Short abstract
Objective
A basicervical femoral neck fracture, which is located at the junction between the femoral neck and intertrochanteric region, is a rare type of fracture. The treatment effects for this type of fracture vary. The present retrospective study was performed to evaluate the clinical and radiological outcomes of proximal femoral nail antirotation and illustrate its effect on improving the clinical prognosis of basicervical femoral neck fractures.
Methods
Fourteen patients with two-part basicervical fractures underwent treatment with proximal femoral nail antirotation.
Results
The treatment exhibited a good effect on decreasing complications such as femoral neck shortening and screw protrusion. Improvements were also noted in the Harris hip score and other clinical prognostic factors. The patients were satisfied with the prognosis, although not all of them returned to their preinjury level of occupation or daily activities.
Conclusion
This research provides clinical data to support the treatment of basicervical femoral neck fractures with proximal femoral nail antirotation and contributes to our understanding of treatment selection in the clinical setting. Selection of the optimal fixation method and subsequent conservative rehabilitation plan will benefit patients with basicervical femoral neck fractures.
Keywords: Basicervical femoral neck fracture, proximal femoral nail antirotation, complication, prognosis, Harris hip score, fixation
Introduction
Femoral neck fracture (FNF) accounts for 3.6% of all fractures and is commonly encountered among older people, for whom it is associated with high mortality and morbidity, and among young, healthy people who have sustained high-energy trauma.1,2 Current implant selections for FNFs remain a topic of interest and controversy and vary substantially depending on the extent of displacement, fracture configuration, physiological age of the patient, bone quality, and other factors. Nonoperative management is considered only when patients are seriously ill or present with excessive surgical risk.2,3 Basicervical FNF is a special type of FNF.
A basicervical FNF is located at the junction between the femoral neck and intertrochanteric region. This is a rare type of fracture with a reported incidence of about 1.8% to 7.6% among all hip fractures.3,4 A basicervical FNF is always obscured by the trochanteric area, which makes the fracture line poorly visible or even invisible.3,5 Some studies have concentrated on basicervical FNF as a separate entity, and the treatment of basicervical FNFs remains controversial.3,5,6 Kuokkanen5 reported that the use of multiple screws was not recommended in the treatment of basicervical FNFs. Some studies have shown that internal fixation with cannulated screws for basicervical FNFs has poor clinical outcomes.3 In recent years, more researchers have concluded that basicervical FNFs should be treated as extracapsular fractures, such as trochanteric fractures.
Improvements to the original design of intramedullary nails have significantly reduced the rates of fixation failure. Because of the proposed benefits of intramedullary nails (a less invasive approach, small transfusion rate, and superior biomechanical characteristics), most surgeon use this treatment technique exclusively for peritrochanteric fractures. Proximal femoral nail antirotation (PFNA) is the most commonly performed treatment for peritrochanteric fractures in our department. A clear consensus that intramedullary fixation is more beneficial to prevent complications such as fixation failure has been reached.7 However, few studies have focused on the outcomes of PNFA in treating basicervical FNFs.4–6 Therefore, the present study was performed to retrospectively evaluate the clinical and radiological outcomes of PFNA and illustrate its effect on improving the clinical prognosis of basicervical FNFs.
Materials and methods
Patients
Among all patients with FNFs who were admitted to and treated in our hospital from January 2015 to March 2017, we analyzed those who had been diagnosed with basicervical FNFs according to the definition by Watson and had no history of hip surgery. Their demographic and radiological data were retrospectively collected from our institutional database. All methods were performed in accordance with the relevant guidelines and regulations in the Third Hospital of Hebei Medical University.7 This retrospective study was conducted in 2018, and the patients were contacted by telephone to ensure that they agreed to participate in the study. Informed consent was obtained from all participants or their legal guardians. The inclusion criteria were the presence of a closed FNF and a follow-up time of >1 year. The exclusion criteria were the presence of a pathological FNF, treatment with internal fixation techniques other than PFNA, and surgical treatment with open reduction. We also excluded fractures in which the lesser trochanter had separated, fractures in which the fracture line ran distal to the lesser trochanter or out the lateral cortex of the greater trochanter, and transcervical fractures. Radiographs were reviewed to ensure that there was no evidence indicating the need to reclassify the fracture patterns as either transcervical or intertrochanteric. This study was approved by the ethics committee of the Third Hospital of Hebei Medical University (trial number NCT03550079). The study was performed in compliance with the STROBE research guidelines.
