Abstract
Introduction
We examined past-12-month quit attempts and smoking cessation from 2006 to 2016 while accounting for demographic shifts in the US population. In addition, we sought to understand whether the current use of electronic cigarettes was associated with a change in past-12-month quit attempts and successful smoking cessation at the population level.
Methods
We analyzed data from 25- to 44-year-olds from the National Health Interview Survey (NHIS) from 2006 to 2016 (N = 26,354) and the Tobacco Use Supplement to the Current Population Survey (TUS-CPS) in 2006–2007, 2010–2011, and 2014–2015 (N = 33,627). Data on e-cigarette use were available in the 2014–2016 NHIS and 2014–2015 TUS-CPS surveys.
Results
Past-12-month quit attempts and smoking cessation increased in recent years compared with 2006. Current e-cigarette use was associated with higher quit attempts (adjusted odds ratio [aOR] = 2.29, 95% confidence interval [CI] = 1.87 to 2.81, p < .001) and greater smoking cessation (aOR = 1.64, 95% CI = 1.21 to 2.21, p = .001) in the NHIS. Multivariable logistic regression of the TUS-CPS data showed that current e-cigarette use was similarly significantly associated with increased past-12-month quit attempts and smoking cessation. Significant interactions were found for smoking frequency (everyday and some-day smoking) and current e-cigarette use for both outcomes (p < .0001) with the strongest positive effects seen in everyday smokers.
Conclusions
Compared with 2006, past-12-month quit attempts and smoking cessation increased among adults aged 25–44 in recent years. Current e-cigarette use was associated with increased past-12-month quit attempts and successful smoking cessation among established smokers. These findings are relevant to future tobacco policy decisions.
Implications
E-cigarettes were introduced into the US market over the past decade. During this period, past-12-month quit attempts and smoking cessation have increased among US adults aged 25–44. These trends are inconsistent with the hypothesis that e-cigarette use is delaying quit attempts and leading to decreased smoking cessation. In contrast, current e-cigarette use was associated with significantly higher past-12-month quit attempts and past-12-month cessation. These findings suggest that e-cigarette use contributes to a reduction in combustible cigarette use among established smokers.
Introduction
Cigarette smoking is a leading cause of preventable death, accounting for more than 480,000 deaths in the United States annually.1 Smoking is linked to heart disease, lung disease, and multiple cancers, and on average, smokers die 10 years earlier than nonsmokers.1,2 In addition to harmful effects on health at both the individual and population levels, smoking imposes an immense financial burden on society, with a cost to the US economy of more than $300 billion each year.1,3
In 2007, the Institute of Medicine (IOM) published “Ending the Tobacco Problem: A Blueprint for the Nation.” Using data from the National Health Interview Survey (NHIS), the report described the smoking behavior of US adults from 1965 to 2005.4 During this 40-year period, the prevalence of current smoking declined from 42% to 21%. This dramatic decline was attributed to a decrease in ever smoking, defined as smoking 100 or more cigarettes lifetime, and to an increase in smoking cessation. In 1965, 56% of respondents reported ever smoking, compared with only 46% of respondents in 2005. The increase in smoking cessation was even more striking, with the percentage of ever smokers who reported now being former smokers rising from 24% in 1965 to 51% in 2005. Further examination revealed that most of the increase in cessation occurred between 1965 and 1991, when cessation almost doubled from 24% to 47%. It then gradually increased from 47% in 1991 to 51% in 2005.
The increase in former smoking that occurred from 1965 to 2005 is attributed to the numerous public health campaigns and interventions that were introduced during this period to encourage smokers to quit. Smoking has been broadly targeted by media campaigns, increases on cigarette taxes, indoor smoking policies, and comprehensive smoke-free laws.5,6 Multiple efforts have also been made to help smokers quit. Prescription nicotine replacement therapy was introduced in the United States in 1984. In 1996, nicotine gum and nicotine patches were approved for over-the-counter sale, and utilization increased over 150% from 1996-1997.7,8 The first non-nicotine replacement medication for smoking cessation, bupropion, was approved by the Food and Drug Administration in 1997, and the second, varenicline, was approved in 2006.9–11
In the past decade, another change in the smoking landscape has been the introduction of electronic cigarettes (e-cigarettes). E-cigarettes first became available to the US market in 2006, and its use grew quickly; they are particularly popular among smokers of combustible cigarettes, as many believe that e-cigarettes can help them quit.12,13 However, the scientific community has been divided on the use of e-cigarettes as a smoking cessation aid.14,15 Some argue that e-cigarettes are less harmful than combustible cigarettes and may help smokers quit,16–19 whereas others express concern that the use of both cigarettes and e-cigarettes (dual use) might prolong smoking. This could occur because the use of e-cigarettes might allow smokers to reduce their smoking modestly, perhaps reducing smokers’ worries about smoking-related harm, reducing the economic costs of smoking, or by providing a way to obtain nicotine in no-smoking contexts.20–22
The debate is further complicated by inconsistent research findings. A recent prospective cohort study by Weaver et al.23 surveyed a random sample of US adults who were current smokers of combustible cigarettes. At 1-year follow-up of 858 respondents who smoked, they found that respondents who had also used e-cigarettes were less likely to have stopped smoking combustibles than those who had not used e-cigarettes. This was true whether the e-cigarette use was reported at baseline, at 1-year follow-up, or at any other point during the study period. Based on their findings, the authors concluded that e-cigarette use may not increase population quit rates of combustible cigarettes.
