Abstract
Home health agencies (HHAs) are one of the most commonly used third-party providers in the assisted living (AL) setting. One way ALs may be potentially able to meet the needs of their residents despite increased impairment is through supplementing the services offered with those delivered by HHAs. We explore the growth in the delivery of HHA services to Medicare beneficiaries in AL compared with other home settings between 2012 and 2014. We also examine demographic, cognitive, and functional characteristics of beneficiaries; HHA provider characteristics; and the variation in the percentage of home health use in ALs across the country. Our findings suggest that there was a slight growth in the share of HHA services being delivered in AL. HHA recipients in AL were more likely to have cognitive and activities of daily living impairments than those receiving HHA services in other settings. This is among the first studies to examine HHA utilization in AL.
Keywords: home health agency, assisted living, third-party provider, long-term care
Introduction
Approximately 32,200 assisted livings (ALs) in the United States care for close to 1 million residents annually (Centers for Medicare and Medicaid Services, 2017; Harris-Kojetin et al., 2016). ALs are defined as a “congregate residential setting that provides or coordinates personal care services, 24-hour staff supervision and assistance (scheduled and unscheduled), activities, and health-related services” (Hawes, Rose, & Phillips, 1999, p. 3). Over the past 25 years, AL has become an increasingly common housing and long-term care choice for older adults (Grabowski, Stevenson, & Cornell, 2012; Hawes, Phillips, Rose, Holan, & Sherman, 2003). These care settings serve as a long-term care option for individuals whose health (either cognitive or physical) declines to the point where they need these additional services but do not require the level of care provided in a setting such as a nursing home. Results from the 2010 National Survey of Residential Care Facilities suggest that the typical resident in AL is White, female, aged 85 years and above, and needs help with more than one activity of daily living (ADL). In addition, half suffer from two to three chronic conditions (Caffrey et al., 2012).
The majority of residents living in an AL pay privately (Kisling-Rundgren, Paul III, & Coustasse, 2016); however, a growing number of states now cover AL costs for low-income individuals enrolled in Medicaid (Metlife Mature Market Institute, 2012). The cost of AL care can vary depending on location, level of care services, and amenities provided. In 2017, the national median annual cost of a private room in an AL setting was $45,000 compared with $97,455 for a private room in a nursing home (Genworth Financial, 2018). ALs differ in their availability of services offered to residents and may also charge additional fees for providing daily living task assistance, housekeeping, organized recreational activities, coordination of health and social services, medication assistance, and transportation services. In addition, they are licensed and governed almost exclusively by state regulations rather than by federal laws (Carder, O’Keefe, & O’Keefe, 2015). Therefore, services and provisions may also vary state to state.
ALs were initially developed to help bridge the gap in services for individuals who could no longer live independently at home but did not require round-the-clock, institutionalized nursing home level of care (Zimmerman et al., 2003). Unlike nursing homes, ALs are generally not required to provide constant nursing care services and/or rehabilitative services such as physical or occupational therapy. However, older adults living in an AL are increasingly facing impairments, and many need high levels of assistance (Khatutsky et al., 2016).
Despite residents’ increased frailty and the need for 24-hour care, many prefer to stay in an AL as opposed to moving to nursing homes by a margin of six to one (Brodie & Blendon, 2001). More recent research has focused on the shift from institutional services toward long-term supports and services being provided in home and community-based settings including AL (Naylor et al., 2016; Newcomer et al., 2016; Wysocki et al., 2015). A fundamental aspect of enabling residents to remain in an AL despite increased frailty is to modify its services and the provision of care to meet residents’ shifting needs and to avoid relocating individuals to institutional care prematurely (Chapin & Dobbs-Kepper, 2001).
New Contribution
One way in which ALs are potentially able to meet the needs of their residents in order to sustain their residence despite increased impairment is through supplementing the services offered with those delivered by outside third-party providers, such as home health care agencies (HHA). HHAs are the fastest growing health care industry in the United States and are one of the most commonly used third-party providers in the AL setting (Carder et al., 2015; U.S. Bureau of Labor Statistics, 2015). HHAs allow older adults to receive services that most states do not require AL settings to provide, such as skilled nursing, therapeutic care, and social work services. Therefore, they may reduce the extent to which common triggering events, like decline in functional status, would prompt institutionalization (Konetzka, Spector, & Limcangco, 2007; Perry, Andersen, & Kaplan, 2014).
Currently, there are 12,600 HHAs staffed with registered nurses, home health aides, social workers, physical therapists, occupational therapists, and nutritionists. HHAs provide short-term medical and therapeutic services (e.g., monitoring unstable health status, wound care, diabetes care, intravenous or nutrition therapy) to individuals recovering from postsurgical events or requiring care for acute and chronic conditions in their home, including AL (Centers for Medicare and Medicaid Services, 2017). Despite the delivery of HHA services in AL, to our knowledge, there are no published studies that describe trends in HHA utilization within these settings or have examined the variation in HHA services utilized in ALs across the country. Therefore, we address this gap in the literature and explore the trends in the delivery of HHA services in AL and the percentage of HHA services provided in ALs across states. We also compare the demographic and functional characteristics of HHA users in the AL setting with those receiving HHA services in other home settings.
