Abstract
Objectives:
To review the demographic and pathological pattern of neuro-epithelial brain tumors in a tertiary referral center in the Eastern Province of Saudi Arabia and to compare the results of our study with other national and international studies.
Methods:
This is a retrospective chart-review study of all patients with neuro-epithelial brain tumors referred and treated in our center between January 2010 and January 2015. The age, gender, tumor location, and histopathology were recorded.
Results:
The total number of cases was 149 including 96 adult cases and 53 pediatric cases. 58% of cases were male, and 42% were female. The age group distribution showed 2 peaks; one in the first 5 years of life and the second was in the age range from 26-45 years old. Glioblastoma multiforme was the most common pathological type (32%), followed by medulloblastoma (13.3%). This study showed similar results to a previous study conducted in the Eastern Province in terms of age and gender distribution, but pathologically, the tumors diagnosed in our study were generally of a higher grading. When comparing our results to other international studies in nearby countries (Jordan and Egypt), we found similarities in pathological patterns and age distribution. However, when comparing our results to a western country (USA), we found considerable differences in the age group distribution.
Conclusion:
Neuro-epithelial brain tumors in Saudi Arabia affect younger population according to our study compared to Western countries. These findings are similar to other studies from Middle Eastern countries. In addition, our study showed a significant increase in high grade gliomas in the Eastern Province compared to an old historical study. This increase should be interpreted cautiously due to possible selection errors, changes in pathological grading, and expertise.
The term “primary brain tumors” refers to a mixed group of neoplasms arising from different intracranial tissues with degrees of malignancy ranging from slow growing to aggressive types. Each type has its own biology, treatment, and prognosis. These tumors are unique and different in their behavior and even “benign” tumors can be catastrophic due to their location, their ability to infiltrate locally, and the potential to transform into malignancy.1 Primary central nervous system (CNS) tumors are divided into the following major groupings: tumors of neuro-epithelial tissue (including gliomas, medulloblastoma, and others), tumors of meninges (including meningiomas), germ cell tumors, tumors of nerve sheath (like vestibular schwannomas), and tumors arising from the seller region (including pituitary adenomas).2 The World Health Organization (WHO) classification for CNS tumors, developed in 1979 and revised in 1999, 2007, and 2016 has been universally adopted in grouping CNS tumors according to their behavior and aggressiveness.3,4 Primary CNS tumors are a rare occurrence accounting for only 2 % of all cancers in adults, but account for approximately 20% of cancers in children.5 Neuro-epithelial brain tumors accounts for almost 80-90% of primary brain malignancies and their occurrence and pathological patterns are used worldwide to analyze the incidence and epidemiology of primary brain cancer in different countries.6 The aim of our study is to review the demographic and pathological pattern of neuro-epithelial brain tumors in our center which is a tertiary referral center for the whole of the Eastern Province and compare our results with other national and international studies.
Methods
King Fahad specialist hospital in Dammam has accommodated the Oncology Center for the whole of Eastern province since 2007. The neuro-oncology multidisciplinary tumor board (MDT) was established in 2009 to review and discuss all neuro-oncological cases referred or treated in our hospital. All cases of primary brain tumors including adult and pediatric are discussed in the meeting for future management. The list of cases discussed in the MDT is saved in a spreadsheet for quality assurance and for future research.
We retrospectively reviewed all cases of neuro-epithelial tumors from our neuro-oncology MDT list between January 2010 and January 2015 (5 years). The IRB approval was obtained for this study. Age, gender, tumor location, imaging and histopathology diagnosis were recorded for our analysis. For grading and pathological diagnosis, we used the 2007 edition of WHO classification for CNS tumors.3
Inclusion and exclusion criteria
The study included all cases of neuro-epithelial tumor with pathological confirmation. We also included certain neuro-epithelial tumors, which can be diagnosed based on radiology diagnosis such as diffuse intrinsic brain stem glioma and optic pathway glioma. All other CNS tumors like metastasis, meningiomas, and lymphomas were excluded.
