Abstract
Purpose
Studies on the incidence and mortality of refractures after primary osteoporotic fracture are limited by the relatively rare incidence of such refractures and small sample sizes. The objectives of this research were: 1) to determine the incidence of osteoporotic refractures and fracture locations and 2) to assess mortality rates associated with osteoporotic refracture over a median follow up of 3 years using nationwide claim database.
Materials and Methods
Patients over 50 years of age who had an osteoporotic fracture that was confirmed operationally were enrolled. Refracture was defined as that after 6 months of an untreated period. Mortality rate was calculated using the Charlson comorbidity index and was analyzed using Cox proportional hazards regression analysis.
Results
A total of 18956 first-time instances of osteoporotic fracture were reported between 2007 and 2012 after a median follow up of 3.1 years (range, 1 to 7 years). Among 18956 patients, 2941 (15.50%) experienced refracture. After follow up for 1 year, cumulative mortality rates for re-fracture and non-refracture groups were 9.1% and 7.2%, respectively. After adjusting for covriates, mortality rate was 1.2 times greater in patients with re-fracture than in patients without re-fracture over a median follow up of 3 years (hazard ratio: 1.20, 95% confidence interval: 1.08–1.34, p<0.001).
Conclusion
The incidence of osteoporotic re-fracture in this nationwide study was 15.5%, and the mortality rate of re-fracture patients was 1.2 times higher than that of non-refracture patients over a median follow up of 3 years.
Keywords: Incidence, mortality, nationwide claim data, osteoporotic fracture, refracture
INTRODUCTION
The population worldwide is aging. With increased life expectancy for older adults, the incidence of osteoporotic fractures has also increased.1,2,3,4,5 To prevent osteoporotic fractures, every nation around the globe is dedicated to treating osteoporosis,6,7,8,9,10,11 and initiatives are growing to minimize the incidence of osteoporotic fractures.12 These fractures in older adults can lead to elevated mortality and morbidity that can decrease the quality of life,6,7,8 and osteoporotic fracture patients are also at danger of secondary osteoporotic fractures.13
According to several studies, the first osteoporotic fracture increases the risk of later fractures.14,15,16 A meta-analysis revealed that a history of fracture considerably increases the danger of any fracture, compared to the lack of a previous fracture (RR: 1.86; 95% CI: 1.75–1.98).17 Furthermore, a second hip fracture increases the risk of mortality, extra comorbidities, and reduced independence.18 Cheung, et al.19 reported the most updated incidence rate and projected population size of hip fractures for nine members of the Asian Federation of Osteoporosis Societies. They predicted that the number of hip fractures would increase from 1124060 in 2018 to 2563488 in 2050, an increase of 2.28-fold. This increase is mainly due to changes in demographics of the population, particularly in China and India, which have the largest population sizes. The direct costs of hip fracture is expected to rise from USD 9.5 billion in 2018 to USD 15 billion in 2050 (a 1.59-fold increase). To keep the total number of hip fractures constant over time, a 2–3% decrease in the incidence rate of hip fracture is required annually. They concluded that, despite the availability of better diagnosis, treatment, and prevention for fracture over recent years, hip fracture remains a key public health issue in Asia and that healthcare policy should aim to reducethe burden of hip fracture in Asia.19 However, studies on the incidence and mortality of refractures following an initial osteoporotic fracture are restricted owing to their comparatively rare incidences and the need for a large sample size.
Therefore, the objectives of this research were: 1) to determine the incidence of osteoporotic refractures and fracture locations and 2) to assess related mortality rates over a median follow up of 3 years using a nationwide claims database.
MATERIALS AND METHODS
Data source
This research used information from the 2002 to 2013 claims database of the Korean National Health Insurance (KNHI). The KNHI gathers cohort information representing the population of the country. The sample cohort covers 1025340 subjects (2.2% of the total population of 47851928) through random stratification according to sex, age, and income level. The database provides reimbursement data for each medical service, including fundamental demographics of the patients, clinic or hospital identifiers, disease code, expenses incurred, health screening outcomes, individual and family health history, health behaviors, and death-related data.20 This study was approved by the Institutional Review Board (IRB) of Chung-Ang University Hospital [IRB No. C2014086(1282)]. The requirement for informed consent was waived as this study was based on review of data that were regularly gathered.
