Abstract
Background and Aims:
Pectoral nerve (PecS II) block is the latest modality for providing postoperative analgesia after breast surgery. The present study was planned to compare the analgesic efficacy of thoracic paravertebral block (TPVB) and PecS II for postoperative analgesia after modified radical mastectomy (MRM).
Methods:
A total of 40 female patients undergoing radical mastectomy were randomly allocated into two groups (n = 20). Group T received ultrasound-guided TPVB, while group P received PecS II block using 0.25% levobupivacaine 24 ml + dexamethasone 1 ml (4 mg) before induction of anesthesia. The primary outcome was duration of analgesia (time to request first analgesic dose), while total rescue analgesic consumption in first 24 h, numeric rating score (NRS), and complication were secondary outcomes. The data were analyzed using IBM SPSS software version 22.0.
Results:
The duration of analgesia was significantly prolonged in the group P than group T (474.1 ± 84.93 versus 371.5 ± 51.53 min, respectively; P < 0.0001). Postoperative morphine consumed at 24 h was less in the group P than group T (11.25 ± 4.75 and 15.0 ± 4.86 mg, respectively; P = 0.018). NRS at movement and rest were lower in the group P as compared to group T at all time intervals (median 3 versus 4). No block-related complication was recorded in any group.
Conclusions:
The 0.25% levobupivacaine with dexamethasone 4 mg in PecS II block provided longer duration of analgesia than the TPVB in patients undergoing MRM without any adverse effects.
Keywords: Dexamethasone, levobupivacaine, modified radical mastectomy, paravertebral block, pectoral nerve block
Introduction
Modified radical mastectomy (MRM) is commonly performed under general anesthesia and is associated with considerable postoperative pain,[1] which in turn leads to increased vulnerability for development of chronic persistent pain.[2,3] Regional anesthesia techniques may provide better postoperative pain control.[4]
Thoracic epidural analgesia (TEA) and thoracic paravertebral block (TPVB) were the most widely used techniques to provide postoperative analgesia after breast surgeries. The patients under TPVB frequently complain of postoperative pain in axilla and upper limbs due to sparing of medial and lateral pectoral nerve. Moreover, TPVB is also associated with risk of pneumothorax, sympathetic block, and hypotension.[5,6]
The pectoral nerve (PecS II) block, which was first described by Blanco et al.,[7] is a relatively new, less-invasive technique of postoperative analgesia and is devoid of major side effects. The Pecs II block[8] is an interfascial plane block, where local anesthetic (LA) is deposited into the plane between the pectoralis major muscle (PMm) and the pectoralis minor muscle (Pmm) (PecS I block) and between Pmm and the serratus anterior muscle at the third rib (Pecs II block). This novel technique also blocks long thoracic and thoracodorsal nerves, lateral and medial pectoral nerves along with lateral branches of intercostal nerves, exiting at the level of mid-axillary line to innervate the breast and the skin innervate from T2 to T6, thus providing good analgesia for mastectomy and axillary clearance.[9,10]
Till date, no study was available on levobupivacaine and dexamethasone combination to compare the efficacy of TPVB and PecS II block for postoperative analgesia after MRM surgeries. Hence the present study was planned to compare the efficacy and safety of ultrasound-guided PecS II block and TPVB using 24 ml of 0.25% levobupivacaine + 1 ml (4 mg) dexamethasone for postoperative analgesia after MRM.
Methods
This prospective, randomized study was conducted between June 2017 and February 2018, after obtaining approval from Institutional Ethics Committee (Reference no. F. 1/Acad/MC/JU/17/10250, dated 20/06/2017) and registered under clinical trial registry of India (CTRI/2017/11/010526). A total of 40 female patients, with American Society of Anesthesiologist (ASA) physical status I/II, aged 18–65 years, who were undergoing elective unilateral MRM under general anesthesia were included in the study. All patients were explained the purpose of the study, and thereafter written informed consent was obtained from all patients undergoing study. Patients with infection at the block site, coagulopathy, morbid obesity [body mass index (BMI) >40 kg/m2], allergy to LA agent, major cardiac disorders, decreased pulmonary reserve, renal dysfunction, preexisting neurological deficits, and psychiatric illness were excluded from the study.
The patients were randomly divided into two equal groups by computer-generated random number table. The group allocation numbers were concealed in sealed opaque envelopes that was opened by an anesthesiologist not involved in the study. The observer who collected perioperative data was blinded to the technique of analgesia used.
