Abstract
Context:
Many patients with advanced serious illness or at the end of life experience delirium, a potentially reversible form of acute brain dysfunction, which may impair ability to participate in medical decision making and to engage with their loved ones. Screening for delirium provides an opportunity to address modifiable causes. Unfortunately, delirium remains under-recognized.
Objectives:
To validate the brief Confusion Assessment Method (bCAM), a 2-minute delirium screening tool, in a veteran palliative care sample.
Methods:
This was a pilot prospective observational study that included hospitalized patients evaluated by the Palliative Care service at a single Veterans’ Administration Medical Center. The bCAM was compared against the reference standard, the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Both assessments were blinded and conducted within 30 minutes of each other.
Results:
We enrolled 36 patients who were a median of 67 years old (IQR: 63 – 73). The primary reasons for admission to the hospital were sepsis or severe infection (33%), severe cardiac disease (including heart failure, cardiogenic shock, and myocardial infarction) and (17%) or gastrointestinal / liver disease (17%). The bCAM performed well against the DSM-5 for detecting delirium, with a sensitivity (95% Confidence Interval) of 0.80 (0.4, 0.96) and specificity of 0.87 (0.67, 0.96).
Conclusion:
Delirium was present in 27% of patients enrolled and never recognized by the Palliative Care service in routine clinical care. The bCAM provided good sensitivity and specificity in a pilot of palliative care patients, providing a method for non-psychiatrically trained personnel to detect delirium.
Keywords: cognition, delirium, palliative care, end-of-life, screening
Introduction
Palliative care (PC) providers frequently discuss treatment options and goals of care for patients with life threatening illnesses or those nearing the end of life. Evaluation of decision-making capacity is an essential component of PC practice. Delirium, a form of acute brain organ dysfunction characterized by inattention and changes in cognition, is a known independent risk factor for excess mortality, length of stay, cost of care, and long-term cognitive impairment.1–8 Delirium is a common, serious and potentially preventable condition that occurs in up to 88% of PC patients at the end of life, and as part of the dying process.9,10 If a patient is delirious, they are acutely cognitively impaired, therefore often lack decision-making capacity and are unable to participate fully in a goals-of-care discussion.
Early recognition of delirium amongst patients at the end of life is imperative. Notably, PC patients have diminished reserve for a burdensome delirium assessment. A valid and reliable quick screening tool that can differentiate delirium from the multiple other medical morbidities experienced by PC patients is optimal. Early identification of delirium allows for expeditious treatment. Effective treatment of delirium could allow an individual to engage meaningfully with their loved ones at the end of life and enhance their decision-making capacity (e.g., to participate in goals of care discussions, etc.).
The development of standardized methods for delirium screening in the PC population, is a necessary first step in this treatment paradigm.11,12 Brief standardized delirium assessments are an understudied part of the PC team approach for cognitive assessment for the purposes of determining decision-making capacity or to aid the patient’s ability to meaningfully interact with their loved ones at the end of life. In this pilot investigation, we set out to validate a brief delirium screening tool in a veteran PC population to improve delirium recognition in severe medical illnesses and at the end of life.
Methods
This was a pilot prospective observational study conducted at a tertiary, academic 146-bed Veterans Affairs Medical Center (VAMC). The local institutional review board reviewed the project proposal and determined it was quality improvement and did not require full board review, as the bCAM was being validated and implemented in the context of a larger quality improvement initiative to improve the recognition and treatment of delirium in Veterans on the PC service. A convenience sample of patients were enrolled. Enrollment occurred between July and December 2016 on days the psychiatrist and nurse (JW and LB) were available to perform paired evaluations of delirium. Patients were eligible for inclusion if they were admitted to the PC Unit or followed by the PC Consultation Service. Patients with a diagnosis of severe dementia, schizophrenia, or central nervous system disease (e.g., severe stroke, anoxic brain injury) were excluded from participation. Patients who met inclusion criteria were approached and verbally agreed to participate. If the patient was unable to verbalize understanding, a caregiver was approached and gave permission. No patients or caregivers who were approached for participation refused.
