Abstract
Bariatric surgery has been considered as an effective treatment for morbid obesity. Apart from procedures related complications, a broad spectrum of neurological disorders affecting any part of neuraxis has been reported following BS. Central nervous system complications, although less common than peripheral nervous system complications, carry significant morbidity and potential mortality. Encephalopathy, behavioral and psychiatric disorders, myelopathy and optic neuropathy are the most frequently reported CNS complications. Early detection and prompt management may improve or completely reverse these neurological complications. It is essential that the treating physicians must be aware of their clinical manifestations and management, so early diagnosis and treatment can prevent patients from suffering significant neurological deficits and even death. This review discusses the clinical manifestations of these complications in detail which will help concerned physician in earlier recognition and hence prevent the delay in specific treatment.
As the prevalence of morbid obesity is increasing worldwide, greater number of persons suffering from obesity is undergoing bariatric surgery (BS) resulting in dramatic worldwide increase in BS in 21st century. In addition to significant weight loss, BS is also associated with improvement in obesity related co-morbidities. Unfortunately, this rise in BS surgery has brought with it a variety of previously unrecognized complications. Among these, the neurological complications have gained attention because of their diversity, complexity, and potentially devastating effects. Failure of recognition and delay in management of these complications especially those affecting the central nervous system (CNS) can lead to irreversible neurological deficits and even death. Most of these complications are attributed to vitamins and micronutrients deficiency. Thiamine, cobalamin, copper, zinc, vitamin A, and folic acid are the common nutrients involved in CNS complications of BS. In this review, we will discuss the clinical features, mechanism and management of different reported CNS complications after BS in detail with special emphasis on early recognition and timely management.
Obesity and its hazards
Obesity is a pathological condition characterized by accumulation and maintenance of excessive adipose tissue.1 Obesity is often assessed by body mass index (BMI) values, where a BMI of 30 kg/m2 or more is considered obesity, while BMI value between 25 and 29.9 kg/m2 is considered overweight.1-3 The terminology of overweight, obesity and severe obesity are continuum of a spectrum.4 Obesity is among one of the major risk factors for cardiovascular and cancer morbidity and mortality contributing to almost 3 million deaths every year worldwide.5 It is associated with an increased prevalence of morbidity and reduced life expectancy. The mortality risk associated with obesity was recognized even in the works of Hippocrates.6
A number of comorbidities have been associated to obesity including coronary artery disease, hypertension, stroke, a variety of cancers, non-insulin dependent diabetes mellitus, gall bladder disease, lipid disorders, osteoarthritis, and pulmonary diseases including sleep apnea as well as gout.2 Obesity has a negative impact on vascular risk factors and has not only been attributed to stroke but also to neurodegenerative disorders including dementia.7-9 Leptin, which is considered as anti-obesity hormone is also thought to have preventive effect on neuronal death and with increasing age, as the levels of circulating leptin decrease, the process of neurodegeneration can accelerate.9
Epidemiology of obesity
Obesity is not the problem of individuals. Obesity has reached pandemic proportions. The 2014 WHO facts sheet suggests that about 13% of world population is obese, with more than 1.9 billion adults 18 years and above being overweight.10 More alarming is the trend with doubling in worldwide prevalence of obesity between 1980 and 2014.10 Approximately 41 million children under the age of 5 were obese in 2014, with more than half of those living in Asia. Not only that, the mortality from obesity and overweight is more than the deaths from underweight.10 The rate of obesity and corresponding obesity associated disease burden has increased in past several decades despite countless research studies, national statements and efforts from worldwide organizations.11
Bariatric surgery: an overview
Obesity is highly preventable through healthier food selection and the implementation of regular physical activity. Surgical therapy for the management of obesity is recommended for people with BMI of ≥40 kg/m2 or for those with BMI ≥35 kg/m2 with additional obesity related complications like hypertension, type 2 diabetes mellitus, dyslipidemia, or obstructive sleep apnea.4 However, tremendous increases in demand for weight loss and the advancement in bariatric surgical procedures and techniques have made BS the most efficacious treatment for morbid obesity.12 Little over 340,000 bariatric surgeries were performed in the year 2011 by more than 6500 bariatric surgeons across the world.12 A number of surgical methods have been tried over past 50 years, many of those abandoned now. Currently the most commonly used methods are sleeve gastrectomy (SG), Roux-en-Y gastric bypass (RYGB), adjustable gastric banding (AGB), and biliopancreatic diversion/duodenal switch (BPD/DS).4,12 These are shown in Figure 1. In addition to surgical management, a number of endoscopic procedures have also been developed using intragastric balloons, sutures, malabsorptive techniques as well as botulinum toxin.13
Figure 1.
