Abstract
Background:
Recent evidence suggests that higher levels of residential greenness may contribute to better mental health. Despite this, few studies have considered its impact on depression, and most are cross-sectional.
Objective:
The objective of this study was to examine surrounding residential greenness and depression risk prospectively in the Nurses’ Health Study.
Methods:
A total of 38,947 women (mean age throughout follow-up 70 y [range 54–91 y]) without depression in 2000 were followed to 2010. Residential greenness was measured using the satellite-based Normalized Difference Vegetation Index (NDVI) and defined as the mean greenness value within and radii of the women’s residences in July of each year. Incidence of depression was defined according to the first self-report of either physician-diagnosed depression or regular antidepressant use. We used Cox proportional hazards models to examine the relationship between greenness and depression incidence and assessed physical activity as a potential effect modifier and mediator.
Results:
Over 315,548 person-years, 3,612 incident depression cases occurred. In multivariable-adjusted models, living in the highest quintile of residential greenness within was associated with a 13% reduction in depression risk ( [95% confidence interval (CI): 0.78, 0.98]) compared with the lowest quintile. The association between greenness and depression did not appear to be mediated by physical activity, nor was there evidence of effect modification by physical activity.
Conclusions:
In this population of mostly white women, we estimated an inverse association between the highest level of surrounding summer greenness and the risk of self-reported depression. https://doi.org/10.1289/EHP1229
Introduction
In recent years, greenness, a feature of the natural environment reflective of the quantity of trees, plants, forests, parks, and gardens, has received increasing attention due to its potential health benefits. Studies have linked higher greenness to reduced obesity prevalence, reduced risk of cardiovascular disease and mortality, and improved birth outcomes (Fong et al. 2018; James et al. 2015). Green spaces may promote health by providing opportunities for physical activity (Bedimo-Rung et al. 2005); fostering social cohesion, which has been linked with better health (Dzhambov et al. 2018; Berkman et al. 2000); enhancing psychological well-being (Lee and Maheswaran 2011); and by reducing exposure to noise (Gidlöf-Gunnarsson and Öhrström 2007), air pollution (Nowak et al. 2006), and heat (Lafortezza et al. 2009), environmental stressors that have been linked with adverse health outcomes (Fong et al. 2018; James et al. 2015).
Because depression is the fourth leading cause of disability globally, can precipitate or exacerbate comorbidities, and adversely affects a range of outcomes including educational attainment, employment, and marital stability (Kessler 2012), identifying modifiable environmental features to help prevent depression is a priority. Several studies have found beneficial associations between greenness and various mental health outcomes (Fong et al. 2018; Gascon et al. 2015). Although these studies hypothesize a causal relationship, almost all are limited by being cross-sectional, including ones examining depression using self-report, psychological symptom scales, and data from electronic medical records (Beyer et al. 2014; Reklaitiene et al. 2014; Araya et al. 2007; Cohen-Cline et al. 2015; Maas et al. 2009a; Triguero-Mas et al. 2015; Wu et al. 2015; Bezold et al. 2018a, 2018b). Additionally, some of these studies relied on subjective greenness assessments rather than objective measures (Araya et al. 2007).
The mechanisms by which exposure to greenness could affect depression may relate to its hypothesized ability to modulate stress and related distress, increase levels of physical activity, and enhance social engagement. Studies have shown that greater neighborhood green space is negatively associated with perceived stress and salivary cortisol level, a biomarker of stress (Roe et al. 2013). Chronic stress has been shown to contribute to depression onset (Vinkers et al. 2014), so its amelioration by natural environments could reduce depression risk. Greenness has been associated with greater physical activity (Fong et al. 2018; James et al. 2015), and physical activity in turn has been shown to reduce both stress (Mobily 1982) and depressive symptoms (Blake 2012; Craft and Perna 2004). Thus, exercise may have direct and indirect effects in the greenness–depression relationship. Because greenness may promote opportunities for social cohesion and engagement (Sugiyama et al. 2008), and social cohesion and engagement can promote health (Dzhambov et al. 2018; Berkman et al. 2000), social networks may underlie the greenness–depression relationship as well.
The objective of this study was to estimate the association between residential greenness and the subsequent risk of developing depression in a cohort of U.S. women, adjusting for an array of potential confounders not considered in previous studies, including those shown to be related to depression in this population, such as social network strength and caregiving responsibilities. We also considered the roles of both physical activity and social engagement, which prior work has shown to be related to greenness (Bedimo-Rung et al. 2005; Sugiyama et al. 2008) and to promote mental health (Sugiyama et al. 2008). We hypothesized that greenness could promote physical activity or social engagement, thereby reducing depression risk. Thus, we assessed potential mediation by physical activity and social engagement. Because any beneficial association between greenness and depression could vary by physical activity level or by urbanicity of the environment (Annerstedt et al. 2012; Astell-Burt et al. 2013), we also assessed effect modification by physical activity and population density, which we have found to be modifiers of associations with greenness in the same cohort (James et al. 2016).