One day before surgery, a detailed preoperative anesthesia evaluation was done and patients were educated about numeric rating score (NRS). All patients were kept fasting as per standard ASA protocol. All patients were premedicated with tab. lorazepam 2 mg and tab. ranitidine 150 mg orally night before and 2 h before surgery. Group P patients received PecS II block, whereas group T received TPVB block with 0.25% levobupivacaine 24 ml and dexamethasone 1 ml (4 mg) with total volume of 25 ml in preoperative area 30 min before surgery with all aseptic precautions under continuous monitoring of heart rate (HR), noninvasive blood pressure (NIBP), and oxygen saturation (SpO2). The blocks were performed on the side of surgery with a 22 G echogenic needle (Pajunk, SonoPlex Stim cannula, Geisingen, Germany; 100 mm) using ultrasound machine (Sonosite, M Turbo Inc., Bothell, WA, USA) and linear array probe (38 mm, 6–13 MHz frequency).
In group P, PecS II block was performed in supine position with ipsilateral upper arm abducted. The ultrasonographic (USG) probe was placed at midclavicular level, inferolaterally to clavicle to locate the axillary artery and axillary vein, and then moved laterally until pectoralis minor and serratus anterior muscles were identified at the level of third rib. After skin infiltration with lidocaine 2%, the needle was advanced under in-plane approach from medial to lateral in an oblique manner until the tip entered the plane between pectoralis minor and serratus anterior, and 15 ml mixture of levobupivacaine 0.25% and dexamethasone was injected in this space. After deposition of drug, the needle was withdrawn until it lays in the plane between pectoralis minor and pectoralis major, and the remaining 10 ml mixture of levobupivacaine 0.25% and dexamethasone was deposited in the space.
In group T, USG-guided TPVB was given at T3 level in sitting position. The skin was infiltrated with 2% lignocaine down to the T2 transverse process. The USG linear probe was placed 5 cm from midline in craniocaudal direction and moved medially to show bony transition from rib to transverse process. The parietal pleura was seen as a bright structure running deep to the adjacent transverse processes, distinct from the deeper lung tissue, which shimmers and moves with patient respirations. The superior costotransverse ligament was seen as a collection of homogeneous linear echogenic bands alternating with echo poor areas running from one transverse ligament to the next. A volume of 25 ml levobupivacaine 0.25% and dexamethasone was deposited in the space between pleura and costotransverse ligament.
After performing the block, the sensory level of block was assessed with pin prick sensation every 5 min in each dermatomal distribution from T1 to T8 for first 30 min by an anesthesiologist who are not aware of study group. Total number of dermatomes that had less pain to pin prick compared with opposite side was noted. If the pin prick sensation does not decrease in any segment up to 30 min, it was considered as block failure and these patients were excluded from the study. Any block-related complications, such as vascular puncture, LA toxicity, Horner's syndrome or pneumothorax, were recorded. Any side-effect in the form of nausea, vomiting, respiratory depression, hypotension, pruritus, and chest pain in the perioperative period was noted. After 30 min of block the patient was shifted to the operating room.
General anesthesia was induced in all patients with fentanyl (1 μg/kg), propofol (2 mg/kg), and vecuronium bromide (0.1 mg/kg). Anesthesia was maintained with air (50%), oxygen (50%), isoflurane with minimum alveolar concentration (MAC) of 0.9–1.0. Supplemental analgesia was provided with fentanyl (1 μg/kg) IV bolus, if HR or mean blood pressure (MBP) exceeded 30% of the preoperative values. Continuous monitoring of HR, NIBP, peripheral SpO2, and end-tidal carbon dioxide (EtCO2) was done every 15 min till the end of surgery. The number of doses and total dose of fentanyl used as supplement analgesia intraoperatively were noted for comparison between two groups. After completion of surgery, residual neuromuscular blockade was reversed with neostigmine 0.05 mg/kg and glycopyrrolate 0.01 mg/kg IV and extubated and transferred to postoperative recovery unit. The total duration of the surgery was also noted.
