Abstract
Purpose
Δ9-Tetrahydrocannabinol-valine-hemisuccinate, a hydrophilic prodrug of Δ9-tetrahydrocannabinol, synthesized with the aim of improving the ocular bioavailability of the parent molecule, was investigated in a lipid-based nanoparticle dosage form for ocular delivery.
Methods
Solid lipid nanoparticles (SLNs) of Δ9-tetrahydrocannabinol-valine-hemisuccinate and Δ9-tetrahydrocannabinol, along with a nanoemulsion of Δ9-tetrahydrocannabinol-valine-hemisuccinate, were tested for glaucoma management in a normotensive rabbit model by using a multiple-dosing protocol. Marketed formulations of timolol maleate and pilocarpine HCl were also tested for their pharmacodynamic profile, post-single dose administration.
Results
A peak intraocular pressure (IOP) drop of 30% from baseline was observed in rabbits treated with SLNs loaded with Δ9-tetrahydrocannabinol-valine-hemisuccinate at 90 minutes. Treated eyes of rabbits receiving Δ9-tetrahydrocannabinol-valine-hemisuccinate SLNs had significantly lower IOP than untreated eyes until 360 minutes, whereas the group receiving the emulsion formulation showed a drop in IOP until 90 minutes only. In comparison to marketed pilocarpine and timolol maleate ophthalmic solutions, Δ9-tetrahydrocannabinol-valine-hemisuccinate SLNs produced a greater effect on IOP in terms of both intensity and duration. In terms of tissue concentrations, significantly higher concentrations of Δ9-tetrahydrocannabinol-valine-hemisuccinate were observed in iris-ciliary bodies and retina-choroid with SLNs.
Conclusion
Δ9-Tetrahydrocannabinol-valine-hemisuccinate formulated in a lipid-based nanoparticulate carrier shows promise in glaucoma pharmacotherapy.
Translational Relevance
Glaucoma therapies usually focus on decreased aqueous humor production and increased outflow. However, such therapy is not curative, and there lies a need in preclinical research to focus efforts on agents that not only affect the aqueous humor dynamics but also provide neuroprotection. Historically, there have been bench-scale studies looking at retinal ganglion cell death post-axonal injury. However, for a smooth translation of this in vitro activity to the clinic, animal models examining IOP reduction, i.e., connecting the neuroprotective activity to a measurable outcome in glaucoma management (IOP), need to be investigated. This study investigated the IOP reduction efficacy of cannabinoids for glaucoma pharmacotherapy in a normotensive rabbit model, bringing forth a new class of agents with the potential of IOP reduction and improved permeation to the back of the eye, possibly providing neuroprotective benefits in glaucoma management.
Keywords: glaucoma, tetrahydrocannabinol, solid lipid nanoparticles, intraocular pressure, normotensive
Introduction
Glaucoma is a neurodegenerative disorder characterized by progressive peripheral vision loss due to structural and functional damage to the optic nerve head.1,2 The latest statistics from the World Health Organization rank glaucoma as the second leading cause of blindness, after cataracts, affecting almost 60 million people worldwide.3 The 2010 report by the National Eye Institute stated that 2.72 million people in United States suffer from glaucoma, which is 23% higher than the 2.22 million affected in the year 2000, and projects almost 6.3 million to be affected by this illness by 2050.3–6
Glaucomatous optic neuropathy is caused by several factors that result in the death of retinal ganglion cells (RGCs) and their axons. The major risk factor for glaucoma is elevated intraocular pressure (IOP), normally regulated by aqueous humor (AH) hydrodynamics in the anterior chamber.7 AH is a fluid secreted by the iris-ciliary bodies (IC).8 AH drains out via the trabecular meshwork (TM) through the canal of Schlemm into venous circulation. The ciliary muscles maintain the tension on the TM structure and control the drainage of AH. The Goldmann equation can be used to describe AH hydrodynamics,9
 |
where, Pe is the episcleral venous pressure (the pressure opposing the drainage of AH through the TM), F is the AH flow, U is the uveoscleral outflow, and Ctrab is the AH outflow from the TM and Schlemm canal.7 The balance between AH production and drainage determines IOP, wherein increased AH production or inadequate AH drainage might result in increased pressure.7,10–12 Glaucoma medications target IOP reduction by acting on the aforementioned factors, i.e., either decreasing the production of AH or increasing AH outflow through TM and through the uveoscleral pathway or both.13–15
Currently, there are five families of treatment governing the market as antiglaucoma agents,16 including adrenergic agonists, beta blockers, prostaglandin F2-α analogs, carbonic anhydrase inhibitors, and cholinergic agents. The mechanism of action of each class and examples of some Food and Drug Administration-approved agents are listed in Table 1. Current glaucoma research is directed toward finding new lines of treatment, pursuing novel mechanisms for lowering of the IOP. The recent Food and Drug Administration approvals on antiglaucoma agents Rhopressa (0.02% netarsudil), a rho-kinase inhibitor, and Vyzulta (0.024% latanoprostene bunod, made of two components, namely, latanoprost and a nitrogen oxide-donating component), are examples of drug products harnessing novel mechanisms of action for IOP reduction.17 There are several investigational treatments such as a sustained release bimatoprost implant and ocular punctal plugs of travoprost and latanoprost; however, all these approaches focus on a formulation-based approach.17 A completely new class of agents would bring forth another perspective for antiglaucoma medications.
Table 1.
Classification and Mechanisms of Action of the Currently Used Antiglaucoma Medications
|
Antiglaucoma Medications |
Mechanism of Action |
FDA-Approved Therapy |
| Prostaglandin analogs | Reduction in hydraulic resistance to uveoscleral outflow, increase in trabecular outflow facility | Xalatan (latanoprost), Lumigan (bimatoprost), Travatan Z (travoprost), Zioptan (tafluprost)16,17 |
| Beta blockers | Reduce aqueous humor production by acting on the β1 and β2 receptors | Timoptic (timolol maleate ophthalmic solution), Betagan (levobunolol hydrochloride ophthalmic solution16,17 |
| Adrenergic agonists | Increases elimination by reducing episcleral venous pressure, increasing uveoscleral outflow by increasing prostaglandin synthesis | Alphagan-P (brimonidine), Iopidine (apraclonidine hydrochloride, ophthalmic solution)16,17 |
| Carbonic anhydrase inhibitors | Inhibit the enzyme carbonic anhydrase, reduce production of aqueous humor | Trusopt (dorzolamide), Azopt (brinzolamide)16,17 |
| Cholinergic agents | Increases aqueous humor outflow by contracting longitudinal fibers in of the ciliary muscles | Isopto Carpine (pilocarpine hydrochloride ophthalmic solution)16,17 |
FDA, Food and Drug Administration.
Cannabinoids have been investigated for the past few decades for their IOP-lowering capacity. Cannabinoids utilize several unique mechanisms for IOP reduction. There are reports suggesting that IOP reduction occurs due to decreased AH production, a result of curtailed release of noradrenaline in ocular tissues.18 Δ9-Tetrahydrocannabinol (THC) (Fig. 1) is an example of a cannabinoid that favors the opening of the endothelial-lined Schlemm's channels draining the AH.18–23 Another suggested mechanism involves the CB1 receptors in IOP reduction. Human ciliary bodies are rich in CB1 mRNA and functional protein, supporting the hypothesis that cannabinoids such as THC, through their action on CB1 receptors, may act directly as vasodilators of the efferent blood vessels of the anterior uvea, favoring AH efflux.24,25 Considering the pathophysiology of glaucoma, along with increased IOP, there is also a neurodegenerative component to the disease. Increased IOP produces early injury in glaucomatous optic atrophy, resulting in structural changes in the lamina cribrosa, a membrane through which the RGC axons pass before condensing to form the optic nerve.26–28 Moreover, the overproduction of free radicals, such as nitric oxide, results in an excessive release of glutamate, which, by activating N-methyl-D-aspartate receptors, results in apoptotic ganglionic cell death.29–31 Findings suggest that THC can inhibit glutamic acid release by increasing K+ and decreasing Ca2+ permeability.30,32,33 It also exhibits antioxidant properties and prevents neuronal cell death by reactive oxygen species scavenging action.22,34 Reportedly, in an animal glaucoma model, treatment with THC for 20 weeks decreased IOP and reduced death of RGCs by approximately 75%.35 This effect of THC on the RGC provides the molecule with an added advantage of not only IOP reduction but also neuroprotection.22,36
Figure 1.
