Abstract
Objective:
To examine patterns of prescription opioid use before TJR and factors associated with continuous use of opioids before TJR.
Design:
We conducted an observational cohort study among Medicare enrollees aged ≥65 years who underwent TJR between 2010 and 2014. Preoperative opioid use was defined as having any opioid prescription in the 12-month period before TJR. Patients who had an opioid prescription every month for a 12-month period were defined as continuous users. We examined patients’ demographics, pain-related conditions, medication use, other comorbidities, healthcare utilization and their association with use of opioids before TJR.
Results:
A total of 473,781 patients underwent TJR: 155,516 THR and 318,265 TKR. Among the total cohort, 60.2% patients had any use of opioids and of those, 12.4% used opioids at least once a month continuously over the 12-month baseline period. Correlates of continuous opioid use included African American race (OR=2.14, 95% CI=2.01-2.28, compared to White patients), history of drug abuse (OR=5.18, 95% CI=3.95-6.79) and back pain (OR=2.32, 95% CI=2.24-2.39).
Conclusions:
In this large cohort of patients undergoing TJR, over 60% ever used opioids and 12.4% of them continuously used opioids in the 12-month prior to surgery. Utilization of opioids became more frequent and high-dosed near the surgery. History of drug abuse, back pain, and African American race were strongly associated with continuous use of opioids preoperatively. Further research is needed to determine short-term and long-term risks of preoperative use of opioids in TJR patients and to optimize pre- and post-TJR pain management of patients with arthritis.
Keywords: total joint replacement, opioids, osteoarthritis
Introduction
Pain is the primary symptom of osteoarthritis (OA), which is one of the leading causes of disability in the U.S. Pain significantly impacts patients’ quality of life and results in public health burden 1. Physicians often start with lifestyle modifications for OA patients including exercise, weight loss, and pharmacologic therapies such as acetaminophen, non-steroidal anti-inflammatory drugs (NSAIDs), intraarticular glucocorticoids, and opioids. For patients who have inadequate response to these lifestyle modifications or pharmacologic therapies, total joint replacement (TJR) is sometimes selected as a treatment for severe symptomatic OA 2. There has been a dramatic increase in the utilization of total hip (THR) and total knee replacement (TKR) over the last decades, where134% increase in TKR alone was observed from1999 to 2008 3,4. In recent years, over 1 million THR and TKR were performed annually, and the demand for both procedures are projected to increase largely by 2030 5,6.
To date, guidelines for preoperative opioid use have been inconsistent 2,7-9. The prevalence of opioid use is particularly high among the older population, possibly due to accumulating evidence of cardiovascular risk of NSAIDs in patients with multiple comorbidities 10. Among Medicare enrollees, 40% of patients with knee OA had at least one opioid prescription in 2009, and over half of patients who underwent TKR had opioids prior to the surgery 11,12. However, increasing utilization of opioids raised concerns about their side effects of prolonged opioid dependence and poor clinical outcomes after TJR. A number of observational studies have demonstrated associations between preoperative opioid use and postoperative opioid dependence and other adverse clinical outcomes after surgery like stiffness, continued pain, and early revisions 13-17.
Appropriate preoperative pain management for arthritis patients remains an unresolved issue for clinicians and surgeons. The objectives of this study were to characterize the patterns of prescription opioid use in the year before undergoing TJR and to identify clinical factors associated with preoperative opioid use patterns.
Method
Data source
We used Medicare claims data (Parts A/B/D 2010-2014) to conduct a cohort study among individuals who underwent TJR. Medicare is a federally funded program that provides health care coverage for nearly all legal residents of the US age 65 and older and some disabled patients younger than 65. Medicare Part A generally covers inpatient care, Part B covers outpatient medical services including some drugs given in a physician’s office or clinic, and Part D covers outpatient prescription drugs. A random sample of one million records of either total hip replacement (THR) or total knee replacement (TKR) during the study period from 2010 to 2014 were obtained from Center for Medicare & Medicaid Services (CMS). The protocol was reviewed and approved by the Brigham and Women’s Health Institutional Review Board.
Study population
Patients who underwent primary TJR were identified using International Classifications of Disease, Ninth Revision, Clinical Modification (ICD-9 CM) codes of 81.51 or 81.54 from the inpatient claims file. We defined cohort entry date (i.e., index date) as the date of the first THR or TKR. We selected patients aged ≥65 years old on the index date and at least 360 days free of TJR before the index date. We required patients to have continuous enrollment in Medicare Parts A, B, and D for at least 360 days before the index date, allowing gaps of ≤ 30 days. Patients without any claims in the 360-day baseline period or those who had both THR and TKR on the same day were excluded. We excluded patients who had both THR and TKR because these patients may have different pain levels and management compared to the rest of the cohort.
Covariates
During the 360-day period prior to TJR, we assessed variables potentially associated with opioid use, including demographics (age, sex, race, region), pain/fracture conditions (falls, migraine, neuropathy, back pain, fractures), other comorbidities (combined comorbidity score, hyperlipidemia, hypertension, atrial fibrillation, heart failure, coronary heart disease, stroke, chronic kidney disease, diabetes, obesity, malignancy, use of tobacco, drug abuse, osteoporosis, psychosis, depression, sleep disorder, and anxiety), medication use (non-selective non-steroidal anti-inflammatory drugs, selective cox-2 inhibitors, corticosteroids, anticonvulsants, antidepressants, antipsychotics, benzodiazepines, other anxiolytics, and total number of unique prescriptions by generic name), and healthcare utilization (emergency room visit, physician visits, and any hospitalization). These covariates were defined using ICD-9-CM diagnosis/procedure code, Current Procedural Terminology (CPT) code, or National Drug Codes (NDC, for medications).
Opioid use
We identified prescription opioids based on 16 different generic names, including: buprenorphine, codeine, dihydrocodeine, fentanyl, hydrocodone, hydromorphone, levorphanol, meperidine, methadone, morphine, oxycodone, oxymorphone, pentazocine, propoxyphene, tapentadol, and tramadol. We defined three subgroups from the total cohort based on their pre-operation opioid use: opioid continuous users, ever-users and never-users. To identify continuous users of opioids before the index TJR, we divided 360-day baseline period into 12 consecutive 30-day periods (eFigure 1), where block 1 was furthest from the index TJR date and block 12 was the closest one to the index TJR date. Use of opioids in each 30-day period was assessed by binary indicator of any opioid use or not. Continuous users were patients who had any opioid prescription in each of twelve 30-day periods; ever-users were patients with any opioid dispensing at any time during the 360-day baseline period; and never-users were patients who never had any opioid dispensing at any time during the 360-day baseline period.