The patients were monitored at 0, 2, 4, 6, 8, 10, 12, 14, 16, 18, 20, 22, and 24 h postoperatively for HR, NIBP, SpO2, respiratory rate (RR), and NRS. The NRS is a segmented numeric version of the visual analog scale (VAS) in which a respondent selects a whole number (0–10 integers) that best reflects the intensity of her pain. The common format is a horizontal bar or line which contains 11-point numeric scale ranging from “0” representing one pain extreme (e.g., “no pain”) to “10” representing the other pain extreme (e.g., “pain as bad as you can imagine” or “worst pain imaginable”). NRS was assessed during rest (NRS-R) and on movement (NRS-M) at predefined intervals postoperatively.
Duration of analgesia defined as the time interval from completion of LA administration till first need of rescue analgesic. The rescue analgesic regime included morphine 3 mg slow IV whenever NRS ≥4 on rest or patient's demand. Total rescue analgesic consumption per patient as described in total dose of morphine used in initial 24 h postoperatively was also recorded.
Any adverse effects, such as bradycardia (HR <40 bpm), hypotension (reduction of MBP ≥30% of baseline), respiratory depression (RR ≤8 breaths/min or SpO2 <90%), nausea, or vomiting, were recorded. Nausea lasting more than 10 min or vomiting was treated with ondansetron 0.1 mg/kg IV. Hypotension was treated with bolus of normal saline and if required mephentermine 6 mg IV was administrated. Bradycardia was treated with atropine 0.6 mg IV. Respiratory depression was treated with oxygen supplementation by ventimask. Patient's satisfaction score was graded as 4 = excellent, 3 = good, 2 = fair, 1 = poor.
The data were collected from all patients included in the study and were subjected to appropriate statistical tests to assess the level of significance difference in results between the two groups.
Sample size and statistical analysis
The sample size was calculated on the basis of a previous study by Kulhari et al.[8] The mean duration of analgesia (time to first rescue analgesia after administration of block) was taken as a primary outcome. Using table of tradeoffs for any combination of sample size (n) and power, a sample size of 16 in each group was needed with the 80% power and 95% confidence interval; α and β errors are 0.05 and 0.02, respectively. To allow for the potential dropouts, a total of 20 patients per group was included in the study. Statistical analysis was done using IBM SPSS software version 22.0. The normally distributed data were compared using Student's unpaired t-test, whereas nonparametric data were compared by χ2-test for intergroup differences. Intraoperative hemodynamics data were compared with baseline by repeated measured by Student's paired t-test.
Results
A total of 47 patients were enrolled during the study period, but only 40 patients participated in the study. Five patients decline to participate in the study and two patients were not fulfilling the criteria [Figure 1]. The groups were comparable with respect to age, weight, ASA physical status, and the duration of surgery [Table 1].
Figure 1.
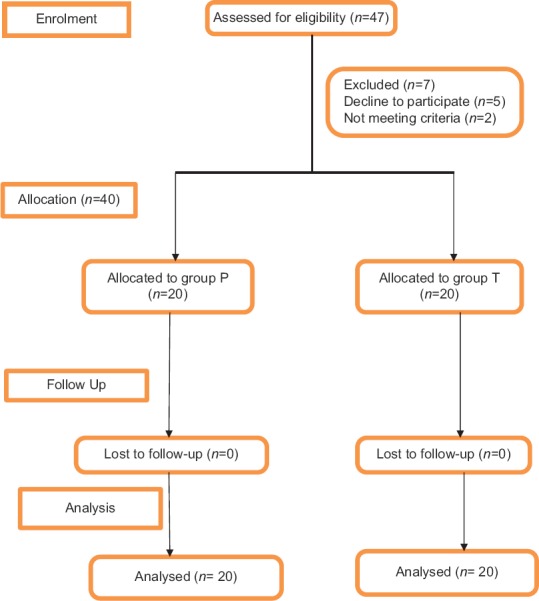
Consort flow diagram of participants through each stage of randomized trial
Table 1.
