Abstract
Rising healthcare costs and quality demands have driven both the Centers for Medicare and Medicaid Services (CMS) and the private sector to seek innovations in health system design by placing institutions at financial risk. Novel care models, such as bundled reimbursement, aim to boost value though quality improvement and cost reduction. The Center for Medicare and Medicaid Innovation (CMMI) is leading the charge in this area with multiple pilots and mandates including Comprehensive Care for Joint Replacement (CJR), and cardiac surgery scheduled on the horizon. Other high cost and high volume procedures could be considered for bundling in the future, including breast reconstruction. Herein conceptual considerations surrounding bundling of breast reconstruction are discussed.
Background
Rising healthcare costs and quality demands have driven both the Centers for Medicare and Medicaid Services (CMS) and the private sector to seek innovations in health system design by placing institutions at financial risk. Novel care models, such as bundled reimbursement, aim to boost value though quality improvement and cost reduction. The Center for Medicare and Medicaid Innovation (CMMI) is leading the charge in this area with multiple pilots and mandates including Comprehensive Care for Joint Replacement (CJR), and cardiac surgery scheduled on the horizon. Other high cost and high volume procedures could be considered for bundling in the future, including breast reconstruction. Herein conceptual considerations surrounding bundling of breast reconstruction are discussed.
Current Payment Reform and Expansion
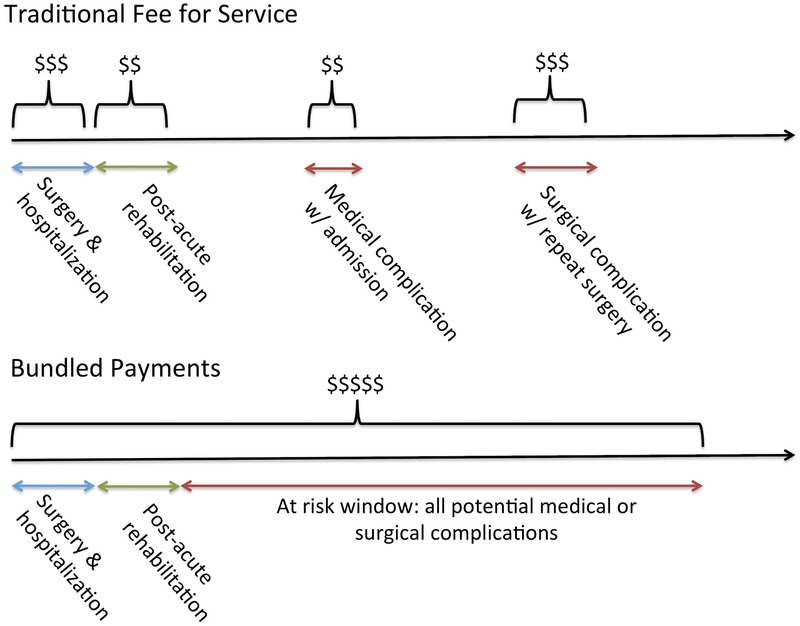
In 2015, a bipartisan effort passed the Medicare Access and CHIP Reauthorization Act (MACRA), a statute that permanently repealed the Sustainable Grown Rate (SGR) in a transition away from fee-for-service (FFS) reimbursement towards value incentivized care. One payment pathway established under the law was Alternative Models (APM). The bundled payments care improvement (BPCI) initiative is a form of APM that was developed by the Center for Medicare and Medicaid Innovation (CMMI). Bundle payment refers to an arrangement wherein hospitals, post-acute care providers (e.g. nursing homes, rehabs) and physicians manage the financial risks and gain, relative to a “target price” for total spending during a defined clinical care episode (Figure 1). The intent is to incentivize quality improvement and cost reduction by increasing accountability and care coordination among previously fragmented participating health systems and siloed providers. BPCI has been piloted for 48 Medical Severity-Diagnosis Related Group (MS-DRG) conditions since 2013(1). Early experience has yielded success in reducing complications and/or lowering costs in lower extremity joint replacement with mixed outcomes for spinal surgery and cardiac surgery (2) (3). These results informed the first mandated bundled payment program from CMMI: Comprehensive Care for Joint Replacement (CJR). Lower Extremity Joint Replacement was chosen because it represents one of the most costly and voluminous procedures in aggregate to Medicare (4).
