Abstract
Background:
In-patient (IP) suicides contribute a small but significant proportion of overall suicides. Despite this, suicide prevention strategies focusing on the general hospital IP population remain relatively underresearched. This paper is intended to provide an overview of various proposed suicide prevention approaches in the general hospital, including psychiatric IP, settings, and their evidence base.
Methodology:
Electronic searches of MEDLINE through PubMed, ScienceDirect, and Google Scholar databases were performed to identify potentially relevant articles from inception till January 2019. The generated abstracts were systematically screened for their eligibility to be included in the review. Included articles were grouped under five broad themes: environmental modification, staff education, pharmacotherapy, psychotherapy, and brain stimulation. Data extraction was done using a structured proforma.
Results:
Environmental modifications and educating the health care professionals appear to be the most promising strategies to reduce suicide-related mortality among IPs. Among pharmacological methods, ketamine has shown initial promise in reducing suicidal ideations. Follow-up data are lacking for most of the described methods. Limited but positive evidence exists for cognitive therapies focusing on the immediate postadmission period and brain stimulation techniques, and it warrants further replication.
Conclusion:
There is a striking paucity of original research on IP suicide prevention. Given the ethical and methodological issues in carrying out studies with IP suicide as the primary outcome, there is a need to focus on intermediate suicide outcome measures, such as knowledge, attitude, and skills among staff handlers of suicidal patients.
Key words: In-patient suicide, psychiatry, review, suicide, suicide prevention
Suicide in the in-patient (IP) setting is considered as a “sentinel event,” an event though not a fallout of the natural course of the illness but nevertheless causes harm to the patient.[1] It is often considered to be preventable and is associated with serious outcomes. Oehmichen and Staak defined IP suicide in a psychiatric setting as “suicide of a patient during IP treatment, both inside and outside the hospital setting, e.g. during a leave, an outing, a trial discharge, or a stay in another hospital with concurrent IP psychiatric treatment.”2 Large-scale data about IP suicides are mainly from western countries. Hanging is the most common method of IP suicide.[3,4] However, in a study from the West, jumping from altitude was the most common method.[1]
National Violent Death Reporting System and Joint Commission's Sentinel Event records that out of suicides over a period of 1 year (2004–2005), 75% happened during psychiatric IP treatment, and 48.5–64.9 IP suicides occurred annually. A 10-year retrospective chart review from forensic medicine records noted that nearly three-quarters of IP suicides within the hospital were carried out by incomplete hanging and the other common means were jumping from altitude and poisoning.[5]
IP suicides comprised 2.5% of all suicides in the United Kingdom (UK), and the incidence was found to be about 1.24/1000 IP discharges.[6] In Finland, the incidence of IP suicides was found to be about 3 per 1000 admissions over an 11-year period as per a retrospective chart review carried out at a general hospital psychiatric IP setting.[7] These data are comparable to older data on incidence rates from Europe.[8] In Taiwan, the standardized IP suicide mortality ratio was found to be 8.25, which was higher compared to the rates for the general population.[9]
Several factors have been found to be closely related to IP suicide. Among Taiwanese IPs, younger females and older males had a higher risk of suicide attempts and suicide-related mortality, respectively.[10,11] History of suicide attempt/deliberate self-harm, family history of suicide, mood disorder, schizophrenia, ideas of hopelessness, guilt, and current suicidal ideation have been identified as risk factors for IP suicides.[12] A qualitative study noted that having a psychiatric illness, perceived serious illness, incurring high medical expenses, poor social support, and unsafe IP environment were the themes associated with a high risk of suicide.[13]
The risk of suicide was found to be the highest immediately following admission as well as immediately after discharge. It was found to be inversely related to the length of stay. IP suicides outside the hospital were commonly found to occur during a leave of absence or transfer to another hospital.[8] Further, IP suicides have been found to be secondary to inadequate staffing/resources as well as an increased number of patients with severe mental illnesses.[14]
Given the evidence, the period of IP care is clearly associated with a high risk of suicide. Consequently, suicide prevention among IPs assumes significance both from an individual as well as public health standpoints. Thereby, it is necessary to synthesize evidence base for interventions aimed at preventing IP suicides to guide clinicians and researchers alike. With this background, this narrative review attempts to provide a comprehensive overview of major methods of suicide prevention among general hospital IP population.
METHODOLOGY
Search Strategy and study selection
Electronic searches of MEDLINE through PubMed, Google scholar, and ScienceDirect databases were carried out from inception till January 2019. Search terms included combinations of following medical subject headings or free text terms: “suicide prevention,” “IP suicide,” “nursing staff,” “education,” “intervention,” “cognitive therapy,” “environment,” “prevention,” “risk reduction,” “psychotropic medication,” “pharmacological,” and “psychosocial intervention”. Since there was no definition available for IP suicide in the medical/surgical setting, IP suicide in this review has been defined as “suicide of a patient during IP treatment occurring in a psychiatric or medical/surgical setting” based on the definition by Oehmichen and Staak.[2] Inclusion criteria were articles published in peer-reviewed English language journals.
The search was carried out independently by two authors. The final articles to be included in the review were decided by discussion and consensus among the authors.
The initial search yielded 880 articles. Further, the references in these articles and abstracts were screened manually to identify potentially relevant articles. Conference proceedings were not included in the review. The study selection is depicted in Figure 1.
Figure 1.
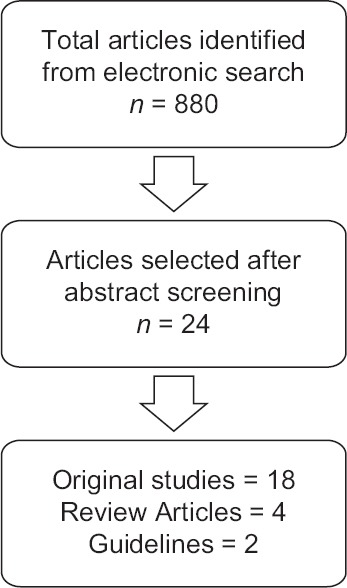
Study selection process
Data extraction
Upon literature search, we observed that the existing literature could be categorized into the following five broad categories: environmental modification, staff education, pharmacological interventions, psychological interventions, and brain stimulation. Hence, the results are being presented under these headings. In the case of original articles, data extraction was done using a structured proforma and included details of the name of the author, year of publication, type of intervention, and chief outcome [Table 1].