Demographic data and duration of surgery
| Variables | Group P (n=20) | Group T (n=20) | P |
|---|---|---|---|
| Age (years), (mean±SD) | 45.96±14.92 | 46.54±15.04 | 0.66 |
| ASA status (number of patients) I/II | 13/7 | 15/5 | 0.731 |
| Duration of surgery (minute), (mean±SD) | 47.90±8.08 | 49.30±6.22 | 0.414 |
| Height (cm), (mean±SD) | 158.15±5.48 | 159.6±3.64 | 0.331 |
| Weight (kg), (mean±SD) | 57.15±5.20 | 57±7.57 | 0.942 |
The mean duration of analgesia was significantly more in group P compared to group T (474.1 ± 84.93 min versus 371.5 ± 51.53 min; P < 0.0001) [Table 2]. In group P, only six patients and in group T 10 patients received fentanyl out of 20, but the difference was not statistically significant (15 ± 1.0 versus 25.0 ± 3.0 μg in group T; P = 0.33). Total dose of morphine consumption in 24 h in group P was less (11.25 ± 4.75 mg) compared to group T (15.0 ± 4.86 mg; P = 0.018) [Table 2]. The median total number of rescue analgesic dose used in group T was significantly higher than group P (5 versus 4; P = 0.018) [Table 2]. The postoperative NRS-R and NRS-M scores were higher in group T in comparison to group P [Tables 3 and 4]. Statistically significant result at rest was found at 2, 4, 6, and 10 h (P = 0.002, 0.035, 0.007, 0.023), which was lower in group P in comparison to group T. There was no statistically significant difference between the groups with respect to HR, SpO2, and MBP during the perioperative period.
Table 2.
Duration of analgesia and total analgesic requirement
| Variable | Group P (n=20) | Group T (n=20) | P |
|---|---|---|---|
| Duration of analgesia [minute] (mean±SD) | 474.1±84.93 | 371.5±51.53 | <0.0001* |
| Intraop fentanyl consumption [µg] (mean±SD) | 15±1 | 25±3 | 0.333 |
| 24-h morphine consumption [mg] (mean±SD) | 11.25±4.75 | 15±4.86 | 0.018* |
| Number of rescue morphine doses (median) | 4 | 5 | 0.018* |
*Duration of analgesia, 24-h morphine consumption and number of rescue morphine doses were significantly prolonged in ultrasound guided pectoral nerve block group in comparison to thoracic paravertebral block group (P<0.0001, 0.018, and 0.018)
Table 3.
Comparison of post-operative NRS-R
| Time | Group P (n=20) | Group T (n=20) | P | ||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| 0 h | 2 | 2-3 | 3 | 2-3 | 0.457 |
| 2 h | 2 | 2-3 | 3 | 2-3 | 0.002* |
| 4 h | 1 | 1-2 | 2 | 1-2 | 0.035* |
| 6 h | 3 | 2-3 | 4 | 3-5 | 0.007* |
| 8 h | 2 | 1-3 | 3 | 2-3 | 0.425 |
| 10 h | 2 | 2-3 | 3 | 2-4 | 0.023* |
| 12 h | 2 | 2-3 | 3 | 2-4 | 0.159 |
| 14 h | 3 | 2-4 | 4 | 3-5 | 0.125 |
| 16 h | 2 | 2-3 | 3 | 3-5 | 0.088 |
| 18 h | 3 | 2-4 | 4 | 3-4 | 0.148 |
| 20 h | 2 | 1-3 | 3 | 2-4 | 0.221 |
| 22 h | 3 | 2-4 | 4 | 3-5 | 0.231 |
| 24 h | 3 | 2-4 | 4 | 3-4 | 0.202 |
*Post-operative NRS-R were significantly prolonged in ultrasound guided pectoral nerve block group at 2 h, 4 h, 6 h and 10 h in comparison to thoracic paravertebral block group (P=0.002, 0.035, 0.007 and 0.023). (NRS-R=Numeric rating score - rest)
Table 4.
Comparison of post-operative NRS-M
| Time | Group P (n=20) | Group T (n=20) | P | ||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| 0 h | 3 | 3-4 | 5 | 4-6 | 0.147 |
| 2 h | 4 | 3-4 | 5 | 4-6 | 0.0007* |
| 4 h | 2 | 1-2 | 3 | 2-3 | 0.0007* |
| 6 h | 3 | 2-4 | 4 | 3-5 | 0.017* |
| 8 h | 3 | 3-5 | 4 | 3-5 | 0.458 |
| 10 h | 3 | 2-3 | 5 | 4-6 | 0.0001* |
| 12 h | 4 | 3-5 | 5 | 4-6 | 0.343 |
| 14 h | 5 | 4-5 | 6 | 5-7 | 0.073 |
| 16 h | 6 | 5-7 | 7 | 6-8 | 0.513 |
| 18 h | 4 | 3-5 | 5 | 4-6 | 0.256 |
| 20 h | 5 | 4-6 | 6 | 5-7 | 0.089 |
| 22 h | 3 | 2-4 | 4 | 3-5 | 0.267 |
| 24 h | 4 | 3-5 | 5 | 4-6 | 0.084 |
*Post-operative NRS-M were significantly prolonged in ultrasound guided pectoral nerve block group at 2 h, 4 h, 6 h and 10 h (P=0.0007, 0.0007, 0.017 and 0.0001) in comparison to thoracic paravertebral block group. Numeric rating score at movement (NRS-M)
In group P, one patient complained of pruritus and one of nausea, whereas in group T, one patient had hypotension and one had sedation; but result was statistically not significant (P = 0.66). Block-related complications, such as pneumothorax, vascular puncture, or LA toxicity was not seen in either of the group. The patient's satisfaction score was more in group P patient then group T patients but difference was not statistically significant (P = 0.07) [Figure 2].