Surgical procedures
All patients were maintained on bed rest until the operation. The operation was performed under either general or regional anesthesia at the anesthesiologist’s discretion. The patient was placed in the supine position followed by fracture reduction and fixation with a PFNA device (Synthes, Solothurn, Switzerland) using an image intensifier. After insertion of the nail, the guide pin was inserted into the center of the femoral head to guide the placement of the helical blade. The blade was placed in the middle-inferior one-third of the femoral neck as confirmed on the anteroposterior view and in the middle one-half as confirmed on the lateral view. The tip of the helical blade was located in the subchondral area of the femoral head. Distal locking screws were inserted to prevent rotation of the nail. The quality of reduction was ensured on the anteroposterior and lateral views, and all operations were conducted by senior surgeons. The stitches were routinely removed at approximately 2 weeks in most patients; removal was delayed when preoperative gross swelling of the wound had occurred.
Perioperative management
Passive knee and hip range-of-motion exercises were performed after the operation. Deep vein thrombosis was prevented by administration of low-molecular-weight heparin for 1 week after the operation. The patients were encouraged to sit on the bed and exercise their lower limb muscles for the first 24 hours. Until 8 weeks postoperatively, the patients were encouraged to perform partial weight-bearing ambulation with assistance. After 8 weeks postoperatively, full weight-bearing ambulation was started at 20 kg with an incremental increase of 5 kg per week when evidence of complete fracture union was present.
Outcome measurement
The patients were followed up clinically and radiologically in the orthopedic clinic at regular intervals, and the progress of fracture union and possible complications were assessed every 2 to 3 months for at least 1 year. Data regarding surgical blood loss, surgical time (from skin incision to skin closure), hospital stay, type of anesthesia (regional or general), and surgical risk according to the American Society of Anesthesiologists classification as assessed by the anesthesiologist were extracted from the medical records.8 The adequacy of fracture reduction (good, acceptable, or poor) and the tip–apex distance (TAD) were also measured on anteroposterior and lateral radiographs using the known diameter of the implanted lag screw on the initial postoperative radiographs according to the method described by Fogagnolo et al.9 The patients were monitored for complications such as femoral neck shortening, screw protrusion, screw cutout, nonunion (defined as a fracture with no sign of healing radiographically or clinically at 12 months postoperatively), and avascular necrosis. Femoral neck shortening measured in the vertical plane was categorized into four degrees: 0, 1, 2, and 3.10,11 The Harris hip score (range, 1–100) was used to evaluate hip function at the end of follow-up.12,13 The results were categorized as excellent (90–100), good (80–89), fair (70–79), or poor (<69). Fixation failure was treated by a reoperation, such as conversion to hip arthroplasty. All radiographic evaluations and measurements were performed by the first author (all authors reviewed all radiographs). Any disagreements in the assessment of categorical data were resolved by the corresponding author.