Statistical analysis
Statistical analysis was performed by using the Statistical Package for Social Science version 12 (SSPS Inc., Chicago, IL, USA). The percentage was calculated in the presence and absence group by pearson’s Chi-square test. The limit of the statistical significance was set at p<0.05.
Results
The total number of cases was 149. Pathological diagnosis was available for 140 patients, and the other 9 cases were treated on the basis of their imaging (cases of diffuse brain stem gliomas and optic pathway gliomas). The percentage of male and female in our study were: 58% male versus 42% female. The percentage of adult and pediatric cases (16 years and below) were: 64.4% adult and 35.6% pediatric. Figure 1 shows the age grouping in percentage for all cases. We have 2 peaks; one in the first 5 years of life and second in the age group (26-45 years). The locations of the tumors were 69% supra-tentorial versus 31% infra-tentorial.
Figure 1.
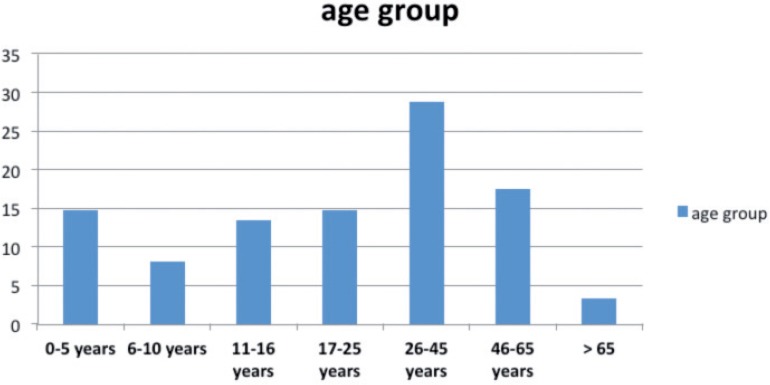
Shows the age grouping in percentage for all cases of the study.
The pathological types for all of our cases are summarized in Table 1. As shown from the table: Glioblastoma Multiform (WHO IV) cases were the highest (32%), Primitive Neuroectodermal tumors (PNET)/ Medulloblastoma (WHO IV) were (12.3%), Pilocytic Astrocytoma (WHO I) 9.3%, Anaplastic Astrocytoma (WHO III) 8.7%, Oligodendroglioma (WHO II, III) 8.6%, Ependymoma (WHO II, III) 7.3%, Diffuse brain stem glioma 6%, Diffuse Astrocytoma (WHO II) 4.6%, and the remaining were less than 3 % each.
Table 1.
Pathological types for all cases of the study.
| Histology type | KFSH-D | (%) |
|---|---|---|
| Pilocytic Astrocytoma (WHO 1) (infra-tentorial) | 11 | (7.3) |
| Pilocytic Astrocytoma (WHO 1) (Optic pathway glioma) | 3 | (2) |
| Diffuse Astrocytoma (WHO 11) | 7 | (4.6) |
| Anaplastic Astrocytoma (WHO 111) | 13 | (8.7) |
| Oligodendroglioma (WHO 11) | 4 | (2.7) |
| Anaplastic oligodendrioglioma (WHO 111) | 9 | (6) |
| Mixed glioma (WHO 11) | 2 | (1.3) |
| Mixed glioma (WHO111) | 2 | (1.3) |
| Diffuse brain stem glioma | 9 | (6) |
| GBM (WHO 1V) | 48 | (32) |
| Gliosarcoma (WHO 1V) | 2 | (1.3) |
| Ependymoma (WHO 11 and WHO 111) | 11 | (7.3) |
| PNET/MB (WHO 1V) (Infra-tentorial) | 16 | (10.7) |
| PNET (WHO 1V) (supra-tentorial) | 2 | (1.3) |
| Pineoblastoma l tumors (WHO 1V) | 2 | (1.3) |
| Choroid plexus papilloma/ carcinoma | 3 | (2) |
| PXA (WHO 11 and 111) | 3 | (2) |
| Central Neurocytoma (WHO 11) | 2 | (1.3) |
| Total | 149 | (100) |
GBM - Glioblastoma multiforme, PNET - Primitive Neuroectrodermal Tumor, MB - Medulloblastoma, PXA-Pleomorphic Xanthoastrocytoma
We have 53 cases of pediatric tumors. The PNET including Medulloblastoma were the highest among children 28.3%, High grade gliomas were 15%, pilocytic astrocytoma including the optic pathway gliomas were 16.8%, ependymoma 15%, and diffuse brain stem gliomas were 11.3%, and the remaining were less than 5%.
