Abstract
Objective:
Evidence-based strategies to address vaccine hesitancy are lacking. Personal values are a measurable psychological construct that could be used to deliver personalized messages to influence vaccine hesitancy and behavior. Our objectives were to develop a valid, reliable self-report survey instrument to measure vaccine values based on the Schwartz theory of basic human values, and to test the hypothesis that vaccine values are distinct from vaccine attitudes and are related to vaccine hesitancy and behavior.
Methods:
Parental Vaccine Values (PVV) scale items were generated using formative qualitative research and expert input, yielding 24 items for testing. 295 parents of children aged 14-30 months completed a self-report survey with measures of Schwartz’s global values, the PVV, vaccine attitudes, and vaccine hesitancy. Factor analysis was used to determine vaccine values factor structure. Associations between vaccine values, vaccine attitudes, vaccine hesitancy, and vaccination behavior were assessed using linear and logistic regression models. Late vaccination was assessed from electronic medical records.
Results:
A six-factor structure for vaccine values was determined with good fit (RMSEA=0.07, Bentler’s CFI=0.91) with subscales for Conformity, Universalism, Tradition, Self-Direction, Security- Disease Prevention, and Security- Vaccine Risk. Vaccine values were moderately associated with Schwartz global values and vaccine attitudes, indicating discriminant validity from these constructs. Multivariable linear regression showed vaccine hesitancy was associated with vaccine values Conformity (partial R2=0.10) and Universalism (0.04) and vaccine attitudes Vaccine Safety (0.52) and Vaccine Benefit (0.16). Multivariable logistic regression showed that late vaccination was associated with vaccine value Self-direction (OR=1.80, 95% CI: 1.26-2.65) and vaccine attitude of Vaccine Benefit (OR=0.44, 95% CI: 0.32-0.60).
Conclusions:
The PVV scale had good psychometric properties and appears related to but distinct from Schwartz global values and vaccine attitudes. Vaccine values are associated with vaccine hesitancy and late vaccination and may be useful in tailoring future interventions.
Introduction
Development of the childhood immunization program has been a remarkable public health achievement that has led to dramatic decreases in rates of vaccine preventable diseases such as poliomyelitis, measles, diphtheria, and pertussis, which led to thousands of deaths every year before widespread immunization uptake1,2.3 However, the individual and public health benefits of vaccination are threatened by increasing numbers of parents who choose to delay or forgo vaccination for their children.4,5 As many as 77% of parents have some concerns about vaccines, including parents who still choose to vaccinate.6 The term ‘vaccine hesitancy’ refers to the concerns that parents have even when they vaccinate their children fully, as well as those concerns that lead some parents to delay or refuse vaccines.7 Geographic clusters of under-immunization related to vaccine hesitancy increase the risk of disease outbreaks as infections spread more easily among unprotected individuals.8-10
Determinants of vaccine hesitancy include knowledge, beliefs, and attitudes about risks and benefits of vaccines, the perceived strength of the evidence base, trust in the healthcare system, and communications from the media and influential leaders from anti- and pro-vaccination lobbies.11 Interventions designed to address vaccine hesitancy have shown limited effectiveness and have mostly evaluated changes in attitudes or intentions rather than vaccination behavior.9,12-17 New research and intervention paradigms are therefore needed to address vaccine hesitancy. One proposed paradigm involves appealing to personal values as a strategy to promote childhood vaccination. There is growing evidence that aligning messages with an individual’s values can improve communication of scientific ideas18 and promote health behavior change.19-23 For example, pairing affirmation of values with a potentially threatening health message related to sedentary behavior and physical activity has shown changes in the neural response to that message along with subsequent positive behavior change.24-26 There have been recent calls to include values in the development, implementation, and communication of evidence-based medicine practices in general,27 and with respect to vaccination specifically.28-32 One recent survey showed differences in personal values to be associated with acceptance or refusal of recommended vaccines.33
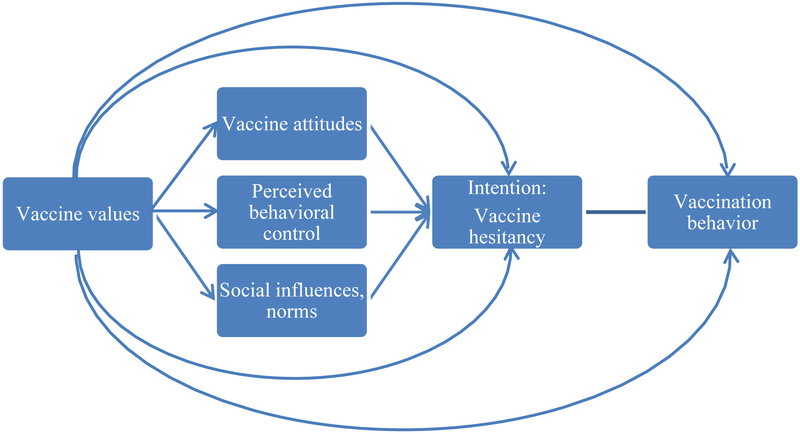
Values are personal priorities and guiding principles for one’s life that transcend specific situations, represent desired goals, and serve as criteria for evaluating decisions.34-36 According to the Schwartz theory of basic human values, there are ten universal values domains recognized across cultures, described in part in Table 1.34 For this paper, Schwartz values will be referred to as global values. Theoretically, values (strongly-held guiding principles for decision making and behavior), and attitudes (judgments of the favorability of the expected outcomes of particular decisions and behaviors) are distinct but related constructs.37 As described in the value-attitude-behavior hierarchy model38, values are known to influence attitude formation and behavior across cultures and domains, such as recycling, consumer behavior, and alcohol consumption among college students.39,40 We propose a similar framework (Figure 1) building upon the theory of planned behavior41 and suggesting that values influence vaccine attitudes, which in turn influence intentions (which we operationalize as vaccine hesitancy) and behavior.
Table 1:
Schwartz Basic Human Value Domainsa and Hypothesized Factor Structure for Parental Vaccine Values Items
| Domain | Description | Parental Vaccine Values Items a priori organization (hypothesized factor structure) |
|---|---|---|
| Universalism | Promoting the welfare of all people and nature (equality, social justice, protecting the environment) |
|
| Benevolence | Promoting the welfare of people you are close to (helpfulness, loyalty, honesty, forgiving) |
|
| Conformity | Controlling impulses to fulfill others’ expectations (self-discipline, obedience) |
|
| Tradition | Maintaining traditions (moderation, respect for tradition, devout) |
|
| Security | Safety and security of self, family, and nation (family security, social order, clean) |
|
| Self-direction | Independence of thought and action (creativity, freedom, independent, curious) |
|
Schwartz values domains of Power, Achievement, Hedonism, and Stimulation were excluded from development of vaccine values items.
Items excluded from final vaccine values factor solution.
Figure 1:
Model of parental vaccine values, vaccine attitudes, hesitancy and behavior
Framing vaccine recommendation messages based on values, rather than simply providing knowledge-correcting information, may help parents perceive the messages as more aligned with their priorities. As a result, parents may be more open to incorporating new information into their existing attitudes. For instance, an individual who values universalism (protecting one’s community) might respond well to a message concerning the benefits of vaccination with regard to herd immunity. Conversely, someone who values self-direction (making thoughtful decisions based on one’s own information gathering) may respond well to a message encouraging review of research summaries and testimonials.
