Abstract
Objective:
A significant subset of college students experience PTSD symptoms, and many engage in problematic alcohol use. Some college students with PTSD symptoms may use alcohol and other substances to cope with their symptoms, and those with PTSD experience more negative alcohol and drug consequences than those without PTSD. Mindfulness-Based Interventions (MBIs) have been successfully utilized for individuals with PTSD or substance use disorders. However, to date, no studies have evaluated MBIs for college students with co-occurring PTSD symptoms and problem drinking.
Method:
This study was a feasibility pilot of a 4-week group loving-kindness meditation (LKM) intervention, a practice of intentionally directing well wishes to oneself and others. LKM was compared to referral to treatment as usual (RTAU) for non-treatment seeking college students (N=75) with PTSD symptoms and problem drinking.
Results:
Overall, the LKM group had low to moderate feasibility and acceptability among college students, as recruitment was lower than expected and attendance at LKM groups was modest. Participants’ PTSD symptoms, drinking quantity, and negative drinking consequences decreased, and state mindfulness increased over the course of the study, but there were no significant differences between LKM and RTAU on these outcomes. Additionally, higher coping drinking motives predicted greater PTSD symptoms and more drinking consequences over the course of the study.
Conclusions:
Effective interventions for college students with PTSD symptoms and problematic alcohol use are needed, especially for individuals who drink to cope with their PTSD symptoms. Future research on LKM that addresses the limitations of the current study is warranted.
Keywords: Mindfulness, Loving-Kindness Meditation, PTSD Symptoms, Problem Drinking, College Students
The majority of college students (66%) experience a traumatic event in their lifetime before college (Read, Ouimette, White, Colder, & Farrow, 2011) and more will experience a traumatic event during college (e.g., Krebs, Lindquist, Warner, Fisher, & Martin, 2009). Reactions to traumatic experiences can persist. Approximately 9% of college students meet current criteria for posttraumatic stress disorder (PTSD; Read et al., 2011), which is higher than the rates in adolescents ages 12 to 17 (six-month prevalence 3.7–6.3%; Kilpatrick et al., 2003) and adults ages 18–64 (12-month prevalence 4.4%; Kessler, Petukhova, Sampson, Zaslavsky, & Wittchen, 2012), demonstrating that while college students are often thought to be a high functioning subset of the population, they may be more vulnerable to PTSD than the general population. Additionally, college students are at risk for problematic alcohol use. Thirty eight percent of college students report heavy episodic or “binge” drinking (four or more drinks in one sitting for females, five or more for males) in the past month (SAMHSA, 2015). Alcohol use disorders are the most common psychiatric disorder among college students, and compared to their non-college-attending peers, they are significantly less likely to have received past-year treatment for alcohol or drug use disorders (Blanco et al., 2008). The high rates of alcohol use, coupled with the low frequency of treatment seeking in this at-risk population, underscores the need for acceptable and effective interventions to address high-risk drinking.
Epidemiological studies have found a high rate of co-occurrence between PTSD and alcohol use (Debell et al., 2014). Among college students who reported heavy episodic drinking in the past month, 16.9% had elevated PTSD symptoms (Monahan et al., 2013). College students experiencing PTSD symptoms often drink heavily to cope with these symptoms (Miranda, Meyerson, Long, Marx, & Simpson, 2002) and those with PTSD have worse drinking outcomes than those who do not (Read et al., 2012). For example, newly matriculated college students with partial and full PTSD had more alcohol and drug consequences than those without PTSD through the first semester of college (Read et al., 2012). Another study found college women with PTSD consumed more alcohol and were at greater risk of experiencing alcohol-related consequences compared to women without PTSD (Stappenbeck, Bedard-Gilligan, Lee, & Kaysen, 2013). Thus, for young adults with PTSD and problem drinking, college may be a critical time for intervention to decrease negative academic, social, and psychological outcomes.
Several different models have been proposed to explain the high rate of co-occurrence of PTSD and alcohol and other substance use, the most prominent of which is the self-medication model, which posits that PTSD symptoms and substance use are functionally related via a negative reinforcement model, wherein individuals use substances to alleviate their PTSD symptoms (McCauley, Killeen, Gros, Brady, & Back, 2012). Put simply, some individuals use substances to avoid, or cope with, negative thoughts and emotions. For example, one study examined PTSD and substance use symptoms in individuals in outpatient substance use treatment and found that weekly PTSD symptom fluctuations were associated with alcohol, cocaine, and/or opiate dependence symptoms the following week (Ouimette, Read, Wade, & Tirone, 2009). Another study examined daily associations between PTSD and alcohol use in a community sample of individuals with PTSD and alcohol dependence and found that elevated PTSD symptoms predicted greater alcohol use on the same day and on the following day (Simpson, Stappenbeck, Luterek, Levahot, & Kaysen, 2014). Additionally, in this study among those with higher coping drinking motives, PTSD symptoms were positively associated with alcohol consumption on higher PTSD days compared to those with lower coping drinking motives. Indeed, drinking in an effort to cope with negative affect is more strongly associated with alcohol-related problems than drinking initiated for other reasons in young adults (Kuntsche, Knibbe, Gmel, & Engels, 2005). Thus, the self-medication model is integral to the rationale behind interventions targeting co-occurring PTSD and substance use, and individuals’ drinking motives are important to examine when developing interventions for this population.
Treatment development for PTSD and co-occurring substance use is ongoing, and while there is some evidence of efficacious treatments, there is a lack of studies demonstrating substantial reductions in both PTSD and substance use. For example, a recent review synthesized findings from randomized clinical trials evaluating behavioral treatments (including exposure-, addiction-, and coping-based treatments) for PTSD and substance use; no favorable outcomes for the experimental treatment were found for both PTSD and substance use beyond comparators (Simpson, Levahot, & Petrakis, 2017), suggesting a need for additional treatment development and evaluation. Additionally, to date, treatments for PTSD and substance use have been studied using clinical samples. Less is known about the efficacy of interventions among non-clinical populations with PTSD symptoms and problematic substance use.
One potential approach for addressing PTSD symptoms and co-occurring problematic alcohol is mindfulness-based intervention (MBI). Mindfulness has been described as “paying attention in a particular way: on purpose, in the present moment, and non-judgmentally” (p. 4, Kabat-Zinn, 1994). A recent meta-analysis examined effects of MBIs for PTSD in randomized controlled trials (Hilton et al., 2017). In a pooled analysis of eight interventions, a small effect of MBIs on PTSD symptoms was found, and MBIs resulted in significantly greater reductions in PTSD symptoms than comparator treatment conditions. Another recent systematic review and meta-analysis examined the efficacy of MBIs for individuals with substance use in 42 randomized controlled trials (Li, Howard, Garland, McGovern, & Lazar, 2017). In all but one study examined, MBIs were superior to the comparator treatment condition on reductions in quantity and frequency of alcohol and drug use, number of alcohol and drug- related problems, and level of craving for substance use. In the subset of studies from which effect sizes could be calculated, compared to comparator treatment conditions, MBIs had a significant, small effect in reducing substance use. These reviews suggest preliminary efficacy of MBIs in adult populations with PTSD symptoms or substance use disorders, although the heterogeneity of MBIs (e.g., yoga interventions, mantram repetition programs) included in the reviews makes it difficult to determine the relative efficacy of the specific interventions.
Importantly, there is preliminary evidence that MBIs may be acceptable to college student drinkers, although efficacy of these interventions is mixed. For example, a study of at-risk college drinkers who reported affective-regulation drinking motives found that students in a brief mindfulness-based intervention experienced increased mindfulness compared to relaxation and control conditions, but the urge to drink after an affect manipulation was not significantly different between conditions (Vinci et al., 2014). However, in another study of college students who had engaged in recent binge drinking, students who participated in a brief mindfulness and cue exposure group reported fewer binge drinking episodes and alcohol consequences four weeks after the intervention, compared to students in a cue exposure only condition (Mermelstein & Garske, 2015). Additionally, attrition was low and students reported high satisfaction with the mindfulness group (Mermelstein & Garske, 2015). While these studies suggest MBIs may be appropriate for college student drinkers, no studies to date have evaluated MBIs for college students with co-occurring PTSD symptoms and problem drinking.