Figure 2.
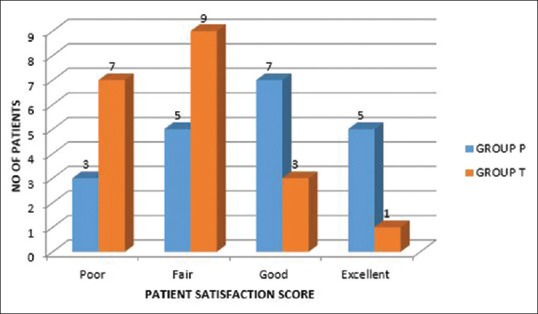
Patient satisfaction score between two groups
Discussion
Management of postoperative pain is important for early mobilization and well-being of the patient. Paravertebral block became the gold standard techniques to achieve this goal. Inadequately control of pain in axilla and higher incidences of complications have been reported with TPVB.[5,6] PecS II block is a new approach, which aims to block the lateral and medial pectoral, the intercostobrachial, the intercostals II, III, IV, V, VI and the long thoracic nerves, needed for providing complete analgesia during and postoperatively after breast surgery.[7,8] The previous studies[9,10] have reported that PecS II block provides better analgesia with various LA agents as compared to TPVB. But to the best of our knowledge, no clinical studies have compared the analgesic efficacy of PecS II and TPVB with LA and dexamethasone mixture.
This prospective, randomized trial was conducted to compare the analgesic efficacy and safety of the PecS II block with TPVB in patients undergoing MRM by using 24 ml of 0.25% levobupivacaine + 1 ml (4 mg) dexamethasone. This study demonstrated that patients receiving PecS II block had significantly prolonged duration of analgesia with less requirement of rescue analgesia [Table 2]. During the 24 h postoperative period, there was a 25% reduction in total morphine consumption in PecS II block group compared with TPVB group.
A study by Kulhari et al.[9] reported prolonged duration of first rescue analgesia after breast surgeries in patients receiving PecS II block compared to TPVB (294.5 ± 52.76 versus 197.5 ± 31.35 min, respectively; P < 0.0001). Wahba and Kamal[10] also performed similar study with levobupivacaine without any additive and concluded that duration of analgesia was significantly longer in the PecS group [175 (155–220) min] than in the PVB group [137.5 (115–165) min], (P < 0.001), while study by El-Sheikh et al.[11] compared between PecS II group and TPVB group, and found no significant difference in time to first rescue analgesic, postoperative 24 h morphine consumption, and first rescue analgesia. Syal and Chandel[12] compared the postoperative analgesic effect of paravertebral block, pectoral nerve block, and local infiltration in patients undergoing MRM. They found that mean duration of analgesia (duration to first analgesic requirement) was found to be significantly prolonged in group 2 (PVB) (639.0 ± 79.6 min) compared to group 3 (PEC) (466.5 ± 37.0 min) and group 1 (LA) (268.5 ± 35.7 min) (P < 0.001). The results of our study were not in accordance to this study. Syal and Chandel[12] compared paravertebral block, pectoral nerve block, and wound infiltration in patients undergoing MRM. The postoperative VAS was lower in TPVB group compared with other two modalities (P < 0.05). Mean duration of analgesia was significantly prolonged in the TPVB group (P < 0,001) with lesser rescue analgesic consumption up to 24 h. The prolonged duration of analgesia in Syal and Chandel[12] study in TPVB compared to PEC and local infiltration may be because they used 0.5% bupivacaine with 1:10,000 adrenaline in TPVB, less volume of drugs in PecS II block, or may be because of relative containment of paravertebral space limiting diffusion and prolonged afferent blockade. Hetta and Rezk[13] compared PecS II block versus TPVB for unilateral mastectomy with axillary dissection using single-shot bupivacaine 0.25%. According to them postoperative morphine consumption was lower in the TPVB group (12 mg versus 20 mg) than in PecS II group, and time to request for morphine was 11 (9–13) h in the TPVB group compared to 6 (5–7) h in PecS II group (P < 0.001). Thoracic epidural produced dense block from T2 to T6 spinal nerves, intercostal nerves, and all lateral and anterior cutaneous branches. However, it spares the lateral and medial pectoral nerves leading to inadequate analgesia.
