Abstract
Background:
Whether use of ultrasound (USG) to cannulate dorsalis pedis artery (DPA) increases first pass successful cannulation, decreases the number of attempts and complications as compared to palpation technique was assessed in this study.
Design:
Randomized controlled trial.
Setting:
Operating room.
Patients:
About 60 adult patients undergoing any head–neck or faciomaxillary surgery requiring arterial cannulation were enrolled.
Intervention:
DPA was cannulated either by USG-guided technique (USG group) or by palpation technique (palpation group) with 30 patients in each group.
Measurement:
Data were assessed for “first-attempt success” of cannulation, number of attempts, assessment time, cannulation time, cannulation failure, and incidence of complications.
Main Results:
Successful first pass DPA cannulation was similar between the groups (ultrasound group vs. palpation group, 76.7% vs. 60%, respectively) [relative risk (95% confidence interval (CI) = 0.69 (0.43, 1.13), P = 0.267)] as was the number of attempts required for successful cannulation [median (interquartile range (IQR) number of attempts 1 (1–2) in palpation group P and USG group U 1 (1–1); P = 0.376]. Median (IQR) assessment time was significantly less (P < 0.0004) in palpation group [palpation group 12 (9–17) vs. USG group U 19 (15–21)]. However, cannulation time was significantly higher (P = 0.0093) in Group P [median (IQR) 17.5 (12–36 s) and 11.5 (9–15)]. Although the total procedure time (sum of both assessment time and cannulation time) remain statistically similar between two groups (P = 0.8882).
Conclusions:
Use of USG for the cannulation of DPA is feasible, but it is not associated with significant increase in first-attempt success rate, decrease in total number of cannulation attempts or total procedure time.
Keywords: Dorsalis pedis artery, first-pass success, number of attempts to cannulate DPA, palpation technique, ultrasound
Introduction
Intra-arterial cannulation enables beat-to-beat blood pressure monitoring, assessment of fluid responsiveness, and frequent blood sampling in the intraoperative period as well as in the intensive care unit. Different sites can be chosen for arterial cannulation, such as the radial, posterior tibial, femoral, brachial, axillary, ulnar, dorsalis pedis, and temporal arteries;[1] all of these have some specific advantages and disadvantages. Traditional arterial cannulation uses the landmark technique by palpating the arterial pulse. The palpation technique needs an experienced physician. Multiple attempts can cause arterial spasms and hematoma.[2] In a study comparing radial and dorsalis pedis artery (DPA) complication rates using traditional palpation techniques, the rates of serious complications were similar for both sites of arterial catheterization. In patients, where radial artery is not felt or in the head and neck surgery cases DPA is cannulated. However, there was a 12.7% lower rate of success when placing DPA catheters.[3] There is no study till date in which palpatory method of DPA cannulation is compared with ultrasound (USG)-guided DPA cannulation in adult population. We hypothesized that using USG to cannulate DPA will help in first pass successful cannulation, decreasing the number of attempts for successful cannulation, and decreasing the complication as it does for radial artery cannulation.
Methods
This randomized clinical trial was conducted in a tertiary care teaching hospital in India. After approval from the institutional ethics committee, n = 60 adult patients (aged between 18–65 years) of either sex undergoing any head–neck surgery or faciomaxillary surgery requiring arterial cannulation were recruited in this randomized controlled trial. This trial was registered at the National Clinical Trial Registry of India (www.ctri.nic.in, Ref No: REF/2018/04/019691).
Following were the exclusion criteria:
Patient's refusal to participate
Patients with absence of an amplitude of DPA pulsation
Skin erosions near the insertion site
Obesity defined by body mass index >30 kg/m2
Sample size estimation
No study has been done to compare the first-attempt success to cannulate DPA and number of attempts to cannulate DPA by in-plane USG and palpation technique. In this present study, 30 patients in each group (n = 60) were recruited on pilot basis. We have chosen n = 30 patients in each group so that normality tests are valid in the population.
Study protocol
Randomization sequence was generated by a web-based randomization program (www.randomizer.org) and it was kept inside serially numbered opaque-sealed envelope. Sealed envelopes were opened to reveal allocation just before the DPA cannulation.
