Short abstract
Objective
This study was performed to evaluate the clinical application value of carotid artery color Doppler ultrasonography and the plasma levels of lipoprotein-associated phospholipase A2 (Lp-PLA2) and cystatin C (Cys C) in the diagnosis and treatment of arteriosclerotic cerebral infarction.
Methods
Sixty patients with arteriosclerotic cerebral infarction and 60 matched healthy participants were included. The patients were divided into mild, moderate, and severe groups according to their National Institutes of Health Stroke Scale (NIHSS) scores. Carotid artery intima plaque formation and the intima–media thickness (IMT) were observed using carotid artery color Doppler ultrasonography. The correlation between IMT and the Lp-PLA2 or Cys C level was statistically analyzed.
Results
Patients with arteriosclerotic cerebral infarction had a higher detection rate of carotid plaques, especially unstable plaques, than healthy participants. The plasma levels of Lp-PLA2 and Cys C were elevated in patients with arteriosclerotic cerebral infarction and increased with the NIHSS scores. The plasma levels of Lp-PLA2 and Cys C in patients with arteriosclerotic cerebral infarction were correlated with IMT.
Conclusion
The combination of carotid artery color Doppler ultrasonography with the Lp-PLA2 and Cys C plasma levels is of great clinical value in the diagnosis and treatment of arteriosclerotic cerebral infarction.
Keywords: Carotid artery color Doppler ultrasonography, lipoprotein-associated phospholipase A2, cystatin C, arteriosclerotic cerebral infarction, intima–media thickness, National Institutes of Health Stroke Scale
Introduction
The common carotid artery is the main arterial trunk in the head and neck, and atherosclerotic lesions of the common carotid artery can cause arterial stenosis or rupture.1 If atherosclerotic plaques break off, they may cause thrombosis, leading to an insufficient blood supply to the brain and cerebral infarction.1 Carotid atherosclerosis reportedly plays an important role in the process of cerebral infarction.2 Vascular stenosis and intimal thickening reduce the blood supply from the carotid artery to the brain. When the body position changes, the blood volume is insufficient, or the blood pressure drops, cerebral infarction is likely to occur. Color Doppler ultrasonography is noninvasive, safe, high-quality, simple, quick, and reliable. The carotid artery is the main channel of the cerebral blood supply, and its position is shallow. When atheromatous lesions occur, color Doppler ultrasonography allows for clear observation of the vascular structure, plaque morphology, degree of vascular stenosis, and changes in hemodynamic parameters.3
Lipoprotein-associated phospholipase A2 (Lp-PLA2) is an inflammatory marker with certain vascular specificity and can be an independent risk factor for the pathological development of coronary heart disease.4 Lp-PLA2 is composed of 441 amino acids and is generally secreted by T lymphocytes, monocytes, and mast cells.5 Lp-PLA2 not only hydrolyzes the acetyl group of platelet activating factor but also hydrolyzes and oxidizes phospholipids in low-density lipoprotein molecules to produce two strong inflammatory factors, namely free fatty acids and lysophosphatidylcholine.6 Therefore, Lp-PLA2 is a risk factor for atherosclerotic plaque formation.
Cystatin C (Cys C) belongs to the serum cysteine protease inhibitor superfamily and has a relatively low molecular weight. Cys C can freely pass through the glomerular filtration membrane and is degraded in the epithelial cells of the proximal convoluted tubule. The Cys C level in blood will markedly increase when the glomeruli are only slightly injured. As the injury becomes more aggravated, the Cys C level will rise increasingly more rapidly.7 Therefore, it is generally believed that Cys C is a sensitive marker that reflects early renal injury.8 Renal injury is a common complication of acute cerebral infarction.9,10 In addition, the Cys C level is reportedly related to cerebral infarction.11
Cerebral infarction is one of the most common cerebrovascular diseases and leads to a variety of neurological impairment symptoms.12,13 The incidence, disability rate, recurrence rate, and mortality of cerebral infarction are high.14 Although various therapeutic drugs and treatments are available for cerebral infarction, effective prevention and accurate assessment of the condition are of great importance in reducing the incidence and improving the prognosis of the disease.15,16 As an inflammatory marker, Lp-PLA2 can be a novel independent predictive factor for ischemic stroke.17 In addition, Cys C participates in the pathological process of atherosclerosis.18 In the present study, we predicted and evaluated the progression of atherosclerotic cerebral infarction using carotid artery color Doppler ultrasonography and the two observation indices Lp-PLA2 and Cys C.