Methods
Study Population
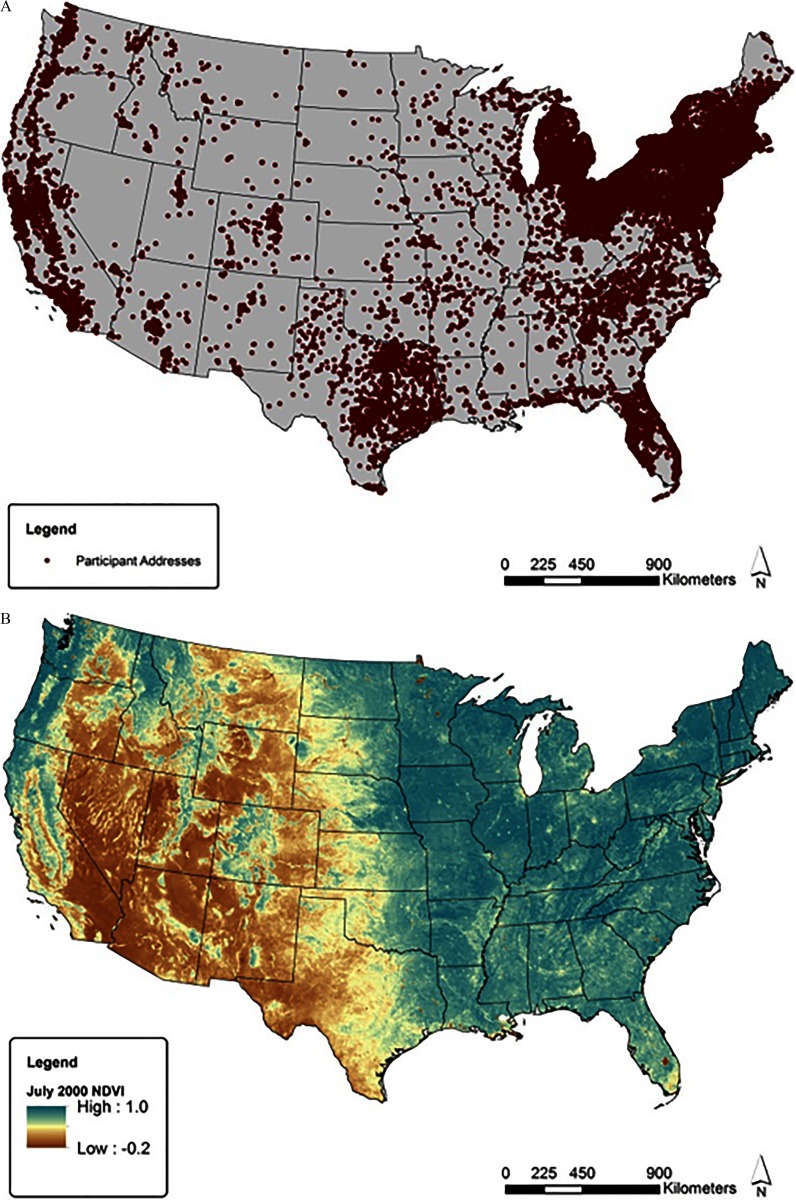
The Nurses’ Health Study (NHS) is a prospective cohort study of U.S. women established in 1976. A total of 121,701 married registered nurses 30–55 y of age and living in 11 states (California, Connecticut, Florida, Maryland, Massachusetts, Michigan, New Jersey, New York, Ohio, Pennsylvania, and Texas) enrolled by responding to an initial questionnaire on their medical history and lifestyle factors. Participants receive biennial questionnaires to collect information on risk factors and disease diagnoses (Bao et al. 2016; Colditz et al. 1997). Questionnaire mailing addresses have been geocoded and updated with changes of address to create a residential address history. By 2000, at least 10 participants were residing in each of the 48 contiguous states (Figure 1A). The study was approved by the institutional review board of Brigham and Women’s Hospital, Boston, MA, and informed consent was implied through return of the questionnaires.
Figure 1.
(A) Nurses’ Health Study addresses at baseline (2000); (B) Normalized Difference Vegetation Index (NDVI). Values based on 1 July 2000 MODIS satellite data.
The information on the greenness exposure variable we used was available starting in 2000. Thus, the current analysis included all women who, as of 2000 were alive, returning questionnaires, and had objective residential greenness information (). We excluded participants who reported being diagnosed with depression before 2000 or who had severe depressive symptoms in 1992 or 1996 as measured by the Mental Health Inventory-5 [based on a score (Ananthakrishnan et al. 2013; Arroyo et al. 2004; Cuijpers et al. 2009; Lucas et al. 2011)] () and those women who did not answer these questions on the 1992, 1996, or 2000 questionnaire, for whom depression status could not be determined (). We excluded those with cancer, diabetes, and heart disease (myocardial infarction or stroke) ever prior to baseline () because having a major chronic disease can lead to depression (Kessler 2012).
Exposure
Residential greenness was characterized objectively using the Normalized Difference Vegetation Index (NDVI), derived from imagery collected by the MODerate-resolution Spectroradiometer (MODIS) onboard NASA’s Terra satellite (Carroll et al. 2004) (Figure 1B). The sensors measure the visible light absorbed and near-infrared light reflected by vegetative growth during photosynthesis, calculating the ratio of the difference between these two measures to their sum. Values of the index range between and 1, with higher values representing greater vegetative cover. MODIS provides an image every 16 d at a pixel size (see example for July 2000 in Figure 1B).
Starting in 2000, we linked each address with an NDVI value using geographic information systems (GIS) software (ArcMap; ESRI) to estimate the mean value inside the and radii around each residence. The buffer was intended to reflect the more immediate visual environment around the nurse’s residence, whereas the buffer was intended to reflect the higher end of the distance range people may be willing to walk from their homes to an environmental feature (James et al. 2014). We considered these two buffer sizes to address uncertainty around the appropriate context for measuring residential greenness. In this study population, the highest levels of NDVI occurred in July. Therefore, we analyzed NDVI levels from July of each year of follow-up, reflecting participants’ maximal residential greenness exposure contemporaneous to each questionnaire period.
Outcome
Incident depression was defined as the first self-report of physician/clinician diagnosis of depression or new regular use of antidepressants on biennial NHS questionnaires. As part of the list of diseases on each questionnaire, participants reported whether they had newly clinician-diagnosed depression or had taken an antidepressant regularly over the past 2 y. Participants were also asked to report the time period in which they were first diagnosed or first started taking antidepressants regularly.