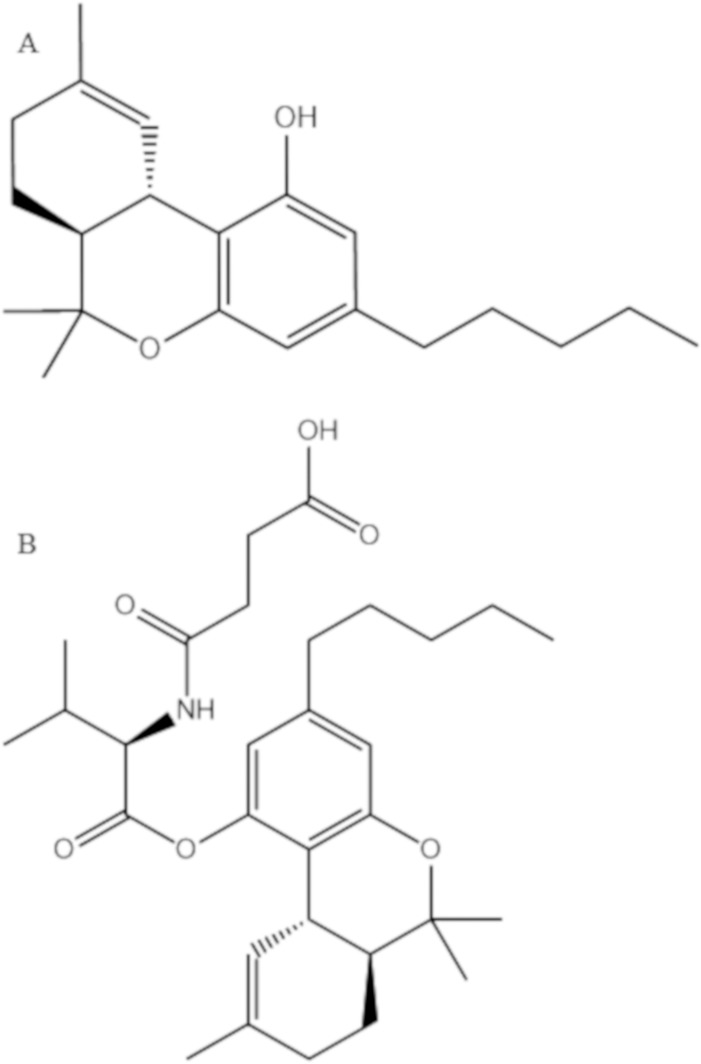
Chemical structures of (A) Δ9-tetrahydrocannabinol and (B) Δ9-tetrahydrocannabinol valine hemisuccinate (THC-VHS).
Hepler and Frank37 reported about a 25% to 30% drop in IOP after smoking marijuana, in a small number of subjects with a duration of action of 3 to 4 hours.38 Crawford and Merritt39 in the late 1970s conducted clinical studies to determine a relationship between changes in heart rate, blood pressure, IOP in normotensive (n = 8) and hypertensive volunteers (n = 8), and also patients diagnosed with open-angle glaucoma (n = 16), and they observed decreased IOP (6–21 mm of Hg lower than control) along with intense cardiovascular effects. Overall, it has been observed that smoking marijuana is accompanied with a drop in both systolic pressure as well as IOP; however, cardiovascular effects, such as tachycardia and postural hypotension, outweigh the IOP-lowering effects, giving rise to the need of investigating the effect of topical application of THC on lowering IOP.38,39 A number of studies examined the topical administration of THC formulated in various oily vehicles.40–43 However, for THC to show both an IOP-reducing and a neuroprotective effect, it is important for it to permeate through the outer layers of the eye to target tissues in the anterior and posterior compartments.24,44 Previously, a prodrug approach was devised aiming to improve the ocular bioavailability of THC.45,46 Adelli et al.4 evaluated the pharmacokinetic and pharmacodynamic (PK-PD) efficacy of a hydrophilic prodrug of THC, Δ9-THC-valine-hemisuccinate (THC-VHS) (Fig. 1) in an elevated IOP model. THC-VHS demonstrated a better permeation profile in comparison to THC, penetrating to the IC and retina choroid (RC), and displayed a corresponding IOP drop for about 180 minutes.47
To understand the IOP-lowering mechanisms of THC-VHS in an intact eye with all the production and drainage mechanisms unimpaired, a normotensive IOP model was opted for in the current set of studies. The goals of this project were to formulate a lipid-based vehicle, solid lipid nanoparticles (SLNs), to improve the delivery of the prodrug THC-VHS to the target tissues. SLNs have been reported to enhance ocular bioavailability by prolonging the residence time of the formulation in the cul de sac, forming a lipid-based drug reservoir interacting with the ocular mucosa.48
The formulation was characterized in terms of drug content (% w/v), particle size (d.nm), polydispersity index (PDI), and scanning transmission electron microscopy (STEM). The stability of the formulations in terms of particle size growth under different storage conditions was investigated. A comparative PK-PD profile of the THC-VHS-SLN formulations was established after single and multiple topical applications in a normotensive rabbit model. The PK-PD profile of THC-VHS-SLN was compared to that of THC-VHS formulated in a soybean oil-based emulsion and THC-SLN to delineate the effect of prodrug derivatization and the effect of vehicle in improving ocular bioavailability. IOP-lowering efficacy (PD profile) of the formulations was also compared against marketed ophthalmic formulations of pilocarpine and timolol maleate in the same model (single dose).
Materials
THC-VHS was synthesized by ElSohly Laboratories, Inc., according to previously established protocols.49 Compritol 888 ATO (glyceryl behenate) was obtained as a gift sample from Gattefossé (Paramus, NJ), glycerin was purchased from Acros Organics (NJ), Pluronic F68 (poloxamer 188) was purchased from Spectrum Pharmaceuticals (Henderson, NV), Tween 80 was received as a gift sample from Croda, Inc., (Mill Hall, PA), and Tocrisolve 100 was purchased from Tocris Biosciences (Bristol, UK). High-performance liquid chromatography (HPLC)-grade solvents and other chemicals (analytical grade) were obtained from Fisher Scientific (Hampton, NH). Amicon Ultra centrifugal filter devices, namely, regenerated cellulose membranes (MWCO 100 kDa), were purchased from EMD Millipore (Billerica, MA). Formalin was purchased from Thermo Scientific (Waltham, MA). Timolol maleate eye drops (0.25% w/v) and pilocarpine HCl eye drops (2% w/v) are commercially available formulations obtained from The University of Mississippi Health Center.
Animals
Male New Zealand White (NZW) rabbits (2–2.5 kg), obtained from Harlan Laboratories (Indianapolis, IN), were used in all studies. All animal experiments conformed to the Association for Research in Vision and Ophthalmology statement “Use of Animals in Ophthalmic and Vision Research” and followed the University of Mississippi Institutional Animal Care and Use Committee approved protocols.
Development of SLNs and Emulsion
THC-VHS-SLNs and THC-SLNs
THC-VHS- or THC-loaded SLNs were prepared by the ultra-sonication technique. Compritol 888 ATO constituted the lipid phase of the SLNs. THC-VHS (equivalent to 0.6% w/v of THC) and 0.6% w/v of THC was mixed with Compritol 888 ATO to obtain a clear lipid phase. The aqueous phase comprising of Pluronic F-68 (0.25% w/v), Tween 80 (0.75% w/v), and glycerin (2.25% w/v) was simultaneously heated in bidistilled water. The hot aqueous phase was added to the melted lipid phase under constant stirring. A coarse emulsion from this premix was formed by emulsification at 11,000 rpm for 5 minutes by using a T 25 digital Ultra-Turrax instrument. This coarse emulsion was subjected to ultrasonification using SONICS Vibra-Cell Ultrasonic Liquid Processor by using previously optimized parameters (amplitude: 40%; pulse on: 10 seconds, pulse off: 15 seconds; time: 10 minutes). The temperature during this entire process was maintained at 70°C. The hot emulsion was slowly cooled to room temperature to form THC-VHS or THC SLNs.