Measurement
The VAMC PC team (i.e., physicians, nurse practitioners, case manager, social worker) elected to utilize the Brief Confusion Assessment Method (bCAM) to evaluate patients for delirium. The bCAM is a modification of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) and intended to improve sensitivity in non-critically ill patients.13 The bCAM takes less than 2 minutes to perform and utilizes objective and subjective testing criteria to determine the presence of altered mental status or fluctuating course (Feature 1), inattention (Feature 2), altered level of consciousness (Feature 3), and disorganized thinking (Feature 4).13 A patient is considered to be delirious if both features 1 and 2 are present and either feature 3 or 4 are present. Validation of the bCAM with older Emergency Department patients demonstrated 84% sensitivity and 96% specificity when performed by a physician, and 78% sensitivity and 97% specificity when performed by a non-physician.13
For the study, two raters each independently assessed the patient for delirium. One rater (LB) performed the bCAM. She reviewed the bCAM training manual and watched instruction videos. The second assessment (reference standard) was a comprehensive psychiatric assessment of delirium, using the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), performed by a consultation liaison psychiatrist (JEW).14 The psychiatrist has over 10 years of clinical experience and routinely diagnoses delirium in clinical practice. To arrive at the diagnosis of delirium, the psychiatrist examined and interviewed the patient, spoke with the nurse and / or family members at the bedside, and reviewed the patient’s medical record before making a final determination.
The bCAM was typically performed first with the psychiatrist’s DSM-5 reference assessment performed within 30 minutes of the bCAM assessment. For most patients, we conducted a single set of paired assessments, but for twelve patients we conducted two sets of paired assessments, and for three patients we conducted three sets of paired assessments. Both assessors were blinded to each other’s determinations. Results were recorded on paper case report forms and then transferred into an Excel spreadsheet by a medical student. Data was cleaned by LB and JEW and two observations were dropped at the end of the study due to patients subsequently meeting ineligibility criteria for study participation (i.e., existing psychotic disorder or dementia.) One additional observation was dropped as the patient participated in a bCAM assessment but later refused DSM-5 assessment. Data entry was double-checked for accuracy. A medical record review was performed to collect age, race, admission diagnosis, and reason for PC consultation.
Electronic Medical Record Review
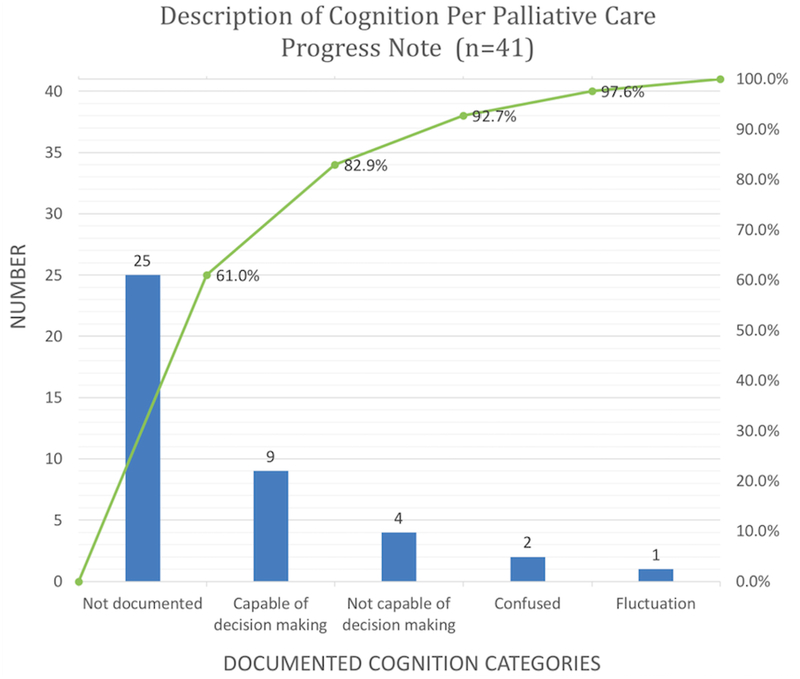
A resident physician reviewed each patient’s electronic medical record for documentation of a mental status evaluation, capacity evaluation or for evidence of consideration of delirium by the PC service. JEW and LB trained the physician to search for keywords suggestive of delirium or encephalopathy including capacity, fluctuation of mental status, confusion, etc.. Key words were collected, tallied and used to create a Pareto Chart (Figure 1).