One type of MBI, Loving-Kindness Meditation (LKM), has shown promise as a treatment for PTSD (Kearney et al., 2013) but has not been evaluated in the context of problematic drinking. LKM is derived from Buddhist traditions and involves increasing positive emotions and kindness towards oneself and others (Hofmann, Grossman, & Hinton, 2011). In LKM, individuals silently repeat phrases of positive intention for themselves, other people in their lives to whom they feel close, a neutral person, a difficult person in their life, and people who are unknown to them. In one open-trial study of a 12-session group LKM intervention for male and female veterans with PTSD, a large effect size was reported for reduction in PTSD symptoms at the end of treatment and 3–months post LKM, and participants found the treatment acceptable (Kearney et al., 2013). LKM may target key mechanisms that maintain PTSD symptoms. It is an approach-oriented practice, as participants repeatedly bring to mind individuals about whom they have ambivalent feelings (potentially including themselves), which facilitates exposure to thoughts and emotions they might otherwise attempt to avoid. In doing so, LKM counteracts internal avoidance behavior, which, along with external avoidance behavior, is believed to maintain PTSD symptoms (Pineles et al., 2011). LKM also emphasizes cultivating positive emotions and thoughts about oneself and others, which may increase self-compassion (Neff, 2003) and help shift pervasive negative beliefs about oneself (e.g., I’m a weak person) and others (e.g., people are not what they seem) common to PTSD that can lead to coping behaviors such as drinking.
The current study was a feasibility pilot of a time-limited, group mindfulness intervention based on LKM for college students with PTSD symptoms and problem drinking compared to referral to treatment as usual (RTAU). The two study hypotheses were: 1) Implementing LKM would be feasible and college students would find the intervention acceptable, and 2) Participants who received LKM would experience significantly greater increases in mindfulness and significantly greater reductions in PTSD symptoms, drinking quantity, and negative drinking consequences at post-treatment and 1-month follow-up, compared to RTAU. An exploratory hypothesis - that baseline coping drinking motives would be associated with greater PTSD symptoms, drinking quantity, and negative drinking consequences - was also examined.
Method
Participants
Inclusion criteria.
Participants (N = 75) were young adult college students (ages 18 to 29) at a large west- coast university who endorsed heavy episodic drinking, defined as drinking four or more (for women) or five or more (for men) drinks on one occasion at least twice in the past month (Wechsler & Nelson, 2001). Eligible participants also reported experiencing a traumatic event based on their endorsement of at least one of 16 types of events on the Life Events Checklist for the DSM-5 (LEC-5; Weathers et al., 2013). Additionally, participants endorsed experiencing at least one PTSD symptom in at least two of the four PTSD symptoms clusters (intrusive symptoms, avoidance, negative alterations in cognition and mood, and alterations in arousal and reactivity) in the past month, to ensure some variability and complexity in their symptoms. Participants’ PTSD symptoms had to have lasted for more than one month, to ensure that their symptomatology was not an acute post-trauma response.
The majority of study participants identified themselves as women (69.3%) and heterosexual (88.0%). Over half identified as white (56.0%), followed by Asian/Pacific Islander (20%), and mixed race (17.3%). Most participants were in their first year of college (57.3%) and the most common living arrangement was a fraternity or sorority house (34.7%). Participant demographics are summarized in Table 1.
Table 1.
Participant Baseline Demographics (N = 75)
| Demographic |
LKM % (n) |
RTAU % (n) |
Total % (n) |
|---|---|---|---|
| Women | 69.4 (25) | 69.2 (27) | 69.3 (52) |
| Age (M (SD)) | 19.2 (1.3) | 19.2 (1.4) | 19.2 (1.3) |
| Sexual orientation | |||
| Straight | 94.4 (34) | 82.1 (32) | 88.0 (66) |
| Gay | 5.6 (2) | 7.7 (3) | 6.7 (5) |
| Bisexual | -- | 5.1 (2) | 2.7 (2) |
| Questioning | -- | 5.1 (2) | 2.7 (2) |
| Race/ethnicity | |||
| White | 61.1 (22) | 51.3 (20) | 56.0 (42) |
| Asian/Pacific Islander | 19.4 (7) | 20.5 (8) | 20.0 (15) |
| Mixed race | 13.9 (5) | 20.5 (8) | 17.3 (13) |
| Latino | 2.8 (1) | 7.7 (3) | 5.3 (4) |
| Black | 2.8 (1) | -- | 1.3 (1) |
| Year in School | |||
| 1st year | 58.3 (21) | 56.4 (22) | 57.3 (43) |
| 2nd year | 25.0 (9) | 20.5 (8) | 22.7 (17) |
| 3rd year | 13.9 (5) | 17.9 (7) | 16.0 (12) |
| 4th year | 2.8 (1) | 5.1 (2) | 4.0 (3) |
| Residence | |||
| Fraternity or sorority house | 41.7 (15) | 28.2 (11) | 34.7 (26) |
| Campus residence hall | 27.8 (10) | 33.3 (13) | 30.7 (23) |
| Off-campus apartment or house | 30.6 (11) | 30.8 (12) | 30.7 (23) |
| At home with parents | -- | 7.7 (3) | 4.0 (3) |
Exclusion criteria.
Students were excluded from the study if they reported active suicidality or psychotic symptoms. At the in-person screening, students completed the P4 survey (Dube, Kurt, Bair, Theobald, & Williams, 2010), a 4-item suicide screening tool. Students in the high-risk category (e.g., intention to act on thoughts of hurting oneself and/or an absence of anything that would prevent or keep them from harming oneself), were excluded from the study, given referrals, and called by the lead researcher for additional risk assessment within 24 hours. In addition, individuals were excluded if they indicated experiencing two out of three items in the psychosis subscale of the Revised Behavior and Symptom Identification Scale (BASIS-24; Eisen, Normand, Belanger, Spiro, & Esch, 2004).
Procedures
This study used a randomized control design. Participants were randomly assigned to one of two conditions: a 4-week Loving-Kindness Meditation (LKM) group or referral to treatment as usual (RTAU). The university’s Institutional Review Board approved all study procedures and the National Institute on Alcohol Abuse and Alcoholism issued a certificate of confidentiality for additional protection of research participants due to the sensitive nature of some of the data collected.
Recruitment.
Participants (non-treatment seeking college students) were recruited from the psychology subject pool comprising of students enrolled in large Psychology classes at the university, primarily from Psychology 101 courses, and through which students could complete a screening survey for the study. If students met the study inclusion criteria contained in the screening survey, they were contacted by email and phone and invited to participate in an additional in-person assessment in which two additional screening measures assessing exclusion criteria (active suicidality and/ or current psychotic symptoms) were administered. If students did not meet exclusion criteria, they were invited into the study, provided informed consent, and asked to complete baseline measures. After completing baseline measures, participants were randomized to study condition (either LKM or RTAU) and informed of their randomization condition via email.
Randomization.
Stratified random assignment using a minimization protocol (Scott, McPherson, Ramsay, & Campbell, 2002) was used to ensure groups were equivalent on gender and level of PTSD symptomology based on the screening survey. Participants were randomized using a 1:1 ratio to either the LKM or RTAU condition.
Participant compensation.
Participants received up to six hours of course extra credit for participation in the study. Students who chose not to participate were still given extra credit for their attendance at the in-person meeting to avoid risk of coercion. Additionally, participants received a $15 electronic Amazon gift card for completing the 1-month follow-up assessment.