Covariates
Time-varying information for known and suspected risk factors for depression was available from the biennial questionnaires and such factors were considered as potential confounders. These covariates were updated as available each questionnaire cycle, and changes of address were incorporated when they occurred. In minimally adjusted models, we controlled for current age (in months), race (white, nonwhite), depressive symptoms at baseline (continuous score on Mental Health Inventory-5, reported in 2000), individual socioeconomic status [nurses’ educational attainment (registered nurse, bachelors, or masters/doctoral degree, reported in 1992), marital status (married, other), husband’s highest level of educational attainment (missing or not married, less than high school, high school graduate, or more than high school, reported in 1992)], and area-level characteristics {socioeconomic status [quintiles of Census tract median home value and median income], population density [quintiles of Census tract median population density], and air pollution [continuous 12-month average particulate matter less than in aerodynamic diameter () predicted at the residential address from spatiotemporal generalized additive mixed models] (Yanosky et al. 2014)}. In fully adjusted models, we additionally considered potential intermediates that might be on the pathway between greenness and depression, including body mass index (BMI; continuous; ), physical activity [quintiles of self-reported metabolic equivalent of task (MET) hours per week] (Wolf et al. 1994), bodily pain [none, mild, moderate, severe, or very severe, reported only in 2000, (USCB 2000)], physical function (good vs. poor, based on activities of daily living able to perform (Hagan et al. 2016), updated every 4 y), cigarette smoking [smoking status (current, former, never) and pack-years smoked (continuous)], alcohol consumption (quintiles, grams per day, updated every 4 y), social network strength based on the Berkman-Syme Index [including marital status, social contact, and group membership, updated every 4 y and categorized as low, medium-low, medium, medium-high, or high (Berkman and Syme 1979)], self-reported difficulty sleeping (reported in 2000), and regular care to ill family members (, per week of caregiving, reported in 2000) (Yanosky et al. 2014).
Statistical Analysis
We used a Cox proportional hazards model to compute hazard ratios (HRs) and 95% confidence intervals (CIs) for the association between quintiles of NDVI and risk of developing depression. The data were structured in Andersen-Gill counting process format, with a single record for each nurse in each questionnaire cycle. Nurses contributed person-time from the date of receipt of their 2000 questionnaire to the date of their last questionnaire return, occurrence of depression, death, or through 2010, whichever occurred first. We conducted ordinal tests for trend across NDVI quintiles. We used models fit with potential confounders (minimally adjusted model) as well as models adding potential causal intermediates (fully adjusted model). Missing data for covariates were incorporated into analyses using the missing-indicator method.
We evaluated both physical activity and social engagement as potential mechanisms by which greenness might affect depression incidence. Comparing models adjusted and unadjusted for physical activity or social engagement level using the publicly available %Mediate macro (https://www.hsph.harvard.edu/donna-spiegelman/software/mediate/), we estimated the proportion of the risk (and 95% CI) for depression explained by higher exposure to greenness (modeled as quintiles of NDVI) attributable to physical activity (modeled as quintiles of self-reported MET hours per week) or social engagement (modeled as indicators for each level of the Berkman-Syme Index). Briefly, the macro compares the exposure effect estimate from the full model that includes the exposure, a potential intermediate variable, and any covariates to the exposure effect estimate obtained from a partial model that leaves out the potential intermediate variable or variables. The mediation proportion is the proportion of depression risk explained by higher exposure to greenness that can be attributed to elevated levels of physical activity or social engagement. Confidence intervals for the mediation proportion were calculated using the data duplication method (Lin et al. 1997). Mediation analyses assumed that there was no unmeasured exposure–outcome confounding, no unmeasured mediator–outcome confounding, no unmeasured exposure–mediator confounding, and no mediator–outcome confounder affected by exposure (VanderWeele 2015). Although these assumptions are unverifiable, we included major confounders in our mediation analyses, and we therefore believe our assumptions are reasonable.
We also investigated effect modification by physical activity (modeled as quintiles of self-reported MET hours per week) and population density (modeled as quintiles of Census tract population density) with greenness modeled in quintiles using multiplicative interaction terms and stratified analyses (USCB 2000). We assessed the statistical significance of these interactions through partial likelihood ratio tests comparing models with the interaction term to models without the term. We also obtained modifier stratum-specific estimates of the association between depression risk and quintiles of NDVI.
Results
The 38,947 participants eligible for analysis contributed 315,548 person-years of follow-up, and 3,612 incident depression cases occurred between 2000 and 2010. The study population was, on average, 70 y of age, mostly white (95%), and mostly currently married (73%) over the follow-up period based on person-time (Table 1). The greatest proportion of study participants (82%) lived in metropolitan areas.
Table 1.
Nurses’ Health Study participant time-varying characteristics over follow-up by quintiles of contemporaneous summer Normalized Difference Vegetation Index (NDVI) within between 2000 and 2010 (). Data are or percentages unless otherwise indicated.
