the large sample size of the present clinical data may compensate for such misclassifications. Second, tinnitus severity is mostly mild, and only 10 to 52% of individuals who experience tinnitus discuss this symptom with their GP.4,5,50 Therefore, GP-reported tinnitus does not capture all cases, and the true rates are likely to be higher than those presented in our study. Nevertheless, the numbers reflect those cases that present to the GPs in real life in the UK. Third, GPs do not systematically record tinnitus characteristics such as severity, duration, or impact on patients’ quality of life. Therefore, it was not possible to carry out detailed analyses to account for these factors or to distinguish between clinically important or less important tinnitus, or between acute or persistent tinnitus. To date, there is no generally accepted definition to consistently10 grade tinnitus severity, and the approaches used in the different studies vary.4,28,30,36–38,50 Finally, a first-time tinnitus diagnosis does likely not coincide with the actual disease onset in a proportion of cases since patients may not seek medical attention immediately.
Conclusion
We investigated the epidemiology of GP-recorded tinnitus in a large sample of the UK population. IRs increased considerably over time in men and women, emphasizing a growing health burden. Recent diagnosis of several otological and vestibular as well as head and neck disorders was strongly associated with the risk of developing tinnitus. However, we cannot derive causality from these analyses, as we did not intend to run an etiologic study, but rather to descriptively characterize tinnitus patients with regard to life style parameters and comorbidities. These observations may support doctors when diagnosing tinnitus and when putting life style and comorbidity patterns of individual patients into perspective of a large population-based assessment.
Supplementary materials
Acknowledgment
We thank Pascal Egger for technical support and programming. Velux Foundation, Switzerland. The sponsor was not involved in any stage from study design to submission of the manuscript for publication.
Data sharing statement
Data for this study were derived from CPRD primary care data obtained under license from the UK Medicines and Healthcare products Regulatory Agency. The data is provided by patients and collected by the NHS as part of their care and support. The interpretation and conclusions contained in the study are those of the authors alone.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.NICE CKS (2017). Tinnitus. Available from: https://cks.nice.org.uk/tinnitus. Accessed May 11, 2018.
- 2.Tunkel DE, Bauer CA, Sun GH, et al. Clinical practice guideline: tinnitus. Otolaryngol Head Neck Surg. 2014;151(2 Suppl):S1–S40. doi: 10.1177/0194599814545325 [DOI] [PubMed] [Google Scholar]
- 3.Baguley D, McFerran D, Hall D. Tinnitus. Lancet. 2013;382(9904):1600–1607. doi: 10.1016/S0140-6736(13)60142-7 [DOI] [PubMed] [Google Scholar]
- 4.Gopinath B, Mcmahon CM, Rochtchina E, Karpa MJ, Mitchell P. Incidence, persistence, and progression of tinnitus symptoms in older adults: the blue mountains hearing study. Ear Hear. 2010;31:407–412. doi: 10.1097/AUD.0b013e3181cdb2a2 [DOI] [PubMed] [Google Scholar]
- 5.Bhatt JM, Lin HW, Bhattacharyya N. Prevalence, severity, exposures, and treatment patterns of tinnitus in the United States. JAMA Otolaryngol Neck Surg. 2016;142(10):959. doi: 10.1001/jamaoto.2016.1700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nondahl DM, Cruickshanks KJ, Dalton DS, et al. The impact of tinnitus on quality of life in older adults. J Am Acad Audiol. 2007;18:257–266. [DOI] [PubMed] [Google Scholar]
- 7.Folmer RL, Griest SE. Tinnitus and insomnia. Am J Otolaryngol. 2000;21:287–293. doi: 10.1053/ajot.2000.9871 [DOI] [PubMed] [Google Scholar]
- 8.Langguth B, Landgrebe M. Tinnitus and depression. Textb Tinnitus. 2011;2975(May):493–498. [Google Scholar]