Results
Of 2291 patients with FNFs treated in our hospital during the study period, 17 consecutive patients with 17 two-part basicervical FNFs were retrospectively reviewed. A representative two-part basicervical FNF is shown in Figure 1. Among the 17 patients, 3 (17.65%) were treated with cannulated screws; the remaining 14 patients were followed up and analyzed in this study. The patients comprised 4 men and 10 women with a mean age of 67.6 years at the time of fracture (range, 56–93 years). The mean follow-up duration was 15 months (range, 12–21 months). Twelve patients were injured after slips, trips, or falls, and two patients were injured in traffic accidents. Tibial tuberosity traction was used in 10 patients to reduce soft tissue contracture and iatrogenic damage to the blood supply; the other 4 patients refused tibial tuberosity traction because of fear regarding complications of this invasive manipulation. All operations were performed by senior orthopedic surgeons using a long PFNA (n = 7) or short PFNA (n = 7) in our department. The average time between injury and surgical intervention was 3 days (range, 2–7 days), mainly because of a delay in reporting to the hospital and the time taken to examine and regulate the patients’ biochemical indices to achieve normal values before surgery. Thirteen patients had a normal ambulation status and one patient used a walker for ambulation (Table 1). Because almost all patients were >60 years of age, 10 of the patients had underlying medical conditions including osteoporosis, cardiovascular disease, and others.
Figure 1.
Radiograph of a two-part basicervical fracture.
Table 1.
General information of patients with basicervical femoral neck fractures.
| Patient no. | Age (years) | Sex | Follow-up time (months) | Time from injury to surgery (days) | Body mass index (kg/m2) | Mechanism | Mean ASA score | Type of anesthesia | Use of walking aid before operation |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 56 | F | 21 | 1 | 27.7 | Slip, trip, or fall | 2 | General | No |
| 2 | 65 | F | 15 | 2 | 22.0 | Traffic accident | 3 | Regional | No |
| 3 | 69 | M | 15 | 2 | 18.5 | Slip, trip, or fall | 2 | General | Yes |
| 4 | 73 | F | 16 | 3 | 19.0 | Slip, trip, or fall | 3 | Regional | No |
| 5 | 93 | M | 14 | 5 | 18.9 | Slip, trip, or fall | 2 | Regional | No |
| 6 | 67 | F | 15 | 2 | 25.0 | Slip, trip, or fall | 3 | General | No |
| 7 | 59 | F | 15 | 3 | 22.5 | Slip, trip, or fall | 3 | General | No |
| 8 | 67 | M | 12 | 4 | 19.4 | Slip, trip, or fall | 3 | Regional | No |
| 9 | 75 | F | 16 | 3 | 22.0 | Slip, trip, or fall | 2 | Regional | No |
| 10 | 67 | F | 14 | 3 | 22.3 | Slip, trip, or fall | 3 | General | No |
| 11 | 66 | M | 12 | 4 | 27.0 | Slip, trip, or fall | 3 | Regional | No |
| 12 | 61 | F | 16 | 3 | 27.0 | Traffic accident | 2 | General | No |
| 13 | 62 | F | 13 | 4 | 26.0 | Slip, trip, or fall | 3 | General | No |
| 14 | 67 | F | 16 | 3 | 20.6 | Slip, trip, or fall | 2 | General | No |
| Total | 67.6 ± 8.88 | 4 M, 10 F | 15 ± 2.22 | 3 ± 1.04 | 22.7 ± 0.51 | 12 slips, trips, or falls; 2 traffic accidents | 2.57 | 6 regional, 8 general | 13 no aid, 1 aid |
Data in “Total” row are presented as mean ± standard deviation or number of patients.
ASA, American Society of Anesthesiologists; M, male; F, female.