In contrast, recent cross-sectional research by Zhu et al.24 found that past year e-cigarette use among combustible cigarette smokers was associated with an increase in past-12-month quit attempts and cessation in a large, nationally representative survey of the United States (N = 23,270). Using data from the Tobacco Use Supplement to the Current Population Survey (TUS-CPS) for the years 2014–2015 (the only years for which e-cigarette data were available), they found that past-12-month quit attempts and cessation rates were significantly higher among smokers who also reported use of e-cigarettes in the past 12 months compared with smokers who did not.24 When analyzing only smokers who did not use e-cigarettes, past-12-month quit attempts and cessation remained flat across four survey periods ranging from 2001–2002 to 2010–2011. A significant increase in cessation at the population level was observed from 2010–2011 to 2014–2015, and this was associated with higher cessation among the e-cigarette users. The authors concluded that the use of e-cigarettes resulted in the first significant increase in the population cessation rate in the United States in the past 15 years.
In this current study, we used two large US national surveys, the NHIS and the TUS-CPS, to examine past-12-month quit attempts and smoking cessation from 2006 to 2016 while adjusting for changes in population demographics during this time. A second purpose of the current study was to use a second national sample, the NHIS, to extend the findings of the Zhu et al.24 study, which suggested that increases in past-12-month quit attempts and smoking cessation observed in the 2014–2015 TUS-CPS were associated with e-cigarette use.
Methods
Sample
We analyzed existing data from two large national surveys: the NHIS25 and the TUS-CPS.26–28 The NHIS and TUS-CPS datasets are coded and publically available through an open access policy.
The NHIS, administered by the Centers for Disease Control and Prevention, is an ongoing survey of a nationally representative sample of the noninstitutionalized US population. The survey has assessed smoking behaviors annually since 1963; we used data from the 2006 to 2016 surveys.25 The survey is conducted annually in approximately 35,000 households using a multistage probability sampling design. A detailed description of the survey methodology can be found on the NHIS website.29
The TUS-CPS is administered by the US Census Bureau and is a nationally representative, cross-sectional survey of tobacco use.30 The core CPS is a labor force survey conducted monthly in approximately 140,000 individuals living in 50,000 households using a multistage probability sampling design. In selected months, CPS sample households are also asked to complete the Tobacco Use Supplement. The TUS-CPS is funded by the National Cancer Institute, and it has been conducted approximately every 3–4 years since 1992. We analyzed data from the 2006–2007, 2010–2011, and 2014–2015 surveys.26–28 Additional details regarding methods and the sampling procedure are published elsewhere.30
We analyzed data from respondents who participated in the NHIS 2006–2016 surveys or the TUS-CPS 2006–2007, 2010–2011, and 2014–2015 surveys; were 25–44 years old; and reported their smoking status. We included respondents who were aged 25–44 years at the time of survey to focus on a more homogeneous segment of the population and to reduce potential age-related differences in smoking behaviors with respect to combustible cigarette and e-cigarette usage. Focusing on this age range also avoids bias among younger participants who may not have had sufficient time to develop their smoking behaviors. Limiting the sample to this age range also avoids bias among older participants who may have health comorbidities that influence their smoking status and eliminates potential for survivor bias because of increased mortality among those who smoke.31,32 In addition, this strategy provides a similarly aged comparison group over time given that the age distribution of the United States has changed over the last several decades.
Measures
In both datasets, current smokers were defined as individuals who had smoked at least 100 cigarettes in their lifetime and answered “every day” or “some days” to the question “Do you now smoke cigarettes every day, some days, or not at all?” Former smokers were defined as ever smokers who answered “not at all” to the question “Do you now smoke cigarettes every day, some days, or not at all?” E-cigarette usage was queried in the most recent NHIS (2014–2016) and TUS-CPS (2014–2015) surveys. Current e-cigarette users were those who answered “every day” or “some days” to the question “Do you now use an e-cigarette every day, some days, or not at all?”
We analyzed past-12-month quit attempts and smoking cessation among respondents who were current smokers or reported quitting less than 12 months ago. In both the NHIS and the TUS-CPS, a quit attempt was defined as having tried to quit smoking and abstaining for at least 1 day in the past 12 months. Past-12-month cessation was defined as the percentage of smokers who had quit in the past 12 months and remained abstinent for at least 3 months at the time of the interview.
