Abstract
Trifluridine/tipiracil (Lonsurf®) is a fixed-dose combination tablet comprising trifluridine, an antineoplastic nucleoside analogue, and tipiracil, a thymidine phosphorylase inhibitor. Trifluridine/tipiracil has recently been granted an additional indication in the USA for the treatment of metastatic gastric cancer, including gastroesophageal junction adenocarcinoma, in patients who have been previously treated with at least two systemic treatment regimens, and has received a positive opinion for this indication in the EU. In the large pivotal phase III TAGS trial, trifluridine/tipiracil plus best supportive care (BSC) significantly prolonged overall survival (OS; primary endpoint) compared with placebo plus BSC in this patient group. Progression-free survival (PFS) and the disease control rate were also improved with trifluridine/tipiracil relative to placebo. Health-related quality of life was not adversely affected by the addition of trifluridine/tipiracil to BSC and time to deterioration of Eastern Cooperative Oncology Group (ECOG) performance status was significantly delayed. The most common adverse events were mainly haematological (neutropenia, leucopenia and anaemia) and gastrointestinal (nausea, vomiting and diarrhoea), and were generally manageable with dosage modifications and/or supportive care. Adverse events ≥ Grade 3 were most frequently haematological in nature. Thus, trifluridine/tipiracil provides a valuable and much needed treatment option for patients with metastatic gastric or gastroesophageal junction adenocarcinoma that has progressed on at least two prior therapies.
Trifluridine/Tipiracil: clinical considerations in metastatic gastric cancer
| Combines trifluridine (which inhibits cell proliferation by interfering with DNA synthesis) with tipiracil (which increases systemic exposure to trifluridine) |
| Prolongs OS, PFS and time to deterioration of ECOG performance status in comparison to placebo |
| Does not adversely affect health-related quality of life |
| Manageable safety and tolerability profile |
Introduction
Gastric cancer is the fifth most frequently diagnosed cancer worldwide, and the third leading cause of cancer-related mortality, resulting in 783,000 deaths globally during 2018 [1]. The aim of treating metastatic gastric cancer is to prolong survival and maximize health-related quality of life (HR-QOL). Unresectable metastatic gastric cancer has traditionally been treated with palliative therapies in combination with best supportive care (BSC) [2, 3]. These regimens can include fluoropyrimidine- [e.g. 5-fluorouracil (5-FU)] and platinum-based regimens (e.g. cisplatin or oxaliplatin), and, at later lines, anti-vascular endothelial growth factor monoclonal antibody- (e.g. ramucirumab), irinotecan- and taxane-based (e.g. paclitaxel) therapies [2]. Patients with human epidermal growth factor receptor 2 (HER2)-positive tumours can also benefit from targeted therapy such as trastuzumab [2]. However, treatment options can become limited once resistance develops, and until recently, the only choices available after second-line treatment failure were to trial another second-line treatment option and/or continue BSC [4]. Additional treatment options for patients who have progressed on multiple therapies therefore represent a significant unmet need.
A fixed-dose combination tablet comprising trifluridine and tipiracil (hereafter referred to as trifluridine/tipiracil) [Lonsurf®] is approved worldwide for use in metastatic colorectal cancer, including in the USA [5], the EU [6] and Japan [7], data for which have been reviewed previously [8] and are beyond the scope of this review. It has also recently been approved in the USA [5], and received a positive opinion in the EU [9], for the treatment of patients with metastatic gastric cancer who have been treated with ≥ 2 prior treatment regimens. Trifluridine/tipiracil is also under review for this indication in Japan [10]. This article reviews pharmacological and clinical data relevant to the use of trifluridine/tipiracil in patients with metastatic gastric cancer. Discussion focuses on the recommended dosage of trifluridine/tipiracil (i.e. 35 mg/m2, based on the trifluridine component and calculated based on body surface area) wherever possible.
Pharmacological Properties
The pharmacological properties of trifluridine/tipiracil have been reviewed in detail previously [8, 11]. This section summarizes the key properties of these agents, focusing on data relevant to metastatic gastric cancer where possible. Data discussed are for the approved dosage of 35 mg/m2 twice daily unless specified otherwise.
Trifluridine/tipiracil comprises trifluridine and tipiracil in a 1:0.5 molar and 1:0.471 weight ratio [5, 6]. The active component is trifluridine, an antineoplastic thymidine-based nucleoside analogue; as trifluridine is readily degraded by thymidine phosphorylase after oral administration, tipiracil (a thymidine phosphorylase inhibitor) is included to increase trifluridine bioavailability [5, 6, 11]. Tipiracil potentiates the antitumour efficacy of trifluridine and enables oral administration in the clinical setting; it is also anti-angiogenic, but the clinical significance of this effect has yet to be determined [12, 13].