Table 1.
Summary of presented studies
| Author | Sample/study characteristics | Intervention | Chief findings |
|---|---|---|---|
| Environmental modification | |||
| Watts et al. (2012)[16] | IPs at VA hospital | Implementation of MHEOCC in 2007 | Reduction in suicide rates from 2.64/100 000 IP mental health admissions before 2007 to 0.87/100 000 admissions during implementation period (2008-2011) |
| Watts et al. (2017)[17] | IPs at VA hospital | Implementation of MHEOCC during 2007-2010 | Suicide rate decreased from 4.2/100,000 admissions prior to implementation to 0.74/100,000 admissions in continuation period 2011-2015 |
| Mohl et al. (2012)[18] | General hospital in a high-rise building | Installing metal rails to prevent jumps | Reduction in jumps from 10/119,269 patients in 114 months prior to installation to 2/104,435 during the 78 months following installation |
| Staff education | |||
| van Landschoot et al. (2017)[29] | 1171 staff in emergency and psychiatry department | Poster campaign offering information on identifying and responding to high risk patients was displayed for four weeks | No significant change in attitude was noted at four weeks compared to baselineHigher knowledge scores at baseline was considered as the possible reason |
| Manister et al. (2017)[25] | 577 nursing staffs | One-hour class on IP suicide prevention which was repeated 40 times | Significant improvement in knowledge and confidence in handling IP suicidal behaviour was found four weeks after the class |
| Inga-Lill Ramberg et al. (2016)[23] | 500 mental health staff: Psychiatrists, doctors under training, nursing staff, contact persons, psychologists, physical therapist, occupational therapist | Mandatory suicide prevention training activities | Significant improvement was noted in attitudes towards prevention of suicide and clarity and confidence regarding the role of participants in suicidal IPs |
| Gask et al. (2006)[27] | 458 community mental health workers, IP mental health staffs, crisis service staffs | STORM | Positive changes in attitudes and confidence was noted but previous evidence of skill acquisition was not replicated immediately after and 4-month post training compared to baseline |
| Appleby et al. (2000)[26] | 359 health personnel belonging to primary care, accident and emergency departments and mental health services | STORM | Feasibility of conducting such an intervention was demonstrated.After six months of intervention, significant improvement in terms of skills pertinent to assessment and management of suicide risk was noted.It was projected that the intervention could be cost effective by reducing suicide rate by 2-5% and preventing ≤99,747 per suicide and gain of ≤3391 per life year |
| Morris et al. (1999)[28] | 33 Non-psychiatrically trained staff (health and voluntary workers) | Eight hours of interview skills training | Confidence and skills for problem solving, future coping, and provision of immediate support improved significantly at one month after training. |
| Pharmacological intervention | |||
| Modestin et al. (2005)[43] | Chart review of 94 IP records | Clozapine for at least six weeks | Rate of suicidal behaviour reduced from 28% in pre-clozapine period to 3% during clozapine period and 18% in post-clozapine period |
| Ballard et al. (2015)[44] | 133 IPs were assessed at 60 min before and at 40,80,120,230 min and 1, 2 and 3 days after infusion | Single subanesthetic dose of ketamine was administered intravenously over 40 min. | Ketamine infusion was associated with significant reductions in suicidal ideation compared to placebo, when controlling for the effects of ketamine on depression |
| Psychological Intervention | |||
| Ghahramanlou-Holloway et al. (2018)[46] | 24 IPs admitted with recent suicidal crisis. Randomized to PACT + EUC or EUC alone, 12 in each group | PACT - Six sessions lasting 60-90 min over the course of 3 days | Significant reduction in depression, hopelessness and suicide ideation noted in patients receiving PACT compared to control group |
| LaCroix et al. (2018)[47] | 36 IPs admitted following a recent suicidal attempt due to trauma-related diagnoses. Randomized to PACT + EUC or EUC alone | PACT - Six sessions lasting 60-90 min | Clinically significant change in depression and hopelessness was noted, but not for suicidal ideation. |
| Ellis et al. (2015)[52] | 52 IPs from a psychiatric hospital who reported some form of suicidality within weeks of admission.Study groups were CAMS-based therapy vs TAU.Nonrandomized comparison study | CAMS based individual therapy | Significant reduction in suicidal ideation and cognition as measured prior to discharge compared to baseline, typical IP stay in the setting being 4-8 weeks |
| Brain stimulation | |||
| George et al. (2014)[53] | 42 IPs, with suicidal ideations being the reason for IP care.Randomized to each group, 20 in rTMS and 21 in sham group. | High dose left prefrontal rTMS for 30 min three times for 3 days | Significant improvement in suicidal ideations was noted over 3 days. |
| Patel et al. (2006)[52] | Records of 30 mentally ill IP who were treated with ECT, were examined | ECT with bilateral frontotemporal electrode placement; 5-10 sessions at a frequency of three per week | Significant improvement was noted in suicide and depression scale items of Brief Psychiatric rating Scale-24 |
| Kellner et al. (2005)[54] | 131 patients expressing suicidal intent | ECT with bitemporal electrode placement | Suicidal intent scores on the item 3 of Hamilton Depression Scale 24 item, decreased from 3-4 to 0 in 80.9% of patients by the end of three weeks (nine ECT sessions) |
| Sharma (1999)[55] | 45 IP records were examined for the use of ECT | Both unilateral and bilateral ECTs were given | Failed to demonstrate that ECT had prevented IP suicide |
VA – United States Department of Veterans Affairs; MHEOCC – Mental Health Environment of Care Checklist; STORM – Skills Training on Risk Management; PACT – Post Admission Cognitive Therapy; CAMS – Collaborative and Management of Suicidality; TAU – Treatment as Usual; EUC – Enhanced Usual Care; IP-In-patient; USA – United States of America; UK -United Kingdom
RESULTS
A total of 24 articles were obtained, out of which 18 were original studies conducted in an IP setting. There were four reviews and two guideline/recommendation documents. The preventive measures are elaborated below.