Method
Data Sources and Study Population
We used data from the Outcome and Assessment Information Set (OASIS) merged with the Medicare Master Beneficiary Summary File (MBSF) for the years 2012 to 2014 to examine differences between Medicare beneficiaries who received HHA services in AL and those who were identified as residing in other, non-AL settings.
The OASIS data set comprises standardized medical, nursing, and rehabilitative assessment items collected by HHAs to evaluate medical and nonmedical needs, determine reimbursement, and measure outcome-based quality improvement and follow-up (Centers for Medicare and Medicaid Services, 2009). All Medicare-certified HHAs are required to conduct OASIS survey assessments for every recipient as part of the comprehensive evaluation when they first begin care, and periodically until home health care services end. The MBSF contains demographic characteristics and Medicare and Medicaid enrollment information for all Medicare beneficiaries in the United States in each year.
To describe HHAs that serve residents in AL versus in other home settings, we linked these data with the 2014 Medicare Provider of Services File, Home Health Compare, and the Home Health Agency Utilization Payment Public Use File. Our sample included all Medicare beneficiaries aged 65 years and older with at least one OASIS Start of Care (SOC) assessment in 2014. We limited our sample to the first SOC assessment for each Medicare beneficiary in that study year.
Measures
AL residence was defined using Question M1100 (Patient living situation) on the OASIS SOC assessment. This question solicits information on where and with whom the recipient resides, and whether any levels of assistance are available in the residence. We considered the response “Patient lives in congregate situation (for example, assisted living, residential care home)” and reported “around the clock” availability of assistance to indicate residence in an AL. The other response options on question M1100, including “Patient lives alone” and “Patient lives with other person(s) in the home,” and any reported availability of assistance (around the clock, regular daytime, regular nighttime, occasional/short-term assistance, no assistance available) were considered home settings other than AL. Descriptive information such as age, gender, and race/ethnicity were determined from the MBSF. We also identified if Medicare beneficiaries received Medicaid benefits and were deemed either full or partial duals using the MBSF.
We used Question M1000 from the OASIS to determine whether or not HHA recipients were discharged in the past 14 days from an inpatient facility. Responses to this item were categorized as discharged from short-stay acute hospital, skilled/nursing facility, or other, which were not mutually exclusive. The facilities categorized as “other” include inpatient rehabilitative facility, psychiatric hospital or unit, and long-term care hospital. Cognitive, behavioral, and psychiatric impairments were also obtained from the OASIS SOC assessment. We used assessment item M1740 to determine whether the HHA recipient had any of the following symptom(s): memory deficit, impaired decision making, verbal disruption, physical aggression, socially inappropriate behavior, and delusions. We specified this variable as having occurred at least once in the past week versus not at all. We also utilized assessment items that addressed the following ADL impairments: grooming (M1800), dressing upper body (M1810), dressing lower body (M1820), bathing (M1830), toileting transfer/toilet hygiene (M1840 and M1845), transferring (M1850), ambulation/locomotion (M1860), and feeding (M1870). For each of these ADL variables, we specified impairment as whether or not an individual required any assistance from another person or device.
In reference to HHA provider characteristics, ownership type (e.g., for-profit, nonprofit, government-run) and rurality classification were obtained from the 2014 Medicare Provider of Services file. We used the 2014 Home Health Agency Public Use file to identify the total number of episodes of care (excluding low utilization payment adjustment episodes), dual eligible beneficiaries, and average age of beneficiaries per HHA provider. Finally, we identified the average number of years that an HHA provider had been certified by using the “Date Certified” variable from the Home Health Compare data set.
Analytic Approach
We compared the demographic characteristics and measures of function and acuity between Medicare beneficiaries receiving HHA services in AL and in other home settings. We also compared the characteristics of HHAs that serve beneficiaries in each of these two locations. We tested for significant differences between groups using chi-square tests and t tests for categorical and continuous variables, respectively. Because there are likely inherent differences in severity between patients receiving HHA services in AL versus in other home settings, we conducted a subgroup analysis in which we considered the subset of HHA recipients with significant cognitive impairment (i.e., requires considerable assistance in routine situations, is not alert and oriented or is unable to shift attention and recall directions more than half the time, or is totally dependent due to disturbances such as constant disorientation, coma, persistent vegetative state, or delirium). We adjusted the state rates of home health use in AL and the state rates of home health use among all beneficiaries in the state for differences in beneficiaries’ age, sex, and race. We compared the standardized percentage of home health use in AL with the standardized percentage of overall home health use, by state.