Materials and methods
Patients and controls
This study included patients with arteriosclerotic cerebral infarction who received treatments at our hospital from August 2016 to November 2017 and healthy participants (controls) who underwent physical examinations at our hospital. Sex, age, and body mass index (BMI) were not significantly different between the patients and the healthy participants. The inclusion criteria were meeting of the clinical diagnostic criteria for cerebral infarction,15 a diagnosis of anterior circulation infarction by imaging examination, a disease course of ≤3 days, and provision of written informed consent. The exclusion criteria were infection, malignant tumors, and immune system disease; serious heart, liver, and kidney diseases; intake of hormones, antibiotics, or antiplatelet drugs within 1 week; any other disease among participants in the control group; and cardiogenic cerebral embolism. According to the National Institutes of Health Stroke Scale (NIHSS), the patients were divided into three groups: the mild group (NIHSS score of <4 points), moderate group (NIHSS score of 4–15 points), and severe group (NIHSS score of >15 points).
Color Doppler ultrasonography of the carotid artery
Carotid artery color Doppler ultrasonography was performed using a Philips HD22 ultrasound machine (Philips, Amsterdam, The Netherlands). The patients were examined in the supine position with their neck fully exposed during the examination. The bilateral carotid arteries were examined using a 7.5- to 10-MHz probe frequency to observe the formation of intima plaques and measure the intima–media thickness (IMT). Plaque formation was diagnosed when the local IMT was >1.2 mm or >1.5 times the surrounding IMT.19 Stable plaques were hard and flat, while unstable plaques were soft, ulcerative, and mixed. The site selected for IMT quantitative measurement was 1.5 cm distal to the carotid artery bifurcation.
Luminescent immunoassay
Venous blood samples were collected the morning after an overnight fast. Luminescent immunoassay was performed to detect the plasma content of Lp-PLA2 using an upconverting phosphor technology-based luminescent immunoanalyzer and relevant kit (Hotgen Biotech, Beijing, China) according to the manufacturer’s manual.
Immunoturbidimetry
Venous blood samples were collected the morning after an overnight fast. The plasma level of Cys C was determined by immunoturbidimetry on an automatic biochemical analyzer (AU5400; Olympus, Tokyo, Japan) using a Cys C assay kit (Beijing Strong Biotechnologies, Inc., Beijing, China) according to the manufacturer’s manual.
Statistical analysis
The results were analyzed using SPSS 20.0 statistical software (IBM Corp., Armonk, NY, USA). The data are expressed as mean ± standard deviation. Data were tested for normality. Multigroup measurement data were analyzed using one-way analysis of variance. In case of homogeneity of variance, the least significant difference and Student–Newman–Keuls methods were used; in case of heterogeneity of variance, Tamhane’s T2 or Dunnett’s T3 method was used. Correlation analysis was performed using Kendall correlation analysis or Spearman correlation analysis. Comparison between two groups was carried out using Student’s t-test. Statistically significant differences were indicated by α = 0.05 and P < 0.05.
Ethical approval and consent to participate
All procedures performed in the current study were approved by the Ethics Committee of the First Hospital of Zibo. Written informed consent was obtained from all patients or their families.
Consent for publication
Written informed consent for publication of any associated data and accompanying images were obtained from all patients or their parents, guardians, or next-of-kin.
Results
Study groups
This study comprised 60 patients with arteriosclerotic cerebral infarction (25 men, 35 women; age range, 45.0–68.0 years; mean age, 57.2 ± 7.1 years; BMI range, 21.0–32.0 kg/m2; mean BMI, 25.9 ± 2.6 kg/m2) and 60 healthy participants (controls) (23 men, 37 women; age range, 43.0–66.0 years; mean age, 56.4 ± 6.7 years; BMI range, 20.0–31.0 kg/m2; mean BMI, 26.1 ± 3.4 kg/m2).