Environmental modification
Often, risk factors associated with the physical environment are neglected because these do not usually find a place in the routine medical education curriculum.[15] Measures of environmental modification can be categorized into two groups - (i) environment-specific and (ii) patient-specific precautions.
Environment-specific precautions
A few studies have demonstrated positive outcomes following environmental modification strategies in the hospital setting [Table 1]. In 2007, the Department of Veteran Affairs, USA developed a checklist termed Mental Health Environment of Care Checklist (MHEOCC). This checklist was developed by a multidisciplinary team of mental health care professionals, engineers, and architects. The final checklist contained 114 items after a comprehensive review by the team. Main components included environmental modifications in the psychiatric intervention rooms and hospital restrooms, such as minimizing fixtures, avoiding ligature points, and reducing breakable and pointed objects. The detailed description and other guidelines regarding the MHEOCC are provided at www.patientsafety.va.gov/professionals/onthejob/mentalhealth.asp. Following its implementation in veteran hospitals, sustained reductions in suicide rates were noted.[16,17] One study reported that installing a metal rail in the windows significantly reduced the rate of a jump.[18]
Patient-specific precautions
No original studies have systematically evaluated the effect of patient-specific precautions on suicidal behaviors. However, patient-specific precautions recommended include routine room searches, planned observations or supervisions, and supervised medication administration. Methods of supervision described ranged from continuous one-to-one supervision to supervising every 15–30 min as well as restricting the movement of patients.[19] Hospital staff such as nursing and housekeeping personnel need to be trained to ensure the safety of cleaning fluids, medicine carts, etc. Further, visitors must be screened for potentially lethal objects such as ropes and bags.[15]
Four levels of supervision, matched to the level of risk, have been described in the literature. Level 1 refers to general observation, wherein the patient's location must be known to the nursing staff at all times. Level 2 refers to intermittent observation. Here, the patient must be checked every 15 min. Level 3 is defined as within eyesight. Level 4 is for those at the highest risk of self-harm, and nursing staff is supposed to be available at “arm's length.”[20,21] However, there is no literature available on the outcomes associated with each of these methods of supervision in the hospital setting.
Staff education
Relationship between the hospital staff and patient is one of the modifiable links which might promote patient wellbeing. Studies have highlighted the inadequacy of and the need to improve skills in handling suicidal patients.[22] Lack of skills in caring for suicidal patients, a negative attitude of the staff, and low staffing are some of the staff-related barriers to suicide prevention.[23,24] Educating the hospital nursing staff can help in preventing IP suicides by increasing their knowledge, attitude, and confidence levels in handling suicidal patients.[23,25]
Several reports on staff education programs for IP suicides are available.[23,25,26,27,28,29] Components of the education programs included classes on IP suicide prevention, training activities for mental health staffs, poster campaign on IP suicide prevention, and skills training as a part of the Skills Training on Risk Management (STORM) project. The STORM training package included modules on assessment, crisis management, problem-solving, and crisis intervention.[27] Except for one Belgian study,[29] all other available studies reported positive change in attitude and knowledge. However, there have been no studies assessing the effect of staff education programs on the rate of IP suicides.
Negative change in the attitude toward prevention of suicide can happen in staff following an in-hospital suicide. This can lead to disruption in coping and distress. Appropriate assistance should be offered to such personnel in order to regain their confidence.[30,31]
Pharmacotherapy
Positive evidence exists for antipsychotics, lithium, antidepressants, and ketamine in reducing general suicidal behavior. Antipsychotics such as olanzapine and risperidone and antidepressants have shown efficacy for a reduction in suicidal behavior.[32,33,34] Of these agents, the highest amount of evidence exists for clozapine and lithium.[35,36,37,38,39,40,41,42] However, there are only two studies, one each on clozapine and ketamine, demonstrating their efficacy in reducing suicidal ideation/behavior in the IP setting[43,44] Table 1.
Psychotherapies
Interventions such as cognitive behavior therapy (CBT) and collaborative assessment and management of suicidality (CAMS) have been reported to reduce IP suicides [Table 1].
-
CBT for suicidal patients:
The efficacy of CBT in reducing suicidal ideation as well as suicidal behavior in adults and adolescents is well demonstrated.[45,46] With respect to cognitive and behavioral therapies for IP suicides, very few trials could be identified. Postadmission cognitive therapy (PACT) is a model of CBT designed for adults hospitalized following a recent self-harm or suicidal attempt.[47] It consists of six sessions divided into three phases. The first phase focuses on building up a therapeutic alliance, delivering psychoeducation, and framing a cognitive conceptualization of the suicide attempt. The second phase deals with improving coping strategies and problem-solving skills and instilling hope. The third phase comprises relapse prevention and developing a safety plan. We identified two trials that evaluated PACT for the prevention of suicidal behavior in the postadmission acute phase.[48,49] Both the trials reported significant reductions in depression, hopelessness, and posttraumatic stress disorder scores. But, only one of them reported a significant reduction in suicidal ideas.[48] Though this intervention appears promising, it clearly requires further replication
The CAMS is a therapeutic framework that involves active collaboration between the patient and the therapist, using a problem-focused suicide-specific approach.[50] It uses a multipurpose assessment, treatment planning, tracking, and outcome tool called the Suicide Status Form (SSF). SSF assess five central suicide markers, such as psychological pain, stress, agitation, hopelessness, and self-hate.[51] Studies using the CAMS framework among suicidal IPs show significant improvement in suicidal ideation and cognition when compared to treatment as usual group.[52]
Brain stimulation
Repetitive transcranial magnetic stimulation (rTMS) is an emerging biological therapy with growing evidence in reduction of suicidal behavior in IP setting.
A randomized controlled trial showed a rapid decline in suicidal ideation scores following administration of rTMS for 3 days, among IPs admitted due to suicidal ideation or attempt.[53] However, this study was primarily conducted to evaluate the feasibility and safety of rTMS in patients with acute suicidal risk, and therefore, these efficacy results must be considered as preliminary. Adequately powered studies are required to confirm the efficacy of rTMS in mitigating IP suicide risk.