In addition, we considered demographic characteristics that might affect smoking behaviors in our logistic regression models, including sex, age, race/ethnicity, education, employment status, geographic region, and annual household income. For the TUS-CPS, we also included combustible cigarette smoking frequency (every day or some days) as a covariate. Smoking frequency was not included as a covariate in the NHIS analyses because this information was only available for current smokers and not for former smokers.
Data Analysis
Data for the NHIS were accessed through the Integrated Public Use Microdata Series (IPUMS).25 Data from the 2010–2011 and 2014–2015 TUS-CPS surveys were downloaded from the TUS-CPS website.26,27 Data from the 2006–2007 TUS-CPS survey were requested from the US Census Bureau.28 All statistical analyses were performed using SAS 9.4 (Cary, NC) using survey procedures and weighted to produce nationally representative estimates and to account for complex sample design. Self-response replicate weights, derived using balanced repeated replication (BRR), were used to obtain estimates of variance for TUS-CPS data analyses. Multivariable logistic regression analyses were used to test whether past-12-month quit attempts and past-12-month cessation rates changed over time by entering survey year as a categorical variable and adjusting for sex, age, race/ethnicity, education, employment status, geographic region, and annual household income. Smoking frequency (every day vs some-day smoking) was also included for TUS-CPS analyses.
For the survey years in which e-cigarette data were available in the NHIS (2014–2016) and TUS-CPS (2014–2015), past-12-month quit attempts and cessation were stratified by e-cigarette use. E-cigarette usage was divided into two categories: (1) current e-cigarette use defined as e-cigarette use every day or some days at the time of the survey and (2) no current e-cigarette use, which included never use of an e-cigarette and previous e-cigarette use, but none at the time of the survey.
Results
The demographic characteristics of the samples analyzed from the NHIS (N = 26,354) and the TUS-CPS (N = 33,627) are presented in Supplementary Table 1. Analyses of past-12-month quit attempts and smoking cessation focused on current smokers (NHIS N = 24,027 and TUS-CPS N = 30,045) and recent former smokers (NHIS N = 2,327 and TUS-CPS N = 3,582).
Past-12-Month Quit Attempts 2006–2016
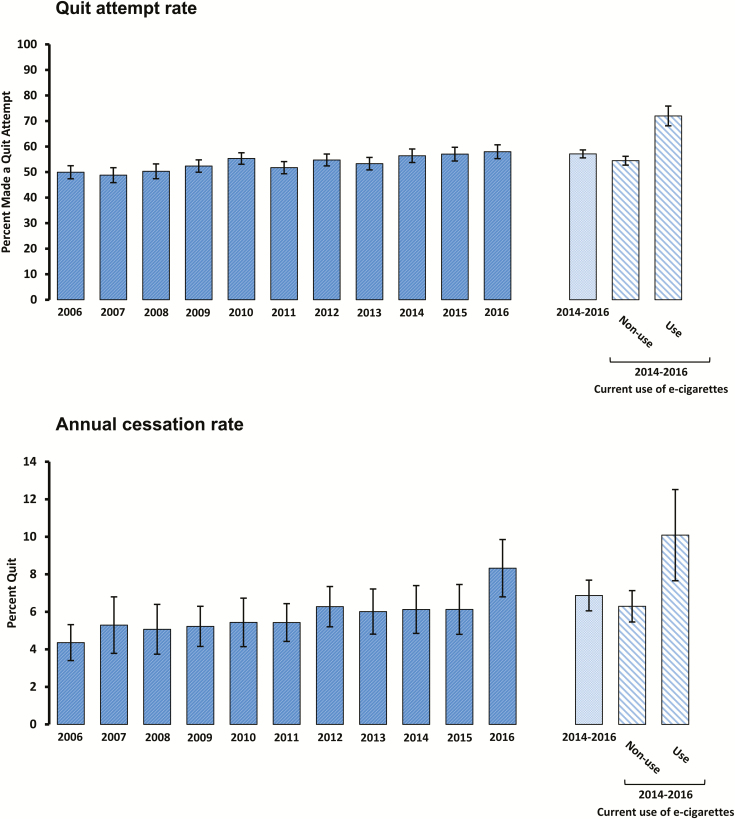
In the NHIS dataset, past-12-month quit attempts increased from 49.9% in 2006 to 58.0% in 2016 (Figure 1A). Multivariable regression analyses showed that past-12-month quit attempts increased significantly in 2014, 2015, and 2016 relative to the year 2006 (p < .05 for all comparisons) (Table 1; results of the full model are included in Supplementary Table 2). In the TUS-CPS dataset, past-12-month quit attempts increased from 38.6% in 2006–2007 to 46.3% in 2014–2015 (Supplementary Figure 1a). Compared with 2006–2007, past-12-month quit attempts increased significantly in 2010–2011 (adjusted odds ratio [aOR] = 1.07, 95% confidence interval [CI] = 1.04 to 1.11, p = .0002) and in 2014–2015 (aOR = 1.29, 95% CI = 1.24 to 1.34, p < .0001) (Supplementary Table 3). In the TUS-CPS dataset, analyses included a comparison between everyday smokers and some-day smokers. Those who smoked every day were significantly less likely to make a quit attempt in the past 12 months (aOR = 0.89, 95% CI = 0.86 to 0.92, p < .0001) compared with some-day smokers.