Subjects
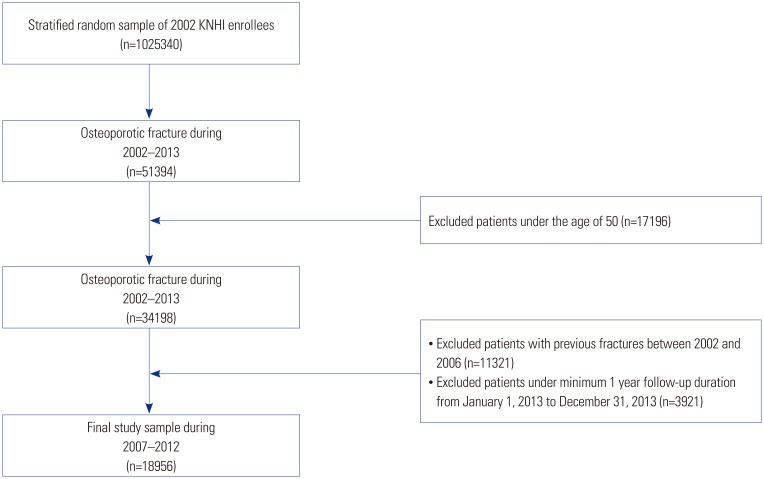
Selection criteria were: 1) those aged 50 years or older who were diagnosed with osteoporotic fractures, including the hip, spine, humerus, and distal radius, in the national database from 2007 to 2012; 2) those who were followed up until 2013 with original fractures reported from 2007 to 2012; and 3) those who were followed up for at least 1 year (Fig. 1). Patients with a history of fracture from 2002 to 2006 were excluded from this research. With the exception of cosmetic surgery and traffic accident-related injuries, the KNHI program includes 100% of the population. All clinics and hospitals send patient information including diagnosis [as described in the International Classification of Diseases, 10th Revision (ICD-10)] and NHIS claims medical expenses. The NHIS database allows for research of non-traumatic osteoporotic fractures as it does not include high-energy injuries, such as traffic accidents or industrial accidents. All information related to patients and diseases can be found from NHIS data. This information has been used in several epidemiological studies in Korea based on diagnostic codes including ICD-10 code and operational definitions for hip, spine, distal radius, and humerus fractures.21,22,23,24
Fig. 1. Flow chart showing selection of the study subjects. KNHI, Korean National Health Insurance.
Definition of osteoporotic fracture
KNHI data of outpatient visits or hospital admissions of patients aged 50 years and older from January 1, 2002 to December 31, 2012 were analyzed. Fractures related to osteoporosis were recognized for seven processes (open reduction of fractured extremity-femur, closed pinning-femur, closed pelvis/femur fixation, closed reduction of fractured extremity-pelvis/femur, bone traction, skin traction, and hemiarthroplasty-hip) and the ICD-10 codes S72.0 (femoral neck fracture), S72.1 (pertrochanteric fracture), S22.0 (traumatic spine fracture), S22.1 (traumatic spine fracture), S32.0 (traumatic spine fracture), M48.4 (traumatic vertebra fracture), M48.5 (traumatic vertebra fracture), S52.5 (traumatic distal fracture), S52.6 (traumatic distal radius/ulna fracture), S42.2 (proximal humerus fracture), and S42.3 (humerus shaft fracture), as well as fractures in general.4,21,25
Definition of refracture and survival duration
Refracture was classified as a fracture of bone in one of four initial components (hip, humerus, spine, and wrist) that occurred after 6 months (180 days) based on the last claim date.26 The re-fracture was defined after a 6-month untreated period using the same operational definition as described previously.27,28 Survival duration was defined as the length from the first fracture date to the date of death between 2007 and 2012.
Mortality after osteoporotic fractures in patients
NHIS data were combined with National Statistical Office domestic mortality data to determine survival for each patient during the follow-up period after osteoporotic fracture. From the index date of the first refracture event, the mortality rate of patients with refracture was calculated.
Adjustment of comorbidity index and disability
Medical comorbidity was based on the modified Charlson's Comorbidity Index, which was calculated as the amount of points given for disease circumstances conditions as follows: one point for myocardial infarction, deep vein thrombosis, congestive heart failure, peripheral vascular disease, dementia, arthritis, chronic obstructive pulmonary disease, diabetes mellitus, or ulcer; two points for stroke or cancer; and three points for liver cirrhosis. Thus, possible total scores ranged from 0 to 15, with higher scores indicating poorer health status.29
In terms of disability, its class (physical disability or all-cause disability) and severity (grade 1: ordinary, grade 1–2: serious, grade 3–6: mild) were obtained from the NHIS database. Disability was assessed by the accountable physician according to particular guidelines developed by the Korean government.
Statistical analyses
To evaluate the relationship between recurrence of osteoporotic fracture and death, the time from incidence to death was calculated, and recurrence from incidence of the final episode to death was calculated. A life table was used to calculate the cumulative incidence of refracture. Cumulative incidence was described as the likelihood of a specific case occurring, such as the occurrence of a specific disease. It was calculated as the amount of topics at the start of the research, separating the amount of new refractures over a period of time. The risk of mortality was calculated using Cox proportional hazards regression. A life table was also used to calculate the rate of survival. All data analyses were performed using SAS statistical package version 9.4 (SAS Institute, Cary, NC, USA).