In the adult group: GBM was the highest 43.7%, followed by anaplastic astrocytoma 9.3%, oligodendroglioma 9.3%, PNET 6.2%, pilocytic astrocytoma 5.2 %, diffuse astrocytoma was 5.2 % and mixed gliomas 5.2%.
Discussion
The incidence of brain cancer in Saudi Arabia is relatively low according to the Saudi Cancer Registry (cancer incidence report 2010).7 Brain cancer forms 3.2% of all cancer in males in Saudi Arabia, and 2% in females. The age standardized incidence rate per 100,000 populations was 1.9 in males and 1.4 in females according to the same report.7 This incidence rate is considered the lowest in comparison to other countries (Figure 2).8
Figure 2.
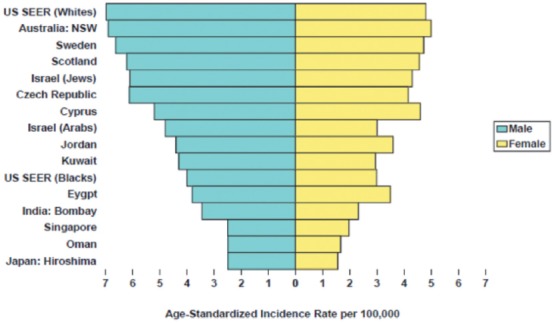
Shows the incidence of brain cancer in different countries.8
The pathological patterns of brain cancer were not published in the Saudi cancer registry since it constitutes a small percentage of all cancer cases.7 In addition, only cases with pathological confirmations of high-grade nature were included in the registry. Therefore, some brain tumors such as low-grade glioma, diffuse brain stem gliomas, and optic pathways gliomas which are diagnosed and treated based on brain imaging only, were not included in the cancer registry. Some of these tumors are considered aggressive and they are treated with chemotherapy and radiation therapy.9,10
Comparison to national studies
We have found few studies in the literature that have reported the pathological patterns of brain tumors in Saudi Arabia. Most of them were small, and they reported all types of brain tumors including meningioma, pituitary adenomas, brain metastasis…etc. The percentage of neuro-epithelial brain tumors in these studies were quite small to make any statistical comparisons11-13
One study from King Fahad University Hospital (KFUH) -Al-Khobar in the Eastern province of Saudi Arabia had a larger sample with a sizable percentage of neuro-epithelial brain tumors. The study included all CNS tumors according to the WHO classifications (1979 edition).14 The authors retrospectively reviewed all CNS tumor cases treated in all Eastern Province hospitals between January 1982 and January 1991 (9 years). A total of 142 cases of neuro-epithelial tumors were reported (Table 2). When comparing their results to our study, we found similarities in the gender and age group distributions; male 61.5%, female 38.5%, adult 58% and pediatrics 42% (in KFUH study). On the other hand, when comparing the pathological patterns between both studies, there were significant differences. We found increase in high-grade gliomas cases in our study (81 cases) compared to KFUH study 49 cases). This difference is significant (p<0.05). similarly, when comparing all cases of low grade gliomas in both studies (28 cases in our study versus 51 cases in KFUH study) the difference is also significant. The differences of other types of neuro-epithelial tumors are not significant.