Results
There were 10,541,795 beneficiary-years with at least one home health OASIS SOC assessment identified from 2012 to 2014 (Table 1), representing 8,057,155 unique individuals. A total of 1,039,616 (9.9%) SOC assessments began in AL, representing 801,078 unique individuals. From 2012 to 2014, the share of HHA services delivered in AL, compared with other home settings, increased from 9.6% to 10.1%.
Table 1.
Distribution of Medicare Beneficiaries Receiving Home Health Agency Services in Assisted Living and Other Home Settings, Over Time (2012-2014).
| Year | Beneficiaries receiving HHA services in AL (n = 1,039,616) |
Beneficiaries receiving HHA services in other home settings (n = 9,502,179) |
Total (n = 10,541,795) |
|---|---|---|---|
| 2012 | 330,150 (9.6%) | 3,107,702 (90.4%) | 3,437,852 |
| 2013 | 346,643 (9.8%) | 3,174,990 (90.2%) | 3,521,633 |
| 2014 | 362,823 (10.1%) | 3,219,487 (89.9%) | 3,582,310 |
Source. Outcome and Assessment Information Set C and Medicare Master Beneficiary Summary File, 2012-2014.
Note. HHA = home health agency. AL = assisted living.
In 2014, HHA recipients in ALs were generally older than HHA recipients in other home settings, with 61.3% of AL residents aged 85 years or older compared with 29.4% of non-AL residents (see Table 2). HHA recipients in AL were also more likely to be female (69.9% vs. 61.4%, p < .001) and more likely to be White (91.1% vs. 77.5%, p < .001) compared with those recipients who did not reside in AL. In addition, 19.8% of beneficiaries receiving HHA services in AL and 18.6% of beneficiaries receiving HHA services in other home settings were classified as full duals (p < .001).
Table 2.
Demographic and Health Characteristics of Medicare Beneficiaries Receiving Home Health Agency Services in Assisted Living and Other Home Settings (2014).
| Beneficiaries receiving HHA services in AL (N= 362,823) |
Beneficiaries receiving HHA services in other home settings (N = 3,219,487) |
Total (N = 3,582,310) |
|
|---|---|---|---|
| Characteristics | n (%)/M (SD) | n (%)/M (SD) | n (%)/M (SD) |
| Age | |||
| 65-69 | 17,272 (4.8) | 490,492 (15.2) | 507,764 (14.2) |
| 70-74 | 23,434 (6.5) | 568,023 (17.6) | 591,457 (16.5) |
| 75-79 | 35,334 (9.7) | 597,131 (18.5) | 632,465 (17.7) |
| 80-84 | 64,275 (17.7) | 616,452 (19.1) | 680,727 (19.0) |
| 85+ | 222,508 (61.3) | 947,389 (29.4) | 1,169,897 (32.7) |
| Sex | |||
| Female | 253,607 (69.9) | 1,977,509 (61.4) | 2,231,116 (62.3) |
| Male | 109,216 (30.1) | 1,241,957 (38.6) | 1,351,173 (37.7) |
| Racea | |||
| White | 330,675 (91.1) | 2,494,733 (77.5) | 2,825,408 (78.9) |
| Black | 13,992 (3.9) | 377,523 (11.7) | 391,515 (10.9) |
| Hispanic | 11,505 (3.2) | 236,056 (7.3) | 247,561 (6.9) |
| Asian/Pacific Islander | 4,264 (1.2) | 69,526 (2.2) | 73,790 (2.1) |
| Native American | 701 (0.2) | 10,305 (0.3) | 11,006 (0.3) |
| Other/unknown | 1,171 (0.3) | 19,014 (0.6) | 20,185 (0.6) |
| Insurance | |||
| Full duals | 71,940 (19.8) | 597,818 (18.6) | 669,758 (18.7) |
| Partial duals | 5,136 (1.4) | 187,061 (5.8) | 192,197 (5.4) |
| Cognitive, behavioral, and psychiatric impairments | |||
| Memory deficit | 168,730 (46.5) | 489,210 (15.2) | 657,940 (18.4) |
| Impaired decision | 157,586 (43.4) | 612,119 (19.0) | 769,705 (21.5) |
| Verbal disruption | 14,292 (3.9) | 32,547 (1.0) | 46,839 (1.3) |
| Physical aggression | 9,195 (2.5) | 15,466 (0.5) | 24,661 (0.7) |
| Socially inappropriate | 8,089 (2.2) | 15,372 (0.5) | 23,461 (0.7) |
| Delusional | 10,578 (2.9) | 30,114 (0.9) | 40,692 (1.1) |
| None of the above | 145,730 (40.2) | 2,383,528 (74.0) | 2,529,258 (70.6) |
| ADL impairments | |||
| Grooming | 326,954 (90.1) | 2,686,997 (83.5) | 3,013,951 (84.1) |
| Dressing upper | 335,858 (92.6) | 2,828,068 (87.8) | 3,163,926 (88.3) |
| Dressing lower | 342,353 (94.4) | 2,938,436 (91.3) | 3,280,789 (91.6) |
| Bathing | 359,903 (99.2) | 3,146,136 (97.7) | 3,506,039 (97.9) |