| Characteristic | Total | NDVI Quintile 1 ()a | NDVI Quintile 2 (0.51, 0.65) | NDVI Quintile 3 (0.65, 0.74) | NDVI Quintile 4 (0.74, 0.81) | NDVI Quintile 5 () |
|---|---|---|---|---|---|---|
| Person-years (n) | 315,548 | 63,039 | 62,956 | 63,111 | 63,174 | 63,268 |
| Age (y)b | ||||||
| BMI () | ||||||
| Smoking status | ||||||
| Never | 48 | 47 | 47 | 48 | 48 | 49 |
| Former | 46 | 47 | 46 | 46 | 46 | 45 |
| Current | 6 | 6 | 6 | 6 | 6 | 6 |
| Pack-years of smoking | ||||||
| Baseline score on MHI-5c | ||||||
| Area-level variables () | ||||||
| Census tract median income (USCB 2000) | ||||||
| Census tract median home value (USCB 2000) | ||||||
| 12-month average () | ||||||
| Race | ||||||
| Non-Hispanic white | 95 | 93 | 95 | 96 | 96 | 96 |
| All others | 5 | 7 | 5 | 4 | 4 | 4 |
| Physical activity (quintiles of MET h/week) | ||||||
| 17 | 17 | 18 | 18 | 17 | 17 | |
| 3 to | 20 | 20 | 20 | 21 | 20 | 20 |
| 9 to | 21 | 21 | 22 | 21 | 21 | 21 |
| 18 to | 15 | 15 | 14 | 14 | 15 | 15 |
| 27 | 28 | 26 | 26 | 27 | 28 | |
| Physical function | ||||||
| Poor | 53 | 53 | 54 | 54 | 53 | 52 |
| Good | 47 | 47 | 46 | 46 | 47 | 48 |
| Bodily pain (baseline) | ||||||
| Moderate, severe, or very severe | 17 | 17 | 17 | 18 | 17 | 17 |
| None, very mild, or mild | 83 | 83 | 83 | 82 | 83 | 83 |
| Alcohol consumption (g/d) | ||||||
| 0 to 4.9 | 63 | 60 | 65 | 66 | 63 | 63 |
| 33 | 36 | 32 | 31 | 34 | 33 | |
| Married | 73 | 71 | 71 | 73 | 75 | 77 |
| Educational attainment | ||||||
| RN | 68 | 61 | 69 | 70 | 70 | 69 |
| Bachelors | 21 | 26 | 21 | 20 | 20 | 20 |
| Masters or doctorate | 11 | 13 | 10 | 10 | 10 | 11 |
| Husband’s highest educationd | ||||||
| <High school | 4 | 4 | 4 | 5 | 5 | 5 |
| High school graduate | 33 | 30 | 33 | 34 | 32 | 33 |
| >High school | 49 | 51 | 47 | 48 | 49 | 49 |
| Missing or not married | 14 | 15 | 16 | 13 | 14 | 13 |
| Berkman-Syme Social Network scoree | ||||||
| Low | 12 | 10 | 12 | 13 | 12 | 12 |
| Medium-low | 20 | 20 | 21 | 21 | 21 | 20 |
| Medium | 24 | 23 | 24 | 24 | 24 | 25 |
| Medium-high | 22 | 22 | 22 | 22 | 22 | 22 |
| High | 21 | 24 | 21 | 20 | 20 | 21 |
| Care to ill family members (h/week) | ||||||
| 22 | 21 | 22 | 23 | 23 | 22 | |
| 78 | 79 | 78 | 77 | 77 | 78 | |
| Trouble sleeping | ||||||
| Some or all of the time | 28 | 28 | 28 | 28 | 28 | 28 |
| Never or little of the time | 72 | 72 | 72 | 72 | 72 | 72 |
| Population density | ||||||
| 22 | 12 | 14 | 18 | 25 | 41 | |
| 250–974 | 21 | 12 | 16 | 20 | 26 | 31 |
| 974–2,327 | 20 | 15 | 20 | 24 | 24 | 17 |
| 2,327–4,481 | 19 | 21 | 25 | 24 | 18 | 8 |
| 18 | 39 | 25 | 14 | 7 | 2 | |
| Census tract urbanicityf | ||||||
| Metropolitan | 82 | 89 | 85 | 82 | 80 | 75 |
| Micropolitan | 10 | 7 | 10 | 11 | 12 | 13 |
| Small town or rural | 7 | 5 | 5 | 7 | 8 | 13 |
Note: Values are age-adjusted, unless noted otherwise. BMI, body mass index; MET, metabolic equivalent of task; MHI-5, Mental Health Inventory-5; RN, registered nurse; SD, standard deviation.
Least green quintile based on buffer.
Value is not age-adjusted.
MHI-5 scale scores range from 0 to 100, with lower values indicating distress.
Education and husband’s education were assessed in 1992; if participants were not married, education status was classified as missing.
Social network strength based on the Berkman-Syme Index including marital status, sociability (number and frequency of social contacts), and group membership.
Urbanicity classified as metropolitan (urban area people), micropolitan (urban cluster of 10,000–49,999), or small town/rural (urban cluster of ) Census tract (USCB 2000).
In age-adjusted models for both buffer sizes, the incidence of depression was lower in the highest NDVI quintile relative to the lowest quintile, although the trend was not statistically significant ( buffer trend ; buffer trend ) (Table 2). In models including hypothesized confounders (minimally adjusted model) as well as in models including all potential confounders and possible pathway variables (fully adjusted model), the test for trend for the association between greenness and depression risk was statistically significant for the buffer. For the buffer, the risk of incident depression was 13% lower (95% CI: 0.78, 0.98) in the most compared with least green quintiles for both minimally adjusted and fully adjusted models (trend for both). For the buffer, the risk of incident depression was 10% lower (95% CI: 0.80, 1.02) in the most compared with least green quintiles in the minimally adjusted and fully adjusted models, although neither trend was statistically significant (trend , respectively).
Table 2.
Hazard ratios (HRs) and 95% confidence intervals (CIs) for the effect of residential contemporaneous summer greenness on incident depression in the Nurses’ Health Study ( with 3,612 depression cases over 315,548 person-years of follow-up, 2000–2010).
| NDVI | Cases/person-years | Age-adjusted [HR (95% CI)] | Minimally adjusted [HR (95% CI)]a | Fully adjusted [HR (95% CI)]b |
|---|---|---|---|---|
| buffer | ||||
| Quintile 1c () | 725/63,039 | Reference | Reference | Reference |
| Quintile 2 (0.51, 0.65) | 738/62,956 | 1.02 (0.92, 1.13) | 0.98 (0.88, 1.09) | 0.98 (0.88, 1.09) |
| Quintile 3 (0.65, 0.74) | 723/63,111 | 0.99 (0.90, 1.10) | 0.93 (0.84, 1.04) | 0.92 (0.83, 1.03) |
| Quintile 4 (0.74, 0.81) | 739/63,174 | 1.02 (0.92, 1.13) | 0.95 (0.85, 1.06) | 0.95 (0.84, 1.06) |
| Quintile 5 () | 687/63,268 | 0.94 (0.85, 1.05) | 0.87 (0.78, 0.98) | 0.87 (0.78, 0.98) |
| p for Trendd | — | 0.34 | 0.02 | 0.02 |
| buffer | ||||
| Quintile 1c () | 696/63,071 | Reference | Reference | Reference |
| Quintile 2 (0.53, 0.66) | 688/62,975 | 0.99 (0.89, 1.10) | 0.94 (0.84, 1.05) | 0.92 (0.82, 1.03) |
| Quintile 3 (0.66, 0.73) | 805/63,052 | 1.15 (1.04, 1.27) | 1.07 (0.96, 1.19) | 1.06 (0.95, 1.18) |
| Quintile 4 (0.73, 0.80) | 735/63,171 | 1.04 (0.93, 1.15) | 0.96 (0.86, 1.08) | 0.95 (0.84, 1.06) |
| Quintile 5 () | 688/63,279 | 0.98 (0.88, 1.10) | 0.90 (0.80, 1.02) | 0.90 (0.80, 1.02) |
| p for Trendd | — | 0.87 | 0.20 | 0.22 |
Note: BMI, body mass index; NDVI, Normalized Difference Vegetation Index; , particulate matter less than in aerodynamic diameter.
