Abstract
Approximately 50% to 80% of individuals with posttraumatic stress disorder (PTSD) also meet criteria for major depressive disorder (MDD). Sleep disturbance is a major concern in both PTSD and MDD, and is associated with poor treatment response, poor functional outcome, and increased suicide risk. Social rhythm regularity, or the consistency of daily habitual behaviors, is theoretically linked to circadian rhythms and may be disturbed in both PTSD and MDD. The present study examined the relationship between social rhythm regularity, sleep disruption, and MDD and PTSD symptoms in a sample of veterans with comorbid PTSD and MDD. Baseline data were obtained from 56 male veterans who met DSM-IV criteria for PTSD and MDD. Veterans completed the Social Rhythm Metric (SRM), a self-report questionnaire that assesses the regularity of routines by determining how regularly individuals completed 17 different types of activities. In a linear regression model, increased minutes awake after sleep onset (WASO) was a significant predictor of increased depression scores on the Hamilton Rating Scale for Depression (p < .05). SRM scores did not significantly predict depressive symptoms, however the interaction of WASO and SRM significantly predicted depressive symptoms (p = <.05), with significant relationships found at SRM scores less than 3.62. Neither minutes awake after sleep onset, SRM scores, nor their interaction was associated with PTSD symptom severity. Social and possibly circadian rhythm regularity may represent a risk or resilience factor for individuals with comorbid PTSD and MDD. Findings highlight the importance of exploring the interactions of sleep and social/circadian rhythms in depression in order to inform continued treatment development.
Keywords: Social Rhythms, Major Depression, Posttraumatic Stress Disorder, Sleep Disturbance
Introduction
Posttraumatic stress disorder (PTSD) is a major mental health concern among veterans. Approximately 4.5% to 11.2% of Vietnam War,1 10.1% of Gulf War,2 and 23% of Operation Enduring Freedom/Operation Iraqi Freedom veterans3 are diagnosed with PTSD in a given year. In addition, 50% to 80% of individuals with PTSD also meet criteria for major depressive disorder (MDD)4,5 and are thus more likely to experience a number of poor outcomes including severe anxiety,6 suicide risk,7,8 and poor physical health-related quality of life.6 Comorbidity, particularly comorbid mental health conditions, can complicate interventions and outcomes;9 thus, research addressing modifiable processes that may be directly related to symptom severity in both disorders is critical to improving care for this vulnerable population.
One potential such process is sleep disturbance, which has been found to be relevant to the onset, severity and course of both MDD and PTSD. Sleep disturbances, including difficulty initiating and maintaining sleep, have been identified as predictors of both MDD10 and PTSD11 onset. After diagnosis, sleep disturbances are reported by up to 90% of individuals with MDD12 and PTSD.13 Sleep disturbance has been linked with maintenance of MDD,14 and, compared to MDD without sleep disturbance, is associated with lower rates of treatment response15 as well as greater risk of relapse15 and suicidality.16,17 Sleep disturbance is similarly linked to maintenance of PTSD. It has been proposed that poor sleep quality elicits greater reactivity to traumatic triggers, thus increasing avoidance behaviors.18 Additionally, Mellman19 has proposed that disturbed sleep impacts the emotional processing of traumatic memories, hampering recovery. Evidence for the role of sleep disturbance in the maintenance and severity of both MDD and PTSD is also borne out by studies demonstrating that treatment of sleep disturbance yields reductions in the severity of symptoms of MDD20,21as well as PTSD22,23. Given the prevalence of sleep disturbances in both disorders, sleep may in fact be a modifiable target for improving symptom severity in individuals with comorbid PTSD and MDD.
Another promising target is the regularity of daily routines, or social rhythms. The original social rhythm model of MDD24 theorizes that stressful life events disturb daily routines or “zeitgebers,” which are external environmental cues that entrain internal circadian rhythms. More recent research has led to a revision of this theory that specifies that circadian entrainment happens as a result of behaviors that modulate access to light exposure.25 In both iterations of the theory, however, disruption of internal circadian rhythms is thought to bring about depressive symptoms and episodes. There is abundant evidence of disturbed social and circadian rhythms in MDD;26 however, these disturbances in PTSD are relatively understudied. Among the limited evidence available in the extant literature is research showing that alterations in circadian rhythms are associated with suicidality in patients with PTSD,27 and that feedback between the circadian and stress response systems has been implicated in the risk for PTSD onset.28 From a social rhythm perspective, a pilot study of Cognitive Behavioral Social Rhythm Therapy (CBSRT) for individuals with PTSD, MDD, and sleep disturbance demonstrated that regularization of social rhythms was associated with reductions in PTSD symptoms following treatment.29
A limitation of studies examining sleep disturbance or social/circadian rhythms in psychiatric disorders is that their relative contributions to symptoms are examined, but potential interactive effects are ignored. This is perhaps because these two constructs are thought to be highly inter-correlated. Studies have shown that low social rhythm regularity is associated with increased risk of depression.26, 30 Greater social rhythm regularity has also been associated with better sleep in depressed30 and healthy31,32samples; however, sleep quality and social rhythm regularity are not always positively correlated. Monk and colleagues,33 for example, found that older adults experienced disturbed sleep relative to controls despite exhibiting greater regularity of daytime routines. To date, no study has examined how the interaction of sleep and social rhythm regularity may impact symptoms of MDD. As social rhythms represent an overarching behavioral pattern in which sleep occurs, we were interested in how sleep disturbance may impact depression as a function of social rhythm regularity. A greater understanding of this relationship, particularly in individuals with comorbid diagnoses, can help to improve intervention efforts.