The operative time, surgical blood loss, hospital stay, and complications are shown in Table 2. Notably, no patients developed a postoperative infection. All patients had good fracture reduction on the initial postoperative radiographs, and no obvious differences were observed between the initial postoperative radiographs and last follow-up radiographs.9 Fracture healing was achieved in all 14 patients, and the incidence of screw cutout was low (Figures 2 and 3). No patients had any evidence of fixation failure of the femoral head at the end of the postoperative follow-up. The TAD was measured from the tip of the lag screw to the apex of the femoral head on the postoperative anteroposterior and lateral radiographs. The TAD was <25 mm in all patients (mean, 20.3 mm; range, 12–24 mm). Mild varus reduction was observed in one patient who had shortening of >10 mm. Radiographic union as evidenced by bony trabeculae crossing the fracture interspace occurred in patients; no radiographs contained visible evidence of nonunion. Ten patients returned to their preinjury level of occupation or daily activities, and the other four experienced chronic mild discomfort around the incision site during bad weather or developed other diseases such as cerebral infarction unrelated to their FNF. However, most patients were satisfied with their prognosis and reported that the results surpassed their expectations. At the end of follow-up, the Harris hip score was excellent in nine patients, good in four, and fair in one (Table 3).
Table 2.
Clinical outcomes of patients with basicervical femoral neck fractures.
| Variables | |
| Surgical blood loss, mL | 300 ± 12.3 |
| Surgical time, minutes | 55.0 ± 14.3 |
| Infection | 0 (0.00) |
| Deep vein thrombosis | 4 (28.57) |
| Hospital stay, days | 16.7 ± 3.2 |
Data are presented as mean ± standard deviation or n (%).
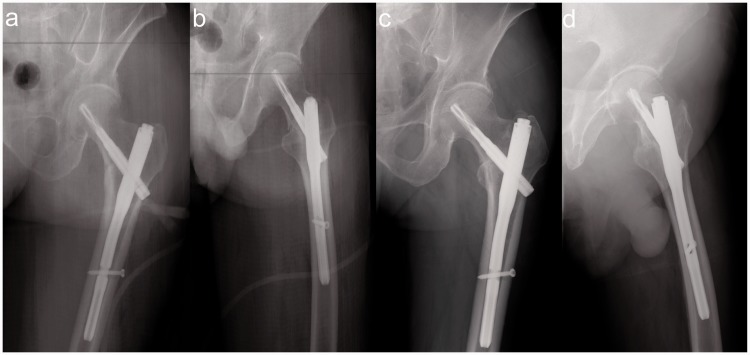
Figure 2.
Postoperative radiographs of a 55-year-old woman treated with short proximal femoral nail antirotation. (a) Postoperative anteroposterior radiograph. (b) Postoperative lateral radiograph. (c, d) Anteroposterior radiographs before completion of follow-up.
Figure 3.
Postoperative radiographs of a 59-year-old woman treated with long proximal femoral nail antirotation. (a) Postoperative anteroposterior radiograph. (b) Postoperative lateral radiograph. (c, d) Anteroposterior radiographs before completion of follow-up.
Table 3.
Postoperative outcomes of patients with basicervical femoral neck fractures.
| Variables | |
| Tip–apex distance, mm | 18.5 (13–25) |
| Shortening of ≥10 mm | 2 |
| Screw protrusion | 0 |
| Screw cutout | 0 |
| Nonunion | 0 |
| Avascular necrosis | 0 |
| Harris hip score | 85.7 ± 3.1 |
Data are presented as median (range), n, or mean ± standard deviation.
Discussion
Although various instrumentation techniques have been reported for stabilization of FNFs, the optimal treatment of basicervical FNFs remains controversial.5,7 Intramedullary and extramedullary fixation are the two main treatment options for two-part basicervical FNFs. Although sufficient evidence may exist to support the use of arthroplasty in treating FNFs, >90% of these fractures may heal and the healing will be uneventful in 85%; the union rate of this special fracture pattern is even higher.1,2,8,10 In the present retrospective study, we reviewed 14 patients treated with long or short PNFA. The surgical time and blood loss were limited; complications such as shortening, cutout, and nonunion were scarce; and the TAD and Harris hip score were satisfactory. Given the rarity of this type of fracture, the present study adds more evidence regarding the efficacy of fixation for this special type of fracture using PFNA. These findings enrich our understanding of PFNA in treating basicervical FNFs and suggest that PFNA should be the first treatment choice for basicervical FNFs.
