Short abstract
Langerhans cell histiocytosis (LCH) is a disorder caused by clonal proliferation of CD1a+/CD207+ cells and characterized by varying degrees of organ involvement. Treatment of LCH is risk adapted; patients with multisystem disease and risk-organ involvement require more intensive therapy. Optimal therapies for multisystem, high-risk LCH remain uncertain. Recently, targeted therapy using inhibitors of mutated BRAF (the gene encoding serine/threonine-protein kinase B-Raf) has proven very effective in patients with multisystem refractory LCH. Herein, we report a case of LCH with involvement of the bones, liver, and lymph nodes. Using next-generation sequencing of the patient’s pathological sample, we identified a mutation in MAP2K1 in exon 3 (c.362G>C, p.Cys121Ser) and no mutation in BRAF; thus, high-risk, multisystem LCH with MAP2K1 mutation and wild-type BRAF was diagnosed. After four chemotherapy treatments (COEP regimen), the patient received autologous hematopoietic stem cell transplantation (auto-HSCT). Complete remission was confirmed by follow-up positron emission tomography–computed tomography, which showed no lesions in liver, lymph nodes, or bones compared with the pretreatment period. To date, the patient has sustained good health for 24 months. In conclusion, auto-HSCT may be an effective treatment option for high-risk, multisystem BRAF V600E-negative LCH.
Keywords: Langerhans cell histiocytosis, high-risk, multisystem, BRAF V600E mutation negative, autologous hematopoietic stem cell transplantation, MAP2K1 mutation
Introduction
Langerhans cell histiocytosis (LCH) is a heterogeneous disease, characterized by accumulation of dendritic cells, that affects patients of different ages, predominantly children. The diagnosis of LCH is based on the histopathological pattern observed in biopsy specimens. Currently, the most commonly used biomarkers to identify active LCH are CD207 and CD1a.1,2
The treatment for LCH depends on the severity and part of body affected. In some cases, no treatment is necessary. Nevertheless, in patients where the disease has affected multiple body areas (i.e., multisystem disease), special treatment may be required, including surgery and low doses of radiotherapy and chemotherapy. A combination of cytarabine and cladribine is currently considered the second-line therapy for refractory cases of LCH with vital organ dysfunction.3
Recent advances in our understanding of the pathogenesis of LCH have promoted the development of new treatment options. The BRAF V600E mutation, responsible for activation of the MAP kinase (RAS-RAF-MEK-ERK) cell-signaling pathway in pathologic histiocytes, is present in ∼55% of LCH cases and associated with recurrence and high-risk presentation.4 Recently, targeted therapy using a newly approved inhibitor of mutated BRAF (vemurafenib) has proven to be very efficient in treating patients with multisystemic refractory LCH.4 Herein, we report a single case of a patient with high-risk, multisystem BRAF V600E− LCH that was successfully treated with autologous hematopoietic stem cell transplantation (auto-HSCT).
Case report
A 28-year-old man was admitted to our hospital on 25 March 2016 because of lower back pain. For 2 months before admission, the patient had experienced low back pain, without the pain radiating to lower limbs, and relief after rest. Blood count, liver and kidney function, and levels of calcium, phosphorus, and alkaline phosphatase were all normal. Abdominal ultrasound revealed liver space-occupying lesions (low-echo nodules, 2.2 × 2.0 cm, in the right anterior lobe of the liver). A whole-spine magnetic resonance image showed bone signal abnormalities of the seventh to ninth thoracic vertebrae (T7 to T9), the second lumbar vertebra (L2), the first sacral vertebra (S1) body and attachment, and the surrounding soft tissue block; T7, T8 vertebral pathological fracture; rear stenosis; and compression of the spinal cord.