Mindfulness intervention.
The material for the LKM group was drawn from the LKM manual used by Kearney et al. (2013) in their open trial; the current study used a 4-week format, a shortened version of the 12-week intervention used in the open trial. The intervention was condensed to allow it to be delivered in one academic quarter, with the goal of developing a time-limited intervention that fit into a collegiate environment and would be well accepted by students. The 4-week intervention maintained the core elements of the full LKM intervention, but combined sessions and shortened some of the exercises, which allowed for multiple exercises to be practiced in each group. Each LKM group included three components: brief didactic teaching of mindfulness principles, an experiential component in which participants practiced mindfulness exercises, and a time for group reflection on the exercises and wrap up. Over the four sessions participants practiced repeating phrases of positive intention, first for a person in their lives to whom they feel close, themselves, a neutral person, a difficult person in their life, a person unknown to them, and finally all beings. Participants were also asked to practice the week’s specific LKM exercises for 15 minutes per day using the provided audio-recorded guided instruction. The LKM groups included between two and 10 participants. Each LKM group met weekly for one hour for four weeks, was held in the late afternoon (between 4pm and 6pm) on weeknights, and was co-facilitated by doctoral students in clinical psychology. Participants randomized to the LKM condition were emailed and called weekly to remind them to attend the group and, if participants missed the group, they were sent an email with the LKM homework exercises and inquiring about their absence. Three graduate students served as group leaders over the course of the study. Each had attended at least one mindfulness meditation retreat and had an independent mindfulness practice. The LKM group was audio recorded and a supervisor with expertise in mindfulness reviewed all sessions to ensure the LKM intervention was being delivered per protocol; however, no treatment fidelity measure was used to rate sessions for specific content. Weekly supervision was provided to all LKM group leaders to allow leaders to reflect on the previous session, troubleshoot specific issues that came up in group, answer questions about LKM delivery, and plan for the next session.
Referral to treatment as usual.
The RTAU group did not meet in person during the four weeks of the study. At baseline, participants in both conditions were provided with a referral list including the number for the county crisis hotline and several low cost or free mental health and substance abuse counseling services on campus and in the community, to help ensure participants had access to standard of care treatments for alcohol use and PTSD symptoms. After randomization, participants in both conditions were encouraged to review the referral list and access relevant services.
Measures
Participants were assessed at baseline, immediately following the 4-week treatment, and at 1-month post-treatment on measures of PTSD symptoms, drinking quantity, and negative drinking consequences, and mindfulness. Additionally, participants completed three brief weekly measures to assess current drinking and PTSD symptomatology and to examine rate and pattern of change over the course of the study. The baseline assessment was completed in paper-and-pencil format; all other assessments were completed online using the software survey tool DatStat Illume. Participants were sent weekly reminder emails asking them to complete the online assessments if they had not yet done so. Data were collected for the study over four academic quarters, between September 2015 and January 2017.
Demographics.
Age, sex, race, sexual orientation, residence, and year in school were assessed through the screening survey.
Traumatic events.
The 17-item LEC-5 (Weathers et al., 2013) was used to determine whether individuals experienced any of a variety of traumatic events. Individuals were considered to have experienced a traumatic event if they indicated the event had happened to them, they witnessed it, learned about it, or if they experienced it as part of their job. The LEC has demonstrated moderate convergent validity with another measure of trauma exposure (the average of the kappas for each item was .55; Gray, Litz, Hsu, & Lombardo, 2004).
PTSD symptoms.
PTSD symptoms were measured via the 20-item PTSD Checklist for the DSM-5 (PCL- 5; Weathers et al., 2013). The PCL-5 asks how much an individual was bothered by a problem (from 0 “not at all” to 4 “extremely”) in the past month. Items reflect symptoms within each of the four PTSD symptom clusters of intrusion, avoidance, negative alterations in cognitions and mood, and alterations in arousal and reactivity. Participants were considered to be experiencing a PTSD symptom if they indicated they were bothered by that symptom “a little bit” (1) or more. The PCL-5 has demonstrated strong internal consistency (α = .94), test-retest reliability (r = .82), and convergent (rs = .74 to .85) and discriminant (rs = .31 to .60) validity (Blevins, Weathers, Davis, Witte, & Domino, 2015).
Drinking.
Heavy episodic drinking was assessed with one item that asked participants if they drank four or more drinks (for females) or five or more (for males) on one occasion at least twice in the past month. Drinking quantity was assessed via the Daily Drinking Questionnaire (DDQ; Collins, Parks, & Marlatt, 1985). The DDQ has demonstrated modest convergent validity (r = .50) with other measures of college student drinking (Collins et al., 1985). Participants reported the average number of drinks they consumed each day of the past week. The quantity of alcohol consumed in the past week was measured by summing an individual’s total drinks per day. Drinking consequences were assessed via the 18-item Rutgers Alcohol Problem Index (RAPI; White & Labouvie, 2000). Participants indicated how many times an event happened in the past month while they were drinking or because of their alcohol use (e.g., had a fight, argument or bad feelings with a friend). The RAPI has demonstrated moderate convergent validity with alcohol use intensity (r = .20 to .57) and strong internal consistency (α = .92) in a sample of nonclinical adolescents (White & Labouvie, 1989). The 18-item version of the RAPI used in the current study highly correlates with the 23-item version (r = .99; White & Labouvie, 2000). Drinking motives were assessed at baseline using the 20-item Drinking Motives Questionnaire-Revised (DMQ-R; Cooper, 1994). The DMQ-R items are categorized into four subscales representing different drinking motives: social (e.g., “because it makes social gatherings more fun”), coping (e.g., “to forget your problems”), enhancement (e.g., “because it gives you a pleasant feeling”), and conformity (e.g., “to fit into a group you like”). The four subscales demonstrate good predictive validity (i.e., explain between 14 and 26 percent of the variance in drinking quantity, frequency, and drinking problems; Cooper, 1994), and each demonstrates adequate internal reliability (α range = .81-.94) (MacLean & Lecci, 2000).
Mindfulness.
Changes in state mindfulness were assessed with the 39-item Five Factor Mindfulness Questionnaire (FFMQ; Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006). The FFMQ consists of a total score, which can be separated into five subscales, each a different component of mindfulness: observing, describing, acting with awareness, nonjudging and nonreactivity to inner experience. Confirmatory factor analyses revealed a five- factor structure demonstrated incremental validity in predicting psychological symptoms and the five facets demonstrate adequate internal reliability (α range = .75-.91) (Baer et al., 2006).
Feasibility and acceptability.
Feasibility was assessed by a) the percentage of psychology subject pool students meeting study criteria who chose to participate in the study (a criterion of ≥80% of students meeting inclusion criteria who agreed to participate was chosen a priori) and b) responses on the 14-item Satisfaction and Acceptability Questionnaire (SAQ) developed for the study which assessed barriers and facilitators to participation including group timing, location, length, transportation issues, and open-ended questions to assess other potential barriers and facilitators to group participation. Acceptability of the LKM group was assessed via questions on the SAQ about overall satisfaction and appealing and unappealing aspects of attending a LKM group. Additionally, LKM group attendance rates were used as an indicator of acceptability.