The overarching objective of this project is to measure parental vaccine values with the intent of later testing effectiveness of vaccine-promotion messages tailored to these values. The view of values as guiding principles that apply to one’s decision making and attitudes across contexts35 suggests that someone who values self-direction would tend to want to exert individual choice in decision making for everything from tonight’s dinner menu to national policy. Thus, a global measure of values may be appropriate for the purpose of a values-tailored intervention for vaccine promotion. Yet one’s global values may not apply equally across all contexts (e.g., self-direction values are expected to matter less than hedonism values when it comes to dessert – I’ll eat that delicious apple pie, even if that’s the only dessert option tonight). To better understand which values matter most when it comes to making decisions about childhood vaccination, it may be important to measure values specific to the context of vaccination in addition to global values.
While measures of global values have been established34, there are no existing, validated measures of vaccine-specific values. The purpose of this investigation was to develop a valid, reliable self-report measure of parental values for childhood vaccination (i.e., “parental vaccine values”), based on the Schwartz values framework. We hypothesized that vaccine-specific values are measurable and are associated with but distinct from global values. To test this hypothesis, we: 1) developed a set of items reflecting parental vaccine values using insights from prior qualitative work and expert input; 2) evaluated the factor structure and reliability; and 3) assessed convergent, discriminant, and predictive validity of the parental’ vaccine values instrument relative to global values, vaccine attitudes, vaccine hesitancy, and late vaccination behavior.
Methods
Participants and Procedures
Parents of Kaiser Permanente Colorado (KPCO) patients 14-30 months of age were invited to participate in a web-based survey including measures of global and vaccine-related values, vaccine attitudes, vaccine hesitancy, and basic demographics. Inclusion criteria included child enrollment in KPCO from 2 through 12 months of age and at least one outpatient visit in the first year of life (to ensure accurate capture of vaccination data in the medical record). The survey was administered via Research Electronic Data Capture (REDCap)42 and SurveyGizmo® (Boulder, CO) online survey systems. Respondents received a $30 gift card upon completion of the survey. This study was approved by the Kaiser Permanente Colorado Institutional Review Board.
An initial convenience sample of 120 participants was recruited January-March 2015 and these survey responses were used for exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) for both vaccine attitudes and vaccine values. A second convenience sample of 175 participants was recruited July-October 2015 and these responses were used for a second round of confirmatory factor analysis for both vaccine attitudes and vaccine values. Both samples completed identical surveys for global values, vaccine values, vaccine attitudes, and vaccine hesitancy; results from both samples are reported here. To evaluate the model fit, root mean square error of approximation (RMSEA) and Bentler’s comparative fit index (CFI) were assessed. RMSEA ranges from 0 to 1, with a smaller value indicating a better model (≤0.08)43; and Bentler’s CFI ranges from 0 to 1, with a higher value indicating a better model (≥ 0.90).44 The factor structures for vaccine attitudes and vaccine values from the first and second samples were evaluated for measurement invariance by comparison of fit statistics (RMSEA and Bentler’s CFI) to justify combination of the two samples for subsequent analyses. Invariance was evaluated through the strict test (holding factor loadings, intercepts, variances, and covariances equal).45
Measures
Global values were measured using Schwartz’s 40-item Portrait Values Questionnaire (PVQ), which measures values across ten domains, as shown in Table 1.35 Parental vaccine values were measured with 24 new items that were developed independently from the Schwartz global values by incorporating prior qualitative work in this population46, literature review, and expert input by two immunization researchers and one health psychologist on the research team. These vaccine values items were further refined by review and comments provided by an expert panel of three immunization researchers and one social psychologist who were not part of the initial research team. Parental vaccine value items were organized a priori into subscales predicted to reflect domains from Schwartz’s global value theory (Table 1). Some Schwartz global value domains were not reflected in this a priori organization of vaccine value items as they did not have plausible association with parental vaccine values (for example hedonism was not considered as a parental vaccine value due to lack of face validity). Global value and vaccine value items were assessed using six-point Likert-type scales with responses ranging from1= “very much like me” to 6= “not at all like me” for global value items and 1 = “very important” to 6 = “not at all important” for vaccine value items.
Vaccine attitudes, vaccine hesitancy, and late vaccination behavior were also assessed. Vaccine attitudes were measured using 13 items, shown in Table 2, including 11 items based on previous work6,47-53 as well as 2 items added for this study to reflect balance between risks and benefits of vaccines. Vaccine attitudes items were assessed using a five-point Likert scale with responses ranging from 1 = “strongly disagree” to 5 = “strongly agree”. Higher scores indicate stronger agreement with the vaccine attitude item. Some item scores were reverse-coded for analysis so that higher scores indicated endorsement of pro-vaccine attitudes.
Table 2:
Vaccine Attitudes Factor Structure and Cronbach’s alpha from Combined Sample
| Factor | Vaccine Attitudes Items | Cronbach’s alpha |
|---|---|---|
| Vaccine Safety |
|
0.89 |
| Vaccine Benefit |
|
0.84 |
Vaccine hesitancy was measured using a validated, five-item, short-form of the Parental Attitudes about Childhood Vaccination survey 48,54 that identifies vaccine-hesitant parents and is associated with late vaccination.55 Hesitancy score was calculated as average of Likert-scale responses with the possible calculated score ranging from 1 to 5 where 1 is the most hesitant.
Late vaccination behavior was measured retrospectively from electronic medical records data using the “days undervaccinated” metric.5 Days undervaccinated is a continuous metric that measures differences between the time when vaccine doses were actually administered and when doses should have been administered according to the Advisory Committee on Immunization Practices (ACIP) schedule56. For example, the first dose of DTaP (diphtheria, tetanus and acellular pertussis) vaccine is due at age two months but is not considered late until age 92 days. Days undervaccinated for this dose begin accruing on day 93. Children with greater than zero cumulative days undervaccinated at one year of age were considered late on vaccination. Late vaccination behavior was dichotomized as on time or late due to the non-normal distribution of days undervaccinated. Days undervaccinated demonstrates heavily right-skewed distribution, with the majority of subjects being zero days late, across most populations when the large majority of children are fully vaccinated.
Demographics were collected by self-report and included maternal age, race, ethnicity, education, employment status, income, number of children, and age and sex of the child.
Data Analysis
Descriptive statistics were generated for global values, vaccine values, vaccine attitudes, vaccine hesitancy, late vaccination, and demographic variables.
Confirmatory and exploratory factor analyses44 were performed to examine the factor structure of vaccine value items for the first sample (n=120). Initial CFA was performed with the first sample to assess fit of the hypothesized factor structure that organized vaccine value items into six subscales based on Schwartz global value domains. RMSEA and Bentler’s CFI were used to assess the fit of the factor model in CFA. Using data from the first sample of parents surveyed, exploratory factor analysis (EFA) was then performed using promax oblique rotation to find the factor structure with the best fit.