Two retrospective studies and one secondary analysis of a multisite study have assessed the efficacy of electroconvulsive therapy (ECT) on expressed suicidal intent. One of the two retrospective studies[54] on ECT showed improvement in the expressed suicidal intent, whereas the other study did not report any positive findings.[55] Another study, which was a part of consortium for research in ECT project, showed a significant reduction in expressed suicidal intent in a depressed patient by the end of nine ECT sessions over a period of 3 weeks.[56] Both the positive studies did not use specific instruments for suicidal intent but instead analyzed items relevant to suicide intent from other scales.
DISCUSSION
Among various strategies for prevention of IP suicides, it is evident that there is a greater focus on staff education. However, a key challenge with the existing literature is that few papers have studied “direct” markers of suicide prevention, such as a decrease in suicidal behaviors.
Staff education
Staff education measures have included components of psychoeducation and crisis intervention.[25,26,27] Though the majority of the studies have demonstrated improvement in knowledge, attitude, and confidence of the health professionals after the intervention, there are several issues to be considered. Improvement in attitude and knowledge might not directly translate into an acquisition of skills. Changes in the benefits to users (decrease of suicidal behavior), type of organizational practice, and the behavior of the participants, which are among the highest levels of the outcome of training, have not been assessed. Another challenge is the sustainability and long-term effects of the intervention and lack of support and coordination from the organization, which might limit the translation of the effects of the intervention in clinical practice.[57] Demonstrating the cost-effectiveness of the intervention could also pave the way for better implementation at the organizational level. However, only one study has reported the projective estimates of implementation of suicide prevention education program.[26] Hence, there is a pressing need for more cost-effectiveness studies, apart from providing hard statistics of a decrease in subsequent suicidal behavior. It is also important to interpret the study findings considering the methodological caveats, such as the effect of prior experience with suicidal patients on staff attitude and unaddressed attrition of participants. Further, in some of the studies, the components of “suicide prevention training” provided to staff were not elaborated.[23] There have been no studies on staff education exclusively from the IP setting. There is a need for qualitative studies to assess the perspective of patients as well as health personnel on barriers for formulating effective staff education programs.
Environmental precautions
As of now, the environmental precautions are guided by recommendations from the Western world given for community as well as hospitals alike. There are three studies on environmental modification, especially on environment-specific precautions, which have demonstrated decreased suicidal behaviors. Given the argument that the physical barrier could have merely encouraged the patients to postpone their suicidal plans until discharge, doubts exist about the durability of these approaches on suicide prevention. Notably, there have been no studies reporting cost-effectiveness of such interventions. It is important to note that the recommendations given for environmental modifications in various reviews are not based on original studies conducted in a hospital setting and are rather extrapolated from preventive measures recommended in the community setting.
Patient-related precautions
There have been no original studies on patient-related precautions such as supervision. This is closely associated with issues such as poor staffing as well as sociocultural and ethical issues involved in managing the patient in the least restrictive setting. With regard to observation/supervision, the most important, and often neglected, part is observation with due respect, freedom, and privacy to the patient, which improves patient self-confidence and the overall therapeutic relationship.[58] Apart from focusing on safety from a psychiatrist's point of view, patient's perspectives on suicide prevention also merit an equal place to design strategies with optimal efficacy and uptake. It has been found that three components - connection (comprising of meeting a caring person, being reassured, and feeling acknowledged as a fellow human), protection (being offered protection and support), and control (developing insight, being ready for discharge, and better ways of coping with the symptoms) were vital, considering the patients' experience of safety in IP setting.[59]
Pharmacotherapy, psychotherapy, and others
Majority of the studies that showed evidence for the efficacy of clozapine and lithium have been conducted in the outpatient setting and the benefits accrued over a period of months to years.[60] Hence, the evidence for acute antisuicidal effects of these agents is not clear.
In this regard, ketamine seems to be a promising agent. Ketamine has been shown to have a rapid antidepressant effect in cases of unipolar as well as bipolar depression in numerous randomized controlled studies.[61,62,63] Meta-analyses demonstrate the rapid effect of intravenous ketamine in reducing suicidal ideation.[1,64] However, the quality of the evidence was found to be very low.
Though there is only a single study reporting the efficacy of ketamine on suicidal ideation in an IP setting, there are six studies including both outpatients and IPs that demonstrated a positive effect of ketamine on suicidal ideation. The onset of action of ketamine was found to occur within 24 h and to last up to about 1 week to 10 days in studies conducted on patients from both outpatient and IP settings.[65,66,67] Crucially, there is a paucity of literature on the long-term effects of ketamine on suicidality on both IP and outpatient populations.
The effect of ketamine on suicidal ideation is purported to be independent of the antidepressant action. There are few studies which have assessed the acute antidepressant role of ketamine in IP setting.[68] However, the effect on suicidal ideation was not reported. Hence, there is a need for studies reporting on antisuicidal effects independent of antidepressant action. Overall, there is a lack of clarity on the extent to which the antisuicidal role of ketamine extends beyond its acute effect on decreasing suicidal ideation. Further, the use of ketamine is compounded by drug-specific issues, such as abuse potential, need for repetitive dosing, and durability of action. Clearly, there is a need for more long-term studies to confirm the efficacy and sustainability of ketamine on outcomes of interest.
The role of psychological interventions is also emerging. CBT and dialectical behavioral therapy are among the most researched psychotherapies for reduction of suicidal cognition or behavior.[69,70] There are limited studies conducted in the IP setting in comparison to the vast evidence base of CBT in suicide prevention among outpatients.[71,72] Certain methodological issues are present in the existing studies, such as the differing nature of comparator, not assessing suicidal ideation directly as well as feasibility issues in delivering the intervention at the organizational level.
There is a need for more studies to delineate the role of rTMS in preventing suicidal behavior. ECT is another intervention which has been recommended for a reduction of suicide risk.[73,74] Despite an acute reduction of suicidal intent in ECT-treated IPs,[54,56] these findings are limited by methodological shortcomings, such as retrospective and quasi-experimental designs, failure to use specific scales for relevant suicide constructs, and problems of statistical power with secondary analysis. Further, the stigma associated with ECT and current practice of reserving ECT for the treatment-resistant patients and as a last resort prevent it from being considered as an early treatment option for suicide risk.[75,76]
At whom should be these preventive measures directed?