Figure 1:
Pareto Chart Pareto chart is shown depicting count (left y-axis) and percent of time (right y-axis) that documentation regarding mental status or capacity was documented by PC service in routine delivery of medical care in the electronic medical record.
Statistical Analysis
To describe the study sample, medians and interquartile range (IQR) are utilized to report central tendency and dispersion for age, and proportions are used to present categorical variables. Sensitivity and specificity of the bCAM are presented with 95% confidence intervals (CI), using the DSM-5 assessment as the reference standard.
In order to use all available measurements while giving equal weight to each patient, before calculating sensitivity and specificity, we first down-weighted the observations from those patients with multiple observations. For example, if a patient had two observations that could be used in the sensitivity analysis, we gave each of those observations a weight of 0.5. We took the weighting into account in the calculation of confidence intervals for the sensitivity and specificity, using established survey-sampling techniques.15 All statistical analyses were performed with R statistical software (version 3.3.2; http://www.r-project.org/).
Results
Study Population
We enrolled 36 patients who underwent 41 assessments. The median age was 67 years old (IQR: 63 – 73). The majority of our patients were male, n = 34 (94%) and White, n = 26 (72%) with either a high school education, n = 12 (33%) or some college, n= 12 (33%). The primary reason for admission to the hospital was sepsis or severe infection, n = 12 (33%). The reasons for PC consult or PC admissions were goals of care, n = 28 (78%), and pain or symptom management, n = 5 (14%). Additional study demographics are listed in Table 1. We conducted a total of 44 paired assessments on the 36 patients. Three observations were dropped due to reasons already mentioned, leaving us with 41 paired assessments on 33 unique patients.
Table 1.
Demographic and Clinical Characteristics of Enrolled Patients
| N = 36 | |
|---|---|
| Age | |
| Median (IQR)* | 67 (63 – 73) |
| Gender | |
| Male^ | 34 (94%) |
| Female | 2 (6%) |
| Race | |
| White | 26 (72%) |
| Black | 7 (19%) |
| Other | 3 (8%) |
| Education | |
| No high school | 4 (11%) |
| Some high school | 3 (8%) |
| Graduated high school | 12 (33%) |
| Some college | 12 (33%) |
| Graduated college | 5 (14%) |
| Reason for Admission | |
| Sepsis (or severe infection) | 12 (33%) |
| Cardiac (heart failure, myocardial infarction, shock, etc.) | 6 (17%) |
| Gastrointestinal / Liver | 6 (17%) |
| Respiratory failure | 3 (8%) |
| Renal / Metabolic | 3 (8%) |
| Pain / Weakness | 3 (8%) |
| Cancer | 2 (6%) |
| Hip Fracture | 1 (3%) |
| Reason for Palliative Care Consultation / Admission | |
| Goals of care | 28 (78%) |
| Pain or symptom management | 5 (14%) |
| Goals of care and pain or symptom management | 3 (8%) |
Medians (IQR; Interquartile Range) were used as the data for continuous variables was not normally distributed
Proportions are utilized to present categorical data
Sensitivity and Specificity Analyses
Twelve assessments on 10 unique patients were delirious according to DSM-5 criteria. Of those considered delirious according to DSM-5 criteria, 10 were also bCAM positive, yielding a sensitivity of 0.80 (0.40, 0.96). Twenty-nine assessments on twenty-three unique patients were non-delirious according to the DSM-5 criteria. Of those considered non-delirious according to the DSM-5, twenty-five assessments were also bCAM negative, which corresponded to a specificity of 0.87 (0.67, 0.96).
