Abstract
Registries are fundamental to the success of population health initiatives to improve care and outcomes for patients, including those with depression. The purpose of this article is to describe the design and clinical implementation of a depression registry as part of a collaborative care for depression intervention at 2 large academic outpatient internal medicine practices. The primary objective of the registry was to identify and track patients with depression and monitor antidepressant therapy. Secondary objectives of the registry were to assist in addressing pay-for-performance and value-based reimbursement metrics for depression screening and remission. The registry design and variables for inclusion in the registry were defined with input from clinicians, institutional leadership, and data analysts. For implementation, specific clinical workflows were established and responsible team roles were designated.
Keywords: registry, registry implementation, collaborative care model, depression
Patients with depression often have poor quality of life, high medical costs,1 poor health outcomes,2 and high mortality rates, especially when they have comorbid medical illness.3,4 Depression also is estimated to cost $83 billion annually in the United States alone.5,6 Despite the known burden of depression, it remains widely undertreated and access to specialty care continues to be limited,7,8 with 43% to 60% of depression managed in primary care.9 Systematic, population-level interventions based on the Chronic Care Model2 have been developed to improve care of chronic illnesses in general, and depression specifically, in primary care. In the Chronic Care Model, clinic staff and interdisciplinary clinicians work together, each with a defined clinic workflow, to provide consistent, reliable, and high-quality care.6,10–12
The best-studied collaborative care model, Collaborative Care for Depression (CCD),11 is based on the Chronic Care Model. In the CCD model, a care manager works closely with a mental health specialist and primary care providers (PCPs) to manage a population of patients with depression.6,13 The care manager systematically tracks patients’ depression symptoms and utilizes treatment protocols to treat patients based on their symptoms. Such CCD interventions have demonstrated improved remission rates and are now considered the standard of care.10,11,14,15 As a result, the Centers for Medicare & Medicaid Services (CMS) has incentivized the use of collaborative care models with value-based reimbursement metrics for depression remission.
Registries are supportive information systems critical to organizing patient data, systematizing care delivery, and tracking patient health outcomes.16,17 They are fundamental to the success of CCD interventions and other population health initiatives. Registries aggregate sets of digitized patient data and trend patient characteristics over time to allow for identification of patients with a particular indication, such as uncontrolled depression.18 Ideally, a registry is integrated into an electronic health record (EHR) in order to automate the sorting and identification of patient subgroups.19 EHR-based registries can reduce the workload on providers, who are often overburdened and underresourced.6 However, there is limited literature describing the design, implementation, or use of a registry for depression management. Faced with a growing population of patients, there is a critical need to disseminate information about the design and implementation of registries for patients with depression.
This article discusses the design and clinical implementation of a depression registry as part of a CCD intervention at 2 large academic outpatient internal medicine practices.
Methods
The study team designed and implemented an automated electronic registry integrated with an EHR to identify and manage patients with depression in the context of a CCD intervention at 2 large academic internal medicine clinics. The goal of the registry was to identify and track patients with depression to improve depression symptom severity and outcomes, including remission and medication safety During the registry design process, the team iteratively applied lessons learned from the design and implementation of other registries including secured leadership, financial and resource support, registry validation and testing for usability, and designated individuals to drive the project.20
Part I: Registry Design and Validation
First, the study team defined key inclusion and exclusion criteria for the registry and characteristics of patients and their care that would assist in identifying, prioritizing, and tracking the population and outcomes. A series of chart reviews were conducted for patients with depression to ensure the registry variables were comprehensive and representative of the intended population. Table 1 describes the inclusion criteria and the variables included in the registry. The Patient Health Questionnaire (PHQ-9), a validated instrument to diagnose and quantify the severity of depression,21 was used to track depression symptoms in the registry. The PHQ-9 and the abbreviated PHQ-2 are used in standard clinical practice and by CMS and value-based reimbursement metrics to measure depression severity and remission.22,23 To facilitate identification, prioritization, and tracking of patients, the registry was designed to be sortable and downloadable in an Excel format from the EHR. Because the registry was designed to be both automated and classifiable, minimal exclusion criteria were applied to maintain its adaptability to measure other depression screening and management practices.