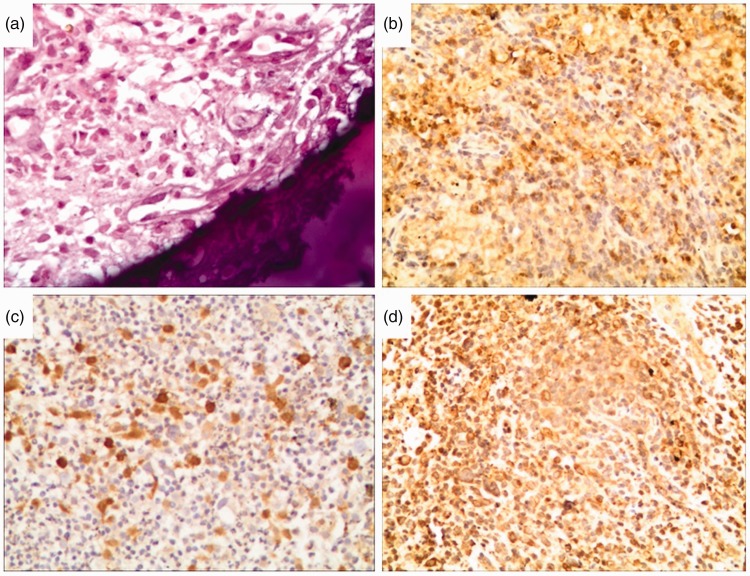
The lesions around the L2 vertebral body were surgically resected. The biopsy report showed a large number of Langerhans cells with eosinophilic granulocytes and small lymphocytes; immunohistochemical staining showed the following: S100 (++), CD1a (+), CD207 (++), CD68 (++), HMB45 (−), CKP (−), EMA (−), CD45 (++), CD21 (−), CD23 (−), Ki-67 nuclear index >20% positive cells (Figure 1). Next-generation sequencing of the pathological sample subsequently identified a MAP2K1 mutation in exon 3 (c.362G>C, p.Cys121Ser); the sample was negative for the BRAF mutation.
Figure 1.
The biopsy of the lesions around the L2 vertebral body showing a large number of Langerhans cells with eosinophilic granulocytes and small lymphocytes. (A) hematoxylin and eosin (HE); (B) CD207++; (C) CD1a+; (D) S100++. ×200.
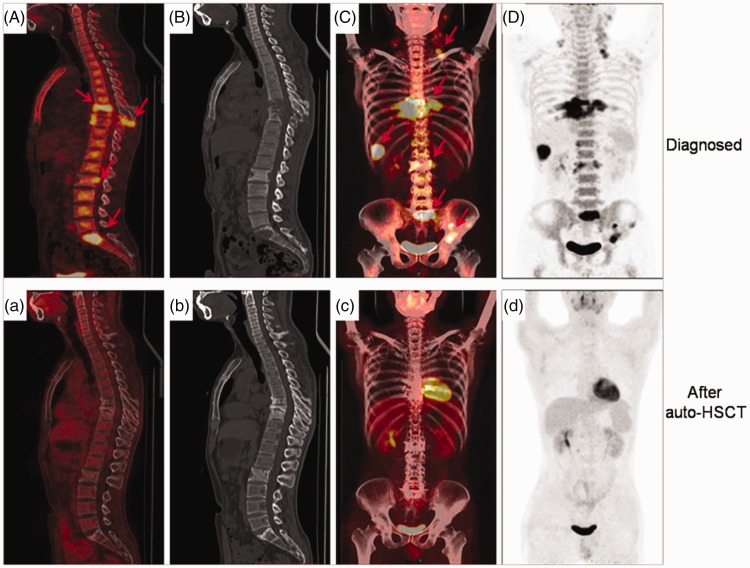
To complete the staging for LCH, a whole-body positron emission tomography-computed tomography scan (PET-CT) was performed on 1 April 2016 and revealed the following: (1) multiple 18F-fluorodeoxyglucose (FDG)-avid lesions in the liver and systemic multiple lymph nodes and osteolytic lesions (T7, T8, T9, and S1) with maximum standardized uptake value (SUVmax) of 10.5; and (2) pathological compression fracture of T8 (Figure 2). A bone marrow smear was within normal limits. A diagnosis of high-risk multisystem LCH with involvement of the bones, liver, and lymph nodes was made.
Figure 2.
The PET-CT images of a 28-year-old male patient with LCH before (1 April 2016) and after (1 January 2017) receiving auto-HSCT. (A–D) Images showing multiple lesions (arrowheads in A and C) in liver, lymph nodes, and bones, as well as osteolytic lesions (T7, T8, T9, and S1) with SUVmax 10.5 before therapy. (a–d) Images showing no highly FDG-avid lesions in liver, lymph nodes, or bones and smaller osteolytic lesions. Compared with the initial diagnosis, we found evidence of peripheral sclerosis (T7, T8, T9, and S1), an indicator of bone regeneration. PET-CT, positron emission tomography–computed tomography; LCH, Langerhans cell histiocytosis; auto-HSCT, autologous hematopoietic stem cell transplantation; SUVmax, maximum standardized uptake value; FDG, 18F-fluorodeoxyglucose.