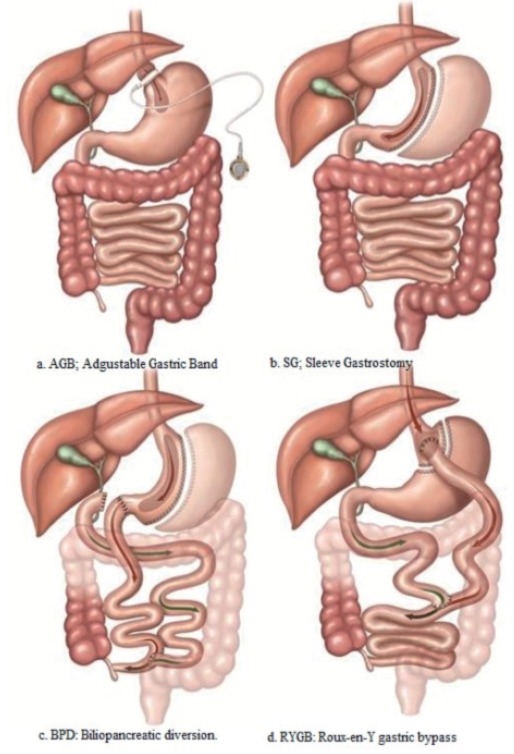
Commonly performed surgical methods for bariatric surgery a) AGB - Adjustable gastric band. A band with an inner inflatable silastic balloon is placed around the proximal stomach just below the gastroesophageal junction. The band is adjusted through a subcutaneous access port by the injection or withdrawal of solution. b) SG - Sleeve gastrectomy. The stomach is transected vertically creating a gastric tube and leaving a pouch of 100 to 200 mL. c) BPD - Biliopancreatic diversion. A 400 mL gastric pouch is formed from the stomach. The small bowel is divided 250 cm proximal to the ileocecal valve and is connected to the gastric pouch to create a Roux-en-Y gastroenterostomy. An anastomosis is performed between the excluded biliopancreatic limb and the alimentary limb 50 cm proximal to the ileocecal valve. d) RYGB - Roux-en-Y gastric bypass. An upper gastric pouch, of 15 to 30 mL in volume, and a lower gastric remnant is formed from the stomach. The jejunum is divided some 30 to 75 cm distal to the ligament of Treitz, and anastomosed to the gastric pouch. The distal jejunum is brought up as a ‘Roux-limb’. The excluded biliary limb, including the gastric remnant, is anastomosed to the bowel some 75 to 150 cm distal to the gastrojejunostomy.78
The primary aims of surgery are restriction of food intake and/or iatrogenic malabsorption of food.4 A number of mechanisms have been suggested to explain the weight loss accomplished by BS. Restriction of food intake due to small volume of the stomach pouch is a major contributor, resulting in decreased calories. Decreased nutrient absorption was considered an added mechanism.14 The decreased appetite and early satiety may not only be due to the decrease in the stomach space, but may also be contributed by neuronal and hormonal modulation.4 The so-called enteroencephalic endocrine axis is considered to contribute significantly through complex interactions between centers in the brain and hormone productions in the intestinal tract, as well as pancreas.14 Bariatric and metabolic surgery have shown to improve or resolve many obesity related complications and improve survival as well.15
Benefits of bariatric surgery
The outcomes following bariatric surgery vary between procedures, and predicting individual outcome is difficult. However, a number of conditions have been shown to improve after BS including cardiovascular health, systemic hypertension, diabetes mellitus, sleep apnea, lipid profile, as well as nonalcoholic fatty liver disease.4 Both fatal and non-fatal myocardial infarctions and strokes are reduced after BS.16 The incidence of first time cancer, and cancer related diagnosis appears to be decreased after BS.17,18 This risk reduction appears to be independent of the type of cancer, whether the cancer is considered obesity related or unrelated. The overall mortality, development of comorbid conditions and overall healthcare use have all been shown to be reduced after BS.19
Complications of bariatric surgery
Though clearly offering benefits to morbidly obese, BS is not a completely benign procedure. A number of complications of BS have been reported including death. Short or long term complication rates around 20% have been reported.20 Increasing expertise, safer methods, and use of laparoscopic procedures seem to have decreased the morbidity significantly.21 The initial reports suggested nearly 2% mortality risk, which over time has improved and mortality rate as low as 0.3% has been reported.22,23 Sepsis secondary to anastomosis leak, cardiac events and pulmonary emboli are the main cause of 30-day mortality.24
Apart from perioperative complications related to surgical procedures, BS is associated with significant gastrointestinal, metabolic, nutritional and neurological complications. Deficiencies of iron, and other essential elements, thiamine (vitamin B1), cobalamin (vitamin B12), folic acid and fat soluble vitamins can occur after BS. The risk of nutritional deficiencies depends on post-operative weight loss, the surgical procedure performed and patient compliance with follow up.25 Nutrient deficiencies that occur after BS are probably the most important long term complications as they may lead to potentially irreversible hematological, metabolic and neurological conditions.26
Neurological complications
Neurological complications occurring in BS are not uncommon. These complications have been reported to occur in 5-10% of patients after BS.27 Recently, a cross sectional study from Jeddah, KSA reported the rate of 3% (15) among 451 patients undergoing BS.28 In another retrospective study involving 592 post sleeve gastrectomy patients, only 7 (1.18%) were found to have neurological complications.29 Almost any region of the nervous system can be affected.27,30 These complications can be early or delayed and can occur months to several years after surgery. A number of neurological complications including encephalopathy, psychiatric disorders, behavioral changes, ataxia, myelopathy, optic neuropathy, plexopathy, peripheral polyneuropathy, mononeuropathy, myopathy, myotonia, and compartment syndrome have been described.27 Wernicke’s encephalopathy and polyneuropathy due to vitamin B1 deficiency can present within few days to week after BS and often proceeded by intractable vomiting. While myelopathy and neuropathy secondary to vitamin B12 deficiency may take years to develop.
Patterns of neurological complications
The neurological complications of BS had been classified in various ways based on timings, early versus late; site of involvement, peripheral versus central; and mechanism.31 Frequently, more than one part of neuraxis is involved.32 Early complications can manifest within days and weeks and include peripheral nerve damage due to stretch or compression injury, Wernicke’s encephalopathy and polyneuropathy or polyradiculoneuropathy. Late complications may only manifest after several years of surgery and include optic neuropathy, myelopathy, peripheral neuropathy and myopathy. In this paper, the neurological complications affecting CNS are reviewed according to site of involvement. Table 1 summarizes the various identified CNS complications after BS.
Table 1.
Central nervous system complications following bariatric surgery.
| Major disorders | Recognized complications |
|---|---|
| Encephalopathy | Wernicke’s encephalopathy (WE) |
| Encephalopathy associated with D-lactic acidosis | |
| • Hyperammonemic encephalopathy | |
| Neuropsychiatric disorders | • Frank eating disorders |
| • Anorexia nervosa | |
| • Bulimia nervosa | |
| • Binge eating behavior | |
| • Eating avoidance disorder | |
| • Suicide | |
| Myelopathy | • Posterolateral myelopathy |
| • Myeloneuropathy | |
| Optic neuropathy | • Nutritional optic neuropathy |
| Other possible conditions (need to be verified by further studies) | • Stroke and Seizures |
| • CNS demyelination | |
| • Spontaneous intracranial hypotension | |
| • Cognitive impairment secondary to focal brain atrophy |
CNS - central nervous system
Mechanisms of neurological complications
The most common underlying mechanism of neurological complications is nutritional deficiencies. Acute weight loss resulting in susceptibility to compression neuropathies is another mechanism. The patient undergoing BS, despite their obesity may have subclinical or overt nutritional deficiencies. After the surgery, the malabsorption results from a variety of mechanisms including decreased gastric acidity, decreased absorption due to bypass of proximal intestine, short food contact time, diarrhea, blind loop syndrome and deficiency of factors required for absorption of certain nutrients resulting from loss of functional gastrointestinal tract.32 Vitamin B12, thiamine, and copper are the commonest micronutrients involved in neurological complications, however, other potential but uncertain contributors include vitamins like folate, pyridoxine, riboflavin, vitamin D and vitamin E, minerals like calcium phosphorus and magnesium, and trace elements like zinc, iodine and selenium.32 Table 2 summarizes the potential mechanism and involved micronutrient in CNS complications of BS.