Table 1.
Key Registry Variables Used to Include, Exclude, and Sort Patientsa.
| Inclusion Criteria | Variables Included |
|---|---|
|
|
Abbreviations: CCD, collaborative care for depression; PCP, primary care provider; PHQ, Patient Health Questionnaire.
If a variable was not applicable for a given patient, that item would be blank.
The critical need for a detailed data dictionary—a list of defined sorting terms, including the origins of data elements and their intended clinical applicability—was identified early in the process of designing the registry and working with the data analyst. The data dictionary facilitated transparency and communication between the clinicians and data analyst and served as an ongoing resource when questions arose about the data source.12 It also bridged the disparate knowledge of the data analyst and clinicians, facilitating collection of the correct data elements to address clinical needs. Using the data dictionary to understand the nuances and origins of specific data elements collected proved critical to the meaningful design of the registry.
Multiple Plan-Do-Study-Act (PDSA) validation cycles were performed to ensure that the registry was complete and accurate. Each cycle consisted of a series of chart reviews to verify the fidelity of data pulled into the registry from the EHR, including PHQ-9 scores and dates, antidepressant medication regimens, diagnoses, and mental health appointments. PDSA cycles were completed until no further concerns or inconsistencies were identified. The completeness of the registry also was assessed by soliciting from physician leadership the identity of patients with depression and confirming their presence in the registry when appropriate.
The university’s multispecialty group practice provided operational and administrative support to build the registry within the health system’s EHR (EPIC; Epic Systems Corporation, Verona, Wisconsin). Although implementation of the registry was planned specifically for 2 academic internal medicine clinics with the CCD intervention, the registry was designed to serve primary care clinics across the health system and to be readily accessible to a broad range of clinicians and appropriate staff members. As such, the registry generated a weekly report specific to each primary care practice across the health system, accessible to download directly from the EHR by the CCD intervention team, primary care practice leadership, clinicians, and designated staff members.
Although the priority of the registry was to improve the quality of care and outcomes for patients with depression, value-based reimbursement metrics related to depression screening and management also were considered. Despite financial incentives to perform well on these metrics and penalties for poor performance, the study team prioritized quality of care when designing and implementing the registry, realizing the need to ensure the registry was adaptable to evolving business needs and changes in evidence-based practices.
Part II: Clinical Implementation Plan
The registry facilitated identification and tracking of 2 cohorts of patients for the CCD intervention: patients with uncontrolled depression and patients with depression who were prescribed a new or increased dose of an antidepressant.
Patients With Uncontrolled Depression.
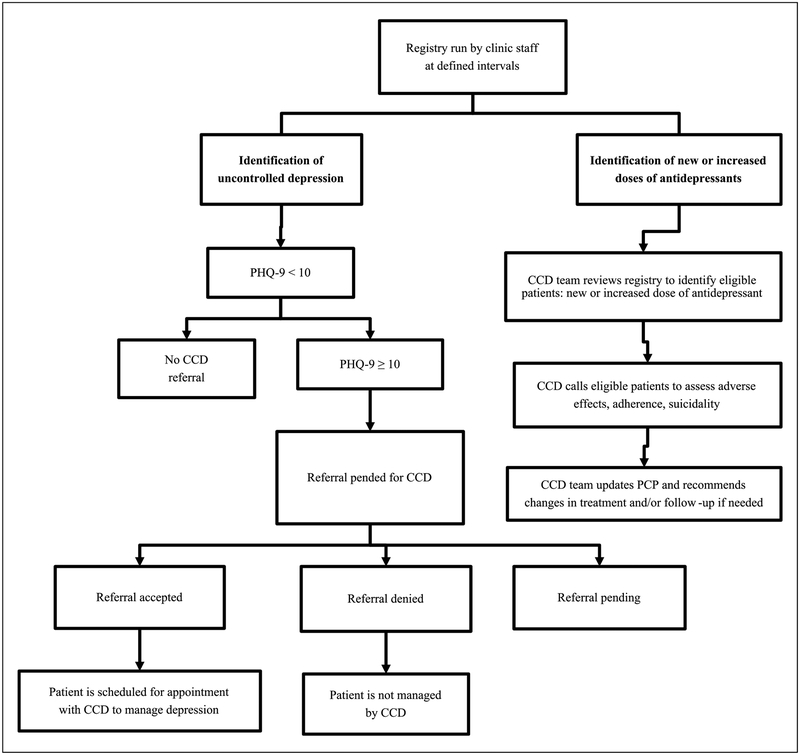