Data Analysis
Analyses for the current study were conducted using SPSS, Version 19.0 statistical software (IBM, 2010). Data were evaluated using intent-to-treat analyses; data from all randomized participants were included, regardless of whether they initiated or continued treatment, or only provided baseline data. Multi-level modeling (MLM) was chosen to evaluate change over time for PTSD symptoms, a continuous outcome variable, because of the longitudinally clustered nature of the data. For comparison of count outcomes (drinking quantity and negative drinking consequences), Generalized Estimating Equations (GEE; Liang & Zeger, 1986) were used. GEE is an extension of the generalized linear model, and can model outcomes with a variety of distributions; a Poisson distribution was used in the current study (Atkins, Baldwin, Zheng, Gallop, & Neighbors, 2013). Regression coefficients from a Poisson model lie on a log scale, so coefficients are typically raised to the base of e and are interpreted as a rate ratio (Atkins et al., 2013). Rate ratios of 1.0 indicate no effect, while rate ratios above 1.0 indicate a percentage increase in the count outcome, and rate ratios below 1.0 indicate a percentage decrease in the count outcome. The fit for the MLM was compared using Bayesian Information Criterion (BIC), and the GEE models were compared using the Quasi Likelihood under Independence Model Criterion. The MLM covariance structure was determined analytically using BIC model fit indices; the variance components structure produced the best fit. For the GEE analyses, the exchangeable (compound symmetry) covariance matrix was chosen to account for the within-person correlation in the data. Time was coded as 0 at baseline and the other time points were coded 1 through 5, respectively, to examine patterns of change across the course of the study. Due to an administrative error, negative drinking consequences (via the RAPI) were only administered at baseline, post-treatment, and 1-month follow-up, and not during the 4-week intervention period.
Post-hoc power analyses using the final sample size (N= 75) and the effect sizes found for the three main outcomes (ranging between Cohen’s f = .11 to .28), indicated power ranged between .23 and .88, suggesting the study was moderately powered to detect the hypothesized main effects. Regarding missing data, data for this study were considered to be missing at random and considered “ignorable nonresponse” as most longitudinal studies have attrition (Schafer & Graham, 2002). MLM and GEE are appropriate when this type of attrition occurs, as they use all the available data for each participant, instead of removing participants with incomplete data. Effect sizes were calculated by subtracting the observed follow-up mean score from the observed baseline mean score and dividing the difference by the pooled standard deviation from these two time points. Cohen’s d was used to categorize the size of the effect, with .2, .5, and .8 indicating small, medium, and large effects, respectively (Cohen, 1992).
Results
No significant differences were found between the LKM and RTAU conditions with respect to participant gender, χ2 (1, N = 75) = .00, p = .98, or total PTSD symptom score at screening (t (73) = .72, p = .47), indicating the minimization randomization protocol was successful. Additionally, no significant differences were found between the conditions on other participant demographics, total drinks per week, or total negative drinking consequences at baseline. The means and standard deviations for the study variables at baseline, post-treatment, and follow-up are summarized in Table 2. Regarding trauma exposure, the most frequently endorsed traumatic events were a transportation accident (92.0%), unwanted or uncomfortable sexual experience (76.0%), and life-threatening illness or injury or physical assault (both 73.3%).
Table 2.
Study Variables at Baseline, Post-treatment, and Follow-up (N = 75)
| Condition | ||||
|---|---|---|---|---|
| LKM | RTAU | |||
| n | M (SD) | n | M (SD) | |
| PCL-5 Total Score | ||||
| Screen | 35 | 22.8 (14.6) | 39 | 25.6 (18.0) |
| Post-treatment | 18 | 16.1 (16.8) | 31 | 18.0 (18.9) |
| 1 month follow-up | 16 | 13.4 (14.4) | 24 | 13.5 (14.1) |
| DDQ Total Drinks Past Week | ||||
| Baseline | 35 | 10.0 (6.2) | 37 | 9.8 (8.1) |
| Post-treatment | 18 | 3.0 (4.7) | 29 | 5.9 (6.4) |
| 1 month follow-up | 19 | 9.1 (11.4) | 28 | 6.8 (6.1) |
| RAPI Total Score | ||||
| Baseline | 34 | 7.2 (4.9) | 39 | 5.9 (5.3) |
| Post-treatment | 17 | 5.2 (8.5) | 33 | 2.9 (3.5) |
| 1 month follow-up | 18 | 3.9 (4.5) | 28 | 3.7 (5.4) |
| FFMQ Total Score | ||||
| Baseline | 34 | 118.0 (14.1) | 118.0 (20.3) | |
| Post-treatment | 17 | 125.5 (20.6) | 31 | 123.2 (22.0) |
| 1 month follow-up | 12 | 136.8 (20.9) | 21 | 125.3 (18.8) |
Note. PCL-5 = PSTD Checklist for DSM-5; DDQ = Daily Drinking Questionnaire; RAPI = Rutgers Alcohol Problem Index; FFMQ = Five Facets Mindfulness Questionnaire
Assessment Attrition.
For assessment of attrition, participants who provided data at baseline and no other time point were considered to have dropped out of the study, although their data were included in the intent-to-treat analyses. Out of 75 participants, 10 (13.3%) provided only baseline data; 65 participants (86.7%) provided data for at least two time points. A significantly greater proportion of participants who dropped out of the study were in their second year of college, χ2 (1, N = 75) = 4.9, p = .04, had more drinking consequences than those who did not drop out of the study (t (71) = −2.4, p = .02), and were in the LKM condition (n = 8) versus the RTAU condition (n = 2), χ2 (1, N = 75) = 4.7, p = .04. None of the participants assigned to the LKM condition and who dropped out of the study (n = 8) attended a LKM group.
Feasibility of LKM intervention.
Over the four school quarters during which data were collected, 346 students met the initial study inclusion criteria and received an invitation to participate. Of those students, six met subsequent exclusion criteria. Thus, a total of 340 students were considered eligible for the study. Of these students, 76 (22.3%) provided informed consent to participate in the study, below the a priori feasibility criteria of ≥80% of eligible participants. Fifteen LKM participants completed the SAQ. The three items most frequently endorsed as barriers to attending the LKM group were: inconvenient timing of group (26.4%), work commitments (20.0%), and inconvenient location of group (13.3%). The three items most frequently endorsed as facilitating group attendance were: on-campus location (60.0%), time of group (53.3%), and two items that were endorsed with equal frequency - email reminders and extra credit for the time spent on the project (both 46.7%).
Acceptability of LKM intervention.
Acceptability of the LKM group was assessed via the SAQ and group attendance. In response to the question “Overall, how would you rate your satisfaction with the loving-kindness meditation group?” all respondents indicated they were somewhat satisfied (13.3%), satisfied (53.3%), or very satisfied (33.3%). When asked if they would recommend the LKM group to a friend experiencing similar difficulties, all respondents indicated either yes, they thought they would (86.7%) or yes, definitely (13.3%). When asked about appealing features of the LKM group, the three items most frequently endorsed items were: group leaders (66.7%), on-campus location (60.0%), and time of group (60.0%). When asked about unappealing features, the most frequently endorsed items were: time of group (26.7%), on-campus location (13.3%), and group length and homework practice (both 13.3%). Regarding LKM group attendance, of the 36 participants randomized to the LKM condition, 14 (38.9%) did not attend any of the LKM groups, two (5.6%) attended one group, three (8.3%) attended two groups, seven (19.4%) attended three groups, and 10 (27.8%) attended all four groups. Participants were considered treatment completers if they attended two or more of the LKM groups, resulting in 20 (55.6%) of the participants randomized to the LKM condition considered treatment completers. LKM treatment completers and non-completers were compared on demographics and baseline PTSD symptoms, drinking quantity, and drinking consequences. No differences were found except a significantly smaller proportion of the LKM non-completers were white compared to LKM completers, χ2 (1, N = 35) = 6.8, p = .02.
Impact of intervention on PTSD symptoms.