This is the next logical question and becomes especially pertinent in low-resource settings. Ideally, the preventive measures must be directed to all patients with a high risk of suicide such as those with a history of suicide attempts, recent psychosocial stressors, family history of suicide, psychosis (particularly commanding type of auditory hallucinations) or a mood disorder, and concurrent active suicidal ideation. The most important question would be to enquire about current suicidal ideation.[77] A number of easy to use questionnaires are available for screening patients with high suicide risk.[78] It is important that preventive efforts must start right at the first contact. To achieve this, all medical as well as paramedical personnel must be sensitized toward effective triage, timely referral, and liaison with mental health professionals.
Unaddressed challenges and future directions
There are many unaddressed issues related to IP suicide which needs to be addressed. One of them is the role of psychoeducation of patients and caregivers in IP suicides. Though from anecdotal evidence we know that psychoeducation plays a vital role, further studies are needed to strengthen the evidence of psychoeducation in the prevention of IP suicide. Another crucial factor is the illness-specific factors leading to IP suicide. There is no research on specific strategies for suicide prevention customized for each psychiatric illness. However, lithium and clozapine were reported to decrease suicides among patients with mood disorders and schizophrenia, respectively. Apart from these factors, there is a tremendous need for developing consultation liaison psychiatry services, especially in medical–surgical IP settings for management as well as sensitizing and training of health personnel. In addition, the administration should play an active role in encouraging multidisciplinary liaison across the departments for timely intervention.
When it comes to designing studies on IP suicide prevention, having suicide as a primary outcome becomes a key component but may involve ethical issues. Risk of suicide in the “placebo arm” or the unknown risks with the newly designed intervention are some key ethical considerations. Hence, studies on intermediate outcome measures, such as knowledge, attitude, and skills in handling suicidal patients and psychometric properties of instruments measuring them should be encouraged and focused upon. Evidence from such studies may help us to design and implement more effective strategies to counter IP suicides.
CONCLUSION
Maximum evidence exists for environmental modifications and staff education approaches with regard to IP suicide prevention. There is limited original literature on the role of various suicide prevention strategies in decreasing IP suicidal behaviors. Rather than relying on evidence extrapolated from the community- or outpatient-based studies, there is a need for more studies, with rigorous methodology, from IP settings. Further emphasis must be laid on developing sustainable and cost-effective yet ethical and socioculturally acceptable preventive strategies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Williams SC, Schmaltz SP, Castro GM, Baker DW. Incidence and method of suicide in hospitals in the United States. Jt Comm J Qual Patient Saf. 2018;44:643–50. doi: 10.1016/j.jcjq.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 2.Oehmichen M, Staak M. Suicide in the psychiatric hospital. International trends and medico legal aspects. Acta Med Leg Soc (Liege) 1988;38:215–23. [PubMed] [Google Scholar]
- 3.Hunt IM, Windfuhr K, Shaw J, Appleby L, Kapur N. National Confidential Inquiry into Suicide and Homicide. Ligature points and ligature types used by psychiatric inpatients who die by hanging: A national study. Crisis. 2012;33:87–94. doi: 10.1027/0227-5910/a000117. [DOI] [PubMed] [Google Scholar]
- 4.Ikeshita K, Shimoda S, Norimoto K, Arita K, Shimamoto T, Murata K, et al. Profiling psychiatric inpatient suicide attempts in Japan. Int J Emerg Ment Health. 2014;16:217–21. doi: 10.4172/1522-4821.1000107. [DOI] [PubMed] [Google Scholar]
- 5.Ruff F, Hemmer A, Bartsch C, Glasow N, Reisch T. [Suicides of Psychiatric Inpatients-A Systematic Recording in Switzerland of the Years 2000 to 2010] Psychiatr Prax. 2018;45:307–13. doi: 10.1055/s-0043-120888. [DOI] [PubMed] [Google Scholar]
- 6.Sakinofsky I. Preventing suicide among inpatients. Can J Psychiatry Rev Can Psychiatr. 2014;59:131–40. doi: 10.1177/070674371405900304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Suominen K, Isometsä E, Heilä H, Lönnqvist J, Henriksson M. General hospital suicides--A psychological autopsy study in Finland. Gen Hosp Psychiatry. 2002;24:412–6. doi: 10.1016/s0163-8343(02)00222-0. [DOI] [PubMed] [Google Scholar]
- 8.Taiminen TJ, Strandberg J, Kujari H. Inpatient suicide on a general hospital psychiatric ward: Does experience with high risk patients help to prevent suicides? Arch Suicide Res. 1996;2:119–24. [Google Scholar]
- 9.Tseng M-CM, Cheng I-C, Hu F-C. Standardized mortality ratio of inpatient suicide in a general hospital. J Formos Med Assoc. 2011;110:267–9. doi: 10.1016/S0929-6646(11)60040-5. [DOI] [PubMed] [Google Scholar]