The registry was core to a systematic process of identifying patients with uncontrolled depression and served to track patient progress and monitor outcomes of depression severity and remission. Patients with uncontrolled depression were identified from the registry to facilitate focused and proactive outreach to optimize management. The registry was screened for patients every 2 weeks by designated clinic staff. Uncontrolled depression was defined as a PHQ-9 score ≥10. Patients with a diagnosis of bipolar or personality disorder were excluded from this outreach, given management of depressive symptoms is different and ideally managed by specialty care. For eligible patients, clinic staff pended an electronic referral order within the EHR asking the PCP to refer the patient to the CCD intervention. If the pended referral was accepted by the PCP, patients with uncontrolled depression were managed by the CCD intervention team. PCPs were still able to adjust antidepressants as usual for patients referred to the CCD. This workflow is illustrated in Figure 1. Of note, PCPs also could bypass the pended referral process and proactively refer patients deemed fit for the CCD.
Figure 1.
Abbreviated flow diagram of the registry implementation process. CCD, collaborative care for depression; PHQ, Patient Health Questionnaire.
Patients With Depression Who Were Prescribed a New or Increased Dose of an Antidepressant.
Patients with depression who were prescribed a new or increased dose of an antidepressant were identified from the registry to facilitate monitoring via telephone from the CCD team within 1 to 2 weeks after the change, regardless of referral. The registry was screened for patients every week by designated clinic staff to identify patients needing a call. Patients needing a call had (1) a diagnosis of depression or PHQ-9 score >9, (2) a new antidepressant initiated or an increased dose of an antidepressant, and (3) the antidepressant was prescribed by a PCP from one of the 2 clinics or by the CCD team. Antidepressants prescribed by an outside provider were deemed to be managed outside of the clinic. Calls assessed and mitigated medication adherence and evaluated for possible adverse effects, including suicidality.
Outcomes collected included reach, defined as the number of referrals and patient calls; referrals, defined as the number of referrals pended and whether they were accepted, rejected, or remained pending; and antidepressant follow-up calls, defined as the number of patients meeting criteria for a call and successful call attempts.
Results
The design, validation, and technical build of the registry occurred over the period of 1 year. The registry was validated by comparing the data within the registry with medical records from ~75 patients over 11 iterations.
Parallel to the design and validation of the registry, clinical workflows for the registry implementation were defined. The registry was successfully built within the EHR to meet the predefined specifications (variables and functionalities) and implemented as planned into clinical workflows.
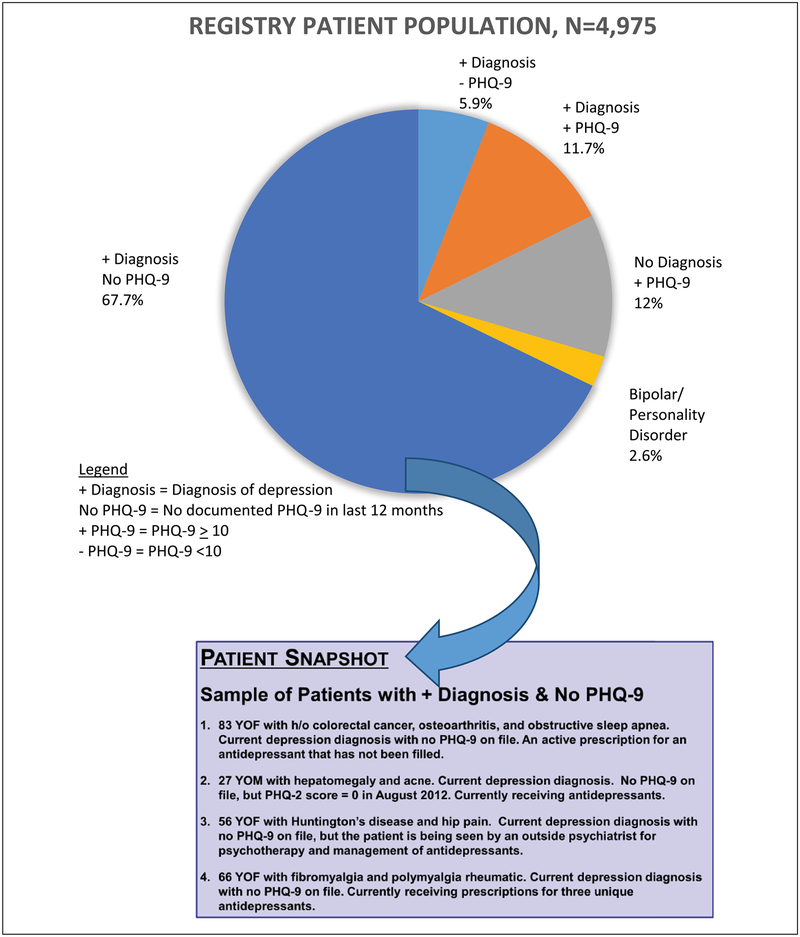
The registry identified 4975 patients with a diagnosis of depression or a positive PHQ-9 suggestive of a diagnosis of depression. Of these patients, 582 had a PHQ-9 ≥10, and thus were eligible to have a referral pended for the CCD intervention. Furthermore, 3368 patients (67.7%) with depression did not have a documented PHQ-9 completed in the past 12 months. Figure 2 displays the types of patients identified by the registry and anecdotal descriptions of patients with a diagnosis of depression who did not have a PHQ-9 in the last 12 months.