We used a factor loading cutoff of ≥0.3 to determine which items belonged to which factor.48,57 When an item loaded on more than one factor, it was placed under the factor in which the loading was highest. We determined the internal consistency or reliability of each factor using Cronbach's alpha.58 A Cronbach’s alpha value of ≥0.70 is generally considered acceptable. To enhance internal consistency within the scale and as a method of item reduction, we reviewed the Cronbach’s alpha and removed those items that reduced the Cronbach’s alpha for each factor and excluded them from the final factor solution derived from the EFA.59,60 Using the second sample (n=175 unique respondents), CFA was then performed using RMSEA and CFI to measure the fit of the factor solution derived from EFA of the first sample. The vaccine values factor structures from the first and second samples were evaluated for measurement invariance by comparison of fit statistics (RMSEA and Bentler’s CFI) to justify combination of the two samples for subsequent analyses.45 CFA for vaccine values was then repeated with the combined sample (n=295), again assessing the factor structure with RMSEA and Bentler’s CFI. To assess convergent and discriminant validity between vaccine values and global values, Spearman rank correlation was used to measure correlation between vaccine values factors and Schwartz global value domains using both the first sample and the combined sample. Spearman correlations were used to protect inference against departures from normality in distribution of data.
Exploratory and confirmatory factor analyses were used to examine the factor structure of vaccine attitude items for the first sample. Cronbach’s alpha was again used to examine item association within each factor. CFA was performed using the second sample to measure the fit of the vaccine attitudes factor solution derived from EFA of the first sample. Measurement invariance was assessed between the first and second sample for the vaccine attitudes factor structure by comparing fit statistics (RMSEA and Bentler’s CFI).
The first and second samples were combined (n=120+175=295) to improve power for further analyses. We assessed convergent, discriminant, and predictive validity of parental vaccine values as related to vaccine attitudes, vaccine hesitancy, and late vaccination. To assess convergent and discriminant validity between vaccine values and vaccine attitudes, Spearman rank correlations were used to measure correlation between vaccine values scores and vaccine attitudes scores. Spearman correlations were also reviewed in considering discriminant validity, noting that variables with higher Spearman coefficients are more highly correlated and less likely to have discriminant validity. To assess both discriminant validity of vaccine values related to vaccine attitudes and predictive validity of vaccine values related to vaccine hesitancy, multivariable linear regression was used to examine the association of vaccine attitudes and vaccine values with vaccine hesitancy. Model reduction was performed with a cutoff of p < 0.05 for inclusion of parameters in the final multivariable model. For this multivariable linear regression model, vaccine hesitancy, vaccine values, and vaccine attitudes were measured as continuous variables. To further assess both discriminant validity of parental vaccine values related to vaccine attitudes and predictive validity of vaccine values related to vaccination behavior, univariable and multivariable logistic regression were used to examine the association of vaccine attitudes and vaccine values with late vaccination behavior. Model reduction was again performed with a cutoff of p < 0.05 for inclusion of parameters in the final multivariable model. For this multivariable logistic regression model, late vaccination was a dichotomous outcome while vaccine values and vaccine attitudes were measured as continuous variables. For linear and logistic regression analyses, vaccine attitudes scales were reverse-coded to allow for intuitive interpretation of correlations.
In EFA and CFA models used to determine the values and attitudes factor structures, fewer than 10% of respondents were dropped from analysis due to item nonresponse. Adequate non-missing items were available for computation of vaccine values and attitudes scales in all respondents, so measures of these scales are reported for all respondents. In the vaccine behavior models, fewer than 10% of respondents in the combined sample were dropped for a missing outcome. Respondents with missing data were dropped rather than imputing missing values to avoid making assumptions about predicted responses during the development of these new scales. Data management and analyses (with the exception of CFA) were performed using SAS software, version 9.4. CFA models were performed in R,61 version 3.3.2, using the lavaan package.62
Results
Sample Characteristics
Response rates were 28% (120/428) and 45% (175/390) for the first and second samples respectively. Respondent parent and child demographic characteristics are presented in Table 3. Twenty-four percent of respondents from the combined sample (70/295) had children who were defined as late on vaccinations according to medical records. Mean vaccine hesitancy score was 3.7 [Standard deviation (SD)=0.8] on a scale from one to five where one is most hesitant. Compared with the first sample, participants from the second sample had children who were slightly older and were less likely to have late vaccination status.
Table 3:
Characteristics of Survey Respondents
| Sample 1 N=120 |
Sample 2 N=175 |
Combined Sample N=295 |
|
|---|---|---|---|
| Parental age in years Mean (SD) | 34 (5) | 34 (5) | 34 (5) |
| Child age in daysa Mean (SD) | 542 (69) | 721 (33) | 642 (103) |
| Education % (n) | |||
| Some college or less | 27% (33) | 16% (28) | 21% (61) |
| College | 73% (87) | 84% (147) | 79% (234) |
| Employment | |||
| Employed part-time or full-time | 74% (89) | 74% (129) | 74% (218) |
| Unemployed | 1% (1) | 1% (1) | 1% (2) |
| Stay at home parent | 25% (30) | 25% (43) | 25% (73) |
| Student | . | 1% (1) | 0% (1) |
| Prefer not to answer | . | 1% (1) | 0% (1) |
| Income | |||
| Missing | 5% (6) | 6% (10) | 5% (16) |
| $80,000 and less | 43% (51) | 38% (67) | 40% (118) |
| More than $80,000 | 53% (63) | 56% (98) | 55% (161) |
| Race/Ethnicity | |||
| White, non-Hispanic | 73% (87) | 85% (148) | 80% (235) |
| Hispanic | 21% (25) | 9% (15) | 14% (40) |
| All other | 7% (8) | 7% (12) | 7% (20) |
| More than one child | 63% (75) | 63% (110) | 63% (185) |
| Late vaccination statusa,b | |||
| Late | 33% (40) | 17% (30) | 24% (70) |
| Missing | . | 13% (23) | 8% (23) |
| Vaccine hesitancy scorec Mean (SD) | 3.6 (0.7) | 3.8 (0.7) | 3.7 (0.8) |
Compared with the sample 1, participants from the sample 2 had children who were slightly older and were less likely to have late vaccination status.
Vaccination status was not evaluable for 23 participants (8%) due to disenrollment of children from the managed care health plan between 2 and 12 months of age.
Vaccine hesitancy score measured on scale 1-5 where 1 is most hesitant.
Vaccine Values Preliminary Confirmatory Factor Analysis
CFA using the first sample (n=120) was performed by grouping the 24 parental vaccine values items into the hypothesized six subscales based on Schwartz global value domains. This hypothesized factor structure showed poor fit to the data (RMSEA 0.12 [90% CI: 0.11-0.12]; Bentler’s CFI 0.66).
Vaccine Values Exploratory Factor Analysis
Using the scree plot of the eigenvalues, EFA suggested an alternate six factor model. Loading scores were assessed for all items and the lowest was 0.30. After review of those vaccine values items that lowered the Cronbach’s alpha, four items that lowered the Cronbach’s alpha within each construct (by 0.2 – 0.5) were dropped. The remaining 20 vaccine values items and the resulting six-factor solution are shown in Table 4 along with factor loading scores and Cronbach’s alpha values for each factor. The factor loading scores of items included in the final model were each ≥0.37. Fit of the resulting factor structure was measured by CFA and was found to be adequate (RMSEA 0.08 [90% CI 0.06-0.09], Bentler’s CFI 0.90).