Figure 1:
Comparison of fee-for-service (FFS) to bundled payments in reimbursement of surgical procedures. Total reimbursement for FFS > bundled payments. Axis represents time.
Under current fee-for-service models, high cost and high volume procedures have demonstrated substantial variation in spending and outcomes that provides an opportunity for standardization; therefore, it is reasonable to expect that any could be considered for inclusion in a bundle(5). While many procedures within the greater field of plastic and reconstructive surgery are high cost (e.g. lower extremity reconstruction) or high volume (e.g. carpal tunnel release), there are select procedures that satisfy both criteria. An estimated 246,000 women were diagnosed with breast cancer in 2016 (6) of which 37–40% received mastectomy (7). Recent studies show upwards of 40% of those undergoing mastectomy receive some form of reconstruction (8), which translates into 36,000–39,000 cancer-related reconstructions in 2016. Considering bilateral reconstructions and prophylactic mastectomies for genetic risk reduction, the American Society of Plastic Surgery (ASPS) reports over 109,000 reconstructive breast operations performed by ASPS members in 2016 (9). The associated 90-day charges for tissue expander and autologous reconstruction are $39,470 and $54,309 per episode respectively (10), with median adjusted payments of $12,732 and 17,519 (11). In light of CJR, Medicare reports an annual knee arthroplasty incidence of 400,000 cases, and pays $16,500 to $33,000 per episode(12). Thus breast reconstruction is smaller in volume by 4-fold with payments on par with CJR.
Is Breast Reconstruction a Potential Candidate for Bundling?
Information targeted at surgeons regarding bundled payment reforms has been limited, largely because pilot models are still ongoing. Nonetheless, The American College of Surgeons (ACS) General Surgery Coding and Reimbursement Committee (GSCRC) published a primer on bundled payment reform, aiming to educate the broader surgical community (13). A logic-driven checklist of criteria for evaluation of bundled payments for any procedure was provided. Table 1 is a consolidated and organized list of criteria.
Table 1:
Criteria for Consideration of Surgical Procedure for Bundled Payments
| Criteria |
|---|
| Procedure Characteristics |
| High volume |
| High cost |
| Ubiquitous across regions and institutions |
| Measureable Variables |
| Costs |
| Outcomes (objective and patient reported) |
| Resource utilization |
| Low vulnerability to up-coding or miscoding |
| Predictability of costs |
| Multidisciplinary total care delivery |
Application of the GSCRC criteria to breast reconstruction shows no obvious grounds for exclusion. The procedure is elective and performed all across the United States (14). Breast cancer affects women with private insurance and Medicare alike(6). Approximately 40% of newly diagnosed breast cancer cases in 2016 will occur in older women(15). Outcomes data are available in longitudinal databases, which offer an opportunity to evaluate resource utilization and cost variation across the entire care continuum. Lastly, its prevalence as the second leading cause of cancer death in women, and high visibility among the public ensures that Medicare will be interested in all elements of breast cancer care including reconstruction.
Should Breast Reconstruction Bundle with Other Aspects of Breast Cancer Treatment?
