Abstract
Health literacy is a key factor in health outcomes that should be considered when creating mobile health promotion apps. In this paper, we detail our work over the past 10 years in developing the theory and practice of targeting the content of mobile apps at a level appropriate for the intended audience. We include a review of our theory of health literacy as expertise, the ASK model, and integrate it with the Theory of Planned Behavior. We then provide data that support both the model and its use. More recently, we have developed a predictive analytic model that uses demographic information and patient performance on a 10-item screening measure to determine patient level of health literacy at a high level of accuracy. The predictive model will enable apps to automatically provide content to users at an appropriate level of health literacy. This strategy, along with other aspects of tailoring, will allow apps to be more personally relevant to users, enhancing their effects in promoting health behavior change.
Introduction
Patients today face the twin challenges of dealing with a healthcare system that is increasingly complex, while at the same time working with providers who have less and less time for patient education and support (Bo, Friis, Osborne, & Maindal, 2014; Bodenheimer, Lorig, Holman, & Grumbach, 2002). They must therefore take more responsibility for their healthcare while receiving less help with that task. Health literacy, defined as an individuals’ ability to acquire, understand, and use the information needed to make health-related decisions (Promotion., 2012), is an especially important factor in patients’ ability to manage their interactions with the healthcare system. Individuals with high levels of health literacy are often better able to find health-related information, understand it, and act on it, than are persons with lower levels of health literacy (Bo et al., 2014). The complexity of the healthcare system and the knowledge needed to understand and manage disease treatment may be an especially acute problem for persons with low levels of health literacy. Studies have shown, for example, that many patients lack the fundamental skills needed to understand basic tasks such as scheduling appointments, taking medications, and monitoring their health (Berkman, Sheridan, Donahue, Halpern, & Crotty, 2011). Studies have shown that health literacy is factor in health status and treatment outcomes (Berkman et al., 2004; Berkman et al., 2011; D.A. Dewalt, Berkman, Sheridan, Lohr, & Pignone, 2004; Sheridan et al., 2011). Low levels of health literacy are associated with poor blood glucose control in patients with diabetes (Schillinger et al., 2002), lower likelihood of participating in cancer screening (Oldach & Katz, 2014), and increased healthcare utilization including more hospitalizations and emergency department visits (Baker et al., 2004; Parker, Ratzan, & Lurie, 2003). The importance of health literacy for health is underscored by studies that show that it is related to risk for mortality (Baker et al., 2007; Sudore et al., 2006; Wu et al., 2013).
Patients want and need information to maintain and improve their health. An enormous amount of information is available to them from providers, health care organizations, governments, and advertisers, but this availability itself creates challenges for individuals with low health literacy (Diviani, van den Putte, Giani, & van Weert, 2015). These more than simply finding relevant information but also evaluating its quality and usefulness. An even larger challenge for many patients is the difficulty of understanding and using health information even when they find it.
When patients succeed in finding the information they want and need, they often encounter a problem created by a discrepancy between the reading difficulty of the information and their own ability to understand and use it. Researchers and policy makers have called for written health information delivery to match patients’ reading abilities, but even well-written presentations targeting consumers are often written at levels beyond the capacity of patients to read easily (Ownby, 2006). Some have argued for a “universal precautions” approach to health literacy, with all information provided to patients at an easy to read level, usually defined as a 5th or 6th grade reading level (D. A. DeWalt et al., 2011). This one size fits all approach can improve but not eliminate the problem, as material at this level is still too difficult for many patients while being unacceptably simple for those with higher reading levels. In this paper, we argue that patients with difficulties acquiring information from written text will benefit from multimedia support in the form of audio narration and illustrative graphic elements. Those who are skilled in text processing can most efficiently be helped by providing information about health conditions and treatment as well as support for improving their skills in managing those conditions.
In this paper we present an approach to the problem of getting usable health information to the people that need it that is scalable and easily integrated into electronic patient portals. It is a group of instructional strategies and multimedia techniques that we developed over the course of several studies of health literacy and patient behavior (Ownby, 2005; Ownby, Acevedo, Waldrop-Valverde, Jacobs, Homs, et al., 2013; Ownby, Hertzog, & Czaja, 2012; Ownby, Waldrop-Valverde, Caballero, & Jacobs, 2012). Our approach is also informed by cognitive load theory (Paas, Renkl, & Sweller, 2004; Sweller, 1988), especially because this approach to instruction emphasizes the importance of working memory, an ability that is often reduced in persons with chronic illness. Our interventions have also been designed to be consistent with findings from research on multimedia instructional strategies (R.E. Mayer, 2009; R. E. Mayer & Moreno, 2003)
In our studies, we have shown that a brief assessment of functional health literacy using a 10-item multiple choice test (Ownby, 2015) combined with demographic information can quickly and efficiently identify patients likely to require substantial support for information presentation in the form of audio and graphic formats (Ownby, Acevedo, & Waldrop-Valverde, 2019). In our current study, we are testing the hypothesis that persons with high levels of health literacy can be most efficiently helped by providing information and teaching skills in a text-based format. Conversely, we are also testing whether those with low levels of health literacy can be most effectively helped by providing information with text at a low level of reading difficulty while being supported by graphics and audio narration (Ownby et al., 2017).
We refer to providing health information to patients in this fashion as precision health information.™ Here we borrow from a current trend in medicine, the idea that precise characterization of patients’ (especially with respect to genetic makeup and its relation to treatment response) can be used to tailor treatments so as to increase their efficacy while keeping adverse effects to a minimum (Jameson & Longo, 2015). In the context of promoting patient health literacy, we define precision health information as giving patients the information they need, when they need it, in a form they can use.
Relevance
Distance learning practitioners may be interested in health literacy because of its relevance to online health education. The proliferation of patient information websites over the past several decades has made distance self-education for health widespread (Project, 2013). The importance of patient information and patient education has been underlined in continuing efforts by the federal government to promote standards for electronic health records (“Patient Protection and Affordable Care Act,” 2010). Although electronic health records are most often thought of repositories for health information such as physician visits and laboratory results, most include a patient portal. Patient portals commonly provide patients access to their records, but can readily include links to relevant online resources, including patient education materials. It is thus a method by which providers can give patients an “information prescription” (Burke, Carey, Haines, Lampson, & Pond, 2010) to learn more about their condition and how to manage it.
The move to providing information resources within the patient portals that are part of most large electronic health record systems has been spurred by mandates in the Affordable Care Act (also known as the law that established Obamacare). When providers (doctors, healthcare organizations) fulfill criteria for the meaningful use of electronic health records, they receive financial incentives for federal reimbursements for healthcare services. Providers can fulfill these criteria by demonstrating that they use the electronic record in several ways, and providing individualized patient education through the record is one of the ways in which organizations can satisfy the requirements of this standard (Snyder & Oliver, 2014).
The implementation of patient education via distance methods is thus a logical strategy for those who provide health education interventions since they can reach those who need them at times and locations that are convenient for the learner. Perhaps equally important, distance health education interventions, depending on their format, may make small demands on providers’ time depending on their degree of automation. Further, once materials are developed and deployed, they can be maintained and revised at low cost, as we have shown in a cost effectiveness study (Ownby, Waldrop-Valverde, Jacobs, Acevedo, & Caballero, 2013).
Computer-delivered health literacy interventions and health disparities
An important observation has been the finding that members of minority groups and the elderly are more likely to have low levels of health literacy (White, 2008). A frequent observation is that health status and outcomes are disparately negative for minorities and economically disadvantaged individuals compared to majority status individuals in a pattern similar to that seen for low levels of health literacy. This has led to the argument that the differences in health literacy for these groups may be an important factor in health disparities (Osborn et al., 2011; Osborn, Paasche-Orlow, Davis, & Wolf, 2007; Paasche-Orlow & Wolf, 2010). Addressing group differences in health literacy may thus be an important part of current efforts to reduce health disparities. A logical question, though, is how to provide large number of individuals, often in difficult to reach situations (economically disadvantaged or rural areas) interventions that can improve their health literacy.