- 10.Chen Y-L, Tzeng D-S, Cheng T-S, Lin C-H. Sentinel events and predictors of suicide among inpatients at psychiatric hospitals. Ann Gen Psychiatry. 2012;11:4. doi: 10.1186/1744-859X-11-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheng I-C, Hu F-C, Tseng M-CM. Inpatient suicide in a general hospital. Gen Hosp Psychiatry. 2009;31:110–5. doi: 10.1016/j.genhosppsych.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 12.Large M, Smith G, Sharma S, Nielssen O, Singh SP. Systematic review and meta-analysis of the clinical factors associated with the suicide of psychiatric in-patients. Acta Psychiatr Scand. 2011;124:18–9. doi: 10.1111/j.1600-0447.2010.01672.x. [DOI] [PubMed] [Google Scholar]
- 13.Huang D, Hu DY, Han YH, Lu CH, Liu YL. Five high-risk factors for inpatient suicide. Chin Nurs Res. 2014;1:14–6. [Google Scholar]
- 14.Bassett D, Tsourtos G. Inpatient suicide in a general hospital psychiatric unit. A consequence of inadequate resources? Gen Hosp Psychiatry. 1993;15:301–6. doi: 10.1016/0163-8343(93)90022-g. [DOI] [PubMed] [Google Scholar]
- 15.Lieberman DZ, Resnik HLP, Holder-Perkins V. Environmental risk factors in hospital suicide. Suicide Life Threat Behav. 2004;34:448–53. doi: 10.1521/suli.34.4.448.53740. [DOI] [PubMed] [Google Scholar]
- 16.Watts BV, Young-Xu Y, Mills PD, DeRosier JM, Kemp J, Shiner B, et al. Examination of the effectiveness of the mental health environment of care checklist in reducing suicide on inpatient mental health units. Arch Gen Psychiatry. 2012;69:588–92. doi: 10.1001/archgenpsychiatry.2011.1514. [DOI] [PubMed] [Google Scholar]
- 17.Watts BV, Shiner B, Young-Xu Y, Mills PD. Sustained effectiveness of the mental health environment of care checklist to decrease inpatient suicide. Psychiatr Serv. 2017;68:405–7. doi: 10.1176/appi.ps.201600080. [DOI] [PubMed] [Google Scholar]
- 18.Mohl A, Stulz N, Martin A, Eigenmann F, Hepp U, Hüsler J, et al. The “Suicide Guard Rail": A minimal structural intervention in hospitals reduces suicide jumps. BMC Res Notes. 2012;5:408. doi: 10.1186/1756-0500-5-408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Green JS, Grindel CG. Supervision of suicidal patients in adult inpatient psychiatric units in general hospitals. Psychiatr Serv. 1996;47:859–63. doi: 10.1176/ps.47.8.859. [DOI] [PubMed] [Google Scholar]
- 20.Assessment and Care of Adults at Risk for Suicidal Ideation and Behaviour [Internet] Toronto, Ont: Registered Nurses’ Association of Ontario; 2011. [Last accessed on 2019 Feb 26]. Registered Nurses' Association of Ontario. Available from: http://ra.ocls.ca/ra/login.aspx?inst=centennial&url=https://www.deslibris.ca/ID/228936. cited 2019 Feb 27. [Google Scholar]
- 21.Reynolds T, O'Shaughnessy M, Walker L, Pereira S. Safe and supportive observation in practice: A clinical governance project: Following a review of observation practices across the North East London Mental Health NHS Trust, a new policy with a greater emphasis on engagement was developed. It gave authority to nurses to review and adjust observation levels. After just three months, the results, say Trish Reynolds and colleagues, indicate increased patient satisfaction with observation practices. Ment Health Pract. 2005;8:13–6. [Google Scholar]
- 22.Awenat Y, Peters S, Shaw-Nunez E, Gooding P, Pratt D, Haddock G. Staff experiences and perceptions of working with in-patients who are suicidal: Qualitative analysis. Br J Psychiatry. 2017;211:103–8. doi: 10.1192/bjp.bp.116.191817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ramberg I-L, Di Lucca M, Hadlaczky G. The impact of knowledge of suicide prevention and work experience among clinical staff on attitudes towards working with suicidal patients and suicide prevention. Int J Environ Res Public Health. 2016;13:195. doi: 10.3390/ijerph13020195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ramberg I-L, Wasserman D. The roles of knowledge and supervision in work with suicidal patients. Nord J Psychiatry. 2003;57:365–71. doi: 10.1080/08039480310002705. [DOI] [PubMed] [Google Scholar]
- 25.Manister NN, Murray S, Burke JM, Finegan M, McKiernan ME. Effectiveness of Nursing Education to Prevent Inpatient Suicide. J Contin Educ Nurs. 2017;48:413–9. doi: 10.3928/00220124-20170816-07. [DOI] [PubMed] [Google Scholar]
- 26.Appleby L, Morriss R, Gask L, Roland M, Perry B, Lewis A, et al. An educational intervention for front-line health professionals in the assessment and management of suicidal patients (The STORM Project) Psychol Med. 2000;30:805–12. doi: 10.1017/s0033291799002494. [DOI] [PubMed] [Google Scholar]
- 27.Gask L, Dixon C, Morriss R, Appleby L, Green G. Evaluating STORM skills training for managing people at risk of suicide. J Adv Nurs. 2006;54:739–50. doi: 10.1111/j.1365-2648.2006.03875.x. [DOI] [PubMed] [Google Scholar]
- 28.Morriss R, Gask L, Battersby L, Francheschini A, Robson M. Teaching front-line health and voluntary workers to assess and manage suicidal patients. J Affect Disord. 1999;52:77–83. doi: 10.1016/s0165-0327(98)00080-9. [DOI] [PubMed] [Google Scholar]
- 29.van Landschoot R, Portzky G, van Heeringen K. Knowledge, self-confidence and attitudes towards suicidal patients at emergency and psychiatric departments: A randomised controlled trial of the effects of an educational poster campaign. Int J Environ Res Public Health. 2017:14. doi: 10.3390/ijerph14030304. doi: 10.3390/ijerph 14030304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bartels SJ. The aftermath of suicide on the psychiatric inpatient unit. Gen Hosp Psychiatry. 1987;9:189–97. doi: 10.1016/0163-8343(87)90007-7. [DOI] [PubMed] [Google Scholar]
- 31.Cotton PG, Drake RE, Whitaker A, Potter J. Dealing with suicide on a psychiatric inpatient unit. Hosp Community Psychiatry. 1983;34:55–9. doi: 10.1176/ps.34.1.55. [DOI] [PubMed] [Google Scholar]