The current diagnostic and therapeutic management of breast cancer is multi-disciplinary and incredibly varied. Consequently, universal treatment pathways are the exception in managing breast cancer as opposed to the norm(16), especially in the era of individualized medicine. The resulting variation in costs is profound, largely reflecting differences in chemotherapy and radiation utilization (16)(17) (18). For example, the use of trastuzumab in human epidermal growth factor receptor 2 (HER2) positive breast cancer costs $78,330 more than HER2 negative variants (19). Whereas cost variation is an opportunity for improvement in standardized procedures with a single disease (such as lower extremity joint replacement for osteoarthritis), cost variation due to inherent disease diversity is not conducive to a single bundled payment, which combines both breast oncology with reconstruction. Recognizing the impact of disease variability on health service utilization, CMMI has instead piloted the Oncology Care Model, which captures all charges (“total cost of care”) and quality metrics within a 180 day window, triggered by the administration of chemotherapy, to incentivize best practices and care redesign (20). Currently, the model is built with bonuses (upside risk) with potential for penalties (downside risk) in coming years.
Combining breast reconstruction with mastectomy in a payment bundle poses other challenges. Firstly, the majority of women undergoing mastectomy do not receive reconstruction. While the incidence of reconstruction is increasing, the rate of immediate reconstruction remains at approximately 40% in recent analyses(8). Any payment target combining reconstruction with mastectomy could incentivize health systems to dissuade or delay reconstruction in order to reap the difference in savings. In addition, a single bundled payment for mastectomy and reconstruction is mutually exclusive with delayed reconstruction. Therefore, for any of these reasons it would appear difficult to consider breast cancer treatment and reconstruction as a single entity for the purposes of bundling.
Assuming that mastectomy and reconstruction parse separately, there is no actuarial or clinical reason to have separate bundles for immediate and delayed reconstruction. Currently, payers prefer that mastectomies and reconstructions be performed concurrently to avoid paying for hospitalization and operating room costs twice. However, with separate bundles for mastectomy and reconstruction, the payer will be agnostic to whether providers combine the operations because the reimbursements are fixed for each episode. This will, however, incentivize healthcare systems to perform mastectomies and reconstructions concurrently in order to reap the savings of a single hospitalization. Similarly, there would be no penalty to either payer or provider if they choose to separate the cases for any reason.
Aspects of Breast Reconstruction to Include in an Episode
A key tenet of bundling is appropriately defining an episode of care. Lower extremity joint replacement has a straightforward episode of care that includes a single operation followed by rehabilitation. Breast reconstruction has a variety of pathways that challenge an episodic definition. Prosthetic reconstruction provides an example. Currently, tissue expander pathways to breast reconstruction reimburse more than direct-to-implant reconstruction because the FFS model views the tissue expander exchange to permanent implant as a separate reimbursable procedure. In contrast, the concept of bundling breast reconstruction would reimburse a single amount regardless of prosthetic reconstruction pathway. This could seemingly incentivize direct to implant methods, but closer evaluation might actually encourage the opposite given lower complication rates with staged reconstruction (21).
Considerations for an episode must also evaluate the role of revisionary surgery. Currently, the Women’s Health and Cancer Rights Act (WHCRA) mandates insurance coverage for breast reconstruction related procedures including all revisions. This has the benefit of protecting women from insurance denials. Bundling revisions in the original episode may undermine the goals of the WHCRA if surgeons are less likely to offer these procedures because of financial disincentives. One solution would be to classify revisions as unique episodes with their own bundle payment amounts; however, completely severing financial ties to revisionary surgery would undermine the premise of bundling, which is providing the highest value original reconstruction. Avoiding repeat visits to the operating room saves money for payers and decreases disruptions in patients’ lives, while simultaneously freeing operating room time for other procedures. Studies on the volume and variation of revisionary surgery are lacking, but could be of assistance in clarifying an episode and duration of breast reconstruction.
Considerations for Defining the Risk Period in Breast Reconstruction
Periods of risk are at the core of bundling (e.g. 30 day, 60 day or 90 day) because it establishes the duration over which the providing health system is exposed to financial risk from costs associated with inpatient and post-acute care (e.g. readmissions, complications, etc.). For CJR, CMMI choose the 90-day window, as this is when both complications and costs plateau (4). It is estimated that 88% of complications following mastectomy without reconstruction occur during the initial hospitalization with a median of two days postoperatively (22). For breast reconstruction, the window of repeat operations and costs is much longer than 30 or even 90 days. In a 2015 study, Fischer et al demonstrated that repeat operations and charges peak around 180 days postoperatively and plateau at nearly 900 days (10). Many of the repeat procedures are not complications, however, and represent revisionary operations (i.e. fat grafting, capsulotomy). Thus, choosing risk windows based on cost-plateaus would generate risk periods between 2–3 years, which is impractical.