Table 2.
Central Nervous System complication and associated micronutrient.
| Conditions | Micronutrient involved and likely pathology |
|---|---|
| Wernicke’s encephalopathy | Thiamin (Vitamin B1) deficiency |
| Episodic encephalopathy | Elevated D-lactate |
| Hyperammonemic encephalopathy (HAE) | Elevated serum ammonia and plasma glutamine levels |
| Zinc deficiency | |
| Underlying Urea cycle disorder | |
| Myelopathy | Cobalamin (Vitamin B12) and Copper deficiency |
| Vitamin E, folate and B6 deficiency (less common) | |
| Optic Neuropathy | Cobalamin (Vitamin B12) deficiency |
| Vitamin A, Copper and zinc deficiency (less common) | |
| Spontaneous intracranial hypotension | Vitamin A and D deficiency |
| Spontaneous CSF leakage |
CSF - cerebrospinal fluid
Central nervous system complications of bariatric surgery
Wernicke’s Korsakoff syndrome (WKS), episodic encephalopathy associated with D-lactic acidosis, behavioral changes and neuropsychiatric disorders, CNS demyelination, myelopathy, myeloneuropathy, and optic neuropathy are some of the reported CNS complications. The relationship of stroke and seizures is still less well defined. Some of the reported complications as stroke, CNS demyelination and cognitive impairment following BS need to be verified by further randomized trials. Diagnostic findings and treatment of common CNS complications are outlined in Table 3.
Table 3.
Diagnosis and treatment of common central nervous system complications.
| Complications | Diagnosis | Treatment |
|---|---|---|
| Wernicke’s encephalopathy | Clinical | Intravenous thiamine 500 mg 3 times a day for 2-3 days followed by 250 mg daily for 3-5 days.32,36,38 |
| Erythrocyte transketolase activation assay or RBC thiamine diphosphate | Oral maintenance dose of 50-100 mg daily for long term | |
| Characteristic paraventricular signals on MRI | ||
| Encephalopathy associated with D-lactic acidosis: | Elevated D- lactate levels in serum and urine | Correction of metabolic acidosis |
| High an ion gap metabolic acidosis | Carbohydrate restriction | |
| Antibiotics43 | ||
| Hyperammonemic encephalopathy (HAE) | Measurement of plasma ammonia, zinc, glutamine and serum albumin level along with genetic testing for OTC enzyme deficiency | Dietary protein restriction Parenteral glucose and lipid infusion |
| Repletion of zinc, other micronutrients and amino acids. | ||
| Hemodialysis44 | ||
| Reversal of surgical procedure49 | ||
| Myelopathy secondary to vitamin B12 deficiency | Serum B12, methylmalonic and plasma homocysteine levels | Intramuscular 1000 mic gram daily for 7 days followed by once weekly and then monthly32 |
| Abnormal signals in dorsal column and corticospinal tract on MRI | ||
| Myelopathy secondary to copper deficiency | Serum and urinary copper | Parenteral; intravenous 2 mg daily of elemental copper for 5 days |
| Serum ceruloplasmin activity | Oral; 8 mg per day of elemental copper for 1st week, 6 mg for 2nd week, 4 mg for 3rd week and 2 mg thereafter32 | |
| MRI findings similar to B12 deficiency | ||
| Myelopathy secondary to folate deficiency | RBCs folate | Parenteral; 1-5 mg daily32 |
| Oral; 1 mg 3 times a day then maintenance dose of 1 mg per day |
RBC - red blood cells, MRI - Magnetic resonance imaging, HAE - Hyperammonemic encephalopathy, OTC - Ornithine transcarbamylase
Wernicke’s Korsakoff Syndrome (WKS)
Wernicke’s Korsakoff syndrome is the best known neurological complications of thiamine (vitamin B1) deficiency. Wernicke’s encephalopathy (WE) characterized by acute confusion, ataxia and nystagmus was described in late 19th century. Korsakoff syndrome (KS) is a sequela of WE seen in about 80 percent of survivors of Wernicke’s encephalopathy.32 The characteristic features of KS are anterograde amnesia, retrograde amnesia, confabulation (invention of new memories), apathy and lack of insight.33 Classically, Wernicke’s encephalopathy and KS have been described in relation to intractable vomiting, hyperemesis gravidarum and excessive alcohol intake. KS is more likely to be seen when WE is related to alcohol abuse.32
A relatively uncommon condition in modern world, WE has emerged as a serious and significant complication of BS. The exact incidence of WE after BS is unknown, however, more than 100 cases have been reported in literature. In an early series of 500 patients with BS, 0.4% patients developed WE.34 Systemic reviews discussing WE after BS have reported finding in 32 and 84 cases.35,36 More than 80% cases were women in both reviews with onset of symptoms between 2 weeks to 18 months of surgery. It happened after all modalities of BS and the patients had between 13-45% weight loss at the time of diagnosis. Recurrent vomiting for several days was the precipitant in most cases. In the patients who did not have recurrent vomiting, avoidance of food, poor appetite, rapid weight loss and noncompliance with vitamin supplementation were the possible precipitants.36 The classic triad of confusion, ataxia, and eye signs is not always present in these patients. Several additional neurological symptoms and signs including third and sixth cranial nerve palsies, dysarthria, dysmetria, asterixis, myoclonus, seizures, psychiatric symptoms, vestibular symptoms, blurred vision, papilledema and gait disturbances were seen.35,36 Polyneuropathy is often an associated complication. The entire spectrum may not be solely explained by the deficiency of thiamine and additional inflammatory mechanisms may play a role.35