| Toileting transfer | 302,902 (83.5) | 2,350,065 (73.0) | 2,652,967 (74.1) |
| Toileting hygiene | 317,454 (87.5) | 2,520,289 (78.3) | 2,837,743 (79.2) |
| Transferring | 344,454 (94.9) | 2,934,075 (91.1) | 3,278,529 (91.5) |
| Ambulation/locomotion | 356,690 (98.3) | 3,096,782 (96.2) | 3,453,472 (96.4) |
| Feeding | 262,324 (72.3) | 1,902,944 (59.1) | 2,165,268 (60.4) |
| Discharged during the past 14 days | |||
| Skilled nursing facility | 63,363 (17.5) | 575,757 (17.9) | 639,120 (17.8) |
| Short-stay acute hospital | 70,577 (19.5) | 1,511,689 (47.0) | 1,582,266 (44.2) |
| Other | 23,261 (6.4) | 268,312 (8.3) | 291,573 (8.1) |
| No inpatient discharge | 212,223 (58.5) | 982,199 (30.5) | 1,194,422 (33.3) |
| Provider characteristics ownership type | |||
| For-profit | 264,371 (72.9) | 1,801,776 (56.0) | 2,066,147 (57.7) |
| Nonprofit | 91,569 (25.2) | 1,317,923 (40.9) | 1,409,492 (39.4) |
| Government | 6,733 (1.9) | 99,158 (3.1) | 105,891 (3.0) |
| Rurality | |||
| Urban | 322,010 (88.8) | 2,683,003 (83.3) | 3,005,013 (83.9) |
| Rural | 33,275 (9.2) | 445,337 (13.8) | 478,612 (13.4) |
| Super rural | 7,538 (2.1) | 91,100 (2.8) | 98,638 (2.8) |
| Total number of episodes (non-LUPA) | 2,002.2 (3,434.5) | 2,779.0 (6,017.9) | 2,700.3 (5,813.3) |
| Number of dual eligible beneficiaries | 343.1 (949.0) | 575.0 (1,801.8) | 551.7 (1,736.4) |
| Average age of beneficiaries | 78.9 (3.3) | 77.1 (2.7) | 77.2 (2.9) |
| Number of years certified | 21.9 (13.6) | 26.2 (14.2) | 25.8 (14.2) |
Note. Differences between settings tested using chi-square analyses and are statistically significant at p < .001. Numbers represent person-years. HHA = home health agency; AL = assisted living; LUPA = low utilization payment adjustment.
Race was defined using the RTI algorithm.
HHA recipients living in AL were more than twice as likely to exhibit cognitive impairments, particularly memory deficit and impaired decision making, than those recipients in other home settings (46.5% and 43.4% vs. 15.2% and 19.0%, p < .001, respectively). HHA recipients living in AL were also more likely to exhibit more ADL impairments than those recipients in other home settings, particularly with feeding (72.3% vs. 59.1%, p < .001), toileting transfer (83.5% vs. 73.0%, p < .001), and toileting hygiene (87.5% vs. 78.3%, p < .001). Moreover, beneficiaries receiving HHA services in AL were significantly more likely to receive home health without a prior inpatient event in the past 14 days (than those beneficiaries receiving HHA services in other home settings (58.5% vs. 30.5%, p < .001). Only 19.5% of recipients residing in an AL setting recently experienced an acute hospital stay in the 14 days prior to receiving HHA services compared with 47.0% of recipients who did not reside in an AL (p < .001).
In terms of HHA provider characteristics, beneficiaries in AL were more likely to be served by smaller HHAs (2002.2 total episodes compared with 2779.0, p < .001), newer HHAs (21.9 years vs. 26.2 years, p < .001), for-profit HHAs (72.7% vs. 56.0%, p < .001), and agencies located in urban areas (88.8% vs. 83.3%, p < .001). In addition, HHAs that served beneficiaries in AL served fewer duals on average than agencies serving individuals in other home settings.
The subgroup of HHA patients with significant cognitive impairment exhibited much higher rates of memory deficit, impaired decision-making symptoms, and ADL impairments than the general population of HHA recipients (see Table A1 in the appendix). The rates of functional impairments in this subgroup were very similar between the beneficiaries receiving HHA in AL and those receiving HHA in other home settings. In terms of cognitive symptoms, a larger share of residents in AL receiving HHA experienced memory deficits and impaired decision making than cognitively impaired HHA recipients in other home settings (89.8% vs. 79.3% and 81.5% vs. 74.2%, respectively).