A more realistic approach could define the period of risk based on true complications following reconstruction (e.g. hematoma, infected prosthesis), as opposed to elective revisions. If the episode is defined as reconstruction, the period of risk may be upwards of 6–12 months to allow for staged prosthetic reconstruction.
Risk Adjustment
Risk adjustment is necessary for appropriate reimbursement in capitated health systems, such as Medicare Advantage, to mitigate the higher costs associated with caring for patients with medical comorbidities. For bundled payment episodes, the issue is more obscure. CMMI chose not to risk adjust in CJR assuming that providers and institutions were of sufficiently high volume that risk pools were balanced. However, some institutions actually provide care for a disproportionate number of patients with significant comorbidities, and should receive higher reimbursements reflecting their increased cost of care (23). Women undergoing breast reconstruction are increasingly medically complex with higher rates of complications (24), suggesting the merits of risk adjustment in this population.
Further, breast reconstruction faces a unique challenge that deserves particular risk adjustment – radiation. Indications for radiotherapy are expanding and delivery portends an increased risk of complications. Compared to non-irradiated implant based reconstruction, those receiving radiation are 2.5–3.9 times more likely to suffer reconstructive failure (25)(26). Likewise, chemotherapy poses similar increased odds of complications(27). The additional downstream costs of these failures have not been studied and deserve further investigation prior to defining bundled reimbursements. Any additional costs from radiation and chemotherapy should be included in either a flexible risk adjusted payment or an entirely separate bundle.
Considering the liability of hardware failure in lower extremity joint replacement, the CJR bundled payment episode is clearly limited to the initial joint replacement and does not cover subsequent revisions(4). Similarly, the reconstructive surgeon and health system should not bear financial risk for implant failure. Subsequent implant exchanges for ruptures would establish a new episode of care, similar to a revisionary joint replacement.
Associations Between Reconstructive Method and Value
Cost variation between different methods of reconstruction deserves consideration. The only longitudinal cost study to date shows that at three years, healthcare charges are $63,806 for tissue expander based reconstruction vs. $66,882 for autologous based reconstruction (10). This difference was statistically significant, which suggests a bundled payment episode should reimburse more for autologous reconstruction. However, this dataset lacked information on unilateral versus bilateral reconstruction, which limits the utility in estimating payment disparities. Regardless, any differences in reimbursement between the two methods should be reflected in separate bundles with unique benchmark payments, such that providers are not encouraged to perform the higher margin operation (which would likely be prosthetic reconstruction).
In terms of laterality, bilateral reconstructions—whether autologous or prosthetic—should reimburse more than unilateral cases, as commensurate with surgeon effort. The bundle benchmark payment would reflect current schemes for incremental reimbursement in bilateral cases (i.e. the difference in professional fees in current unilateral versus bilateral cases would transfer into the separate bundle payment scheme).
Outcome metrics offer the potential to differentiate quality and give insight into differences in payment bundling between autologous and implant based reconstruction. Unlike CJR which has patient reported outcomes related to ambulation and activities of daily living(4), breast reconstruction outcomes are related to subjective quality of life measures. The BREAST-Q is a validated 100 question survey that indexes quality of life related to breast health following reconstruction (28). Studies show autologous reconstruction achieves a higher score than implant based reconstruction, which is amplified in bilateral reconstruction (29)(30). In a healthcare climate steering towards value, autologous reconstruction may be viewed as the superior method of reconstruction—assuming equitable differences in costs—through gains in patient reported outcomes.