RESULTS
A total of 18956 first-time instances of osteoporotic fracture were reported between 2007 and 2012, with a median follow-up of 3.1 years (range, 1 to 7 years). Demographic features of each fracture site and the refracture states of patients are summarized in Table 1.
Table 1. Demographic Characteristics in Terms of Osteoporotic Fracture Pattern.
| Variables | Total | Recurrence | p value | First fracture location | p value | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-refracture | Re-fracture | Spine | Humerus | Wrist | Hip | ||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | ||||
| Total | 18956 | 16015 | 84.50 | 2941 | 15.50 | 8600 | 45.40 | 829 | 4.40 | 6243 | 32.90 | 3284 | 17.30 | ||
| Sex | <0.001 | 0.046 | |||||||||||||
| Male | 4641 | 4105 | 88.45 | 536 | 11.55 | 2262 | 48.74 | 222 | 4.78 | 1044 | 22.50 | 1113 | 23.98 | ||
| Female | 14315 | 11910 | 83.20 | 2405 | 16.80 | 6338 | 44.28 | 607 | 4.24 | 5199 | 36.32 | 2171 | 15.16 | ||
| Age (yr) | <0.001 | <0.001 | |||||||||||||
| 50–54 | 1770 | 1617 | 91.36 | 153 | 8.64 | 534 | 30.17 | 111 | 6.27 | 946 | 53.45 | 179 | 10.11 | ||
| 55–59 | 2109 | 1932 | 91.61 | 177 | 8.39 | 634 | 30.06 | 110 | 5.22 | 1176 | 55.76 | 189 | 8.96 | ||
| 60–64 | 2192 | 1935 | 88.28 | 257 | 11.72 | 819 | 37.36 | 107 | 4.88 | 1040 | 47.45 | 226 | 10.31 | ||
| 65–69 | 2914 | 2436 | 83.60 | 478 | 16.40 | 1362 | 46.75 | 133 | 4.56 | 1052 | 36.10 | 367 | 12.59 | ||
| 70–74 | 3336 | 2678 | 80.28 | 658 | 19.72 | 1754 | 52.58 | 132 | 3.96 | 916 | 27.46 | 534 | 16.00 | ||
| 75–79 | 2976 | 2417 | 81.22 | 559 | 18.78 | 1670 | 56.12 | 115 | 3.86 | 572 | 19.22 | 619 | 20.80 | ||
| 80–84 | 2025 | 1619 | 79.95 | 406 | 20.05 | 1064 | 52.54 | 67 | 3.31 | 328 | 16.20 | 566 | 27.95 | ||
| ≥85 | 1634 | 1381 | 84.52 | 253 | 15.48 | 763 | 46.70 | 54 | 3.30 | 213 | 13.04 | 604 | 36.96 | ||
| Income quintile | 0.322 | <0.001 | |||||||||||||
| 0 | 1073 | 920 | 85.74 | 153 | 14.26 | 548 | 51.07 | 55 | 5.13 | 212 | 19.76 | 258 | 24.04 | ||
| 1 | 2867 | 2433 | 84.86 | 434 | 15.14 | 1281 | 44.68 | 117 | 4.08 | 991 | 34.57 | 478 | 16.67 | ||
| 2 | 2291 | 1932 | 84.33 | 359 | 15.67 | 1020 | 44.52 | 106 | 4.63 | 792 | 34.57 | 373 | 16.28 | ||
| 3 | 2917 | 2463 | 84.44 | 454 | 15.56 | 1310 | 44.91 | 120 | 4.11 | 1034 | 35.45 | 453 | 15.53 | ||
| 4 | 3687 | 3142 | 85.22 | 545 | 14.78 | 1612 | 43.72 | 168 | 4.56 | 1296 | 35.15 | 611 | 16.57 | ||
| 5 | 6121 | 5125 | 83.73 | 996 | 16.27 | 2829 | 46.22 | 263 | 4.30 | 1918 | 31.33 | 1111 | 18.15 | ||
| Disability severity classification | 0.037 | <0.001 | |||||||||||||
| Normal | 15628 | 13239 | 84.71 | 2389 | 15.29 | 7014 | 44.88 | 686 | 4.39 | 5568 | 35.63 | 2360 | 15.10 | ||
| Mild | 2604 | 2157 | 82.83 | 447 | 17.17 | 1262 | 48.46 | 81 | 3.11 | 582 | 22.35 | 679 | 26.08 | ||
| Severe | 724 | 619 | 85.50 | 105 | 14.50 | 324 | 44.75 | 62 | 8.56 | 93 | 12.85 | 245 | 33.84 | ||