Consequently, the patient received an induction chemotherapy COEP regimen (cyclophosphamide 750 mg/m2 on day 1, vincristine 1.4 mg/m2 on day 1, etoposide 60 mg/m2/day from day 1 to 7, and dexamethasone 25 mg/m2/day from day 1 to 7). The lower back pain was relieved after two courses of COEP and the patient received two additional courses of COEP as consolidation chemotherapy. After four COEP treatments, we made a comprehensive physical review of the patient. The chest CT showed multiple osteolytic lesions (T7, T8, T9 vertebral body and appendage, right ninth posterior rib, and bilateral eighth posterior rib). Abdominal ultrasound revealed a slightly reduced liver hepatic lesion (low-echo nodules of 2.0 × 1.6 cm in the right anterior lobe of the liver). Thus, after four COEP treatments, the patient’s condition was almost stable. A matched donor was not available for an allogeneic stem cell transplant; thus, we proceeded with auto-HSCT therapy.
In August 2016, the patient received a transplant conditioning regimen, including total body irradiation and multidrug chemotherapy, as follows: 7.0 Gy total body irradiation (5.0 Gy on lungs, dose rate <10 cGy/min) on day −5; vincristine 2 mg/day (day −5); etoposide 100 mg/day (from day −5 to day −4); idarubicin 10 mg/day (from day −5 to day −3); Ara-C (cytarabine) 1000 mg twice a day (from day −5 to day −3); cyclophosphamide 60 mg/kg on day −2, followed by infusion of 8.36 × 106 cells/kg of body weight CD34+ autologous stem cells. The post-transplant course was uneventful, with a neutropenic episode lasting 9 days. Granulocyte-colony stimulating factor (G-CSF), 300 µg/day, was administered from day +5 to day +12. Leukocyte (40,000/mL) and platelet engraftment (420,000/mL) occurred on day +12 and day +22, respectively.
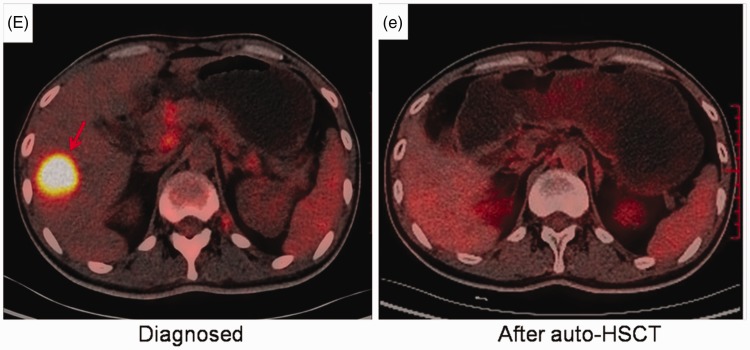
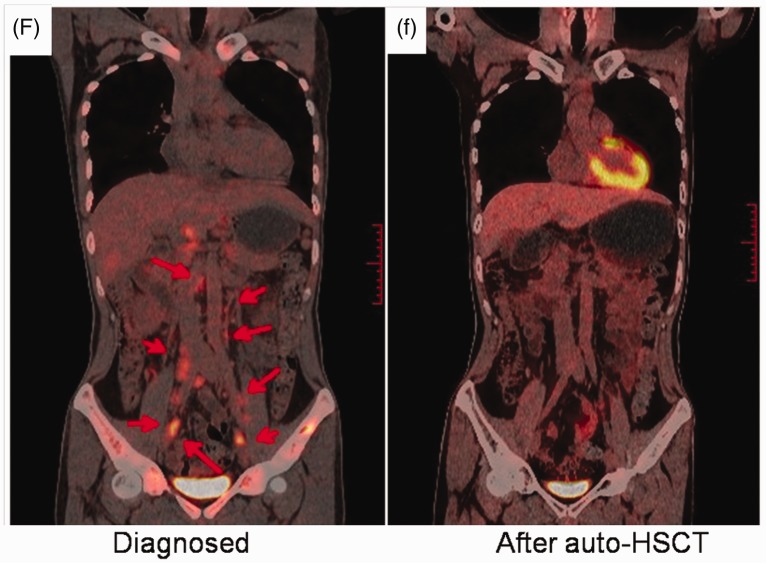
One month after therapy, no liver hepatic lesions were visible by abdominal ultrasound. Subsequently, on 1 January 2017, 17 October 2017, and 28 August 2018, the patient underwent whole-body PET-CT; the results showed no FDG-avid lesions in liver, lymph nodes, or bones, compared with the results of PET-CT on 1 April 2016 (Figures 2 to 4). To date, the patient has sustained good health for 24 months.