Figure 1.
Past-12-month quit attempts and smoking cessation in 25- to 44-year-olds, NHIS 2006–2016. (A) Quit attempt rate (defined as having tried to quit smoking and stopping smoking for at least 1 day during the past 12 months). For survey years containing data on e-cigarette use (2014–2016), the quit attempt rate is stratified according to current e-cigarette use. (B) Annual cessation rate (defined as quitting during the past 12 months and remaining abstinent for at least 3 months at the time of interview). For survey years containing data on e-cigarette use (2014–2016), the cessation rate is stratified according to current e-cigarette use.
Table 1.
Adjusted Odds Ratiosa for Past-12-Month Quit Attempts and Past-12-Month Smoking Cessation, NHIS 2006–2016
| Quit attemptb | Smoking cessationc | |||||
|---|---|---|---|---|---|---|
| aOR | 95% CI | p | aOR | 95% CI | p | |
| Year | ||||||
| 2006 | ref | ref | ||||
| 2007 | 0.92 | 0.79–1.06 | .25 | 1.16 | 0.79–1.70 | .44 |
| 2008 | 0.96 | 0.82–1.11 | .58 | 1.10 | 0.78–1.56 | .59 |
| 2009 | 1.04 | 0.90–1.20 | .62 | 1.17 | 0.85–1.61 | .33 |
| 2010 | 1.16 | 1.01–1.34 | .04 | 1.20 | 0.85–1.70 | .29 |
| 2011 | 1.00 | 0.87–1.14 | .98 | 1.21 | 0.89–1.65 | .23 |
| 2012 | 1.13 | 0.98–1.29 | .09 | 1.37 | 1.01–1.84 | .04 |
| 2013 | 1.07 | 0.94–1.23 | .31 | 1.33 | 0.97–1.81 | .08 |
| 2014 | 1.20 | 1.03–1.39 | .02 | 1.35 | 0.97–1.89 | .08 |
| 2015 | 1.26 | 1.08–1.46 | .003 | 1.39 | 0.99–1.95 | .05 |
| 2016 | 1.26 | 1.08–1.47 | .003 | 1.89 | 1.38–2.59 | <.0001 |
aOR = adjusted odds ratio; CI = confidence interval.
aAdjusted for sex, age, race/ethnicity, educational attainment, employment status, geographic region, and annual household income.
bDefined as having tried to quit smoking and stopping smoking for at least 1 day during the past 12 months.
cDefined as quitting during the past 12 months and remaining abstinent for at least three months at the time of the interview.
Past-12-Month Smoking Cessation 2006–2016
From 2006 to 2016, past-12-month smoking cessation increased from 4.4% to 8.3% in the NHIS sample (Figure 1B). Multivariable logistic regression results indicated that the only significant increase in annual cessation occurred in 2016 relative to 2006 (aOR = 1.89, 95% CI = 1.38 to 2.59, p < .0001) (Table 1; results of the full model are included in Supplementary Table 2). Similar trends were seen in the TUS-CPS, with annual cessation increasing from 4.6% in 2006–2007 to 6.0% in 2014–2015 (Supplementary Figure 1b). Compared with 2006–2007, the only significant increase in annual cessation was seen in the most recent survey period 2014–2015 (aOR = 1.24, 95% CI = 1.15 to 1.34, p < .0001) (Supplementary Table 3). Everyday smokers were less likely to report past-12-month cessation compared with some-day smokers (aOR = 0.82, 95% CI = 0.76 to 0.87, p < .0001).
Relation of Past-12-Month Quit Attempts and E-Cigarette Use 2014–2016
We further focused on the NHIS surveys from 2014–2016 to examine the relation of past-12-month quit attempts and e-cigarette use. Of these respondents, 15.2% (N = 1,045) were current e-cigarette users. Past-12-month quit attempts for the years 2014–2016 for smokers who were not currently using e-cigarettes at the time of the survey (54.5%) were similar to those in previous years (50.0% in 2006 to 53.3% in 2013) (Figure 1A). However, among those using e-cigarettes at the time of the survey, 72.0% reported making a quit attempt during the past 12 months. Multivariable regression analyses for the years 2014–2016 revealed that past-12-month quit attempts for current e-cigarette users were significantly higher than for nonusers (aOR = 2.29, 95% CI = 1.87 to 2.81, p < .0001) (results of the full model are included in Supplementary Table 4).