Figure 2.
Registry patient population and description of patients without recent PHQ-9. PHQ, Patient Health Questionnaire.
During the first 15 months of registry implementation, 146 patients with uncontrolled depression were identified from the registry and had referrals pended. Of these patients, 58% (84 of 146) of patient referrals to the CCD intervention were approved by PCPs; 40% of the referrals were left pending.
During the same 15 months, there were 750 instances of patients with depression who were prescribed a new or increased dose of an antidepressant, about which the CCD team attempted to call. After a maximum of 2 phone call attempts, 62% of patients were successfully contacted by the CCD team.
Discussion
A depression registry was designed and implemented into the clinical workflows of 2 internal medicine clinics with a CCD intervention to improve depression remission and outcomes. The registry was foundational for the CCD to identify and track patients with depression and monitor antidepressant therapy The registry also was designed to assist in addressing CMS and other value-based reimbursement metrics for depression screening and remission. Although the registry was developed for specific collaborative care for depression interventions, many other interventions in primary care are dependent on registries. The study depression registry design and implementation process can be used by others who seek to implement a registry to support collaborative care for depression interventions in primary care. Identification of clear objectives for the registry and defining specific clinical workflows for its use with designated and responsible team roles were key to the registry’s successful implementation. Furthermore, the combined effort, support and input from PCPs, leadership, and data analysts were critical to the success of the registry.
Because of the registry, the study team was able to implement proactive interventions to optimize care for patients with depression and identify care gaps in the current process. Identification of patients who had an antidepressant initiated or intensified facilitated follow-up telephone calls to monitor safety and efficacy As previously published, 40% of these phone calls resulted in interventions to optimize efficacy or safety, including suicidal ideation, nonadherence, and adverse effects24 Although CCD referral and management of patients with uncontrolled depression is still ongoing, many patients have been proactively outreached as a result of the registry. Although some CCD referrals are left pending, this does not reflect quality of PCP care provided, but rather could simply reflect PCPs’ desire to manage their patients or desire to consider the referral at a later time. Left pending means care continued as usual with no change and PCPs would continue to manage depression per usual care in this clinic. Patients with pending orders had no change in their care; however, per PCP stakeholders’ request, PCPs retained the ability to opt patients in to the CCD at a later time. With any new clinical service, change management principles must be followed to ensure success of the change, including stakeholder buy-in. In this instance, PCP stakeholders expressed the need to have a voice and the decision of whether or not to opt in.