| Charlson comorbidity score | <0.001 | <0.001 | |||||||||||||
| 0 | 8303 | 7212 | 86.86 | 1091 | 13.14 | 3523 | 42.43 | 360 | 4.34 | 3309 | 39.85 | 1111 | 13.38 | ||
| 1 | 6151 | 5049 | 82.08 | 1102 | 17.92 | 2915 | 47.39 | 256 | 4.16 | 1815 | 29.51 | 1165 | 18.94 | ||
| 2 | 2474 | 2058 | 83.19 | 416 | 16.81 | 1150 | 46.48 | 116 | 4.69 | 693 | 28.01 | 515 | 20.82 | ||
| ≥3 | 2028 | 1696 | 83.63 | 332 | 16.37 | 1012 | 49.90 | 97 | 4.78 | 426 | 21.01 | 493 | 24.31 | ||
There were 4641 (24.50%) male patients and 14315 (75.50%) female patients. A total of 724 (3.80%) patients showed serious impairment related with the severity of the disease, and 2999 (15.80%) patients died during the follow-up period. Of 18956 patients, 2941 (15.50%) had at least one refracture. There were statistically significant differences in sex, age, and mortality between the refracture group and the non-refracture group (Table 1, Fig. 1). Osteoporotic fracture in the spine had the highest number of cases (n=8600, 45.40%), followed by wrist fracture (n=6243, 32.90%), fracture in the humerus (n=829, 4.40%), and hip fracture (n=3284, 17.30%). Of 2941 patients with refractures, 1116 (37.95%), 815 (27.71%), 677 (23.02%), and 333 (11.32%) events were associated with the spine, hip, wrist, and humerus, respectively. The incidences of re-fracture according to the first fracture site were 12.83% (1103/8600) in spine and 22.50% (739/3284) in hip. The incidence of wrist refracture in a previous wrist fracture was 6.63% (414/6243), and the frequency of humeral re-fracture involving a previous humeral fracture was 35.83% (297/829) (Table 2).
Table 2. Refracture Rate according to First Osteoporotic Fracture Site.
| Number of subject | Location of re-fracture | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Spine | Humerus | Wrist | Hip | |||||||
| n | % | n | % | n | % | n | % | n | % | ||
| Total | 18956 | 2941 | 15.50 | 1424 | 7.51 | 297 | 1.57 | 467 | 2.46 | 753 | 3.97 |
| Location of first fracture | |||||||||||
| Spine | 8600 | 1116 | 12.98 | 1103 | 12.83 | 0 | 0.00 | 5 | 0.06 | 8 | 0.09 |
| Humerus | 829 | 333 | 40.17 | 4 | 0.48 | 297 | 35.83 | 30 | 3.62 | 2 | 0.24 |
| Wrist | 6243 | 677 | 10.84 | 259 | 4.15 | 0 | 0.00 | 414 | 6.63 | 4 | 0.06 |
| Hip | 3284 | 815 | 24.82 | 58 | 1.77 | 0 | 0.00 | 18 | 0.55 | 739 | 22.50 |
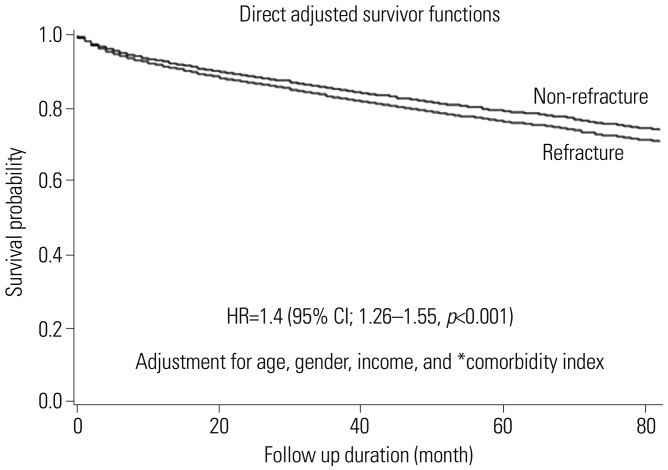
Mortality in the re-fracture group (63.5/1000 person-years) was higher than that in the non-refracture group (44.5/1000 person-years) during the study period (Table 3). After adjusting for age, sex, income, and comorbidity index, the mortality rate in patients with re-fracture was 1.4 times [hazard ratio (HR): 1.4, 95% confidence interval (CI): 1.26–1.55, p<0.001] higher than that in patients without re-fracture over a median follow-up of 3 years (Fig. 2).