Pareto Chart
A review of the electronic medical record (Figure) revealed that in the context of routine clinical care, 61% of the time (n = 25) there was no explicit mention of an evaluation by the PC service of the patient’s cognition or capacity for medical decision making suggestive of an evaluation for delirium, 32% (n = 13) documented capacity (or lack of capacity) to engage in medical decision-making, 5% (n = 2) documented “confusion,” and 2% (n = 1) documented “fluctuation” of mental status. There was no mention in any of the medical documentation by the PC service of delirium / encephalopathy, nor formal assessment of delirium, by DSM-5 criteria or validated delirium screening instrument as part of the clinical PC assessment and consult prior to or during this initiative and assessment period.
Discussion
In this pilot investigation, we sought to validate the bCAM, a brief delirium screening tool in PC patients at a single VAMC. We found that the bCAM provided good sensitivity and specificity for detecting delirium, with a sensitivity of 80% and specificity of 87%. Anecdotally, PC team members reported the bCAM to be a quick and easy tool to evaluate for delirium within the Veteran population. Delirium was not routinely screened for in this population and the presence or absence of acute mental status changes suggestive of delirium was frequently missed in routine clinical care. This discrepancy is remarkable, considering that 27% of patients (n = 10 of 36), in this pilot investigation, were delirious, according to DSM-5 criteria.
For the purpose of a comprehensive evaluation of delirium in the PC population, the DSM-5 or the International Classification of Diseases, 11th edition (ICD-11), should serve as the gold standard for a clinical diagnosis of delirium. However, in the PC setting, a comprehensive interview and examination may not be feasible nor tolerable given the severity of medical illnesses, and burden of medical interventions, especially with the shift of focus in care toward liberation from distress and suffering. Therefore, a quick bedside assessment performed by a PC team member, nursing staff, or family would be preferable to an exhaustive delirium assessment.
Previous studies have evaluated the use of the Confusion Assessment Method (CAM), Confusion Assessment for the ICU (CAM-ICU), Intensive Care Delirium Screening Checklist (ICDSC), Delirium Rating Scale (DRS), and Memorial Delirium Assessment Scale (MDAS), in advanced cancer and PC populations.16–18 The CAM and DRS were found to be sensitive (88% and 80% respectively) and specific (100% and 76% respectively) for identifying delirium, but take >15 minutes to complete.17,18 Likewise, the MDAS, primarily a delirium severity scale, was sensitive (68%) and specific (94%) for delirium in cancer patients, but takes >10 minutes to complete.18 Interestingly, the CAM-ICU and the ICDSC were shown to be specific (≥98% for both instruments) but not sensitive for delirium in a non-critically ill oncology population16.
This pilot investigation represents a first attempt to validate a brief (<2 minute) delirium screening tool in a PC cohort and was found to have good sensitivity and good specificity in this population. Our hope is that this pilot trial would encourage others to pursue, in a larger-scale format, the characterization, diagnosis and treatment / management of delirium in this vulnerable patient population. By improving our recognition of delirium at the end of life, we may be able to better optimize cognition, garnering improved patient engagement with loved ones, and with the care team, hopefully improving their ability to be meaningfully present at the end of life.
This study has several strengths. The patient sample represents a diverse set of diagnoses beyond cancer with the largest number admitted for treatment of sepsis or severe infection. The investigators completing the bCAM and DSM-5 evaluations, were blinded to one another’s assessment results, and completed the majority of paired assessments within 10 minutes of each other. Despite these strengths, the study also has important limitations. Our sample is small, largely male, Veteran-only sample and thus may not generalize to the larger PC population. In addition, the sample was one of convenience based on availability of the investigators.
Conclusion
Recognition of delirium is frequently missed in routine clinical care on the PC service. The bCAM provides good sensitivity and specificity in a pilot of PC patients, providing an efficient and effective method for non-psychiatrically trained personnel to evaluate reliably for delirium. Further investigations utilizing a larger sample are needed.