Thiamine is a water soluble vitamin that has small reserves in the body and can be depleted in less than 3 weeks with decreased oral intake.37 The diagnosis remains mainly clinical, supported by laboratory and imaging studies. Serum and urine thiamine levels after BS are not reliable indicators of tissue levels. Red blood cell assays of relevant enzymes may be more sensitive indicators.32 MRI brain is the imaging modality of choice, although it may be normal in some cases. The typical abnormalities are seen in periventricular region, thalamus, hypothalamus, mammillary bodies, periaqueductal region, as well as other parts of brainstem and cerebellum. Rarely corpus callosum and basal ganglia may be involved.32,35 Untreated, the condition may be fatal. The treatment regimen is not very well defined; however, parenteral treatment is mostly recommended.32,36,38 Patients at risk should get parenteral thiamine before administration of glucose.32 In cases with established thiamine deficiency, supplementation with 30 mg twice daily for several months should be considered.38 In the reported literature of WE after BS, more than half of the patients made complete recovery. Those with incomplete recovery had residual cognitive deficits, psychosis, gait disturbances, and nystagmus. Fortunately, death was a rare complication.32,35
Encephalopathy associated with D-lactic acidosis
Few reports of encephalopathy characterized by episodes of confusion, behavioral abnormalities, weakness, lethargy, ataxia and dysarthria in association with D-lactic acidosis have been described after jujenoileostomy.39-43 The neurological symptoms often precipitated after high carbohydrate diets and believed to result from fermentation of carbohydrates in the colon or bypassed segment of the small bowel resulting in elevated levels of D-lactate. Although severe metabolic acidosis was considered to be associated with this condition, the serum chemistries and absence of anion gap may be misleading.42 Diagnosis is established by marked increase in D-lactate concentration in serum and urine. It is of note that most laboratories routinely check L-lactate and do not check the D-lactate levels. When this condition is suspected, D-lactate levels should be determined as L-lactate levels may be normal. High carbohydrate ingestion can reproduce the condition, whereas fasting and administration of intravenous amino acids reverses the metabolic changes and improves symptoms.40 A case report published in 2000 reported the occurrence of the condition 23 years post-surgery 42 and another in 2017 reported it in a 48 years old woman 4 years after BS.43 The condition has been treated with correction of metabolic acidosis, carbohydrate restriction or fasting and antibiotics acting on gut flora.43 This condition should always be considered as an important differential diagnosis in cases of episodic confusion with no other explained etiology.
Hyperammonemic encephalopathy (HAE)
Hyperammonemic encephalopathy has been recognized as a serious and potentially treatable CNS complications following gastric BS. Nearly 25 cases of HAE have been reported following RYGB in the absence of overt hepatic disease.44 It is hypothesized that nutritional complications following gastric BS may unmask preexisting subclinical urea cycle disorder such as ornithine transcarbamylase deficiency (OTC) which can lead to fatal hyperammonemia.45-47 In a retrospective review of 20 patients with gastric bypass associated hyperammonemia (GaBHA), 95% of patients were female. Weight loss, HAE associated with increased plasma glutamine levels, lack of evidence of cirrhosis, low serum albumin levels and reduced plasma zinc levels were commonly identified features. Mortality rate as high as 50% has been reported.48 Measurement of plasma ammonia, zinc, glutamine and serum albumin level along with genetic testing for OTC enzyme deficiency helps in early diagnosis of this clinical entity which carries high mortality rate. Dietary protein restriction, parenteral glucose and lipid infusion along with repletion of zinc, other micronutrients and amino acids is the mainstay of treatment. Hemodialysis is done in refractory cases.44 Reversal of surgical procedure may be one option.49
Neuropsychiatric disorders
Several neuropsychiatric and psychobehavioral disorders have been described in relation to BS. Many of the patients have existing psychological conditions prior to BS. Mood disorders, anxiety disorders and binge eating disorder comprise the large majority of pre-existing conditions in this population.50 Improvement in psychopathology after BS has been reported in studies.51,52 However, psychiatric disorders may appear following BS as well. Frank eating disorders like anorexia nervosa and bulimia are not uncommon. Few patients develop eating avoidance post surgically, the so called postsurgical eating avoidance disorder.53 Some patients with pre-surgical binge eating disorder may resort to binge eating behavior, however, gastric restrictions limits the ingestion of large amounts. Night eating syndrome, in which there is a potential circadian shift of eating and sleep, appears to decrease after BS.54
Alcohol use and other substance use disorder probably do not change much after BS. In a cohort of about 2000 patients, the alcohol use disorder was more common in the second postoperative year, compared to the first postoperative year and the year prior to surgery.55 There is inconclusive evidence about other addictive behaviors like gambling, compulsive shopping, and compulsive sexual behavior.53
The risk of suicide is higher in bariatric BS patients. Tindle et al56 reported the suicide rate as high as 6.6/10,000, while another systematic review of 28 studies reported a rate of suicide as 4.1/10,000. The suicide was usually committed between 18 months to 5 years postoperatively. Pre-existing psychiatric conditions, particularly long-term depression were the most plausible explanation for this finding.57 Acute mania has been reported by Nepal et al58 in 57 years old female 2 months after RYGB. Pre-surgical psychiatric evaluation before BS is recommended to monitor the at risk patients.53 Pre surgical counseling and psychoeducation should be planned for patients with suicide risk. Pharmacotherapy and psychotherapy should be implemented where indicated.59
Stroke and seizure
Stroke and seizure are not common after BS. A case of stroke and seizure 4 months post gastric bypass surgery had other risk factors for strokes and malnutrition and dehydration were the possible precipitant.60 This finding needs to be confirmed by further studies.