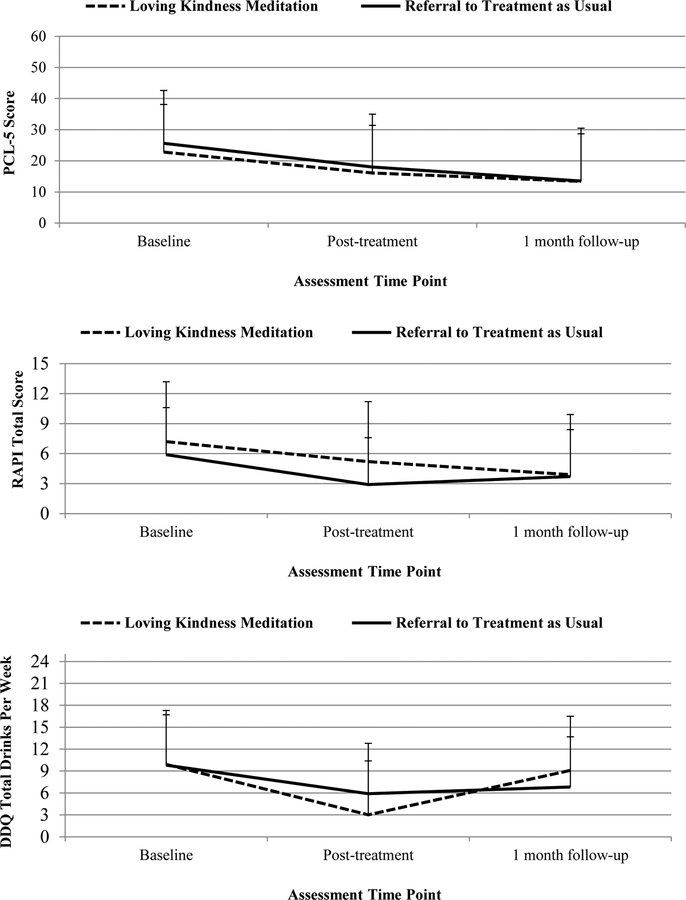
Figure 1 depicts changes in the three outcomes (PTSD symptoms, drinking quantity, and negative drinking consequences) over the course of the study by condition. For PTSD symptoms, the fixed effect of time was significant, (coefficient estimate = 1.23, 95% CI [−2.25, −0.52]), which indicated that, on average, participants’ total PTSD symptom score (as measured by the PCL-5) decreased by 1.23 points at each assessment time point. The effect size for the effect of time on PTSD symptoms from baseline to 1-month follow-up was medium (d = .63). Additionally, the random effect of time was significant, suggesting that the rate of change in individuals’ PTSD symptoms differed between people. Condition was added as a fixed effect and was non-significant, 95% CI [−10.09, 2.63], suggesting condition assignment did not predict level of PTSD symptoms. The effect size for the LKM and RTAU conditions from baseline to 1-month follow-up was medium (d = .66 and d = .74), and the between-group effect size at follow-up was small (d = .01). An interaction between time and condition was entered into the model as a fixed effect, and was non-significant, 95% CI [−1.89, 1.67], suggesting the change in PTSD symptoms over time was not significantly related to condition assignment. When the interaction term was added to the model, the main effect of time was no longer significant, likely due to the high multicollinearity between time and the interaction between time and condition (r = .86). Adding each predictor improved model fit. The final model is displayed on Table 3.
Figure 1.
Changes in observed total PTSD symptoms, drinking quantity, and negative drinking consequences over time by condition
Table 3.
Multilevel Model Predicting PTSD Symptoms (N = 75)
| Fixed Effects | Coefficient | S.E. | 95% CI |
|---|---|---|---|
| Intercept | 21.21 | 8.15 | [4.96, 37.47] |
| Time | −1.23 | 1.32 | [−3.88, 1.42] |
| Condition | −3.63 | 3.30 | [−10.20, 2.94] |
| Time × Condition | −0.11 | 0.89 | [−1.89, 1.67] |
| Social drinking motives | −0.41 | 0.49 | [−1.40, 0.57] |
| Coping drinking motives | 2.07 | 0.41 | [1.26, 2.89]*** |
| Enhancement drinking motives | −0.36 | 0.48 | [−1.33, 0.60] |
| Conformity drinking motives | −0.26 | 0.48 | [−1.22, 0.70] |
| Random Effects | Variance | S.E. | 95% CI |
|---|---|---|---|
| Intercept | 131.76 | 29.13 | [61.55, 92.54]*** |
| Time | 5.64 | 2.10 | [2.72, 11.71]** |
Note.
p <.05,
p <.01,
p <.001
Impact of intervention on drinking quantity.
Similar to the MLM analyses, GEE analyses revealed a significant effect of time, rate ratio = .90, 95% CI [−0.17, −0.06], indicating a 10% decrease in total drinks per week over the study. The effect size for the effect of time on drinking quantity from baseline to follow-up was small (d = .21). There was no significant effect of condition, rate ratio = .97, 95% CI [−0.29, 0.23], or time by condition interaction, rate ratio = .97, 95% CI [−0.15, 0.09]. The effect size from baseline to 1-month follow-up was small for LKM (d = .09) and medium for RTAU (d = .41), and the between-group effect size at follow-up was small (d = .25). Including the interaction term in the model resulted in the main effect of time no longer being significant, likely due to multicollinearity issues. Adding each predictor improved model fit, except for the interaction between time and condition, which worsened fit. The final model is displayed in Table 4.
Table 4.
Generalized Estimating Equation Predicting Drinking Quantity (N = 75)
| Parameter | Coefficient | Rate Ratio | S.E. | 95% CI |
|---|---|---|---|---|
| Intercept | 0.40 | 1.43 | 0.35 | [−0.27, 1.08] |
| Time | −0.07 | 0.93 | 0.08 | [−0.23, 0.08] |
| Condition | 0.02 | 1.02 | 0.15 | [−0.28, 0.31] |
| Time × Condition | −0.03 | 0.97 | 0.06 | [−0.15, 0.09] |
| Social drinking motives | 0.09 | 1.09 | 0.03 | [0.04, 0.14]*** |
| Coping drinking motives | 0.00 | 1.00 | 0.02 | [−0.03, 0.04] |
| Enhancement drinking motives | 0.02 | 1.02 | 0.01 | [−0.01, 0.05] |
| Conformity drinking motives | −0.01 | 0.99 | 0.02 | [−0.05, 0.03] |
Note.
p <.05,
p <.01,
p <.001
Impact of intervention on negative drinking consequences.
GEE analyses revealed a significant effect of time, rate ratio = .74, 95% CI [−0.49, −0.11], which indicated a 26% decrease in drinking consequences over the course of the study. The effect size for the effect of time on drinking consequences from baseline to 1 -month follow- up was medium (d = .55). There was no significant effect of condition, rate ratio = 1.24, 95% CI [−0.10, 0.53], or time by condition interaction, rate ratio = .98, 95% CI [−0.39, 0.35]. The effect size for the LKM and RTAU conditions from baseline to 1-month follow-up was medium (d = .70 and d = .41), and the between-group effect size at follow-up was small (d = .04). Including the interaction term in the model resulted in the main effect of time no longer being significant, again likely due multicollinearity issues. As with the GEE model for drinking quantity, adding each predictor improved model fit except for the interaction between time and condition, which worsened fit. The final model is displayed in Table 4.
Mindfulness.
To assess change in state mindfulness, a repeated measures factorial analysis of variance was conducted to examine the main effects of condition and time, and the interaction between the two, on mindfulness. While individuals in the LKM group had higher mean levels of mindfulness at post-treatment and follow-up than the RTAU group (Table 2), there was no significant effect of time, F(2, 48) = 2.06, p = .34, condition, F(1, 24) = 0.50, p = .49, or time by condition interaction, F(2, 48) = 1.09, p = .34.
Baseline moderators.