Pharmacodynamic Properties
Trifluridine acts predominantly through its incorporation into DNA [5, 11]; it can also inhibit thymidylate synthase (a key enzyme in DNA synthesis), although this does not seem to be a key cytotoxic mechanism for the drug when dosed orally [14]. Once the drug enters the cancer cells (via nucleoside transporters), trifluridine is rapidly phosphorylated by thymidine kinase to trifluridine triphosphate, which is misincorporated into DNA preferentially over thymidine bases [11, 12, 14]. This interrupts DNA function, and tumour growth is inhibited by the subsequent reduction in cell proliferation [12, 15]. Trifluridine/tipiracil incorporates extensively into tumour cell DNA and to a lesser extent into white blood cell DNA [15]. Myelosuppressive toxicities are associated with trifluridine/tipiracil treatment (Sect. 4) [16], and may result from significant uptake of trifluridine into white blood cell DNA [15].
Although classified as a fluoropyrimidine, trifluridine’s predominant mechanism of action differs from that of traditional fluoropyrimidines such as 5-FU [12, 17, 18]. For instance, when gastric cell lines resistant to 5-FU due to overexpression of thymidylate synthase (a major mode of resistance to 5-FU therapy) were compared with their parental cell lines, they were found to incorporate trifluridine into DNA to a similar extent and two of the three cell lines evaluated were also as sensitive to the drug [18]. The 5-FU resistant cell line that displayed cross-resistance to trifluridine had the highest thymidylate synthase levels, which possibly were not fully inhibited by trifluridine and may therefore have reduced sensitivity to the drug. However, this cross-resistance was overcome when trifluridine/tipiracil was administered orally twice daily in corresponding xenograft models [18], consistent with DNA incorporation being the main mechanism of action of trifluridine/tipiracil when used as recommended in the clinic.
At the recommended dosage, trifluridine/tipiracil had no clinically relevant effect on the corrected QT interval [5, 19] or cardiac repolarization [19] in patients with advanced solid tumours. Based on animal studies, trifluridine/tipiracil can cause embryo-foetal harm if administered during pregnancy and may be present in breast milk [5]. Females of reproductive age and their male partners should use effective contraception during treatment and for ≥ 6 months (females) or 3 months (males), after treatment has been completed; pregnant women should be advised of the potential foetal risk and nursing mothers advised to avoid breastfeeding during, and for 1 day after the last dose of therapy [5].
Pharmacokinetic Properties
The administration of trifluridine/tipiracil improved the peak plasma concentration (Cmax) and area under the curve (AUC) of trifluridine by ≈ 22- and 37-fold, respectively, compared with the administration of trifluridine alone in patients with advanced solid tumours [5, 20]. Accumulation of trifluridine was seen after multiple doses of trifluridine/tipiracil in the first treatment cycle (twofold for Cmax at steady state and threefold increase for AUC from time 0 to 12 h), with no further accumulation in subsequent cycles; no accumulation was seen for tipiracil [5, 20]. The mean time to Cmax for trifluridine was 2 h and for tipiracil was 3 h after multiple doses of trifluridine/tipiracil in patients with advanced solid tumours [6]. Following single-dose administration of trifluridine/tipiracil after a standardised high-fat, high calorie meal, the Cmax of trifluridine and tipiracil and the AUC of tipiracil decreased by ≈ 40% relative to administration in a fasting state [5, 21]. Trifluridine/tipiracil should be taken with food [5].
In vitro, trifluridine is highly (≥ 96%) bound to human plasma proteins (largely to human serum albumin), regardless of drug concentration or the presence of tipiracil [5]. The plasma protein binding of tipiracil is < 8% [5]. In patients with advanced solid tumours receiving a single dose of trifluridine/tipiracil, the apparent volume of distribution was 21 L for trifluridine and 333 L for tipiracil [6].
Trifluridine is extensively metabolized via thymidine phosphorylase to its major inactive metabolite, 5-trifluoromethyluracil, and trifluridine glucuronides, which are excreted in the urine [6, 12]. In patients with advanced solid tumours receiving a single oral dose of trifluridine/tipiracil 60 mg containing [14C]-trifluridine, approximately half (55%) of the radiolabelled trifluridine component was recovered as 5-trifluoromethyluracil and trifluridine glucuronide isomers in the urine within 24 h, with < 3% recovered in faeces and expired air [5, 22]. In contrast, after a single oral dose of trifluridine/tipiracil 60 mg containing [14C]-tipiracil, the radiolabelled tipiracil component was recovered as unchanged parent drug (major component) and 6-hydroxymethyluracil (major metabolite) in faeces (50%) and in urine (27%) [5, 22]. Trifluridine and tipiracil are not metabolized by cytochrome P450 (CYP) enzymes [5].
Following multiple doses of trifluridine/tipiracil, the mean elimination half-life was 2.1 h for trifluridine and 2.4 h for tipiracil (at steady state) [5]. Following single-dose administration of trifluridine/tipiracil, oral clearance was 10.5 L/h for trifluridine and 109 L/h for tipiracil [6].