The answer may be electronic interventions delivered over the Internet. Health information provided in an on-demand format might take several forms. These range from the simple provision of a video of a provider giving information to well-developed multimedia applications that may include text, audio, and motion graphics as well as video. Decisions on formats of interventions will depend on available resources including money for the costs of production as well as staff availability and planned target audience.
This is a strategy that will allow interventions to reach a large audience, especially if an intervention is developed with access on a smart phone in mind. Even with limitations to cell phone and broadband access, many individuals in economically disadvantaged groups and those in rural area now access the Internet on a regular basis for health care information (Project, 2013). Although it is often believed that older adults and the economically disadvantaged are less likely to be technology users, current evidence shows that the proportion of minority and low socioeconomic status (SES) persons in the US who have access to cellular telephones, and increasingly smart phones, is similar to the rest of the population (Center, 2018). In fact, for many members of minority groups cellular telephone service is often their primary mode for accessing the Internet for web browsing and e-mail (Fox & Duggan, 2012). Given the many challenges members of minorities face in accessing affordable healthcare and their disadvantage with respect to understanding the healthcare system compared to better-educated individuals, making healthcare information more widely available on the Internet via mobile apps may be an important strategy for addressing health disparities (Jerant, Sohler, Fiscella, Franks, & Franks, 2011; Paskett et al., 2016).
Currently a large number of mobile apps for health-related conditions (Donker et al., 2013; Payne, Lister, West, & Bernhardt, 2015). Examples include an app created at the Stanford University focused on sleep problems (Kuhn et al., 2016). The focus of other apps included diabetes, hypertension, pain, and depression (Donker et al., 2013; Hou et al., 2018; Kang & Park, 2016; Thurnheer, Gravestock, Pichierri, Steurer, & Burgstaller, 2018). The content of apps usually includes condition-related information, skill building directions, and the ability to self-monitor over time to allow individual assessment of progress. Some apps allow automated tracking of health-related behavior such as diet and physical activity (Flores Mateo, Granado-Font, Ferré-Grau, & Montaña-Carreras, 2015; Middelweerd, Mollee, van der Wal, Brug, & te Velde, 2014). Finally, a focus of development is the integration of self-monitoring with electronic health records so that providers will be able to monitor patients’ daily status on variables critical to disease management, such as blood pressure in hypertension and blood glucose levels in diabetes.
Health literacy and health education
A close examination of health education and health literacy interventions suggests that in many respects they are similar. While some have argued that the two areas are distinct, we think both can readily be defining health education as a means and health literacy as an end: simply put, health education is the means by which individuals develop and improve their health literacy. As explained more fully below, in our projects on health literacy interventions we believed it would be important to develop a model of health literacy that would allow us to operationalize its measurement and provide a framework for intervention development (Ownby, Acevedo, Waldrop-Valverde, Jacobs, & Caballero, 2014). As part of one project, we developed a new and potentially more useful measure of health literacy (Ownby, 2015; Ownby, Acevedo, Jacobs, Caballero, & Waldrop-Valverde, 2014; Ownby, Acevedo, Waldrop-Valverde, Jacobs, Homs, et al., 2013).
Development of a new measure of health literacy
In a project to create a new computer-delivered measure of health literacy, we developed more than 200 items assessing conceptual knowledge as well as its application in health-related tasks (Ownby, Acevedo, Waldrop-Valverde, Jacobs, Homs, et al., 2013). Questions included a broad range of topics from knowing how to take medications through exercise, diet, and preventive health. Questions were first pilot tested, rewritten when indicated, and assessed for difficulty and differential item functioning (Teresi, 2006). Items were then created in Spanish after further testing, with a final group of 98 items administered to 247 English-and 252 Spanish-speaking adults aged 18 to 93 years.
In order to validate the new measure simultaneously with administering the new measure our participants completed several widely-used measures of health literacy, including the Test of Functional Health Literacy in Adults, or TOFHLA (Parker, Baker, Williams, & Nurss, 1995), the Rapid Estimate of Adult Literacy in Medicine, or REALM for English speakers (Murphy, Davis, Long, Jackson, & Decker, 1993) or the Short Assessment of Health Literacy in Spanish-speaking Adults, or SAHLSA for Spanish speakers (Lee, Bender, Ruiz, & Cho, 2006). In addition, we asked participants to complete an extensive set of questionnaires asking about their health-related quality of life, nature and types of health conditions, their symptoms, mood, sleep, and physical and mental activity. Greater detail on the development and validation process is provided in a series of papers (Ownby, Acevedo, Jacobs, et al., 2014; Ownby, Acevedo, Waldrop-Valverde, et al., 2014; Ownby, Acevedo, Waldrop-Valverde, Jacobs, Homs, et al., 2013). These studies showed that the new measure was robustly related to existing measures of health literacy as well as significantly related to measures of quality of life, mood, health status, and healthcare utilization. As a part of the project, we also developed a framework for understanding the constituents of health literacy, since health literacy is often discussed as a multifactorial concept. This model and its application to health literacy interventions is the subject of the next section.
The ASK Model
A problem for the field of health literacy has been the lack of an operational model of health literacy that would inform a clear measurement strategy as well as clear targets for interventions. We approached creating an operational model of health literacy as an empirical rather than conceptual task, one that could be accomplished by examining relations among health-related behaviors and key individual-level variables hypothesized to be part of many definitions of health literacy. In this effort, we drew heavily on reviews by Sorenson et al (2012) and the theoretical work of Baker (2006) and Paasche-Orlow and Wolf (2007) on links between health literacy and health.
Working from these sources and our own observations, we formulated the Abilities, Skills, and Knowledge model of health literacy (Ownby, Acevedo, Waldrop-Valverde, et al., 2014). It is based on the hypothesis that after taking personal characteristics into account, health literacy comprises a combination of basic cognitive abilities, academic skills, and health-related knowledge. We tested this model under the assumption that currently-available measures could be used to define health literacy—in essence, by implicitly assuming that health literacy is what tests of health literacy measure. This assumption was based on the extensive research that has shown that these widely-used measures of health literacy, whatever their shortcomings (Pleasant, 2014), are clearly related to health status, behaviors, and outcomes.
In hierarchical regression models with successive blocks of variables, we first evaluated the relation of demographic variables such as age, gender, language, and socioeconomic status (SES) to standard measures of health literacy. In the modeling process, we then added blocks of variables representing cognitive ability, academic skills, and health-related conceptual knowledge. Results confirmed the usefulness of the ASK model in understanding health literacy as a type of expertise (Charness & Tuffiash, 2008) rooted in basic cognitive skills and academic skills but also requiring health-related conceptual knowledge. To the extent that health literacy tests actually sample the domain of health behavior, successful performance in the area of health improvement and maintenance requires basic cognitive abilities, skills usually acquired in education such as reading and arithmetic, and an understanding of basic health concepts (Ownby, Acevedo, Waldrop-Valverde, et al., 2014).
Implications of the ASK Model
This model has important implications for the design and implementation of interventions designed to improve health literacy. While it is difficult or impossible to change a person’s race, age, or basic cognitive abilities, it is clearly possible to improve individuals’ reading and math skills and their health-related conceptual knowledge. This led us to conclude that health literacy interventions should target improving patients’ skills in areas such as reading, arithmetic, and quantitative reasoning (applicable to understanding risk of treatments, for example), and their knowledge of health conditions and treatments. An important implication of the model is that interventions may be different for those with different levels of reading or quantitative skills. Interventions for skilled readers, for example, should emphasize improving a person’s understanding of their health condition and techniques to manage it. They can employ traditional instructional strategies that rely heavily on text. Interventions for less skilled readers, on the other hand, may emphasize support for limited reading skills in knowledge acquisition through instructional strategies that emphasize graphics and audio narration of text that is itself at lower levels of grammatical and vocabulary complexity.