Table 3. Mortality Rates during Follow Up (2007 to 2012).
| Year | Non-refracture* | Refracture* |
|---|---|---|
| 2007 | 44.0 | 74.1 |
| 2008 | 46.6 | 65.8 |
| 2009 | 41.7 | 52.6 |
| 2010 | 42.7 | 69.9 |
| 2011 | 45.9 | 60.9 |
| 2012 | 47.0 | 66.3 |
| Average | 44.5 | 63.5 |
*1000 person-years.
Fig. 2. Survival probability according to the incidence of refracture. *Medical comorbidities were based on the modified Charlson's Comorbidity Index.24 HR, hazard ratio; CI, confidence interval.
According to the site of first fracture, mortality risk was decreased in the order of hip (HR: 1.68, p<0.001), humerus (HR: 1.41, p<0.001), spine (reference), and wrist (HR: 0.52, p<0.001). In addition, the mortality risks according to the site of first refracture (reference=non-refracture) were decreased in the order of hip (HR=1.52, p<0.001), spine (HR=1.09, p=0.329), humerus (HR=0.93, p=0.722), and wrist (HR=0.69, p=0.072) (Table 4).
Table 4. Mortality Risk for Each Refracture Site in Refracture Patients, Compared to Non-Refracture Patients.
| Fracture location | Original fracture | Refracture (reference: non-refracture) | ||||
|---|---|---|---|---|---|---|
| Hazard ratios | 95% CI | p value | Hazard ratios | 95% CI | p value | |
| Spine | Reference | 1.09 | 0.92–1.28 | 0.329 | ||
| Humerus | 1.41 | 1.18–1.69 | <0.001 | 0.93 | 0.61–1.41 | 0.722 |
| Wrist | 0.52 | 0.46–0.58 | <0.001 | 0.69 | 0.45–1.03 | 0.072 |
| Hip | 1.68 | 1.55–1.82 | <0.001 | 1.52 | 1.31–1.76 | <0.001 |
CI, confidence interval.
Adjusted for age, sex, income, and Charlson Comorbidity Index.
Adults >85 years of age showed greater danger of re-fracture than those aged between 50 and 54 years (HR: 1.43, 95% CI: 1.17–1.76, p<0.001). The risk of re-fracture was higher in female (HR: 1.37, 95% CI: 1.30–1.44, p<0.001) than in male.
DISCUSSION
Although attempts have been made to prevent secondary fractures in patients with osteoporotic fracture over the past several centuries, information about the incidence, morbidity, mortality, and financial burden associated with secondary fractures is still limited for patients with osteoporotic fractures. Thus, this study determined the incidence and mortality of osteoporotic refractures based on information from domestic claims for health insurance. During the study period with a median follow-up of 3 years (range, 1 to 7 years), the incidence of refractures among complete osteoporotic fractures was 15.5% (2941/18956 patients). Incidences rates of refractures in the spine, hip, wrist, and humerus were 37.95%, 27.71%, 23.02%, and 11.32%, respectively. Cumulative mortality rates for nonrefracture and re-fracture groups at 1 year of follow up were 7.2% and 9.1%, respectively. During the study period, cumulative mortality was higher in the re-fracture group than that in the non-refracture group. After adjusting for age, sex, income, and comorbidity, the mortality rate was 1.2 times greater in patients with re-fracture than that in patients without re-fracture (Model 2, HR: 1.20, 95% CI: 1.08–1.34, p<0.001). Risk ratios for hip, humerus, and wrist refractures were 1.68, 1.41, and 0.52, respectively. Adults >85 years of age had a greater risk of refracture than those aged between 50 and 54 years (HR: 1.43, 95% CI: 1.17–1.76, p<0.001), and the risk of refracture was greater in females (HR: 1.37, 95% CI: 1.30–1.44, p<0.001) than in males.
Hsiao, et al.30 determined the incidence of osteoporotic fracture in patients over 65 years of age using the National Health Insurance Database. They indicated that within the first year of original fracture, 45% experienced complete refractures. Although the overall incidence of secondary fracture depended on follow-up periods, 50% of cases showed refractures within 3 years after the primary fracture.27,31,32 In the present study, the incidence of re-fracture during follow up corresponded with the results of other studies. The incidence of refracture improved significantly up to 2 years in this research, and it decreased gradually to a plateau. Of all refractures, 21% and 55% occurred at 1 and 2 years, respectively. Considering such trends in patients with primary osteoporotic fractures, early prevention appears mandatory to minimize the incidence of refracture.
Nakayama, et al.33 performed a historical cohort study of all patients aged at least 50 years who had a 6-month history of minimal trauma fracture and presented to the emergency departments of a tertiary hospital with and without a fracture liaison service. They reported a 30% reduction in the rate of refracture at the fracture liaison service hospital and a 40% reduction in major refractures (hip, spine, femur, pelvis, or humerus).