Hazard ratios are adjusted for age, race, baseline Mental Health Inventory-5 score, marital status, educational attainment, husband’s educational attainment, Census tract population density, Census tract median income, Census tract median home value, level.
Hazard ratios are adjusted for covariates in minimally adjusted , smoking status and pack-years of smoking, alcohol consumption, physical activity, physical function, bodily pain (baseline), social network strength, care to ill family members (baseline), difficulty sleeping (baseline).
Least green quintile.
Trend p derived based on ordinal quintile values.
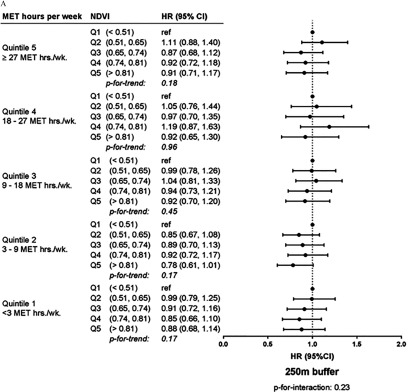
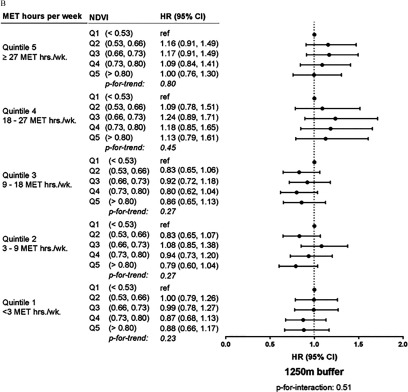
We did not observe evidence that the association between NDVI (within either buffer size) and depression was mediated by either physical activity or social engagement (see Table S1). There was no statistically significant effect modification by physical activity (Figure 2) or by population density (see Figure S1).
Figure 2.
Stratum-specific hazard ratios (HRs) and 95% confidence intervals (CIs) for the effect of residential contemporaneous summer greenness on incident depression within leisure time physical activity levels in the Nurses’ Health Study ( with 3,612 cases over 315,548 person-years of follow-up, 2000–2010). HRs are from stratified models adjusted for age, race, body mass index, smoking status and pack-years of smoking, alcohol consumption, physical function, bodily pain (baseline), marital status, social network strength, care to ill family members (baseline), difficulty sleeping (baseline), baseline mental health, educational attainment, husband’s educational attainment, Census tract population density, Census tract median income, Census tract median home value, and level (USCB 2000). MET, metabolic equivalent of task; NDVI, Normalized Difference Vegetation Index; , particulate matter less than in aerodynamic diameter; Q1, least green quintile. p for interaction from single model with interaction term.
Discussion
In this population of older, mostly white women in the United States between 2000 and 2010, participants living in the highest quintile of residential greenness had a lower risk of depression compared with those in the lowest quintile. Our finding of evidence that incidence of depression was reduced in areas with the highest compared with lowest exposures to greenness was consistent with a number of other studies considering an array of mental health outcomes (Fong et al. 2018; Gascon et al. 2015). It also generally agrees with prior studies that found beneficial associations between residential greenness and depression. These prior results were generally stronger among studies that used NDVI to characterize natural environment exposure as opposed to those that used land use databases, potentially because NDVI assesses existing vegetation, whereas land use databases may classify land types such as parks and recreational areas as natural environments even if these land types have limited vegetative coverage (Araya et al. 2007; Beyer et al. 2014; Cohen-Cline et al. 2015; Maas et al. 2009b; Reklaitiene et al. 2014; Triguero-Mas et al. 2015; Wu et al. 2015). In addition, our findings were consistent with a study in the same cohort that found a reduced risk of mortality among those living in areas with the highest residential greenness, an association that appeared to be mediated in part by reduced depression (James et al. 2016).
Several studies have explored both effect modification and mediation of associations with greenness by physical activity. Contrary to our findings, physical activity modified the greenness–mental health relationship in two studies: Annerstedt et al. (2012) found a reduced risk of poor mental health only among women who were physically active and had access to green space associated with the qualities of “serenity” and “space.” Similarly, Astell-Burt et al. (2013) showed that greater green space was associated with lower psychological distress among more physically active subjects, but not among the least active. Two other studies reported evidence suggesting that physical activity did not mediate the relationship between perceived or objective greenness and mental health (de Vries et al. 2013; Triguero-Mas et al. 2015), whereas another concluded it was a partial mediator (Sugiyama et al. 2008). In the present study, the observed association between NDVI and depression did not appear to be mediated by physical activity level, although the underlying assumptions of the mediation analysis cannot be confirmed.
Previous research has also considered social factors as mediators of the greenness–mental health relationship. Similar to our analysis, Sugiyama et al. (2008) found no evidence that social coherence mediated the relationship between greater greenness and better mental health. Conversely, in a Dutch study in which exposure data was collected through observations throughout four cities, researchers found, using the Baron and Kenny (1986) method on cross-sectional data, that social cohesion appeared to fully mediate the relationship between quantity of greenness and mental health but not the relationship between quality of greenness and mental health (de Vries et al. 2013).