The ASK Model and Health Behavior
Key questions that must also be addressed in the design of health literacy interventions are (1) how skills and knowledge are related to patient behavior, (2) how to target skills and knowledge to change behavior, and (3) how do patient characteristics (race, gender, age) affect the efficacy of interventions?
We would argue that the answer to the first question is that skills and knowledge have a crucial impact on health-related behavior through their effects on attitudes and behavioral intentions. Here, we draw heavily on concepts from the theory of planned behavior (Ajzen, 2012). This highly influential theory of health behavior states that an individual’s intention to perform a behavior depends on that person’s attitude toward the behavior, norms about the behavior (others’ beliefs and attitudes), and the person’s appraisal of their ability to perform the behavior (perceived behavioral control). Once an intent is formed, the likelihood of the behavior occurring is increased, although its actual performance can be affected by a number of factors such as opportunities, competing time demands, and the availability of alternative behaviors. The integration of the ASK model with the Theory of Planned Behavior is illustrated in Figure 1.
Figure 1.
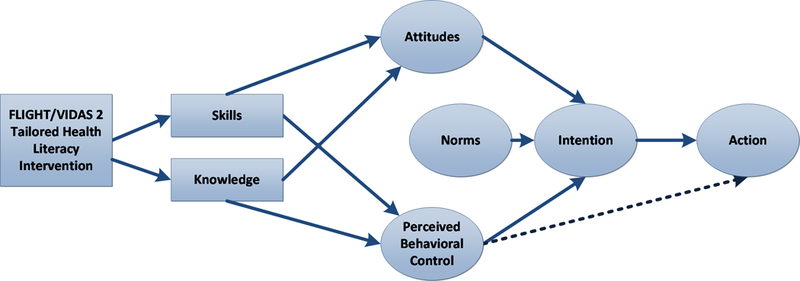
Integration of Health Literacy with Theory of Planned Behavior
Finding information and understanding it (for example, learning that diet and physical activity affect a person’s risk for developing diabetes or heart disease) are keys to changing a patient’s attitudes toward behaviors. Providing the person with knowledge, strategies for behavioral change, and encouragement can enhance their perception that behavior change is not only desirable but within their power, thus having an impact on perceived behavioral control. Changing these elements can thus help patients form the intention to change their behavior, a key step in the process of changing behavior.
Health literacy interventions can have a positive impact on patients’ skills and knowledge with respect to health and health management. These changes thus can have an impact on attitudes toward health behaviors (including the desirability of behaviors related to treatment adherence, diet, exercise, and other aspects of self-management). The changes can also have an impact on perceived behavioral control, since increased knowledge and skill may change patients’ perceptions of their ability to carry out desirable behaviors. Changes in attitudes and perceived behavioral control thus have an impact on intentions to act, behavior, and ultimately, a person’s health.
A central focus of any intervention to change patients’ health literacy in a way that can have an impact on their behavior is thus to find a way to effectively transmit health information in a form that the patient can understand. We believe at a minimum this means presenting health information at a difficulty level that is appropriate to the patient’s skills and cognitive abilities. Since much of the information available on the web and in current patient portals is written at greater levels of difficulty that exceed the capacities of most patients, this clearly is an issue that should be addressed in creating health literacy interventions.
The answer to the second question about the best way to maximize the impact of health literacy interventions on patient behavior involves a more extensive discussion of how to create and deliver tailored information.
Tailored Information
Research as well as everyday experience suggests to us that simply knowing something (such as “smoking is bad for you”) may not have much impact on our behavior. Attempts to enhance the impact of the information by multiple repetitions, as in repeated television announcements, may not do much increase its impact. How then, can we make help patients use health information to become healthier and live longer?
Many studies have shown that providing tailored information can increase the impact of health information on patient behavior (Lustria et al., 2013; Noar, Benac, & Harris, 2007). This strategy focuses on making information personally relevant to the patient through individual tailoring to make it specific and related to the patient’s needs and characteristics. Tailored information has been shown to have a much greater impact on patient behavior than simple delivery of information without tailoring (Kroeze, Werkman, & Brug, 2006; Noar et al., 2007).
The tailored information approach is based in a theory of how people process information called the elaboration likelihood model (Petty & Cacioppo, 1986). The model posits that people have two ways of processing information. In the peripheral route people don’t pay much attention to the content or logic of the message. To the extent that they notice the information, their attention is controlled by how attractive it is. In this route, an advertisement that features an attractive person or situation (people in bathing suits beside a pool, for example) may have an impact on hotel or airline choice.
In the central route, people take the information in and engage in more intensive processing. They pay attention to message content and the logic of arguments in the message. Information processed in this way is much more likely to have an impact on attitudes and beliefs and thus is more likely to be associated with changes in patient behavior. Since tailoring increases the likelihood of central processing of health-related messages, it has a better chance of helping patients change their behavior and becoming healthier.
Tailored information can be made more relevant to patients in a number of ways (Hawkins, Kreuter, Resnicow, Fishbein, & Dijkstra, 2008). Information should be tailored to address the patient’s perceived need for it and it should be delivered in a format that makes it appear personally relevant to and can be easily understood by the patient. Information can be made personally relevant by tailoring the presentation to the personal characteristics of the patient. In our current study, for example, we have created a multimedia intervention that enhances personal relevance by including graphic elements of persons similar in age, race, and gender to the patient (Ownby et al., 2017). Personal relevance is also enhanced by asking the patient for specific information about their experience of various health problems such as sleep disturbance or pain, and then providing them individually-tailored recommendations about how to manage the problem.
As previously noted, making the information provided to patients understandable can be a complex task. Given the wide range of health literacy abilities in the population, presenting information at the appropriate level of difficulty requires an assessment of patients’ capabilities to understand written or orally-presented information. A number of influential sources have advocated matching information presentation with patient skill (Promotion., 2012), although few have provided concrete guidance on how to accomplish this. We thus needed a way to quickly determine a person’s level of health literacy in order to determine the most effective way to provide them with the health information they need.
Precision Health Information™
We approached this problem by examining the task demands of the health literacy assessment questions developed in the FLIGHT/VIDAS study (Ownby, Acevedo, Waldrop-Valverde, Jacobs, Homs, et al., 2013). Three of us (Drs. Ownby, Acevedo, and Waldrop-Valverde) reviewed item content and categorized each item’s task demands according to the criteria used in the 2003 National Assessment of Health Literacy (White & Dillow, 2005) as initially derived by the Educational Testing Service (Kirsch, 2001) as below basic, basic, intermediate, or proficient.
A Below Basic item might require, for example, identification of a fact in a simple declarative sentence. Basic items might require additional skill such as integrating two pieces of information to direct an activity, such as “Take two pills three times a day.” Intermediate items might require extraction of information from a text passage at 6th to 8th grade level when multiple facts are presented. At this level, the person is asked to not only identify a specific bit of information but extract the most relevant information from a complex context. Finally, Proficient items require more complex skills, including extracting information in the context of conflicting information or integrating several bits of information to make an inference.