THC-VHS and THC Emulsion
THC-VHS and THC emulsion were prepared by dispersing a weighed amount of THC (0.6% w/v) or THC-VHS (0.98% w/v, equivalent to 0.6% w/v THC) in the Tocrisolve emulsion vehicle (THC-TOC and THC-VHS-TOC), a soya-bean oil emulsion composed of a 1:4 ratio of soya oil/water, purchased from Tocris Bioscience. Tocrisolve is a water-soluble emulsion used for formulating hydrophobic moieties such as cannabinoids. The soybean oil solubilizes the cannabinoid molecule, and the emulsion is stabilized by the block copolymer Pluronic-F68, preventing the lipid droplets from coalescing in the dispersion. This mixture was vortexed for 5 minutes on Ultra Cylone and sonicated for 10 minutes.
Formulation Characterization
Drug Content
To determine the drug content in the SLNs and the emulsion, the lipid/oil was precipitated using ethanol. An accurately measured volume of the formulation was extracted in 1 mL ethanol, and this suspension was centrifuged at 13,000 rpm for 15 minutes. The drug content in the supernatant was analyzed using the following HPLC-ultraviolet method.
In Vitro Sample Analysis
The samples were analyzed for THC and THC-VHS by using an HPLC-ultraviolet system comprising a Waters 717 plus Autosampler, Waters 600E pump controller, Waters 2487 dual λ absorbance detector, and an Agilent 3395 integrator. Stock solutions of THC-VHS and THC were prepared in acetonitrile and used immediately. A mobile phase consisting of 60:40 (acetonitrile:water) with 0.1% glacial acetic acid was used on a Phenomenex C18 (4.6 × 250 mm) column at a flow rate of 1 mL/min. Detection was carried out at 226 nm.
Particle Size and PDI
The mean particle size and the PDI of the THC-VHS-SLN, THC-SLN, and THC-VHS-TOC formulations were determined by the Dynamic Light Scattering technique using the Zetasizer Nano ZS Zen3600 (Malvern Instruments, Inc., Malvern, UK) at 25°C and 173° detection optics by using the Non-Invasive-Back-Scatter technology. The cells used were disposable folded capillary clear cells. The measurements were obtained using a helium-neon laser of 633nm, and the particle-size analysis data were evaluated using intensity distributions. To measure the particle size distribution, the samples were diluted (1:500) with bidistilled water filtered using 0.2-micron filters.
STEM Studies
A negative staining procedure was used to conduct the STEM studies. THC-VHS-SLNs were characterized by a scanning transmission electron microscope Zeiss Auriga-40 dual beam by using 1% w/v uranyl acetate as a stain. Twenty microliters of the sample was placed on a piece of parafilm, and a glow discharged 200 mesh copper grid with a thin carbon film was floated on the top of the sample (film side down) for 30 seconds. After taking the grid off the drop, the excess sample was blotted using a piece of filter paper. The grid was then floated on a drop of distilled water for a couple of seconds. Once the excess water was removed, the grid, sample side down, was floated on a drop of 1% uranyl acetate for 1 minute. After blotting and drying, the samples were imaged in a Zeiss Libra operating at 30 kV and in STEM mode.
Physical and Chemical Stability
THC-VHS-SLNs were evaluated for changes in % drug content, particle size, and PDI on storage at conditions of 40°C/60% relative humidity (RH), 25°C/75% RH, and 4°C.
Corneal Histology
Six NZW rabbits were used for comparison of corneal histology after treatment with placebo-SLNs or with isotonic phosphate buffer saline (IPBS) as the control (n = 3). The placebo-SLNs were topically administered to the eye of normotensive NZW rabbits to observe the effect of the vehicle on the histological characteristics of the cornea. Rabbit corneas dosed with IPBS, under similar experimental conditions, were used as controls. The study was conducted for 120 minutes, after which the animals were euthanized, and the corneas were excised. Extracted corneas were fixed in 10% neutral buffered Formalin. Histological evaluation was carried out at Excalibur Pathology Inc. (Oklahoma City, OK) as per previously reported protocols. Corneas embedded in paraffin were sliced into 5-μm cross sections by using a microtome (American Optical 820 Rotary Microtome). These sections were placed on a slide and dried overnight in an oven at 68°C. The slide was washed with xylene to remove paraffin and washed with alcohol and water to hydrate the tissue. This was then stained with nuclear dye Gill III hematoxylin (StatLab Medical, McKinney, TX) for 10 min and rinsed and then counterstained with eosin. These slides were then washed in reverse manner (running water, alcohol, and xylene), cover slipped, and examined under a microscope (Chroma Vision ACIS II).
Efficacy Studies
Multiple-Dose Studies
The rabbits were acclimatized to the environment, personnel, and IOP measurements by using a Tono-Pen Vet (Reichert Technologies, Depew, NY) for a period of 2 to 3 weeks. The formulations THC-VHS-SLNs, THC-VHS-TOC, and THC-SLNs were dosed topically, conforming to a predetermined multiple-dosing protocol in 18 NZW rabbits (n = 6). Fifty microliters of SLNs or nanoemulsion (in Tocrisolve) was instilled topically in the cul de sac of the left eye of normotensive rabbits, twice a day, for 5 consecutive days. The right eye served as the control. To avoid spillage, the eyelid was closed for 10 seconds. On day 1, for the single-dose IOP-time profiling, IOP was measured before (baseline IOP), and every 30 minutes after administration until IOP returned to 90% of the baseline. From day 2 onward, the IOP was measured before (baseline) and 60 to 90 minutes after administration of the dose. The IOP value displayed by the Tono-Pen Vet was an average of five concurrent IOP measurements, and each time point was measured in triplicate. The decrease in IOP was recorded as a function of single dose and multiple dosing, that is an intraday as well as an interday IOP trend was monitored. On day 5, IOP-time profiling was done similar to day 1. On day 6, the animals were sacrificed at two time points: the first time point, which showed the lowest drop in IOP on day 5, and the second time point right before the IOP returned to 90% IOP from the baseline.
Eye Dissection and Tissue Collection
At the time points mentioned before, the rabbits were administered ketamine (35 mg/kg) and xylazine (3.5 mg/kg) intramuscularly and euthanized under anesthesia with an overdose of pentobarbital administered through the marginal ear vein. The eyes were immediately enucleated after washing with ice-cold isotonic phosphate-buffered saline. Enucleated eyeballs were then dissected and the AH, vitreous humor (VH), IC, and RC tissues were collected. All samples were weighed and stored at −80°C until further processing.
Bioanalytical Methods for Quantification
An AB Sciex QTrap 4500 (Framingham, MA) liquid chromatography-tandem mass spectrometry quadrupole interfaced with Shimadzu Nexera HPLC (Kyoto, Japan) was used to analyze both the THC and THC-VHS content. Calibration curves were prepared by spiking THC and THC-VHS into blank ocular tissues along with the internal standard D3-THC. The tissues analyzed were AH, VH, IC, RC, and plasma. Protein precipitation took place after the addition of ice-cold acetonitrile, followed by extraction of THC and THC-VHS. The samples were vortexed and then centrifuged at 13,000 rpm for 30 minutes. The supernatant was filtered through a 0.2-μm filter, and the filtrate was analyzed for THC and THC-VHS content. The calibration curves were prepared with both THC and THC-VHS in AH (2.5–100 ng/mL), VH (2.5–100 ng/mL), IC (2.5–100 ng/mL), RC (2.5–100 ng/mL), and plasma (2.5–100 ng/mL). Tissues collected from the multiple-dosing studies were also prepared per this protocol. A Phenomenex Synergi Hydro Reverse Phase, 100 A, 50 × 3-mm, 2.5-μm column was used with a gradient elution method; the solvent phase was composed of water and acetonitrile with 0.1% w/v formic acid.
Single-Dose Studies
Single-dose IOP-lowering efficacy studies were conducted with the marketed ophthalmic formulations of timolol maleate (0.25% w/v) and pilocarpine HCl (2% w/v) in NZW rabbits (n = 4). Fifty microliters of each test formulation was instilled into the lower cul de sac of the left eye of the rabbits, while the right eye acted as the control. The eyelids were closed after the instillation for 10 seconds to avoid spillage. IOP was measured before instillation (baseline IOP) and every 30 minutes postinstillation until the IOP returned to 90% of baseline IOP. The drop in IOP was also expressed as ΔIOP or percent baseline IOP (± SEM), that is (measured IOP/baseline IOP) × 100.