Table 2.
Shows the pathological types of the KFUH study.14
| Low grade glioma (pilocytic WHO 1) and(diffuse astrocytoma (WHO 11) | 40 | (28) |
|---|---|---|
| Anaplastic Astrocytoma (WHO 111) | 18 | (12.5) |
| Oligodendroglioma (WHO 11) | 8 | (6) |
| Anaplastic oligodendrioglioma | 1 | (0.7) |
| Mixed glioma (WHO 11) | 3 | (2.1) |
| GBM (WHO 1V) | 30 | (21) |
| Ependymoma (WHO 1 and 11) | 7 | (4.9) |
| PNET (WHO 1V) | 28 | (19.5) |
| Choroid plexus papilloma/ carcinoma | 4 | (2.8) |
| Pineal tumors | 3 | (1) |
| Total | 142 | (100) |
GBM - Glioblastoma multiforme, PNET - Primitive Neuroectrodermal Tumor, MB - Medulloblastoma
The increase in high grade gliomas in our study in comparison to the KFUH study should be cautiously interpreted. It could be attributed to a selection bias since the historical (KFUH) study included cases from 4 major hospitals in the region while our study included only cases treated in or referred to our center for adjuvant therapy (chemotherapy or radiotherapy). The differences in pathological grading and expertise between the 2 studies might also affect the results of the pathological diagnosis.3 In addition, environmental factors could also be considered. In our view, more collaborative and prospective studies are needed to investigate these results further.
Comparison to international studies
The Middle East Cancer Consortium (MECC) previously published a large report on the incidence of cancers and their pathological patterns in several Middle Eastern countries.8 It also reported the incidence and pathologies of these tumors in the United State for comparison purposes. The report covered the period between 1996 and 2001. We compared our results to 2 Middle Eastern countries (Egypt and Jordan) in addition to the US results. We found no major differences in the pathological patterns of neuro-epithelial brain tumors between our results and the results of the three counties (Figure 3).
Figure 3.
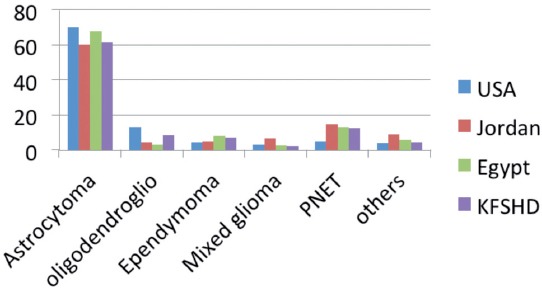
Shows the pathological patterns in 3 countries (Egypt, Jordan, and USA) and the in our study.8
When comparing the age group between our study and the MECC report, we found that neuro-epithelial tumors in our study are more common in younger patients (41.6% in patients below 20 years and 39.5% in patients between 20 and 49 years) and less common in older patients (16.1% between 50 and 69 years and only 2.6% above 70). Similar results were observed in the other 2 Middle Eastern countries. However, when compared to the USA study, the age groups affected by brain cancer in the US study were older, only 14% below 20 years, 28% (20-49 years) 31% (50-69 years) and 27% above 70 (Figure 4). This difference is more often linked to the differences in population age structure, rather than underlying incidence rates.7,8
Figure 4.