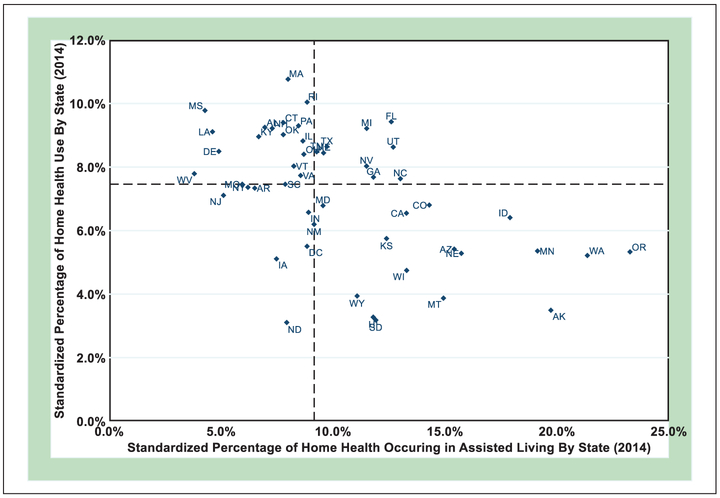
The share of HHA services delivered in AL varied widely across states (see Figure 1). HHAs are disproportionately providing services in the AL setting in Oregon, Washington, Alaska, Minnesota, and Idaho. While these states exhibited some of the highest standardized percentages of home health use (17.9% to 23.3%) occurring in AL, these states also showed lower standardized percentages of home health utilization overall (3.5% to 6.5%; Figure 1). Similarly, Massachusetts, Mississippi, Rhode Island, Florida, and Michigan were among those states that had the highest standardized percentages of home health usage (9.2% to 10.7%), but HHAs in these states are disproportionately providing fewer services in the AL setting (4.3% to 12.6%).
Figure 1.
State-level standardized percentage of home health agency services delivered in assisted living and standardized percentage of home health use among all Medicare beneficiaries in the state (2014).
Source. Outcome and Assessment Information Set C and Medicare Master Beneficiary Summary File, 2014.
Note. State rates standardized by age, sex, and race. Dashed lines indicate median values.
Discussion
This study provides new data on the delivery of HHA services in AL. In this national study of HHA use in AL, we saw a slight growth in the share of HHA services being delivered in the AL setting between 2012 and 2014. Consistent with what we know about the AL population, we found that Medicare beneficiaries receiving HHA services in AL were more likely to be female, White, and 85 years of age or older than HHA recipients in other settings. We also found that HHA recipients in AL were also more likely to have cognitive and ADL impairments than those receiving HHA in other settings. In addition, these rates of impairments are higher than what has been observed among the general population of AL residents (Caffrey & Sengupta, 2018). Finally, our study highlighted the state variability in the delivery of HHA services in AL.
Despite having more care needs, we found that HHA recipients in AL were less likely to have been recently discharged from an acute care setting compared with those receiving HHA services in other home settings. This finding potentially alludes to AL residents utilizing HHA services more so for health maintenance than for postacute care services and corroborates the assumption that HHAs may allow individuals with increasing care needs to reside in AL longer. Because health insurers, such as Medicare, cover the costs of HHA services, AL operators may be increasingly receptive to contracting with third-party providers in order to assist residents in remaining in AL despite increasing impairment. Future work is needed to understand the impact of receiving HHA in AL on extending an individual’s residence in these settings.
We also found that HHAs serving residents in AL are different from those providing services in other home settings. It may be the case that ALs have a preferred provider relationship or are contracting with particular HHAs to meet their residents’ increasing care needs. Or it may be the case that ALs are located in different areas than where HHA is delivered in other settings. While the mechanisms driving these differences would not be visible in our data, our findings do suggest that AL residents are receiving services from a different kind of HHA than those in other settings. This finding sets the stage for future work examining differences in precipitating factors, services provided, and patient outcomes associated with receipt of HHA in AL versus the community.
Our analysis suggests that there is wide geographic variation in the percentage of HHA services delivered in ALs across the country. Particularly, we find disproportionate relationships in certain states in relation to the percentage of home health services provided in the AL setting compared with the overall percentage of home health use in the state, in general. There are a number of factors that may contribute to the disproportionate use of HHA in AL in some states that we are unable to measure, including the size of the AL industry, differences in AL resident impairments, and HHA practice patterns. One factor that may be driving this variation is differences in how states regulate AL. For example, staff requirements and provisions in Massachusetts, Mississippi, Rhode Island, and Florida in 2014, all states with low standardized percentages of HHA utilization in AL, require a licensed nurse (RN, LPN) to be part of the AL staff (Carder et al., 2015). In contrast, certain states that exhibited high standardized percentages of HHA delivered in AL (e.g., Oregon, Alaska, and Idaho) do not have such specific staffing regulations (Carder et al., 2015). Washington and Minnesota also exhibited similar trends and their respective state regulations simply require a licensed nurse to be “on-call” or “available.” It is possible that differences in availability of trained staff in AL to care for residents with increasing impairment and care needs are contributing to these variations in delivery of HHA in AL. Additionally, some states require formal contracts and verification that third-party HHA-contracted providers have undergone criminal background checks prior to coming on-site to the AL, while other states do not have formal provisions in place (Carder et al., 2015). States that do not have such formal requirements demonstrated some of the higher standardized percentages of HHA utilization in AL (e.g., Oregon, Washington, and Alaska; Carder et al., 2015). Further study is required to better understand the range and combination of factors that may be contributing to the state-level variation in HHA utilization in AL (e.g., supply of HHAs, supply of AL beds, AL resident impairments, HHA practice patterns, and regulations).