Statistical Analysis
To assess the effect of formulation on change in IOP over time, a repeated measures model was used. Between and within group differences were modeled using the proc mixed procedure with treatment, time and interaction of treatment and time as independent factors in the model. A two-tailed P value of ≤0.05 was considered statistically significant. Data analysis was conducted using Statistical Analysis System 9.4 software (SAS Institute, Cary, NC). A P value of less than 0.05 was considered statistically significant.
Results
Formulation Characterization
A detailed description of the compositions of these formulations has been listed in Table 2.
Table 2.
Optimized Composition of THC-VHS-SLN, THC-VHS-TOC, and THC-SLN Formulations
|
Ingredients |
THC-VHS-SLN, % w/v |
THC-VHS-TOC, % w/v |
THC-SLN, % w/v |
| Compritol 888 ATO | 3 | - | 3 |
| Glycerin | 2.25 | - | 2.25 |
| Poloxamer 188 | 0.25 | - | 0.25 |
| THC | - | - | 0.6 |
| THC-VHS (0.6% THC equivalent) | 0.98 | 0.98 | - |
| Tocrisolve emulsion | - | Q.S | - |
| Tween 80 | 0.75 | - | 0.75 |
| Water, HPLC grade | Q.S | - | Q.S |
Q.S, quantum sufficit.
The homogenization-ultrasonication process yielded SLNs with hydrodynamic radii less than 300 d.nm and a narrow distribution range. However, their particle size was slightly greater than that of Tocrisolve emulsion. Tocris Bioscience reports the mean droplet size of the emulsion as 182 nm, and our investigated values for THC-VHS-TOC particle size fall along similar lines (189.75 ± 22.7 d.nm). The physicochemical properties of the test formulations are listed in Table 3. A narrow PDI suggests no aggregation/coalescence of the nanocolloidal formulations.
Table 3.
Particle Size, PDI, and Drug Content of Test Formulations THC-VHS-SLN, THC-VHS-TOC, and THC-SLN
|
Formulation |
Particle Size, d.nm |
PDI |
Drug Content, % w/v |
| THC-VHS-SLN, mean ± SD | 287.80 ± 7.35 | 0.29 ± 0.01 | 93.57 ± 4.68 |
| THC-VHS-TOC, mean ± SD | 189.75 ± 22.7 | 0.15 ± 0.06 | 87.74 ± 3.6 |
| THC-SLN, mean ± SD | 269.2 ± 5.66 | 0.32 ± 0.15 | 96.84 ± 0.02 |
STEM Studies
Morphological characteristics of THC-VHS-SLNs were studied using STEM (Fig. 2). STEM technique images samples based on absorption of an electron beam as it passes through an ultra-thin layer of sample. The transmitted beam is then projected on a phosphorescent screen or detector, providing us with information regarding the morphological characteristics of the particles as well as the hydrodynamic radius. The electron microscopy pictures at different magnifications (Fig. 2) show the presence of spherical nanoparticles with a smooth, well-defined periphery.
Figure 2.
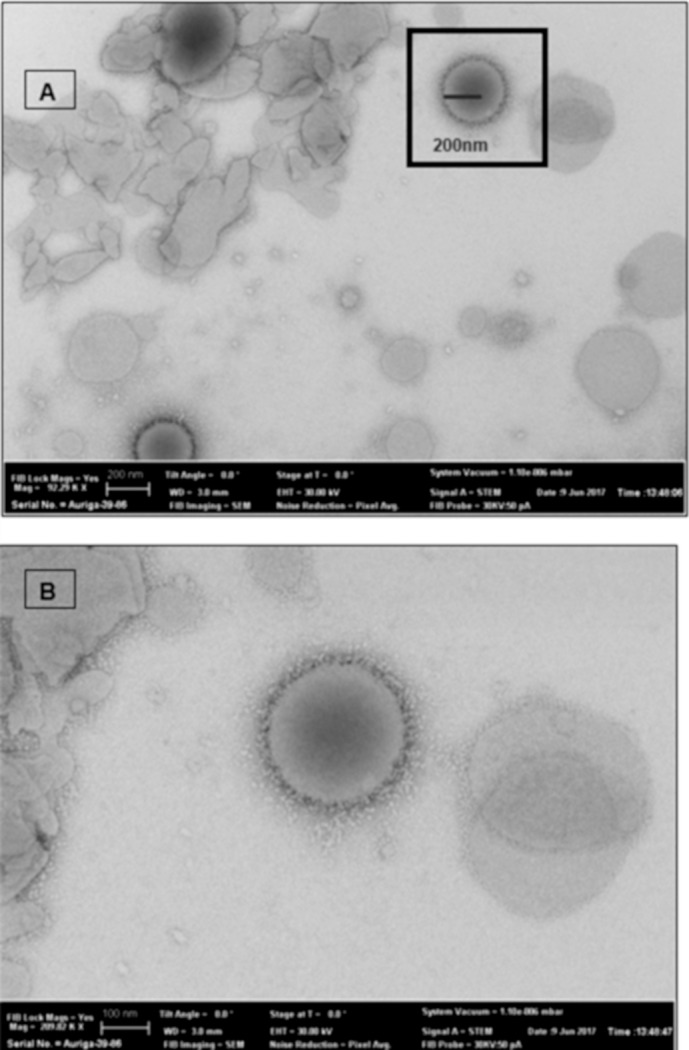
STEM images of THC-VHS-SLN at (A) 92.29 KX and (B) 209.82 KX magnification.
Physical and Chemical Stability
The particle size and PDI of THC-VHS-SLNs was observed for 6 months at 40°C/60% RH 25°C/75% RH, and 4°C. The formulations were stable over a period of 6 months at both 4°C and 25°C, with particle size remaining around 200 to 300 d.nm and a PDI of 0.3 (Fig. 3).50 However, after 1 month at 40°C, a 95% increase in particle size was observed from the original diameter of 248.9 nm and a PDI of 0.4. In terms of drug content, the THC-VHS-SLN was stable with a change in drug content of ±1.5% when stored at 4°C and 25°C over a period of 23 days (the last timepoint checked).
Figure 3.
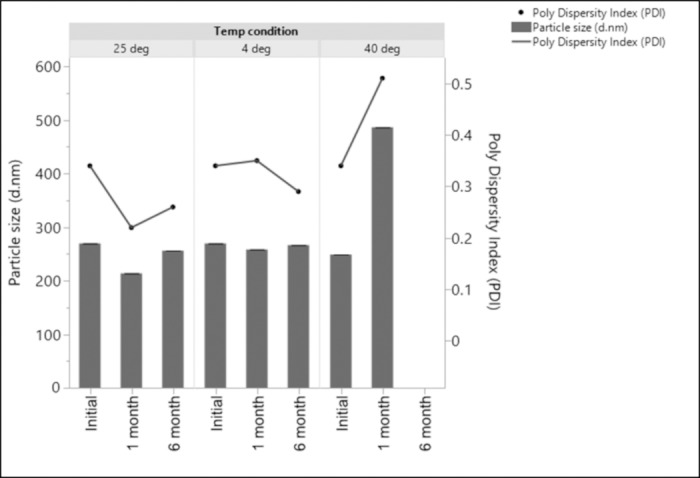
Particle size and polydispersity index of THC-VHS-SLNs stored at conditions of 40°C/60% RH, 25°C/75% RH, and 4°C over a period of 6 months.