Central nervous system demyelination
Central nervous system demyelination resembling multiple sclerosis (MS) has been described after BS. A study from Brazil describing 26 patients with neurological complications identified CNS demyelination in five patients. MRI in four cases fulfilled diagnostic criteria for multiple sclerosis. However it was not well established that the findings were an effect of BS, or incidental co-existing multiple sclerosis.61 Monophasic CNS demyelination was reported in 2 and relapsing and remitting MS in 1 out of 15 patients with neurological complications after BS by Falah et al.62
Cognitive impairment and bariatric surgery
Higher midlife BMI has been identified as an independent risk factor for dementia such as Alzheimer’s disease and vascular dementia.63 Changes in cognitive abilities may begin in childhood. Blanco-Gomez et al64 reported greater deficit in inhibitory control in overweight and obese children compared with age-matched and gender-matched controls.64 BS has been shown to improve cognitive function rapidly after surgery and the effect lasts for years.65-67
Graff-Radford et al68 described a case series of 10 patients developing cognitive complaints following RYGB. The cognitive impairment was attributed to bilateral posterior thalamic focal brain atrophy detected on volumetric MRI.68 The findings need to be verified by further studies.
Spontaneous intracranial hypotension (SIH)
A case-control study has identified BS as a possible risk factor for spontaneous intracranial hypotension (SIH). In this study, 3.3% of the patients with SIH were found to have past history of BS compared with 0.8% of patients with un ruptured intracranial aneurysms. Effect of vitamin A and D deficiency on CSF absorption and possible spontaneous CSF leakage were the likely given explanation.69
Myelopathy/Myeloneuropathy
Posterolateral myelopathy is one of the common and potentially disabling CNS complications of BS. Myelopathy may be associated with peripheral neuropathy resulting in a picture of myeloneuropathy. Myelopathy involves mostly the posterior columns with dorsal root ganglia. The onset is usually several years after the surgery and clinical manifestations include loss of proprioception, vibration, gait ataxia, hyperreflexia and Babinski sign. Sphincter dysfunction and limb weakness may also be seen. Involvement of the peripheral nerves can give glove and stocking pattern of sensory change.30,32 The myelopathy is mostly attributed to vitamin B12 deficiency after gastric bypass surgery; however, copper deficiency is now another well-established cause of myelopathy.30,70
Optic neuropathy can be seen along with myeloneuropathy in copper deficiency. Folate deficiency is also a potential contributor and the clinical features are indistinguishable from vitamin B12 deficiency.32,71,72 Vitamin E (tocopherol) deficiency has also been identified as a cause of treatable myelopathy.73,74 Pyridoxine deficiency is another cause as described by Koffman et al.72 The treatment of these micronutrient deficiencies often result in improvement in clinical signs and symptoms. Initial parenteral replacement is followed by oral supplementation. Hematological parameters improve quickly and completely, however, the neurological recovery lags behind and may not be complete.32 Copper replacement can be done intravenously, followed by long term oral replacement. Serum copper levels should be periodically checked.32 Vitamin B12 is usually given intramuscularly.32 Diagnosis and treatment of these common complications are outlined in Table 3.
Optic neuropathy
Bariatric procedures associated with gastrointestinal malabsorption of vitamins and microelements may constitute a risk factor for nutritional optic neuropathy (NON). The NON results either from complete lack or insufficient dietary supply of nutrients needed for normal functioning of nerve fibers. Unilateral or bilateral optic neuropathy has been described after gastric bypass surgery associated with vitamin B12, copper, as well as vitamin A deficiency.30,75,76 A case of dermatitis and optic neuropathy due to zinc deficiency following BS has also been reported.77 The optic neuropathy can manifest slowly or acutely and can occur several years after BS. The pathogenesis is likely related to demyelination, however, the recovery may be incomplete and the blindness may be permanent.
In conclusions, With increasing obesity and increasing use of BS, it is likely that the neurologists and other healthcare professionals might encounter more neurological complications of these procedures in future. Patients, surgeons, internal medicine physicians, and neurologist need to be aware of these potential complications and should recognize that time to diagnosis and treatment matters. Early diagnosis and timely management may improve and possibly reverse the neurological deficit completely. Fortunately, many of these complications are potentially preventable. Lack of adherence to the postoperative nutritional replacement is still a significant issue. We strongly recommend the preoperative nutritional as well as psychological assessment of patients undergoing BS to prevent many of known complications. Appropriate screening, counselling and postoperative nutritional replacement should be the mainstay of management to avoid such catastrophic neurological complications. A routine multidisciplinary approach might help in reducing these complications as well. The review aims to raise awareness for the potentially permanent neurological complications and offers an overview of the most common CNS complications that can be encountered after BS. Neurological complications after endoscopic bariatric procedures, not described here separately need to be addressed as well and compared with other BS.
Acknowledgment
The authors gratefully acknowledge thank Dr. Fahd Sultan for his help in acquiring the original articles listed in the references.