- 9.Pattyn T, Van den Eede F, Vanneste S, et al. Tinnitus and anxiety disorders: a review. Hear Res. 2016;333:255–265. doi: 10.1016/j.heares.2015.08.014 [DOI] [PubMed] [Google Scholar]
- 10.Edmondson-jones M, Mccormack A, Somerset S, Hall D. A systematic review of the reporting of tinnitus prevalence and severity. Hear Res. 2016;337:70–79. doi: 10.1016/j.heares.2016.05.009 [DOI] [PubMed] [Google Scholar]
- 11.Martinez C, Wallenhorst C, McFerran D, Hall DA. Incidence rates of clinically significant tinnitus: 10-year trend from a cohort study in England. Ear Hear. 2015;36(3):e69–75. doi: 10.1097/AUD.0000000000000121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stockdale D, McFerran D, Brazier P, et al. An economic evaluation of the healthcare cost of tinnitus management in the UK. BMC Health Serv Res. 2017;17(1):577. doi: 10.1186/s12913-017-2527-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maes C, Vlaeyen AJ. Tinnitus: a cost study. Ear Hear. 2013;34(4):508–514. doi: 10.1097/AUD.0b013e31827d113a [DOI] [PubMed] [Google Scholar]
- 14.Henry JA, Roberts LE, Caspary DM, Theodoroff SM, Salvi RJ. Underlying mechanisms of tinnitus: review and clinical implications. J Am Acad Audiol. 2014;25(1):5–22. doi: 10.3766/jaaa.25.1.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cima RFF, Mazurek B, Haider H, et al. A multidisciplinary European guideline for tinnitus: diagnostics, assessment, and treatment. HNO. 2019;67(March):10–42. doi: 10.1007/s00106-019-0633-7 [DOI] [PubMed] [Google Scholar]
- 16.Langguth B, Elgoyhen AB, Cederroth CR. Therapeutic approaches to the treatment of tinnitus. Annu Rev Pharmacol Toxicol. 2018;59(1):291–313. doi: 10.1146/annurev-pharmtox-010818-021556 [DOI] [PubMed] [Google Scholar]
- 17.Zenner H-P, Delb W, Kroener-Herwig B, et al. A multidisciplinary systematic review of the treatment for chronic idiopathic tinnitus. Eur Arch Oto-Rhino-Laryngol. 2017;274:2079–2091. doi: 10.1007/s00405-016-4401-y [DOI] [PubMed] [Google Scholar]
- 18.Cederroth CR, Dyhrfjeld-Johnsen J, Langguth B. An update: emerging drugs for tinnitus. Expert Opin Emerg Drugs. 2018;23(4):251–260. doi: 10.1080/14728214.2018.1555240 [DOI] [PubMed] [Google Scholar]
- 19.Hall DA, Haider H, Szczepek AJ, et al. Systematic review of outcome domains and instruments used in clinical trials of tinnitus treatments in adults. Trials. 2016;17(1):1–19. doi: 10.1186/s13063-015-1128-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hall DA, Hibbert A, Smith H, et al. One size does not fit all: developing common standards for outcomes in early-phase clinical trials of sound-, psychology-, and pharmacology-based interventions for chronic subjective tinnitus in adults. Trends Hear. 2019;23:1-16. doi: 10.1177/2331216518824827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cederroth CR, Gallus S, Hall DA, et al. Editorial: towards an understanding of tinnitus hetero.geneity. Front Aging Neurosci. 2019;11(March):1–7. doi: 10.3389/fnagi.2019.00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Herrett E, Gallagher AM, Bhaskaran K, et al. Data resource profile: Clinical Practice Research Datalink (CPRD). Int J Epidemiol. 2015;44(3):827–836. doi: 10.1093/ije/dyv098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Herrett E, Thomas SL, Schoonen WM, Smeeth L, Hall AJ. Validation and validity of diagnoses in the General Practice Research Database: a systematic review. Br J Clin Pharmacol. 2010;69(1):4–14. doi: 10.1111/j.1365-2125.2009.03537.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Williams T, van Staa T, Puri S, Eaton S. Recent advances in the utility and use of the General Practice Research Database as an example of a UK Primary Care Data resource. Ther Adv Drug Saf. 2012;3(2):89–99. doi: 10.1177/2042098611435911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khan NF, Harrison SE, Rose PW. Validity of diagnostic coding within the General Practice Research Database: a systematic review. Br J Gen Pract. 2010;60(572):199–206. doi: 10.3399/bjgp10X483562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jick S, Kaye J, Vasilakis-Scaramozza C, et al. Validity of the General Practice Research Database. Pharmacotherapy. 2003;23(5):686–689. [DOI] [PubMed] [Google Scholar]