Figure 3.
The liver PET-CT scan showing significantly decreased FDG signal after the administration of auto-HSCT (e; 1 January 2017) compared with the pretreatment period (E; 1 April 2016). PET-CT, positron emission tomography–computed tomography; FDG, 18F-fluorodeoxyglucose; auto-HSCT, autologous hematopoietic stem cell transplantation.
Figure 4.
Metabolic changes in retroperitoneal lymph nodes at the initial diagnosis (1 April 2016) and after auto-HSCT (1 January 2017). (F) Multiple FDG-avid lesions in retroperitoneal lymph nodes (arrowheads). (f) No FDG-avid lesions in retroperitoneal lymph nodes. Auto-HSCT, autologous hematopoietic stem cell transplantation; FDG, 18F-fluorodeoxyglucose.
This case report was approved by the Medical Ethics Committee of the Lanzhou General Hospital. Verbal consent was obtained from the patient.
Discussion
LCH is a rare disorder with variable clinical manifestations. A definitive diagnosis of LCH is based on immunohistochemical detection of CD1a and CD207 antigens in the biopsy specimen. Mutant BRAF V600E, a driver mutation in LCH, has an important role in the pathogenesis of LCH but it is not specific to the diagnosis of LCH. In the present case, histological examination revealed positive staining for CD1a, CD207, and S-100 protein. LCH may sometimes result in life-threatening multisystem diseases, which depends on “risk organ” involvement (bone marrow, liver, and spleen).
The RAS-RAF-MEK-ERK-MAP kinase pathway is activated in all patients with LCH, including those with wild-type BRAF.5 In addition to BRAF mutations in ∼55% of LCH, MAP2K1 mutations have been reported in 33% to 50% of patients with wild-type BRAF.6,7 Mutations in KRAS and ARAF have also been observed in rare cases. Our patient harbored a MAP2K1 mutation in exon 3 (c.362G>C, p.Cys121Ser) and wild-type BRAF.
Several retrospective case reports and one prospective clinical trial have shown that vemurafenib is effective for patients with the BRAF V600E mutation. Dabrafenib, another BRAF inhibitor, is efficacious and safe in refractory/relapsed LCH, as verified by a retrospective case series.8 The response rates of MEK inhibitors (alone or in combination with a BRAF inhibitor)9,10 appear to be similar to those of BRAF inhibitors.
The goal of targeted treatment and prevention of LCH-related mortality may soon become a reality. Nevertheless, it is very unlikely that the currently available MAPK pathway inhibitors will become the standard of care for all patients with LCH because of their high cost and serious side effects. Many patients require dose reductions or discontinuation of vemurafenib because of its toxicity.11,12 Furthermore, about 75% of patients in remission relapsed after BRAF inhibitors were stopped.13
Various treatments have been used for LCH but not always with successful outcomes. Allogeneic HSCT is considered an effective therapeutic option for patients with LCH who do not receive systemic chemotherapy or those with refractory or multisystem disease.14–16 Conter et al.17 reported three patients with refractory LCH who received autologous HSCT. The disease remained refractory in two cases, eventually leading to death, but transiently improved in the third case; however, the patient relapsed 3 months after therapy. Although there are several reports of effective autologous HSCT for LCH, these remain very rare.18
PET-CT has shown to be useful in identifying active lesions, stratifying disease stage, monitoring treatment response, and detecting LCH reactivation.19 Phillips et al.20 demonstrated that LCH disease activity and response to therapy may be detected using an FDG tracer, which is thought to be more accurate than bone scans or plain X-rays. In the current case, complete remission was confirmed by follow-up PET-CT; our data indicated no lesions in liver, lymph nodes, or bones compared with the pretreatment period. Furthermore, we observed a dramatic improvement in the appearance of multiple lytic bone lesions following HSCT, with lesions decreasing in size. There was also evidence of peripheral sclerosis, which is an indication of bone regeneration. In conclusion, auto-HSCT may be a good treatment choice for high-risk, multisystem BRAF V600E− LCH.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This work was supported by a grant-in-aid from the National Science Foundation of China (No. 81372132).