Similar findings were seen in the TUS-CPS dataset, with 13.5% (N = 1,215) of respondents reporting current e-cigarette use. The prevalence of past-12-month quit attempts for smokers who were not using e-cigarettes at the time of the 2014–2015 survey was 43.3%, which was similar to the prevalence in 2006–2007 (38.6%) and 2010–2011 (41.5%). Among smokers who were current e-cigarette users in 2014–2015, 65.8% had made a past-12-month quit attempt (Supplementary Figure 1a). The TUS-CPS dataset had additional information on smoking frequency (every day vs some days) in those who quit in the past 12 months. We divided combustible cigarette smokers into those who smoked some days and those who smoked every day and examined past-12-month quit attempts and current e-cigarette use. Current e-cigarette use at the time of the survey was associated with increased past-12-month quit attempts in both some-day and everyday combustible cigarette smokers. Among some-day smokers, 60.9% who currently used e-cigarettes reported making a quit attempt during the past 12 months compared with 46.7% of those who did not use e-cigarettes (Supplementary Figure 2a). Among everyday smokers, a past-12-month quit attempt was made by 67.1% of those who used e-cigarettes and by 42.2% of those who did not use e-cigarettes (Supplementary Figure 2a).
A multivariable logistic regression of the TUS-CPS 2014–2015 data revealed a significant interaction between smoking frequency (everyday and some-day smoking) and current e-cigarette use (p < .0001) in influencing past-12-month quit attempts. Some-day smokers who were not current e-cigarette users served as the reference group. Some-day smokers who currently used e-cigarettes were more likely to make past-12-month quit attempts (aOR = 1.70, 95% CI = 1.43 to 2.01, p < .0001; Supplementary Table 5) as were everyday smokers who used e-cigarettes (aOR = 2.42, 95% CI = 2.18 to 2.67, p < .0001). Everyday smokers who were not currently using e-cigarettes were less likely to make a quit attempt in the past 12 months (aOR = 0.86, 95% CI = 0.81 to 0.92, p < .0001).
Relation of Past-12-Month Cessation and E-Cigarette Use 2014–2016
With respect to smoking cessation in the past 12 months, current e-cigarette users also had higher rates of smoking cessation than nonusers in the NHIS dataset. For 2014–2016, 10.1% of those currently using e-cigarettes reported quitting in the past 12 months compared with 6.3% of those not currently using e-cigarettes (Figure 1B). Multivariable logistic regression confirmed that current e-cigarette use was associated with significantly higher past-12-month cessation for 2014–2016 (aOR = 1.64, 95% CI = 1.21 to 2.21, p = .001) (results of the full model are included in Supplementary Table 4).
Results were similar in the 2014–2015 TUS-CPS dataset, with a past-12-month cessation rate of 9.5% for current e-cigarette users compared with 5.5% for those not currently using e-cigarettes (Supplementary Figure 1b). Current e-cigarette use made no significant difference in past-12-month cessation among some-day smokers; 5.6% of those who currently used e-cigarettes reported quitting as did 7.1% of those who did not use e-cigarettes (Supplementary Figure 2b). Among everyday smokers, however, current e-cigarette use made a significant difference in past-12-month cessation; 10.6% of everyday smokers who used e-cigarettes reported quitting in the past 12 months as compared with 5.0% of everyday smokers who did not use e-cigarettes (Supplementary Figure 2b).
Multivariable logistic regression of TUS-CPS 2014–2015 data showed that current e-cigarette use was significantly associated with increased past-12-month smoking cessation, and yielded a significant interaction for smoking frequency (everyday and some-day smoking) and current e-cigarette use (p < .0001). Current e-cigarette use was not associated with combustible cigarette smoking cessation in the past 12 months among some-day smokers (aOR = 0.74, 95% CI = 0.54 to 1.02, p = .06; Supplementary Table 5). Everyday smokers who were not currently using e-cigarettes were less likely to have successfully quit smoking in the past 12 months (aOR = 0.86, 95% CI = 0.75 to 0.98, p = .03) compared with some-day smokers who were not current e-cigarette users. Everyday smokers who currently used e-cigarettes were significantly more likely to quit smoking during the past 12 months compared with the reference group of some-day smokers who did not currently use e-cigarettes (aOR = 1.89, 95% CI = 1.57 to 2.28, p < .0001).