Each of us rated the items independently on their task demands, and approximately 80% agreement was initially obtained. Discrepancies were resolved in a conference. Items categorized by task demand were assembled into subscales of the original measure, and each participant in the original study was assigned a score on each of the new subscales. These scores were then used as input into a latent profile analysis using Mplus statistical analysis software (Muthén & Muthén, 2017) of participant performance on the items to identify subgroups who performed at various levels of health literacy. Number of classes in solutions from 1 to 6 groups was assessed with criteria including Aikaike’s information criterion (AIC), the entropy (Celeux & Soromenho, 1996), and the Lo-Mandell-Rubin test (Nylund, Asparouhov, & Muthen, 2007). While increases in the number of groups resulted in progressively better fit, the four-group solution we adopted resulted in a low AIC, a significant difference in the Lo-Mandell-Rubin likelihood ratio test, and an entropy of 0.87, greater than the cutoff value considered to indicate desirable value of 0.80 (Ramaswamy, Desarbo, Reibstein, & Robinson, 1993).
Groups performed differently on each of the subscales. For example, one group performed moderately well on items at the below basic level but very poorly on items in all other groups. A second group showed a good level of performance on below basic and most basic items but performed much less well on intermediate and proficient items. The other two groups performed at progressively better levels on the other groups of items. Level of performance on each of the subscales is illustrated in Figure 2.
Figure 2.
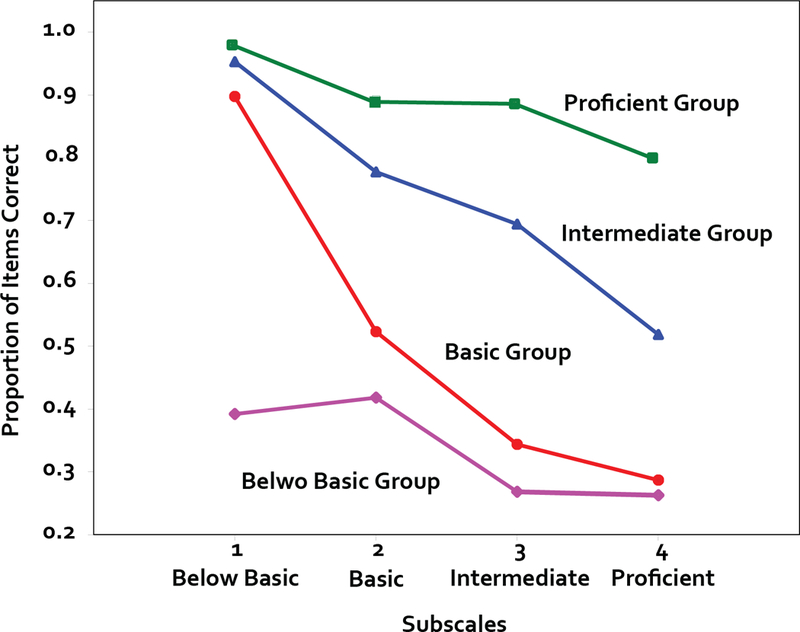
Subgroup performance on each subtest
In order to validate these groups, we conducted known groups validation (Davidson, 2014) to characterize individuals in each group from the latent profile analysis. Across-groups differences were assessed on variables in the ASK model of health literacy (Ownby, Acevedo, Waldrop-Valverde, et al., 2014), including age and years of education, abilities, academic skills, and healthcare knowledge.
Abilities were assessed using the Verbal Composite score and academic skills were assessed using the Passage Comprehension and Applied Problems subtests of the Woodcock Johnson Psycho-Educational Battery or Woodcock-Muñoz for Spanish speakers (Woodcock, McGrew, & Mather, 2007; Woodcock, Muñoz-Sandoval, McGrew, & Mather, 2007). General healthcare knowledge was assessed using the FACT subscale of the FLIGTH/VIDAS measure (Ownby, Acevedo, Waldrop-Valverde, Jacobs, & Caballero, 2013). Chi-square tests were used to assess the relation of group to categorical variables, and univariate analyses of variance (ANOVAs) were completed across groups for continuous variables. Descriptive statistics and results of the tests are presented in Table 1 (next page).
Table 1.
Description of Sample and Between-Groups Differences on Variables from ASK model used to characterize groupsa
| Below Basic | Basic | Intermediate | Proficient | Overall | df | χ2 | p | |
|---|---|---|---|---|---|---|---|---|
| N | 59 | 132 | 153 | 145 | 489 | |||
| Gender (Men/Women) | 20/39 | 44/88 | 57/96 | 65/80 | 186/303 | 3 | 4.55 | 0.21 |
| Language (English/Spanish) | 19/40 | 52/80 | 72/81 | 99/46 | 242/247 | 3 | 33.27 | <0.001 |
| Race (White/Black/Other) | 47/12/0 | 89/41/2 | 116/36/1 | 112/32/1 | 364/121/4 | 6 | 5.73 | 0.45 |
| df | F | p | ||||||
| Education | 9.12 (3.63) | 11.31 (2.76) | 12.68 (2.43) | 14.18 (2.43) | 12.32 (3.06) | 3, 488 | 61.20 | < 0.001 |
| Age | 68.20 (18.46) | 58.25 (16.21) | 48.32 (18.46) | 47.97 (18.46) | 53.07 (18.35) | 3, 488 | 23.70 | < 0.001 |
| SES | −0.84 (0.84) | −0.35 (0.91) | −0.01 (0.80) | 0.62 (0.97) | −0.01 (1.01) | 3, 488 | 47.54 | < 0.001 |
| Verbal | 84.12 (11.51) | 85.16 (10.59) | 91.11 (6.93) | 100.60 (10.21) | 91.45 (11.56) | 3, 488 | 76.64 | < 0.001 |
| Comp | 31.07 (6.19) | 33.37 (3.98) | 35.70 (3.24) | 39.92 (3.87) | 35.46 (4.85) | 3, 487 | 65.68 | < 0.001 |
| Comp GEb | 5.1 | 6.7 | 8.9 | 13.0 | 8.9 | |||
| Math | 37.12 (6.29) | 38.78 (5.15) | 43.88 (4.27) | 49.59 (6.45) | 43.36 (7.19) | 3, 488 | 120.06 | < 0.001 |
| Math GEb | 5.7 | 6.4 | 8.7 | 13.1 | 8.7 | |||
| FACT | 4.81 (2.60) | 5.89 (2.27) | 7.71 (2.38) | 9.37 (2.44) | 7.40 (2.87) | 3, 479 | 71.62 | < 0.001 |
All continuous variables are presented as means and standard deviations. Education = years of formal school; SES = score on index including education, income, and occupational status (mean = 0, SD = 1); Verbal = Woodcock-Johnson or Woodcock-Munoz (WJ/WM) Verbal Comprehension score (mean 100, SD = 15); Comp = WJ/WM Passage Comprehension raw score; Math = WJ/WM Applied Problems raw score; FACT = raw score on FLIGHT/VIDAS general health information scale (range 0 – 14).
Grade equivalent scores for the subtest means listed in the row above.
These analyses showed that both race and gender were not related to group membership. Individuals who were Spanish speaking were more likely to be in the below basic and basic groups compared to English speakers. Persons in the below basic and basic groups were older, less well education, and had a lower SES. They had lower scores the elements of the ASK model, with lower scores on general verbal ability, reading and math skills, and general health knowledge.
Based on these results and our previous analysis of the task demands of each item, we developed recommended instructional strategies to appropriately match individual abilities and skills when providing health-related information. For example, given the below basic group’s performance on general verbal abilities, reading skills, and healthcare information, we hypothesize that they will benefit from text presented in small semantic units at a level with minimal demands on reading skills (e.g., 3rd grade level) supplemented by graphics and audio narration. Other suggested instructional strategies followed a similar pattern of consideration of each group’s cognitive abilities, academic skills, and healthcare knowledge.
General descriptions of the capacities of individuals in each group and recommended instructional strategies follow:
Below Basic:
Individuals with less than basic health literacy will struggle with even rudimentary medication instructions such as “take one pill three times a day.” In our work, these individuals overall have poor reading skills although they often have very basic decoding skills. They are word-by-word readers who struggle with complex grammatical structures and unfamiliar vocabulary.