Only 0.61% (14/2291) of all FNFs treated at our hospital during the study period were identified as basicervical FNFs. This is comparable with other reports.4,7,14,15 Although extramedullary fixation has been traditionally considered the gold standard for treatment of hip fractures, increasingly more research is showing that intramedullary fixation is more appropriate for basicervical fractures. In their biomechanical comparison, Imren et al.16 found that intramedullary fixation bore a higher mechanical load than other fixation methods. However, not all intramedullary fixation techniques are suitable for basicervical FNFs. Hu et al.17 reported that cephalomedullary hip nail fixation could be used for basicervical intertrochanteric fractures and that it provided stable fixation and allowed early exercise. However, the fracture patterns in their study varied; they included not only two-part intertrochanteric fractures but also fractures with greater or lesser trochanteric fragments. Basicervical fractures should be defined as two-part fractures located at the base of the femoral neck and exiting above the lesser trochanter. After application of strict inclusion criteria, Watson et al.7 found that intramedullary fixation was not suitable for basicervical proximal FNFs. However, a proximal femoral nail was commonly used in their study. In our department, instead of multiple screws and extramedullary fixation, intramedullary nailing with a helical blade (PFNA) is always used to treat basicervical fractures because of the difficulty of treating these fractures. Compared with other hip nails such as proximal femoral nails, PFNA exhibits excellent femoral head purchase because of the bone tissue suppression that occurs during drilling and insertion and the maximal compression of the fracture site.
Most surgeons accept that basicervical FNFs should be treated as intertrochanteric fractures. We noted that Pauwel’s angle was greater than that in other patterns of FNFs. Su et al.18 found that basicervical fractures had greater biomechanical instability and collapsed more easily than intertrochanteric fractures. Bojan et al.19 also reported a relatively high incidence of screw cutout in basicervical fractures treated by gamma nails. However, PFNA in our study provided good fracture reduction and a low rate of fixation failure. Additionally, the TAD, which is defined as the best predictor of lag screw cutout, was <25 mm in our study and was considered to be associated with fewer failures (average of 17.4 mm). Watson et al.7 reported high rates of nonunion and cutout in a series of 11 patients, but this may have been caused by the fixation they used, which produced less compression between fractures. The patients in our study were treated by long or short PFNA, and we found no other relevant reports on the treatment of basicervical FNFs with long or short fixation. Hou et al.20 reported there were no differences in the union and complication rates between patients with peritrochanteric femoral fractures treated with short and long cephalomedullary nails. Krigbaum et al.21 also found that the use of long or short cephalomedullary nails had similar rates of complications, readmission, and reoperations. These special fractures were always treated as peritrochanteric fractures, so we imagine that the use of a long or short nail may not affect the results. Additionally, most patients in the study were of advanced age and had osteoporosis; the relatively conservative rehabilitation plan and late time to weight bearing were other important reasons for our good results except the effect of fixation.
A major strength of this study is that it excluded many of the intertrochanteric fractures present in the study by Hu et al.17 and included basicervical fractures comparable with those in the study by Watson et al.7 The results showed a better prognosis than that reported by Watson et al.7 One reason for this difference is that although Watson et al.7 strictly defined basicervical FNFs as two-part fractures that were located at the base of the femoral neck and exited above the lesser trochanter and treated all of these fractures with cephalomedullary nailing, the fixations in their study included two internal fixations that cannot accurately explain the results. Fixation by PFNA has become popularized in our department. All patients in the present study were treated by PFNA, which reportedly has superior mechanical properties than other types of nails. Another reason may be that collapse of the fracture, movement of the position of the lag screw in the femoral head, and nonunion of the fracture were all defined as failure of fixation in the study by Watson et al.7 Movement of the lag screw or mild collapse may not always render a poor prognosis in the clinical setting and may be compensated by walking gait. Additionally, four factors were found to contribute to the complication of cutout: the implant design, a complex fracture pattern, nonanatomical reduction, and a nonoptimal screw position.19 Insertion of the screw into the femoral neck placed the screw in an unsatisfactory position (more superior lag screw placement) in the study by Watson et al.,7 but our orthopedic surgeons ensured that all screws were located upon the femoral calcar (inferior placement of the lag screw) and centrally on the lateral radiograph, and this increased the anchor strength, thus minimizing complications.7 Although a comparative study was conducted by Lee et al.,22 the patients enrolled did not originate from the same period, and their rehabilitation protocol was more aggressive than ours. The average age of their patients was higher than that of our patients, which may be another reason for the differences in the prognosis.