Statistical analyses
We summarized baseline patient characteristics of the study cohort by the surgery type (THR or TKR). Opioid types (short- or long-acting), mean morphine milligram equivalent (MME) per day, and proportion of days covered (PDC) of any opioids were assessed. PDC was calculated in each 30-day block as the total number of days of supply of opioids dispensed in a given block divided by 30. MME was calculated using MME conversion factors provided by CMS 18. To examine the associations between pre-operative opioid use and baseline characteristics, we performed multivariable logistic model to estimate the probability of continuous opioid dispensing (yes/no). We built the multivariable logistic regression model by adding in 5 dimensions to the model sequentially: 1) demographics, 2) pain-related conditions, 3) medication use, 4) comorbidities, and 5) healthcare utilization. We used c-statistics to measure and compare the goodness of model fit. C-statistics range between 0.5 and 1: c-statistic 0.5 indicates the model is no better than random chance in predicting an event, and 1 means a perfect prediction of an event. To assess the multi-collinearity between covariates, we examined the variance inflation faction (VIF) of the full model 19. The VIFs of all the covariates were low, ranging between 1.02-2.68 20. We reported the odds ratios (OR) and their 95% confidence intervals (CI) of covariates in the selected model. All analyses were performed using SAS 9.4.
Results
Baseline characteristics
There were initially 1,046,658 claims with TJR identified from January 2010 to December 2014. After applying inclusion and exclusion criteria, 40% claims were eligible for the current study (eFigure 2). Among them, 155,516 were THR procedures and 318,265 were TKR procedures. Most of the patients were White (>90%), and there were more females (>60%) than males. The mean (±standard deviation, SD) age was 75.2 (±6.6) years in the THR group and 73.9 (±5.8) years in the TKR group (Table 1). Volumes of THR and TKR increased over time over the study period. In general, THR patients had more comorbidities than TKR patients, with higher combined comorbidity score, higher rate of cardiovascular diseases and falls/pains. Back pain, neuropathy, and diabetes were common comorbidities in both groups. As expected, non-selective NSAIDs, oral corticosteroids and antidepressants were frequently used.
Table 1.
Selected baseline characteristics of TJR patients, by procedure types
| Covariates | THR | TKR |
|---|---|---|
| N | 155,516 | 318,265 |
| Percentage or mean (±standard deviation) | ||
| Demographics | ||
| Age, years | 75.2 (±6.6) | 73.9 (±5.8) |
| Female | 66.5 | 67.8 |
| Race | ||
| White | 93.6 | 90.4 |
| Black | 4.1 | 4.9 |
| Othersa | 10.5 | 4.7 |
| Region | ||
| MidWest | 28.3 | 28.5 |
| NorthEast | 18.8 | 15.6 |
| South | 34.2 | 38.0 |
| West | 18.6 | 17.7 |
| Index Year | ||
| 2010 | 0.20 | 0.20 |
| 2011 | 20.7 | 21.8 |
| 2012 | 22.7 | 23.1 |
| 2013 | 25.6 | 25.7 |
| 2014 | 30.8 | 29.2 |
| Opioids use | ||
| Any use of opioids | 64.3 | 58.2 |
| Continuous opioids use | 8.0 | 7.2 |
| Any use of long-acting opioids | 5.4 | 3.4 |
| Any use of short-acting opioids | 63.9 | 57.8 |
| Pain-related conditions | ||
| Falls | 10.3 | 5.7 |
| Migraine | 8.4 | 9.4 |
| Neuropathy | 36.0 | 27.6 |
| Back pain | 61.9 | 46.8 |
| Hip fracture | 1.8 | 0.3 |
| Other fracture | 16.0 | 7.3 |
| Other comorbidities | ||
| Combined comorbidity scoreb | 1.5 (±2.5) | 1.1 (±2.2) |
| Hyperlipidemia | 74.9 | 77.4 |
| Hypertension | 81.4 | 84.3 |
| Atrial fibrillation | 15.0 | 13.0 |
| Heart failure | 10.7 | 8.9 |
| Coronary heart disease | 8.9 | 8.1 |
| Stroke | 12.9 | 11.5 |
| Malignancy | 21.3 | 19.0 |
| Diabetes | 26.3 | 31.7 |
| Obesity | 12.4 | 17.1 |
| Chronic kidney disease | 11.7 | 10.8 |
| Tobacco | 17.1 | 12.8 |
| Drug abuse | 0.3 | 0.2 |
| Osteoporosis | 18.2 | 14.6 |
| Psychosis | 2.5 | 1.5 |
| Depression | 16.4 | 15.5 |
| Sleep disorder | 15.8 | 18.0 |
| Anxiety | 12.6 | 11.5 |
| Medication use | ||
| Non-selective NSAIDs | 39.8 | 40.8 |
| Selective coxibs | 10.4 | 9.9 |
| Corticosteroids | 36.3 | 35.5 |
| Anticonvulsants | 17.6 | 16.7 |
| Antidepressants | 28.1 | 29.2 |
| Antipsychotics | 2.4 | 2.1 |
| Benzodiazepines | 10.7 | 10.2 |
| Other anxiolytics | 11.7 | 11.9 |
| Healthcare utilization | ||
| No. of unique prescriptions | 10.2 (±5.8) | 10.6 (±5.8) |
| No. of physician visits | 12.7 (±8.1) | 12.7 (±7.7) |
| Emergency room visit | 31.2 | 26.1 |
Abbreviations: NSAIDs non-steroid anti-inflammatory drugs; COXIBs cyclooxygenase-2 inhibitors
Including Hispanic and other race/ethnics
A combined comorbidity score ranges from −2 to 26, taking into account of 20 common individual conditions.