Patients with arteriosclerotic cerebral infarction had a higher detection rate of carotid plaques, especially unstable plaques, than healthy controls
Carotid artery color Doppler ultrasonography was performed to examine the size and shape of the carotid plaques and narrowing of the coronary arteries. Some patients had multiple mixed echoes, suggesting the existence of mixed plaques; some had inhomogeneous low echoes with irregular shapes, suggesting the existence of soft plaques; some had progressive strong echoes, suggesting the existence of hard plaques; and some had lower echoes on the edge and a hollow on the top of a wide base, suggesting the existence of ulcerative plaques. The detection rate of carotid artery plaques was significantly higher in patients than in controls (P < 0.05). In addition, the detection rate of unstable plaques was significantly higher in patients than in controls (P < 0.05) (Table 1). These results suggest that patients with arteriosclerotic cerebral infarction have a higher detection rate of carotid plaques, especially unstable plaques, than healthy subjects.
Table 1.
Numbers of patients with positive or negative detection of carotid plaques.
| Groups | Patients with positive detection of
plaques |
Patients with negative detection of plaques | |
|---|---|---|---|
| Patients with stable plaques | Patients with unstable plaques | ||
| Controls (n = 60) | 21 (35.00) | 13 (21.67) | 26 (43.33) |
| Patients (n = 60) | 12 (20.00) | 38 (63.33) | 10 (16.67) |
| χ 2 | 28.515 | 9.653 | |
| P | 0.000 | 0.004 | |
Data are presented as n (%).
Plasma levels of Lp-PLA2 and Cys C were elevated in patients with arteriosclerotic cerebral infarction and increased with the NIHSS scores
Luminescent immunoassay and immunoturbidimetry were performed to determine the plasma levels of Lp-PLA2 and Cys C, respectively. The data showed that the plasma levels of Lp-PLA2 and Cys C were significantly higher in patients with arteriosclerotic cerebral infarction than in controls (P < 0.05). In addition, the levels of Lp-PLA2 and Cys C increased with the elevation of the NIHSS scores (P < 0.05) (Table 2). These results indicate that the plasma levels of Lp-PLA2 and Cys C are elevated in patients with arteriosclerotic cerebral infarction and increase with the NIHSS scores.
Table 2.
Levels of Lp-PLA2 and Cys C in plasma according to NIHSS scores.
| Groups | NIHSS score | Lp-PLA2 (µg/L) | Cys C (mg/L) |
|---|---|---|---|
| Patients with arteriosclerotic cerebral infarction | <4 points | 196.11 ± 19.13 | 1.02 ± 0.65 |
| 5–15 points | 224.32 ± 17.09 | 1.18 ± 0.22 | |
| >15 points | 265.44 ± 27.11 | 2.15 ± 0.61 | |
| Control group | 168.21 ± 14.23 | 0.67 ± 0.11 | |
| t value | 0.573 | ||
| P value | 0.012 |
Data are presented as mean ± standard deviation. Lp-PLA2, lipoprotein-associated phospholipase A2; Cys C, cystatin C; NIHSS, National Institutes of Health Stroke Scale.