Instructional Strategy:
These individuals will benefit from audio narration of visually-presented material. Use of simple vocabulary and graphic illustrations of basic concepts will facilitate their understanding. As in other levels, checking patient understanding of key concepts through questioning and providing reteaching as needed will help to ensure mastery of essential concepts. In our current study (Ownby et al., 2017), this instructional strategy is represented in our multimedia intervention by presenting text at a third grade or less level supplemented by graphics and audio narration.
Basic:
Individuals with basic health literacy can understand simple instructions such as “take one pill every day.” They will show an inconsistent ability to follow more complex instructions, such as take “30 mg a day” when 10 mg tablets are dispensed. When presented with written information, they can understand simple declarative grammatical constructions but may not understand complex constructions or conditional statements.
Strategy:
Provide information in short and declarative sentences, such as “Take this medication at least two hours before eating” (not “on an empty stomach”). These persons will benefit from supplementation of expositions of more complex concepts with graphics and audio narration.
Intermediate:
Individuals with this level of health literacy will have moderate proficiency in basic reading skills and will generally be able to extract meaning from written information. They may not be able to correctly draw inferences that require integration of several facts or understanding of conditional or oblique references to concepts in written information. They may also benefit from supplementation of written information with graphic elements, especially when verbal information refers to visuospatial information (such as map locations or readily-visualized anatomic structures).
Strategy:
Provide written information at a sixth-grade reading level, with clear references to concepts in complex grammatical structures. Use graphic elements or illustrations to supplement and reinforce learning. In general, audio narration is not needed for most text and may be distracting for proficient readers. Continue to provide learning checks during instruction and provide reteaching as indicated.
Proficient:
These individuals will be proficient readers who experience little or no difficulty in extracting information from written text, even with complex grammatical structures such as embedded clauses and distant pronominal references. Key instructional strategies for these individuals will be providing basic health or disease-related information and providing directions to useful resources. For these individuals, interventions can focus primarily on imparting information rather than the channels or methods by which information is transmitted. Most patient education interventions are created at this level under the misguided assumption by their creators that others are similar with respect to reading and information extraction skills to the creators.
Determining Level of Health Literacy
An effective way to determine individuals’ level of health literacy is likely to be useful to guide interventions and instruction. We evaluated ways of making this determination by using polytomous logistic regression analysis to predict membership in each health literacy group based on demographic characteristics and performance on a 10-item health literacy screening measure created from FLIGHT/VIDAS items (Ownby, 2015). When membership in one of the four groups was the criterion, predictive accuracy of our model was about 75%.
Examining prediction errors, however, showed that most incorrect classifications were caused by erroneously classifying individuals to below basic vs basic levels or those assigned to intermediate vs proficient levels. Since the difference between basic and lower skills compared to intermediate and higher had major implications for instructional strategy in terms of text difficulty and need for audio and graphic support, we conducted additional analyses comparing two groups. We combined the lower and upper two groups since we judged that the difference between those groups was the most important in terms of health literacy and instructional needs. When a binary logistic regression model was created for two groups (below basic and basic vs. intermediate and proficient) using only demographic information and education, 80% of individuals were correctly classified (upper section, Table 2). When the 10-item health literacy screening test was included, more than 90% of individuals were correctly assigned (lower section, Table 2).
Table 2.
Classification tables for the models
| Model with Demographics and Education Only | ||||
|---|---|---|---|---|
| Predicted Classification |
Percent Correct |
|||
| Below Basic and Basic |
Intermediate and Proficient |
|||
| Actual Classification | Below Basic and Basic | 128 | 63 | 67.0 |
| Intermediate and Proficient | 34 | 263 | 88.6 | |
| Overall Percentage | 80.1 | |||
| Model with Demographics, Education and 10-Item Screen | ||||
| Predicted Classification |
Percent Correct |
|||
| Below Basic and Basic |
Intermediate and Proficient |
|||
| Actual Classification | Below Basic and Basic | 167 | 24 | 87.4 |
| Intermediate and Proficient | 18 | 279 | 93.9 | |
| Overall Percentage | 91.4 | |||
We further evaluated the performance of the model in classification using receiver operating characteristic (ROC) curves. ROC curves are a plot of a test’s sensitivity (ability to detect persons with a characteristic) compared to its specificity ability to detect persons without a characteristic). The approach allows the evaluation of various classification cutoff scores so that maximal sensitivity or specificity characteristics can be determined. A plot of these values results in a curve, and the area under the curve (AUC) is a measure of how well a classification technique works. The AUCs, along with their standard errors and probabilities in comparison to a random classification model, are presented in Table 3 (next page) and the ROC curve for the full prediction model is presented in Figure 3 (next page).
Table 3.
Receiver operating characteristic curve statistics
| Model with Demographic Variable and Years of Education | |||
|---|---|---|---|
| Area Under the Curve | Standard Error | P | 95% CI |
| 0.86 | 0.02 | < 0.001 | 0.81 – 0.88 |
| Model with Demographic Variable, Years of Education and 10-item Screen | |||
| 0.97 | 0.006 | < 0.001 | 0.96 – 0.99 |
Figure 3.
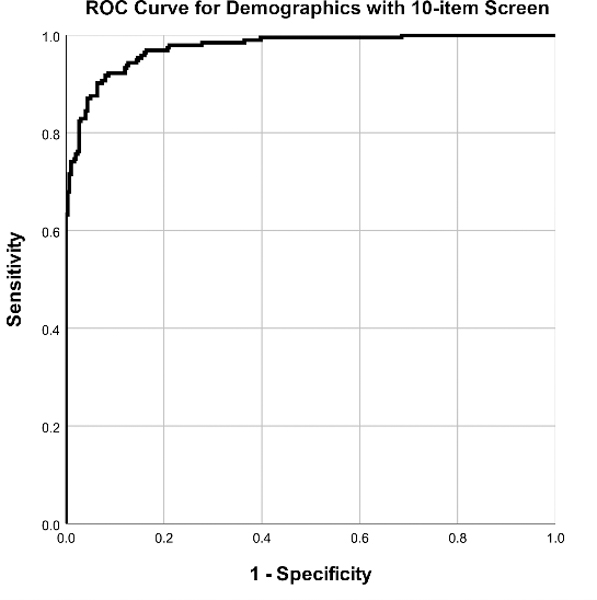
Receiver operating characteristic curve for full model
A combination of personal characteristics and performance on a brief measure of health literacy may thus be way to quickly and accurately identify individuals who may have different instructional needs in improving their health literacy.
Multimedia Electronic Health Literacy Interventions
An examination of the content of most educational interventions contents shows that a significant proportion of any intervention involves frequent teaching and reteaching of the same basic material (e.g., 2 + 2 = 4). We suggest that the burden of repetitively teaching and reteaching basic material can readily be assumed by computer-delivered interventions, freeing skilled educators to pursue the critically important task of providing individualized instruction that cannot be automated. In addition, automated applications can provide essentially unlimited repetitions of materials to be learned based on individual rather than small group or classroom needs.
Computer-delivered interventions offer the additional benefit of providing a convenient and potentially powerful platform to deliver multimedia content over the Internet, at the least including graphics and audio but potentially including motion graphics and video. These latter elements can facilitate health-related skill acquisition through the process of social modeling, consistent with social learning theory. Further, computer-delivered interventions once developed can be widely disseminated at low cost. In a previous study, we showed that a web-based intervention could be cost-effective and could even be cost saving depending on number of users (Ownby, Waldrop-Valverde, et al., 2013).