Any preoperative opioid use
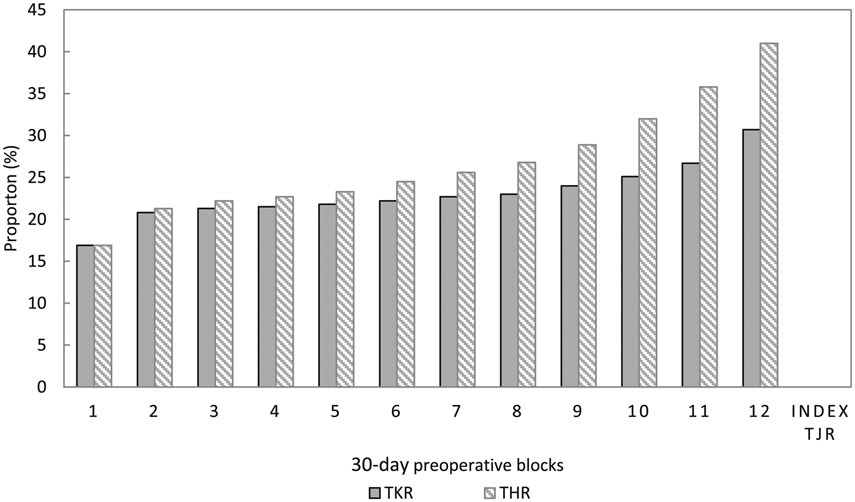
Among the total cohort, 60.5% patients (64.3% of THR and 58.2% of TKR patients) had any opioids in 12 months preceding the surgery. 8% of THR patients used opioids continuously in every 30-day period among THR patients, and 7.2% of TKR patients did so. Of the ever users of opioids, 12.4% were continuous users. Prevalence of any opioid use increased as approaching the index surgery date (Figure 1). Hydrocodone was the most commonly used (45-47% in each month) agent, followed by tramadol (23-30%) and oxycodone (13-18%). There was no significant change in the proportion of each type of opioids used over time prior to the surgery.
Figure 1. Change in any opioid use among overall cohort over time before TJR.
Proportion of any prescription opioid use among overall cohort in each 30-day preoperative blocks by procedure type.
Continuous preoperative opioid use
We further compared baseline characteristics between continuous opioid users and never users (Table 2). 12,381 continuous and 55,455 never users were identified from THR; in the TKR cohort, there were 22,964 continuous and 133,062 never users. Almost all continuous users (99%) used short-acting opioids, and over 20% (27.7% in THR and 20.9% in TKR) used long-acting opioids concomitantly. In both THR and TKR cohorts, continuous users were younger than never users, and there were more female and African Americans among continuous users. Continuous users had more comorbid conditions, concomitant medications and frequent healthcare utilizations than never-users. Particularly, continuous users had more psychiatric comorbidities and used more medications such as benzodiazepines.
Table 2.
Selected baseline covariates for opioids continuous users versus never users
| THR cohort | TKR cohort | |||
|---|---|---|---|---|
| Covariate | Continuous users |
Never users | Continuous users |
Never users |
| N | 12,381 | 55,455 | 22,964 | 133,062 |
| Percentage or mean (±standard deviation) | ||||
| Demographics | ||||
| Age | 74.1 (±6.6) | 75.5 (±6.6) | 72.7 (±5.7) | 74.3 (±5.8) |
| Female | 74.0 | 63.3 | 76.1 | 64.0 |
| Race | ||||
| White | 91.1 | 94.8 | 88.3 | 92.0 |
| Black | 7.1 | 2.7 | 8.1 | 3.4 |
| Othersa | 1.8 | 2.5 | 3.6 | 4.6 |
| Region | ||||
| MidWest | 26.4 | 29.8 | 25.8 | 31.1 |
| NorthEast | 13.2 | 22.4 | 10.5 | 18.6 |
| South | 41.7 | 29.7 | 45.2 | 33.8 |
| West | 18.6 | 18.0 | 18.5 | 16.3 |
| Opioid use | ||||
| Any use of long-acting opioids | 27.7 | - | 20.9 | - |
| Any use of short-acting opioids | 98.8 | - | 98.7 | - |
| Pain-related conditions | ||||
| Falls | 15.0 | 8.3 | 10.9 | 3.0 |
| Migraine | 12.6 | 5.9 | 15.7 | 6.3 |
| Neuropathy | 51.9 | 23.9 | 44.9 | 18.7 |
| Back pain | 79.4 | 48.8 | 71.2 | 35.4 |
| Other fracture | 20.8 | 13.7 | 12.2 | 3.9 |
| Other comorbidities | ||||
| Combined comorbidity scoreb | 2.2 (±2.8) | 1.1 (±2.2) | 1.9 (±2.6) | 0.8 (±1.8) |
| Hyperlipidemia | 73.6 | 73.3 | 75.3 | 76.6 |
| Hypertension | 88.7 | 76.4 | 89.7 | 81.2 |
| Atrial fibrillation | 16.8 | 13.3 | 13.6 | 12.0 |
| Heart failure | 17.9 | 7.6 | 15.3 | 6.3 |
| Coronary heart disease | 12.9 | 6.8 | 11.3 | 6.4 |
| Stroke | 14.5 | 11.1 | 13.6 | 10.1 |
| Malignancy | 18.1 | 20.4 | 16.0 | 18.6 |
| Diabetes | 32.5 | 22.1 | 38.2 | 28.4 |
| Obesity | 17.9 | 8.6 | 22.7 | 13.7 |
| Chronic kidney disease | 16.4 | 8.8 | 16.1 | 8.2 |
| Tobacco | 27.4 | 12.1 | 21.4 | 9.3 |
| Drug abuse | 1.5 | 1.3 | 0.1 | 0.0 |
| Osteoporosis | 22.4 | 15.8 | 18.4 | 12.7 |
| Psychosis | 4.3 | 1.7 | 3.2 | 0.9 |
| Depression | 31.1 | 10.7 | 31.3 | 10.0 |
| Sleep disorder | 24.1 | 10.9 | 27.1 | 13.4 |
| Anxiety | 23.9 | 8.5 | 23.6 | 7.5 |
| Medication use | ||||
| Non-selective NSAIDs | 46.2 | 28.6 | 50.1 | 31.2 |
| COXIBs | 12.2 | 7.5 | 12.1 | 7.5 |
| Corticosteroids | 45.9 | 26.9 | 45.9 | 28.3 |
| Anticonvulsants | 39.0 | 8.6 | 39.9 | 8.9 |
| Antidepressants | 51.2 | 18.5 | 54.0 | 19.9 |
| Antipsychotics | 5.0 | 1.8 | 5.5 | 1.2 |
| Benzodiazepines | 21.1 | 6.2 | 22.3 | 6.2 |
| Other anxiolytics | 22.3 | 6.6 | 24.3 | 7.1 |
| No. of unique prescriptions | 14.9 (±6.5) | 7.0 (±4.4) | 15.5 (±6.7) | 7.8 (±4.5) |
| Healthcare utilization | ||||
| Emergency room visit | 44.2 | 22.3 | 39.3 | 16.2 |
| No. of emergency room visits | 1.0 (±1.9) | 0.3 (±0.8) | 0.8 (±1.7) | 0.2 (±0.6) |
| No. of physician visits | 15.9 (±9.4) | 10.2 (±6.7) | 16.2 (±9.6) | 10.7 (±6.5) |
Abbreviations: NSAIDs non-steroid anti-inflammatory drugs; COXIBs cyclooxygenase-2 inhibitors
Including Hispanic and other race/ethnics
A combined comorbidity score ranges from −2 to 26, taking into account of 20 common individual conditions.