Technologic Innovation and Value
Plastic surgery is fundamentally a problem-based specialty (as opposed to anatomic or disease) that solves inquiry through innovation. In prior decades of medicine, there was little focus on cost or value, which provided an unabated environment for technology generation and advancement. Breast reconstruction has benefitted from this trend as witnessed by the myriad of tools available to accomplish a successful reconstruction. Acellular dermal matrix, remote pulse oximetry monitoring, intraoperative indocyanine green angiography, and preoperative computed tomography angiography are a few examples of technologies used to varying degrees by surgeons to achieve successful reconstruction. In the FFS model, surgeons, institutions, and health systems utilize these technologies without regard to cost. Cost-effectiveness/utility analyses attempt to quantify the benefits of technology in light of greater costs to society. In bundled payment models, it is not society but the health system (e.g. surgeon, surgical center, hospital) that must critically evaluate the utility of technology against cost. There is potential that such constraints could stifle innovation and subsequently limit continual quality improvement. On the other hand, bundled payments create an environment where health systems profit from providing the highest quality care using the least costly technique.
The recent Federal Drug Administration approval of the patient-controlled tissue expander, AeroForm (AirXpanders Inc, California, USA), is an example of novel technology in breast reconstruction that would need to be critically evaluated for value. The incremental cost of the device will be weighed against the impact on total cost of care delivery. For example, fewer patient visits, more rapid expansion, and shorter time to final reconstruction within an episode may argue for total cost savings. However, if the device is simply convenience at an elevated cost, risk bearing health systems may be reluctant to adopt such technology.
Conclusions
Value based care will continue expanding as cost-cutting measures and quality improvements are sought in healthcare redesign. By placing health systems at risk and offering financial incentives, bundled payment models aim to improve value. Regardless of changes to national healthcare policy related to the Affordable Care Act, bundle payment models are implemented through MACRA, which continues to have strong bipartisan support. However, breast reconstruction poses multiple unique factors to bundling that should be evaluated prior to assuming this strategy. Notably, considerations of episodic definition, episodic duration, risk adjustment, and method of reconstruction distinguish this operation from other currently bundled surgeries(31) (32). The plastic surgery community under the leadership of the American Society of Plastic Surgeons has an opportunity to engage in thoughtful conversation on value based contracting and provide a “voice in modern healthcare redesign.” Importantly, patients may benefit from well-designed payment realignment if the benefits of bundling translate into better coordination of care, potentially fewer operations to achieve reconstructive goals, and elevated patient reported outcomes. Research investigating value-based approaches is burgeoning throughout surgery and is needed within breast reconstruction prior to adoption.
Footnotes
Financial Disclosure: None of the authors has a financial interest in any of the products, devices, or drugs mentioned in this manuscript.
References
- 1.Press MJ, Rajkumar R, Conway PH. Medicare’s New Bundled Payments: Design, Strategy, and Evolution. JAMA. 2016. January 12;315(2):131–2. [DOI] [PubMed] [Google Scholar]