- 27.Eurostat. Revision of the European Standard Population: Report of Eurostat’s Task Force. Luxembourg: Publications Office of the European Union. 2013. [Google Scholar]
- 28.Nondahl DM, Cruickshanks KJ, Wiley TL, Klein R, Klein BEK, Tweed TS. Prevalence and 5-year incidence of tinnitus among older adults: the epidemiology of hearing loss study. J Am Acad Audiol. 2002;13(6):323–331. [PubMed] [Google Scholar]
- 29.Nondahl DM, Cruickshanks KJ, Huang GH, et al. Tinnitus and its risk factors in the Beaver Dam Offspring Study. Int J Audiol. 2011;50(5):313–320. doi: 10.3109/14992027.2010.551220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCormack A, Edmondson-Jones M, Fortnum H, et al. The prevalence of tinnitus and the relationship with neuroticism in a middle-aged UK population. J Psychosom Res. 2014;76(1):56–60. doi: 10.1016/j.jpsychores.2013.08.018 [DOI] [PubMed] [Google Scholar]
- 31.Davis AC. The prevalence of hearing impairment and reported hearing disability among adults in Great Britain. Int J Epidemiol. 1989;18(4):911–917. doi: 10.1093/ije/18.4.911 [DOI] [PubMed] [Google Scholar]
- 32.Gilles A, Van Hal G, De Ridder D, Wouters K, Van de Heyning P. Epidemiology of noise-induced tinnitus and the attitudes and beliefs towards noise and hearing protection in adolescents. PLoS One. 2013;8(7):e0070297. doi: 10.1371/journal.pone.0070297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Henderson E, Testa MA, Hartnick C. Prevalence of noise-induced hearing-threshold shifts and hearing loss among US youths. Pediatrics. 2011;127(1):e39–e46. doi: 10.1542/peds.2010-0926 [DOI] [PubMed] [Google Scholar]
- 34.Shargorodsky J, Curhan GC, Farwell WR. Prevalence and characteristics of tinnitus among US adults. Am J Med. 2010;123(8):711–718. doi: 10.1016/j.amjmed.2010.02.015 [DOI] [PubMed] [Google Scholar]
- 35.Nondahl DM, Cruickshanks KJ, Huang G-H, et al. Generational differences in the reporting of tinnitus. Ear Hear. 2012;33(5):640–644. doi: 10.1097/AUD.0b013e31825069e8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nondahl DM, Cruickshanks KJ, Wiley TL, et al. The ten-year incidence of tinnitus among older adults. Int J Audiol. 2010;49(8):580–585. doi: 10.3109/14992021003753508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Park RJ, Moon JD. Prevalence and risk factors of tinnitus: the Korean National Health and Nutrition Examination Survey 2010–2011, a cross-sectional study. Clin Otolaryngol. 2014;39(2):89–94. doi: 10.1111/coa.12232 [DOI] [PubMed] [Google Scholar]
- 38.Kim H-J, Lee H-J, An S-Y, et al. Analysis of the prevalence and associated risk factors of tinnitus in adults. PLoS One. 2015;10(5):e0127578. doi: 10.1371/journal.pone.0127578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McCormack A, Edmondson-Jones M, Mellor D, et al. Association of dietary factors with presence and severity of tinnitus in a middle-aged UK population. PLoS One. 2014;9(12):e0114711. doi: 10.1371/journal.pone.0114711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gallus S, Lugo A, Garavello W, et al. Prevalence and determinants of tinnitus in the Italian adult population. Neuroepidemiology. 2015;45(1):12–19. doi: 10.1159/000431376 [DOI] [PubMed] [Google Scholar]
- 41.Bhatt IS. Prevalence of and risk factors for tinnitus and tinnitus-related handicap in a college-aged population. Ear Hear. 2018;39(3):517–526. doi: 10.1097/AUD.0000000000000503 [DOI] [PubMed] [Google Scholar]
- 42.Mahboubi H, Oliaei S, Kiumehr S, Dwabe S, Djalilian HR. The prevalence and characteristics of tinnitus in the youth population of the United States. Laryngoscope. 2013;123(8):2001–2008. doi: 10.1002/lary.24015 [DOI] [PubMed] [Google Scholar]
- 43.Loprinzi PD, Maskalick S, Brown K, Gilham B. Association between depression and tinnitus in a nationally representative sample of US older adults. Aging Ment Health. 2013;17(6):714–717. doi: 10.1080/13607863.2013.775640 [DOI] [PubMed] [Google Scholar]