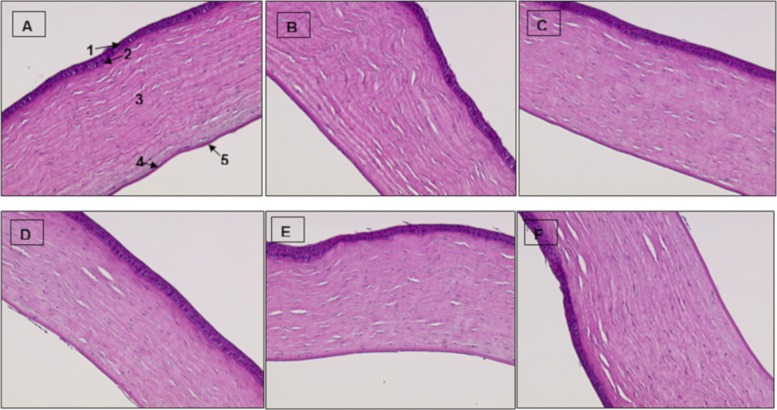
Corneal Histology
To observe the effect of formulation on the corneal histology, cross sections of rabbit corneas treated with placebo-SLNs (Figs. 4A, 4B, 4C) and IPBS (control) were studied (Figs. 4D, 4E, 4F). The cornea is composed of five membranes, namely, the corneal stratified squamous epithelium (1), Bowman's membrane (2), stroma consisting of collagen fibers and keratocytes (3), Descemet's membrane (4), and the endothelium (5), as marked in Figure 4A. The corneal epithelium of all the rabbits treated with control or placebo-SLNs looked intact and attached to the Bowman's membrane, without any signs of edema.
Figure 4.
Histological sections of rabbit corneas (magnification, 10×) excised from NZW rabbits (n = 3) treated with placebo-SLNs (A, B, C) and IPBS (control) (D, E, F) 120 minutes after application.
Efficacy Studies
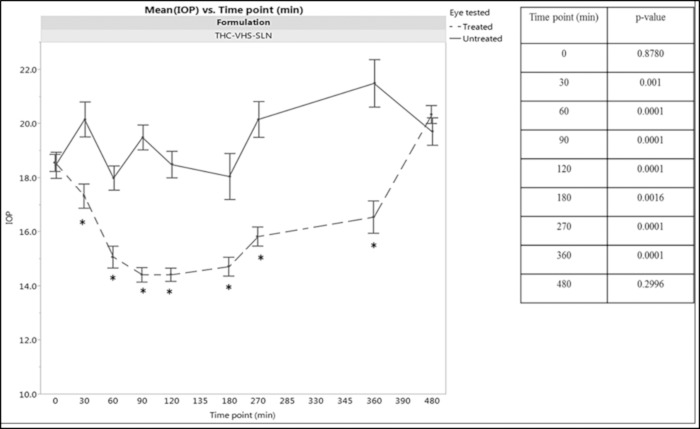
Multiple-Dosing Regimen for THC-VHS-SLN
It has been previously reported that THC fails to lower the IOP of normotensive rabbits. The data obtained on normotensive rabbits for studies with THC-VHS-SLN formulations show a significant IOP-lowering effect by THC-VHS when formulated in SLNs. Figure 5 depicts the 5-day mean IOP versus time profile for a treated eye after dosing with THC-VHS-SLN over the 5-day dosing regimen in comparison to the contralateral eye IOP (untreated eye). The IOP of the treated eye was significantly lower than the untreated eye from the 30-minute time point, and this effect lasted until 360 minutes.
Figure 5.
Mean IOP versus time profile for treated (dotted line) and untreated (solid line) eyes in normotensive rabbits (n = 6) dosed with 50 μL of 0.98% w/v THC-VHS-SLN twice a day for 5 consecutive days. The line represents the mean of these data points at each time point (± SEM). The IOP profiles of the treated were contralateral rabbit eyes were compared using a proc mixed repeated measures model. The P values for treated versus untreated eyes are also listed.
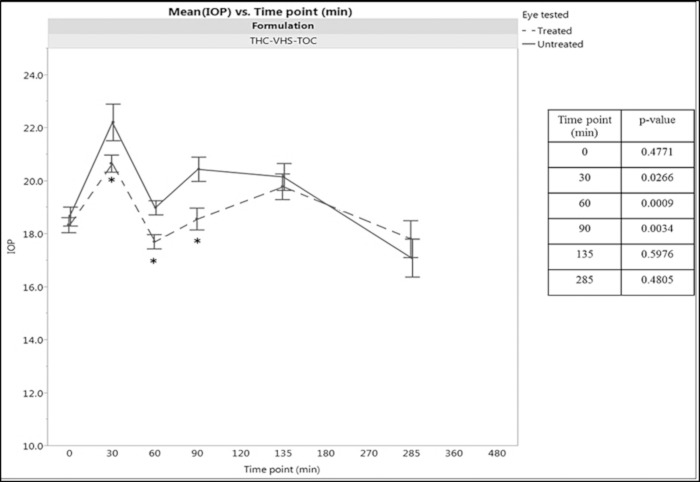
Multiple-Dosing Regimen for THC-VHS-TOC
The THC-VHS-TOC emulsion formulation did not have a significant effect on the IOP of normotensive rabbits. The 5-day mean IOP versus time profile for the eye treated with THC-VHS-TOC in comparison to the contralateral eye is shown in Figure 6. The IOP drop in the treated eye lasts for about 90 minutes, with IOP significantly lower than the contalateral eye at the 30-, 60-, and 90-minute time points.
Figure 6.
Mean IOP versus time profile for treated (dotted line) and untreated (solid line) eyes in normotensive rabbits (n = 6) dosed with 50 μL of 0.98% w/v THC-VHS-TOC twice a day for 5 consecutive days. The lines represent the mean of these data points at each time point (± SEM). The IOP profile of the treated versus contralateral rabbit eyes were compared using proc mixed repeated measures model. The P values for treated versus untreated eyes are listed in the figure.
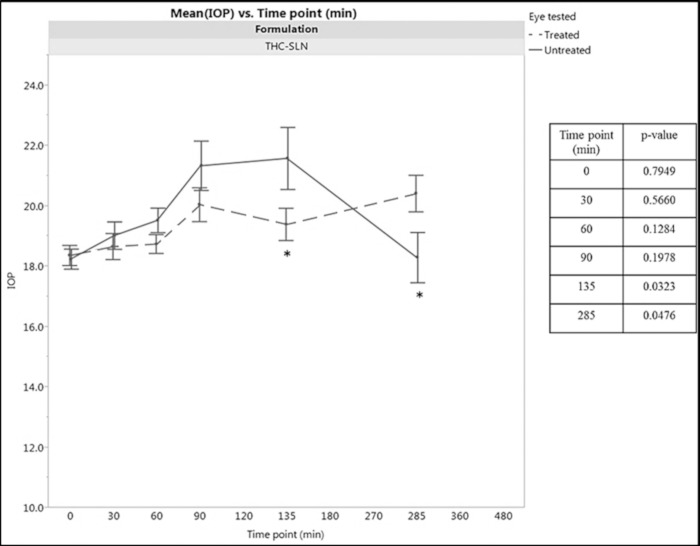
Multiple-Dosing Regimen for THC-SLN
To elucidate the effect of prodrug derivatization, the efficacy of the THC-SLN formulations was also tested. The mean 5-day IOP versus time profile comparing the THC-SLN treated and contralateral eyes is shown in Figure 7. The eyes receiving THC-SLNs did not show a significant drop in IOP in comparison to the contralateral eye up to 90 minutes. However, at the 135-minute time point, the IOP of the treated eye was significantly lower than the contralateral eye. After a period of 2.5 hours, at the 285 minute time point, this effect was reversed and the contralateral eye showed significantly lower IOP in comparison to the treated eye.
Figure 7.
Mean IOP versus time profile for treated (dotted line) and untreated (solid line) eyes in normotensive rabbits (n = 6) dosed with 50 μL of 0.6% w/v THC-SLNs twice a day for 5 consecutive days. The line represents the mean of these data points at each time point (± SEM). The IOP profiles of the treated versus contralateral rabbit eyes were compared using a proc mixed repeated measures model. The P values for treated versus untreated eyes are listed in the figure.