Special Populations and Drug Interactions
In a population pharmacokinetic analysis, age, sex and race (white or Asian) did not affect the pharmacokinetics of trifluridine/tipiracil to a clinically relevant extent [5]. Exposure to the components of trifluridine/tipiracil is not impacted to any clinically relevant extent by mild or moderate renal impairment [creatinine clearance (CRCL) 30–89 mL/min] or mild or moderate hepatic impairment; trifluridine/tipiracil has not been studied in patients with severe renal impairment (CRCL < 30 mL/min), end-stage renal disease or severe hepatic impairment. No dosage adjustments are required for mild or moderate renal impairment or mild hepatic impairment; however, trifluridine/tipiracil is not recommended in patients with hepatic impairment that is moderate (as grade 3–4 increases in bilirubin levels have occurred with trifluridine/tipiracil in this population) or severe [5].
In in vitro studies, trifluridine, tipiracil and the metabolite 5-trifluoromethyluracil were not inhibitors of any of the CYP isoforms evaluated (CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1 and CYP3A4/5) and were not inducers of CYP1A2, CYP2B6 or CYP3A4/5 [6]. Therefore, trifluridine and tipiracil are not expected to have significant CYP-mediated medication interactions. Trifluridine and tipiracil are not in vitro substrates (or inhibitors) of human uptake and efflux transporters, with the exception of MATE1 and OCT2 which are inhibited by tipiracil, although only at concentrations much higher than its steady-state Cmax in humans after administration of the approved dosage. Trifluridine/tipiracil is therefore unlikely to cause MATE1 or OCT2 interactions when used at the recommended dosage, although tipiracil transport via these proteins may be impacted by drugs that are MATE1 or OCT2 inhibitors. Trifluridine is also a substrate of several nucleoside transporters (CNT1, ENT1 and ENT2). Concomitant use of trifluridine/tipiracil with other human thymidine kinase substrates (e.g. antiviral products) may result in competition between trifluridine and the co-administered drug for activation via thymidine kinases [6].
Therapeutic Efficacy of Trifluridine/Tipiracil
This section focuses on the clinical efficacy of oral trifluridine/tipiracil 35 mg/m2 twice daily on days 1–5 and 8–12 of each 28-day cycle in patients with metastatic gastric cancer who had previously been treated with ≥ 2 chemotherapy regimens for advanced disease, as evaluated in the randomized, double-blind, placebo-controlled, global, pivotal, phase III TAGS trial (n = 507) [16].
TAGS enrolled adult patients aged ≥ 18 years (or ≥ 20 years in Japan) with histologically confirmed, non-resectable, metastatic gastric or gastroesophageal junction adenocarcinoma, as defined by the American Joint Committee on Cancer staging classification (7th edition) [16]. Eligible patients must have previously received at least two lines of chemotherapy, which included a fluoropyrimidine, a platinum agent, either irinotecan or a taxane or both, and HER2/neu-targeted therapy if appropriate [5, 16]. Patients were required to have an Eastern Cooperative Oncology Group (ECOG) performance status of 0–1 and either radiological disease progression ≤ 3 months after their last dose of previous therapy or intolerance of their last therapy. Patients with recurrent disease could participate provided they had previously received ≥ 2 lines of chemotherapy [16]. Adjuvant chemotherapy could be considered as a prior regimen for advanced disease in certain patients with disease recurrence during or ≤ 6 months after completion of the adjuvant chemotherapy [5].
Patients from 17 countries were enrolled and randomized (2:1) to trifluridine/tipiracil plus BSC or placebo plus BSC. Patients were stratified by geographical region (Japan vs rest of the world), ECOG performance status (0 vs 1) and previous ramucirumab treatment (yes vs no) [16]. Baseline demographic and disease characteristics were generally similar between the two patient groups. Most patients (80%) were from Europe, with the rest being from Japan (14%) or the USA (5%). The median age of patients was 63 years, with the majority being white (70%) and male (73%) [5]. The primary site of malignancy was gastric in the majority (71%) of patients in both treatment arms [16].
At baseline, about one third of patients in each treatment group had previously received ramucirumab (34% of trifluridine/tipiracil recipients vs 32% of placebo recipients) and approximately one half (54% vs 58%) had previously received irinotecan; almost all patients had previously received a platinum agent, fluoropyrimidine or taxane (91–100%) [16]. Around one quarter of patients in each group (23% of trifluridine/tipiracil recipients vs 27% of placebo recipients) had received ≥ 4 previous chemotherapy regimens and over half (54% vs 58%) had ≥ 3 metastatic sites. A baseline ECOG performance status of 1 was reported in 64% and 60% of patients in the trifluridine/tipiracil and placebo groups, respectively, while 44% in both groups had previously undergone a gastrectomy. A proportion of patients were HER2-positive in each group (20% and 16%); almost all of these patients had received anti-HER2 therapy prior to the study (18% and 14% of the total patients in each group) [16].
Patients in the TAGS study received oral trifluridine/tipiracil or placebo, along with BSC, until disease progression or unacceptable toxicity [5, 16]. The median treatment duration in the respective treatment groups was 6.7 and 5.7 weeks [16]. The primary endpoint was overall survival (OS), defined as the time from randomization to death in the intent-to-treat population [16].
In patients with heavily pretreated metastatic gastric cancer receiving BSC, median OS was significantly longer with trifluridine/tipiracil relative to placebo [by > 50%; HR of 0.69 (median 5.7 vs 3.6 months), p < 0.0006], corresponding to a 31% reduction in the risk of death (Table 1) [16]. At a median follow-up of 10.7 months, 28% of patients in the trifluridine/tipiracil group were still alive compared with 18% in the placebo group [16].