The current study aimed to characterize the relationship between sleep disturbance and social rhythm regularity in their contribution to MDD and PTSD symptoms using baseline data from sample of veterans with co-occurring MDD and PTSD who were to be treated with CBSRT. Consistent with the literature, we hypothesized that greater sleep disturbance and lower social rhythm regularity would be associated with greater MDD and PTSD symptom severity. Given previous evidence of reduced depression following CBSRT in veterans with sleep disturbance, we also hypothesized that the regularity of routines could modify relationships between sleep disturbance and symptom severity, such that sleep disturbance may not be associated with MDD or PTSD symptom severity in the context of highly regular routines.
Materials and Methods
The sample for this study is comprised of participants from two treatment studies: a pilot open-case study (n = 20) and a pilot randomized controlled trial (RCT; n = 36) testing the response to Cognitive Behavioral Social Rhythm Therapy.29 Data were collected from 2009 to 2011. All study procedures were approved by the University of Arizona Human Subjects Protection Program or the Southern Arizona VA Health Care System Institutional Review Board.
Participants
Participants were 56 male veterans who met DSM-IV-TR34 criteria for (1) current PTSD, with the Criterion A exposure to trauma occurring after the age of 18; and (2) current MDD. To participate in the studies, veterans were also required to have disturbances in daily routine or sleep. Individuals who reported experiencing significant distress or impairments in functioning due to variability in their routine (i.e., a self-reported awakening, retiring, or meal time that varies by > 1 hour each day) were considered to have a daily routine disturbance. Disturbances in sleep constituted either (a) a positive DSM-IV-TR diagnosis of primary insomnia, insomnia related to PTSD, or nightmare disorder (without the PTSD exclusion) on the Duke Structured Interview for Sleep Disorders35 or (b) a Pittsburgh Sleep Quality Index (PSQI)36 global score > 5 (Buysse et al., 1989) or PSQI PTSD Addendum37 score > 3 (Germain et al., 2005). A full clinical sleep interview was conducted if the participant’s responses on self-reports indicated a primary sleep disorder to exclude potential participants with strong suspicion of sleep disordered breathing, restless leg syndrome, narcolepsy, circadian rhythm disorders, and parasomnias (note that nightmare disorder was not diagnosed in the presence of PTSD). If not excluded based on semi-structured interview, subjects then participated in an overnight sleep study to rule out primary sleep disorders. Studies were scored in accordance with the American Academy of Sleep Medicine Manual for the Scoring of Sleep and Associated Events38 utilizing 30 second epochs and reviewed by physicians who were board-certified in sleep medicine. Participants were excluded if they had a respiratory distress index ≥ 3039 or a periodic limb movement index ≥ 25.40
To maintain a representative sample of individuals with PTSD, participants were not excluded if they had mild sleep disorders or mild traumatic brain injuries (mTBI), as these disturbances are often comorbid with PTSD. Patients were excluded if they sustained moderate or severe TBI (e.g., altered or loss of consciousness > 30 minutes, posttraumatic amnesia > 24 hours) or if the mTBI occurred within the last 3 months.41 Individuals were included in the analysis if they had at least four days of data to compute a Social Rhythm Metric score.
Procedure
Participants were screened for PTSD and MDD diagnoses using the Structured Clinical Interview for the DSM IV-TR (see Measures). Severity of symptoms was assessed with the Clinician Administered PTSD Scale for the DSM-IV-TR (CAPS) and the Hamilton Rating Scale for Depression (HRSD). Once sleep disorders were ruled-out via overnight sleep study, participants were trained on the Social Rhythm Metric and daily sleep diary and instructed to complete the measures for 7 days. All participants were required to telephone the results of their daily sleep diary every morning to the study phone line. Staff phoned participants who did not call-in their results. These procedures were put in place to minimize retrospective recall bias.
Measures
All research staff completed structured training programs for the completion of diagnostic and clinical interviews. Raters were considered competent when they achieved independent scores of videotaped interviews that were within 1 point of the reference score for each item and a total summed score within 4 points of the reference total score. The reference score was provided by a licensed clinical psychologist with 10+ years of clinical and research experience providing PTSD care within the VA (PLH). Upon achieving competency, all raters had to establish an interclass correlation coefficient (ICC) of >.80 with reference ratings for an additional 3 videotaped interviews. Thereafter, raters participated in weekly conferences for interview integrity checks to prevent rater drift, and reliability analyses were conducted at 6 month intervals.