- 44.Salviati M, Bersani FS, Terlizzi S, et al. Tinnitus: Clinical experience of the psychosomatic connection. Neuropsychiatr Dis Treat. 2014;10:267–275. doi: 10.2147/NDT.S49425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Robinson SK, Viirre ES, Stein MB. Antidepressant therapy in tinnitus. Hear Res. 2007;226(1–2):221–231. doi: 10.1016/j.heares.2006.08.004 [DOI] [PubMed] [Google Scholar]
- 46.Wallhäusser-Franke E, Schredl M, Delb W. Tinnitus and insomnia: is hyperarousal the common denominator? Sleep Med Rev. 2013;17(1):65–74. doi: 10.1016/j.smrv.2012.04.003 [DOI] [PubMed] [Google Scholar]
- 47.Schlee W, Hall DA, Edvall NK, Langguth B, Canlon B, Cederroth CR. Visualization of global disease burden for the optimization of patient management and treatment. Front Med. 2017;4:(June):1–12. doi: 10.3389/fmed.2017.00086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lugo A, Trpchevska N, Liu X, et al. Sex-specific association of tinnitus with suicide attempts. JAMA Otolaryngol Head Neck Surg. 2019;451:17–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sindhusake D, Golding M, Wigney D, Newall P, Jakobsen K, Mitchell P. Factors predicting severity of tinnitus: a population-based assessment. J Am Acad Audiol. 2004;15:269–280. [DOI] [PubMed] [Google Scholar]
- 50.Sindhusake D, Mitchell P, Newall P, Golding M, Rochtchina E, Rubin G. Prevalence and characteristics of tinnitus in older adults: the Blue Mountains Hearing Study. Int J Audiol. 2003;42(5):289–294. [DOI] [PubMed] [Google Scholar]
- 51.Sindhusake D, Golding M, Newall P, Rubin G, Jakobsen K, Mitchell P. Risk factors for tinnitus in a population of older adults: the Blue Mountains Hearing Study. Ear Hear. 2003;24(6):501–507. doi: 10.1097/01.AUD.0000100204.08771.3D [DOI] [PubMed] [Google Scholar]
- 52.Folmer RL, Griest SE. Chronic tinnitus resulting from head or neck injuries. Laryngoscope. 2003;113(5):821–827. doi: 10.1097/00005537-200305000-00010 [DOI] [PubMed] [Google Scholar]
- 53.Tranter RMD, Graham JR. A review of the otological aspects of whiplash injury. J Forensic Leg Med. 2009;16(2):53–55. doi: 10.1016/j.jflm.2008.09.001 [DOI] [PubMed] [Google Scholar]
- 54.Zeigelboim BS, Fonseca VR, Mesti JC, Gorski LP, Faryniuk JH, Marques JM. Neurotological findings at a health unit for adults with cervicalgia. Int Arch Otorhinolaryngol. 2016;20(2):109–113. doi: 10.1055/s-0036-1572563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bernhardt O, Mundt T, Welk A, et al. Signs and symptoms of temporomandibular disorders and the incidence of tinnitus. J Oral Rehabil. 2011;38(12):891–901. doi: 10.1111/j.1365-2842.2011.02224.x [DOI] [PubMed] [Google Scholar]
- 56.Michiels S, De Hertogh W, Truijen S, Van De Heyning P. Cervical spine dysfunctions in patients with chronic subjective tinnitus. Otol Neurotol. 2015;36(4):741–745. doi: 10.1097/MAO.0000000000000670 [DOI] [PubMed] [Google Scholar]
- 57.Lee C-F, Lin M-C, Lin H-T, Lin C-L, Wang T-C, Kao C-H. Increased risk of tinnitus in patients with temporomandibular disorder: a retrospective population-based cohort study. Eur Arch Oto Rhino Laryngol. 2016;273(1):203–208. doi: 10.1007/s00405-015-3491-2 [DOI] [PubMed] [Google Scholar]
- 58.Porto De Toledo I, Stefani FM, Porporatti AL, et al. Prevalence of otologic signs and symptoms in adult patients with temporomandibular disorders: a systematic review and meta-analysis. Clin Oral Investig. 2017;21(2):597–605. doi: 10.1007/s00784-016-1926-9 [DOI] [PubMed] [Google Scholar]
- 59.Haider HF, Hoare DJ, Costa RFP, et al. Pathophysiology, diagnosis and treatment of somatosensory tinnitus: a scoping review. Front Neurosci. 2017;11(Apr). doi: 10.3389/fnins.2017.00207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.El-Shunnar SK, Hoare DJ, Smith S, et al. Primary care for tinnitus: practice and opinion among GPs in England. J Eval Clin Pract. 2011;17(4):684–692. doi: 10.1111/j.1365-2753.2011.01696.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- NICE CKS (2017). Tinnitus. Available from: https://cks.nice.org.uk/tinnitus. Accessed May 11, 2018.