Table 1.
Efficacy of oral trifluridine/tipiracil vs placebo in the phase III TAGS trial in patients with metastatic gastric cancer who had previously completed at least two chemotherapy regimens [16]
| Treatmenta (no. of ITT pts) | Median OSb | Median PFS | ORR | Disease controlc | Median time to deteriorationd | |||
|---|---|---|---|---|---|---|---|---|
| Months | HR (95% CI) | Months | HR (95% CI) | % of pts | % of pts | Months | HR (95% CI) | |
| FTD/TPI (337) | 5.7 | 0.69* (0.56–0.85) | 2.0 | 0.57** (0.47–0.70) | 4 | 44** | 4.3 | 0.69* (0.56–0.85) |
| Placebo (170) | 3.6 | 1.8 | 2 | 14 | 2.3 | |||
BSC best supportive care, CI confidence interval, ECOG Eastern Cooperative Oncology Group, FTD/TPI trifluridine/tipiracil, HR hazard ratio vs placebo, ITT intent to treat, ORR objective response rate, OS overall survival, PFS progression-free survival, pts patients
*p < 0.001, **p < 0.0001 vs placebo (two-sided p value)
aPatients received 35 mg/m2 FTD/TPI or placebo orally twice daily on days 1–5 and 8–12 of each 28-day cycle (in addition to BSC)
bPrimary endpoint
cProportion of pts with a complete response, a partial response or stable disease (tumour response was assessable in 290 pts in the FTD/TPI group and 145 pts in the placebo group)
dTime from randomisation to deterioration of ECOG performance status to 2 or greater
Median progression-free survival (PFS) was also longer with trifluridine/tipiracil relative to placebo [HR of 0.57 (median 2.0 vs 1.8 months), p < 0.0001], corresponding to a 43% reduction in the risk of disease progression or death (Table 1) [16]. However, as initial on-tumour assessment was done approximately 8 weeks (1.9 months) after treatment had started, median PFS values were confounded by this delay. At 6 months, PFS events (i.e. no disease progression) were reported in 2.5-fold more patients in the actively treated arm compared with placebo (15% vs 6%). The majority of patients in both groups had disease progression or had died by the data cut-off date (85% vs 92%) [16].
In prespecified subgroup analyses, the treatment benefit effect of trifluridine/tipiracil over placebo on OS and PFS (indicated by a hazard ratio < 1) was generally consistent regardless of baseline patient and disease characteristics, including prior gastrectomy. A prespecified multivariate Cox regression analysis indicated that no baseline patient or disease characteristic was likely to be predictive of OS. Some characteristics (age, ECOG performance status, HER2 status, number of metastatic sites and number of prior chemotherapy regimens) were prognostic of OS improvement, although the benefit of trifluridine/tipiracil over placebo was of a similar magnitude as in the primary analysis after adjusting for these factors [16].
Significantly more patients in the trifluridine/tipiracil group achieved disease control than in the placebo group (44% vs 14%; p < 0.0001), but a statistical difference in objective tumour response was not seen between the two groups (Table 1) [16]. Baseline ECOG performance status (i.e. 0–1) was maintained for a longer duration with trifluridine/tipiracil than with placebo, corresponding to a 34% reduction in risk of deterioration to a higher status (Table 1). The proportion of patients in the respective groups who experienced deterioration events was 78% and 85%. Approximately a quarter of patients in both groups received post-study systemic anti-cancer treatment [16].
HR-QOL was assessed via the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire Version 3.0 (EORTC QLQ-C30) and the EORTC Quality of Life Questionnaire-Stomach (QLQ-STO22) [23]. Clinically relevant changes from baseline (a change of ≥ 10 points on any scale) were not seen in most variables tested in either treatment group; however, the score changes differed to a clinically relevant extent between the treatment groups for some items, including pain relief at cycle 2 (in favour of trifluridine/tipiracil) and role functioning at cycle 3 (in favour of placebo) [23]. This suggests HR-QOL was generally maintained with trifluridine/tipiracil treatment.
Tolerability of Trifluridine/Tipiracil
Trifluridine/tipiracil plus BSC had a manageable tolerability profile in patients with heavily pretreated metastatic gastric cancer in the TAGS trial [16]. The safety and tolerability profile of trifluridine/tipiracil in this indication was consistent with that seen previously in patients with metastatic colorectal cancer (RECOURSE trial) [6], although the difference in incidences of gastrointestinal disorders when compared to placebo were higher in RECOURSE patients than in TAGS patients [24]. AEs were generally managed by dosage modifications and/or supportive care [16, 25].