Footnotes
References
- 1.Lee EB, Mattson MP. The neuropathology of obesity: insights from human disease. Acta Neuropathol. 2014;127:3–28. doi: 10.1007/s00401-013-1190-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:1–253. [PubMed] [Google Scholar]
- 3.Stevens GA, Singh GM, Lu Y, Danaei G, Lin JK, Finucane MM, et al. National, regional, and global trends in adult overweight and obesity prevalences. Popul Health Metr. 2012;10:22. doi: 10.1186/1478-7954-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Poirier P, Cornier MA, Mazzone T, Stiles S, Cummings S, Klein S, et al. Bariatric surgery and cardiovascular risk factors: a scientific statement from the American Heart Association. Circulation. 2011;123:1683–1701. doi: 10.1161/CIR.0b013e3182149099. [DOI] [PubMed] [Google Scholar]
- 5.Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet. 2011;377:557–567. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lavie CJ, Milani RV. Obesity and cardiovascular disease: the hippocrates paradox? J Am Coll Cardiol. 2003;42:677–679. doi: 10.1016/s0735-1097(03)00784-8. [DOI] [PubMed] [Google Scholar]
- 7.Lee EB. Obesity, leptin, and Alzheimer's disease. Ann N Y Acad Sci. 2011;1243:15–29. doi: 10.1111/j.1749-6632.2011.06274.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Debette S, Seshadri S, Beiser A, Au R, Himali JJ, Palumbo C, et al. Midlife vascular risk factor exposure accelerates structural brain aging and cognitive decline. Neurology. 2011;77:461–468. doi: 10.1212/WNL.0b013e318227b227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Doherty GH. Obesity and the ageing brain: could leptin play a role in neurodegeneration? Curr Gerontol Geriatr Res. 2011;2011:708154. doi: 10.1155/2011/708154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Obesity and overweight. Geneva (CH): 2017. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/ [Google Scholar]
- 11.Dubnov-Raz G, Berry EM. The dietary treatment of obesity. Med Clin North Am. 2011;95:939–952. doi: 10.1016/j.mcna.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 12.Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23:427–36. doi: 10.1007/s11695-012-0864-0. [DOI] [PubMed] [Google Scholar]
- 13.Espinet-Coll E, Nebreda-Durán J, Gómez-Valero JA, Muñoz-Navas M, Pujol-Gebelli J, Vila-Lolo C, et al. Current endoscopic techniques in the treatment of obesity. Rev Esp Enferm Dig. 2012;104:72–87. doi: 10.4321/s1130-01082012000200006. [DOI] [PubMed] [Google Scholar]
- 14.Park CW, Torquati A. Physiology of weight loss surgery. Surg Clin North Am. 2011;91:1149–1161. doi: 10.1016/j.suc.2011.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith BR, Schauer P, Nguyen NT. Surgical approaches to the treatment of obesity: bariatric surgery. Med Clin North Am. 2011;95:1009–1030. doi: 10.1016/j.mcna.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 16.Sjöström L, Peltonen M, Jacobson P, Sjöström CD, Karason K, Wedel H, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307:56–65. doi: 10.1001/jama.2011.1914. [DOI] [PubMed] [Google Scholar]
- 17.Sjöström L, Gummesson A, Sjöström CD, Narbro K, Peltonen M, Wedel H, et al. Swedish Obese Subjects Study. Effects of bariatric surgery on cancer incidence in obese patients in Sweden (Swedish Obese Subjects Study): a prospective, controlled intervention trial. Lancet Oncol. 2009;10:653–662. doi: 10.1016/S1470-2045(09)70159-7. [DOI] [PubMed] [Google Scholar]
- 18.Christou NV, Lieberman M, Sampalis F, Sampalis JS. Bariatric surgery reduces cancer risk in morbidly obese patients. Surg Obes Relat Dis. 2008;4:691–695. doi: 10.1016/j.soard.2008.08.025. [DOI] [PubMed] [Google Scholar]
- 19.Christou NV, Sampalis JS, Liberman M, Look D, Auger S, McLean AP, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 2004;240:416–423. doi: 10.1097/01.sla.0000137343.63376.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coblijn UK, Karres J, de Raaff CA, de Castro SM, Lagarde SM, van Tets WF, et al. Predicting postoperative complications after bariatric surgery: the Bariatric Surgery Index for Complications, BASIC. Surg Endosc. 2017;31:4438–4445. doi: 10.1007/s00464-017-5494-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Encinosa WE, Bernard DM, Du D, Steiner CA. Recent improvements in bariatric surgery outcomes. Med Care. 2009;47:531–535. doi: 10.1097/MLR.0b013e31819434c6. [DOI] [PubMed] [Google Scholar]
- 22.Buchwald H, Estok R, Fahrbach K, Banel D, Sledge I. Trends in mortality in bariatric surgery: a systematic review and meta-analysis. Surgery. 2007;142:621–632. doi: 10.1016/j.surg.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 23.Longitudinal Assessment of Bariatric Surgery (LABS) Consortium. Flum DR, Belle SH, King WC, Wahed AS, Berk P, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009;361:445–454. doi: 10.1056/NEJMoa0901836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith MD, Patterson E, Wahed AS, Belle SH, Berk PD, Courcoulas AP, et al. Thirty-day mortality after bariatric surgery: independently adjudicated causes of death in the longitudinal assessment of bariatric surgery. Obes Surg. 2011;21:1687–1692. doi: 10.1007/s11695-011-0497-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ziegler O, Sirveaux MA, Brunaud L, Reibel N, Quilliot D. Medical follow up after bariatric surgery: nutritional and drug issues. General recommendations for the prevention and treatment of nutritional deficiencies. Diabetes Metab. 2009;35:544–557. doi: 10.1016/S1262-3636(09)73464-0. [DOI] [PubMed] [Google Scholar]
- 26.Tack J, Deloose E. Complications of bariatric surgery: dumping syndrome, reflux and vitamin deficiencies. Best Pract Res Clin Gastroenterol. 2014;28:741–749. doi: 10.1016/j.bpg.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 27.Berger JR. The neurological complications of bariatric surgery. Arch Neurol. 2004;61:1185–1189. doi: 10.1001/archneur.61.8.1185. [DOI] [PubMed] [Google Scholar]