Table 4.
Vaccine Values Factor Structure from Exploratory Factor Analysis (Sample 1) and Confirmatory Factor Analysis (combined Sample)
| Sample 1: EFA | Combined sample: CFA | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Vaccine Value Factor |
Universalism | Security- Disease Prevention |
Security- Vaccine Risk |
Tradition | Self- direction |
Conformity | Universalism | Security- Disease Prevention |
Security- Vaccine Risk |
Tradition | Self- direction |
Conformity | |
| Cronbach’s alpha | 0.87 | 0.85 | 0.80 | 0.76 | 0.70 | 0.63 | 0.86 | 0.74 | 0.73 | 0.79 | 0.66 | 0.62 | |
| Survey Item |
Standardized Factor Loading Scores | ||||||||||||
| Factor 1 | B1 | 0.99 | −0.12 | 0.03 | 0.01 | −0.07 | −0.02 | 0.78 | . | . | . | . | . |
| B2 | 0.92 | 0.01 | −0.01 | 0.06 | 0.08 | −0.10 | 0.81 | . | . | . | . | . | |
| U1 | 0.92 | 0.01 | 0.08 | 0.02 | −0.09 | −0.04 | 0.75 | . | . | . | . | . | |
| U2 | 0.63 | 0.03 | −0.24 | 0.15 | 0.36 | 0.05 | 0.59 | . | . | . | . | . | |
| U3 | 0.40 | 0.05 | 0.01 | −0.33 | 0.23 | 0.29 | 0.30 | . | . | . | . | . | |
| C4 | 0.30 | 0.16 | −0.07 | 0.14 | 0.29 | 0.17 | . | . | . | . | . | . | |
| Factor 2 | Se1 | −0.09 | 0.91 | −0.03 | −0.03 | −0.05 | 0.02 | . | 0.26 | . | . | . | . |
| Se2 | 0.05 | 0.84 | 0.00 | 0.03 | 0.06 | −0.10 | . | 0.22 | . | . | . | . | |
| Se3 | 0.05 | 0.67 | 0.00 | 0.04 | −0.22 | 0.04 | . | 0.25 | . | . | . | . | |
| B3 | −0.01 | 0.39 | 0.13 | −0.16 | 0.19 | 0.07 | . | . | . | . | . | . | |
| Factor 3 | Se4 | 0.09 | 0.00 | 0.81 | −0.02 | −0.10 | −0.07 | . | . | 0.71 | . | . | . |
| Se5 | −0.07 | 0.14 | 0.68 | 0.10 | 0.10 | 0.03 | . | . | 0.84 | . | . | . | |
| Se6 | −0.02 | −0.04 | 0.56 | 0.02 | 0.34 | 0.07 | . | . | 0.75 | . | . | . | |
| Sd4 | −0.09 | −0.09 | 0.45 | 0.09 | 0.17 | 0.08 | . | . | . | . | . | . | |
| Factor 4 | T1 | −0.01 | −0.01 | −0.01 | 0.71 | −0.08 | −0.08 | . | . | . | 1.35 | . | . |
| T2 | 0.07 | 0.00 | 0.06 | 0.70 | −0.08 | 0.23 | . | . | . | 1.21 | . | . | |
| T3 | 0.06 | −0.02 | 0.14 | 0.66 | 0.07 | 0.07 | . | . | . | 1.18 | . | . | |
| Factor 5 | Sd1 | −0.01 | −0.11 | 0.04 | −0.10 | 0.65 | 0.07 | . | . | . | . | 0.60 | . |
| Sd2 | 0.00 | −0.02 | 0.26 | 0.00 | 0.62 | −0.12 | . | . | . | . | 1.23 | . | |
| Se7 | 0.33 | 0.09 | 0.15 | −0.05 | 0.47 | −0.11 | . | . | . | . | . | . | |
| Factor 6 | C1 | −0.15 | −0.06 | −0.01 | 0.19 | 0.13 | 0.58 | . | . | . | . | . | 0.25 |
| C2 | 0.16 | 0.06 | 0.02 | 0.10 | −0.08 | 0.51 | . | . | . | . | . | 0.66 | |
| C3 | 0.35 | 0.04 | −0.01 | −0.12 | −0.11 | 0.45 | . | . | . | . | . | 0.69 | |
| Sd3 | 0.34 | −0.01 | 0.07 | −0.11 | −0.21 | 0.37 | . | . | . | . | . | 0.55 | |
For Sample 1, bolded text indicates the standardized factor loading score for each item that was retained in the six factor parental vaccine values structure. For the combined sample, factor loading scores shown include loading scores <0.3 for several items, however Cronbach’s alpha for each factor and overall fit statistics in the combined sample (RMSEA 0.07 [0.06-0.08]; Bentler’s CFI 0.91) confirmed reliability of each factor and good fit of the six factor structure.
Vaccine Values Final Confirmatory Factor Analysis
CFA of the second sample (n=175) using the 20 vaccine values items identified through EFA generally supported the six-factor structure arrived at by EFA of the initial sample (RMSEA 0.08 [0.06-0.09]; Bentler’s CFI 0.87). Reliability of factors was similar across samples. CFA was repeated with the combined sample (n=295, Table 4) using 20 vaccine values items and supported the six-factor structure (RMSEA 0.07 [0.06-0.08]; Bentler’s CFI 0.91). The six factor parental vaccine values structure had acceptable variance inflation factor scores (maximum VIF=2.18, all others <2) that did not suggest multicollinearity. Two factors were most highly correlated with the global Security domain and the other four factors correlated with global values domains of Universalism, Tradition, Self-direction, and Conformity (Table 5). Vaccine values items that were hypothesized to represent the global values domains of Universalism and Benevolence formed one factor that was most highly correlated with the global value Universalism domain based on the factor loadings and so were combined into one Universalism domain. The two vaccine values factors that both correlated with the global value Security domain represented distinct factors based on the model and were renamed ‘Security- Disease Prevention’ and ‘Security- Vaccine Risk’ based on the content of the vaccine values items that comprised each factor.
Table 5:
Univariable Relationships among Vaccine Values, Vaccine Attitudes, Vaccine Hesitancy, and Vaccination Behavior (combined sample, n=295)
| Variable | Mean (SD) |
Vaccine Attitude Safety |
Vaccine Attitude Benefit |
Highest Correlated PVQ factor (Spearman correlation) |
Vaccine Hesitancy: Linear regression Parameter estimate (p value) ‡ |
Late Vaccination: Logistic regression OR (95% CI) |
|---|---|---|---|---|---|---|
| Spearman’s rank correlation† | ||||||
| Vaccine Value Universalism | 1.8 (0.7) |
0.21** | 0.30** | Universalism (0.35)** |
−0.14* | 0.72 (0.55,0.93) |
| Vaccine Value Security-Disease Prevention | 1.1 (0.3) |
0.28** | 0.39** | Security (0.20)** |
−0.26** | 0.66 (0.50,0.84) |
| Vaccine Value Security-Vaccine Risk | 2.2 (0.9) |
−0.38** | −0.26** | Security (0.33)** |
0.27** | 1.55 (1.16,2.13) |
| Vaccine Value Tradition | 4.4 (1.4) |
−0.42** | −0.35** | Tradition (0.62)** |
0.26** | 1.28 (0.97,1.68) |
| Vaccine Value Self-direction | 2.3 (1.1) |
−0.33** | −0.17* | Self-direction (0.28)** |
0.28** | 1.98 (1.43,2.84) |
| Vaccine Value Conformity | 2.8 (0.7) |
0.31** | 0.25** | Conformity (0.24)** |
−0.32** | 0.57 (0.43,0.76) |
| Vaccine Attitude Safety | 3.5 (0.8) |
. | . | . | −0.63** | 0.44 (0.32,0.59) |
| Vaccine Attitude Benefit | 4.5 (0.6) |
. | . | . | −0.52** | 0.42 (0.30,0.56) |
p<0.01,
p<0.001
For Spearman’s rank correlations between vaccine attitudes and vaccine values scores, negative and positive correlations are as represented in the table
For linear regression of vaccine hesitancy, a positive parameter estimate for vaccine values or vaccine attitudes scores indicates that endorsing the vaccine value or attitude is associated with increased vaccine hesitancy.