- 2.Dummit LA, Kahvecioglu D, Marrufo G, Rajkumar R, Marshall J, Tan E, et al. Association Between Hospital Participation in a Medicare Bundled Payment Initiative and Payments and Quality Outcomes for Lower Extremity Joint Replacement Episodes. JAMA. 2016. September 27;316(12):1267. [DOI] [PubMed] [Google Scholar]
- 3.CMS Bundled Payments for Care Improvement Initiative Models 2–4: Year 2 Evaluation & Monitoring Annual Report August 2016 - bpci-models2–4-yr2evalrpt.pdf [Internet]. [cited 2016 Oct 27]. Available from: https://innovation.cms.gov/Files/reports/bpci-models2-4-yr2evalrpt.pdf
- 4.Centers for Medicare and Medicaid Services. Medicare Program; Comprehensive Care for Joint Replacement payment model for acute care hospitals furnishing lower extremity joint replacement services: final rule. Fed Regist. 2015; 80(226):73273–73554. [PubMed] [Google Scholar]
- 5.Alphs Jackson H, Walsh B, Abecassis M. A Surgeon’s Guide to Bundled Payment Models for Episodes of Care. JAMA Surg. 2016. January 1;151(1):3. [DOI] [PubMed] [Google Scholar]
- 6.Howlader N, Noone AM, Krapcho M, et al. (editors). SEER Cancer Statistics Review, 1975–2013. Table 1.12. National Cancer Institute; Bethesda, MD, http://seer.cancer.gov/csr/1975_2013/, 2016 [Google Scholar]
- 7.Habermann EB, Abbott A, Parsons HM, Virnig BA, Al-Refaie WB, Tuttle TM. Are mastectomy rates really increasing in the United States? J Clin Oncol Off J Am Soc Clin Oncol. 2010. July 20;28(21):3437–41. [DOI] [PubMed] [Google Scholar]
- 8.Albornoz CR, Bach PB, Mehrara BJ, Disa JJ, Pusic AL, McCarthy CM, et al. A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013. January;131(1):15–23. [DOI] [PubMed] [Google Scholar]
- 9.2016 National Clearinghouse of Plastic Surgery Statistics - 2016-plastic-surgery-statistics-report.pdf [Internet]. [cited 2017 Mar 21]. Available from: https://d2wirczt3b6wjm.cloudfront.net/News/Statistics/2016/2016-plastic-surgery-statistics-report.pdf
- 10.Fischer JP, Fox JP, Nelson JA, Kovach SJ, Serletti JM. A Longitudinal Assessment of Outcomes and Healthcare Resource Utilization After Immediate Breast Reconstruction-Comparing Implant- and Autologous-based Breast Reconstruction. Ann Surg. 2015. October;262(4):692–9. [DOI] [PubMed] [Google Scholar]
- 11.Bai G, Anderson GF. Variation in the Ratio of Physician Charges to Medicare Payments by Specialty and Region. JAMA. 2017. January 17;317(3):315–8. [DOI] [PubMed] [Google Scholar]
- 12.Comprehensive Care for Joint Replacement Model ∣ Center for Medicare & Medicaid Innovation [Internet]. [cited 2016 Oct 31]. Available from: https://innovation.cms.gov/initiatives/CJR
- 13.ACS releases primer on bundled payment [Internet]. The Bulletin. 2013. [cited 2016 Oct 27]. Available from: http://bulletin.facs.org/2013/06/acs-releases-primer-on-bundled-payment/
- 14.Albornoz CR, Bach PB, Pusic AL, McCarthy CM, Mehrara BJ, Disa JJ, et al. The influence of sociodemographic factors and hospital characteristics on the method of breast reconstruction, including microsurgery: a U.S. population-based study. Plast Reconstr Surg. 2012. May;129(5):1071–9. [DOI] [PubMed] [Google Scholar]
- 15.Santosa KB, Qi J, Kim HM, Hamill JB, Pusic AL, Wilkins EG. Effect of Patient Age on Outcomes in Breast Reconstruction: Results from a Multicenter Prospective Study. J Am Coll Surg. 2016. December;223(6):745–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Campbell JD, Ramsey SD. The costs of treating breast cancer in the US: a synthesis of published evidence. PharmacoEconomics. 2009;27(3):199–209. [DOI] [PubMed] [Google Scholar]
- 17.Blumen H, Fitch K, Polkus V. Comparison of Treatment Costs for Breast Cancer, by Tumor Stage and Type of Service. Am Health Drug Benefits. 2016. February;9(1):23–32. [PMC free article] [PubMed] [Google Scholar]