Extension of Analyses to Other Age Groups
We repeated the analysis of past-12-month quit attempts and smoking cessation by current e-cigarette use for smokers aged 18–24 and those aged 45 and older. In keeping with the results for 25- to 44-year-olds, in 18- to 24-year-olds a significantly higher proportion of e-cigarette users reported past-12-month quit attempts in the NHIS (aOR = 1.89, 95% CI = 1.22 to 2.91, p < .005) and the TUS-CPS (aOR = 1.75, 95% CI = 1.46 to 2.12, p < .0001). The same was true for those aged 45 years and older in both the NHIS (aOR = 2.12, 95% CI = 1.68 to 2.68, p < .0001) and the TUS-CPS (aOR = 2.21, 95% CI = 2.06 to 2.37, p < .0001). There was no difference in past-12-month smoking cessation between current e-cigarette users and nonusers among the 18- to 24-year-olds in either dataset. However, consistent with the results for 25- to 44-year-olds, among those aged 45 years and older, a significantly higher proportion of e-cigarette users reported past-12-month cessation than nonusers in both the NHIS (aOR = 2.05, 95% CI = 1.39 to 3.01, p = .0003) and the TUS-CPS (aOR = 1.76, 95% CI = 1.56 to 1.99, p < .0001).
Discussion
Since the introduction of e-cigarettes to the US market, there has been speculation that e-cigarettes will have a detrimental effect on smoking cessation by delaying quit attempts or reducing smoking cessation success among those who attempt to quit. In two large, nationally representative surveys, past-12-month quit attempts and successful smoking cessation significantly increased in the years of increased e-cigarette use as compared with 2006. Importantly, combustible cigarette smokers who reported current use of e-cigarettes at the time of the survey also reported significantly more past-12-month attempts to quit smoking and had higher rates of successful cessation in the past 12 months than did those who did not currently use e-cigarettes. These data are inconsistent with the hypothesis that e-cigarette usage has been detrimental to smoking cessation among established combustible cigarette smokers at a population-based level.
Strengths and Limitations
Our study has several methodological strengths. We used two large, nationally representative surveys of the US population to examine and confirm trends in past-12-month quit attempts and smoking cessation among adults. We also adjusted for demographic changes in the population during this period of time while examining trends in smoking behavior. Furthermore, our study focused analyses on those aged 25–44, as this group has transitioned through the development of smoking behaviors and is less affected than older adults by health conditions that may influence smoking status. We decided to analyze data from 2006 to 2016 because that period encompassed years that preceded and years that followed the introduction and widespread use of e-cigarettes into the US market; this was intended to enhance detection of e-cigarette effects.
The findings of this study are limited by several factors. Our study was cross-sectional, preventing the determination of temporal relations and stronger causal inference. Also, the current analyses focused on those who were currently using e-cigarettes; this may over-represent those who found e-cigarettes especially effective or satisfying. The surveys used relied on participant self-report, and questions about smoking behavior and cessation strategies were limited. In addition, questions about the use of e-cigarettes were not introduced into the surveys until 2014, so the lack of information regarding use of e-cigarettes in earlier survey years prevented a fuller exploration of the relationship between e-cigarette use and past-12-month quit attempts and smoking cessation.
Association of Smoking Cessation and E-cigarette Use
Nonetheless, our findings show that among combustible cigarette smokers, past-12-month quit attempts and smoking cessation were not lower among those using e-cigarettes, and instead e-cigarette use may have contributed to the recent increase in past-12-month quit attempts and smoking cessation. Examining the period from 2014 to 2016, and after adjusting for many characteristics that influence past-12-month quit attempts and smoking cessation (sex, age, race, education, employment status, geographic region, and annual household income), smokers who used e-cigarettes at the time of the survey reported significantly higher past-12-month quit attempts and smoking cessation than did smokers who did not use e-cigarettes. This finding was seen across both population-based datasets and is in keeping with Zhu et al.24 and other studies that found that e-cigarette use was positively associated with quit attempts and smoking cessation.13,16,33–35 In contrast, these population-based results did not confirm the prospective cohort study by Weaver et al.23 In that study of 858 combustible cigarette smokers who were followed over 1 year, those who used electronic nicotine devices (ENDs) were less likely to quit in the follow-up period. This study had just 248 ENDs users in the sample, which may not have captured the range of smoking behavior in a larger population-based study.
Extension of Association of E-cigarette Use and Smoking Cessation to Other Age Groups
The association between e-cigarette use and past-12-month quit attempts and smoking cessation also extends to other age groups. Past-12-month quit attempts were increased among those who currently used e-cigarettes in both younger (18–24 years) and older (45 years and older) age groups. E-cigarette use was associated with increased past-12-month smoking cessation in the older group, but not among the group under 25 years of age.
Interplay Between E-cigarette Use and Smoking Frequency
We were able to further examine past-12-month quit attempts and cessation according to smoking frequency (everyday and some-day smoking) in the TUS-CPS dataset. We found a significant interaction between smoking frequency and current e-cigarette use for both past-12-month quit attempts and smoking cessation. E-cigarette use was associated with increased quit attempts and successful smoking cessation in the group who overall was less likely to quit. Among everyday smokers, current e-cigarette use was significantly associated with past-12-month quit attempts (67.1% vs 42.2%) and cessation (10.6% vs 5.0%) compared with non–e-cigarette users. Among some-day smokers, current e-cigarette use was associated with increased past-12-month quit attempts (60.9% vs 46.7%), but did not alter past-12-month smoking cessation (5.6% vs 7.1%).