From the six-factor structure, mean scores in the combined data (n=295) for each vaccine values factor were calculated. Vaccine Value Security- Disease Prevention was the most highly rated value at 1.1 (where 1 is very important and 6 is not important at all), followed by Universalism at 1.8, Security-Vaccine Risk at 2.2, Self-direction at 2.3, Conformity at 2.8 and lastly Tradition at 4.4 (Table 5).
Vaccine Attitudes Exploratory and Confirmatory Factor Analyses
EFA of vaccine attitudes items suggested a two-factor solution, corresponding to vaccine safety (7 items) and vaccine benefits (6 items). A CFA for the combined sample supported the two-factor structure (RMSEA 0.08 [0.06-0.09]; Bentler’s CFI 0.94).
Combining First and Second Sample Data
The factor structures for both vaccine attitudes and vaccine values showed acceptable measurement invariance.45 For values, the configural model had a CFI below the acceptable limit (0.884), however the RMSEA remained acceptable (0.076) and the maximum increase (from the configural to the weak, strong and strict constraints) was 0.002. The configural model for attitudes had a CFI of 0.932 and an RMSEA of 0.084. Only the CFI showed any degradation, changing by −0.001 when the configural model was compared against the strict. Given these results the two samples were combined for subsequent analyses.
Vaccine Values Convergent and Discriminant Validity
Univariable relationships among vaccine values, vaccine attitudes, vaccine hesitancy, and late vaccination are shown in Table 5. Parental vaccine values scores were correlated as expected with corresponding global values scores (demonstrating convergent validity, Spearman correlations shown in Table 5). With the exception of Tradition, the Spearman correlation coefficients for each parental vaccine value was <0.5, demonstrating moderate correlation and suggesting discriminant validity between parental vaccine values and global values. Similarly, as shown in Table 5, vaccine values were correlated with vaccine attitudes and had Spearman correlation coefficients of <0.5 for each parental vaccine value and attitude association. These results indicate discriminant validity among parental vaccine values and vaccine attitudes as well. Spearman correlations among each of the six parental vaccine values are presented in Supplemental Table 1 and each of these correlations was <0.5.
Vaccine Values Predictive Validity
Endorsing certain parental vaccine values (Universalism, Conformity, and Security-Disease Prevention) was associated with more positive vaccine attitudes, while endorsing other vaccine values (Security- Vaccine Risk, Self-direction, and Tradition) was associated with more negative vaccine attitudes (Table 5).
Multivariable linear regression revealed that two of the vaccine values (Conformity and Universalism) and both vaccine attitudes were significantly associated with vaccine hesitancy (Table 6). The reduced multivariable model accounted for 77% of the variance in vaccine hesitancy (adjusted R2=0.77). Endorsement of the vaccine value of Conformity and vaccine attitudes of Safety and Benefit were associated with decreased vaccine hesitancy, whereas endorsement of the vaccine value of Universalism was associated with increased vaccine hesitancy.
Table 6:
Multivariable linear regression of vaccine hesitancy on vaccine values and vaccine attitudes
| Combined sample R2=0.771 |
||
|---|---|---|
| Variable | Parameter estimate | Partial R2 |
| Vaccine Value Conformity | −0.136 | 0.098 |
| Vaccine Value Universalism | 0.085 | 0.042 |
| Vaccine Attitude Safety | −0.481 | 0.520 |
| Vaccine Attitude Benefit | −0.204 | 0.159 |
Reduced multivariable model based on initial inclusion of six vaccine values (Conformity, Security-Disease Prevention, Security- Vaccine Risk, Self-direction, Tradition, and Universalism) and two vaccine attitudes (Safety and Benefit). A positive parameter estimate for vaccine values or vaccine attitudes indicates that endorsement of that value or attitude as important is associated with increased vaccine hesitancy.
Univariable logistic regression showed that parental vaccine values of Security- Vaccine Risk, and Self-Direction were each associated with increased odds of late vaccination. Parental vaccine values of Security- Disease Prevention, Universalism, and Conformity as well as vaccine attitudes of Vaccine Safety and Vaccine Benefit were each associated decreased odds of late vaccination. The reduced multivariable model showed that the vaccine value of Self-Direction remained significantly associated with increased odds of late vaccination (OR=1.80, 95% CI: 1.26-2.65) and the attitude Vaccine Benefit remained significantly associated with decreased odds of late vaccination (OR=0.44, 95% CI: 0.32-0.60).
Discussion
The purpose of this study was to develop a valid, reliable measure of parental values with regard to childhood vaccination. The resulting Parental Vaccine Values (PVV) scale is a twenty-item self-report survey with 6 subscales corresponding to, but distinct from, 5 domains from the Schwartz theory of basic human values. The factor structure of parental vaccine values was confirmed in two independent samples of parents with vaccine-eligible children and in a sample combining the two groups. Results from this combined sample of parents show the PVV subscales are valid (have convergent, discriminant, and predictive validity and a factor structure consistent with existing values theory) and internally consistent (Cronbach’s alphas for each subscale > 0.60). Notably, vaccine values were associated with, but distinct from, Schwartz global values 34 and vaccine attitudes. Of the six vaccine values subscales, three were associated with pro-vaccination attitudes (Conformity, Security- Disease Prevention, and Universalism), and three were associated with anti-vaccination attitudes (Security- Vaccine Risk, Self-Direction, and Tradition).
Studies related to other health behaviors have focused on affirmation of existing global personal values paired with an intervention related to a specific health behavior.19,24,63 However, adapting global values to a specific health behavior context, such as vaccines, may be favorable if those context-specific values are more strongly related to the downstream attitudes and behaviors of interest. Several Schwartz global values including Hedonism, Achievement, and Stimulation lacked face validity in the vaccination context. We also found the Schwartz global Security value was represented by two distinct vaccine values factors. While both Security-vaccine safety and Security- disease prevention vaccine values were rooted in global Security values, each showed opposite associations with vaccine attitudes, hesitancy, and behavior. This suggests that global values may lack some nuance for understanding values in the context of vaccines. Thus, we chose to focus on vaccine-specific values as potential factors for tailoring interventions.