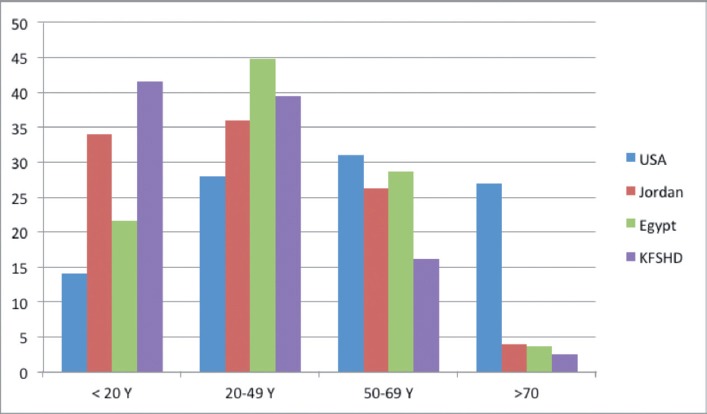
Shows the age distribution in the Middle East Cancer Consortium study in comparison to our study.8
Despite the small size of our sample, our results provide useful information on the pathological and the demographic patterns of neuro-epithelial primary brain tumors in the Eastern Province region and possibly in the whole of Saudi Arabia.
Acknowledgment
We would like to thank Mrs. Nada Alfarhan for her kind help in the English editing of this paper.
Footnotes
References
- 1.Mckinney PA. Brain tumours: incidence, survival, and aetiology. J Neurol Neurosurg Psychiatry. 2004;75:ii12–ii17. doi: 10.1136/jnnp.2004.040741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DeAngelis LM. Brain tumors. N Engl J Med. 2001;344:114–23. doi: 10.1056/NEJM200101113440207. [DOI] [PubMed] [Google Scholar]
- 3.Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114:97–109. doi: 10.1007/s00401-007-0243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016;131:803–820. doi: 10.1007/s00401-016-1545-1. [DOI] [PubMed] [Google Scholar]
- 5.Fisher JL, Schwartzbaum JA, Wrensch M, Wiemels JL. Epidemiology of brain tumors. Neurol Clin. 2007;25:867–890. doi: 10.1016/j.ncl.2007.07.002. vii. [DOI] [PubMed] [Google Scholar]
- 6.Landis SH, Murray T, Bolden S, Wingo PA. Cancer statistics 1999. CA Cancer J Clin. 1999;49:8–31. doi: 10.3322/canjclin.49.1.8. [DOI] [PubMed] [Google Scholar]
- 7.Saudi Cancer Registry. Cancer Incidence Report Saudi Arabia 2010. Kingdom of Saudi Arabia: Council of Health Services. 2014. Apr, Available from: www.chs.gov.sa/Ar/mediacenter/NewsLetter/2010%20Report%20(1).pdf .
- 8.Freedman LS, Edwards BK, Ries LAG, Young JL. Cancer Incidence in Four Member Countries (Cyprus, Egypt, Israel, and Jordan) of the Middle East Cancer Consortium (MECC) Compared with US SEER. Bethesda (MD): National Cancer Institute; Available from: www.seer.cancer.gov/archive/publications/mecc/mecc_monograph.pdf . [Google Scholar]
- 9.Hargrave D, Bartlets U, Bouffet E. Diffuse brainstem glioma in children: critical review of clinical trials. Lancet Oncol. 2006;7:241–248. doi: 10.1016/S1470-2045(06)70615-5. [DOI] [PubMed] [Google Scholar]
- 10.Jahrans C, Tarbell N. Optic pathway gliomas. Pediatr Blood Cancer. 2006;46:586–596. doi: 10.1002/pbc.20655. [DOI] [PubMed] [Google Scholar]
- 11.Jamjoom Z. Pattern of intracranial space-occupying lesions: the experience of King Khalid University Hospital. Ann Saudi Med. 1989:3–10. [Google Scholar]
- 12.Bangash M. Incidence of brain tumors at an academic centre in western Saudi Arabia. East African Medical Journal. 2012;88:138–142. [Google Scholar]
- 13.Ibrahim AW. C.N.S. tumors in eastern Saudi Arabia. Neurosurg Rev. 1992;15:295–302. doi: 10.1007/BF00257809. [DOI] [PubMed] [Google Scholar]
- 14.Al-Luwim I. Clinical and Epidemiological Study of CNS Tumours in the Eastern Province of Saudi Arabia. Pan Arab Journal of Neurosurgery. 1999:12–21. [Google Scholar]