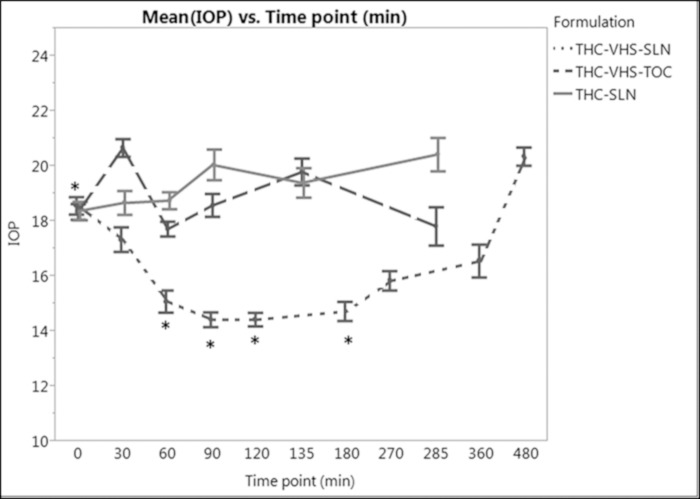
Figure 8 illustrates statistically significant within-group differences, comparing IOP for the same treatment with baseline IOP (time point 0) and between-group differences for different formulations at various time points. Looking at the within-group differences for treatment THC-VHS-SLNs, the drop in IOP at time points 60, 90, 120, and 180 minutes is significantly lower than baseline IOP (time point, 0 minutes), with P values of 0.011, <0.0001, <0.0001, and 0.0021, respectively. A proc mixed repeated measures model was used with a Tukey Kramer adjustment to assess these differences. Other treatment formulations, THC-VHS-TOC, and THC-SLNs do not show significantly lower IOP in comparison to baseline IOP. Analyzing between-group differences, THC-VHS-SLNs demonstrated significantly lower IOP than THC-SLNs (P < 0.0001) and THC-VHS-TOC (P = 0.0019) at time points 60, 90, and 90 minutes, respectively.
Figure 8.
Comparative mean IOP versus time profiles for rabbits treated with 50 μL of 0.98% THC-VHS-SLN, 0.98% w/v THC-VHS-TOC, or 0.6% w/v THC-SLNs (n = 6) twice a day for 5 consecutive days. The line represents the mean of these data points at each time point (± SEM). The rabbit eyes receiving the different formulations were compared using a proc mixed repeated measures model.
Ocular Bioavailability
For THC-VHS-SLN, the maximum drop in the IOP from the baseline (ΔIOPmax) was 31% and 29.3% on day 1 and day 5, respectively. The time to achieve ΔIOPmax (Tmax) on day 1 and day 5, was 90 minutes, and the duration of action for THC-VHS-SLN, or the time required for ΔIOP to reach 90% of baseline IOP, was 480 minutes on both days 1 and 5. The two sacrificial time points, determined based on the IOP data, were 90 and 360 minutes. Table 4 displays the concentration of both THC-VHS and the parent molecule at the two sacrificial time points. At 90 minutes, THC-VHS concentrations were 10.67 ± 2.28 ng/50 mg in AH and decreased to 3.84 ± 0.53 ng/50 mg at 360 minutes. In comparison to AH, higher levels of the prodrug were observed in the IC and RC, with 1466 ± 514.5 ng/50 mg and 902 ± 372 ng/50 mg observed at 90 minutes and 77.6 ± 69.5 ng/50 mg and 238.3 ± 143.3 ng/50 mg observed at the 360-minute time points, respectively. At 360 minutes, 6.36 ± 3.83 ng/50 mg of bioreversed THC was observed in the IC. Significant amounts of drug permeated to the RC and IC tissues, which are both important from the point of view of neuroprotection and IOP lowering, and a corresponding IOP drop was observed as the pharmacodynamic response. THC-VHS was not observed in the plasma even after multiple administration, which helps rule out central nervous system involvement through systemic exposure.
Table 4.
Tissue Concentrations of THC-VHS and THC on Day 6 Postinstillation of 50 μL of 0.98% w/v THC-VHS-SLNs, at 90 Minutes (n = 3) and 360 Minutes (n = 3) in Aqueous Humor, Vitreous Humor, Retina Choroid, and Iris Ciliary Bodies. Dose Equivalent to 300 μg THC.
|
Tissue Analyzed |
Time Point (min) |
THC-VHS, ng/50 mg, mean ± SE |
THC, ng/50 mg, mean ± SE |
| Aqueous humor | 90 | 10.7 ± 2.3 | ND |
| 360 | 3.8 ± 0.5 | ND | |
| Vitreous humor | 90 | ND | ND |
| 360 | ND | ND | |
| Iris ciliary bodies | 90 | 1466 ± 514.5 | ND |
| 360 | 77.6 ± 69.5 | 6.4 ± 3.8 | |
| Retina choroid | 90 | 902 ± 372 | ND |
| 360 | 238.3 ± 143.3 | ND |
ND, below limits of detection.
For THC-VHS-TOC, the ΔIOPmax for day 1 and day 5 of dosing was 11.7% and 10.9%, respectively, and the Tmax was 60 minutes. Thus, the sacrifice time points determined for this formulation were 60 and 120 minutes. The ocular concentrations of THC-VHS obtained with the THC-VHS-TOC formulation were significantly lower than those obtained with the THC-VHS SLN formulation (Table 5).
Table 5.
Tissue Concentrations of THC-VHS and THC on Day 6 Postadministration of 50 μL of 0.98% w/v THC-VHS-TOC, at 60 Minutes (n = 3) and 120 Minutes (n = 3) in Aqueous Humor, Vitreous Humor, Retina Choroid, and Iris Ciliary Bodies. Dose equivalent to 300 μg THC.a
|
Tissue Analyzed |
Time Point (min) |
THC-VHS, ng/50 mg, mean ± SE |
THC, ng/50 mg, mean ± SE |
| Aqueous humor | 60 | 91.2 ± 1.85 | ND |
| 120 | ND | ND | |
| Vitreous humor | 60 | ND | ND |
| 120 | ND | ND | |
| Iris ciliary bodies | 60 | 24.2 ± 5.06 | 53 ± 28.9 |
| 120 | 11.3 ± 0.50 | 57.4 ± 18.5 | |
| Retina choroid | 60 | 15.5 ± 6.70 | 5.2 ± 0.2 |
| 120 | 7.5b | 5.3b |
ND, below limits of detection.
Table has been reproduced with permission.4
Drug levels observed in a single animal only.
Consistent with the previously reported data, THC did not produce as intense or as prolonged an IOP drop from baseline IOP in comparison to the THC-VHS formulations.4 A 6.9% drop in IOP in comparison to the baseline IOP was observed with THC-SLNs at 60 minutes on day 5. Animals were sacrificed at two time points on day 6 at 60 and 120 minutes (Table 6). THC levels of 12.53 ± 3.51 ng/50 mg and 9.87 ± 3.22 ng/50 mg were observed in the IC at 60 and 120 minutes, respectively.
Table 6.
Tissue Concentrations of THC on Day 6 Postadministration of 50 μL of 0.98% w/v THC-SLN, at 60 Minutes (n = 3), and 120 Minutes (n = 3) in Aqueous Humor, Vitreous Humor, Retina Choroid, and Iris Ciliary Bodies. Dose equivalent to 300 μg THC.
|
Tissue Analyzed |
Time Point (min) |
THC, ng/50 mg, mean ± SE |
| Aqueous humor | 60 | ND |
| 120 | ND | |
| Vitreous humor | 60 | ND |
| 120 | ND | |
| Iris ciliary bodies | 60 | 12.5 ± 3.5 |
| 120 | 9.9 ± 3.2 | |
| Retina choroid | 60 | ND |
| 120 | ND |
ND, below limits of detection.
Single-Dose Efficacy Studies
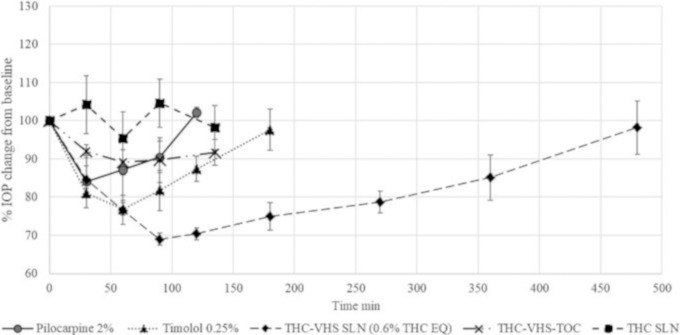
Pilocarpine HCl (2% w/v) exhibited a ΔIOPmax of 15.9% at 30 minutes, and its IOP-lowering effect lasted for 120 minutes (Fig. 9). The graphs represent %IOP drop from the baseline IOP. Timolol maleate (0.25% w/v) resulted in a more intense ΔIOPmax of 23.1% at 60 minutes, with a duration of action of 180 minutes for the IOP to reach 90% of the baseline IOP. THC-TOC emulsion or the placebo-SLNs did not result in any reduction in IOP (data not shown). The IOP versus time profiles of the marketed preparations are compared to that of the THC-VHS-SLNs, THC-VHS-TOC, and THC-SLNs in Figure 9.