Balance Between Smoking Initiation and Cessation
The proportion of the population who smoke combustible cigarettes represents a dynamic balance between the number of individuals who initiate smoking and those who successfully quit and become former smokers. Most individuals initiate smoking by age 18,1 and our analyses focused on those aged 25–44 years from 2006 to 2016, which represented a population that established combustible cigarette smoking prior to the widespread entrance of e-cigarettes into the US market. E-cigarettes may be beneficial to this group in reducing combustible cigarette use; however, whether e-cigarettes contribute to greater initiation of combustible cigarette use among younger groups remains a public health concern and is not addressed in this study.
Conclusion
We examined past-12-month quit attempts and smoking cessation among adults aged 25–44 in the United States from 2006 to 2016. This is a particularly important period to analyze smoking behaviors given that it encompasses the introduction of e-cigarettes into the US market in 2006 and their subsequent increased use. Notably, during the period of time when e-cigarette use was markedly increasing, the use of combustible cigarettes declined. Past-12-month quit attempts and cessation rates are on the rise and show significant increases in the most recent NHIS and TUS-CPS surveys. At the very least, these findings suggest that current e-cigarette use does not delay quit attempts or prevent smoking cessation in this age group. In fact, the strongest findings with respect to e-cigarette use and past-12-month cessation were seen among everyday smokers—the group who has the most difficulty quitting. These findings clearly show that the introduction of e-cigarettes has not prevented a reduction of smoking in the population to date and may have encouraged it, though the use and effects of e-cigarettes may certainly change in the future. The current findings may be relevant to future tobacco control policies and interventions.
Supplementary Material
Supplementary data are available at Nicotine & Tobacco Research online.
Funding
Research reported in this paper was supported by National Institute on Drug Abuse (NIDA) grants R01DA036583 (LJB), R01DA042195 (RAG), R01DA038076 (LSC), R21DA033827 (RCC), and K12DA041449 (ATR); National Cancer Institute (NCI) grants U19CA203654 (LJB), P30CA091842 (LJB), and P30CA091842-16S2 (LSC); National Heart, Lung, and Blood Institute (NHLBI) grant R01HL109031 (TBB), National Institute on Alcohol Abuse and Alcoholism grant R21AA024888 (SMH), National Center For Advancing Translational Sciences grant TL1TR002344 (LJ), a grant from the Foundation for Barnes-Jewish Hospital (ATR), and by Grant 2015215 from the Doris Duke Charitable Foundation (SMH).
Declaration of Interests
LJB is listed as an inventor on Issued U.S. Patent 8,080,371, “Markers for Addiction” covering the use of certain single nucleotide polymorphisms in determining the diagnosis, prognosis, and treatment of addiction. The other authors have no financial disclosures.
References
- 1. U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: U.S. Dept of Health and Human Services; 2014. [Google Scholar]
- 2. Jha P, Ramasundarahettige C, Landsman V, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341–350. [DOI] [PubMed] [Google Scholar]
- 3. Xu X, Bishop EE, Kennedy SM, Simpson SA, Pechacek TF. Annual healthcare spending attributable to cigarette smoking: an update. Am J Prev Med. 2015;48(3):326–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Institute of Medicine. Ending the Tobacco Problem: A Blueprint for the Nation. Washington D.C: National Academies Press; 2007. [Google Scholar]
- 5. Wilson LM, Avila Tang E, Chander G, et al. Impact of tobacco control interventions on smoking initiation, cessation, and prevalence: a systematic review. J Environ Public Health. 2012;2012:961724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Levy DT, Tam J, Kuo C, Fong GT, Chaloupka F. The impact of implementing tobacco control policies: the 2017 tobacco control policy scorecard. J Public Health Manag Pract. 2018;24(5):448–457. doi: 10.1097/PHH.0000000000000780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shiffman S, Gitchell J, Pinney JM, Burton SL, Kemper KE, Lara EA. Public health benefit of over-the-counter nicotine medications. Tob Control. 1997;6(4):306–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shiffman S, Rolf CN, Hellebusch SJ, et al. Real-world efficacy of prescription and over-the-counter nicotine replacement therapy. Addiction. 2002;97(5):505–516. [DOI] [PubMed] [Google Scholar]
- 9. Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel Liaisons, and Staff. A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. Public Health Service report. Am J Prev Med. 2008;35(2):158–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ebbert JO, Wyatt KD, Hays JT, Klee EW, Hurt RD. Varenicline for smoking cessation: efficacy, safety, and treatment recommendations. Patient Prefer Adherence. 2010;4:355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wilkes S. The use of bupropion SR in cigarette smoking cessation. Int J Chron Obstruct Pulmon Dis. 2008;3(1):45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. National Academies of Sciences, Engineering, and Medicine. Public Health Consequences of E-cigarettes. Washington, D.C: The National Academies Press; 2018. [PubMed] [Google Scholar]