- 28.Alqahtani HA, Khan AS, Khan MA, Aldarmahi AA, Lodhi Y. Neurological complications of bariatric surgery. Neuroscience (Riyadh) 2016;21:241–245. doi: 10.17712/nsj.2016.3.20160039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tabbara M, Carandina S, Bossi M, Polliand C, Genser L, Barrat C. Rare neurological complications after sleeve gastrostomy. Obesity Surg. 2016;26:2843–2848. doi: 10.1007/s11695-016-2227-8. [DOI] [PubMed] [Google Scholar]
- 30.Juhasz-Pocsine K, Rudnicki SA, Archer RL, Harik SI. Neurologic complications of gastric bypass surgery for morbid obesity. Neurology. 2007;68:1843–1850. doi: 10.1212/01.wnl.0000262768.40174.33. [DOI] [PubMed] [Google Scholar]
- 31.Frantz DJ. Neurologic complications of bariatric surgery: involvement of central, peripheral, and enteric nervous systems. Curr Gastroenterol Rep. 2012;14:367–372. doi: 10.1007/s11894-012-0271-7. [DOI] [PubMed] [Google Scholar]
- 32.Kumar N. Neurologic complications of bariatric surgery. Continuum (Minneap Minn) 2014;20:580–597. doi: 10.1212/01.CON.0000450967.76452.f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kopelman MD. The Korsakoff syndrome. Br J Psychiatry. 1995;166:154–173. doi: 10.1192/bjp.166.2.154. [DOI] [PubMed] [Google Scholar]
- 34.Abarbanel JM, Berginer VM, Osimani A, Solomon H, Charuzi I. Neurologic complications after gastric restriction surgery for morbid obesity. Neurology. 1987;37:196–200. doi: 10.1212/wnl.37.2.196. [DOI] [PubMed] [Google Scholar]
- 35.Singh S, Kumar A. Wernicke encephalopathy after obesity surgery: a systematic review. Neurology. 2007;68:807–811. doi: 10.1212/01.wnl.0000256812.29648.86. [DOI] [PubMed] [Google Scholar]
- 36.Aasheim ET. Wernicke encephalopathy after bariatric surgery: a systematic review. Ann Surg. 2008;248:714–720. doi: 10.1097/SLA.0b013e3181884308. [DOI] [PubMed] [Google Scholar]
- 37.Stroh C, Meyer F, Manger T. Beriberi, a severe complication after metabolic surgery - review of the literature. Obes Facts. 2014;7:246–252. doi: 10.1159/000366012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kühn AL, Hertel F, Boulanger T, Diederich NJ. Vitamin B1 in the treatment of Wernicke's encephalopathy due to hyperemesis after gastroplasty. J Clin Neurosci. 2012;19:1303–1305. doi: 10.1016/j.jocn.2011.11.030. [DOI] [PubMed] [Google Scholar]
- 39.Traube M, Bock JL, Boyer JL. D-Lactic acidosis after jejunoileal bypass: identification of organic anions by nuclear magnetic resonance spectroscopy. Ann Intern Med. 1983;98:171–3. doi: 10.7326/0003-4819-98-2-171. [DOI] [PubMed] [Google Scholar]
- 40.Dahlquist NR, Perrault J, Callaway CW, Jones JD. D-Lactic acidosis and encephalopathy after jejunoileostomy: response to overfeeding and to fasting in humans. Mayo Clin Proc. 1984;59:141–145. doi: 10.1016/s0025-6196(12)60764-2. [DOI] [PubMed] [Google Scholar]
- 41.Thurn JR, Pierpont GL, Ludvigsen CW, Eckfeldt JH. D-lactate encephalopathy. Am J Med. 1985;79:717–721. doi: 10.1016/0002-9343(85)90522-4. [DOI] [PubMed] [Google Scholar]
- 42.Narula RK, El Shafei A, Ramaiah D, Schmitz PG. D-lactic acidosis 23 years after jejuno-ileal bypass. Am J Kidney Dis. 2000;36:E9. doi: 10.1053/ajkd.2000.9005. [DOI] [PubMed] [Google Scholar]
- 43.Fabian E, Kramer L, Siebert F, Högenauer C, Raggam RB, Wenzl H, et al. D-lactic acidosis - case report and review of the literature. Z Gastroenterol. 2017;55:75–82. doi: 10.1055/s-0042-117647. [DOI] [PubMed] [Google Scholar]
- 44.Naqarur A, Fenves AZ. Late presentation of fatal hyperammonemic encephalopathy after Roux-en-Y gastric bypass. Proc (Bayl Univ Med Cent) 2017;30:41–43. doi: 10.1080/08998280.2017.11929521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hu WT, Kantarci OH, Merritt JL, 2nd, McGrann P, Dyck PJ, Lucchinetti CF, et al. Ornithine transcarbamylase deficiency presenting as encephalopathy during adulthood following bariatric surgery. Arch Neurol. 2007;64:126–128. doi: 10.1001/archneur.64.1.126. [DOI] [PubMed] [Google Scholar]
- 46.Kromas ML, Mousa OY, John S. Hyperammonemia-induced encephalopathy: A rare devastating complication of bariatric surgery. World J Hepatol. 2015;7:1007–1111. doi: 10.4254/wjh.v7.i7.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Acharya G, Mehra S, Patel R, Frunza-Stefan S, Kaur H. Fatal Nonhepatic Hyperammonemia in ICU Setting: A Rare but Serious Complication following Bariatric Surgery. Case Rep Crit Care. 2016;2016:8531591. doi: 10.1155/2016/8531591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fenves AZ, Shchelochkov OA, Mehta A. Hyperammonemic syndrome after Roux-en-Y gastric bypass. Obesity (Silver Spring) 2015;23:746–749. doi: 10.1002/oby.21037. [DOI] [PubMed] [Google Scholar]
- 49.Estrella J, Yee G, Wilcken B, Tchan M, Talbot M. Hyperammonemic encephalopathy complicating bariatric surgery: a case study and review of the literature. Surg Obes Relat Dis. 2014;10:e35–e38. doi: 10.1016/j.soard.2013.10.020. [DOI] [PubMed] [Google Scholar]
- 50.Kalarchian MA, Marcus MD, Levine MD, Courcoulas AP, Pilkonis PA, Ringham RM, et al. Psychiatric disorders among bariatric surgery candidates: relationship to obesity and functional health status. Am J Psychiatry. 2007;164:328–334. doi: 10.1176/ajp.2007.164.2.328. [DOI] [PubMed] [Google Scholar]
- 51.Faulconbridge LF, Wadden TA, Thomas JG, Jones-Corneille LR, Sarwer DB, Fabricatore AN. Changes in depression and quality of life in obese individuals with binge eating disorder: bariatric surgery versus lifestyle modification. Surg Obes Relat Dis. 2013;9:790–796. doi: 10.1016/j.soard.2012.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Burgmer R, Legenbauer T, Müller A, de Zwaan M, Fischer C, Herpertz S. Psychological outcome 4 years after restrictive bariatric surgery. Obes Surg. 2014;24:1670–1678. doi: 10.1007/s11695-014-1226-x. [DOI] [PubMed] [Google Scholar]