Screening Measures.
Structured Clinical Interview for the DSM-IV.
The SCID42 is a standardized semi-structured interview for diagnosing DSM-IV-TR (formerly) Axis I mental disorders. The SCID has been shown to have adequate reliability and validity for most diagnoses, and it is considered the gold standard for psychiatric diagnostic assessment.
Duke Structured Interview for Sleep Disorders35
The DSI is a standardized, semi-structured interview for diagnosing both DSM-IV-TR and International Classification for Sleep Disorder-2 current and lifetime sleep disorders.
Pittsburgh Sleep Quality Index (PSQI) with Addendum36,37.
The PSQI is a self-report measure used to assess sleep quality and sleep disturbances over a one-month period of time. The 7-item addendum assesses the frequency of disruptive nocturnal behaviors commonly reported by PTSD patients (Germain et al., 2005).
Outcome Measures
Hamilton Rating Scale for Depression (HRSD). 43
The HRSD is a clinician-rated assessment of depressive symptoms with adequate internal reliability, convergent and discriminant validity.44 The current study utilized the standard 17-item version with the sleep items removed (e.g., items 4 [early insomnia], 5 [middle insomnia], and 6 [late insomnia]). Total scores range from 0 to 52.
Clinician Administered PTSD Scale for the DSM-IV-TR (CAPS) 45
The CAPS is a clinician-administered, structured interview of PTSD symptomatology developed by the National Center for PTSD that is considered a reliable and valid measure of PTSD symptom severity.46 Sleep items were removed for analyses (e.g., item 2 - experiencing unpleasant dreams, waking from dreams and having difficulty getting back to sleep). Scores range from 0 to 120.
Daily Sleep Diary.
A daily sleep diary was used to record subjective sleep/wake behaviors. In the morning upon waking, participants recorded information about their sleep from the previous night including what time they got into bed, the time they intended to begin sleeping, the time of their final morning awakening, and what time they arose from bed in the morning. They also recorded their own estimates of the time it took them to fall asleep (sleep onset latency), the time they spent asleep during the night (total sleep time), the number of awakenings they experienced in the middle of the night and the length of these awakenings, whether or not they took daytime naps, nightmare intensity and frequency, and subjective sleep quality every day for the previous night. Data were included if participants completed a minimum of four nights on the daily sleep diary to reflect the majority of the week. Average days’ completion across the sample was 6.69 days (SD = .69).
Social Rhythm Metric (SRM). 47
The SRM is a daily self-report measure designed to assess social rhythms in a manner similar to a daily sleep diary. Participants are asked to report when and with whom 18 different types of events occurred; two of which are “write-ins” to represent two additional activities he/she performs at least three times per week that are not otherwise represented on the questionnaire. Participants completed the SRM each evening prior to going to sleep. SRM scores were derived based on the Monk et al. algorithm,47 using up to 7 days’ worth of logs analyzed as a single unit. Range of possible scores for the SRM are 0 – 7. Participants completed the SRM for 1 week. An individual’s SRM score is representative of the regularity of an individual’s life, with greater scores indicating greater regularity of daily routines. Data were included for participants who completed a minimum of 4 days of recording as this represented the majority of the week. Average days’ completion across the sample was 6.68 (SD = .72).
Data Analysis
Analyses were conducted using SPSS Version 25 (SPSS Inc., Chicago, IL, USA). To limit multiple testing, we operationalized sleep disturbance as indices of sleep onset latency and wake after sleep onset (WASO) derived from self-reported daily sleep diaries. These indices were selected for several reasons: they are clinical targets used for assessing insomnia severity and frequency,48 within our sample, they were significantly correlated with other indices of sleep disturbance (e.g., total sleep time, sleep quality, ps <.03), and they were not derived from other indices of sleep disturbance (e.g., sleep efficiency, which is a ratio of time in bed and total sleep time). Analyses were conducted using multiple linear regression with all sleep items and SRM scores plus interactions of SRM and onset latency and WASO as independent variables. Conditional effects of SRM scores on the depression/insomnia relationship were obtained using the PROCESS syntax from Preacher and Hayes49 using Johnson- Neyman50 output to obtain region of significance for continuous moderators. Separate models were used to predict HRSD and CAPS symptoms.