- 13. Delnevo CD, Giovenco DP, Steinberg MB, et al. Patterns of electronic cigarette use among adults in the United States. Nicotine Tob Res. 2016;18(5):715–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fairchild AL, Lee JS, Bayer R, Curran J. E-cigarettes and the harm-reduction continuum. N Engl J Med. 2018;378(3):216–219. [DOI] [PubMed] [Google Scholar]
- 15. Fairchild AL, Bayer R. Public health. Smoke and fire over e-cigarettes. Science. 2015;347(6220):375–376. [DOI] [PubMed] [Google Scholar]
- 16. Bullen C, Howe C, Laugesen M, et al. Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet. 2013;382(9905):1629–1637. [DOI] [PubMed] [Google Scholar]
- 17. Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2016;9:CD010216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhuang YL, Cummins SE, Sun JY, Zhu SH. Long-term e-cigarette use and smoking cessation: a longitudinal study with US population. Tob Control. 2016;25(Suppl 1):i90–i95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cahn Z, Siegel M. Electronic cigarettes as a harm reduction strategy for tobacco control: a step forward or a repeat of past mistakes?J Public Health Policy. 2011;32(1):16–31. [DOI] [PubMed] [Google Scholar]
- 20. Glantz SA, Bareham DW. E-cigarettes: use, effects on smoking, risks, and policy implications. Annu Rev Public Health. 2018;39:215–235. doi: 10.1146/annurev-publhealth-040617-013757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pisinger C. Why public health people are more worried than excited over e-cigarettes. BMC Med. 2014;12:226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. American Lung Association. Statement on E-cigarettes 2015. http://www.lung.org/our-initiatives/tobacco/oversight-and-regulation/statement-on-e-cigarettes.html. Accessed March 5, 2018.
- 23. Weaver SR, Huang J, Pechacek TF, Heath JW, Ashley DL, Eriksen MP. Are electronic nicotine delivery systems helping cigarette smokers quit? Evidence from a prospective cohort study of U.S. adult smokers, 2015-2016. PLoS One. 2018;13(7):e0198047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zhu SH, Zhuang YL, Wong S, Cummins SE, Tedeschi GJ. E-cigarette use and associated changes in population smoking cessation: evidence from US current population surveys. BMJ. 2017;358:j3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Blewett LA, Rivera Drew JA, Griffin R, King ML, Williams KC.. IPUMS Health Surveys: National Health Interview Survey, Version 6.2. Minneapolis, MN: University of Minnesota; 2016. [Google Scholar]
- 26. U.S. Department of Commerce, Census Bureau. National Cancer Institute-sponsored Tobacco Use Supplement to the Current Population Survey (2010–11). Data Files and Technical Documentation 2012. https://thedataweb.rm.census.gov/ftp/cps_ftp.html#cpssupps. Accessed February 23, 2018.
- 27. U.S. Department of Commerce, Census Bureau. National Cancer Institute and Food and Drug Administration Co-sponsored Tobacco Use Supplement to the Current Population Survey. 2014–15 2016. https://cancercontrol.cancer.gov/brp/tcrb/tus-cps/. Accessed February 23, 2018.
- 28. U.S. Department of Commerce, Census Bureau. National Cancer Institute and Centers for Disease Control and Prevention Co-sponsored Tobacco Use Supplement to the Current Population Survey (2006–07) 2008. https://cancercontrol.cancer.gov/brp/tcrb/tus-cps/. Accessed February 23, 2018.
- 29. Centers for Disease Control. About the National Health Interview Survey 2017. https://www.cdc.gov/nchs/nhis/about_nhis.htm. Accessed December 17, 2017.
- 30. National Cancer Institute, Division of Cancer Control & Population Sciences. What is the TUS-CPS?2018. https://cancercontrol.cancer.gov/brp/tcrb/tus-cps/. Accessed February 23, 2018.
- 31. Woloshin S, Schwartz LM, Welch HG. The risk of death by age, sex, and smoking status in the United States: putting health risks in context. J Natl Cancer Inst. 2008;100(12):845–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alzahrani T, Pena I, Temesgen N, Glantz SA. Association between electronic cigarette use and myocardial infarction. Am J Prev Med. 2018;55(4):455–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Levy DT, Yuan Z, Luo Y, Abrams DB. The relationship of e-cigarette use to cigarette quit attempts and cessation: Insights from a large, nationally representative U.S. Survey. Nicotine Tob Res. 2018;20(8):931–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Caponnetto P, Campagna D, Cibella F, et al. EffiCiency and Safety of an eLectronic cigAreTte (ECLAT) as tobacco cigarettes substitute: a prospective 12-month randomized control design study. PLoS One. 2013;8(6):e66317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Giovenco DP, Delnevo CD. Prevalence of population smoking cessation by electronic cigarette use status in a national sample of recent smokers. Addict Behav. 2018;76:129–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.