Klotzbuecher, et al.34 performed a meta-analysis and revealed that past history of wrist fracture not only increases the risk of subsequent wrist fracture [odds ratio (OR): 3.3], but also increases the risk of hip fracture (OR: 1.9). Similarly, past history of hip fracture increased the risk of subsequent hip fracture (OR: 2.3) in peri- or post-menopausal females. A common fracture, irrespective of its location, reduced the danger of subsequent fracture, including pooled vertebral and non-vertebral fractures (OR: 2).34
van Staa, et al.35 used British cohort information to evaluate the incidence of subsequent fractures. They found that a previous tibia, fibula, ankle, femur, hip, radius, ulna, rib, or humerus fracture increased the risk of subsequent fracture, with corresponding ORs ranging from 2 to 3. Specifically, patients with a history of radius or ulna fracture had the highest risk of humerus fracture (OR: 5.8, 95% CI: 5.5–6.1).35
Overall, patients with osteoporotic fracture reported greater hip, spine, proximal humerus, and distal radius mortality. These results often matched secondary fractures in main fractures. Bliuc, et al.36 performed a long-term follow-up cohort study to investigate the mortality of osteoporotic fractures in patients above 60 years of age. They reported 2.99-fold and 1.91-fold increases in mortality in male and female patients with refractures, respectively. Refracture within 5 years of an initial fracture significantly increased the mortality. Furthermore, mortality was moderately increased within 10 years. In the present study, the mortality rate in patients with refracture was 1.2 times higher than that in the non-refracture group (HR: 1.20, 95% CI: 1.08–1.34, p<0.001) after adjusting for age, sex, income, and comorbidity index. During a follow-up duration of 4 years, risks of mortality rate (HR: 1.27 at 1 year, 1.25 at 2 years, 1.29 at 3 years, 1.10 at 4 years, and 0.99 at 5 years) were higher in the re-fracture group than those in the non-refracture group.
Hsiao, et al.30 found that important risk factors are hip (HR=1.45), spine (HR=1.59), female sex (HR=1.41), and age over 85 years (HR=1.26). Our findings also showed that advanced age and female sex were risk factors for refracture. However, the frequency of refracture in this study was the highest at the humerus and hip joints depending on the primary fracture site. The incidence of humerus-related refracture was 3.7 times greater than in the hip and 2 times greater than in the spine.
This study has several limitations. First, bone mineral density data or laboratory data, such as vitamin D, calcium, body mass index, smoking/alcohol status, or caffeine use, were not considered because this study was based on the National Claims Registry database. Second, although the operative definition of this study excluded pathologic fractures, it was impossible to clinically diagnose any disease associated fractures. Therefore, fracture incidence might have been overestimated. Third, mortality due to a specific medical condition or non-medical usage was not analyzed. Additional research studies investigating refracture and mortality based on large-scale registry data are needed. Fourth, trends in refracture could be compared to other studies. The secular trend of re-fracture in this study cannot be generalized due to the study period and the characteristics of the database. Finally, cox-regression analysis was used to analyze the effect of refracture on mortality. However, competing risk analysis was not performed. In addition, statistical processing was difficult due to the use of claim data. Nevertheless, cohort data from the NHIS were used to analyze refracture patterns for a nationally representative population. Reporting the incidence according to different scenarios of major osteoporotic refractures would be meaningful.
In summary, in this nationwide study, the incidence of osteoporotic re-fracture was 15.5%. The mortality rate in refracture patients was found to be 1.2 times higher than that in non-refracture patients over a median follow-up of 3 years.
ACKNOWLEDGEMENTS
This study used National Health Insurance Service (NHIS)-National Sample Cohort data (REQ0000016926) provided by NHIS. This research was supported by a grant (HC15C1189) from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI) funded by the Ministry of Health & Welfare, Republic of Korea.
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: Jun-Il Yoo and Yong-Chan Ha.
- Data curation: Rock-Beum Kim and Sung-Hyo Seo.
- Formal analysis: Ki Soo Park.
- Funding acquisition: Jun-Il Yoo and Yong-Chan Ha.
- Investigation: Kyung-Hoi Koo.
- Methodology: Rock-Beum Kim, Sung-Hyo Seo, and Ki Soo Park.
- Project administration: Kyung-Hoi Koo.
- Resources: Rock-Beum Kim and Sung-Hyo Seo.
- Software: Rock-Beum Kim and Sung-Hyo Seo.
- Supervision: Jun-Il Yoo and Yong-Chan Ha.
- Validation: Rock-Beum Kim and Sung-Hyo Seo.
- Visualization: Jun-Il Yoo.
- Writing—original draft: Jun-Il Yoo and Yong-Chan Ha.
- Writing—review & editing: Jun-Il Yoo, Yong-Chan Ha, and Ki Soo Park.