Participants’ drinking motives were added as baseline moderators to the three models. Regarding PTSD symptoms, participants’ coping drinking motives significantly predicted PTSD symptoms over time, estimate = 2.07, 95% CI [1.26, 2.89], such that for a one-point increase in coping motives, participants’ PTSD symptom score increased by 2.07 points. Regarding drinking quantity, participants’ social drinking motives significantly predicted total drinking quantity, rate ratio = 1.09, 95% CI [0.04, 0.14], indicating a 9% increase in drinking quantity over the course of the study. Regarding negative drinking consequences, participants’ coping drinking motives significantly predicted negative drinking consequences, rate ratio = 1.07, 95% CI [0.03, 0.11], indicating a 7% increase in drinking consequences over the course of the study.
Completer analyses.
To reduce the potential influence of LKM group non-attendance on outcomes, exploratory post hoc analyses were conducted including only participants in the LKM condition who attended at least two LKM groups (n = 20). In line with the intent-to-treat analyses, a significant effect of time was found for PTSD symptoms, estimate = −1.42, 95% CI [−2.31, −.52], drinking quantity, rate ratio = .91, 95% CI [−.15, −.04], and negative drinking consequences, rate ratio = .78, 95% CI [−.48, −.07], but not a significant effect of condition or interaction between time and condition. When the interaction between time and condition was added to the models, the effect of time was no longer significant.
Discussion
This study evaluated the feasibility, acceptability, and preliminary efficacy of a 4-week group loving-kindness meditation (LKM) intervention for college students with PTSD symptoms and problem drinking, compared to referral to treatment as usual (RTAU).
Feasibility of group LKM.
Only 22% of college students who met study criteria chose to participate in the study, which fell below the a priori feasibility criteria of ≥80% of eligible students choosing to participate in the study. Thus, the study, as implemented, failed to enroll a large percentage of eligible college students. Lower-than- anticipated recruitment could be due to several factors. Students were enrolling in a randomized clinical trial rather than simply agreeing to treatment and some may have found random assignment, rather than the treatment, to be unacceptable. It is also possible that students were reluctant to take part in a study focused on treatment. Given that participants were recruited from a non-clinical setting (the psychology subject pool), students may not have considered themselves in need of treatment to manage their PTSD symptomatology or address their drinking behavior. Previous research in college student populations has identified students’ lack of perceived need for care as one barrier to accessing treatment (Hunt & Eisenberg, 2010). Finally, the nature or language of the approach, i.e., “loving kindness” or “meditation” may have limited the number of students who self-selected into the study.
Additional insight into feasibility issues was provided by participants’ reports of barriers and facilitators to attending LKM groups. Practical barriers to attending psychotherapy are commonly reported (e.g., Mohr et al., 2006) and remain an important consideration when designing and delivering interventions. Feasibility of group interventions for a college population might be improved if sessions are offered at a variety of times and locations. Additionally, students reported that email reminders, a relatively low-effort tool, were helpful in facilitating their group attendance. Email communication is often discouraged because of privacy concerns, but if individuals find this form of communication acceptable and agree to be contacted via email, it may be preferable to telephone reminders.
Acceptability of group LKM.
Overall, participants who completed the Satisfaction and Acceptability Questionnaire (SAQ) (n=15) reported they were satisfied with the intervention. Additionally, all participants reported they would likely recommend the LKM group to a friend who was experiencing similar difficulties. Only one individual reported the group format was unappealing, while eight participants endorsed the group format as an appealing feature. This suggests that college students who attended the sessions largely found LKM acceptable when delivered in a group format.
LKM group attendance represented a second method for assessing acceptability. Twenty participants (55.6%) attended at least half of the LKM groups. It is unclear how LKM attendance compares to other groups for non-treatment seeking college students, as these rates are not widely reported. In clinical samples of individuals with PTSD and alcohol dependence, treatment retention is modest (44–51%; Simpson et al., 2017). Importantly, a substantial number of participants (38.9%) did not attend any of the LKM groups, and their reasons for lack of attendance are unknown. Complete non-attendance may have resulted from feasibility issues (conflicts with the time and day the LKM group was offered), or not perceiving a need for help (Hunt & Eisenberg, 2010). Alternatively, complete non-attendance may have resulted from unacceptability of, or a general lack of interest in, the group LKM intervention or in treatment more generally. The responses of those who did participate in the LKM group suggest that the intervention - despite being somewhat unusual in that it consists of repeating phrases of positive intention to oneself and others - appears to be acceptable to college students and 20 of the 22 students who attended at least one session were considered completers (attended at least half of the groups). Nevertheless, overall attendance at LKM groups was moderate and a significant minority of individuals did not attend any of the LKM groups. Additionally, more non-white individuals did not complete the LKM intervention than completed it. Thus, it is possible that the group LKM may not have been acceptable to participants of color. More work is needed to explore the racial disparities in LKM completion to improve the inclusiveness of this intervention strategy.
Efficacy.
The second hypothesis ‒ that participants who received LKM would experience significantly greater reductions in PTSD symptoms, drinking quantity, and negative drinking consequences at post treatment and 1-month follow-up compared to RTAU ‒ was not supported. Participants experienced decreases in PTSD symptoms, drinking quantity, and negative drinking consequences over the course of the study irrespective of their treatment condition, although the main effect of time was no longer significant when the interaction between time and condition was entered into the model, likely due to the to the high multicollinearity between the variables.
LKM may not have demonstrated differential benefit above the RTAU condition due to the study sample, which was comprised of a non-treatment seeking college student sample with a low to moderate level of PTSD symptoms. Study inclusion criteria were kept broad to be able to determine the effects of LKM in a nonclinical sample; however, LKM may not be effective for individuals with modest levels of PTSD symptomatology. Treatment fidelity in the current study may also have been compromised. The LKM intervention was delivered by graduate students who, despite training and experience with mindfulness-based practices, were new to LKM treatment delivery. Thus, the graduate student leaders were simultaneously learning how to best facilitate the LKM groups while the study was ongoing and data were being collected. Additionally, while a clinical psychologist with expertise in mindfulness reviewed the audio files of the LKM group and provided weekly supervision to group leaders, fidelity to the LKM intervention was not directly assessed. Moreover, the 4-week LKM intervention in the current study was a compressed version of the 12-week intervention from Kearney et al.’s (2013) study. It is possible that the “dose” of LKM in the current study, including group time devoted to practicing the exercises and discussing the participants’ experiences with the exercises, was not sufficient. While participants in the LKM group reported increases in mindfulness at post-treatment and follow-up, these changes were not significantly different from changes in individuals in RTAU, suggesting the LKM intervention, as delivered, may not have led to expected increases in mindfulness. Unfortunately, the absence of a significant difference in self-reported mindfulness is typical following brief mindfulness interventions (Visted, Vellestad, Nielsen, & Nielsen, 2015). Future studies may benefit from assessment of mindfulness practice (Enkema & Bowen, 2017), or the application of intensive longitudinal methods such as experience sampling (Brown & Ryan, 2003), as opposed to self-report. Finally, group LKM may simply not be an effective intervention for college students with PTSD symptoms and problem drinking; thus, no effect would have been demonstrated even if the issues outlined above had been addressed. LKM is a relatively non-directive intervention, and while it does provide the opportunity to discuss thoughts and feelings that result from the meditation exercises, group leaders do not engage individuals in extended conversations about their trauma experiences, trauma-related cognitions, or drinking behaviors. College students may need a more directive intervention to be able to effectively modify certain post-traumatic cognitions (e.g., “I can’t stop bad things from happening to me”) and shift related emotions (e.g., fear, shame). Additionally, students may not have connected their PTSD symptoms with their drinking behavior (e.g., drinking to cope), and so may not have viewed their drinking as problematic or in need of change. Students may need more explicit psychoeducation and discussion about their drinking, including how it may relate to their PTSD symptoms, to enhance their understanding and ability to modify this behavior.