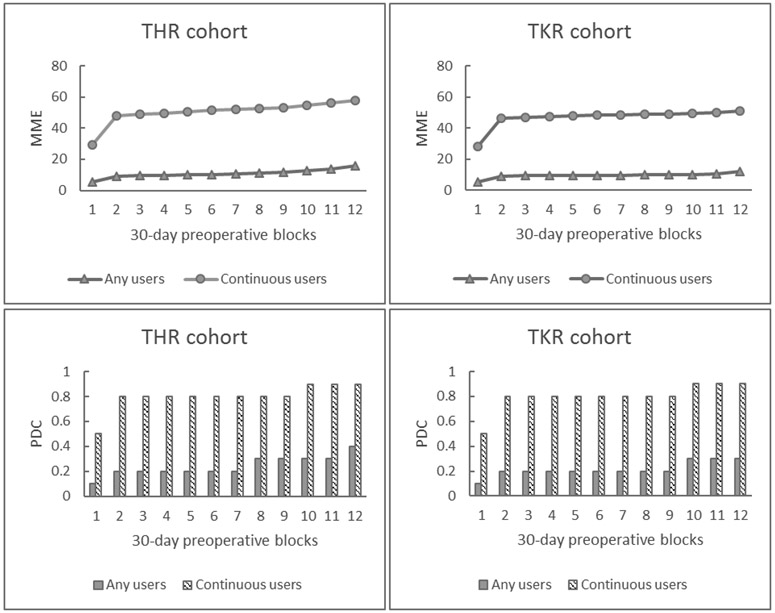
Comparisons of MME and PDC between continuous users and ever-users in each 30-day baseline period showed noticeable differences. MME and PDC were higher in continuous uses at any time point with an increasing trend over time (Figure 2). Continuous users reached > 50 MME per day 30 days before the index surgery and 90% PDC.
Figure 2. Pattern of opioid use over time before TJR.
Mean daily opioid morphine milligram equivalents (MME) and proportion of days covered (PDC) during 30-day preoperative periods among any users versus continuous users, stratified by procedure type (THR or TKR).
Factors associated with continuous preoperative opioid use
In the first step of multivariable logistic regression analysis with demographic factors only, the model had a c-statistic of 0.645. It was increased to 0.761 after adding pain-related conditions (listed in Table 3) to the model. Further including use of other medications to the model greatly increased the model goodness of fit (c-statistic 0.880). After adding other comorbidities and healthcare utilization, the final model with all covariates had a c-statistic of 0.885.
Table 3.
Factors associated with continuous use of opioids before TJR.
| Covariates | ORa (95% CI), continuous vs never use of opioids | ||
|---|---|---|---|
| Total cohort | THR cohort | TKR cohort | |
| Index TJR | |||
| TKR vs THR | 0.73 (0.71, 0.76) | - | - |
| Demographics | |||
| Index year | |||
| 2010 vs 2014 | 1.62 (1.19, 2.20) | 1.59 (0.94, 2.67) | 1.65 (1.13, 2.42) |
| 2011 vs 2014 | 1.38 (1.33, 1.44) | 1.36 (1.26, 1.47) | 1.40 (1.32, 1.47) |
| 2012 vs 2014 | 1.35 (1.30, 1.41) | 1.38 (1.28, 1.48) | 1.34 (1.27, 1.41) |
| 2013 vs 2014 | 1.10 (1.06, 1.15) | 1.12 (1.04, 1.19) | 1.10 (1.04, 1.15) |
| Age | 0.97 (0.97, 0.97) | 0.97 (0.97, 0.98) | 0.97 (0.96, 0.97) |
| Gender | |||
| Female vs male | 1.10 (1.06, 1.14) | 1.17 (1.10, 1.24) | 1.06 (1.02, 1.11) |
| Race | |||
| African American vs White | 2.14 (2.01,2.28) | 2.41 (2.14, 2.72) | 2.05 (1.90, 2.21) |
| Othersb vs White | 0.52 (0.48, 0.57) | 0.59 (0.49, 0.71) | 0.52 (0.47, 0.57) |
| Region | |||
| West vs NorthEast | 1.98 (1.88, 2.08) | 1.87 (1.72, 2.04) | 2.05 (1.92, 2.19) |
| South vs NorthEast | 1.89 (1.80, 1.98) | 1.82 (1.69, 1.96) | 1.95 (1.84, 2.06) |
| MidWest vs NorthEast | 1.51 (1.43, 1.58) | 1.52 (1.40, 1.64) | 1.50 (1.41, 1.59) |
| Others vs NorthEast | 0.30 (0.17, 0.52) | 0.54 (0.23, 1.27) | 0.20 (0.09, 0.44) |
| Pain-related conditions | |||
| Falls | 1.12 (1.06, 1.19) | 1.00 (0.91, 1.11) | 1.31 (1.21, 1.41) |
| Migraine | 0.83 (0.79, 0.87) | 0.73 (0.66, 0.80) | 0.88 (0.83, 0.94) |
| Neuropathy | 1.30 (1.26, 1.35) | 1.41 (1.33, 1.49) | 1.25 (1.20, 1.30) |
| Back pain | 2.32 (2.24, 2.39) | 2.23 (2.10, 2.37) | 2.34 (2.25, 2.43) |
| Hip fracture | 0.63 (0.54, 0.75) | 0.65 (0.53, 0.80) | 0.86 (0.63, 1.16) |
| Other fracture | 1.32 (1.25, 1.39) | 1.04 (0.96, 1.13) | 1.75 (1.63, 1.88) |
| Other comorbidities | |||
| Combined comorbidity scorec | 0.98 (0.97, 0.99) | 0.98 (0.97, 1.00) | 0.99 (0.98, 1.00) |
| Hyperlipidemia | 0.60 (0.58, 0.62) | 0.59 (0.56, 0.63) | 0.60 (0.57, 0.62) |
| Hypertension | 1.12 (1.07, 1.18) | 1.21 (1.12, 1.31) | 1.08 (1.02, 1.15) |
| Atrial fibrillation | 0.80 (0.77, 0.84) | 0.82 (0.75, 0.88) | 0.79 (0.74, 0.83) |
| Heart failure | 1.06 (1.00, 1.12) | 1.04 (0.95, 1.14) | 1.07 (1.00, 1.14) |
| Coronary heart disease | 0.91 (0.86, 0.95) | 0.91 (0.83, 1.00) | 0.90 (0.84, 0.96) |
| Stroke | 0.76 (0.72, 0.80) | 0.72 (0.67, 0.78) | 0.78 (0.73, 0.82) |
| Malignancy | 0.82 (0.79, 0.85) | 0.81 (0.76, 0.87) | 0.82 (0.78, 0.86) |
| Diabetes | 0.74 (0.72, 0.77) | 0.75 (0.70, 0.80) | 0.74 (0.71,0.78) |