Results
Descriptive Statistics
On average, participants were 52.2 years old (SD = 11.8 years), predominantly Caucasian (70%) and predominantly veterans of the Vietnam War (57%). Participants presented with moderate to severe symptoms of MDD (HSRD M = 22.0; SD = 5.2) and PTSD (CAPS M = 73.4; SD = 19.4). There were no significant differences between the pilot and RTC samples on any clinical variable. For the purposes of analyses, sleep items were removed from the CAPS and HRSD to avoid double counting the effects of sleep disturbance on symptom severity (HRSD without sleep problems M =18.0 SD =4.6; CAPS without sleep items M =62.6; SD =17.7). The average MDD and PTSD symptom severity calculated without corresponding sleep disturbance items still met severe thresholds (e.g., “moderate” CAPS and HRSD ranges are 40–59 and 14–18 respectively; “severe” CAPS and HRSD ranges are ≥ 60 and ≥ 19 respectively).
Average SRM scores of participants was 3.10 (SD = 1.00). As social rhythm regularity is typically only studied in psychiatric samples, a “healthy” level of social rhythm regularity is not often reported in the literature. However, in one study of 1249 subjects, social rhythm metric scores in a healthy population demonstrated average scores of 3.48 during a typical week.51 A single-sample t-test revealed the mean SRM scores in our sample are significantly lower than those of healthy individuals (t = −2.75, p <.05); and 58.9% of our sample had SRM scores below 3.48. Complete means and standard deviations of demographic and clinical variables are presented in Table 1.
Table 1.
Clinical and demographic characteristics of study sample (n=56).
| Demographic/Clinical | Mean (SD) |
|---|---|
| Age | 52.24 (11.79) |
| HRSD | 22.01 (5.22) |
| HRSD without sleep items | 17.99 (4.57) |
| CAPS | 73.42 (19.38) |
| CAPS without sleep items | 62.55 (17.68) |
| SRM | 3.11 (1.01) |
| Sleep Onset Latency (minutes) | 46.23 (52.06) |
| Wake After Sleep Onset (minutes) | 46.72 (47.08) |
| Gender/Ethnicity | n (%) |
| Male | 56 (100%) |
| Caucasian | 39 (70%) |
| Hispanic | 11 (20%) |
| African American | 1 (1.8%) |
| Pacific Islander | 1 (1.8%) |
| Native American | 2 (3.6%) |
| Other | 2 (3.6%) |
| Military Era | n (%) |
| Vietnam | 32 (57.1%) |
| OEF/OIF | 11 (19.6%) |
| Gulf War/Desert Storm | 7 (12.5%) |
| Other | 6 (10.7%) |
CAPS = Clinician Rated PTSD Scale; HRSD = Hamilton Rating Scale for Depression; OEF/OIF = Operation Enduring Freedom/Operation Iraqi Freedom; SRM = Social Rhythm Metric
Depressive Symptoms
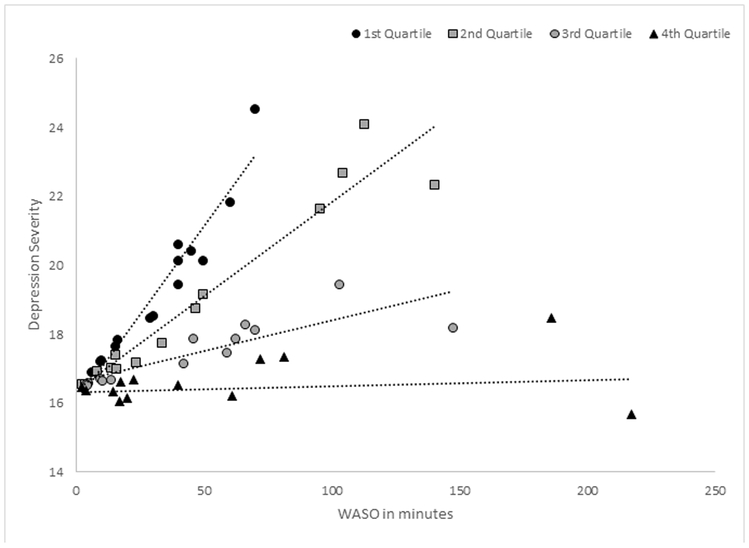
In the linear model predicting MDD symptom severity, greater wake time after sleep onset (B = .150; p <0.05) was associated with greater depression severity, such that for every minute of time spent awake after sleep onset, depression scores will increase by .15 points. Greater sleep onset latency did not significantly predict depressive symptoms, nor did social rhythm regularity. Although social rhythm regularity did not independently predict depressive symptom severity, the interaction of social rhythm regularity with wake after sleep onset was significant (B = −0.036, p <0.05 ). Visual review of the Johnson-Neyman region of significance output from the PROCESS macro revealed that greater time spent awake after sleep onset significantly related to depressive symptoms only when SRM scores were below 3.62. Scores below this threshold reflect a majority of the third and all of the fourth quartiles of SRM scores in the sample (see Figure 1).
Figure 1. Interaction of wake after sleep onset and social rhythm regularity predicting depression severity.