Participants did experience a decrease in PTSD symptoms, drinking quantity, and negative drinking consequences over the course of the study. One explanation for this change is regression to the mean, or the tendency of individuals’ scores in an extreme group to be closer to the population mean when reassessed. This shift in scores may be due to genuine variability in individuals’ symptoms over time or to random measurement error of the observed variables (Bland & Altman, 1994).
Drinking motivation and PTSD symptomatology.
Participants’ drinking motives significantly predicted PTSD symptoms, drinking quantity, and negative drinking consequences. Specifically, higher coping drinking motives predicted greater PTSD symptoms and more drinking consequences, while social drinking motives predicted greater drinking quantity over the course of the study. These findings are consistent with previous research suggesting that, while college students who drink to cope may consume less than those who drink for social facilitation (Read, Wood, Kahler, Maddock, & Palfai, 2003), they experience more alcohol-related consequences than those who drink for other reasons (e.g., Kuntsche et al., 2005; Cooper, 1994). Students who drink to cope may drink in ways that impair their day-to-day functioning (e.g., drinking in the morning before classes) and they may have fewer protective factors (e.g., trusted peers ensuring they get home safely) than those who drink for social facilitation reasons, who likely drink in social settings. Drinking to cope may result from the negative reinforcement cycle that substance use can perpetuate: alcohol can temporarily dampen PTSD symptoms, leading to continued alcohol use, which in turn interferes with natural or intervention-mediated recovery from PTSD symptomatology.
Limitations and future directions.
There were several limitations to this study. Regarding measurement of outcomes, participants’ trauma exposure and PTSD symptoms were assessed via self-report, which can lead to an overestimation of PTSD symptomatology and may not be specific enough to detect symptoms unique to PTSD, and instead may represent negative affect or general distress (Arbisi et al., 2012). Participant’s drinking quantity was assessed via alcohol consumed in the past week, a short time frame in which drinking can vary considerably in college populations. Additionally, the a priori criteria for feasibility (≥80% of students meeting inclusion criteria agreeing to participate) was likely too stringent and may not have served as an accurate benchmark for expected enrollment in group treatment, including LKM, in a college population. Regarding acceptability, while participants were asked about the group generally, they were not asked about specific components of LKM itself, which could have helped determine which aspects of the intervention were and were not appealing to students. There were also limitations related to LKM intervention delivery: although participants were given a guided LKM meditation audio file and encouraged to practice the LKM exercises during the week, practice between LKM sessions was not directly assessed. Between- session practice is related to increased mindfulness skills after a mindfulness-based intervention (Bowen & Kurz, 2012). Because between-session practice was not assessed, we do not know the frequency and relation to PTSD symptom and drinking outcomes of between-session practice. Finally, sampling limitations were also present. The sample size of the study was smaller than anticipated, which resulted in less power to detect differences between the conditions. Substantial attrition over the course of the study further reduced the ability to detect effects.
Although LKM was not associated with reductions in PTSD symptoms, drinking quantity, or negative drinking consequences beyond those of RTAU, the study revealed several opportunities to improve feasibility and acceptability of a group mindfulness-based intervention in the college population. For example, delivering treatment in a group format, leveraging multiple forms of student outreach, and offering students convenient times and locations for treatment may facilitate engagement and completion of treatment. Future research that addresses the limitations of the current study, such as extending the length of the LKM intervention and monitoring LKM treatment fidelity and homework completion, or targeting students who perceive they are in need of treatment, may improve outcomes and should be considered. Alternatively, other low-cost, accessible treatments for college students with PTSD symptoms and problem drinking should be evaluated. Specifically, interventions that address the needs of college students who drink to cope is critical, as there is evidence from the current study that coping drinking motives lead to greater PTSD symptoms and more negative drinking consequences. Students who drink to cope may benefit from treatment that focuses on the function of their drinking and addresses PTSD symptoms, while teaching more adaptive ways to cope with these symptoms. Successfully treating individuals during college may allow them to transition into adulthood with a greater capacity to lead meaningful and rewarding lives.
Table 5.
Generalized Estimating Equation Predicting Negative Drinking Consequences (N = 75)
| Parameter | Coefficient | Rate Ratio | S.E. | 95% CI |
|---|---|---|---|---|
| Intercept | −0.12 | 0.89 | 0.47 | [−1.04, 0.80] |
| Time | −0.27 | 0.76 | 0.35 | [−0.95, 0.41] |
| Condition | 0.23 | 1.26 | 0.19 | [−0.15, 0.61] |
| Time × Condition | −0.02 | 0.98 | 0.19 | [−0.39, 0.35] |
| Social drinking motives | 0.05 | 1.05 | 0.03 | [−0.01, 0.10] |
| Coping drinking motives | 0.07 | 1.07 | 0.02 | [0.03, 0.11]*** |
| Enhancement drinking motives | −0.02 | 0.98 | 0.03 | [−0.07, 0.04] |
| Conformity drinking motives | 0.00 | 1.00 | 0.02 | [−0.05, 0.05] |
Note.
p <.05,
p <.01,
p <.001
Acknowledgments:
This paper is derived from a doctoral thesis by Helen Valenstein-Mah submitted to the University of Washington.
Funding: This study was funded by the National Institute on Alcohol Abuse and Alcoholism (F31AA023420–01A1).
Footnotes
Ethical approval: All study procedures involving human participants were in accordance with the ethical standards of the University of Washington Institutional Review Board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflict of Interest: The authors declare that they have no conflicts of interest.
References
- Arbisi PA, Kaler ME, Kehle-Forbes SM, Erbes CR, Polusny MA, & Thuras P (2012). The predictive validity of the PTSD Checklist in a nonclinical sample of combat-exposed National Guard troops. Psychological Assessment, 24, 1034–1040. [DOI] [PubMed] [Google Scholar]
- Atkins DC, Baldwin SA, Zheng C, Gallop RJ, & Neighbors C (2013). A tutorial on count regression and zero-altered count models for longitudinal substance use data. Psychology of Addictive Behaviors, 27, 166–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, & Toney L (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13, 27–45. [DOI] [PubMed] [Google Scholar]
- Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu SM, & Olfson M (2008). Mental health of college students and their non-college-attending peers: Results from the national epidemiologic study on alcohol and related conditions. Archives of General Psychiatry, 65, 1429–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland JM, & Altman DG (1994). Statistics notes: Some examples of regression towards the mean. The BMJ, 309, 780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The Posttraumatic Stress Disorder Checklist for (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28, 489–498. [DOI] [PubMed] [Google Scholar]
- Bowen S, & Kurz AS (2012). Between-session practice and therapeutic alliance as predictors of mindfulness after mindfulness-based relapse prevention. Journal of Clinical Psychology, 68, 236–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, & Ryan RM (2003). The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84, 822–848. [DOI] [PubMed] [Google Scholar]
- Cohen J (1992). A power primer. Psychological Bulletin, 112, 155–159. [DOI] [PubMed] [Google Scholar]
- Collins RL, Parks GA, & Marlatt GA (1985). Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology, 53, 189–200. [DOI] [PubMed] [Google Scholar]
- Cooper Lynne, M. (1994). Motivations for alcohol use among adolescents: Development and validation of a four- factor model. Psychological Assessment, 6, 117–128. [Google Scholar]