Our study had several limitations. Although NDVI provides an objective measure of green space, it does not convey information about the quality or usability of the green space, and the measure is somewhat coarse at a spatial scale of . The NHS did not collect information on participants’ perceptions of their environment, so we could not assess how perceived greenness was related either to NDVI or depression incidence. Additionally, we calculated NDVI around the women’s homes, but we did not have information about their workplaces or other natural environment exposures. In general, uncertainty in this area of study persists over the appropriate location and scale for accurately measuring greenness exposures. Although we were unable to adjust for potential environmental risk factors such as noise and heat, we did adjust for urbanicity and annual average air pollution.
Depression misclassification may be a concern, as some cases of incident depression are likely to go undiagnosed or untreated, and conversely, antidepressants may be used for indications other than depression (Stearns et al. 2003)—in any case, diagnoses and prescriptions depend on clinician behavior. The incidence of new cases of depression declines with age (Kessler 2012). Therefore, excluding women with a history of depression at baseline (when the mean age of the cohort was 70 y) may have resulted in a study population of healthy survivors who were less susceptible to developing depression than women in the cohort as a whole. If greenness is truly related to lower depression risk, this may lead to more conservative findings because there would be fewer susceptible individuals in low greenness neighborhoods. Data on stress in NHS participants was limited; therefore, we did not assess stress as a potential mediator of associations between residential greenness and depression. Generalizability of this study may be limited by the fact that this population consisted of mostly white, older, professional women.
Our study also had several strengths. This is the first prospective study of greenness and depression risk in a U.S. cohort of which we are aware, and the prospective design reduces concerns about potential reverse causality. The availability of detailed follow-up information in the NHS allowed us to model risk of depression over time among those not previously depressed and to account for time-varying potential confounders such as socioeconomic status. We were also able to explore whether associations between greenness and depression appeared to differ because of or depending on physical activity level; in fact our findings suggest physical activity does not play a significant role as a mediator in the relation between green space and incident depression in this population.
Conclusions
This paper contributes to our understanding of whether greenness, a modifiable feature of the environment, may influence depression, a leading cause of global disease burden. Consistent with other studies on this topic, ours finds greater greenness to be associated with reduced incidence of depression, strengthening the evidence base supporting the greenness–mental health relationship. We did not, however, observe evidence that this association was mediated by physical activity or social engagement; further studies should explore potential mediators including stress reduction. Over half the world’s population currently lives in urban areas, with 68% projected to live in cities by 2050 (United Nations 2018). Urban green spaces have been shown to provide co-benefits to health (James et al. 2015) and social equity (McEachan et al. 2016; Markevych et al. 2014; Jenerette et al. 2011) and have been suggested as part of climate change mitigation and adaptation efforts (Beaudoin and Gosselin 2016; Buscail et al. 2012; Hudson 2012). Municipalities can enhance greenness through planning measures, which may provide actionable public health and planning interventions to promote mental health.
Supplementary Material
Acknowledgments
The research conducted for this manuscript was supported by the National Institutes of Health [Harvard–National Institute of Environmental Health Sciences (NIEHS) Environmental Epidemiology training grant T32 ES 07069; National Heart, Lung, and Blood Institute Cardiovascular Epidemiology training grant T32 HL 098048; National Cancer Institute grants K99CA201542 and UM1 CA186107; and NIEHS grants R01 ES017017 and P30 ES000002].
References
- Ananthakrishnan AN, Khalili H, Pan A, Higuchi LM, de Silva P, Richter JM, et al. . 2013. Association between depressive symptoms and incidence of Crohn’s disease and ulcerative colitis: results from the Nurses’ Health Study. Clin Gastroenterol Hepatol 11(1):57–62, PMID: 22944733, 10.1016/j.cgh.2012.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annerstedt M, Ostergren PO, Björk J, Grahn P, Skärbäck E, Währborg P. 2012. Green qualities in the neighbourhood and mental health—results from a longitudinal cohort study in Southern Sweden. BMC Public Health 12:337, PMID: 22568888, 10.1186/1471-2458-12-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araya R, Montgomery A, Rojas G, Fritsch R, Solis J, Signorelli A, et al. . 2007. Common mental disorders and the built environment in Santiago, Chile. Br J Psychiatry 190:394–401, PMID: 17470953, 10.1192/bjp.bp.106.024596. [DOI] [PubMed] [Google Scholar]
- Arroyo C, Hu FB, Ryan LM, Kawachi I, Colditz GA, Speizer FE, et al. . 2004. Depressive symptoms and risk of type 2 diabetes in women. Diabetes Care 27(1):129–133, PMID: 14693978, 10.2337/diacare.27.1.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astell-Burt T, Feng X, Kolt GS. 2013. Mental health benefits of neighbourhood green space are stronger among physically active adults in middle-to-older age: evidence from 260,061 Australians. Prev Med 57(5):601–606, PMID: 23994648, 10.1016/j.ypmed.2013.08.017. [DOI] [PubMed] [Google Scholar]