The 1st quartile represents the lowest 25% of social rhythm regularity scores among participants; the 4th quartile represents the highest 25% of social rhythm regularity scores among participants. WASO is significantly related to depression severity in 62.5% of the sample, from the first to within approximately mid-way through the 3rd quartile of SRM values. WASO was derived from daily sleep diaries; Depression severity was derived from the Hamilton Rating Scale for Depression with the sleep items removed.
PTSD Symptoms
No indices of sleep disturbance or social rhythms, nor their interaction, were significantly associated with PTSD symptoms. See Table 2 for complete results.
Table 2.
Sleep disturbance and social rhythm regularity predicting depression and PTSD symptom severity.
| Predicting Depression Severity | ||||||
|---|---|---|---|---|---|---|
| B | S.E. | t | p | Lower C.I. | Upper C.I. | |
| Social Rhythm Metric | −.765 | .814 | −.939 | .352 | −2.398 | .869 |
| Sleep Onset latency | .028 | .030 | .925 | .359 | −.033 | .088 |
| SRM*SOL Interaction | −.005 | .016 | −.327 | .745 | −.037 | .026 |
| Social Rhythm Metric | .013 | .838 | .015 | .988 | −1.668 | 1.694 |
| Wake After Sleep Onset | .150 | .056 | 2.699 | .009 | .038 | .261 |
| SRM*WASO Interaction | −.036 | .015 | −2.385 | .021 | −.066 | −.006 |
| Predicting PTSD Severity | ||||||
| B | S.E. | t | p | Lower C.I. | Upper C.I. | |
| Social Rhythm Metric | −2.775 | 3.253 | −.853 | .398 | −9.307 | 3.757 |
| Sleep Onset latency | .103 | .121 | .853 | .398 | −.139 | .346 |
| SRM*SOL Interaction | −.041 | .063 | −.655 | .515 | −.167 | .085 |
| Social Rhythm Metric | −4.222 | 3.522 | −1.199 | .236 | −11.293 | 2.850 |
| Wake After Sleep Onset | .120 | .234 | .514 | .610 | −.349 | .589 |
| SRM*WASO Interaction | −.020 | .063 | −.311 | .757 | −.147 | .108 |
SOL = sleep onset latency; SRM = social rhythm metric; WASO = wake after sleep onset
Discussion
The present study examined the associations of sleep disturbance and social rhythms with MDD and PTSD symptoms in veterans with comorbid diagnoses. We found partial support for our hypotheses. While social rhythm regularity was not significantly associated with MDD or PTSD symptom severity, greater levels of wakefulness after sleep onset were associated with greater levels of depressive symptoms. Additionally, social rhythm regularity significantly interacted with wakefulness after sleep onset to predict MDD severity but not PTSD severity. Specifically, wakefulness after sleep onset was only significantly associated with MDD symptom severity when social rhythm regularity was low. The point at which WASO becomes significantly associated with MDD severity is at an SRM score of approximately 3.6. As mentioned previously, the average SRM score of healthy individuals has been reported to be approximately 3.5.51 Thus, it appears that even slight reductions in “healthy” levels of routine regularity may make an individual with wakefulness after sleep onset more prone to depressive symptoms. This is a relationship that warrants further research in longitudinal studies.
The cross-sectional nature of the analyses prohibits causal interpretations; however it is helpful to consider hypotheses for future longitudinal studies. It is possible that activities that individuals engage in when awake during the middle of the night (e.g., using electronics and exposing themselves to light, ruminating in bed) may extend their wakefulness, make it difficult for them to have a consistent wake time, and cause a domino effect of future social rhythm irregularity leading to worsening of depressive symptoms. As Haynes and colleagues (2016) have suggested,25 access to light exposure can influence circadian entrainment. In this way, mid-sleep light exposure may have direct effects on internal circadian rhythms leading to depressive symptoms in vulnerable individuals. Conversely, individuals with strong social rhythms may avoid altering their schedules greatly even in the face of continued mid-sleep awakenings, thus preventing the disruption of internal circadian rhythms and, hypothetically, the onset of depressive symptoms. The plausibility of these explanations as well as the direction of effects should be pursued in future research.
Our results suggest that social and possibly, by extension, circadian rhythm regularity may represent a risk/resilience factor for individuals with PTSD and MDD. It follows that treatment of sleep disturbance in individuals with PTSD and MDD that also emphasizes stability of daily routines may be particularly useful. Indeed, a possible mechanism of the aforementioned CBT-I is the stabilization of routines elicited through stimulus control strategies and regularization of the sleep/wake cycle. This is of course speculative, but a hypothesis that may be worth pursuing in future studies.