Treatment-related AEs were more frequent in trifluridine/tipiracil recipients than placebo recipients in TAGS (81% vs 57%) [16]. AEs (of any cause) that were reported most commonly (incidence > 15%) with trifluridine/tipiracil and occurred with an incidence ≥ 5% higher than with placebo included haematological AEs (neutropenia, anaemia, leucopenia and thrombocytopenia), gastrointestinal AEs (nausea, vomiting and diarrhoea) and fatigue (Fig. 1). Grade ≥ 3 treatment-related AEs occurred in 53% of trifluridine/tipiracil recipients and 13% of placebo recipients. Neutropenia, anaemia and leucopenia were the most frequently reported grade ≥ 3 AEs of any cause in the trifluridine/tipiracil group (Fig. 1); the placebo group mostly reported abdominal pain, general deterioration of physical health (7% and 9% of patients in the respective groups) and anaemia (Fig. 1). Supportive treatment for neutropenia was received by 17% of patients in the trifluridine/tipiracil group and 2% in the placebo group. Few trifluridine/tipiracil recipients experienced grade 3–4 febrile neutropenia (1.8%) [16] or grade ≥ 3 cardiac events (1%) [24].
Fig. 1.
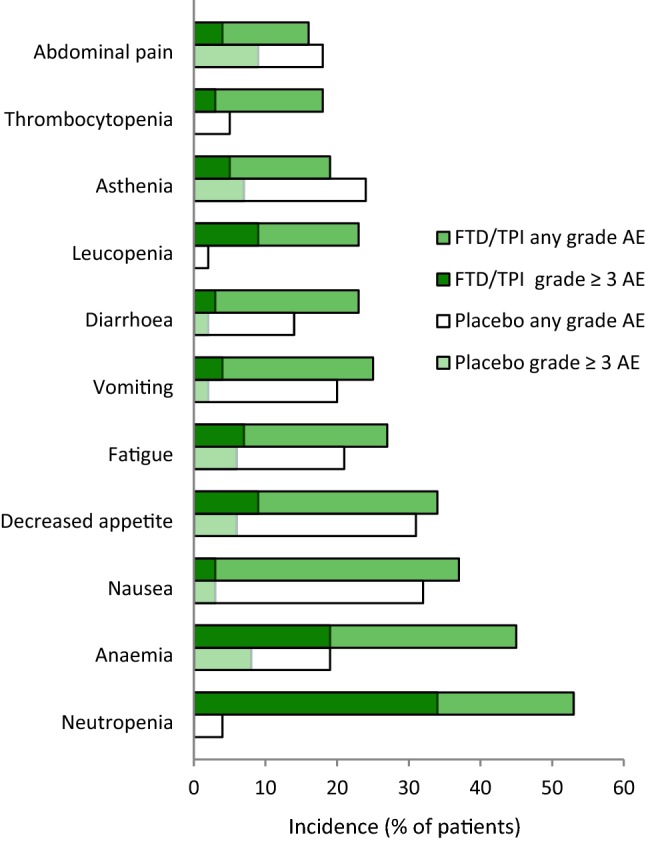
Most common (incidence ≥ 15% in the active treatment group) adverse events of any grade or cause in patients with metastatic gastric cancer who received trifluridine/tipiracil (n = 335) or placebo (n = 168) in the phase III TAGS trial [16]. No grade ≥ 3 thrombocytopenia, leucopenia or neutropenia was reported in the placebo group. AE adverse event, FTD/TPI trifluridine/tipiracil
Serious treatment-related AEs were reported in 12% of trifluridine/tipiracil recipients (most commonly pancytopenia, anaemia and diarrhoea; 2% incidence for each) and 4% of placebo recipients [16]. Death due to a treatment-related AE occurred in one patient in each treatment arm (cardiopulmonary arrest and toxic hepatitis, respectively) [16].
AEs of any grade or cause led to dosage modifications (i.e. dosing delays or dose reductions) in 58% of trifluridine/tipiracil recipients and 22% of placebo recipients, and dose reductions in 11% and 1% of patients. Grade ≥ 3 AEs led to dosage modifications in 44% of patients receiving trifluridine/tipiracil and 17% of patients receiving placebo [16]. All treatment-related AEs leading to treatment discontinuation were grade ≥ 3 AEs (4% of trifluridine/tipiracil recipients vs 1% of placebo recipients); the most commonly reported AEs in the trifluridine/tipiracil group were thrombocytopenia, diarrhoea, nausea, and neutropenic sepsis (each 1% incidence) [16]. Patients aged ≥ 65 years may experience a higher incidence of grade ≥ 3 haematological abnormalities than younger patients, according to a pooled analysis of TAGS and RECOURSE [5].
Dosage and Administration of Trifluridine/Tipiracil
Trifluridine/tipiracil has received a positive opinion in the EU [9], and is approved in the USA [5], for the treatment of adult patients with metastatic gastric cancer, including adenocarcinoma of the gastroesophageal junction, who have been previously treated with ≥ 2 systemic treatment regimens for advanced disease. Prior regimens can include a fluoropyrimidine, a platinum, either a taxane or irinotecan, and if appropriate, HER2/neu-targeted therapy [5]. The recommended dosage of trifluridine/tipiracil is 35 mg/m2 (based on the trifluridine component and calculated based on body surface area) twice daily on days 1–5 and 8–12 of each 28-day treatment cycle. The tablets are to be taken with food and swallowed whole. Doses are to be rounded to the nearest 5 mg, with a maximum daily dose of 80 mg twice daily. A maximum of three 5 mg/m2 dose reductions are allowed if tolerability issues occur; however, treatment must be permanently discontinued in patients who cannot tolerate a minimum dosage of 20 mg/m2 twice daily or experience unacceptable toxicity or disease progression. There is a warning pertaining to severe myelosuppression; complete blood counts should be obtained before each treatment cycle (or more frequently if clinically indicated), and if required, treatment should be withheld and then resumed at the next lower dosage. Trifluridine/tipiracil is not recommended in patients with moderate to severe hepatic impairment (Sect. 2.3) [5].