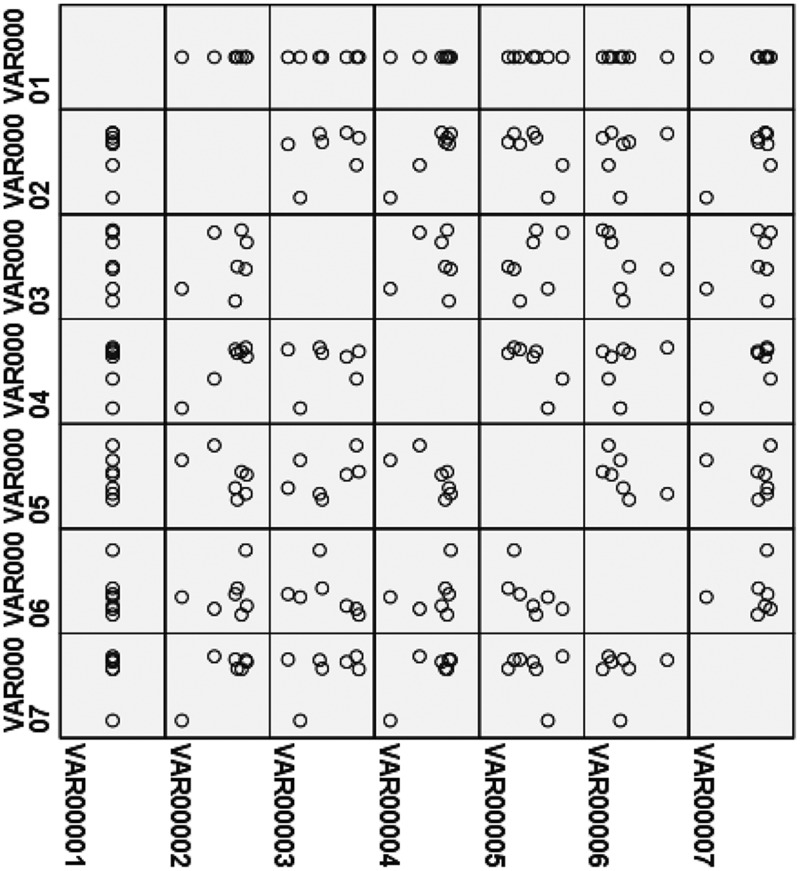
Plasma levels of Lp-PLA2 and Cys C in patients with arteriosclerotic cerebral infarction were correlated with IMT
Kendall correlation analysis or Spearman correlation analysis was performed to examine the correlation of the plasma levels of Lp-PLA2 and Cys C with IMT. The Kendall correlation factors between IMT in the control group (1.02 ± 0.41 mm) and the plasma LP-PLA2 or Cys C level in the control group were both 0.00, with no statistical significance; in addition, the Spearman correlation factors were −0.02 and −0.01, respectively, also without statistical significance. However, the Kendall correlation factor between IMT in the control group (1.62 ± 0.58 mm) and the plasma LP-PLA2 level was 0.917 (P < 0.01), and the Spearman correlation factor was 0.979 (P < 0.01). Moreover, the Kendall correlation factor between IMT in the control group (1.62 ± 0.58 mm) and plasma Cys C level was 0.873 (P < 0.01), and the Spearman correlation factor was 0.969 (P < 0.01) (Figure 1). These results suggest that the plasma levels of Lp-PLA2 and Cys C in patients with arteriosclerotic cerebral infarction are correlated with IMT.
Figure 1.
Correlation analysis of plasma levels of lipoprotein-associated phospholipase A2 and cystatin C with intima–media thickness. Kendall correlation analysis or Spearman correlation analysis was performed.
Discussion
Acute cerebral infarction is a type of cerebral ischemia and necrosis caused by cerebral thrombosis or embolism and is associated with high disability and death rates. The main causes of acute cerebral infarction are hypertension, diabetes, hyperlipidemia, and formation of carotid atherosclerotic plaques.20 An epidemiological study showed that cerebral infarction has become one of the most important diseases that lead to death in China, and the incidence of the disease is increasing each year with changes in lifestyles.21 Therefore, effective prevention and accurate assessment of cerebral infarction is of great importance in reducing its incidence and improving patients’ prognosis. Clinical observation shows that cerebral infarction caused by atherosclerosis accounts for about 35% of all cases of cerebral infarction, and atherosclerosis is believed to be the leading cause of cerebral infarction.22
Atherosclerosis can lead to the release of a large number of inflammatory factors such as Lp-PLA2, which in turn lead to the formation of atherosclerotic plaques. Arterial thrombosis caused by ruptured atherosclerotic plaques can obstruct intracranial arteries through the artery–artery pathway and lead to the occurrence of cerebral infarction. The present study showed that IMT and the Lp-PLA2 plasma level were higher in patients than in controls. The formation of vulnerable plaques of carotid atherosclerosis is significantly correlated with the development of ischemic stroke. Vulnerable plaques of carotid atherosclerosis are not only an early sign of atherosclerosis but also an important predictor of the occurrence of cerebral infarction.23
Cys C is composed of 150 amino acid residues and 5 disulfide bonds. The coding gene of Cys C can be continuously transcribed and expressed in all tissues.24 Cys C is widely distributed in plants, bacteria, viruses, protozoa, and mammalian tissues; its yield is constant and its expression is not tissue-specific.25 Cys C has the highest concentration in cerebrospinal fluid at about 2% to 4% (5.5 times higher than that in blood), and its concentration is lowest in urine.25 The physiological functions of Cys C include regulating the activity