Chronic Disease Self-Management
The most common health condition in older persons in the United States is multimorbidity (Tinetti, Fried, & Boyd, 2012). Most individuals over 50 years of age have more one than one chronic condition. While a number of disease-specific skills rare elated to each condition, some problems occur in older adults with multiple conditions that are not disease specific. These include pain, fatigue, sleep disturbance, and mood problems, for example. Older persons may also have problems in understanding and navigating the health care system and in working with a team of providers. Skills related to managing multiple chronic diseases are thus important for many older adults. Acquiring chronic disease self-management (CDSM) skills (Bodenheimer et al., 2002) is thus an important target for health literacy interventions.
Current Project: FLIGHT/VIDAS 2
In our current project, we seek to capitalize on results of previous work while evaluating our hypotheses about the impact of tailoring health information by reading level and instructional strategy for persons with low health literacy (Ownby et al., 2017). We also will evaluate the usefulness of matching health information delivery to level of health literacy by randomly assigning participants to one of three conditions in which they receive the same content related to chronic disease self-management at one of three grade levels, either 8th, 6th, or 3rd. Participants are completing an extensive battery of questionnaires similar to that used in the original FLIGHT/VIDAS study, assessing health-related quality of life, healthcare utilization, diagnoses, symptoms, sleep, mood, and activity. In this study we will also include measures of patient-provider relationship and patient activation (Hibbard, Stockard, Mahoney, & Tusler, 2004).
Figures 4 to 6 illustrate our approach, with graphics that support comprehension of page contents. These figures also illustrate different levels of text difficulty. Figure 4 shows a slide that illustrates teaching material about acute versus chronic pain. Text is at a third-grade level. Figure 5 is an example from an intervention module focused on treatment adherence that aims to help patients work effectively with healthcare providers. Text is at a sixth-grade level.
Figure 4.
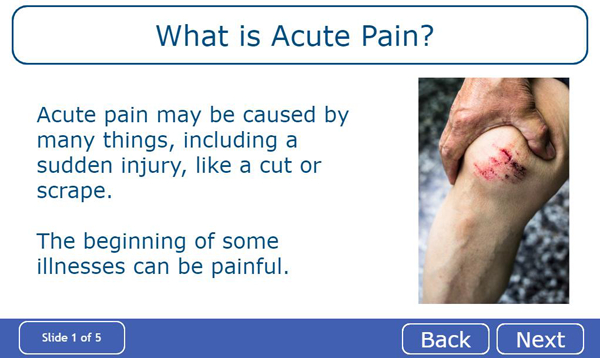
Acute vs. Chronic Pain
Figure 6.

Using a Medication Organizer
Figure 5.
Making an Appointment
Figure 6 is also drawn from a module on treatment adherence that explains how use of a pill organizer can be helpful in remembering to take medication. Text here is also at a sixth-grade level.
Summary
In this paper, we reviewed our previous work on effective ways to help patients maintain and improve their health by improving health literacy. We think that this information may be useful to distance learning practitioners interested in health education, since we outline possible strategies to ensure that information presented in distance learning apps can be understood and acted upon by learners. We provided a brief recounting of our previous studies and discussed how they helped us develop the ASK model of health literacy as a way to make operational the elements of heath literacy that should be targets for interventions. We showed how health literacy, made operational as skills and knowledge, can be integrated into an influential theory of health behavior, the Theory of Planned Behavior. We discussed the usefulness of tailored information as a strategy for enhancing the usefulness and impact of interventions designed to improve health literacy.
Finally, we provided a brief overview of how we can use information about a person’s level of health literacy to determine the likely optimal instructional strategy to ensure that information imparted to them has the maximum impact on their attitudes toward health behaviors and on their perceptions of their ability to perform the behaviors. In our current project, ongoing, we are testing key hypotheses that matching patient level of health literacy to interventions will produce optimal improvements in patients’ health literacy, self-efficacy, and improve their ability to work with providers.
Contributor Information
Raymond L Ownby, Department of Psychiatry and Behavioral Medicine, Nova Southeastern University, Fort Lauderdale, FL.
Amarilis Acevedo, College of Psychology, Nova Southeastern University, Fort Lauderdale, FL.
Drenna Waldrop-Valverde, Nell Hodgson Woodruff School of Nursing, Emory University, Atlanta GA.
References
- Ajzen I (2012). The theory of planned behavior In Lange PAM, Kruglanski AW, & Higgins ET (Eds.), Handbook of theories of social psychology (pp. 438–459). London: Sage. [Google Scholar]
- Baker DW (2006). The meaning and the measure of health literacy. Journal of General Internal Medicine, 21(8), 878–883. doi: 10.1111/j.1525-1497.2006.00540.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, … Peel J (2004). Health literacy and use of outpatient physician services by Medicare managed care enrollees. Journal of General Internal Medicine, 19(3), 215–220. doi: 10.1111/j.1525-1497.2004.21130.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, & Huang J (2007). Health literacy and mortality among elderly persons. Archives of Internal Medicine, 167(14), 1503–1509. doi: 10.1001/archinte.167.14.1503 [DOI] [PubMed] [Google Scholar]
- Berkman ND, Dewalt DA, Pignone MP, Sheridan SL, Lohr KN, Lux L, … Bonito AJ (2004). Literacy and health outcomes. Evidence Report/Technology Assessmet No. 87. AHRQ Publication No. 04-E007–2. Rockville, MD: Agency for Healthcare Research and Quality; Accessed at: https://www.ncbi.nlm.nih.gov/books/NBK11942/ [Google Scholar]
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, & Crotty K (2011). Low health literacy and health outcomes: an updated systematic review. Annals of Internal Medicine, 155(2), 97–107. doi: 10.1059/0003-4819-155-2-201107190-00005 [doi] [DOI] [PubMed] [Google Scholar]
- Bo A, Friis K, Osborne RH, & Maindal HT (2014). National indicators of health literacy: ability to understand health information and to engage actively with healthcare providers -a population-based survey among Danish adults. BMC Public Health, 14, 1095. doi: 10.1186/1471-2458-14-1095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodenheimer T, Lorig K, Holman H, & Grumbach K (2002). Patient self-management of chronic disease in primary care. JAMA, 288(19), 2469–2475. doi: 10.1001/jama.288.19.2469 [DOI] [PubMed] [Google Scholar]
- Burke M, Carey P, Haines L, Lampson AP, & Pond F (2010). Implementing the information prescription protocol in a family medicine practice: a case study. Journal of the Medical Library Association, 98(3), 228–234. doi: 10.3163/1536-5050.98.3.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celeux G, & Soromenho G (1996). An entropy criterion for assessing the number of clusters in a mixture model. Journal of Classification, 13, 195–212. [Google Scholar]
- Pew Research Center. (2018). Internet/Broadband Fact Sheet. Retrieved from http://www.pewinternet.org/fact-sheet/internet-broadband/
- Charness N, & Tuffiash M (2008). The role of expertise research and human factors in capturing, explaining, and producing superior performance. Humam Factors, 50(3), 427–432. doi: 10.1518/001872008X312206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson M (2014). Known-groups validity In Michalos AC (Ed.), Encyclopedia of Quality of Life and Well-Being Research (pp. 3481–3482). Dordrecht: Springer Netherlands. [Google Scholar]