Local prescribing information should be consulted for detailed information regarding dosing according to body surface area, dosage modifications for adverse events, warnings, precautions, and use in specific populations.
Current Status of Trifluridine/Tipiracil in Metastatic Gastric Cancer
Trifluridine/tipiracil is a fixed-dose oral tablet comprising a fluoropyrimidine (trifluridine) and a thymidine phosphorylase inhibitor (tipiracil), with the latter being vital in maintaining trifluridine at plasma levels sufficient for cytotoxic effect (Sect. 2.2). The predominant mechanism of action of trifluridine differs to that of traditional fluoropyrimidines, enabling trifluridine to overcome 5-FU resistance (Sect. 2). Based on its pharmacokinetic profile, trifluridine/tipiracil is not likely to be affected by many patient characteristics or concomitant medications (Sect. 2.3); this may maximize the pool of patients who may be eligible for treatment.
Recently, trifluridine/tipiracil was approved in the USA, and has received a positive opinion for approval in the EU, for the treatment of metastatic gastric cancer in patients who have previously received ≥ 2 chemotherapy regimens (Sect. 5). This approval was based on data from the pivotal phase III TAGS trial (Sect. 3), which showed that trifluridine/tipiracil significantly prolonged median OS compared with placebo in patients with heavily pretreated metastatic gastric cancer. While the survival time gained (a median 2.1 months) may seem relatively short, prolonging life expectancy by such a degree in palliative patients can be clinically meaningful [26]. PFS, disease control rate, and time to deterioration of ECOG performance status were also improved with trifluridine/tipiracil relative to placebo (Sect. 3). The study population in TAGS was representative of a general population with advanced gastric cancer (with regards to primary site of disease and previous gastrectomy status), further supporting the clinical significance of the treatment benefits seen with trifluridine/tipiracil in this study [16]. Prespecified subgroup analyses did not reveal any meaningful differences in efficacy between subgroups based on demographic and baseline characteristics (including prior gastrectomy and ramucirumab pre-treatment); therefore treatment with trifluridine/tipiracil is expected to be effective regardless of these factors. HR-QOL was generally maintained with trifluridine/tipiracil therapy [16].
The safety and tolerability profile of trifluridine/tipiracil was generally manageable with dosage modifications and (for patients with neutropenia) supportive care. The most common AEs with trifluridine/tipiracil in TAGS were largely haematological and gastrointestinal in nature (Sect. 5), which is typical of the AEs often associated with third-line chemotherapy options used worldwide in advanced gastric cancer (i.e. neutropenia, anaemia, thrombocytopenia, fatigue and anorexia) [3, 27]. Treatment-related grade ≥ 3 AEs were reported in approximately half of the trifluridine/tipiracil recipients and more than four times more frequently than in the placebo group (Sect. 4). Although there were patients in the trifluridine/tipiracil group who required dosage modification because of these AEs, this did not markedly impact the ability of patients to receive therapy, as indicated by the low incidence of treatment discontinuation (Sect. 4). In a cohort study of trifluridine/tipiracil in patients with metastatic colorectal cancer, chemotherapy-induced neutropenia after 1 month of treatment was associated with significantly longer OS and PFS [28]. However, predictive and/or prognostic markers for trifluridine/tipiracil efficacy in metastatic gastric cancer have yet to be established.
Based on its efficacy and tolerability, the current National Comprehensive Cancer Network (NCCN) guidelines recommend trifluridine/tipiracil as a preferred option for the third- or subsequent-line treatment of metastatic gastric cancer in patients with low-volume gastric cancer with few or no symptoms, and who can tolerate oral drug administration [2]. Irinotecan or a taxane are among the agents recommended in the second-line or subsequent setting, provided they have not already been used for second-line therapy [2]. The latest European Society for Medical Oncology clinical practice guidelines for gastric cancer were published prior to the approval of trifluridine/tipiracil in this indication, and thus currently do not include the drug as a treatment option [4].
Trifluridine/tipiracil was not estimated to be a cost-effective third- or subsequent-line treatment option relative to placebo, when used in combination with BSC in heavily pre-treated patients with metastatic gastric cancer in a recent pharmacoeconomic analysis conducted from the US payer perspective; the incremental cost per quality-adjusted life year gained ($US 986,333) was well above the willingness-to-pay threshold of $US 50,000–150,000 [29]. Further pharmacoeconomic analyses would be of interest.