References:
- 1.Milbrandt EB, Deppen S, Harrison PL, et al. Costs associated with delirium in mechanically ventilated patients. Critical care medicine. 2004;32(4):955–962. [DOI] [PubMed] [Google Scholar]
- 2.Shehabi Y, Riker RR, Bokesch PM, et al. Delirium duration and mortality in lightly sedated, mechanically ventilated intensive care patients. Critical care medicine. 2010;38(12):2311–2318. [DOI] [PubMed] [Google Scholar]
- 3.Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA: the journal of the American Medical Association. 2004;291(14):1753–1762. [DOI] [PubMed] [Google Scholar]
- 4.Lat I, McMillian W, Taylor S, et al. The impact of delirium on clinical outcomes in mechanically ventilated surgical and trauma patients. Critical care medicine. 2009;37(6):1898–1905. [DOI] [PubMed] [Google Scholar]
- 5.Ely EW, Gautam S, Margolin R, et al. The impact of delirium in the intensive care unit on hospital length of stay. Intensive care medicine. 2001;27(12):1892–1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, van Gool WA. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA: the journal of the American Medical Association. 2010;304(4):443–451. [DOI] [PubMed] [Google Scholar]
- 7.Pandharipande PP, Girard TD, Jackson JC, et al. Delirium as an independent predictor of long-term cognitive impairment: Results from the BRAIN ICU (Bringing to light the risk factors and incidence of neuropsychological dysfunction in ICU survivors) study. Am J Respir Crit Care Med. 2013;187:A5237. [Google Scholar]
- 8.Girard TD, Jackson JC, Pandharipande PP, et al. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Critical care medicine. 2010;38(7):1513–1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Close JF, Long CO. Delirium: opportunity for comfort in palliative care. Journal of Hospice & Palliative Nursing. 2012;14(6):386–394. [Google Scholar]
- 10.Hosie A, Davidson PM, Agar M, Sanderson CR, Phillips J. Delirium prevalence, incidence, and implications for screening in specialist palliative care inpatient settings: a systematic review. Palliat Med. 2013;27(6):486–498. [DOI] [PubMed] [Google Scholar]
- 11.Lawlor PG, Davis DH, Ansari M, et al. An analytical framework for delirium research in palliative care settings: integrated epidemiologic, clinician-researcher, and knowledge user perspectives. J Pain Symptom Manage. 2014;48(2):159–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leonard MM, Nekolaichuk C, Meagher DJ, et al. Practical assessment of delirium in palliative care. J Pain Symptom Manage. 2014;48(2):176–190. [DOI] [PubMed] [Google Scholar]
- 13.Han JH, Wilson A, Vasilevskis EE, et al. Diagnosing delirium in older emergency department patients: validity and reliability of the delirium triage screen and the brief confusion assessment method. Ann Emerg Med. 2013;62(5):457–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Association AP. Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub; 2013. [DOI] [PubMed] [Google Scholar]
- 15.Lumley T Survey: Analysis of Complex Survey Samples. Journal of Statistical Software. 2004;9(1):1–19. [Google Scholar]
- 16.Neufeld KJ, Hayat MJ, Coughlin JM, et al. Evaluation of two intensive care delirium screening tools for non-critically ill hospitalized patients. Psychosomatics. 2011;52(2):133–140. [DOI] [PubMed] [Google Scholar]
- 17.Ryan K, Leonard M, Guerin S, Donnelly S, Conroy M, Meagher D. Validation of the confusion assessment method in the palliative care setting. Palliat Med. 2009;23(1):40–45. [DOI] [PubMed] [Google Scholar]
- 18.Grassi L, Caraceni A, Beltrami E, et al. Assessing delirium in cancer patients: the Italian versions of the Delirium Rating Scale and the Memorial Delirium Assessment Scale. J Pain Symptom Manage. 2001;21(1):59–68. [DOI] [PubMed] [Google Scholar]