The main limitations of our study are the small number of patients and retrospective design. Other types of intramedullary nails, such as Gamma and InterTan nails, were not included. However, the clinical outcomes of each of these devices are controversial, and the results of different fixation techniques may vary. All patients were treated with PFNA, and the deficiency of a control group was another limitation of this study. The femoral head is considered safe from the occurrence of avascular necrosis after a 5-year clinical observation period, and the relatively short follow-up period in this study may have been insufficient to register all cases of femoral head necrosis, especially late avascular necrosis. However, the average follow-up period of 15 months was still sufficient to demonstrate the occurrence of bone union or most complications after the operation.
Conclusions
This retrospective study showed that PFNA is an appropriate treatment choice for strictly defined two-part basicervical FNFs followed by a relatively conservative rehabilitation plan. Selection of the optimal fixation method and subsequent conservative rehabilitation plan will benefit patients with basicervical FNFs. However, research involving more patients and longer follow-up periods for this specific fracture pattern is needed to provide definitive conclusions. Relevant anatomical or other studies should also be performed to obtain greater familiarity with this special fracture type.
Abbreviations
FNF = femoral neck fracture, PFNA = proximal femoral nail antirotation.
Acknowledgment
This research was supported by the Main Medical Scientific Research of Hebei (Award Number 20180451). We had no writing assistance.
Author contributions
Data curation: Zhiyong Hou, Weichong Dong.
Formal analysis: Weichong Dong.
Methodology: Ruipeng Zhang.
Project administration: Zhiyong Hou.
Resources: Jialiang Guo, Lin Jin.
Software: Yingzhao Yin.
Supervision: Yingze Zhang.
Validation: Zhiyong Hou.
Writing – original draft: Jialaing Guo.
Writing – review and editing: Yingze Zhang.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research was supported by the Main Medical Scientific Research of Hebei (Award Number 20180451) and the Science and Technology Program of the Department of Science and Technology of Hebei (Award Number 19277728D).
References
- 1.Broderick JM, Bruce-Brand R, Stanley E, et al. Osteoporotic hip fractures: the burden of fixation failure. Scientific World Journal 2013; 2013: 515197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilk R, Skrzypek M, Kowalska M, et al. Standardized incidence and trend of osteoporotic hip fracture in Polish women and men: a nine year observation. Maturitas 2014; 77: 59–63. [DOI] [PubMed] [Google Scholar]
- 3.Saarenpaa I, Partanen J, Jalovaara P. Basicervical fracture–a rare type of hip fracture. Arch Orthop Trauma Surg 2002; 122: 69–72. [DOI] [PubMed] [Google Scholar]
- 4.Chen CY, Chiu FY, Chen CM, et al. Surgical treatment of basicervical fractures of femur–a prospective evaluation of 269 patients. J Trauma 2008; 64: 427–429. [DOI] [PubMed] [Google Scholar]
- 5.Kuokkanen HO. Treatment options for basicervical fractures of the femoral neck. A clinical follow-up. Acta Orthop Belg 1991; 57: 162–168. [PubMed] [Google Scholar]
