Abstract
To avoid the complications related to thoracic epidural and paravertebral block, we performed mid-point transverse process to pleura (MTP) block in a patient with multiple rib fractures. A patient with 2nd--5th rib fractures came with complains of severe pain and difficulty in breathing. Ultrasound (US)-guided continuous MTP block was given at T4 level and 15 ml of 0.375% ropivacaine was deposited, followed by the catheter insertion at the same level. Patient reported decreased sensation from T2--T8 dermatomes and reduced VAS scores from 9/10 to 1/10 within 20 min of block insertion. Continuous MTP block is efficacious in providing thoracic analgesia and has higher safety margin as needle is inserted further away from pleura.
Keywords: Mid-point transverse process to pleura, multiple rib fractures, pain, thoracic epidural
Introduction
Rib fracture is generally associated with moderate to severe pain. Modalities used for pain relief ranges from oral administration of analgesic drugs to regional nerve blocks. The advances in regional anesthesia include numerous interfascial blocks, which differentially block the dorsal, lateral, and anterior cutaneous nerves of the thorax and abdomen. One of the most recently described technique is mid-point transverse process to pleura (MTP) block.[1] We report the use of this block in a patient suffering from extreme pain associated with multiple rib fractures.
Case Report
A 45-year-old asthmatic male patient was admitted in the emergency department with history of bull horn injury. He complained of severe pain on back and right side of chest and was unable to take deep breath and cough. His visual analogue score (VAS) for pain at rest was 9/10 despite administration of intravenous diclofenac sodium and paracetamol, for which he was referred to our department. On examination, patient had bruises and tenderness over the right lateral chest wall with paradoxical breathing and poor air entry over the right mid and lower zones. Chest X-Ray revealed fracture of 2nd-5th ribs on right side [Figure 1]. NCCT thorax was also done which showed right sided hydropneumothorax with multiple rib fractures.
Figure 1.
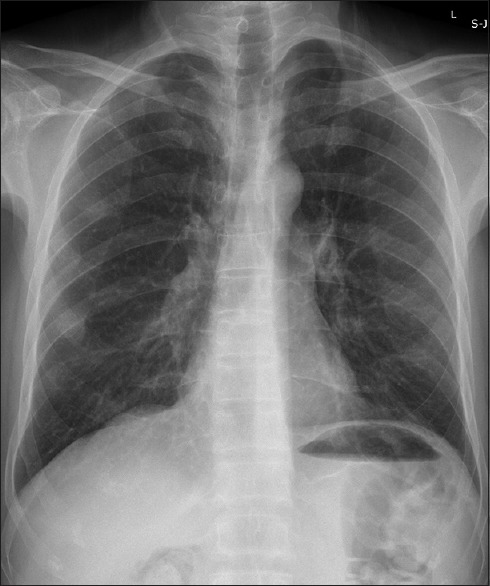
Shows the Chest X-Ray of patient
After informed consent and application of standard monitoring, a right-sided ultrasound (US)-guided (LOGIQe, GE Healthcare, China) MTP block was given at T4 level using high frequency (8--15 MHz) linear probe [Figure 2]. The transducer was placed oblique parasagittally 3 cm lateral to T4 spinous process [Figure 3]. After skin infiltration with 2% xylocaine, a 50 mm long block needle (contiplex, B BRAUN) was inserted in-plane and 15 ml of 0.375% ropivacaine was injected at the mid-point between the posterior border of the transverse process and the pleura, followed by insertion of catheter through the needle.
Figure 2.
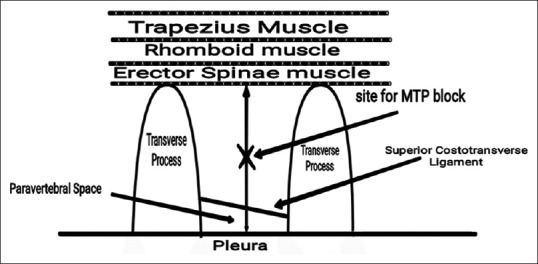
Schematic diagram showing the site of MTP block
Figure 3.

Patient in sitting position with high-frequency probe placed over the transverse process and needling from cranial to caudal direction
Sensory assessment was done with a cold swab and blunt 26-G needle tip along the posterior scapular line, midaxillary line, midclavicular line, and parasternal line at 5-min intervals for 20 min. There was decreased sensation from T2--T8 dermatomes. Twenty minutes after the block, patient was relieved from pain with VAS 1/10. A continuous infusion of 0.2% of ropivacine was started at rate of 5 ml/h, which was continued for 4 days. Patient was able to mobilise in the ward and did not require any rescue analgesia during this period. The catheter was removed after 4 days when he became comfortable and could easily be managed with mild oral analgesics.
Discussion
Rib fractures are detected in around 10% of all trauma patients and over 30% of chest trauma patients.[2] Multiple fractured ribs are associated with extreme pain, which compromises patient's ability to cough and to take deep breaths, predisposing him to numerous complications, including sputum retention, atelectasis, infection, and respiratory insufficiency. This lethal cascade is associated with increase in intensive care admissions and mortality (25%).[3] Hence, pain control is the cornerstone of rib fracture management.
Thoracic epidural (TE) analgesia has become the gold standard especially in patients with multilevel rib fractures, flail chest, and functional respiratory compromise. However, it has a failure rate of approximately 15%.[4] Moreover, in patients with multiple trauma, it may result in hypotension and cardiovascular collapse, especially in inadequately resuscitated patients.