This study has a number of limitations to note. First, the OASIS instrument provides a generic measure of health conditions and impairments for those who utilize HHA services. More specific clinical information could provide a more detailed understanding of the differences between HHA patients who do and do not reside in AL. Second, there are no national data systematically collected on all AL residents. Therefore, it remains unclear how recipients of HHA services compare with the overall population of AL residents. Given this limitation, our results should be interpreted as the share of HHA users residing in AL, and not the share of AL residents who use HHA services. Third, in an effort to create measures that were similar across symptoms and impairments, we dichotomized recipients’ cognitive symptoms and ADL impairments and may, therefore, have missed important details regarding their magnitude. This may contribute to the higher rates of functional impairment among HHA recipients that we observed compared with past work (Scharpf & Madigan, 2010). Finally, a potential limitation relates to the Place of Residence code that we used to identify HHA users in AL. AL is an example of a congregate situation; however, residents in group homes, adult family care homes, or other congregate living situations may also be included in our sample. There is a need for future work to confirm our findings, potentially through incorporating a new methodology to identify AL residents (Thomas et al., 2018).
In conclusion, HHA utilization in AL and variation by state have thus far received sparse attention despite the increasing complexity of Medicare beneficiaries who reside in AL. This is among the first studies to examine the delivery of HHA in AL and sets the stage for future research examining a number of questions related to the delivery of HHA services in AL that, among many, include the following: What factors contribute to receipt of HHA in AL? What is the quality of care that residents in AL receiving services from HHA experience? What are the potential cost savings of providing HHA services in AL compared with nursing home care? And, how do state regulations increase/decrease access to HHA in AL? With the large and growing number of Medicare beneficiaries receiving home health in AL, the answers to these questions become even more important.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by National Institute on Aging (Grant ID: R21AG047303, T-32 HS-00011).
Appendix
In the subgroup analysis, we used Question M1700 from OASIS to determine significant cognitive impairment. A Medicare beneficiary was defined as having a significant cognitive impairment if the beneficiary scored a (3)—requires considerable assistance in routine situations, is not alert and oriented, or is unable to shift attention and recall directions more than half the time—or a (4)—totally dependent due to disturbances such as constant disorientation, coma, persistent vegetative state, or delirium. Our new subgroup analysis of Medicare beneficiaries with significant cognitive impairment exhibited much higher rates of memory deficit, impaired decision-making symptoms, and ADL impairments. However, the rates of functional impairments were very similar between the group receiving HHA in AL and those receiving HHA in other home settings. In terms of cognitive symptom measures, a larger share of residents in AL receiving HHA experienced memory deficits and impaired decision making than cognitively impaired HHA recipients in other home settings (89.8% vs. 79.3% and 81.5% vs. 74.2%, respectively).
Table A1. Demographic and Health Characteristics of Medicare Beneficiaries With Significant Cognitive Impairment Receiving Certified Home Health Agency Services in Assisted Living and Other Home Settings (2014).