- 53.Marcus MD, Kalarchian MA, Courcoulas AP. Psychiatric evaluation and follow-up of bariatric surgery patients. Am J Psychiatry. 2009;166:285–291. doi: 10.1176/appi.ajp.2008.08091327. [DOI] [PubMed] [Google Scholar]
- 54.de Zwaan M, Marschollek M, Allison KC. The Night Eating Syndrome (NES) in Bariatric Surgery Patients. Eur Eat Disord Rev. 2015;23:426–234. doi: 10.1002/erv.2405. [DOI] [PubMed] [Google Scholar]
- 55.King WC, Chen JY, Mitchell JE, Kalarchian MA, Steffen KJ, Engel SG, et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012;307:2516–2525. doi: 10.1001/jama.2012.6147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tindle HA, Omalu B, Courcoulas A, Marcus A, Hammers J, Kuller LH. Risk of suicide after long term follow up from bariatric surgery. Am J Med. 2010;123:1036–1042. doi: 10.1016/j.amjmed.2010.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Peterhänsel C, Petroff D, Klinitzke G, Kersting A, Wagner B. Risk of completed suicide after bariatric surgery: a systematic review. Obes Rev. 2013;14:369–382. doi: 10.1111/obr.12014. [DOI] [PubMed] [Google Scholar]
- 58.Nepal H, Bhattarai M, Agustin ET. New onset mania following bariatric surgery. Psychiatry Investig. 2015;12:152–154. doi: 10.4306/pi.2015.12.1.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yen YC, Huang CK, Tai CM. Psychiatric aspects of bariatric surgery. Curr Opin Psychiatry. 2014;27:374–379. doi: 10.1097/YCO.0000000000000085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Choi JY, Scarborough TK. Stroke and seizure following a recent laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2004;14:857–860. doi: 10.1381/0960892041590890. [DOI] [PubMed] [Google Scholar]
- 61.Fragoso YD, Alves-Leon SV, Anacleto Ade C, Brooks JB, Gama PD, Gomes S, et al. Neurological complications following bariatric surgery. Arq Neuropsiquiatr. 2012;70:700–703. doi: 10.1590/s0004-282x2012000900010. [DOI] [PubMed] [Google Scholar]
- 62.Falah M, Al-Ghawi E, Adnan R, Al-Sarawi A, Al-Harbi T. Neurological complications of bariatric surgery: A review of 15 patients (P3.380) Neurology. 2016;86:380. [Google Scholar]
- 63.Anstey KJ, Cherbuin N, Budge M, Young J. Body mass index in midlife and late-life as a risk factor for dementia: a meta-analysis of prospective studies. Obes Rev. 2011;12:e426–e437. doi: 10.1111/j.1467-789X.2010.00825.x. [DOI] [PubMed] [Google Scholar]
- 64.Blanco-Gómez A, Ferré N, Luque V, Cardona M, Gispert-Llauradó M, Escribano J, et al. Being overweight or obese is associated with inhibition control in children from six to ten years of age. Acta Paediatr. 2015;104:619–625. doi: 10.1111/apa.12976. [DOI] [PubMed] [Google Scholar]
- 65.Alosco ML, Galioto R, Spitznagel MB, Strain G, Devlin M, Cohen R, et al. Cognitive function after bariatric surgery: evidence for improvement 3 years after surgery. Am J Surg. 2014;207:870–876. doi: 10.1016/j.amjsurg.2013.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Miller LA, Crosby RD, Galioto R, Strain G, Devlin MJ, Wing R, et al. Bariatric surgery patients exhibit improved memory function 12 months postoperatively. Obes Surg. 2013;23:1527–1535. doi: 10.1007/s11695-013-0970-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Spitznagel MB, Hawkins M, Alosco M, Galioto R, Garcia S, Miller L, et al. Neurocognitive Effects of Obesity and Bariatric Surgery. Eur Eat Disord Rev. 2015;23:488–495. doi: 10.1002/erv.2393. [DOI] [PubMed] [Google Scholar]
- 68.Graff-Radford J, Whitwell JL, Trenerry MR, Ahlskog JE, Jensen MD, Jack CR, Jr, et al. Focal brain atrophy in gastric bypass patients with cognitive complaints. J Clin Neurosci. 2011;18:1671–1676. doi: 10.1016/j.jocn.2011.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Schievink WI, Goseland A, Cunneen S. Bariatric surgery as a possible risk factor for spontaneous intracranial hypotension. Neurology. 2014;83:1819–1822. doi: 10.1212/WNL.0000000000000985. [DOI] [PubMed] [Google Scholar]
- 70.Kumar N, Ahlskog JE, Gross JB., Jr Acquired hypocupremia after gastric surgery. Clin Gastroenterol Hepatol. 2004;2:1074–1079. doi: 10.1016/s1542-3565(04)00546-4. [DOI] [PubMed] [Google Scholar]
- 71.Kazemi A, Frazier T, Cave M. Micronutrient-related neurologic complications following bariatric surgery. Curr Gastroenterol Rep. 2010;12:288–295. doi: 10.1007/s11894-010-0120-5. [DOI] [PubMed] [Google Scholar]
- 72.Koffman BM, Greenfield LJ, Ali II, Pirzada NA. Neurologic complications after surgery for obesity. Muscle Nerve. 2006;33:166–176. doi: 10.1002/mus.20394. [DOI] [PubMed] [Google Scholar]
- 73.Becker DA, Bacler LJ, Galetta SL. The Neurological Complications of Nutritional Deficiency following Bariatric Surgery. J Obes. 2012;2012:608534. doi: 10.1155/2012/608534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Martana MR, Davis WE. Vitamin deficiency after gastric bypass surgery: a review. South Med J. 2009;102:1025–1031. doi: 10.1097/SMJ.0b013e3181b62614. [DOI] [PubMed] [Google Scholar]
- 75.Naismith RT, Shepherd JB, Weihl CC, Tutlam NT, Cross AH. Acute and bilateral blindness due to optic neuropathy associated with copper deficiency. Arch Neurol. 2009;66:1025–1027. doi: 10.1001/archneurol.2009.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fok JS, Li JY, Yong TY. Visual deterioration caused by vitamin A deficiency in patients after bariatric surgery. Eat Weight Disord. 2012;17:e144–e146. doi: 10.1007/BF03325340. [DOI] [PubMed] [Google Scholar]
- 77.Ramos-Leví AM, Sánchez-Pernaute A, Rubio Herrera MA. Dermatitis and optic neuropathy due to zinc deficiency after malabsortive bariatric surgery. Nutr Hosp. 2013;28:1345–1347. doi: 10.3305/nh.2013.28.4.6606. [DOI] [PubMed] [Google Scholar]
- 78.Neff KJ, Olbers T, Le Roux CW. Bariatric surgery: the challenges with candidate selection, individualizing treatment and clinical outcomes. BMC Med. 2013;11:8. doi: 10.1186/1741-7015-11-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