References
- 1.Lems WF, Raterman HG. Critical issues and current challenges in osteoporosis and fracture prevention. An overview of unmet needs. Ther Adv Musculoskelet Dis. 2017;9:299–316. doi: 10.1177/1759720X17732562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M. Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet. 2017;389:1323–1335. doi: 10.1016/S0140-6736(16)32381-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Doherty DA, Sanders KM, Kotowicz MA, Prince RL. Lifetime and five-year age-specific risks of first and subsequent osteoporotic fractures in postmenopausal women. Osteoporos Int. 2001;12:16–23. doi: 10.1007/s001980170152. [DOI] [PubMed] [Google Scholar]
- 4.Dennison E, Mohamed MA, Cooper C. Epidemiology of osteoporosis. Rheum Dis Clin North Am. 2006;32:617–629. doi: 10.1016/j.rdc.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Lee YK, Kim JW, Lee MH, Moon KH, Koo KH. Trend in the age-adjusted incidence of hip fractures in South Korea: systematic review. Clin Orthop Surg. 2017;9:420–423. doi: 10.4055/cios.2017.9.4.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teng GG, Curtis JR, Saag KG. Mortality and osteoporotic fractures: is the link causal, and is it modifiable? Clin Exp Rheumatol. 2008;26(5 Suppl 51):S125–S137. [PMC free article] [PubMed] [Google Scholar]
- 7.Nazrun AS, Tzar MN, Mokhtar SA, Mohamed IN. A systematic review of the outcomes of osteoporotic fracture patients after hospital discharge: morbidity, subsequent fractures, and mortality. Ther Clin Risk Manag. 2014;10:937–948. doi: 10.2147/TCRM.S72456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jung HJ, Park YS, Seo HY, Lee JC, An KC, Kim JH, et al. Quality of life in patients with osteoporotic vertebral compression fractures. J Bone Metab. 2017;24:187–196. doi: 10.11005/jbm.2017.24.3.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu CH, Chen CH, Chen PH, Yang JJ, Chang PC, Huang TC, et al. Identifying characteristics of an effective fracture liaison service: systematic literature review. Osteoporos Int. 2018;29:1023–1047. doi: 10.1007/s00198-017-4370-z. [DOI] [PubMed] [Google Scholar]
- 10.Noordin S, Allana S, Masri BA. Establishing a hospital based fracture liaison service to prevent secondary insufficiency fractures. Int J Surg. 2018;54(Pt B):328–332. doi: 10.1016/j.ijsu.2017.09.010. [DOI] [PubMed] [Google Scholar]
- 11.Chang YF, Huang CF, Hwang JS, Kuo JF, Lin KM, Huang HC, et al. Fracture liaison services for osteoporosis in the Asia-Pacific region: current unmet needs and systematic literature review. Osteoporos Int. 2018;29:779–792. doi: 10.1007/s00198-017-4347-y. [DOI] [PubMed] [Google Scholar]
- 12.Binkley N, Blank RD, Leslie WD, Lewiecki EM, Eisman JA, Bilezikian JP. Osteoporosis in crisis: it's time to focus on fracture. J Bone Miner Res. 2017;32:1391–1394. doi: 10.1002/jbmr.3182. [DOI] [PubMed] [Google Scholar]
- 13.Stolnicki B, Oliveira LG. For the first fracture to be the last. Rev Bras Ortop. 2016;51:121–126. doi: 10.1016/j.rboe.2016.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dreinhöfer KE, Féron JM, Herrera A, Hube R, Johnell O, Lidgren L, et al. Orthopaedic surgeons and fragility fractures. A survey by the Bone and Joint Decade and the International Osteoporosis Foundation. J Bone Joint Surg Br. 2004;86:958–961. doi: 10.1302/0301-620x.86b7.15328. [DOI] [PubMed] [Google Scholar]
- 15.Johnell O, Kanis JA, Odén A, Sernbo I, Redlund-Johnell I, Petterson C, et al. Fracture risk following an osteoporotic fracture. Osteoporos Int. 2004;15:175–179. doi: 10.1007/s00198-003-1514-0. [DOI] [PubMed] [Google Scholar]
- 16.Lauritzen JB, Lund B. Risk of hip fracture after osteoporosis fractures. 451 women with fracture of lumbar spine, olecranon, knee or ankle. Acta Orthop Scand. 1993;64:297–300. doi: 10.3109/17453679308993629. [DOI] [PubMed] [Google Scholar]
- 17.Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004;35:375–382. doi: 10.1016/j.bone.2004.03.024. [DOI] [PubMed] [Google Scholar]