- 32.Reeves H, Batra S, May RS, Zhang R, Dahl DC, Li X. Efficacy of risperidone augmentation to antidepressants in the management of suicidality in major depressive disorder: A randomized, double-blind, placebo-controlled pilot study. J Clin Psychiatry. 2008;69:1228–36. doi: 10.4088/jcp.v69n0805. [DOI] [PubMed] [Google Scholar]
- 33.Verkes RJ, Van der Mast RC, Hengeveld MW, Tuyl JP, Zwinderman AH, Van Kempen GM. Reduction by paroxetine of suicidal behavior in patients with repeated suicide attempts but not major depression. Am J Psychiatry. 1998;155:543–7. doi: 10.1176/ajp.155.4.543. [DOI] [PubMed] [Google Scholar]
- 34.Ward A, Ishak K, Proskorovsky I, Caro J. Compliance with refilling prescriptions for atypical antipsychotic agents and its association with the risks for hospitalization, suicide, and death in patients with schizophrenia in Quebec and Saskatchewan: A retrospective database study. Clin Ther. 2006;28:1912–21. doi: 10.1016/j.clinthera.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 35.Cipriani A, Hawton K, Stockton S, Geddes JR. Lithium in the prevention of suicide in mood disorders: Updated systematic review and meta-analysis. BMJ. 2013;346:f3646. doi: 10.1136/bmj.f3646. [DOI] [PubMed] [Google Scholar]
- 36.Guzzetta F, Tondo L, Centorrino F, Baldessarini RJ. Lithium treatment reduces suicide risk in recurrent major depressive disorder. J Clin Psychiatry. 2007;68:380–3. doi: 10.4088/jcp.v68n0304. [DOI] [PubMed] [Google Scholar]
- 37.Hennen J, Baldessarini RJ. Suicidal risk during treatment with clozapine: A meta-analysis. Schizophr Res. 2005;73:139–45. doi: 10.1016/j.schres.2004.05.015. [DOI] [PubMed] [Google Scholar]
- 38.Kasckow J, Felmet K, Zisook S. Managing suicide risk in patients with schizophrenia. CNS Drugs. 2011;25:129–43. doi: 10.2165/11586450-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Meltzer HY, Alphs L, Green AI, Altamura AC, Anand R, Bertoldi A, et al. Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT) Arch Gen Psychiatry. 2003;60:82–91. doi: 10.1001/archpsyc.60.1.82. [DOI] [PubMed] [Google Scholar]
- 40.Riesselman A, Johnson E, Palmer E. Lithium and clozapine in suicidality: Shedding some light to get out of the dark. Ment Health Clin. 2015;5:237–43. [Google Scholar]
- 41.Smith KA, Cipriani A. Lithium and suicide in mood disorders: Updated meta-review of the scientific literature. Bipolar Disord. 2017;19:575–86. doi: 10.1111/bdi.12543. [DOI] [PubMed] [Google Scholar]
- 42.Volavka J. Clozapine may be more effective than olanzapine for reducing suicidal behaviour in people with schizophrenia at high risk. Evid Based Ment Health. 2003;6:93. doi: 10.1136/ebmh.6.3.93. [DOI] [PubMed] [Google Scholar]
- 43.Modestin J, Dal Pian D, Agarwalla P. Clozapine diminishes suicidal behavior: A retrospective evaluation of clinical records. J Clin Psychiatry. 2005;66:534–8. doi: 10.4088/jcp.v66n0418. [DOI] [PubMed] [Google Scholar]
- 44.Ballard ED, Ionescu DF, Voort JL, Niciu MJ, Richards EM, Luckenbaugh DA, et al. Improvement in suicidal ideation after ketamine infusion: Relationship to reductions in depression and anxiety. J Psychiatr Res. 2014;58:161–6. doi: 10.1016/j.jpsychires.2014.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Menon V, Subramanian K, Selvakumar N, Kattimani S. Suicide prevention strategies: An overview of current evidence and best practice elements. Int J Adv Med Health Res. 2018;5:43. [Google Scholar]
- 46.Mewton L, Andrews G. Cognitive behavioral therapy for suicidal behaviors: Improving patient outcomes. Psychol Res Behav Manag. 2016;9:21–9. doi: 10.2147/PRBM.S84589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ghahramanlou-Holloway M, Cox DW, Greene FN. Post-admission cognitive therapy: A brief intervention for psychiatric inpatients admitted after a suicide attempt. Cogn Behav Pract. 2012;19:233–44. [Google Scholar]
- 48.Ghahramanlou-Holloway M, LaCroix JM, Perera KU, Neely L, Grammer G, Weaver J, et al. Inpatient psychiatric care following a suicide-related hospitalization: A pilot trial of post-admission cognitive therapy in a military medical center? Gen Hosp Psychiatry. 2018 doi: 10.1016/j.genhosppsych.2018.11.006. doi: 10.1016/j.genhosppsych. 2018.11.006. [DOI] [PubMed] [Google Scholar]
- 49.LaCroix JM, Perera KU, Neely LL, Grammer G, Weaver J, Ghahramanlou-Holloway M. Pilot trial of post-admission cognitive therapy: Inpatient program for suicide prevention. Psychol Serv. 2018;15:279–88. doi: 10.1037/ser0000224. [DOI] [PubMed] [Google Scholar]
- 50.Jobes DA. Managing Suicidal Risk: A Collaborative Approach. Second edition. New York: The Guilford Press; 2016. p. 270. [Google Scholar]
- 51.Jobes DA. The Collaborative Assessment and Management of Suicidality (CAMS): An evolving evidence-based clinical approach to suicidal risk. Suicide Life Threat Behav. 2012;42:640–53. doi: 10.1111/j.1943-278X.2012.00119.x. [DOI] [PubMed] [Google Scholar]
- 52.Ellis TE, Rufino KA, Allen JG, Fowler JC, Jobes DA. Impact of a suicide-specific intervention within inpatient psychiatric care: The collaborative assessment and management of suicidality. Suicide Life Threat Behav. 2015;45:556–66. doi: 10.1111/sltb.12151. [DOI] [PubMed] [Google Scholar]
- 53.George MS, Raman R, Benedek DM, Pelic CG, Grammer GG, Stokes KT, et al. Atwo-site pilot randomized 3 day trial of high dose left prefrontal repetitive transcranial magnetic stimulation (rTMS) for suicidal inpatients. Brain Stimulat. 2014;7:421–31. doi: 10.1016/j.brs.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 54.Patel M, Patel S, Hardy DW, Benzies BJ, Tare V. Should electroconvulsive therapy be an early consideration for suicidal patients? J ECT. 2006;22:113–5. doi: 10.1097/00124509-200606000-00007. [DOI] [PubMed] [Google Scholar]