Finally, as a result of the registry, a large portion of patients were identified who had diagnoses of depression but who had not had a documented PHQ-9 in the past 12 months, which points to a gap in care or a faulty process. As a result, this has led to quality improvement efforts to understand why patients with depression do not have PHQ-9 scores documented at least annually. These quality improvement efforts are hoped to lead to corrective action and evaluation of the impact via the registry.
Lessons Learned
Many lessons have been learned throughout this process that can be applied to future registry design and implementation efforts. Although the value-based reimbursement metrics are a step forward in holding providers accountable for providing evidence-based and quality care for patients with depression, there are limitations in the clinical applicability of the current set of metrics, which likely will be refined and change over time. For example, the CMS depression remission metric requires that a patient’s follow-up PHQ-9 must be administered within 11 to 13 months after the initially elevated PHQ-9. This depression remission metric lacks clinical practicality, given fulfilling the metric would not necessarily influence follow-up treatment or screening (eg, a patient was diagnostically in remission at month 10 after the initial PHQ-9). Nonetheless, the registry was designed to allow monitoring of progress with the current set of value-based reimbursement metrics, while prioritizing evidence-based metrics for depression management and anticipating changes in evidence-based and value-based reimbursement metrics over time. Adaptability of the registry to support ever-changing evidence-based management practices and value-based reimbursement metrics for depression challenged the study team to think more broadly about what variables should be included in the registry design.
A high-priority next step to improve the registry is to define clear workflows and designate responsible staff to track patients once they are enrolled in the CCD. A systematic process of screening and outreach to patients with depression who are lost to follow-up (eg, missed visits) would advance the ability to improve clinical outcomes for patients with depression and potentially reveal further areas for quality improvement.
Limitations of the Registry
As with any automated registry, the study registry is dependent on clinicians to document clinical care within the EHR accurately, consistently, and completely. The information contained in the registry is subject to human error of inaccuracies and omission of documentation. Furthermore, other institutions may not be able to implement the registry into clinical workflows in the same way as was done in this study if they do not have a systematic process of screening and monitoring using validated tools, such as the PHQ-9, captured as discrete variables in the EHR. In the present instance, the study team relied on PHQ-9 scores to determine if a patient had uncontrolled depression, which was only possible because of past initiatives to standardize PHQ-9 use and documentation as a discrete variable within the EHR. However, for institutions without a systematic depression screening and monitoring process, the registry could be used to identify this gap in care and monitor progress toward accomplishing this process change.
Conclusion
A registry was designed and implemented to identify patients in primary care who need monitoring or intensification of depression therapy and follow-up of antidepressant medication changes. The designation of key team roles, the creation of a meaningful data dictionary, and the definition of clinically applicable objectives and workflows were central to the success of the registry and its implementation.
Acknowledgments
The support of the Leadership | Education | Advocacy | Development | Scholarship (LEADS) Track at the University of Colorado School of Medicine.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was supported by the University of Colorado Medicine (CU Medicine).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. 2015;76:155–162. [DOI] [PubMed] [Google Scholar]
- 2.Egede LE, Nietert PJ, Zheng D. Depression and all-cause and coronary heart disease mortality among adults with and without diabetes. Diabetes Care. 2005;28:1339–1345. [DOI] [PubMed] [Google Scholar]
- 3.Hamer M, Batty GD, Stamatakis E, Kivimaki M. The combined influence of hypertension and common mental disorder on all-cause and cardiovascular disease mortality. J Hypertens. 2010;28:2401–2406. [DOI] [PubMed] [Google Scholar]