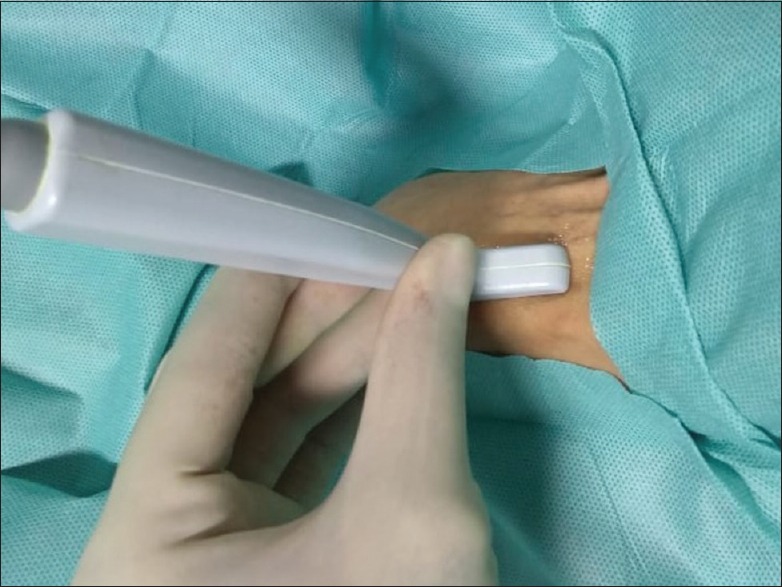
After induction of general anesthesia using a standard protocol, all aseptic precautions were exercised and a 20G arterial cannula (BD) percutaneously punctured the DPA either by the palpation technique at dorsal most prominence of the navicular bone[4] or by the USG-guided technique using a vascular transducer small footprint (8–13 MHz) and a two-dimensional M-Turbo ultrasound system (SonoSite, Inc, Bothell, WA). For USG-guided artery cannulation DPA was imaged in short axis at the point of bifurcation of DPA and then USG probe was adjusted to bring DPA in long-axis view [Figure 1]. The needle was inserted by in-plane technique in real time [Figure 2]. The assessment time (T1) was defined as “time between start of palpation/screening of artery to skin puncture by needle” and cannulation time (T2) was defined as “time between the initial needle penetration through the skin to successful cannulation of artery.” The successful arterial cannulation was defined as “removal of the metal needle/stylet and continuation of a flash of arterial blood.” Failure was defined as “failure of successful cannulation after three attempts.” In both cases, crossover with technique was tried for one more attempt before abandoning the procedure. Cannulation attempts were quantified as “the numbers of needle tips completely withdrawn from the skin.” The success rate was defined as “successful cannulation of the DPA in three attempts or fewer.” After successful cannulation, USG was used to measure the diameter of the artery in cross section in both the groups. All the cannulations were performed by a single investigator (Rahul Kumar Anand) who had experience of >50 DPA cannulations using each technique to minimize inter-individual variability in skills.
Figure 1.
Ultrasound-guided technique for dorsalis pedis artery cannulation
Figure 2.

Catheter in dorsalis pedis artery
Outcome data
Primary outcome of this study is the “ first-attempt success” of cannulation. Secondary outcomes are: number of attempts to cannulate, screening time, cannulation time, cannulation failure, incidence of complications (digital ischemia, hemorrhage, thrombosis, and hematoma formation). Primary and secondary outcome data were collected by an unblinded anesthesiologist who were not a part of this study.
Statistical analysis
Shapiro–Wilk normality test was conducted to identify normally distributed variables. Normally distributed continuous variables (such as age, body weight, and height) were expressed as mean and standard deviation (SD) and non-normally distributed variables and categorical variables (such as cannulation time, total procedure time, and number of attempts to cannulation) were expressed as median and IQR. Binary variables (such as sex and first attempt success rate) were expressed as absolute numbers and proportions. Independent sample t-test was used to compare normally distributed continuous variables in two groups. Results were interpreted from P value; a P value <0.05 was considered to be statistically significant. Categorical variables and non-normally distributed continuous variables were compared by the Mann–Whitney U test and a P value <0.05 was considered statistically significant. Median difference was calculated by the Hodges–Lehmann method when statistical significance was obtained. Binary variables were compared with the Chi-square test or Fisher's exact test and a relative risk with 95% CI and absolute risk reduction was reported for all clinical outcomes. All statistical analyses were conducted in the STATA 12 software for Mac OS (StataCorp. 2011. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP). All statistical analyses were conducted by Souvik Maitra, who was unaware about allocation of the patients.