| Obesity | 1.09 (1.04, 1.13) | 1.21 (1.12, 1.31) | 1.04 (0.99, 1.09) |
| Chronic kidney disease | 1.20 (1.14, 1.26) | 1.09 (0.99, 1.19) | 1.25 (1.18, 1.34) |
| Tobacco | 1.65 (1.58, 1.71) | 1.68 (1.57, 1.80) | 1.64 (1.56, 1.72) |
| Drug abuse | 5.18 (3.95, 6.79) | 3.89 (2.56, 5.93) | 6.72 (4.68, 9.66) |
| Osteoporosis | 1.04 (1.00, 1.08) | 1.04 (0.97, 1.12) | 1.04 (0.99, 1.09) |
| Psychosis | 0.75 (0.68, 0.84) | 0.74 (0.62, 0.88) | 0.79 (0.69, 0.92) |
| Depression | 1.14 (1.09, 1.19) | 1.07 (1.00, 1.16) | 1.16 (1.11, 1.23) |
| Sleep disorder | 0.90 (0.87, 0.94) | 0.90 (0.84, 0.97) | 0.90 (0.86, 0.94) |
| Anxiety | 1.13 (1.08, 1.18) | 1.09 (1.01, 1.18) | 1.16 (1.10, 1.22) |
| Medication use | |||
| Non-selective NSAIDs | 1.09 (1.05, 1.12) | 1.06 (1.00, 1.12) | 1.09 (1.05, 1.13) |
| COXIBs | 1.01 (0.97, 1.06) | 1.01 (0.93, 1.10) | 1.01 (0.95, 1.07) |
| Corticosteroids | 0.70 (0.68, 0.73) | 0.67 (0.63, 0.71) | 0.72 (0.69, 0.75) |
| Anticonvulsants | 2.11 (2.03, 2.18) | 2.16 (2.03, 2.29) | 2.08 (1.99, 2.17) |
| Antidepressants | 1.40 (1.35, 1.45) | 1.42 (1.33, 1.51) | 1.39 (1.33, 1.45) |
| Antipsychotics | 0.64 (0.58, 0.70) | 0.48 (0.41,0.57) | 0.75 (0.67, 0.83) |
| Benzodiazepines | 1.68 (1.60, 1.76) | 1.55 (1.42, 1.68) | 1.75 (1.65, 1.85) |
| Other anxiolytics | 1.44 (1.38, 1.50) | 1.35 (1.25, 1.45) | 1.50 (1.42, 1.57) |
| Healthcare utilization | |||
| No. of unique prescriptions | 0.99 (0.99, 1.00) | 1.00 (0.99, 1.00) | 0.99 (0.99, 0.99) |
| No. of physician visits | 1.13 (1.11, 1.15) | 1.09 (1.06, 1.13) | 1.17 (1.14, 1.19) |
| No. of emergency room visits | 1.25 (1.24, 1.25) | 1.28 (1.27, 1.29) | 1.23 (1.23, 1.24) |
Abbreviations: NSAIDs non-steroid anti-inflammatory drugs; COXIBs cyclooxygenase-2 inhibitors
Adjusted for all the covariates in this table.
Including Hispanic and other race/ethnics
A combined comorbidity score ranges from −2 to 26, taking into account of 20 common individual conditions.
The final multivariable logistic regression model identified several risk factors associated with continuous use versus never use (Table 3). Compared to the index TJR in 2014, patients who had TJR in previous years (2010-2013) were significantly more likely to use opioids continuously before the surgery. For African Americans had over two-fold odds of continuously using opioid before TJR compared to White Americans (OR=2.14, 95% CI=2.01-2.28) after adjusting for other variables. In contrast, the other race/ethnicity group had 48% lower odds of continuous opioid use (OR=0.52, 95% CI=0.48-0.57). In addition, we observed significant associations between geographic region with continuous opioid use. Compared with patients in the Northeast, patients in the West and South had almost 2-fold odds of being continuous opioid users. Living in the Midwest was also associated with higher odds of continuous opioid use.
Pain-related conditions including neuropathy, back pain, and fractures (excluding hip fracture) were more likely associated with continuous opioid use. Particularly, patients with back pain had more than 2-fold increased odds of receiving opioids continuously compared with those without back pain (OR = 2.32, 95% CI = 2.24-2.39). While a history of hip fracture had a reverse association with continuous opioid use among THR cohort (OR = 0.65, 95% CI = 0.53-0.80), the number of hip fracture patients was very small and some of patients likely underwent THR due to a hip fracture. Specifically, among patients with history of hip fracture (1.8%) in THR cohort, more than 50% had the diagnosis within 30 days prior to their index THR date. In both TKR and THR cohorts, patients with migraine had about 20% lower odds of using opioids continuously prior to the surgery.