- Dewalt DA, Berkman ND, Sheridan S, Lohr KN, & Pignone MP (2004). Literacy and health outcomes: A systematic review of the literature. Journal of General Internal Medicine 19(12), 1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeWalt DA, Broucksou KA, Hawk V, Brach C, Hink A, Rudd R, & Callahan L (2011). Developing and testing the health literacy universal precautions toolkit. Nursing Outlook, 59(2), 85–94. doi: 10.1016/j.outlook.2010.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diviani N, van den Putte B, Giani S, & van Weert JC (2015). Low health literacy and evaluation of online health information: A systematic review of the literature. Journal of Medical Internet Research, 17(5), e112. doi: 10.2196/jmir.4018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donker T, Petrie K, Proudfoot J, Clarke J, Birch M-R, & Christensen H (2013). Smartphones for smarter delivery of mental health programs: A systematic review. Journal of Medical Internet Research, 15(11), e247. doi: 10.2196/jmir.2791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores Mateo G, Granado-Font E, Ferré-Grau C, & Montaña-Carreras X (2015). Mobile phone apps to promote weight loss and increase physical activity: A systematic review and meta-analysis. Journal of Medical Internet Research, 17(11), e253–e253. doi: 10.2196/jmir.4836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox S, & Duggan M (2012). Mobile health 2012. Washington DC: Pew Research Center’s Internet & Amerian Life Project; Retrieved from: http://www.pewinternet.org/Reports/2012/Mobile-Health.aspx. [Google Scholar]
- Hawkins RP, Kreuter M, Resnicow K, Fishbein M, & Dijkstra A (2008). Understanding tailoring in communicating about health. Health. Education Research, 23(3), 454–466. doi: 10.1093/her/cyn004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard JH, Stockard J, Mahoney ER, & Tusler M (2004). Development of the Patient Activation Measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Services Research, 39(4 Pt 1), 1005–1026. doi: 10.1111/j.1475-6773.2004.00269.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou C, Xu Q, Diao S, Hewitt J, Li J, & Carter B (2018). Mobile phone applications and self-management of diabetes: A systematic review with meta-analysis, meta-regression of 21 randomized trials and GRADE. Diabetes, Obesity and Metabolism, 20(8), 2009–2013. doi: 10.1111/dom.13307 [DOI] [PubMed] [Google Scholar]
- Jameson JL, & Longo DL (2015). Precision medicine--personalized, problematic, and promising. New England Journal of Medicine, 372(23), 2229–2234. doi: 10.1056/NEJMsb1503104 [DOI] [PubMed] [Google Scholar]
- Jerant A, Sohler N, Fiscella K, Franks B, & Franks P (2011). Tailored interactive multimedia computer programs to reduce health disparities: Opportunities and challenges. Patient Education and Counseling, 85(2), 323–330. doi: 10.1016/j.pec.2010.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang H, & Park HA (2016). A mobile app for hypertension management based on clinical practice guidelines: Development and deployment. JMIR mHealth and uHealth, 4(1), e12–e12. doi: 10.2196/mhealth.4966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirsch I (2001). The International Adult Literacy Survey (IALS): Understanding what was measured. Princeton, NJ: Educational Testing Service; Retrieved from: https://www.ets.org/Media/Research/pdf/RR-01-25-Kirsch.pdf [Google Scholar]
- Kroeze W, Werkman A, & Brug J (2006). A systematic review of randomized trials on the effectiveness of computer-tailored education on physical activity and dietary behaviors. Annals of Behavioral Medicine, 31(3), 205–223. doi: 10.1207/s15324796abm3103_2 [DOI] [PubMed] [Google Scholar]
- Kuhn E, Weiss BJ, Taylor KL, Hoffman JE, Ramsey KM, Manber R, … Trockel M (2016). CBT-I Coach: A description and clinician perceptions of a mobile app for cognitive behavioral therapy for insomnia. Journal of Clinical Sleep Medicine, 12(4), 597–606. doi: 10.5664/jcsm.5700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SY, Bender DE, Ruiz RE, & Cho YI (2006). Development of an easy-to-use Spanish health literacy test. Health Services Research, 41(4 Pt 1), 1392–1412. doi: 10.1111/j.1475-6773.2006.00532.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lustria ML, Noar SM, Cortese J, Van Stee SK, Glueckauf RL, & Lee J (2013). A meta-analysis of web-delivered tailored health behavior change interventions. Journal of Health Communication, 18(9), 1039–1069. doi: 10.1080/10810730.2013.768727 [DOI] [PubMed] [Google Scholar]
- Mayer RE (2009). Multimedia learning (2nd ed.). New York: Cambridge. [Google Scholar]
- Mayer RE, & Moreno R (2003). Nine ways to reduce cognitive load in multimedia learning. Educational Psychologist, 38(1), 43–52. doi: 10.1207/S15326985EP3801_6 [DOI] [Google Scholar]
- Middelweerd A, Mollee JS, van der Wal CN, Brug J, & te Velde SJ (2014). Apps to promote physical activity among adults: a review and content analysis. International Journal of Behavioral Nutrition and Physical Activity, 11(1), 97. doi: 10.1186/s12966-014-0097-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy PW, Davis TC, Long SW, Jackson RH, & Decker BC (1993). Rapid Estimate of Adult Literacy in Medicine (REALM): A quick reading test for patients. Journal of Reading, 37, 124–130. [Google Scholar]
- Muthén LK, & Muthén BO (2017). Mplus user’s guide (8th ed.). Los Angeles: Muthén & Muthén. [Google Scholar]
- Noar SM, Benac CN, & Harris MS (2007). Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin, 133(4), 673–693. doi: 10.1037/0033-2909.133.4.673 [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, & Muthen BO (2007). Deciding on the number of classes in a latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling, 14, 535–569. doi: 10.1080/10705510701575396 [DOI] [Google Scholar]
- Oldach BR, & Katz ML (2014). Health literacy and cancer screening: A systematic review. Patient Education and Counseling, 94(2), 149–157. doi: 10.1016/j.pec.2013.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborn CY, Cavanaugh K, Wallston KA, Kripalani S, Elasy TA, Rothman RL, & White RO (2011). Health literacy explains racial disparities in diabetes medication adherence. Journal of Health Communication, 16 Suppl 3, 268–278. doi: 10.1080/10810730.2011.604388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborn CY, Paasche-Orlow MK, Davis TC, & Wolf MS (2007). Health literacy: An overlooked factor in understanding HIV health disparities. American Journal of Preventive Medicine, 33(5), 374–378. doi: 10.1016/j.amepre.2007.07.022 [DOI] [PubMed] [Google Scholar]
- Ownby RL (2005). Development of an interactive tailored information application to improve patient medication adherence. AMIA Annual Symposium Proceedings, 2005, 1069 Retireved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1560773. [PMC free article] [PubMed] [Google Scholar]
- Ownby RL (2006). Readability of consumer-oriented geriatric depression information on the Internet. Clinical Gerontologist, 29(6), 17–32. doi: 10.1300/J018v29n04_02 [DOI] [Google Scholar]
- Ownby RL (2015). FLIGHT/VIDAS User Manual. Fort Lauderdale, FL: Enalan Communications, Inc. [Google Scholar]
- Ownby RL, Acevedo A, Jacobs RJ, Caballero J, & Waldrop-Valverde D (2014). Quality of life, health status, and health service utilization related to a new measure of health literacy: FLIGHT/VIDAS. Patient Education and Counselling, 96(3), 404–410. doi: 10.1016/j.pec.2014.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ownby RL, Acevedo A, & Waldrop-Valverde D (2019, March). Predictive analytic model to identify the most effective tailoring strategy for a chronic disease self‐management mobile app. Paper presented at the Society for Behavioral Medicine, Washington DC Accessed at: https://osf.io/bephg/ [Google Scholar]
- Ownby RL, Acevedo A, Waldrop-Valverde D, Caballero J, Simonson M, Davenport R, … Jacobs RJ (2017). A mobile app for chronic disease self-management: Protocol for a randomized controlled trial. JMIR Research Protocols, 6(4), e53. doi: 10.2196/resprot.7272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ownby RL, Acevedo A, Waldrop-Valverde D, Jacobs RJ, & Caballero J (2013, October). A new computer-administered measure of health literacy: Validity and relation to quality of life in Spanish and English speakers. Paper presented at the International Conference on Communication in Healthcare, Montreal, Canada. [Google Scholar]