This study has several important strengths. First, this study examined the interaction of social rhythm regularity and sleep disturbance rather than focusing only on the relationship of one or the other to depression symptom severity. The relationship of sleep, social rhythms and depression is likely complex, and thus advances in treatments for MDD will be advanced by examining these factors in an interactive manner. Second, severity of MDD and PTSD was clinician-rated rather than self-reported, and the outcome variables of symptom severity were independent of the contribution of sleep disturbance, thus limiting the potential confound of the fact that sleep disturbance comprises diagnostic criteria for both disorders. Finally, sleep and social rhythm regularity were recorded on a daily basis, thus limiting the effects of retrospective bias. These strengths notwithstanding, there were also limitations. First, the sample is entirely male, which limits generalizability and misses the contributions of sex differences to sleep and circadian functioning. Future studies should incorporate both sexes. Unlike symptom severity, sleep disturbance was entirely self-reported via daily sleep diaries. As individuals with insomnia have been shown to over-report time spent awake relative to objective measures of sleep (e.g., actigraphy or polysomnography);52 it is possible that findings would be different with objective measures of sleep. Although seven consecutive days of daily recording of social rhythms and sleep are recommended, we included individuals who had at least 4 days’ worth of recordings as they represented the majority of the week. The relationship between social and circadian rhythms is still largely theoretical; while there is evidence that both social and circadian rhythm disruption leads to depressive symptoms, the full chain of events as outlined in the social rhythm hypothesis remains unconfirmed. In our study, we conceptualized social rhythm regularity as a moderator of the sleep and depression relationship, however it is also possible to conceive of sleep disturbance as the moderating variable. For example, greater sleep disturbance could strengthen the relationship between low daily routine regularity and increased depression symptoms. As more studies examine interactive relationships of sleep and social rhythms, evidence may emerge to support one conceptualization as opposed to the other. Finally, as previously mentioned, the cross-sectional nature of the analyses prohibits the confirmation of causal hypothesis.
Together, our results suggest that future examinations of sleep and social rhythm disturbance should be examined in terms of their potential interactive relationships to depressive symptoms, and highlight the importance of better understanding the intersection of sleep and circadian rhythms in MDD. Individuals with comorbid PTSD and MDD are at increased risk for a number of poor clinical and functional outcomes. Our results support the potential of both sleep and social rhythms as independent as well as interactive treatment targets for this vulnerable population.
Acknowledgments
Funding for this research was supported by Department of Defense under Grant W81XWH-08–2-0121 (PI: Haynes) and American Sleep Medicine Foundation under Grant 37-CA-06 (PI: Haynes). Analysis and presentation of this research supported by: Department of Veterans Affairs under Grant IK2-CX001501 (PI: Boland) and National Institute of Mental Health under Grant R01 MH107571 (PI: Gehrman). The contents of this manuscript are solely the responsibility of the authors and do not represent the official views of the US government.
References
- 1.Marmar CR, Schlenger W, Henn-Haase C, Qian M, Purchia E, Li M, Corry N, Williams CS, Ho CL, Horesh D, Karstoft K, Shalev A, Kulka R. Course of Posttraumatic stress disorder 40 years after the Vietnam War: Findings from the National Vietnam Veterans Longitudinal Study. JAMA Psychiatry. 2015. 72(9):875–881. [DOI] [PubMed] [Google Scholar]
- 2.Kang HK, Natelson BH, Mahan CM, Lee KY, Murphy FM. Post-Traumatic Stress Disorder and Chronic Fatigue Syndrome-like illness among Gulf War Veterans: A population-based survey of 30,000 Veterans. Am J Epidemiol. 2003. 157(2):141–148.. [DOI] [PubMed] [Google Scholar]
- 3.Fulton JJ, Calhoun PS, Wagner HR, Schry AR, Hair LP, Feeling N, Elbogen E, Beckham JC. The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) veterans: A meta-analysis. J Affect Disord. 2015. 31:98–107. [DOI] [PubMed] [Google Scholar]
- 4.Hankin CS, Spiro III A, Miller DR, Kazis L. Mental disorders and mental health treatment among US Department of Veterans Affairs outpatients: the Veterans Health Study. Am J Psychiatry. 1999; 156(12):1924–1930. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995. 52(12):1048–1060. [DOI] [PubMed] [Google Scholar]