- 4.Katon W, Fan MY, Unutzer J, Taylor J, Pincus H, Schoenbaum M. Depression and diabetes: a potentially lethal combination. J Gen Intern Med. 2008;23:1571–1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donohue J, Pincus HA. Reducing the societal burden of depression: a review of economic costs, quality of care and effects of treatment. Pharmacoeconomics. 2007;25(1): 7–24. [DOI] [PubMed] [Google Scholar]
- 6.Margolis KL, Solberg LI, Asche SE, Whitebird RR. Use of practice system tools by medical groups for depression. Am J Manag Care. 2007;13:305–311. [PubMed] [Google Scholar]
- 7.Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:603–613. [DOI] [PubMed] [Google Scholar]
- 8.Hirschfeld RM, Keller MB, Panico S, et al. The National Depressive and Manic-Depressive Association consensus statement on the undertreatment of depression. JAMA. 1997;277:333–340. [PubMed] [Google Scholar]
- 9.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62: 629–640. [DOI] [PubMed] [Google Scholar]
- 10.Zimmermann T, Puschmann E, van den Bussche H, et al. Collaborative nurse-led self-management support for primary care patients with anxiety, depressive or somatic symptoms: cluster-randomised controlled trial (findings of the SMADS study). Int J Nurs Stud. 2016;63: 101–111. [DOI] [PubMed] [Google Scholar]
- 11.Gunn J, Diggens J, Hegarty K, Blashki G. A systematic review of complex system interventions designed to increase recovery from depression in primary care. BMC Health Serv Res. 2006;6:88–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ouwens M, Wollersheim H, Hermens R, Hulscher M, Grol R. Integrated care programmes for chronically ill patients: a review of systematic reviews. Int J Qual Health Care. 2005;17:141–146. [DOI] [PubMed] [Google Scholar]
- 13.Pietruszewski PB, Mundt MP, Hadzic S, Brown RL. Effects of staffing choices on collaborative care for depression at primary care clinics in Minnesota. Psychiatr Serv. 2015;66:101–103. [DOI] [PubMed] [Google Scholar]
- 14.Eghaneyan BH, Sanchez K, Mitschke DB. Implementation of a collaborative care model for the treatment of depression and anxiety in a community health center: results from a qualitative case study. J Multidiscip Healthc. 2014;7:503–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Richards DA, Hill JJ, Gask L, et al. Clinical effectiveness of collaborative care for depression in UK primary care (CADET): cluster randomised controlled trial. BMJ. 2013;347:f4913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wagner E, Austin B, VonKorff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74: 511–544. [PubMed] [Google Scholar]
- 17.Coventry PA, Hudson JL, Kontopantelis E, et al. Characteristics of effective collaborative care for treatment of depression: a systematic review and metaregression of 74 randomised controlled trials. PLoS One. 2014;9(9):e108114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Committee for Quality Assurance. Patient-centered medical home (PCMH) recognition. http://www.ncqa.org/programs/recognition/practices/patient-centered-medical-home-pcmh. Accessed May 1, 2017.
- 19.Baus A, Wood G, Pollard C, Summerfield B, White E. Registry-based diabetes risk detection schema for the systematic identification of patients at risk for diabetes in West Virginia primary care centers. Perspect Health Inf Manag. 2013; 10(Fall): 1f. [PMC free article] [PubMed] [Google Scholar]
- 20.Holtrop JS, Hall TL, Rubinson C, Dickinson LM, Glasgow RE. What makes for successful registry implementation: a qualitative comparative analysis. J Am Board Fam Med. 2017;30:657–665. [DOI] [PubMed] [Google Scholar]
- 21.Chang TE, Jing Y, Yeung AS, et al. Depression monitoring and patient behavior in the Clinical Outcomes in MEasurement-Based Treatment (COMET) Trial. Psychiatr Serv. 2014;65:1058–1061. [DOI] [PubMed] [Google Scholar]
- 22.Löwe B, Kroenke K, Herzog W, Gräfe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord. 2004;81:61–66. [DOI] [PubMed] [Google Scholar]
- 23.McMillan D, Gillbody S, Richards D. Defining successful treatment outcome in depression using the PHQ-9: a comparison of methods. J Affect Disord. 2010;127: 122–129. [DOI] [PubMed] [Google Scholar]
- 24.Bhat S, Kroehl M, Trinkley KE, et al. Evaluation of a clinical pharmacist-led multidisciplinary antidepressant telemonitoring service in the primary care setting [published online December 6, 2017]. Popul Health Manag. doi: 10.1089/pop.2017.0144. [DOI] [PMC free article] [PubMed] [Google Scholar]