| Beneficiaries receiving CHHA services in AL (N = 49,300) |
Beneficiaries receiving CHHA services in other home settings (N = 108,216) |
Total (N = 157,516) |
|
|---|---|---|---|
| Characteristics | n (%)/M (SD) | n (%)/M (SD) | n (%)/M (SD) |
| Age | |||
| 65-69 | 1,596 (3.2) | 5,860 (5.4) | 7,456 (4.7) |
| 70-74 | 2,698 (5.5) | 9,595 (8.9) | 12,293 (7.8) |
| 75-79 | 4,962 (10.1) | 15,487 (14.3) | 20,449 (13.0) |
| 80-84 | 9,329 (18.9) | 22,948 (21.2) | 32,277 (20.5) |
| 85+ | 30,715 (62.3) | 54,326 (50.2) | 85,041 (54.0) |
| Sex | |||
| Female | 34,978 (70.9) | 69,246 (64.0) | 104,224 (66.2) |
| Male | 14,322 (29.1) | 38,970 (36.0) | 53,292 (33.8) |
| Racea | |||
| White | 45,296 (91.9) | 77,414 (71.5) | 122,710 (77.9) |
| Black | 1,783 (3.6) | 17,197 (15.9) | 18,980 (12.0) |
| Hispanic | 1,293 (2.6) | 8,956 (8.3) | 10,249 (6.5) |
| Asian/Pacific Islander | 600 (1.2) | 3,343 (3.1) | 3,943 (2.5) |
| Native American | 95 (0.2) | 349 (0.3) | 444 (0.3) |
| Other/unknown | 164 (0.3) | 710 (0.7) | 874 (0.6) |
| Cognitive, behavioral, and psychiatric impairments | |||
| Memory deficit | 44,278 (89.8) | 85,857 (79.3) | 130,135 (82.6) |
| Impaired decision | 40,157 (81.5) | 80,255 (74.2) | 120,412 (76.4) |
| Verbal disruption | 6,622 (13.4) | 10,222 (9.4) | 16,844 (10.7) |
| Physical aggression | 5,488 (11.1) | 7,566 (7.0) | 13,054 (8.3) |
| Socially inappropriate | 4,154 (8.4) | 6,209 (5.7) | 10,363 (6.6) |
| Delusional | 4,197 (8.5) | 8,433 (7.8) | 12,630 (8.0) |
| None of the above | 1,259 (2.6) | 8,505 (7.9) | 9,764 (6.2) |
| ADL impairments | |||
| Grooming | 48,858 (99.1) | 106,625 (98.5) | 155,483 (98.7) |
| Dressing upper | 49,009 (99.4) | 106,991 (98.9) | 156,000 (99.0) |
| Dressing lower | 49,075 (99.5) | 107,234 (99.1) | 156,309 (99.2) |
| Bathing | 49,266 (99.9) | 108,000 (99.8) | 157,266 (99.8) |
| Toileting transfer | 48,485 (98.3) | 105,565 (97.6) | 154,050 (97.8) |
| Toileting hygiene | 47,969 (97.3) | 104,437 (96.5) | 152,406 (96.8) |
| Transferring | 48,020 (97.4) | 105,642 (97.6) | 153,662 (97.6) |
| Ambulation/locomotion | 48,654 (98.7) | 106,979 (98.9) | 155,633 (98.8) |
| Feeding | 45,780 (92.9) | 100,692 (93.0) | 146,472 (93.0) |
| Discharged during the past 14 days | |||
| Skilled nursing facility | 6,240 (12.7) | 19,151 (17.7) | 25,391 (16.1) |
| Short-stay acute hospital | 9,141 (18.5) | 36,726 (33.9) | 45,867 (29.1) |
| Other | 2,399 (4.9) | 7,746 (7.2) | 10,145 (6.4) |
| No inpatient discharge | 32,177 (65.3) | 47,411 (43.8) | 79,588 (50.5) |
| Insurance | |||
| Full duals | 8,701 (17.7) | 28,187 (26.1) | 36,888 (23.4) |
| Partial duals | 335 (0.7) | 4,170 (3.9) | 4,505 (2.9) |
| Provider characteristics ownership type | |||
| For-profit | 34,572 (70.1) | 59,297 (54.8) | 93,869 (59.6) |
| Nonprofit | 13,508 (27.4) | 45,554 (42.1) | 59,062 (37.5) |
| Government | 1,201 (2.4) | 3,344 (3.1) | 4,545 (2.9) |
| Rurality | |||
| Urban | 43,908 (89.1) | 90,464 (83.6) | 134,372 (85.3) |
| Rural | 4,366 (8.9) | 14,572 (13.5) | 18,938 (12.0) |
| Super rural | 1,026 (2.1) | 3,179 (2.9) | 4,205 (2.7) |
| Total number of episodes | 2,088.6 (3,443.3) | 3,036.0 (6,745.7) | 2,739.3 (5,929.7) |
| Number of dual eligible beneficiaries | 350.4 (952.6) | 652.9 (2,043.9) | 558.5 (1,782.3) |
| Average age of beneficiaries | 79.1 (3.2) | 77.4 (2.7) | 77.9 (3.0) |
| Number of years certified | 23.1 (13.7) | 27.1 (14.4) | 25.9 (14.3) |
Source. Outcome and Assessment Information Set C and Medicare Master Beneficiary Summary File, 2010-2014.
Note. Differences between settings tested using chi-square analyses and are statistically significant at p < .001. Numbers represent person-years. CHHA = certified home health agency; AL = assisted living.
RTI algorithm.
Footnotes
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Nazareno is a co-owner of an assisted living facility in California.