Vaccine values of Conformity and Universalism were associated with positive attitudes toward vaccination; Conformity was also associated with decreased vaccine hesitancy. Conformity is valuing obedience to authority, doing what is expected, and politeness; Universalism encompasses concepts of unity, equality, and social justice. These findings suggest that pro-vaccination arguments based on recommendations from experts and concerns about protecting those who are too young or immunocompromised to receive vaccines themselves may be most effective at increasing positive vaccine attitudes among those who value universalism and conformity. Oddly, high endorsement of the vaccine value Universalism was also associated with increased vaccine hesitancy in the multivariable model. It seems counter-intuitive that parents who value Universalism would also have increased vaccine hesitancy and this relationship needs further exploration with future studies of parental vaccine values.
Conformity reflects the individual’s relationship with society and a concept of social norms. With mixed success, other researchers have used social norms to influence behaviors such as smoking, drinking and energy consumption by providing participants with information about behaviors of peers.64,65 These studies did not, however, incorporate any evaluation or recognition of individual values. Our finding that conformity is associated with positive vaccine attitudes and decreased hesitancy supports the notion that appealing to social norms (as a reflection of conformity) may improve the effectiveness of communications and interventions promoting vaccination.
In contrast to the value of Conformity, Self-Direction reflects a value for making one’s own decisions based on one’s own efforts to gather and interpret information. In the context of vaccinations, this may include doing research for one’s self and maintaining control over the health and care of one’s children. Higher endorsement of the vaccine value Self-Direction was associated with more negative vaccine attitudes and late vaccination behavior. Strategies to address vaccine hesitancy through correction of knowledge deficits either with lectures from physicians or written material may conflict with the value of Self-Direction. Indeed, the self-direction value may reflect an increased need for autonomy support, as defined by self-determination theory.21 That is, healthcare providers of children whose parents highly value autonomy support may need to pay special attention to eliciting and respecting individual preferences and perspectives in the process of decision making, rather than trying to persuade parents on the basis of scientific evidence and expert recommendations alone. An area for future research is testing whether tailoring the presentation of vaccine information based on parental vaccine values impacts the effect that the information communicated has on attitudes and behaviors.
Most parents in this study endorsed the vaccine value Security- Disease Prevention, in that parents nearly universally valued preventing their child from having a dangerous disease. In contrast, there was more variability in endorsement of the Security- Vaccine Risk value, such that some parents were more cautious about doing potential harm to their child through vaccination. The Security – Vaccine Risk value is similar to the concept of a commission bias (bias towards avoiding harm due to some action taken), whereas Security- Disease Prevention is similar to the concept of an omission bias (bias towards avoiding harm due to some action not taken).66 Other studies have observed the role of preference for omission bias in perceptions of MMR and pertussis vaccines.67,68 The tension between commission and omission biases may relate to perception of future regret, which leads some parents to choose to vaccinate to avoid regret of their child becoming ill and others to forgo vaccination to avoid regret of their child suffering an adverse effect from a vaccine.69 These moral dilemmas are not easily resolved through rational argument. Many studies have identified vaccine safety as a common parental concern 13,47,70 and future study of vaccine values may reveal ways to address these concerns beyond providing factual information about vaccine safety, and instead focusing on the affective or emotional aspects of vaccine-decision making.
Multivariable analysis including vaccine values and attitudes showed that attitudes controlling for attitudes decreased the effect of values on hesitancy, while attitudes continued to have a strong direct effect on hesitancy, consistent with a mediation hypothesis and our proposed framework (Figure 1). In the multivariable model of behavior, most of the associations between vaccine values and late vaccination seen in the univariable analyses became non-significant, except for Self-Direction, which retained significance even when accounting for vaccine attitudes. Endorsing Self-Direction values was negatively associated with on-time vaccination behavior over and above the effects of attitudes, suggesting both direct and indirect effects of the Self-Direction vaccine value on vaccine behavior. A rigorous test of a potential indirect effects of values on behavior requires a prospective, experimental design.
Limitations
This study should be considered in the context of several limitations. Possibly due to range restriction, non-normal distributions, and small sample size, we may have had limited power to detect relationships among less common variations in parental vaccine values in this pilot study. The study was conducted as a regional survey in one state and results may not be generalizable to other geographic settings and populations. In addition, survey respondents were limited to those who were English-speaking and had access to email. Survey respondents may have differed from non-respondents in demographic factors, values, vaccine attitudes, and behaviors. We did not assess the PVV scale as a whole, so it is possible that only some of the vaccine values subscales contribute to vaccine attitudes, hesitancy and behavior. This scale development study found that only some parental vaccine values were associated with vaccine hesitancy and late vaccination, therefore analysis in a future trial is needed to confirm replicability of these associations and to prospectively test for associations between other factors and relevant vaccine outcomes. Associations between vaccine values or vaccine attitudes and vaccination behavior cannot be interpreted as predictive because attitudes and values were measured among parents when children were already over one year of age and vaccination behavior up to one year had already occurred. Future study is needed to delineate the impacts of values and attitudes on vaccine hesitancy, noting that some attitudes and hesitancy items are similar in content and may be collinear. Vaccine knowledge was not directly measured in this survey because this was outside of the scope of the project objectives. We focused our evaluation on vaccine specific values rather than global values. Intervention studies are needed to determine whether global or vaccine-specific values are a more effective intervention target.
Conclusions
The Parental Vaccine Values scale is a valid and reliable instrument for assessing parental vaccine values and examining relationships with vaccine attitudes, intentions, and late vaccination behavior, and represents a psychological construct distinct from attitudes, which have been the focus of many prior intervention studies to increase vaccination. Parental vaccine values therefore represent a promising and novel target for interventions related to vaccine hesitancy and vaccination behavior. Many people view scientific information with skepticism for a variety of reasons that may reflect a spectrum of attitudes and values. Connecting the presentation of scientific facts to these vaccine values may improve communication with the public29,71 and influence the way information is received. Testing interventions that incorporate vaccine values to address vaccine hesitancy and change vaccination behavior may serve as an innovative strategy for engaging parents in this vital public health action.
Supplementary Material
Supplemental Table 1: Bivariate Correlations Between Parental Vaccine Values (combined sample, n=295)
*p<0.05, **p<0.01, ***p<0.001
Highlights:
The Parental Vaccine Values (PVV) scale measures vaccination-specific values
The PVV subscales are valid and internally consistent
Vaccine values were associated with vaccine attitudes, hesitancy, and behavior
Tailoring vaccine promotion messages to vaccine values may improve effectiveness
Acknowledgements:
The authors wish to thank the staff from the participating offices as well as the parents who participated in the surveys for this study.
Funding source: This project was supported by a grant from the Department of Health and Human Services, National Institutes of Health, Grant Number: 1R01HD079457-01 (PIs: Amanda Dempsey and Jason Glanz).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure Statement: Amanda Dempsey serves on advisory boards for Merck, Pfizer, and Sanofi Pasteur. She does not receive research funding from these companies. The other authors have no relevant financial disclosures.