- 18.Park YG, Jang S, Ha YC. Incidence, morbidity and mortality in patients older than 50 years with second hip fracture in a Jeju cohort study. Hip Pelvis. 2014;26:250–255. doi: 10.5371/hp.2014.26.4.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheung CL, Ang SB, Chadha M, Chow ES, Chung YS, Hew FL, et al. An updated hip fracture projection in Asia: The Asian Federation of Osteoporosis Societies study. Osteoporos Sarcopenia. 2018;4:16–21. doi: 10.1016/j.afos.2018.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim L, Kim JA, Kim S. A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples. Epidemiol Health. 2014;36:e2014008. doi: 10.4178/epih/e2014008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yoon HK, Park C, Jang S, Jang S, Lee YK, Ha YC. Incidence and mortality following hip fracture in Korea. J Korean Med Sci. 2011;26:1087–1092. doi: 10.3346/jkms.2011.26.8.1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park C, Ha YC, Jang S, Jang S, Yoon HK, Lee YK. The incidence and residual lifetime risk of osteoporosis-related fractures in Korea. J Bone Miner Metab. 2011;29:744–751. doi: 10.1007/s00774-011-0279-3. [DOI] [PubMed] [Google Scholar]
- 23.Choi HJ, Shin CS, Ha YC, Jang S, Jang S, Park C, et al. Burden of osteoporosis in adults in Korea: a national health insurance database study. J Bone Miner Metab. 2012;30:54–58. doi: 10.1007/s00774-011-0280-x. [DOI] [PubMed] [Google Scholar]
- 24.Lee YK, Jang S, Jang S, Lee HJ, Park C, Ha YC, et al. Mortality after vertebral fracture in Korea: analysis of the National Claim Registry. Osteoporos Int. 2012;23:1859–1865. doi: 10.1007/s00198-011-1833-5. [DOI] [PubMed] [Google Scholar]
- 25.Lee YK, Ha YC, Park C, Yoo JJ, Shin CS, Koo KH. Bisphosphonate use and increased incidence of subtrochanteric fracture in South Korea: results from the National Claim Registry. Osteoporos Int. 2013;24:707–711. doi: 10.1007/s00198-012-2016-8. [DOI] [PubMed] [Google Scholar]
- 26.Kang HY, Yang KH, Kim YN, Moon SH, Choi WJ, Kang DR, et al. Incidence and mortality of hip fracture among the elderly population in South Korea: a population-based study using the national health insurance claims data. BMC Public Health. 2010;10:230. doi: 10.1186/1471-2458-10-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee YK, Ha YC, Yoon BH, Koo KH. Incidence of second hip fracture and compliant use of bisphosphonate. Osteoporos Int. 2013;24:2099–2104. doi: 10.1007/s00198-012-2250-0. [DOI] [PubMed] [Google Scholar]
- 28.Brozek W, Reichardt B, Zwerina J, Dimai HP, Klaushofer K, Zwettler E. Antiresorptive therapy and risk of mortality and refracture in osteoporosis-related hip fracture: a nationwide study. Osteoporos Int. 2016;27:387–396. doi: 10.1007/s00198-015-3415-4. [DOI] [PubMed] [Google Scholar]
- 29.Kim KH. Comorbidity adjustment in health insurance claim database. Health Policy Manag. 2016;26:71–78. [Google Scholar]
- 30.Hsiao PC, Chen TJ, Li CY, Chu CM, Su TP, Wang SH, et al. Risk factors and incidence of repeat osteoporotic fractures among the elderly in Taiwan: a population-based cohort study. Medicine (Baltimore) 2015;94:e532. doi: 10.1097/MD.0000000000000532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Center JR, Bliuc D, Nguyen TV, Eisman JA. Risk of subsequent fracture after low-trauma fracture in men and women. JAMA. 2007;297:387–394. doi: 10.1001/jama.297.4.387. [DOI] [PubMed] [Google Scholar]
- 32.Ruan WD, Wang P, Ma XL, Ge RP, Zhou XH. Analysis on the risk factors of second fracture in osteoporosis-related fractures. Chin J Traumatol. 2011;14:74–78. [PubMed] [Google Scholar]
- 33.Nakayama A, Major G, Holliday E, Attia J, Bogduk N. Evidence of effectiveness of a fracture liaison service to reduce the re-fracture rate. Osteoporos Int. 2016;27:873–879. doi: 10.1007/s00198-015-3443-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721–739. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
- 35.van Staa TP, Leufkens HG, Cooper C. Does a fracture at one site predict later fractures at other sites? A British cohort study. Osteoporos Int. 2002;13:624–629. doi: 10.1007/s001980200084. [DOI] [PubMed] [Google Scholar]
- 36.Bliuc D, Nguyen ND, Nguyen TV, Eisman JA, Center JR. Compound risk of high mortality following osteoporotic fracture and refracture in elderly women and men. J Bone Miner Res. 2013;28:2317–2324. doi: 10.1002/jbmr.1968. [DOI] [PubMed] [Google Scholar]