Figure 9.
Percent IOP change from baseline versus time profile for THC-VHS-SLN, THC-VHS-TOC, and THC-SLN and 2% w/v pilocarpine and 0.25% w/v timolol maleate marketed formulations. A single drop (50 μL) was instilled. Data represent mean ± SE.
Discussion
In 1977, Green et al.51 reported a 17% drop in the IOP, 60 minutes after dosing, by using THC formulated in light mineral oil as the vehicle in adult albino rabbits. The tissue concentrations obtained were extremely low, namely, about 1 ng of 14C-labeled THC/mg of wet tissue weighed 4 hours after dosing in the cornea and IC. Hingorani et al.52 observed that the amount of THC permeating into the ocular tissues was below levels of detection in rabbit AH, VH, RC, and IC, 1 hour postadministration of THC in light mineral oil (0.1% w/v), emulsion (0.37% w/v), or micellar solutions (0.125% w/v THC, 0.5% w/v Cremophor RH 40) in NZW rabbits, with detectable levels only in the cornea and sclera. Such findings suggest that the lipophilic nature of THC prevents its partitioning from the oily vehicle into the tear film, in turn affecting its overall ocular bioavailability. THC has poor aqueous solubility (1–2 μg/mL) and high log P (6.42), which makes the development of an eye drop for the molecule challenging. The lack of activity through the topical route of application, as observed in the abovementioned reports, could be due to the ineffective delivery of THC to the target ocular tissues rather than the absence of local pharmacological activity. The delivery of a therapeutic agent to the deeper ocular tissues depends on the type of formulation, physicochemical properties of the molecule, and absorption pathway.53 These properties determine the permeation profile of the molecule across alternating lipophilic and hydrophilic tissue layers and through the corneal tight junctions. For targeting a molecule to the back of the eye, it should possess optimum physicochemical properties and be formulated in appropriate dosage forms.54
To improve the intrinsic solubility of THC, a prodrug strategy was used by Hingorani et al.52,55 by using a hemiglutarate (dicarboxylic acid) ester (THC-HG), which, being ionized at physiological pH, would have better aqueous solubility (19 μg/mL). One hour postinstillation of 50 μL of THC-HG, formulated in 0.5% w/v Cremophor RH 40, 35.6 ± 12.5 ng of THC/50 mg of tissue was observed in the IC and 32.1 ± 12.6 ng of THC/100 μL was detected in AH of NZW rabbits, whereas the THC tissue concentrations obtained postdosing of 50 μL THC formulated in 0.5% w/v Cremophor RH 40 were below detection levels. This finding suggested that hydrophilic prodrug derivatization is an efficient method to improve the ocular bioavailability of THC.52 However, in terms of chemical stability, THC-HG was extremely unstable and underwent rapid degradation at acidic and alkaline pH conditions, as well as at physiological pH.55,56
In subsequent studies, THC-VHS was designed as an amino acid-dicarboxylic acid prodrug, with the amide linkage enhancing its stability. In terms of the physicochemical properties, THC-VHS is stable from pH 5 to pH 9.49 Adelli et al.4 observed the efficacy of THC-VHS in a soybean oil-based emulsion in an elevated IOP-glaucoma model. THC-VHS demonstrated an IOP drop comparable to the marketed ophthalmic solution of 2% (w/v) pilocarpine HCl.47 However, the IOP versus time profile indicated that frequent dosing would be necessary. Thus, developing a formulation strategy that could increase the amount of THC-VHS that could enhance the bioavailability as well as retention of the therapeutic agent at the ocular surface would be desirable.
Posttopical application, a molecule has to overcome significant barriers, such as vascular and lymphatic drainage in the conjunctiva, sclera, and choroid, restricting its passage from the ocular surface to posterior ocular tissues.57 SLNs enhance the ocular bioavailability of poorly soluble compounds by acting as unit carriers of the target molecules and prolonging its residence time in the cul de sac and forming a lipid-based drug reservoir that interacts with the ocular mucosa.48,54,58,59 SLNs, being solid at room temperature, have a modulated drug release profile in comparison to a liquid based-formulation.60 Punyamurthula et al.48 demonstrated enhanced delivery of Δ8 THC-SLNs to all ocular tissues attributed to the probable uptake of the SLNs by the conjunctival and corneal membranes, resulting in sustained release of the drug.
However, to develop an SLN formulation of THC-VHS, the thermal stability of the prodrug would play an important role during formulation development. Both molecules, THC and THC-VHS, are amorphous with the absence of a definite crystal lattice structure, making them susceptible to atmospheric degradation.56,61 THC undergoes rapid thermo-oxidative degradation into its metabolite cannabinol. The use of polymeric stabilizers and cross-linked matrices can be considered as a way of controlling the oxidative degradation of amorphous molecules such as THC.61–63 Compritol 888 ATO is a crystalline amphiphilic material with a melting point of about 70°C. The crystalline structure of the bulk lipid can form protective barriers increasing the storage stability of the formulation.64 The high solubility of THC and THC-VHS in Compritol 888 ATO, along with the stabilizing effect provided by the crystalline lipid, make it a good choice of lipid for the development of the SLN formulation. Previous reports show that THC-VHS shows only about 3% degradation of drug when heated at 120°C for 10 minutes.49 Taking into consideration this along with the melting point of Compritol 888 ATO, a temperature of 70°C was chosen to formulate the SLNs.
The physicochemical data suggest that a structured lipid phase comprising of Compritol 888 ATO (stabilized by a poloxamer 188-Tween 80 surfactant system) resulted in a stable nanoparticulate system. The data obtained from the STEM indicate that the size of the well-rounded nanoparticles is slightly greater than 200 nm, which is also consistent with the results obtained from Dynamic Light Scattering. In the case of multimodal data, particle size may not agree across different measurement techniques; however, for a monodisperse formulation, the particle size data might be comparable.65,66 At the 6-month time point, complete gelation of the SLN formulation at the storage condition of 40°C/60% RH was observed (Fig. 2). The temperature-dependent dynamics of an emulsifier-stabilized colloidal system has been governed by an interplay of several variables. Increase in the temperature at the storage condition of 40°C/60% RH in turn increases the entropy of the system, increasing the interparticle interactions. At a lower temperature, the emulsifier stabilizing the nano particles avoids fusion of the particles due to its microviscosity (film rigidity). However, at a higher temperature, the microviscosity of the emulsifier is reduced. This reduced microviscosity along with the increased interparticle interactions could lead to aggregation and gelation, a phenomenon not observed when the formulation was stored at lower temperatures.67
Histological analysis of the rabbit corneas treated with the SLNs helps understand the toxicity profile of the SLNs. In corneas treated with control (Figs. 4D, 4E, 4F), we observe structurally disturbed collagen bonds in areas close to the Descemet membrane invagination. However, considering the exclusivity of this event, the damage to this cornea can be attributed to mechanical stress during the enucleation and the fixing of the cornea. For corneas treated with placebo-SLNs (Figs. 4A, 4B, 4C), the stroma is present as even layers with signs of edema ranging from slight to none.68
Topical THC-VHS-SLNs produced a prolonged and intense drop in the IOP in normotensive rabbits in comparison to THC-VHS-TOC as well as THC-SLNs. THC-VHS-SLNs lowered the IOP of the treated eye in comparison to the untreated eye and maintained IOP below baseline until 360 minutes. In comparison, rabbit eyes treated with THC-VHS-TOC produced a significant drop in IOP in comparison to the untreated eye at 30, 60, and 90 minutes only. Comparing the P values for differences in the IOP for treated and untreated eyes, the IOP drop produced by THC-VHS-TOC was not as significant as THC-VHS-SLN. SLNs, being colloidal carriers, have advantages of better penetration, stability, drug loading, and sustained release of the drug.69 The large surface area provided by the nanoparticulate system increased the contact area, ensuring close contact with the ocular mucosa after instillation. Lipid-based nanoparticles have an occlusive effect and form a depot in the cul de sac, slowly releasing the drug over a prolonged duration of time.70,71 The additives present in the formulations, such as surfactants, also play a role in permeation enhancement via fluidization of the lipid bilayers of the ocular membranes.72
The THC-SLN-treated eyes showed a statistically significant lower IOP in comparison to the untreated eyes at the 135-minute time point only. Based on the IOP data, THC-VHS was effectively delivered to the target tissues within the first 30 minutes from both the SLN and emulsion-based formulations, whereas the parent molecule required about 2 hours to demonstrate a pharmacodynamic response.