Potential Conflicts of Interest: Amanda Dempsey serves on advisory boards for Merck, Pfizer and Sanofi Pasteur. She does not receive any research funds from these companies. The other authors have no relevant conflicts of interest.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Roush SW, Murphy TV, Vaccine-Preventable Disease Table Working G. Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. JAMA. 2007;298(18):2155–2163. [DOI] [PubMed] [Google Scholar]
- 2.Hamborsky J, Kroger A, Wolfe C. Epidemiology and Prevention of Vaccine-preventable Diseases: The Pink Book: Course Textbook. Public Health Foundation; 2015. [Google Scholar]
- 3.Centers for Disease C, Prevention. Impact of vaccines universally recommended for children--United States, 1990-1998. MMWR Morb Mortal Wkly Rep. 1999;48(12):243–248. [PubMed] [Google Scholar]
- 4.Omer SB, Pan WK, Halsey NA, et al. Nonmedical exemptions to school immunization requirements: secular trends and association of state policies with pertussis incidence. JAMA. 2006;296(14):1757–1763. [DOI] [PubMed] [Google Scholar]
- 5.Glanz JM, Newcomer SR, Narwaney KJ, et al. A population-based cohort study of undervaccination in 8 managed care organizations across the United States. JAMA Pediatr. 2013;167(3):274–281. [DOI] [PubMed] [Google Scholar]
- 6.Kennedy A, Lavail K, Nowak G, Basket M, Landry S. Confidence about vaccines in the United States: understanding parents' perceptions. Health Aff (Millwood). 2011;30(6):1151–1159. [DOI] [PubMed] [Google Scholar]
- 7.Salmon DA, Dudley MZ, Glanz JM, Omer SB. Vaccine Hesitancy: Causes, Consequences, and a Call to Action. Am J Prev Med. 2015;49(6 Suppl 4):S391–398. [DOI] [PubMed] [Google Scholar]
- 8.Hill HA, Elam-Evans LD, Yankey D, Singleton JA, Kolasa M. National, State, and Selected Local Area Vaccination Coverage Among Children Aged 19-35 Months - United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64(33):889–896. [DOI] [PubMed] [Google Scholar]
- 9.Salmon DA, Sotir MJ, Pan WK, et al. Parental vaccine refusal in Wisconsin: a case-control study. WMJ. 2009;108(1):17–23. [PMC free article] [PubMed] [Google Scholar]
- 10.Kempe A, O'Leary ST, Kennedy A, et al. Physician response to parental requests to spread out the recommended vaccine schedule. Pediatrics. 2015;135(4):666–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.MacDonald NE, Hesitancy SWGoV. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. [DOI] [PubMed] [Google Scholar]
- 12.Gowda C, Dempsey AF. The rise (and fall?) of parental vaccine hesitancy. Hum Vaccin Immunother. 2013;9(8):1755–1762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dube E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J. Vaccine hesitancy: an overview. Hum Vaccin Immunother. 2013;9(8):1763–1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaufman J, Synnot A, Ryan R, et al. Face to face interventions for informing or educating parents about early childhood vaccination. Cochrane Database Syst Rev. 2013(5):CD010038. [DOI] [PubMed] [Google Scholar]
- 15.Dube E, Gagnon D, MacDonald NE, Hesitancy SWGoV. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine. 2015;33(34):4191–4203. [DOI] [PubMed] [Google Scholar]
- 16.Jarrett C, Wilson R, O'Leary M, Eckersberger E, Larson HJ, Hesitancy SWGoV. Strategies for addressing vaccine hesitancy - A systematic review. Vaccine. 2015;33(34):4180–4190. [DOI] [PubMed] [Google Scholar]
- 17.Odone A, Ferrari A, Spagnoli F, et al. Effectiveness of interventions that apply new media to improve vaccine uptake and vaccine coverage. Hum Vaccin Immunother. 2015;11(1):72–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kahan D. Fixing the communications failure. Nature. 2010;463(7279):296–297. [DOI] [PubMed] [Google Scholar]
- 19.Cohen GL, Sherman DK. The psychology of change: Self-affirmation and social psychological intervention. Annual review of psychology. 2014;65:333–371. [DOI] [PubMed] [Google Scholar]
- 20.Sweeney AM, Moyer A. Self-affirmation and responses to health messages: a meta-analysis on intentions and behavior. Health Psychol. 2015;34(2):149–159. [DOI] [PubMed] [Google Scholar]
- 21.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78. [DOI] [PubMed] [Google Scholar]
- 22.Williams GC, Rodin GC, Ryan RM, Grolnick WS, Deci EL. Autonomous regulation and long-term medication adherence in adult outpatients. Health Psychol. 1998;17(3):269–276. [DOI] [PubMed] [Google Scholar]
- 23.Williams GC, Gagne M, Ryan RM, Deci EL. Facilitating autonomous motivation for smoking cessation. Health Psychol. 2002;21(1):40–50. [PubMed] [Google Scholar]
- 24.Falk EB, O'Donnell MB, Cascio CN, et al. Self-affirmation alters the brain's response to health messages and subsequent behavior change. Proc Natl Acad Sci U S A. 2015;112(7):1977–1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kang Y, O'Donnell MB, Strecher VJ, Taylor SE, Lieberman MD, Falk EB. Self-Transcendent Values and Neural Responses to Threatening Health Messages. Psychosom Med. 2017;79(4):379–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Finley AJ, Crowell AL, Schmeichel BJ. Self-affirmation enhances processing of negative stimuli among threat-prone individuals. Soc Cogn Affect Neurosci. 2018;13(6):569–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kelly MP, Heath I, Howick J, Greenhalgh T. The importance of values in evidence-based medicine. BMC Med Ethics. 2015;16(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leask J, Macartney K. Parental decisions about vaccination: collective values are important. J Paediatr Child Health. 2008;44(10):534–535. [DOI] [PubMed] [Google Scholar]
- 29.Witteman HO. Addressing Vaccine Hesitancy With Values. Pediatrics. 2015;136(2):215–217. [DOI] [PubMed] [Google Scholar]
- 30.Attwell K, Freeman M. I Immunise: An evaluation of a values-based campaign to change attitudes and beliefs. Vaccine. 2015;33(46):6235–6240. [DOI] [PubMed] [Google Scholar]
- 31.Opel DJ, Schwartz JL, Omer SB, et al. Achieving an Optimal Childhood Vaccine Policy. JAMA Pediatr. 2017. [DOI] [PubMed] [Google Scholar]
- 32.Amin AB, Bednarczyk RA, Ray CE, et al. Association of moral values with vaccine hesitancy. Nature Human Behaviour. 2017;1(12):873. [DOI] [PubMed] [Google Scholar]
- 33.Flannigan L, Orenstein WA, Bednarczyk R, et al. Personal Values as Mediators of Receipt of Non-influenza Childhood Vaccines. Paper presented at: Open Forum Infectious Diseases 2017. [Google Scholar]
- 34.Schwartz SH. An overview of the Schwartz theory of basic values. Online readings In Psychology and Culture. 2012;2(1):11. [Google Scholar]
- 35.Schwartz SH, Melech G, Lehmann A, Burgess S, Harris M, Owens V. Extending the cross-cultural validity of the theory of basic human values with a different method of measurement. Journal of Cross-Cultural Psychology. 2001;.32(5):pp. [Google Scholar]