- Bao Y, Bertoia ML, Lenart EB, Stampfer MJ, Willett WC, Speizer FE, et al. . 2016. Origin, methods, and evolution of the three Nurses’ Health Studies. Am J Public Health 106(9):1573–1581, PMID: 27459450, 10.2105/AJPH.2016.303338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. 1986. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 51(6):1173–1182, PMID: 3806354, 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beaudoin M, Gosselin P. 2016. An effective public health program to reduce urban heat islands in Québec, Canada. Rev Panam Salud Publica 40(3):160–166, PMID: 27991973. [PubMed] [Google Scholar]
- Bedimo-Rung AL, Mowen AJ, Cohen DA. 2005. The significance of parks to physical activity and public health: a conceptual model. Am J Prev Med 28(2 suppl 2):159–168, PMID: 15694524, 10.1016/j.amepre.2004.10.024. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE. 2000. From social integration to health: Durkheim in the new millennium. Soc Sci Med 51(6):843–857, PMID: 10972429, 10.1016/S0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Syme SL. 1979. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol 109(2):186–204, PMID: 425958, 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- Beyer KM, Kaltenbach A, Szabo A, Bogar S, Nieto FJ, Malecki KM. 2014. Exposure to neighborhood green space and mental health: evidence from the Survey of the Health of Wisconsin. Int J Environ Res Public Health 11(3):3453–3472, PMID: 24662966, 10.3390/ijerph110303453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezold CP, Banay RF, Coull BA, Hart JE, James P, Kubzansky LD, et al. . 2018a. The association between natural environments and depressive symptoms in adolescents living in the United States. J Adolesc Health 62(4):488–495, PMID: 29273301, 10.1016/j.jadohealth.2017.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezold CP, Banay RF, Coull BA, Hart JE, James P, Kubzansky LD, et al. . 2018b. The relationship between surrounding greenness in childhood and adolescence and depressive symptoms in adolescence and early adulthood. Ann Epidemiol 28(4):213–219, PMID: 29426730, 10.1016/j.annepidem.2018.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake H. 2012. Physical activity and exercise in the treatment of depression. Front Psychiatry 3:106, PMID: 23233842, 10.3389/fpsyt.2012.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buscail C, Upegui E, Viel JF. 2012. Mapping heatwave health risk at the community level for public health action. Int J Health Geogr 11:38, PMID: 22974194, 10.1186/1476-072X-11-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll ML, DiMiceli CM, Sohlber RA, Townshend JRG. 2004. 250m MODIS Normalized Difference Vegetation Index. College Park, MD: University of Maryland. [Google Scholar]
- Cohen-Cline H, Turkheimer E, Duncan GE. 2015. Access to green space, physical activity and mental health: a twin study. J Epidemiol Community Health 69(6):523–529, PMID: 25631858, 10.1136/jech-2014-204667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colditz GA, Manson JE, Hankinson SE. 1997. The Nurses’ Health Study: 20-year contribution to the understanding of health among women. J Womens Health 6(1):49–62, PMID: 9065374, 10.1089/jwh.1997.6.49. [DOI] [PubMed] [Google Scholar]
- Craft LL, Perna FM. 2004. The benefits of exercise for the clinically depressed. Prim Care Companion J Clin Psychiatry 6(3):104–111, PMID: 15361924, 10.4088/PCC.v06n0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Smits N, Donker T, ten Have M, de Graaf R. 2009. Screening for mood and anxiety disorders with the five-item, the three-item, and the two-item Mental Health Inventory. Psychiatry Res 168(3):250–255, PMID: 19185354, 10.1016/j.psychres.2008.05.012. [DOI] [PubMed] [Google Scholar]
- de Vries S, van Dillen SM, Groenewegen PP, Spreeuwenberg P. 2013. Streetscape greenery and health: stress, social cohesion and physical activity as mediators. Soc Sci Med 94:26–33, PMID: 23931942, 10.1016/j.socscimed.2013.06.030. [DOI] [PubMed] [Google Scholar]
- Dzhambov A, Hartig T, Markevych I, Tilov B, Dimitrova D. 2018. Urban residential greenspace and mental health in youth: different approaches to testing multiple pathways yield different conclusions. Environ Res 160:47–59, PMID: 28961469, 10.1016/j.envres.2017.09.015. [DOI] [PubMed] [Google Scholar]
- Fong KC, Hart JE, James P. 2018. A review of epidemiologic studies on greenness and health: updated literature through 2017. Curr Environ Health Rep, PMID: 29392643, 10.1007/s40572-018-0179-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gascon M, Triguero-Mas M, Martínez D, Dadvand P, Forns J, Plasència A, et al. . 2015. Mental health benefits of long-term exposure to residential green and blue spaces: a systematic review. Int J Environ Res Public Health 12(4):4354–4379, PMID: 25913182, 10.3390/ijerph120404354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gidlöf-Gunnarsson A, Öhrström E. 2007. Noise and well-being in urban residential environments: the potential role of perceived availability to nearby green areas. Landsc Urban Plan 83(2–3):115–126, 10.1016/j.landurbplan.2007.03.003. [DOI] [Google Scholar]
- Hagan KA, Chiuve SE, Stampfer MJ, Katz JN, Grodstein F. 2016. Greater adherence to the Alternative Healthy Eating Index is associated with lower incidence of physical function impairment in the Nurses’ Health Study. J Nutr 146(7):1341–1347, PMID: 27170727, 10.3945/jn.115.227900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson B. 2012. Federal constitutions, global governance, and the role of forests in regulating climate change. Indiana Law J 87:1455. [Google Scholar]
- James P, Banay RF, Hart JE, Laden F. 2015. A review of the health benefits of greenness. Curr Epidemiol Rep 2(2):131–142, PMID: 26185745, 10.1007/s40471-015-0043-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James P, Berrigan D, Hart JE, Hipp JA, Hoehner CM, Kerr J, et al. . 2014. Effects of buffer size and shape on associations between the built environment and energy balance. Health Place 27:162–170, PMID: 24607875, 10.1016/j.healthplace.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James P, Hart JE, Banay RF, Laden F. 2016. Exposure to greenness and mortality in a nationwide prospective cohort study of women. Environ Health Perspect 124(9):1344–1352, PMID: 27074702, 10.1289/ehp.1510363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenerette GD, Harlan SL, Stefanov WL, Martin CA. 2011. Ecosystem services and urban heat riskscape moderation: water, green spaces, and social inequality in Phoenix, USA. Ecol Appl 21(7):2637–2651, PMID: 22073649, 10.1890/10-1493.1. [DOI] [PubMed] [Google Scholar]