In conclusion, trifluridine/tipiracil improves overall survival and has a manageable tolerability profile in patients with metastatic gastric cancer who have received at least two prior therapies for advanced disease. Given its efficacy and tolerability, trifluridine/tipiracil provides a useful treatment option beyond second line for patients who have progressed on prior therapies, and have limited treatment options and a poor prognosis.
Data Selection trifluridine/tipiracil: 158 records identified
| Duplicates removed | 44 |
| Excluded during initial screening (e.g. press releases; news reports; not relevant drug/indication; preclinical study; reviews; case reports; not randomized trial) | 62 |
| Excluded during writing (e.g. reviews; duplicate data; small patient number; nonrandomized/phase I/II trials) | 23 |
| Cited efficacy/tolerability articles | 5 |
| Cited articles not efficacy/tolerability | 24 |
| Search Strategy: EMBASE, MEDLINE and PubMed from 1946 to present. Clinical trial registries/databases and websites were also searched for relevant data. Key words were trifluridine/tipiracil, Lonsurf, gastric cancer. Records were limited to those in English language. Searches last updated 29 August 2019. | |
Acknowledgements
During the peer review process the manufacturer of trifluridine/tipiracil was also offered an opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Compliance with Ethical Standards
Funding
The preparation of this review was not supported by any external funding.
Conflicts of interest
Connie Kang, Sohita Dhillon and Emma D. Deeks are salaried employees of Adis International Ltd/Springer Nature, are responsible for the article content and declare no relevant conflicts of interest.
Footnotes
Additional information for this Adis Drug Evaluation can be found at 10.6084/m9.figshare.9696506.
The manuscript was reviewed by:S.V. Sakpal, Department of Surgery, Medical College of Wisconsin, Milwaukee, Wisconsin, WI, USA, H. Hochster, Rutgers Cancer Institute of New Jersey, New Brunswick, New Jersey, NJ, USA, B.M. Chan, University of Southern California Norris Comprehensive Cancer Center, Los Angeles, CA, USA.
The original version of this article was revised due to a retrospective Open Access order.
Change history
9/18/2019
The article Trifluridine/Tipiracil: A Review in Metastatic Gastric Cancer, written by Connie Kang, Sohita Dhillon and Emma D. Deeks, was originally published Online First without open access
References
- 1.The Union for International Cancer Control. New Global Cancer Data: GLOBOCAN 2018. 2018. https://www.uicc.org/news/new-global-cancer-data-globocan-2018. Accessed 29 Aug 2019.
- 2.National Comprehensive Cancer Network. NCCN Guidelines Version 2.2019 Gastric Cancer. 2019. https://www.nccn.org. Accessed 29 Aug 2019.
- 3.Chan WL, Lam KO, So TH, et al. Third-line systemic treatment in advanced/metastatic gastric cancer: a comprehensive review. Ther Adv Med Oncol. 2019;11:1–11. doi: 10.1177/1758835919859990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smyth EC, Verheij M, Allum W, et al. Gastric Cancer: ESMO Clinical Practice Guidelines. Ann Oncol. 2016;27(Suppl 5):v38–v49. doi: 10.1093/annonc/mdw350. [DOI] [PubMed] [Google Scholar]
- 5.Taiho Oncology Inc. Lonsurf (trifluridine and tipiracil) tablets for oral use: US prescribing information. 2019. https://www.fda.gov. Accessed 29 Aug 2019.
- 6.European Medicines Agency. Lonsurf® (trifluridine/tipiracil): summary of product characteristics. 2017. https://www.ema.europa.eu. Accessed 29 Aug 2019.
- 7.Pharmaceuticals and Medical Devices Agency. Lonsurf Combination Tablets T15/Lonsurf Combination Tablets T20: Japanese prescribing information 2017. https://www.pmda.go.jp. Accessed 29 Aug 2019.
- 8.Burness CB, Duggan ST. Trifluridine/tipiracil: a review in metastatic colorectal cancer. Drugs. 2016;76(14):1393–1402. doi: 10.1007/s40265-016-0633-9. [DOI] [PubMed] [Google Scholar]
- 9.European Medicines Agency. Lonsurf receives CHMP positive opinion to include metastatic gastric cancer in European label [media release]. 2019. https://www.ema.europa.eu/en/medicines/human/summaries-opinion/lonsurf. Accessed 25 July 2019.
- 10.Taiho Pharmaceutical Co. Ltd. Anti-malignant tumor agent “LONSURF®” approved by European CHMP (Pharmaceutical Commission) Recommendation for additional indication of unresectable advanced/recurrent gastric cancer [media release]. 2019. https://www.taiho.co.jp/release/2019/20190729.html. Accessed 29 July 2019.