In the study by Kulhari et al.,[9] none of the patients required additional fentanyl during the intraoperative period, whereas in the study by Wahba and Kamal[10] intraoperative fentanyl consumption was significantly lower in PecS group [105 (95–110) μg] compared with TPVB group [127.5 (110–145) μg] (P < 0.001).
In our study total dose of morphine consumption in 24 h in group P was less compared to group T [Table 2]. The results of the study by Kulhari et al.[9] found that 24 h morphine consumption was also less in the PecS II block group compared to TPVB group (3.90 ± 0.79 mg versus 5.30 ± 0.98 mg; P < 0.0001). In Wahba and Kamal[10] study morphine consumption at 24 h was significantly lower in PecS group [21 (20–25) mg] in comparison with TPVB group [28 (22–31) mg], (P = 0.002). Similarly, Bashandy and Abbas[14] compared quality of analgesia after MRM surgery using general anesthesia and PecS II blocks versus general anesthesia alone. They reported that postoperative morphine consumption in the PECS group (2.9 ± 1.714 mg) was lower in the first 12 h after surgery than in the control group (6.9 ± 1.861 mg) (P < 0.001).
In our study postoperative NRS-R and NRS-M scores were higher in group T in comparison to group P [Tables 3 and 4]. Statistically significant result was found at 2, 4, 6, and 10 h, which was lower in group P in comparison to group T. The results obtained in our study were in consistent with Kulhari et al.[9] study, where postoperative pain scores were lower in the PecS II group compared with the TVPB group in the initial 2 h after surgery [median (IQR), 2 (2–2.5) versus 4 (3–4), respectively; P < 0.0001]. In Wahba and Kamal[10] NRS at rest was significantly lower in the PecS II group than in the TPVB group at 1, 6, and 12 h (P < 0.001), but at 18 and 24 h it was lower in the TPVB group compared with the PecS group (P = 0.008 and < 0.001), while at 18 and 24 h, it was significantly lower in the TPVB group (P < 0.001). El-Sheikh et al.[11] found significant difference in VAS in postanesthetic care unit (P = 0.003) and VAS before discharge between the two groups (P = 0.018). Our result was inconsistent with Syal and Chandel[12] who found that the postoperative VAS scores were lower in the TPVB group compared with other groups at 0, 2, 4, 12, and 24 h (P < 0.05).
Advantages of PecS II block when compared to TPVB include less chance of complications such as pneumothorax, hypotension, Horner's syndrome, respiratory depression, nerve injury, short-segment contralateral block, vascular puncture, and failure rate as well.[15] In our study in group P, one patient complained of pruritus and one of nausea, whereas in group T, one patient had hypotension and one had sedation but the result was statistically not significant. Block-related complications, such as pneumothorax, vascular puncture, or LA toxicity, were not seen in either of the groups. In the El-Sheikh et al.[11] study, the incidence of nausea and vomiting in PecS II was 10%, while 19% in TPVB groups; and in two patients pneumothorax was found, which was statistically significant (P = 0.002).
The patient's satisfaction score was better in the PecS II group compared to TPVB, due to prolonged duration of analgesia, less need of rescue analgesia dose, less NRS score at rest and movement, and less side effect of morphine such as nausea and vomiting, but the difference was not statistically significant. However, in the study by Wahba and Kamal,[10] patient's satisfaction for postoperative analgesia was comparable in both the groups.
Limitations of the study
In this study we did not insert a catheter to prolong the analgesic effect of LA to avoid patient discomfort and complications such as epidural migration or pleural puncture in both groups. Another limitation of this study was that study population was small to draw a definitive conclusion about complications.