Results
Baseline demographic variables were comparable in both the groups [Table 1]. Successful first pass DPA cannulation was 76.7% in USG group (23 of 30 patients) and 60% (18 of 30 patients) in palpation group, and it was statistically similar [relative risk (95% confidence interval (CI) = 0.69 (0.43, 1.13), P = 0.267; Chi-square test)] [Table 2]. Number of attempts required for successful DPA cannulation were also found to be statistically similar in between the two groups [median (IQR) number of attempts 1 (1–2) in palpation group and 1 (1–1); P = 0.376, Mann–Whitney U test) as was the requirement of alternative techniques (P > 0.99, Fisher's exact test). Median (IQR) assessment time was 12 (9–17 s) in palpation group, whereas it was 19 (15–21 s) in USG group which was significantly less (P = 0.0004). However, cannulation time was significantly higher in palpation group; [median (IQR) were 17.5 (12–36 s) and 11.5 (9–15 s), respectively, in palpation and USG group; P = 0.009]. Although the total procedure time (sum of both assessment time and cannulation time) remain statistically similar between two groups (P = 0.8882, Mann–Whitney U test). Complications were not noticed in any of the two groups. There was no correlation in gender and successful first pass cannulation. Crossover was done in three patients (one patient in USG group U and two patients in palpation group), successful cannulation was there in one patient of palpation group and in rest of the two patients procedure was abandoned.
Table 1.
Comparison of baseline demographic parameters of the patients
| Group P (n=30) | Group U (n=30) | Significance | |
|---|---|---|---|
| Age (in years) | 41.4±19.0 | 41.4±16.2 | P=0.99# |
| Sex (Male/Female) | 18/12 | 16/14 | P=0.60$ |
| Body weight (in kgs) | 58.6±9.8 | 55.2±8.5 | P=0.16# |
| Height (in cm) | 166.8±13.5 | 164.7±12.9 | P=0.54# |
| Type of surgery (ENT/maxilla-facial) | 21/9 | 22/8 | P=0.78$ |
Table 2.
Comparison of cannulation characteristics in two groups
| Group P (n=30) | Group U (n=30) | Significance | |
|---|---|---|---|
| First attempt success (Yes/No) | 18/12 | 23/7a | P=0.267$ |
| Number of attempts to cannulation | 1 [1-2] | 1 [1-1] | P=0.3736@ |
| Requirement of alternative techniques | 1/29 | 1/29 | P>0.99$ |
| Assessment time | 12 [9-17] | 19 [15-21] | P=0.0004@ |
| Cannulation time | 17.5 [12-36] | 11.5 [9-15] | P=0.0093@ |
| Total procedure time | 33.5 [24-48] | 31.5 [27-39] | P=0.8882@ |
$Chi- square test, @Mann- Whitney U test, #Independent sample t-test
Discussion
In this study, we have found that the use of USG for the cannulation of DPA is feasible although it is neither associated with significant increase in first attempt success rate as compared to palpation technique nor it is associated with significant decrease in total number of cannulation attempts or total procedure time.