- 6.Kramer TL, Booth BM, Han X, Williams DK. Service utilization and outcomes in medically ill veterans with posttraumatic stress and depressive disorders. J Trauma Stress. 2003. 16(3):211–219. [DOI] [PubMed] [Google Scholar]
- 7.Conner KR, Bossarte RM, He H, Arora J, Lu N, Tu XM, Katz IR. Posttraumatic stress disorder and suicide in 5.9 million individuals receiving care in the Veterans Health Administration health system. J Affect Disord. 2014. 166:1–5. [DOI] [PubMed] [Google Scholar]
- 8.Pukay‐Martin ND, Pontoski KE, Maxwell MA, Calhoun PS, Dutton CE, Clancy CP, Hertzberg MA, Collie CF, Beckham JC. The Influence of Depressive Symptoms on Suicidal Ideation Among US Vietnam‐Era and Afghanistan/Iraq‐Era Veterans With Posttraumatic Stress Disorder. J Trauma Stress. 2012. 25(5):578–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harvey AG, Murray G, Chandler RA, Soehner A. Sleep disturbance as transdiagnostic: Consideration of neurobiological mechanisms. Clin Psychol Rev. 2011. 31(2):225–235. doi: 10.1016/j.cpr.2010.04.003) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Staner L Comorbidity of insomnia and depression. Sleep Med Rev. 2010. 14(1):35–46. [DOI] [PubMed] [Google Scholar]
- 11.Gehrman P, Seelig AD, Jacobson IG, Boyko EJ, Hooper TI, Gackstetter GD, Ulmer CS, Smith TC, Millennium Cohort Study Team. Predeployment sleep duration and insomnia symptoms as risk factors for new-onset mental health disorders following military deployment. Sleep. 2013. 36(7):1009–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsuno N, Besset A, Ritchie K. Sleep and depression. J Clin Psychiatry. 2005. 66(10): 1254–1269. [DOI] [PubMed] [Google Scholar]
- 13.Maher MJ, Rego SA, Asnis GM. Sleep disturbances in patients with post-traumatic stress disorder: epidemiology, impact and approaches to management. CNS Drugs. 2006. 20(7):567–591. [DOI] [PubMed] [Google Scholar]
- 14.Swanson LM, Hoffmann R, Armitage R. Sleep macroarchitecture in depression: Sex differences. Open Sleep J. 2010. 3(3):12–18. [Google Scholar]
- 15.Franzen PL, Buysse DJ. (2008). Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci. 2008. 10(4):473–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. 2012. 73(9):e1160–e1167. [DOI] [PubMed] [Google Scholar]
- 17.Woznica AA, Carney CE, Kuo JR, Moss TG. (2015). The insomnia and suicide link: toward an enhanced understanding of this relationship. Sleep Med Rev. 2015 22:37–46. [DOI] [PubMed] [Google Scholar]
- 18.Rothbaum BO, Mellman TA. Dreams and exposure therapy in PTSD. J Trauma Stress. 2001. 14(3):481–490. [DOI] [PubMed] [Google Scholar]
- 19.Mellman TA. Psychobiology of sleep disturbances in posttraumatic stress disorder. Ann N Y Acad Sci. 1997. 821(1):142–149. [DOI] [PubMed] [Google Scholar]
- 20.Manber R, Edinger JD, Gress JL, Pedro-Salcedo MGS, Kuo TF, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008. 31(4), 489–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taylor DJ, Lichstein KL, Weinstock J, Sanford S, Temple JR. (2007). A pilot study of cognitive-behavioral therapy of insomnia in people with mild depression. Behav Ther. 2007. 38(1):49–57. [DOI] [PubMed] [Google Scholar]
- 22.Lamarche LJ, De Koninck J. (2007). Sleep disturbance in adults with posttraumatic stress disorder: a review. J Clin Psychiatry. 2007. 68(8):1257–1270. [DOI] [PubMed] [Google Scholar]
- 23.Talbot LS, Maguen S, Metzler TJ, Schmitz M, McCaslin SE, Richards A, Perlis ML, Posner DA, Weiss B, Ruoff L, Varbel J, Neylan TC. Cognitive behavioral therapy for insomnia in posttraumatic stress disorder: a randomized controlled trial. Sleep. 2014. 37(2):327–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ehlers CL, Frank E, Kupfer DJ. Social zeitgebers and biological rhythms: a unified approach to understanding the etiology of depression. Arch Gen Psych. 1988. 45(10), 948–952. [DOI] [PubMed] [Google Scholar]
- 25.Haynes PL, Gengler D, Kelly M. Social rhythm therapies for mood disorders: an update. Curr Psychiatry Rep. 2016. 18(8):75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Germain A, Kupfer DJ. Circadian rhythm disturbances in depression. Hum Psychopharmacol. 2008. 23(7):571–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dell’Osso L, Massimetti G, Conversano C, Bertelloni CA, Carta MG, Ricca V, Carmassi C. Alterations in circadian/seasonal rhythms and vegetative functions are related to suicidality in DSM-5 PTSD. BMC Psychiatry. 2014. 14(1):352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Landgraf D, McCarthy MJ, Welsh DK. Circadian clock and stress interactions in the molecular biology of psychiatric disorders. Curr Psychiatry Rep. 2014. 16(10):483. [DOI] [PubMed] [Google Scholar]