References
- 1.Allen CE, Li L, Peters TL, et al. Cell-specific gene expression in Langerhans cell histiocytosis lesions reveals a distinct profile compared with epidermal Langerhans cells. J Immunol 2010; 184: 4557–4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Milne P, Bigley V, Bacon CM, et al. Hematopoietic origin of Langerhans cell histiocytosis and Erdheim-Chester disease in adults. Blood 2017; 130: 167–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arico M. Langerhans cell histiocytosis in children: from the bench to bedside for an updated therapy. Br J Haematol 2016; 173: 663–670. [DOI] [PubMed] [Google Scholar]
- 4.Haroche J, Cohen-Aubart F, Emile JF, et al. Dramatic efficacy of vemurafenib in both multisystemic and refractory Erdheim-Chester disease and Langerhans cell histiocytosis harboring the BRAF V600E mutation. Blood 2013; 121: 1495–1500. [DOI] [PubMed] [Google Scholar]
- 5.Badalian-Very G, Vergilio JA, Degar BA, et al. Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood 2010; 116: 1919–1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berres ML, Merad M, Allen CE. Progress in understanding the pathogenesis of Langerhans cell histiocytosis: back to Histiocytosis X? Br J Haematol 2015; 169: 3–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nelson DS, van Halteren A, Quispel WT, et al. MAP2K1 and MAP3K1 mutations in Langerhans cell histiocytosis. Genes Chromosomes Cancer 2015; 54: 361–368. [DOI] [PubMed] [Google Scholar]
- 8.Bhatia A, Ulaner G, Rampal R, et al. Single‐agent dabrafenib for BRAFV600E‐mutated histiocytosis. Haematologica 2018; 103: e177–e180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al Bayati A, Plate T, Al Bayati M, et al. Dabrafenib and trametinib treatment for Erdheim–Chester disease with brain stem involvement. Mayo Clin Proc Innov Qual Outcomes 2018; 2: 303–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen Aubart F, Emile JF, Maksud P, et al. Efficacy of the MEK inhibitor cobimetinib for wild-type BRAF Erdheim–Chester disease. Br J Haematol 2018; 180: 150–153. [DOI] [PubMed] [Google Scholar]
- 11.Haroche J, Cohen-Aubart F, Emile JF, et al. Reproducible and sustained efficacy of targeted therapy with vemurafenib in patients with BRAF(V600E)-mutated Erdheim-Chester disease. J Clin Oncol 2015; 33: 411–418. [DOI] [PubMed] [Google Scholar]
- 12.Hyman DM, Puzanov I, Subbiah V, et al. Vemurafenib in multiple nonmelanoma cancers with BRAF V600 mutations. N Engl J Med 2015; 373: 726–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen Aubart F, Emile JF, Carrat F, et al. Targeted therapies in 54 patients with Erdheim–Chester disease, including follow-up after interruption (the LOVE study). Blood 2017; 130: 1377–1380. [DOI] [PubMed] [Google Scholar]
- 14.Veys PA, Nanduri V, Baker KS, et al. Haematopoietic stem cell transplantation for refractory Langerhans cell histiocytosis: outcome by intensity of conditioning. Br J Haematol 2015; 169: 711–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cruz-Chacon A, Mathews J, Ayala E. Transplantation in rare lymphoproliferative and histiocytic disorders. Cancer Control 2014; 21: 335–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akkari V, Donadieu J, Piguet C, et al. Hematopoietic stem cell transplantation in patients with severe Langerhans cell histiocytosis and hematological dysfunction: experience of the French Langerhans Cell Study Group. Bone Marrow Transplant 2003; 31: 1097–1103. [DOI] [PubMed] [Google Scholar]
- 17.Conter V, Reciputo A, Arrigo C, et al. Bone marrow transplantation for refractory Langerhans' cell histiocytosis. Haematologica 1996; 81: 468–471. [PubMed] [Google Scholar]
- 18.Ichikawa K, Nomura S, Ishii K, et al. Autologous stem cell transplantation for refractory Langerhans' cell histiocytosis. Bone Marrow Transplant 2007; 40: 807–808. [DOI] [PubMed] [Google Scholar]
- 19.Kaste SC, Rodriguez-Galindo C, McCarville ME, et al. PET-CT in pediatric Langerhans cell histiocytosis. Pediatr Radiol 2007; 37: 615–622. [DOI] [PubMed] [Google Scholar]
- 20.Phillips M, Allen C, Gerson P, et al. Comparison of FDG-PET scans to conventional radiography and bone scans in management of Langerhans cell histiocytosis. Pediatr Blood Cancer 2009; 52: 97–101. [DOI] [PubMed] [Google Scholar]