References
- Brodie M, & Blendon R (2001). National Survey on Nursing Homes. Menlo Park, CA: Kaiser Family Foundation. [Google Scholar]
- Caffrey C, & Sengupta M (2018). Variation in residential care community resident characteristics, by size of community: United States, 2016 (NCHS Data Brief No. 299). Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Caffrey C, Sengupta M, Park-Lee E, Moss A, Rosenoff E, & Harris-Kojetin L (2012). Residents living in residential care facilities: United States, 2010 (NCHS Data Brief No. 91). Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Carder P, O’Keefe J, & O’Keefe C (2015). Compendium of residential care and assisted living regulations and policy. Washington, DC: RTI International. [Google Scholar]
- Centers for Medicare and Medicaid Services. (2009). OASIS C Assessment Instrument. Retrieved from https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/homehealthqualityinits/downloads/hhqioasiscalltimepoint.pdf
- Centers for Medicare and Medicaid Services. (2017). CMS finalizes new Medicare and Medicaid home health care rules and beneficiary protections. Retrieved from https://www.cms.gov/newsroom/press-releases/cms-finalizes-new-medicare-and-medicaid-home-health-care-rules-and-beneficiary-protections
- Chapin R, & Dobbs-Kepper D (2001). Aging in place in assisted living: Philosophy versus policy. The Gerontologist, 41, 43–50. [DOI] [PubMed] [Google Scholar]
- Genworth Financial. (2018). Compare long-term care costs across the United States. Retrieved from https://www.genworth.com/aging-and-you/finances/cost-of-care.html
- Grabowski DC, Stevenson DG, & Cornell PY (2012). Assisted living expansion and the market for nursing home care. Health Services Research, 47, 2296–2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris-Kojetin L, Sengupta M, Park-Lee E, Valverde R, Caffrey C, Rome V, & Lendon J (2016). Long-term care providers and service users in the United States: Data from the National Study of Long-Term Care Providers, 2013-2014. Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Hawes C, Rose M, & Phillips CD (1999). A national assisted living for the frail elderly: Results of a national survey of facilities. Beachwood, OH: Meyers Research Institute. [Google Scholar]
- Hawes C, Phillips CD, Rose M, Holan S, & Sherman M (2003). A national survey of assisted living facilities. The Gerontologist, 43, 875–882. [DOI] [PubMed] [Google Scholar]
- Khatutsky G, Ormond C, Wiener JM, Greene AM, Johnson R, Jessup EA, & Harris-Kojetin L (2016). Residential care communities and their residents in 2010: A national portrait (DHHS Publication No. 2016-1041). Hyattsville, MD: National Center for Health Statistics. [Google Scholar]
- Kisling-Rundgren A, Paul DP III, & Coustasse A (2016). Costs, staffing, and services of assisted living in the United states: A literature review. The Health Care Manager, 35(2), 156–163. [DOI] [PubMed] [Google Scholar]
- Konetzka T, Spector W, & Limcangco M (2007). Reducing hospitalizations from long-term care settings. Medical Care Research and Review, 65(1), 40–66. [DOI] [PubMed] [Google Scholar]
- Metlife Mature Market Institute (2012). Market survey of long-term care costs: The 2012 metlife market survey of nursing home, Assisted Living, Adult Day Services, and Home Care Costs. Retrieved from https://www.theltcstore.com/uploads/mmi-2012-market-survey-long-term-care-costs.pdf
- Naylor MD, Hirschman KB, Hanlon AL, Bowles KH, Bradway C, McCauley KM, & Pauly MV (2016). Effects of alternative interventions among hospitalized, cognitively impaired older adults. Journal of Comparative Effectiveness Research, 5, 259–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomer RJ, Ko M, Kang T, Harrington C, Hulett D, & Bindman A (2016). Health care expenditures after initiating long-term services and supports in the community versus in a nursing facility. Medical Care, 54, 221–228. [DOI] [PubMed] [Google Scholar]
- Outcome and Assessment Information Set C and Medicare Master Beneficiary Summary File (2012-2014). Retrieved from https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/OASIS/index.html
- Outcome and Assessment Information Set C and Medicare Master Beneficiary Summary File (2010-2014). Retrieved from https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/OASIS/index.html
- Outcome and Assessment Information Set C and Medicare Master Beneficiary Summary File (2014). [Google Scholar]
- Perry T, Andersen T, & Kaplan D (2014). Relocation remembered: Perspectives on senior transitions in the living environment. The Gerontologist, 54, 75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scharpf T, & Madigan E (2010). Functional status outcome measures in home health care patients with heart failure. Home Health Care Services Quarterly, 29, 155–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas KS, Dosa D, Gozalo PL, Grabowski DC, Nazareno J, Makineni R, Mor V (2018). A methodology to identify a cohort of medicare beneficiaries residing in large assisted living facilities using administrative data. Medical Care, 56(2), e10–e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Bureau of Labor Statistics. (2015). Monthly labor review: Industry employment and output projections to 2024. Retrieved from https://www.bls.gov/opub/mlr/2015/article/industry-employment-and-output-projections-to-2024.htm
- Wysocki A, Butler M, Kane RL, Kane RA, Shippee T, & Sainfort F (2015). Long-term services and supports for older adults: A review of home and community-based services versus institutional care. Journal of Aging & Social Policy, 27, 255–279. [DOI] [PubMed] [Google Scholar]
- Zimmerman S, Gruber-Baldini AL, Sloane PD, Eckert JK, Hebel JR, Morgan LA, & Konrad TR (2003). Assisted living and nursing homes: Apples and oranges? The Gerontologist, 43, 107–117. [DOI] [PubMed] [Google Scholar]