After accounting for some common baseline comorbidities, drug abuse was strongly associated with increased odds of continuous opioid use (OR=5.18, 95% CI=3.95-6.79). Patients with hyperlipidemia, atrial fibrillation, stroke, diabetes, and psychosis were less likely to be on long-term opioid use. Interestingly, both psychosis comorbidity (OR = 0.75, 95% CI 0.68-0.84) and use of antipsychotics (OR = 0.64, 95% CI = 0.58-0.70) were associated with decreased odds of continuous opioid use prior to surgery. Use of corticosteroid also showed a negative association with being continuous users of opioids (OR = 0.70, 95% CI = 0.68-0.73). However, presence of depression, anxiety or use of related medications such as antidepressants, benzodiazepines, or other anxiolytics was associated with an increased likelihood of continuous opioid use. Use of anticonvulsants was associated with a 2-fold greater odds of using opioid continuously before the TJR. We found no association between number of prescription drugs and continuous opioid use; however, continuous opioid users were more likely to see physicians or have visits to the emergency room. We observed similar patterns of associations among THR and TKR cohorts.
Discussion
In this large cohort study of Medicare enrollees who underwent TJR, 60.2% of patients used opioids at least once during the baseline period. Of those, 12.4% used opioids continuously for 12 months. Compared to any opioid users, continuous users received higher doses (>50 MME) of opioids more frequently (PDC=90%) in the month prior to the surgery. Factors strongly associated with preoperative continuous opioid use were earlier calendar year of surgery (i.e., 2010-2013 versus 2014), African American (versus White), and history of drug abuse and back pain. While a few prior studies have reported association between patients’ characteristics and persistent opioid use after surgery, none of them studied risk factors of preoperative continuous opioid use 12,21-23. We presented important preoperative characteristics of patients who are at risk for prolonged preoperative opioid use, which adds another valuable piece of evidence for clinicians in pain management strategy decisions. However, one must be cautious to not over-interpret the findings; we examined mostly cross-sectional associations between patients’ pattern of opioid use and their characteristics prior to the surgery; thus we cannot exclude the possibility of reverse causation.
In this current study, we observed a similar prevalence of opioid use as seen in previous studies. Politzer et al. reported 54.8% preoperative opioid use among TKR patients 23 compared to 60.2% among both THR and TKR patients in our study. Bedard et al. reported 32.4% opioid use in 3-month preoperative period among TKR patients 21, which is also similar to our estimation (25.1, 26.7, and 30.7% in 3 months prior to the surgery in TKR group). Our study showed a steadily increasing trend of any opioid use over the 12-month period prior to the surgery, with higher daily MME and PDC closer to the surgery date. It is likely that these findings are related to the progression in arthritic pain over time, inadequate response to prior pharmacologic therapy, and/or development of tolerance to opioids which required higher doses. Hydrocodone was the most commonly used opioid, followed by tramadol and oxycodone. This is consistent with findings from Kim et al. and Politzer et al. 22,23 Both of these studies identified hydrocodone as the most frequently used opioids prior to the surgery 24. Despite hydrocodone being used more frequently, tramadol is generally considered safer than other opioids, and some treatment guidelines recommend tramadol as one of the pharmacological therapies before other opioids 2,7,25 This discrepancy highlights one of the gaps that exist between treatment guidelines and real-world practice in pain management for OA patients.
According to the Center for Disease Control and Prevention (CDC) guideline for prescribing opioids for chronic pain, when starting opioids therapy for chronic pain is necessary, clinicians are suggested to start with immediate-release (short-acting) opioids and to prescribe the lowest effective dose as possible. The CDC guideline also adds that opioid dosage of ≥50 MME/day should be considered carefully and increasing dosage to ≥90 MME/day should be avoided. Many studies have reported that longer duration of opioid use, higher MME, and higher PDC prior to the surgery were positively associated with persistent opioid use after surgery 12,13,21,22. The present study estimated 8.0% continuous opioid users in THR and 7.2% in TKR who had any opioids in every month during 12-month preoperative period. These continuous users might be particularly at high risk of opioid addiction and adverse clinical outcomes after the surgery since they also had higher average daily MME and PDC compared to any opioid users. Although 99% of opioid users in the total cohort were prescribed short-acting agents, more than 20% of patients also used long-acting opioids concomitantly, which would likely impose higher risk of opioid addiction or opioid-related adverse outcomes. Our study results suggest that the pattern of opioid use in practice still needs careful evaluation to identify the underlying rationales for clinicians’ decisions regarding opioid type and find a balance between safe opioid use and effective pain management.
While most (>90%) of patients undergoing TJR in our study cohort were White and only 4% were African Americans, we found 60% higher odds of continuous opioid use among African Americans versus White. A number of studies have shown racial disparity in receipt of TJR, and such disparity is growing 26-28. Higher prevalence of continuous opioid use among African Americans could be partly due to multi-level barriers prior to the final decision on the TJR surgery. These barriers include differential access to healthcare facilities, surgeon preferences, and patient preference, acceptance or expectations of the surgery 27,29. Furthermore, the present study showed associations between geographic regions and continuous opioid use prior to TJR, where patients from the Midwest and South were more likely to be continuous opioid users compared to patients from the Northeast. In a previous study, our research group showed that regional variation was a key determinant of long-term opioid use among patients who underwent TJR 30.
This study also highlights the strong association between back pain and continuous use of opioids. This is not surprising as opioids are reported to be the most commonly prescribed drug class for low back pain in the U.S. 31. Patients with both OA and low back pain may have more widespread pain and higher pain intensity, requiring stronger pain medications like opioids. Whether use of chronic opioids regardless of the indication (i.e., for knee or hip OA versus back pain) has any impact on post-TJR outcome needs to be further studied. If it does, a better preoperative management strategy for their OA as well as other painful condition such as back pain needs to be implemented.
Migraine showed a negative association with continuous opioid use, where the association is in opposite direction compared to other pain-related conditions like neuropathy, back pain, and fractures (excluding hip fracture). While we are unable to fully explain these different associations, continuous opioid use pattern appears to be more likely associated with chronic or severe pain conditions.