of cysteine protease, affecting the migration of neutrophils, participating in inflammatory reactions, inhibiting the activity of enzymes and hormone precursors, and participating in the production and degradation of the extracellular matrix and the dynamic balance of the proteases and antiproteases of the vascular wall.26 In the present study, cervical plaques were more unstable in patients than in controls. In addition, the plasma concentration of Cys C was significantly higher in patients than in controls. Therefore, Cys C is an independent risk factor for plaque instability in the neck, consistent with a previous study.27
In conclusion, the present study has demonstrated that the combination of carotid artery color Doppler ultrasonography with the plasma levels of Lp-PLA2 and Cys C is of great clinical application value in the diagnosis and treatment of arteriosclerotic cerebral infarction.
Acknowledgement
The authors wish to thank their department and research team for their help and dedication.
Author contributions
The final version of the manuscript has been read and approved by both authors, and each author believes that the manuscript represents honest work. LH and SY collaborated to design the study, perform the experiments, and analyze the data. Both authors collaborated to interpret the results and develop the manuscript.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Yang X, Zhu F. Clinical significance of carotid artery color Doppler ultrasound in detecting atherosclerotic plaques in elderly patients with cerebral infarction. China Prac Med 2009; 6: 69–70. [Google Scholar]
- 2.Ding S, Zhang Y, Zhang M. The stability of carotid plaque in the pathogenesis of acute ischemic stroke. Chin J Ultrasonogr 2006; 15: 597. [Google Scholar]
- 3.Sun DJ, Zhuang AX, Zeng QH, et al. A study of microemboli monitoring of atherosclerotic thrombotic cerebral infarction and artery stenosis. Genet Mol Res 2014; 13: 6734–6745. [DOI] [PubMed] [Google Scholar]
- 4.Li Y, Liang L, Zhang Z, et al. Changes of serum lipoprotein associated phospholipase A2 and high sensitivity C reactive protein in patients with coronary heart disease. Int J Lab Med 2016; 37: 2757–2759. [Google Scholar]
- 5.Sha X, Wang D, Qiao Y, et al. Relationship between level of serum lipoprotein associated phospholipase A2 and coronary atherosclerotic lesion. Jiangsu Medical Journal 2016; 42: 764–767. http://d.old.wanfangdata.com.cn/Periodical/jsyy201607007. [Google Scholar]
- 6.Yang L, Liu Y, Wang S, et al. Association between Lp-PLA2 and coronary heart disease in Chinese patients. J Int Med Res 2017; 45: 159–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang S, Yin A. Research progress about C-reactive protein and diabetic nephropathy. Medical Recapitulate 2008; 14: 432–434. http://med.wanfangdata.com.cn/Paper/Detail?id=PeriodicalPaper_yxzs200803048. [Google Scholar]
- 8.Chi X, Chen J, Yan D. Study on the diagnostic value of combinative measuring of serum cystatin C and urinary proteins in patients with early diabetic nephropathy. J Trop Med 2009; 9: 403–405. [Google Scholar]
- 9.Gu G, Bai Y. Determination of serum cysteine proteinase inhibitor C and its clinical application. Chin J Lab Med 2007; 30: 952–954. [Google Scholar]
- 10.Sun Y, Zeng Z, Jiang T, et al. Application of cystatin C in the evaluation of renal function. Chin J Nephr 2006; 22: 503–504. [Google Scholar]
- 11.Zhu G. Evaluation of the application of serum cystatin C in renal diseases. Int J Lab Med 2007; 28: 470–471. [Google Scholar]