- 18.Hughes DR, Jiang M, McGinty G, Shetty SK, Duszak R. An Empirical Framework for Breast Screening Bundled Payments. J Am Coll Radiol. 14:1723.e1. [DOI] [PubMed] [Google Scholar]
- 19.Giordano SH, Niu J, Chavez-MacGregor M, et al. Estimating regimen-specific costs of chemotherapy for breast cancer: Observational cohort study. Cancer. E-published ahead of print October 10, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oncology Care Model. Performance-Based Payment Methodology. Centers for Medicare and Medicaid Services. July 27, 2016. [cited 2016 Oct 31]. Available from: https://innovation.cms.gov/Files/x/ocm-methodology.pdf
- 21.Basta MN, Gerety PA, Serletti JM, Kovach SJ, Fischer JP. A Systematic Review and Head-to-Head Meta-Analysis of Outcomes following Direct-to-Implant versus Conventional Two-Stage Implant Reconstruction. Plast Reconstr Surg. 2015. December;136(6):1135–44. [DOI] [PubMed] [Google Scholar]
- 22.Al-Hilli Z, Thomsen KM, Habermann EB, Jakub JW, Boughey JC. Reoperation for Complications after Lumpectomy and Mastectomy for Breast Cancer from the 2012 National Surgical Quality Improvement Program (ACS-NSQIP). Ann Surg Oncol. 2015. December;22 Suppl 3:S459–469. [DOI] [PubMed] [Google Scholar]
- 23.Ellimoottil C, Ryan AM, Hou H, Dupree J, Hallstrom B, Miller DC. Medicare’s New Bundled Payment For Joint Replacement May Penalize Hospitals That Treat Medically Complex Patients. Health Aff Proj Hope. 2016. September 1;35(9):1651–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Albornoz CR, Cordeiro PG, Pusic AL, McCarthy CM, Mehrara BJ, Disa JJ, et al. Diminishing relative contraindications for immediate breast reconstruction: a multicenter study. J Am Coll Surg. 2014. October;219(4):788–95. [DOI] [PubMed] [Google Scholar]
- 25.Cordeiro PG, Albornoz CR, McCormick B, Hudis CA, Hu Q, Heerdt A, et al. What Is the Optimum Timing of Postmastectomy Radiotherapy in Two-Stage Prosthetic Reconstruction: Radiation to the Tissue Expander or Permanent Implant? Plast Reconstr Surg. 2015. June;135(6):1509–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Farhangkhoee H, Matros E, Disa J. Trends and concepts in post-mastectomy breast reconstruction. J Surg Oncol. 2016. June;113(8):891–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Warren Peled A, Itakura K, Foster RD, Hamolsky D, Tanaka J, Ewing C, et al. Impact of chemotherapy on postoperative complications after mastectomy and immediate breast reconstruction. Arch Surg Chic Ill 1960. 2010. September;145(9):880–5. [DOI] [PubMed] [Google Scholar]
- 28.Pusic AL, Klassen AF, Scott AM, Klok JA, Cordeiro PG, Cano SJ. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009. August;124(2):345–53. [DOI] [PubMed] [Google Scholar]
- 29.Momoh AO, Cohen WA, Kidwell KM, et al. Tradeoffs Associated With Contralateral Prophylactic Mastectomy in Women Choosing Breast Reconstruction: Results of a Prospective Multicenter Cohort. Ann Surg. 2017;266:158164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Matros E, Albornoz CR, Razdan SN, Mehrara BJ, Macadam SA, Ro T, et al. Cost-effectiveness analysis of implants versus autologous perforator flaps using the BREAST-Q. Plast Reconstr Surg. 2015. April;135(4):937–46. [DOI] [PubMed] [Google Scholar]
- 31.Appleby J. UnitedHealthcare Expands Effort To Rein In Rising Costs Of Cancer Treatment [Internet]. Kaiser Health News; 2015. [cited 2016 Nov 21]. Available from: http://khn.org/news/unitedhealthcare-expands-effort-to-rein-in-rising-costs-of-cancer-treatment/ [Google Scholar]
- 32.Creating Physician-Owned Bundled Payments [Internet]. NEJM Catalyst. 2016. [cited 2016 Nov 10]. Available from: http://catalyst.nejm.org/creating-physician-owned-bundled-payments/