- Ownby RL, Acevedo A, Waldrop-Valverde D, Jacobs RJ, & Caballero J (2014). Abilities, skills and knowledge in measures of health literacy. Patient Education and Counseling, 95(2), 211–217. doi: 10.1016/j.pec.2014.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ownby RL, Acevedo A, Waldrop-Valverde D, Jacobs RJ, Homs AM, Czaja SJ, & Loewenstein D (2013). Development and initial validation of a computer-administered health literacy assessment in Spanish and English: FLIGHT/VIDAS. Patient Related Outcome Measures, 4, 1–15. doi: 10.2147/PROM.S48384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ownby RL, Hertzog C, & Czaja SJ (2012). Tailored information and automated reminding to improve medication adherence in Spanish-and English-speaking elders treated for memory impairment. Clinical Gerontologist, 35(3), 221–238. doi: 10.1080/07317115.2012.657294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ownby RL, Waldrop-Valverde D, Caballero J, & Jacobs RJ (2012). Baseline medication adherence and response to an electronically delivered health literacy intervention targeting adherence. Neurobehavioral HIV Medicine, 4, 113–121. doi: 10.2147/NBHIV.S36549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ownby RL, Waldrop-Valverde D, Jacobs RJ, Acevedo A, & Caballero J (2013). Cost effectiveness of a computer-delivered intervention to improve HIV medication adherence. BMC Medical Informatics and Decision Making, 13, 29. doi: 10.1186/1472-6947-13-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paas F, Renkl A, & Sweller J (2004). Cognitive Load Theory: Instructional implications of the interaction between information structures and cognitive architecture. Instructional Science, 32(1), 1–8. [Google Scholar]
- Paasche-Orlow MK, & Wolf MS (2007). The causal pathways linking health literacy to health outcomes. American Journal of Health Behavior, 31(Suppl 1), S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19 [DOI] [PubMed] [Google Scholar]
- Paasche-Orlow MK, & Wolf MS (2010). Promoting health literacy research to reduce health disparities. Journal of Health Communication, 15 (Suppl 2), 34–41. doi: 10.1080/10810730.2010.499994. [DOI] [PubMed] [Google Scholar]
- Parker RM, Baker DW, Williams MV, & Nurss JR (1995). The Test of Functional Health Literacy in Adults: A new instrument for measuring patients’ literacy skills. Journal of General Internal Medicine, 10, 537–541. doi: 10.1007/BF02640361 [DOI] [PubMed] [Google Scholar]
- Parker RM, Ratzan SC, & Lurie N (2003). Health literacy: a policy challenge for advancing high-quality health care. Health Affairs (Millwood), 22, 147–153. doi: 10.1377/hlthaff.22.4.147 [DOI] [PubMed] [Google Scholar]
- Paskett E, Thompson B, Ammerman AS, Ortega AN, Marsteller J, & Richardson D (2016). Multilevel interventions to address health disparities show promise in improving population health. Health Affairs, 35, 1429–1434. doi: 10.1377/hlthaff.2015.1360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patient Protection and Affordable Care Act, 42 USC, 18001 Stat. (2010). Accessed at: https://www.hhs.gov/sites/default/files/ppacacon.pdf.
- Payne HE, Lister C, West JH, & Bernhardt JM (2015). Behavioral functionality of mobile apps in health interventions: a systematic review of the literature. JMIR mHealth and uHealth, 3(1), e20. doi: 10.2196/mhealth.3335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petty RE, & Cacioppo JT (1986). The elaboration likelihood model of persuasion In Berkowitz L (Ed.), Advances in Experimenal Social Psychology (pp. 123–205). San Diego: Academic Press. [Google Scholar]
- Pleasant A (2014). Advancing health literacy measurement: A pathway to better health and health system performance. Journal of Health Communication, 19(12), 1481–1496. doi: 10.1080/10810730.2014.954083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Internet Project (2013). Majority of adults look online for health information. Retrieved from http://www.pewresearch.org/fact-tank/2013/02/01/majority-of-adults-look-online-for-health-information/
- U. S. Department of Health and Human Services (2012). Health People 2020. Washington DC: Author; Available at http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=8. [Google Scholar]
- Ramaswamy V, Desarbo WS, Reibstein DJ, & Robinson WT (1993). An empirical pooling approach for estimating marketing mix elasticities with PIMS data. Marketing Science, 12, 103–124. [Google Scholar]
- Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, … Bindman AB (2002). Association of health literacy with diabetes outcomes. JAMA, 288, 475–482. doi: 10.1001/jama.288.4.475 [DOI] [PubMed] [Google Scholar]
- Sheridan SL, Halpern DJ, Viera AJ, Berkman ND, Donahue KE, & Crotty K (2011). Interventions for individuals with low health literacy: a systematic review. Journal of Health Communication, 16 (Suppl 3), 30–54. doi: 10.1080/10810730.2011.604391 [DOI] [PubMed] [Google Scholar]
- Snyder E, & Oliver J (2014). Evidence based strategies for attesting to meaningful use of electronic health records: An integrative review. Online Journal of Nursing Informatics, 18(3). Accessed at: https://www.himss.org/evidence-based-strategies-attesting-meaningful-use-electronic-health-records-integrative-review. [Google Scholar]
- Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, & Brand H (2012). Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health, 12, 80. doi: 10.1186/1471-2458-12-80 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudore RL, Yaffe K, Satterfield S, Harris TB, Mehta KM, Simonsick EM, … Schillinger D (2006). Limited literacy and mortality in the elderly: The health, aging, and body composition study. Journal of General Internal Medincine, 21, 806–812. doi: 10.1111/j.1525-1497.2006.00539.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweller J (1988). Cognitive load during problem solving: Effects on learning. Cognitive Science, 12, 257–285. [Google Scholar]
- Teresi JA (2006). Overview of quantitative measurement methods. Equivalence, invariance, and differential item functioning in health applications. Medical Care, 44 (11 Suppl 3), S39–S49. doi: 10.1097/01.mlr.0000245452.48613.45 [DOI] [PubMed] [Google Scholar]
- Thurnheer SE, Gravestock I, Pichierri G, Steurer J, & Burgstaller JM (2018). Benefits of mobile apps in pain management: Systematic review. JMIR mHealth and uHealth, 6(10), e11231. doi: 10.2196/11231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinetti ME, Fried TR, & Boyd CM (2012). Designing health care for the most common chronic condition--multimorbidity. JAMA, 307, 2493–2494. doi: 10.1001/jama.2012.5265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White S (2008). Assessing the nation’s health literacy. Chicago: AMA Foundation. [Google Scholar]
- White S, & Dillow S (2005). Key concepts and features of the 2003 National Assessment of Adult Literacy (NCES 2006–471). Washington DC: US Department of Education, National Center for Educational Statistics; Accessed at: https://nces.ed.gov/NAAL/PDF/2006471_1.PDF. [Google Scholar]
- Woodcock RW, McGrew KS, & Mather N (2007). Woodcock-Johnson III Normative Update. Rolling Meadows, IL: Riverside. [Google Scholar]
- Woodcock RW, Muñoz-Sandoval AF, McGrew KS, & Mather N (2007). Batería III Woodcock-Muñoz. Rolling Meadows, IL: Riverside. [Google Scholar]
- Wu JR, Holmes GM, DeWalt DA, Macabasco-O’Connell A, Bibbins-Domingo K, Ruo B, … Pignone M (2013). Low literacy is associated with increased risk of hospitalization and death among individuals with heart failure. Journal of General Internal Medicine, 28, 1174–1180. doi: 10.1007/s11606-013-2394-4 [DOI] [PMC free article] [PubMed] [Google Scholar]