- 12.Bao J, Chen S, Zhang B, et al. Dynamic changes of leukocytes and prognoses of patients with right and left middle cerebral artery infarction: a comparative study. Chine J Neuromedicine 2013; 12: 801–805. [Google Scholar]
- 13.Chen Y, Lei C, Liu M, et al. Association between clinical outcome and hemorrhagic transformation after acute cerebral infarction: a system review. Chin J Stroke 2015; 10: 827–834. [Google Scholar]
- 14.Jenkins PO, Turner MR, Jenkins PF. What is the place of thrombolysis in acute stroke. A review of the literature and a current perspective. Clin Med 2008; 8: 238–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cerebrovascular disease group, neurological branch of Chinese Medical Association. 2014 Level two prevention guide for ischemic stroke and transient ischemic attack in China 2014. Chin J Neurol 2015; 48: 258–273. [Google Scholar]
- 16.Xu P, Guo G, Gao Y, et al. Distribution features of stroke types of patients in Changde city. Chin J Neuromedicine 2013; 12: 707–710. [Google Scholar]
- 17.Oei HH, vail der Meer M, Hofman A, et al. Lipoprotein-associated phospholipase A2 activity is associated risk of coronary heart disease and ischemic stroke: the Rotterdam Study. Circulation 2005; 111: 570–575. [DOI] [PubMed] [Google Scholar]
- 18.Kyhse-Andersen J, Schmidt C, Nordin G, et al. Serum cystatin C, determined by a rapid, automated particle-enhanced turbidimetric method, is a better marker than serum creatinine for glomerular filtration rate. Clin Chem 1994; 40: 1921–1926. [PubMed] [Google Scholar]
- 19.Zhang D, Li X. Relationship between the plasma homocysteine, high-sensitive-reactive protein and carotid artery stenosis in acute cerebral infarction. J Tianjin Medical University 2012; 18: 221–229. [Google Scholar]
- 20.Eriksson P, Deguchi H, Samnegard A, et al. Human evidence that the cystatin C gene is implicated in focal progression of coronary artery disease. Arterioscler Thromb Vasc Biol 2004; 54: 551–557. [DOI] [PubMed] [Google Scholar]
- 21.Liu G, Wang S, Liang C, et al. Epidemiological characteristics and prognosis of acute cerebral infarction in primary hospitals. Youjiang Med J 2013; 41: 555–556. [Google Scholar]
- 22.Han X, Zhao X, Liu D, et al. Correlation between intracranial and extracranial symptomatic carotid atherosclerotic plaques. Chin J Geriatr Heart Brain Vessel Dis 2014; 16: 181–184. [Google Scholar]
- 23.Zheng J, Wu W, Han Z, et al. Risk factors and intervention schemes of stroke in the elderly in Zhongshan, China. Academic Journal of Guangzhou Medical College 2014; 42: 27–29. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=gzyxyxb201402012. [Google Scholar]
- 24.Vilhjalmsson DT, Blondal H, Thormodsson FR. Solubilized cystatin C amyloid is cytotoxic to cultured human cerebrovascular smooth muscle cells. Exp Mol Pathol 2007; 83: 357–360. [DOI] [PubMed] [Google Scholar]
- 25.Newman DJ, Thakkar H, Edwards RG, et al. Serum cystatin C measured by automated immunoassay: a more sensitive marker of changes in GFR than serum creatinine . Kidney Int 1995; 47: 315. [DOI] [PubMed] [Google Scholar]
- 26.Wang F, Chu Z. Research progress of correlation between cystatin C and ischemic cerebrovascular disease. Stroke and Nervous Diseases 2010; 17: 309–311. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zzysjjb201005018. [Google Scholar]
- 27.Wang J, Liu Q, Liu B, et al. Changes of serum cystatin C and homocysteine levels in patients with acute myocardial infarction. Chinese Journal of Gerontology 2013; 33: 1626–1627. http://med.wanfangdata.com.cn/Paper/Detail?id=PeriodicalPaper_zglnxzz201307061. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.