- 6.Blair B, Koval KJ, Kummer F, et al. Basicervical fractures of the proximal femur. A biomechanical study of 3 internal fixation techniques. Clin Orthop Relat Res 1994; 306: 256–263. [PubMed] [Google Scholar]
- 7.Watson ST, Schaller TM, Tanner SL, et al. Outcomes of low-energy basicervical proximal femoral fractures treated with cephalomedullary fixation. J Bone Joint Surg Am 2016; 98: 1097–1102. [DOI] [PubMed] [Google Scholar]
- 8.Quach S, Hennessy DA, Faris P, et al. A comparison between the APACHE II and Charlson Index Score for predicting hospital mortality in critically ill patients. BMC Health Serv Res 2009; 9: 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fogagnolo F, Kfuri M, Jr, Paccola CA. Intramedullary fixation of pertrochanteric hip fractures with the short AO-ASIF proximal femoral nail. Arch Orthop Trauma Surg 2004; 124: 31–37. [DOI] [PubMed] [Google Scholar]
- 10.Boraiah S, Paul O, Hammoud S, et al. Predictable healing of femoral neck fractures treated with intraoperative compression and length-stable implants. J Trauma 2010; 69: 142–147. [DOI] [PubMed] [Google Scholar]
- 11.Zlowodzki M, Jonsson A, Paulke R, et al. Shortening after femoral neck fracture fixation: is there a solution? Clin Orthop Relat Res 2007; 461: 213–218. [DOI] [PubMed] [Google Scholar]
- 12.Marchetti P, Binazzi R, Vaccari V, et al. Long-term results with cementless Fitek (or Fitmore) cups. J Arthroplasty 2005; 20: 730–737. [DOI] [PubMed] [Google Scholar]
- 13.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 1969; 51: 737–755. [PubMed] [Google Scholar]
- 14.Mallick A, Parker MJ. Basal fractures of the femoral neck: intra- or extra-capsular. Injury 2004; 35: 989–993. [DOI] [PubMed] [Google Scholar]
- 15.Kweon SH, Lee SH, Kook SH, et al. Outcomes of cephalomedullary nailing in basicervical fracture. Hip Pelvis 2017; 29: 270–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Imren Y, Gurkan V, Bilsel K, et al. Biomechanical comparison of dynamic hip screw, proximal femoral nail, cannulated screw, and monoaxial external fixation in the treatment of basicervical femoral neck fractures. Acta Chir Orthop Traumatol Cech 2015; 82: 140–144. [PubMed] [Google Scholar]
- 17.Hu SJ, Yu GR, Zhang SM. Surgical treatment of basicervical intertrochanteric fractures of the proximal femur with cephalomeduallary hip nails. Orthop Surg 2013; 5: 124–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Su BW, Heyworth BE, Protopsaltis TS, et al. Basicervical versus intertrochanteric fractures: an analysis of radiographic and functional outcomes. Orthopedics 2006; 29: 919–925. [DOI] [PubMed] [Google Scholar]
- 19.Bojan AJ, Beimel C, Taglang G, et al. Critical factors in cut-out complication after Gamma Nail treatment of proximal femoral fractures. BMC Musculoskelet Disord 2013; 14: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hou Z, Bowen TR, Irgit KS, et al. Treatment of pertrochanteric fractures (OTA 31-A1 and A2): long versus short cephalomedullary nailing. J Orthop Trauma 2013; 27: 318–324. [DOI] [PubMed] [Google Scholar]
- 21.Krigbaum H, Takemoto S, Kim HT, et al. Costs and complications of short versus long cephalomedullary nailing of OTA 31-A2 proximal femur fractures in U.S. veterans. J Orthop Trauma 2016; 30: 125–129. [DOI] [PubMed] [Google Scholar]
- 22.Lee YK, Yoon BH, Hwang JS, et al. Risk factors of fixation failure in basicervical femoral neck fracture: which device is optimal for fixation? Injury 2018; 49: 691–696. [DOI] [PubMed] [Google Scholar]