- 55.Sharma V. Retrospective controlled study of inpatient ECT: Does it prevent suicide? J Affect Disord. 1999;56:183–7. doi: 10.1016/s0165-0327(98)00207-9. [DOI] [PubMed] [Google Scholar]
- 56.Kellner CH, Fink M, Knapp R, Petrides G, Husain M, Rummans T, et al. Relief of expressed suicidal intent by ECT: A consortium for research in ECT study. Am J Psychiatry. 2005;162:977–82. doi: 10.1176/appi.ajp.162.5.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ramberg I-L, Wasserman D. Suicide-preventive activities in psychiatric care: Evaluation of an educational programme in suicide prevention. Nord J Psychiatry. 2004;58:389–94. doi: 10.1080/08039480410005954. [DOI] [PubMed] [Google Scholar]
- 58.Pitula CR, Cardell R. Suicidal inpatients' experience of constant observation. Psychiatr Serv. 1996;47:649–51. doi: 10.1176/ps.47.6.649. [DOI] [PubMed] [Google Scholar]
- 59.Berg SH, Rørtveit K, Aase K. Suicidal patients' experiences regarding their safety during psychiatric in-patient care: A systematic review of qualitative studies. BMC Health Serv Res. 2017;17:73. doi: 10.1186/s12913-017-2023-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ahrens B, Müller-Oerlinghausen B, Grof P. Length of lithium treatment needed to eliminate the high mortality of affective disorders. Br J Psychiatry Suppl. 1993:27–9. [PubMed] [Google Scholar]
- 61.Berman RM, Cappiello A, Anand A, Oren DA, Heninger GR, Charney DS, et al. Antidepressant effects of ketamine in depressed patients. Biol Psychiatry. 2000;47:351–4. doi: 10.1016/s0006-3223(99)00230-9. [DOI] [PubMed] [Google Scholar]
- 62.Zarate CA, Brutsche NE, Ibrahim L, Franco-Chaves J, Diazgranados N, Cravchik A, et al. Replication of ketamine's antidepressant efficacy in bipolar depression: A randomized controlled add-on trial. Biol Psychiatry. 2012;71:939–46. doi: 10.1016/j.biopsych.2011.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zarate CA, Singh JB, Carlson PJ, Brutsche NE, Ameli R, Luckenbaugh DA, et al. Arandomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatr. 2006;63:856–64. doi: 10.1001/archpsyc.63.8.856. [DOI] [PubMed] [Google Scholar]
- 64.Bartoli F, Riboldi I, Crocamo C, Di Brita C, Clerici M, Carrà G. Ketamine as a rapid-acting agent for suicidal ideation: A meta-analysis. Neurosci Biobehav Rev. 2017;77:232–6. doi: 10.1016/j.neubiorev.2017.03.010. [DOI] [PubMed] [Google Scholar]
- 65.Soleimani L, Welch A, Murrough JW. “Does ketamine have rapid anti-suicidal ideation effects?”. Curr Treat Options Psychiatry. 2015;2:383–93. doi: 10.1007/s40501-015-0065-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wilkinson ST, Ballard ED, Bloch MH, Mathew SJ, Murrough JW, Feder A, et al. The effect of a single dose of intravenous ketamine on suicidal ideation: A systematic review and individual participant data meta-analysis. Am J Psychiatry. 2018;175:150–8. doi: 10.1176/appi.ajp.2017.17040472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wilkinson ST, Sanacora G. Ketamine: A potential rapid-acting antisuicidal agent? Depress Anxiety. 2016;33:711–7. doi: 10.1002/da.22498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sos P, Klirova M, Novak T, Kohutova B, Horacek J, Palenicek T. Relationship of ketamine's antidepressant and psychotomimetic effects in unipolar depression. Neuro Endocrinol Lett. 2013;34:287–93. [PubMed] [Google Scholar]
- 69.Comtois KA, Linehan MM. Psychosocial treatments of suicidal behaviors: A practice-friendly review. J Clin Psychol. 2006;62:161–70. doi: 10.1002/jclp.20220. [DOI] [PubMed] [Google Scholar]
- 70.Tarrier N, Taylor K, Gooding P. Cognitive-behavioral interventions to reduce suicide behavior: A systematic review and meta-analysis. Behav Modif. 2008;32:77–108. doi: 10.1177/0145445507304728. [DOI] [PubMed] [Google Scholar]
- 71.Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: A randomized controlled trial. JAMA. 2005;294:563–70. doi: 10.1001/jama.294.5.563. [DOI] [PubMed] [Google Scholar]
- 72.Rudd MD, Bryan CJ, Wertenberger EG, Peterson AL, Young-McCaughan S, Mintz J, et al. Brief cognitive-behavioral therapy effects on post-treatment suicide attempts in a military sample: Results of a randomized clinical trial with 2-year follow-up. Am J Psychiatry. 2015;172:441–9. doi: 10.1176/appi.ajp.2014.14070843. [DOI] [PubMed] [Google Scholar]
- 73.American Psychiatric Association. Task Force on Electroconvulsive Therapy. The Practice of ECT: Recommendations for Treatment, Training and Privileging. Convuls Ther. 1990;6:85–120. [PubMed] [Google Scholar]
- 74.Easton A, Waite J. The ECT Handbook. 17 Belgrave Square, London: RCPsych Publications; 2013. [Google Scholar]
- 75.Dowman J, Patel A, Rajput K. Electroconvulsive therapy: Attitudes and misconceptions. J ECT. 2005;21:84–7. doi: 10.1097/01.yct.0000161043.00911.45. [DOI] [PubMed] [Google Scholar]
- 76.Payne NA, Prudic J. Electroconvulsive therapy: Part II: A biopsychosocial perspective. J Psychiatr Pract. 2009;15:369–90. doi: 10.1097/01.pra.0000361278.73092.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Clarke DE, Brown A-M, Giles-Smith L. Triaging suicidal patients: Sifting through the evidence. Int Emerg Nurs. 2008;16:165–74. doi: 10.1016/j.ienj.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 78.Ronquillo L, Minassian A, Vilke GM, Wilson MP. Literature-based recommendations for suicide assessment in the emergency department: A review. J Emerg Med. 2012;43:836–42. doi: 10.1016/j.jemermed.2012.08.015. [DOI] [PubMed] [Google Scholar]