- 36.Schwartz SH. Les valeurs de base de la personne: théorie, mesures et applications. Revue française de sociologie. 2006;47(4):929–968. [Google Scholar]
- 37.Fiske ST, Gilbert DT, Lindzey G, Jongsma AE. Handbook of social psychology. 5th ed. Hoboken, N.J.: Wiley; 2010. [Google Scholar]
- 38.Homer PM, Kahle LR. A structural equation test of the value-attitude-behavior hierarchy. Journal of Personality and social Psychology. 1988;54(4):638. [Google Scholar]
- 39.Boer D, Fischer R. How and when do personal values guide our attitudes and sociality? Explaining cross-cultural variability in attitude-value linkages. Psychol Bull. 2013;139(5):1113–1147. [DOI] [PubMed] [Google Scholar]
- 40.Shim S, Maggs J. A cognitive and behavioral hierarchical decision-making model of college students' alcohol consumption. Psychology & Marketing. 2005;22(8):649–668. [Google Scholar]
- 41.Ajzen I. The theory of planned behavior. Organizational behavior and human decision processes. 1991;50(2):179–211. [Google Scholar]
- 42.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical Informatics. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological methods. 1996;1(2):130. [Google Scholar]
- 44.Thompson B Exploratory and confirmatory factor analysis : understanding concepts and applications. 1st ed. Washington, DC: American Psychological Association; 2004. [Google Scholar]
- 45.Kline RB. Principles and practice of structural equation modeling. Fourth edition. ed. New York: The Guilford Press; 2016. [Google Scholar]
- 46.Glanz JM, Wagner NM, Narwaney KJ, et al. A mixed methods study of parental vaccine decision making and parent-provider trust. Acad Pediatr. 2013;13(5):481–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Parental vaccine safety concerns in 2009. Pediatrics. 2010;125(4):654–659. [DOI] [PubMed] [Google Scholar]
- 48.Opel DJ, Taylor JA, Mangione-Smith R, et al. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. 2011;29(38):6598–6605. [DOI] [PubMed] [Google Scholar]
- 49.Salmon DA, Moulton LH, Omer SB, DeHart MP, Stokley S, Halsey NA. Factors associated with refusal of childhood vaccines among parents of school-aged children: a case-control study. Arch Pediatr Adolesc Med. 2005;159(5):470–476. [DOI] [PubMed] [Google Scholar]
- 50.Gust DA, Kennedy A, Shui I, Smith PJ, Nowak G, Pickering LK. Parent attitudes toward immunizations and healthcare providers the role of information. Am J Prev Med. 2005;29(2):105–112. [DOI] [PubMed] [Google Scholar]
- 51.Shoup JA. Concerns, Attitudes, Beliefs and Intentions of Parents about Vaccines for their Child: Development and Evaluation of a Survey Instrument in an Integrated Health Care System in Colorado. Denver, Colorado, USA: Scool of Public Affairs, University of Colorado Denver; 2015. [Google Scholar]
- 52.Gellin BG, Maibach EW, Marcuse EK. Do parents understand immunizations? A national telephone survey. Pediatrics. 2000;106(5):1097–1102. [DOI] [PubMed] [Google Scholar]
- 53.Dempsey AF, Pyrzanowski J, Donnelly M, et al. Acceptability of a hypothetical group B strep vaccine among pregnant and recently delivered women. Vaccine. 2014;32(21):2463–2468. [DOI] [PubMed] [Google Scholar]
- 54.Opel DJ, Mangione-Smith R, Taylor JA, et al. Development of a survey to identify vaccine-hesitant parents: the parent attitudes about childhood vaccines survey. Hum Vaccin. 2011;7(4):419–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Oladejo O, Allen K, Amin A, Frew PM, Bednarczyk RA, Omer SB. Comparative analysis of the Parent Attitudes about Childhood Vaccines (PACV) short scale and the five categories of vaccine acceptance identified by Gust et al. Vaccine. 2016;34(41):4964–4968. [DOI] [PubMed] [Google Scholar]
- 56.Strikas RA, Centers for Disease C, Prevention, Advisory Committee on Immunization P, Group ACAIW. Advisory committee on immunization practices recommended immunization schedules for persons aged 0 through 18 years--United States, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(4):93–94. [PMC free article] [PubMed] [Google Scholar]
- 57.De Vaus DA. Surveys in social research. Sixth edition. ed. Abingdon, Oxon: Routledge; 2014. [Google Scholar]
- 58.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. [Google Scholar]
- 59.DeVellis RF. Scale development: Theory and applications. Vol 26: Sage publications; 2016. [Google Scholar]
- 60.Tavakol M, Dennick R. Making sense of Cronbach's alpha. Int J Med Educ. 2011;2:53–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Team RC. R: A language and environment for statistical computing ****[Internet]. Vienna, Austria; 2014. 2017. [Google Scholar]
- 62.Oberski D. lavaan. survey: An R package for complex survey analysis of structural equation models. Journal of Statistical Software. 2014;57(1):1–27.25400517 [Google Scholar]
- 63.Sherman DA, Nelson LD, Steele CM. Do messages about health risks threaten the self? Increasing the acceptance of threatening health messages via self-affirmation. Personality and Social Psychology Bulletin. 2000;26(9):1046–1058. [Google Scholar]
- 64.Foxcroft DR, Moreira MT, Almeida Santimano NM, Smith LA. Social norms information for alcohol misuse in university and college students. Cochrane Database Syst Rev. 2015(12):CD006748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schultz PW, Nolan JM, Cialdini RB, Goldstein NJ, Griskevicius V. The constructive, destructive, and reconstructive power of social norms. Psychol Sci. 2007;18(5):429–434. [DOI] [PubMed] [Google Scholar]
- 66.Fagerlin A, Peters E, Schwartz A, Zikmund-Fisher BJ. Cognitive and affective influences on health decisions. Handbook of Health Psychology and Behavioral Medicine. 2010;1:49. [Google Scholar]
- 67.Meszaros JR, Asch DA, Baron J, Hershey JC, Kunreuther H, Schwartz-Buzaglo J. Cognitive processes and the decisions of some parents to forego pertussis vaccination for their children. J Clin Epidemiol. 1996;49(6):697–703. [DOI] [PubMed] [Google Scholar]
- 68.Wroe AL, Bhan A, Salkovskis P, Bedford H. Feeling bad about immunising our children. Vaccine. 2005;23(12): 1428–1433. [DOI] [PubMed] [Google Scholar]
- 69.Connolly T, Reb J. Omission bias in vaccination decisions: Where’s the “omission”? Where’s the “bias”? Organizational Behavior and Human Decision Processes. 2003;91(2):186–202. [Google Scholar]
- 70.Allred NJ, Shaw KM, Santibanez TA, Rickert DL, Santoli JM. Parental vaccine safety concerns: results from the National Immunization Survey, 2001-2002. Am J Prev Med. 2005;28(2):221–224. [DOI] [PubMed] [Google Scholar]
- 71.Kahan DM, Braman D, Cohen GL, Gastil J, Slovic P. Who fears the HPV vaccine, who doesn't, and why? an experimental study of the mechanisms of cultural cognition. Law Hum Behav. 2010;34(6):501–516. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1: Bivariate Correlations Between Parental Vaccine Values (combined sample, n=295)
*p<0.05, **p<0.01, ***p<0.001