We also observed several patients who were diagnosed with drug abuse (Table 1). As expected, drug abuse was strongly associated with opioid use. Since prescription opioid abuse itself is also considered drug abuse, some of these patients might already have misused opioids before surgery, while some abused other drugs (i.e. sedative, hypnotic or anxiolytic, cocaine, cannabis, amphetamine, and hallucinogen) or combinations of opioids and other drugs. It is also possible that some patients abused multiple substances at the same time, which could enhance the toxicity and increase the risk of death. However, we were unable to differentiate between specific types of drug abuse.
Concomitant use of benzodiazepines should be avoided in patients on opioids because of increased potential for drug abuse and risk of emergency care due to drug overdose 32-34. Nevertheless, we observed more than 20% of continuous users had benzodiazepines prescribed during the same time and positive associations between continuous opioid use and use of benzodiazepines, anticonvulsants, and antipsychotics. Our results of positive associations between continuous opioid use and anticonvulsants, antidepressants, benzodiazepines, and other anxiolytics are consistent with findings from previous studies 35-38, adding further evidence for caution in the management of chronic pain in patients with mental health issues.
Our study has several strengths. First, we investigated a large cohort of 473,781 TJR patients enrolled in Medicare. Thus, the study has high generalizability to older patients in the U.S. Second, we evaluated both THR and TJR patients whereas only few previous observational studies did so, even though both THR and TKR are common in the U.S. and share many similar treatment patterns and risk factors. Third, our large cohort size enabled us to examine more detailed patterns of preoperative opioid use in monthly intervals which revealed deeper insights to trends in opioid use during the months preceding surgery. Furthermore, this study included comprehensive data on patients’ demographics, comorbidities, medication use, and history of healthcare utilizations so that we could control for confounding in different dimensions.
This study has limitations. First, we did not have a direct measure for severity of disease/pain scores and whether patients used opioids for other diseases than hip and knee OA. However, we included pain-related comorbidities and other medications commonly used for pain management as covariates to account for this issue. Second, while our study was based on administrative claims data with detailed prescription information, we were unable to verify whether patients consumed the opioids as prescribed. Third, 360-day baseline period may not be long enough to capture true incident TJR in some patients as it is possible that prior TJRs may have occurred beyond 360-day baseline period or our data availability (2010). Fourth, in the current study, ICD-9 procedure codes that we used to define TJR procedure cannot differentiate whether patients went through unilateral or bilateral THR/TKR. Fifth, this study did not examine association between prescriber’s specialty and opioid use. Lastly, as an inherent issue of claim-based observational studies, our study relied on diagnosis and procedure code-based algorithms to identify various baseline characteristics, leading to potential misclassification.
Conclusion
In this large, population-based cohort of elderly patients undergoing TJR, 60.2% of patients were prescribed opioids at least once. Of those, 12.4% used opioids continuously for 12 consecutive months prior to their surgeries. In both THR and TKR cohorts, opioid utilization became more frequent and high-dosed near the surgery date. Earlier year of surgery, African Americans and presence of back pain or drug abuse history were associated with continuous use of opioids before TJR. Understanding patterns of prescription opioid use prior to TJR would help optimize pain management for patients during and after the surgery. Further efforts are needed to carefully determine risks and benefits of opioids for patients based on their individual characteristics before and after TJR and to minimize the adverse outcomes due to the chronic preoperative opioid use.
Supplementary Material
Acknowledgments
Funding source:
This study was supported by grants from the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases (Grant Number: 1R01AR069557-01A1)
Role of the funding source
The study sponsor was not involved in the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing interests
The authors do not have competing interests. YCL received a research grant from Pfizer and stock in Express Scripts. SCK received research grants to Brigham and Women’s Hospital from Pfizer, Roche and Bristol-Myers Squibb for unrelated studies.
References
- 1.Theis KA, Roblin DW, Helmick CG, Luo R. Prevalence and causes of work disability among working-age U.S. adults, 2011-2013, NHIS. Disability and health journal. January 2018;11(1):108–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis care & research. April 2012;64(4):465–474. [DOI] [PubMed] [Google Scholar]
- 3.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991–2010. JAMA. 2012;308(12):1227–1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The Dramatic Increase in Total Knee Replacement Utilization Rates in the United States Cannot Be Fully Explained by Growth in Population Size and the Obesity Epidemic. The Journal of Bone and Joint Surgery. American volume. February/01 2012;94(3):201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maradit Kremers H, Larson DR, Crowson CS, et al. Prevalence of Total Hip and Knee Replacement in the United States. The Journal of bone and joint surgery. American volume. September 2 2015;97(17):1386–1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. The Journal of bone and joint surgery. American volume. April 2007;89(4):780–785. [DOI] [PubMed] [Google Scholar]
- 7.Hauk L Treatment of knee osteoarthritis: a clinical practice guideline from the AAOS. American family physician. June 1 2014;89(11):918–920. [PubMed] [Google Scholar]
- 8.McAlindon TE, Bannuru RR, Sullivan MC, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis and cartilage. March 2014;22(3):363–388. [DOI] [PubMed] [Google Scholar]
- 9.Pendleton A, Arden NK, Dougados M, et al. EULAR recommendations for the management of knee osteoarthritis. Report of a task force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Vol 592001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trelle S, Reichenbach S, Wandel S, et al. Cardiovascular safety of non-steroidal anti-inflammatory drugs: network meta-analysis. BMJ. 2011;342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wright EA, Katz JN, Abrams S, Solomon DH, Losina E. Trends in Prescription of Opioids From 2003–2009 in Persons With Knee Osteoarthritis. Arthritis care & research. 2014;66(10):1489–1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hansen CA, Inacio MCS, Pratt NL, Roughead EE, Graves SE. Chronic Use of Opioids Before and After Total Knee Arthroplasty: A Retrospective Cohort Study. The Journal of Arthroplasty. 2017/March/01/ 2017;32(3):811–817.e811. [DOI] [PubMed] [Google Scholar]
- 13.Zywiel MG, Stroh DA, Lee SY, Bonutti PM, Mont MA. Chronic opioid use prior to total knee arthroplasty. JBJS. 2011;93(21):1988–1993. [DOI] [PubMed] [Google Scholar]
- 14.Joseph P, H BR, Keith B, et al. Opioids and the Management of Chronic Severe Pain in the Elderly: Consensus Statement of an International Expert Panel with Focus on the Six Clinically Most Often Used World Health Organization step III Opioids (Buprenorphine, Fentanyl, Hydromorphone, Methadone, Morphine, Oxycodone). Pain Practice. 2008;8(4):287–313. [DOI] [PubMed] [Google Scholar]
- 15.Fisher DA, Dierckman B, Watts MR, Davis K. Looks good but feels bad: factors that contribute to poor results after total knee arthroplasty. J Arthroplasty. September 2007;22(6 Suppl 2):39–42. [DOI] [PubMed] [Google Scholar]
- 16.Franklin PD, Karbassi JA, Li W, Yang W, Ayers DC. Reduction in narcotic use after primary total knee arthroplasty and association with patient pain relief and satisfaction. J Arthroplasty. September 2010;25(6 Suppl):12–16. [DOI] [PubMed] [Google Scholar]
- 17.Pivec R, Issa K, Naziri Q, Kapadia BH, Bonutti PM, Mont MA. Opioid use prior to total hip arthroplasty leads to worse clinical outcomes. International orthopaedics. June 2014;38(6):1159–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Factors OOMMEMC. https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Opioid-Morphine-EQ-Conversion-Factors-Aug-2017.pdf. 2017.