Ipsilateral thoracic paravertebral block (TPVB) is a simple technique, which provides analgesia comparable to TE and is associated with minimal hemodynamic disturbance. End point of US-guided TPVB is to pierce the superior costotransverse ligament (SCTL) and injection of drug in the paravertebral space. The possible associated complications are inadvertent vascular puncture (4.6%), pleural puncture (1.1%), pneumothorax (0.5%), and inadvertent epidural or intrathecal spread.[5] Since, TPVB produces ipsilateral segmental thoracic anesthesia, it can safely be used for pain management in patients with unilateral multiple fractured ribs.
As paravertebral is not a well-defined space, local anesthetic injected outside it can still block thoracic spinal nerves. This concept has been well highlighted by few TPVB variants such as erector spinae plane (ESP),[6] retrolaminar,[7] and paraspinal[8] blocks. In ESP block, transverse processes of thoracic vertebrae are the main target structures and local anesthetic drug is injected deep to erector spinae muscle.[6] Retrolaminar block is a laminar approach of paravertebral block, where drug is administered into the space between the lamina of the thoracic vertebra and the erector spinae muscles.[7] Another variant, paraspinal block is less commonly used and involves infiltration of drug between extrathoracic fascia and paraspinal muscles.[8]
One of the recently described approach is MTP block as described by Costache et al.[1] In this, the anesthetic drug is deposited at the mid-point between the transverse process and pleura and it reaches the paravertebral space by diffusion [Figure 4]. With this technique, even if SCTL is not visible, effective block can be achieved. In addition, needle is placed far away from pleura minimizing the rate of pneumothorax. Previous studies have reported the presence of gap between medial and lateral parts of superior costal transverse ligament, the intermingling of lateral fibres with internal costal membrane and the fenestrated nature of SCTL.[9,10] These probably explain the diffusion of drug in MTP block, to reach the nerve roots in the paravertebral space. This block is reported to be successful in unilateral mastectomy and mammoplasty surgeries where drug was injected at multiple levels.[1]
Figure 4.
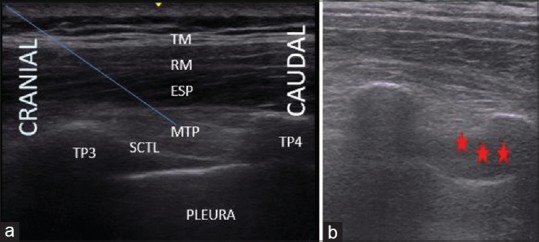
Image of US guided MTP block: Sagittal view - T3-T4 transverse process, (a) before local anesthetic (LA) deposition; arrow indicates needle direction from cranial to caudal. (b) after LA deposition ***LA spread
Local anesthetic injected in or around paravertebral space should cover 4--6 dermatomes. Therefore, we decided to insert a catheter in this case and found satisfactory analgesia with no side effects as the target point is far from the pleura than currently described techniques. To the best of our knowledge, ours is the first case report documenting the efficacy of continuous MTP catheter in a patient with multiple fractured ribs. Future larger randomized studies are needed to document the efficacy of MTP continuous catheter block in patients with multiple fractures.
Conclusion
US-guided MTP block is a safe and effective technique for providing analgesia for unilateral chest injuries, with lesser incidence of side effects.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Costache I, de Neumann L, Ramnanan CJ, Goodwin SL, Pawa A, Abdallah FW, et al. The mid-point transverse process to pleura (MTP) block: A new end-point for thoracic paravertebral block. Anaesthesia. 2017;72:1230–6. doi: 10.1111/anae.14004. [DOI] [PubMed] [Google Scholar]
- 2.Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma. 1994;37:975–9. doi: 10.1097/00005373-199412000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Karmakar MK, Critchley LA, Ho AM, Gin T, Lee TW, Yim AP. Continuous thoracic paravertebral infusion of Bupivacaine for pain management in patients with multiple fractured ribs. Chest. 2003;123:424–31. doi: 10.1378/chest.123.2.424. [DOI] [PubMed] [Google Scholar]
- 4.Yeh DD, Kutcher ME, Knudson MM, Tang JF. Epidural analgesia for blunt thoracic injury-which patients benefit most? Injury. 2012;43:1667–71. doi: 10.1016/j.injury.2012.05.022. [DOI] [PubMed] [Google Scholar]
- 5.Dittmann M, Keller R, Wolff G. A rationale for epidural analgesia in the treatment of multiple rib fractures. Intensive Care Med. 1978;4:193–7. doi: 10.1007/BF01902546. [DOI] [PubMed] [Google Scholar]
- 6.Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: A novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–7. doi: 10.1097/AAP.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 7.Murouchi T, Yamakage M. Retrolaminar block: Analgesic efficacy and safety evaluation. J Anesth. 2016;30:1003–7. doi: 10.1007/s00540-016-2230-1. [DOI] [PubMed] [Google Scholar]
- 8.Roue C, Wallaert M, Kacha M, Havet E. Intercostal/paraspinal nerve block for thoracic surgery. Anaesthesia. 2015;71:110–2. doi: 10.1111/anae.13358. [DOI] [PubMed] [Google Scholar]
- 9.Luyet C, Eichenberger U, Greif R, Vogt A, Szucs FZ, Moriggl B. Ultrasound-guided paravertebral puncture and placement of catheters in human cadavers: An imaging study. Br J Anaesth. 2009;102:534–9. doi: 10.1093/bja/aep015. [DOI] [PubMed] [Google Scholar]
- 10.Jiang H, Raso JV, Moreau MJ, Russell G, Hill D, Bagnall KM. Quantitative morphology of the lateral ligaments of the spine: Assessment of their importance in maintaining lateral stability. Spine. 1994;19:2676–82. [PubMed] [Google Scholar]