- 11.Lyseng-Williamson KA, Burness CB, Duggan ST. Trifluridine/tipiracil in metastatic colorectal cancer: a guide to its use. Drugs Ther Perspect. 2017;33(3):110–118. doi: 10.1007/s40267-017-0385-y. [DOI] [Google Scholar]
- 12.Lenz H, Stintzing S, Loupakis F. TAS-102, a novel antitumor agent: a review of the mechanism of action. Cancer Treat Rev. 2015;41(9):777–783. doi: 10.1016/j.ctrv.2015.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Emura T, Suzuki N, Fujioka A, et al. Potentiation of the antitumor activity of α, α, α-trifluorothymidine by the co-administration of an inhibitor of thymidine phosphorylase at a suitable molar ratio in vivo. Int J Oncol. 2005;27(2):449–455. [PubMed] [Google Scholar]
- 14.Tanaka N, Sakamoto K, Okabe H, et al. Repeated oral dosing of TAS-102 confers high trifluridine incorporation into DNA and sustained antitumor activity in mouse models. Oncol Rep. 2014;32(6):2319–2326. doi: 10.3892/or.2014.3487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yamashita F, Komoto I, Oka H, et al. Exposure-dependent incorporation of trifluridine into DNA of tumors and white blood cells in tumor-bearing mouse. Cancer Chemother Pharmacol. 2015;76(2):325–333. doi: 10.1007/s00280-015-2805-9. [DOI] [PubMed] [Google Scholar]
- 16.Shitara K, Doi T, Dvorkin M, et al. Trifluridine/tipiracil versus placebo in patients with heavily pretreated metastatic gastric cancer (TAGS): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2018;19(11):1437–1448. doi: 10.1016/S1470-2045(18)30739-3. [DOI] [PubMed] [Google Scholar]
- 17.Emura T, Suzuki N, Yamaguchi M, et al. A novel combination antimetabolite, TAS-102, exhibits antitumor activity in FU-resistant human cancer cells through a mechanism involving FTD incorporation in DNA. Int J Oncol. 2004;25(3):571–578. [PubMed] [Google Scholar]
- 18.Matsuoka K, Nakagawa F, Kobunai T, et al. Trifluridine/tipiracil overcomes the resistance of human gastric 5-fluorouracil-refractory cells with high thymidylate synthase expression. Oncotarget. 2018;9(17):13438–13450. doi: 10.18632/oncotarget.24412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bendell JC, Patel MR, Yoshida K, et al. Phase 1 study of cardiac safety of TAS-102 in patients with advanced solid tumors. Cancer Chemother Pharmacol. 2016;77(6):1275–1283. doi: 10.1007/s00280-016-3031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cleary JM, Rosen LS, Yoshida K, et al. A phase 1 study of the pharmacokinetics of nucleoside analog trifluridine and thymidine phosphorylase inhibitor tipiracil (components of TAS-102) vs trifluridine alone. Investig New Drugs. 2017;35(2):189–197. doi: 10.1007/s10637-016-0409-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yoshino T, Kojima T, Bando H, et al. The effect of food on the pharmacokinetics of TAS-102 and its efficacy and safety in patients with advanced solid tumors. Cancer Sci. 2016;107(5):659–665. doi: 10.1111/cas.12912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee JJ, Seraj J, Yoshida K, et al. Human mass balance study of TAS-102 using 14C analyzed by accelerator mass spectrometry. Cancer Chemother Pharmacol. 2016;77(3):515–526. doi: 10.1007/s00280-016-2965-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alsina M, Tabernero J, Shitara K, et al. Analysis of symptoms and functional HRQoL scales in TAGS, a phase III trial of trifluridine/tipiracil (FTD/TPI) in metastatic gastric cancer (mGC) [abstract no. 4043 plus poster]. J Clin Oncol. 2019;37(Suppl 1).
- 24.Van Cutsem E, Hochster H, Shitara K, et al. Pooled safety analysis from phase 3 studies of trifluridine/tipiracil (FTD/TPI) in patients (pts) with metastatic gastric/gastroesophageal junction cancer (mGC/mGEJC) and metastatic colorectal cancer (mCRC) [abstract no. 4039 plus poster]. J Clin Oncol. 2019;37(Suppl 1).
- 25.Bando H, Doi T, Muro K, et al. A multicenter phase II study of TAS-102 monotherapy in patients with pre-treated advanced gastric cancer (EPOC1201) Eur J Cancer. 2016;62(Jul):46–53. doi: 10.1016/j.ejca.2016.04.009. [DOI] [PubMed] [Google Scholar]
- 26.Neugut AI, Prigerson HG. Curative, life-extending, and palliative chemotherapy: new outcomes need new names. Oncologist. 2017;22(8):883–885. doi: 10.1634/theoncologist.2017-0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zheng Y, Zhu XQ, Ren XG. Third-line chemotherapy in advanced gastric cancer: a systematic review and meta-analysis. Medicine (Baltimore). 2017;96(24):e6884. doi: 10.1097/MD.0000000000006884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kasi PM, Kotani D, Cecchini M, et al. Chemotherapy induced neutropenia at 1-month mark is a predictor of overall survival in patients receiving TAS-102 for refractory metastatic colorectal cancer: a cohort study. BMC Cancer. 2016;16(1):467. doi: 10.1186/s12885-016-2491-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhou K, Zhou J, Zhang M, et al. Cost-effectiveness of trifluridine/tipiracil (TAS102) for heavily pretreated metastatic gastric cancer. Clin Transl Oncol. 2019 doi: 10.1007/s12094-019-02127-6. [DOI] [PubMed] [Google Scholar]