- Kessler RC. 2012. The costs of depression. Psychiatr Clin North Am 35(1):1–14, PMID: 22370487, 10.1016/j.psc.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafortezza R, Carrus G, Sanesi G, Davies C. 2009. Benefits and well-being perceived by people visiting green spaces in periods of heat stress. Urban For Urban Green 8(2):97–108, 10.1016/j.ufug.2009.02.003. [DOI] [Google Scholar]
- Lee AC, Maheswaran R. 2011. The health benefits of urban green spaces: a review of the evidence. J Public Health (Oxf) 33(2):212–222, PMID: 20833671, 10.1093/pubmed/fdq068. [DOI] [PubMed] [Google Scholar]
- Lin DY, Fleming TR, De Gruttola V. 1997. Estimating the proportion of treatment effect explained by a surrogate marker. Stat Med 16(13):1515–1527, PMID: 9249922, . [DOI] [PubMed] [Google Scholar]
- Lucas M, Mirzaei F, O’Reilly EJ, Pan A, Willett WC, Kawachi I, et al. . 2011. Dietary intake of n-3 and n-6 fatty acids and the risk of clinical depression in women: a 10-y prospective follow-up study. Am J Clin Nutr 93(6):1337–1343, PMID: 21471279, 10.3945/ajcn.111.011817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maas J, van Dillen SME, Verheij RA, Groenewegen PP. 2009a. Social contacts as a possible mechanism behind the relation between green space and health. Health Place 15(2):586–595, PMID: 19022699, 10.1016/j.healthplace.2008.09.006. [DOI] [PubMed] [Google Scholar]
- Maas J, Verheij RA, de Vries S, Spreeuwenberg P, Schellevis FG, Groenewegen PP. 2009b. Morbidity is related to a green living environment. J Epidemiol Community Health 63(12):967–973, PMID: 19833605, 10.1136/jech.2008.079038. [DOI] [PubMed] [Google Scholar]
- Markevych I, Thiering E, Fuertes E, Sugiri D, Berdel D, Koletzko S, et al. . 2014. A cross-sectional analysis of the effects of residential greenness on blood pressure in 10-year old children: results from the GINIplus and LISAplus studies. BMC Public Health 14:477, PMID: 24886243, 10.1186/1471-2458-14-477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEachan RR, Prady SL, Smith G, Fairley L, Cabieses B, Gidlow C, et al. . 2016. The association between green space and depressive symptoms in pregnant women: moderating roles of socioeconomic status and physical activity. J Epidemiol Community Health 70(3):253–259, PMID: 26560759, 10.1136/jech-2015-205954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mobily K. 1982. Using physical activity and recreation to cope with stress and anxiety: a review. Am Correct Ther J 36(3):77–81, PMID: 7051794. [PubMed] [Google Scholar]
- Nowak DJ, Crane DE, Stevens JC. 2006. Air pollution removal by urban trees and shrubs in the United States. Urban For Urban Green 4(3–4):115–123, 10.1016/j.ufug.2006.01.007. [DOI] [Google Scholar]
- Reklaitiene R, Grazuleviciene R, Dedele A, Virviciute D, Vensloviene J, Tamosiunas A, et al. . 2014. The relationship of green space, depressive symptoms and perceived general health in urban population. Scand J Public Health 42(7):669–676, PMID: 25118199, 10.1177/1403494814544494. [DOI] [PubMed] [Google Scholar]
- Roe JJ, Thompson CW, Aspinall PA, Brewer MJ, Duff EI, Miller D, et al. . 2013. Green space and stress: evidence from cortisol measures in deprived urban communities. Int J Environ Res Public Health 10(9):4086–4103, PMID: 24002726, 10.3390/ijerph10094086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stearns V, Beebe KL, Iyengar M, Dube E. 2003. Paroxetine controlled release in the treatment of menopausal hot flashes: a randomized controlled trial. JAMA 289(21):2827–2834, PMID: 12783913, 10.1001/jama.289.21.2827. [DOI] [PubMed] [Google Scholar]
- Sugiyama T, Leslie E, Giles-Corti B, Owen N. 2008. Associations of neighbourhood greenness with physical and mental health: do walking, social coherence and local social interaction explain the relationships? J Epidemiol Community Health 62(5):e9, PMID: 18431834, 10.1136/jech.2007.064287. [DOI] [PubMed] [Google Scholar]
- Triguero-Mas M, Dadvand P, Cirach M, Martínez D, Medina A, Mompart A, et al. . 2015. Natural outdoor environments and mental and physical health: relationships and mechanisms. Environ Int 77:35–41, PMID: 25638643, 10.1016/j.envint.2015.01.012. [DOI] [PubMed] [Google Scholar]
- United Nations. 2018. “World Urbanization Prospects: The 2018 Revision.” https://population.un.org/wup/Publications/Files/WUP2018-KeyFacts.pdf [accessed 2 January 2019].
- (USCB) U.S. Census Bureau. 2000. Census 2000 Data for the United States. https://www.census.gov/census2000/states/us.html [accessed 7 May 2015].
- VanderWeele T. 2015. Explanation in Causal Inference: Methods for Mediation and Interaction. New York:Oxford University Press. [Google Scholar]
- Vinkers CH, Joëls M, Milaneschi Y, Kahn RS, Penninx BW, Boks MP. 2014. Stress exposure across the life span cumulatively increases depression risk and is moderated by neuroticism. Depress Anxiety 31(9):737–745, PMID: 24753162, 10.1002/da.22262. [DOI] [PubMed] [Google Scholar]
- Wolf AM, Hunter DJ, Colditz GA, Manson JE, Stampfer MJ, Corsano KA, et al. . 1994. Reproducibility and validity of a self-administered physical activity questionnaire. Int J Epidemiol 23(5):991–999, PMID: 7860180, 10.1093/ije/23.5.991. [DOI] [PubMed] [Google Scholar]
- Wu YT, Prina AM, Brayne C. 2015. The association between community environment and cognitive function: a systematic review. Soc Psychiatry Psychiatr Epidemiol 50(3):351–362, PMID: 25087013, 10.1007/s00127-014-0945-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanosky JD, Paciorek CJ, Laden F, Hart JE, Puett RC, Liao D, et al. . 2014. Spatio-temporal modeling of particulate air pollution in the conterminous United States using geographic and meteorological predictors. Environ Health 13:63, PMID: 25097007, 10.1186/1476-069X-13-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.