- 19.Neter J, Wasserman W, Kutner M. Applied Linear Statistical Models (3rd Edition). The Journal of the Operational Research Society. 1991;42(9):815. [Google Scholar]
- 20.Vatcheva KP, Lee M, McCormick JB, Rahbar MH. Multicollinearity in Regression Analyses Conducted in Epidemiologic Studies. Epidemiology (Sunnyvale, Calif.). 2016;6(2):227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.A. BN, E. DD, B. DS, J. CJ. Trends and risk factors for prolonged opioid use after unicompartmental knee arthroplasty. The Bone & Joint Journal. 2018;100-B(1_Supple_A):62–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim SC, Choudhry N, Franklin JM, et al. Patterns and predictors of persistent opioid use following hip or knee arthroplasty. Osteoarthritis and cartilage. September 2017;25(9):1399–1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Politzer CS, Kildow BJ, Goltz DE, Green CL, Bolognesi MP, Seyler TM. Trends in Opioid Utilization Before and After Total Knee Arthroplasty. The Journal of Arthroplasty. 2017/November/14/ 2017. [DOI] [PubMed] [Google Scholar]
- 24.Smith SRBA, Bido JBA, Collins JEP, Yang HMSMPH, Katz JNMDM, Losina EPa. Impact of Preoperative Opioid Use on Total Knee Arthroplasty Outcomes. Journal of Bone & Joint Surgery - American Volume. 2017;99(10):803–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Solomon DH, Rassen JA, Glynn RJ, et al. The comparative safety of opioids for nonmalignant pain in older adults. Archives of Internal Medicine. 2010;170(22):1979–1986. [DOI] [PubMed] [Google Scholar]
- 26.Racial disparities in total knee replacement among Medicare enrollees -- United States, 2000-2006. MMWR: Morbidity & Mortality Weekly Report. 2009;58(6):133–138. [PubMed] [Google Scholar]
- 27.Bang H, Chiu YL, Memtsoudis SG, et al. Total hip and total knee arthroplasties: trends and disparities revisited. American journal of orthopedics (Belle Mead, N.J.). September 2010;39(9):E95–102. [PubMed] [Google Scholar]
- 28.Katz BP, Freund DA, Heck DA, et al. Demographic variation in the rate of knee replacement: a multi-year analysis. Health services research. June 1996;31(2):125–140. [PMC free article] [PubMed] [Google Scholar]
- 29.Kerman HM, Smith SR, Smith KC, et al. Disparities in total knee replacement: Population losses in quality-adjusted life years due to differential offer, acceptance, and complication rates for Black Americans. Arthritis care & research. January 24 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Desai RJ, Jin Y, Franklin PD, et al. Association of geography and access to healthcare providers with long term prescription opioid use in Medicare patients with severe osteoarthritis: A cohort study. Arthritis & rheumatology (Hoboken, N.J.). 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ivanova JI, Birnbaum HG, Schiller M, Kantor E, Johnstone BM, Swindle RW. Real-world practice patterns, health-care utilization, and costs in patients with low back pain: the long road to guideline-concordant care. The Spine Journal. 2011/July/01/ 2011;11(7):622–632. [DOI] [PubMed] [Google Scholar]
- 32.Jann M, Kennedy WK, Lopez G. Benzodiazepines: A Major Component in Unintentional Prescription Drug Overdoses With Opioid Analgesics. Journal of Pharmacy Practice. 2014/February/01 2014;27(1):5–16. [DOI] [PubMed] [Google Scholar]
- 33.Jones JD, Mogali S, Comer SD. Polydrug abuse: A review of opioid and benzodiazepine combination use. Drug & Alcohol Dependence. 2012;125(1):8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Braden JB, Sullivan MD, Ray GT, et al. Trends in long-term opioid therapy for noncancer pain among persons with a history of depression. General Hospital Psychiatry. 2009/November/01/ 2009;31(6):564–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Musich S, Wang SS, Slindee L, Kraemer S, Yeh CS. Prevalence and characteristics associated with high dose opioid users among older adults. Geriatric Nursing. 2019/January/01/ 2019;40(1):31–36. [DOI] [PubMed] [Google Scholar]
- 36.Parsells Kelly J, Cook SF, Kaufman DW, Anderson T, Rosenberg L, Mitchell AA. Prevalence and characteristics of opioid use in the US adult population. PAIN. 2008/September/15/ 2008;138(3):507–513. [DOI] [PubMed] [Google Scholar]
- 37.Eriksen J, SjØgren P, Bruera E, Ekholm O, Rasmussen NK. Critical issues on opioids in chronic non-cancer pain:: An epidemiological study. Pain. 2006/November/01/ 2006;125(1):172–179. [DOI] [PubMed] [Google Scholar]
- 38.Braden JB, Zhang L, Fan M-Y, Unützer J, Edlund MJ, Sullivan MD. Mental Health Service Use by Older Adults: The Role of Chronic Pain. The American Journal of Geriatric Psychiatry. 2008/February/01/ 2008;16(2):156–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.