The DPA represents the continuation of the anterior tibial artery distal to the level of the ankle joint. The use of dynamic two-dimensional (2D) USG guidance for radial artery catheterization decreases first-attempt failure, mean attempts to success, mean time to success, and the occurrence of hematoma formations. Dynamic 2D USG guidance is recommended as an aid to radial arterial catheterization.[5] However, the data about use of USG for cannulation of DPA are lacking. The non-superiority of USG for the cannulation of DPA may be because of its anatomical position and the fact that it is difficult to bring DPA to horizontal frame during assessment, which is evident by the fact that the assessment time was significantly higher in Group U. Moreover, although the DPA cannulations were performed by anesthesiologist who had experience of >50 USG-guided radial artery cannulation; he was far more experienced in palpation technique for the same. Palpation is a generic skill that all anesthesiologists develop while training as medical students. Though the results were not clinically significant, there was 17% higher rate of first-pass successful cannulation in USG group as compared to palpation group. In radial artery cannulation USG is associated with a 14–28% increase in first-pass success.[6,7] So, the results of the study are encouraging and further studies using larger sample size of or using trainee anesthesiologist who are not so experienced in palpation technique may yield better results in favor of USG group.
We have found that cannulation time was lower with use of USG, but wide CI in median difference limits its clinical utility. A higher assessment time in USG resulted similar total procedure time between two groups.
USG might be particularly useful for the Seldinger cannulation method, which was not the default choice in our study as a guidewire can increase the rate of cannulation following arterial puncture, particularly for inexperienced personnel.[8] Our results cannot be generalized to children, in whom any advantage of USG for arterial cannulation might be dependent on age.[9,10]
Conclusion
USG-guided DPA cannulation is feasible in adults, although it is not associated with higher first pass successful cannulation, decrease in the number of attempts to successful cannulation, and total procedure time. Further randomized control trial with adequate sample size may be contributory.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Miller AG, Bardin AJ. Review of ultrasound-guided radial artery catheter placement. Respir Care. 2016;61:383–8. doi: 10.4187/respcare.04190. [DOI] [PubMed] [Google Scholar]
- 2.Shiver S, Blaivas M, Lyon M. A prospective comparison of ultrasound-guided and blindly placed radial arterial catheters. Acad Emerg Med. 2006;13:1275–9. doi: 10.1197/j.aem.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 3.Martin C, Saux P, Papazain L, Goulin F. Long-term arterial cannulation in ICU patients using the radial artery or dorsalis pedis artery. Chest. 2001;119:901–6. doi: 10.1378/chest.119.3.901. [DOI] [PubMed] [Google Scholar]
- 4.Mowlavi A, Whiteman J, Wilhelmi BJ, Neumeister MW, McLafferty R. Dorsalis pedis arterial pulse: Palpation using a bony landmark. Postgrad Med J. 2002;78:746–7. doi: 10.1136/pmj.78.926.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhattacharjee S, Maitra S, Baidya DK. Comparison between ultrasound guided technique and digital palpation technique for radial artery cannulation in adult patients: An updated meta-analysis of randomized controlled trials. J Clin Anesth. 2018;47:54–9. doi: 10.1016/j.jclinane.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 6.Shiver S, Blaivas M, Lyon M. A prospective comparison of ultrasound-guided and blindly placed radial arterial catheters. Acad Emerg Med. 2006;13:1275–9. doi: 10.1197/j.aem.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 7.Ueda K, Bayman EO, Johnson C, Odum NJ, Lee JJ. A randomised controlled trial of radial artery cannulation guided by doppler vs palpation vs ultrasound. Anaesthesia. 2015;70:1039–44. doi: 10.1111/anae.13062. [DOI] [PubMed] [Google Scholar]
- 8.Mangar D, Thrush DN, Connell GR, Downs JB. Direct or modified seldinger guide wire-directed technique for arterial catheter insertion. Anesth Analg. 1993;76:714–7. [PubMed] [Google Scholar]
- 9.Ganesh A, Kaye R, Cahill AM, Stern W, Pachikara R, Gallagher PR, et al. Evaluation of ultrasound guided radial artery cannulation in children. Pediatr Crit Care Med. 2009;10:45–8. doi: 10.1097/PCC.0b013e31819368ca. [DOI] [PubMed] [Google Scholar]
- 10.Ueda K, Puangsuvan S, Hove MA, Bayman EO. Ultrasound visual image-guided vs doppler auditory-assisted radial artery cannulation in infants and small children by non-expert anaesthesiologists: A randomized prospective study. Br J Anaesth. 2013;110:281–6. doi: 10.1093/bja/aes383. [DOI] [PubMed] [Google Scholar]