- 29.Haynes PL, Kelly M, Warner L, Quan SF, Krakow B, Bootzin RR. Cognitive behavioral social rhythm group therapy for veterans with posttraumatic stress disorder, depression, and sleep disturbance: results from an open trial. J Affect Disord. 2016. 192:234–243. [DOI] [PubMed] [Google Scholar]
- 30.Brown LF, Reynolds III CF, Monk TH, Prigerson HG, Dew MA, Houck PR., Mazumdar S, Buysse DJ, Hoch CC, Kupfer DJ (1996). Social rhythm stability following late-life spousal bereavement: associations with depression and sleep impairment. Psychiatry Res. 1996. 62(2):161–169. [DOI] [PubMed] [Google Scholar]
- 31.Carney CE, Edinger JD, Meyer B, Lindman L, Istre T. (2006). Daily activities and sleep quality in college students. Chronobiol Int. 2006. 23(3):623–637. [DOI] [PubMed] [Google Scholar]
- 32.Monk TH, Petrie SR, Hayes AJ, Kupfer DJ. Regularity of daily life in relation to personality, age, gender, sleep quality and circadian rhythms. J Sleep Res. 1994. 3(4):196–205. [DOI] [PubMed] [Google Scholar]
- 33.Monk TH, Reynolds III CF, Machen MA, Kupfer DJ. Daily social rhythms in the elderly and their relation to objectively recorded sleep. Sleep. 1992. 15(4):322–329. [DOI] [PubMed] [Google Scholar]
- 34.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders Fourth Edition Text Revision. Washington (DC): American Psychiatric Association; 2001. [Google Scholar]
- 35.Edinger J, Wyatt JK, Olsen MK, Stetchuchak KM, Carney CE, Chiang A, Krystal AD, Lineberger MD, Means MK, Radtke RA, Knauss F. 2009. Reliability and validity of insomnia diagnoses derived from the Duke Structured Interview for Sleep Disorders. Sleep. 32: A265. [Google Scholar]
- 36.Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. 1989. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 28(2):193–213. [DOI] [PubMed] [Google Scholar]
- 37.Germain A, Hall M, Krakow B, Shear MK, Buysse DJ. 2005. A brief sleep scale for posttraumatic stress disorder: Pittsburgh Sleep Quality Index Addendum for PTSD. Journal of Anxiety Disorders, 19(2): 233–244. [DOI] [PubMed] [Google Scholar]
- 38.Iber C, Ancoli-Israel S, Chesson A, Quan SF for the American Academy of Sleep Medicine. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. Westchester (IL): American Academy of Sleep Medicine; 2007. [Google Scholar]
- 39.Loube DI, Gay PC, Strohl KP, Pack AI, White DP, Collop NA. Indications for positive airway pressure treatment of adult obstructive sleep apnea patients: a consensus statement. Chest. 1999. 115(3):863–866. [DOI] [PubMed] [Google Scholar]
- 40.American sleep disorders association. International classification of sleep disorders, revised: Diagnostic and coding manual. Rochester (MD): American Sleep Disorders Association; 1997. [Google Scholar]
- 41.Binder LM, Rohling ML, Larrabee GJ. A review of mild head trauma. Part I: Meta-analytic review of neuropsychological studies. J Clin Exp Neuropsychol. 1997. 19(3):421–431. [DOI] [PubMed] [Google Scholar]
- 42.First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition SCID-I/P. New York (NY): Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 43.Hamilton M (1960). A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960. 23(1): 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bagby RM, Ryder AG, Schuller DR, Marshall MB. The Hamilton Depression Rating Scale: has the gold standard become a lead weight? Am J Psychiatry. 2004. 161(12):2163–2177. [DOI] [PubMed] [Google Scholar]
- 45.Blake DD. A clinician rating scale for assessing current and lifetime PTSD. The CAPS-1. Behav Ther. 1990. 18:187–188. [Google Scholar]
- 46.Weathers FW, Keane TM, Davidson JR. Clinician‐Administered PTSD Scale: A review of the first ten years of research. Depress Anxiety. 2001. 13(3):132–156. [DOI] [PubMed] [Google Scholar]
- 47.Monk TK, Flaherty JF, Frank E, Hoskinson K, Kupfer DJ. The Social Rhythm Metric: An instrument to quantify the daily rhythms of life. J Nerv Ment Dis. 1990. 178(2):120–126. [DOI] [PubMed] [Google Scholar]
- 48.Lineberger MD, Carney CE, Edinger JD, Means MK. Defining insomnia: Quantitative criteria for insomnia severity and frequency. Sleep. 2006. 29(4): 479–485. [DOI] [PubMed] [Google Scholar]
- 49.Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. [White paper]. 2012. Retrieved from http://afhayes.com/public/process2012.pdf. [Google Scholar]
- 50.Preacher KJ, Curran PJ, Bauer DJ. (2006). Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006. 31(4):437–448. [Google Scholar]
- 51.van Tienoven TP, Minnen J, Daniels S, Weenas D, Raaijmakers A, Glorieux I. Calculating the social rhythm metric (SRM) and examining its use in interpersonal social rhythm therapy (IPSRT) in a healthy population study. Behav Sci. 2014. 4(3):265–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vallières A, Morin CM. Actigraphy in the assessment of insomnia. Sleep. 2003. 26:902–6. [DOI] [PubMed] [Google Scholar]