- Debell F, Fear NT, Head M, Batt-Rawden S, Greenberg N, Wessely S, & Goodwin L (2014). A systematic review of the comorbidity between PTSD and alcohol misuse. Social Psychiatry and Psychiatric Epidemiology, 49, 1401–1425. [DOI] [PubMed] [Google Scholar]
- Dube P, Kurt K, Bair MJ, Theobald D, & Williams LS (2010). The P4 screener: Evaluation of a brief measure for assessing potential suicide risk in 2 randomized effectiveness trials of primary care and oncology patients. Primary Care Companion to The Journal of Clinical Psychiatry, 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisen SV, Normand SL, Belanger AJ, Spiro A, & Esch D (2004). The Revised Behavior and Symptom Identification Scale (BASIS-R): Reliability and validity. Medical Care, 42, 1230–1241. [DOI] [PubMed] [Google Scholar]
- Enkema MC, & Bowen S (2017). Mindfulness practice moderates the relationship between craving and substance use in a clinical sample. Drug and Alcohol Dependence, 179, 1–7. [DOI] [PubMed] [Google Scholar]
- Gray M, Litz B, Hsu J, & Lombardo T (2004). Psychometric properties of the life events checklist. Assessment, 11, 330–341. [DOI] [PubMed] [Google Scholar]
- Hilton L, Maher AR, Colaiaco B, Apaydin E, Sorbero ME, Booth M, … & Hempel S (2017). Meditation for posttraumatic stress: Systematic review and meta-analysis. Psychological Trauma: Theory, Research, Practice, and Policy, 9, 453–460. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Grossman P, & Hinton DE (2011). Loving-kindness and compassion meditation: Potential for psychological interventions. Clinical Psychology Review, 31, 1126–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt J, & Eisenberg D (2010). Mental health problems and help-seeking behavior among college students. Journal of Adolescent Health, 46, 3–10. [DOI] [PubMed] [Google Scholar]
- IBM Corp. Released 2010. IBM SPSS statistics for MAC, Version 19.0 Armonk, NY: IBM Corp. [Google Scholar]
- Kabat-Zinn J (1994). Wherever you go, there you are: Mindfulness meditation in everyday life. New York, NY: Hyperion. [Google Scholar]
- Kearney DJ, Malte CA, McManus C, Martinez ME, Felleman B, & Simpson TL (2013). Loving-kindness meditation for posttraumatic stress disorder: A pilot study. Journal of Traumatic Stress, 26, 426–434. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, & Wittchen HU (2012). Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research, 21, 169–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, & Best CL (2003). Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of Adolescents. Journal of Consulting and Clinical psychology, 71, 692–700. [DOI] [PubMed] [Google Scholar]
- Krebs CP, Lindquist CH, Warner TD, Fisher BS, & Martin SL (2009). College women’s experiences with physically forced, alcohol-or other drug-enabled, and drug-facilitated sexual assault before and since entering college. Journal of American College Health, 57, 639–649. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, & Engels R (2005). Why do young people drink? A review of drinking motives. Clinical Psychology Review, 25, 841–861. [DOI] [PubMed] [Google Scholar]
- Li W, Howard MO, Garland EL, McGovern P, & Lazar M (2017). Mindfulness treatment for substance misuse: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 75, 62–96. [DOI] [PubMed] [Google Scholar]
- Liang KY, & Zeger SL (1986). Longitudinal data analysis using generalized linear models. Biometrika, 73, 13–22. [Google Scholar]
- MacLean MG, & Lecci L (2000). A comparison of models of drinking motives in a university sample. Psychology of Addictive Behaviors, 14, 83–87. [DOI] [PubMed] [Google Scholar]
- McCauley JL, Killeen T, Gros DF, Brady KT, & Back SE (2012). Posttraumatic stress disorder and co-occurring substance use disorders: Advances in assessment and treatment. Clinical Psychology: Science and Practice, 19, 283–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mermelstein LC, & Garske JP (2015). A brief mindfulness intervention for college student binge drinkers: A pilot study. Psychology of Addictive Behaviors, 29, 259–269. [DOI] [PubMed] [Google Scholar]
- Miranda R, Meyerson LA, Long PJ, Marx BP, & Simpson SM (2002). Sexual assault and alcohol use: Exploring the self-medication hypothesis. Violence and Victims, 17, 205–217. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Hart SL, Howard I, Julian L, Vella L, Catledge C, & Feldman MD (2006). Barriers to psychotherapy among depressed and nondepressed primary care patients. Annals of Behavioral Medicine, 32, 254–258. [DOI] [PubMed] [Google Scholar]
- Monahan CJ, McDevitt-Murphy ME, Dennhardt AA, Skidmore JR, Martens MP, & Murphy JG (2013). The impact of elevated posttraumatic stress on the efficacy of brief alcohol interventions for heavy drinking college students. Addictive Behaviors, 38, 1719–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff K (2003). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2, 85–101. [Google Scholar]
- Ouimette P, Read JP, Wade M, & Tirone V (2010). Modeling associations between posttraumatic stress symptoms and substance use. Addictive Behaviors, 35, 64–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pineles SL, Mostoufi SM, Ready CB, Street AE, Griffin MG, & Resick PA (2011). Trauma reactivity, avoidant coping, and PTSD symptoms: A moderating relationship? Journal of Abnormal Psychology, 120, 240–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Colder CR, Merrill JE, Ouimette P, White J, & Swartout A (2012). Trauma and posttraumatic stress symptoms predict alcohol and other drug consequence trajectories in the first year of college. Journal of Consulting and Clinical Psychology, 80, 426–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Ouimette P, White J, Colder C, & Farrow S (2011). Rates of DSM-IV-TR trauma exposure and posttraumatic stress disorder among newly matriculated college students. Psychological Trauma: Theory, Research, Practice, and Policy, 3, 148–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Wood MD, Kahler CW, Maddock JE, & Palfai TP (2003). Examining the role of drinking motives in college student alcohol use and problems. Psychology of Addictive Behaviors, 17, 13–23. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2015). National Survey on Drug Use and Health. Retrieved from: www.samhsa.gov. [PubMed]
- Schafer JL, & Graham JW (2002). Missing data: Our view of the state of the art. Psychological Methods, 7, 147–177. [PubMed] [Google Scholar]
- Scott NW, McPherson GC, Ramsay CR, & Campbell MK (2002). The method of minimization for allocation to clinical trials: A review. Controlled Clinical Trials, 23, 662–674. [DOI] [PubMed] [Google Scholar]
- Simpson TL, Lehavot K, & Petrakis IL (2017). No wrong doors: Findings from a critical review of behavioral randomized clinical trials for individuals with co-occurring alcohol/drug problems and PTSD. Alcoholism: Clinical and Experimental Research, 41, 681–702. [DOI] [PubMed] [Google Scholar]
- Simpson TL, Stappenbeck CA, Luterek JA, Lehavot K, & Kaysen DL (2014). Drinking motives moderate daily relationships between PTSD symptoms and alcohol use. Journal of Abnormal Psychology, 123, 237–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stappenbeck CA, Bedard-Gilligan M, Lee CM, & Kaysen D (2013). Drinking motives for self and others predict alcohol use and consequences among college women: The moderating effects of PTSD. Addictive Behaviors, 38, 1831–1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinci C, Peltier MR, Shah S, Kinsaul J, Waldo K, McVay MA, & Copeland AL (2014). Effects of a brief mindfulness intervention on negative affect and urge to drink among college student drinkers. Behaviour Research and Therapy, 59, 82–93. [DOI] [PubMed] [Google Scholar]
- Visted E, Vøllestad J, Nielsen MB, & Nielsen GH (2015). The impact of group-based mindfulness training on self-reported mindfulness: A systematic review and meta-analysis. Mindfulness, 6, 501–522. [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013). The Life Events Checklist for DSM-5 (LEC-5). Retrieved from: www.ptsd.va.gov.
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5). Retrieved from: www.ptsd.va.gov.
- Wechsler H, & Nelson TF (2001). Binge drinking and the American college student: What’s five drinks? Psychology of Addictive Behaviors, 15, 287–291. [DOI] [PubMed] [Google Scholar]
- White HR, & Labouvie EW (1989). Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol, 50, 30–37. [DOI] [PubMed] [Google Scholar]
- White HR, & Labouvie EW (2000). Longitudinal trends in problem drinking as measured by the Rutgers Alcohol Problem Index. Alcoholism: Clinical and Experimental Research, 24, 76A. [Google Scholar]