Conclusion
The addition of dexamethasone with levobupivacaine 0.25% in PecS II block is a more effective, safe, and alternative technique of TPVB, in terms of better pain relief for longer duration of analgesia, low pain scores, and less total morphine consumption in 24 h postoperative period and greater patient satisfaction after unilateral MRM surgery with axillary dissection.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Jaffe SM, Campbell P, Bellman M, Baildam A. Post operative nausea and vomiting in women following breast surgery: An audit. Eur J Anaesthesiol. 2000;17:261–4. doi: 10.1046/j.1365-2346.2000.00637.x. [DOI] [PubMed] [Google Scholar]
- 2.Poleshuck EL, Katz J, Andrus CH, Hogan LA, Jung BF, Dworkin RH. Risk factors for chronic pain following breast cancer surgery: A prospective study. J Pain. 2006;7:626–34. doi: 10.1016/j.jpain.2006.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gärtner R, Jensen MB, Nielsen J, Ewertz M, Kroman N, Kehlet H. Prevalence of and factors associated with persistent pain following breast cancer surgery. JAMA. 2009;302:1985–92. doi: 10.1001/jama.2009.1568. [DOI] [PubMed] [Google Scholar]
- 4.Bolin E.D, Harvey N.R, Wilson S.H. Current Anesthesiology Report. New York: Springer Science Media; 2015. Regional anaesthesia techniques and benefits. [Google Scholar]
- 5.Moller JF, Nikolajsen L, Rodt SA, Ronning H, Carlsson PS. Thoracic paravertebral block for breast cancer surgery: A randomized double-blind study. Anesth Analg. 2007;105:1848–51. doi: 10.1213/01.ane.0000286135.21333.fd. [DOI] [PubMed] [Google Scholar]
- 6.Schnabel A, Reichl SU, Kranke P, Pogatzki-Zahn EM, Zahn PK. Efficacy and safety of paravertebral blocks in breast surgery: A meta-analysis of randomized controlled trials. Br J Anaesth. 2010;105:842–52. doi: 10.1093/bja/aeq265. [DOI] [PubMed] [Google Scholar]
- 7.Blanco R. The pecs block: A novel technique for providing analgesia after breast surgery. Anaesthesia. 2011;66:847–8. doi: 10.1111/j.1365-2044.2011.06838.x. [DOI] [PubMed] [Google Scholar]
- 8.Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of PecS II (Modified PecS I): A novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012;59:470–5. doi: 10.1016/j.redar.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 9.Kulhari S, Bharti N, Bala I, Arora S, Singh G. Efficacy of pectoral nerve block v/s TPVB for postoperative analgesia after radical mastectomy, randomized controlled trial. Br J Anaesth. 2016;117:382–6. doi: 10.1093/bja/aew223. [DOI] [PubMed] [Google Scholar]
- 10.Wahba SS, Kamal SM. Thoracic paravertebral block versus pectoral nerve block for analgesia after breast surgery. Egypt J Anaesth. 2013;30:129–35. [Google Scholar]
- 11.El-Sheikh SM, Fouad A, Bashandy GM, Al-Azzb MA, Gamal RA. Ultrasound guided modified pectoral nerves block versus thoracic paravertebral block for perioperative analgesia in major breast surgery. Med J Cairo Univ. 2016;84:189–95. [Google Scholar]
- 12.Syal K, Chandel A. Comparison of the post-operative analgesic effect of paravertebral block, pectoral nerve block and local infiltration in patients undergoing modified radical mastectomy: A randomized double-blind trial. Indian J Anaesth. 2017;61:643–8. doi: 10.4103/ija.IJA_81_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hetta DF, Rezk KM. Pectoralis serratus interfascial plane block vs. thoracic paravertebral block for unilateral radical mastectomy with axillary evacuation. J Clin Anaesth. 2016;34:91–7. doi: 10.1016/j.jclinane.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 14.Bashandy GMN, Abbas DN. Pectoral nerves I and II blocks in multimodal analgesia for breast cancer surgery: A randomized clinical trial. Reg Anesth Pain Med. 2015;40:68–74. doi: 10.1097/AAP.0000000000000163. [DOI] [PubMed] [Google Scholar]
- 15.Lönnqvist PA, Mackenzie J, Soni AK, Conacher ID. Paravertebral blockade: Failure rate and complications. Anaesthesia. 1995;50:813–5. doi: 10.1111/j.1365-2044.1995.tb06148.x. [DOI] [PubMed] [Google Scholar]