The pharmacokinetic data suggest that the SLN formulations deliver an almost 60 times greater concentration of THC-VHS in the IC in comparison to the emulsion formulation. THC levels in the ocular tissues from the THC-VHS-SLN formulations were extremely low (below detection levels in most cases) in comparison to that obtained from the THC-VHS-TOC or THC-SLN formulations. However, the duration of IOP drop observed with the THC-VHS-SLNs was significantly more prolonged. A possible explanation for this disconnect between the PK-PD observations could be that the site of action might not be the IC. It could also be possible that the prodrug being more permeable could be distributing deeper into the tissues better than THC (administered as such or THC generated from THC-VHS). As a result, a correlation between the prodrug concentration, rather than THC concentration, and IOP-lowering effect are observed. The lack of a pharmacodynamic response even though the ocular tissues exhibited significant THC concentrations (with the THC-VHS-TOC and THC-SLN formulations) could be because of THC forming a depot in the ocular tissues, rather than penetrating and distributing across the ocular tissues (e.g., IC). As a result, concentrations at the site of action may be low even though the overall tissue concentrations are high.22 The reason why THC-VHS-TOC is not as effective as THC-VHS-SLN could be because the emulsion formulation is not protecting the prodrug from bioreversion (chemical or enzymatic), as a result of which higher THC tissue concentrations are observed from THC-VHS-TOC, thus decreasing the concentration deeper in the tissues. On the other hand, the SLN formulation protects against bioreversion of THC-VHS to THC, as evidenced by the lack of detectable THC concentrations from the THC-VHS-SLN formulations.
The overall tissue distribution profile indicates a noncorneal route of absorption. With THC-VHS-SLN, we observe 1466 ± 514.50 ng/50 mg tissue of THC-VHS in the IC at 90 minutes. The prodrug concentrations dropped almost 20-fold at 360 minutes, which can be explained by elimination and slow conversion into THC, which was also detected then. We also observe THC-VHS partitioning into the RC, from both THC-VHS-TOC and THC-VHS-SLN formulations, which is important for the neuroprotective action. With THC-SLNs, however, we observe THC levels in the IC at both sacrifice time points, but THC fails to distribute itself across other tissues. The preferential accumulation of THC in the IC could indicate binding of THC to an IC-specific protein.
The IOP-lowering duration with THC-VHS-SLNs lasted almost twice as long as the marketed formulations 2.5% w/v pilocarpine or 0.2% w/v timolol maleate. A combined effect of prodrug derivatization and the dosage form can be attributed to this effect, as the prodrug alone (in an emulsion formulation) or the parent compound THC in an SLN formulation were not effective. The molecule design facilitated easy passage of the parent molecule across the ocular tissues and the lipid-based nanocarrier system acted as a long-acting depot, resulting in a formulation with better PK-PD profile.
Conclusion
THC has been demonstrated to be effective in glaucoma management, helping to lower IOP in human subjects after smoking marijuana; however, the molecule fails to manifest a similar effect when dosed topically. This research explores molecular bioengineering and formulation-based strategies to improve the ocular bioavailability of THC, facilitating the molecule to translate into a dosage form capable of demonstrating a desired IOP-lowering effect even on topical application. These studies suggest that formulation development efforts along with prodrug derivatization can effectively improve the overall ocular bioavailability of THC. THC-VHS-SLNs were successfully formulated and tested in a normotensive rabbit model. Results suggested that the prodrug THC-VHS has a better permeation profile than THC due to its modified structure. SLNs are efficient in the delivery of THC-VHS to the RC, which is important from the point of view of neuroprotection. THC-VHS-SLNs, on multiple dosing, were able to achieve an intense IOP drop, with its effect lasting for a longer duration than the marketed solutions of 2.5% w/v pilocarpine HCl and 0.2% w/v timolol maleate. Thus, THC-VHS represents a potential new therapy option for the treatment and management of glaucoma by virtue of its superiority in lowering IOP when compared to antiholinergic and beta blockers, as studied in this model. Further analyses are needed to understand the impact of the endocannabinoid-receptor system in the eye and its relation to the THC-VHS mechanism of action as well as the impact on the direct neuroprotective activity of preserving RGCs by cannabinoids.
Acknowledgments
Supported by a research grant from Emerald Bioscience, Inc. The authors thank Monica M. Jablonski, The University of Tennessee Health Science Center, for her insight toward the corneal histology analysis and interpretation. This research is sponsored by Emerald Bioscience, Inc., and may lead to the development of products from which Waseem Gul, Mahmoud A. ElSohly, and Soumyajit Majumdar may receive income as part of licensing fees and royalties paid to the University of Mississippi.
Disclosure: P.S. Taskar, None; A. Patil, None; P. Lakhani, None; E. Ashour, None; W. Gul, None; M.A. ElSohly, Emerald Bioscience Inc. (C); B. Murphy, Emerald Bioscience Inc. (S); S. Majumdar, None
References
- 1.Quigley HA, Addicks EM, Green W, Maumenee AE. Optic nerve damage in human glaucoma. II. The site of injury and susceptibility to damage. Arch Ophthalmol. 1981;99:635–649. doi: 10.1001/archopht.1981.03930010635009. [DOI] [PubMed] [Google Scholar]
- 2.Abe RY, Diniz-Filho A, Costa VP, Gracitelli CPB, Baig S, Medeiros FA. The impact of location of progressive visual field loss on longitudinal changes in quality of life of patients with glaucoma. Ophthalmology. 2016;123:552–557. doi: 10.1016/j.ophtha.2015.10.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cook C, Foster P. Epidemiology of glaucoma: what's new? Can J Ophthalmol. 2012;47:223–226. doi: 10.1016/j.jcjo.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 4.Adelli GR, Bhagav P, Taskar P, et al. Development of a delta9-tetrahydrocannabinol amino acid-dicarboxylate prodrug with improved ocular bioavailability. Invest Ophthalmol Vis Sci. 2017;58:2167–2179. doi: 10.1167/iovs.16-20757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–267. doi: 10.1136/bjo.2005.081224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.NEI. Glaucoma, Open-angle. https://nei.nih.gov/eyedata/glaucoma. [Google Scholar]
- 7.Grüb M, Mielke J. Aqueous humor dynamics [In German] Ophthalmologe. 2004;101:357–365. doi: 10.1007/s00347-003-0939-3. [DOI] [PubMed] [Google Scholar]
- 8.Macri FJ, Cevario SJ. The formation and inhibition of aqueous humor production: a proposed mechanism of action. Arch Ophthalmol. 1978;96:1664–1667. doi: 10.1001/archopht.1978.03910060290023. [DOI] [PubMed] [Google Scholar]
- 9.Brubaker RF. Goldmann's equation and clinical measures of aqueous dynamics. Exp Eye Res. 2004;78:633–637. doi: 10.1016/j.exer.2003.07.002. [DOI] [PubMed] [Google Scholar]
- 10.Goel M, Picciani RG, Lee RK, Bhattacharya SK. Aqueous humor dynamics: a review. Open Ophthalmol J. 2010;4:52–59. doi: 10.2174/1874364101004010052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gabelt BAT, Kaufman PL. Changes in aqueous humor dynamics with age and glaucoma. Prog Retin Eye Res. 2005;24:612–637. doi: 10.1016/j.preteyeres.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 12.Yablonski ME, Zimmerman TJ, Waltman SR, Becker B. A fluorophotometric study of the effect of topical timolol on aqueous humor dynamics. Exp Eye Res. 1978;27:135–142. doi: 10.1016/0014-4835(78)90083-0. [DOI] [PubMed] [Google Scholar]
- 13.Tătaru CP, Purcărea VL. Antiglaucoma pharmacotherapy. J Med Life. 2012;5:247–251. [PMC free article] [PubMed] [Google Scholar]
- 14.Toris CB. Pharmacology of aqueous humor formation A2. In: Dartt DA, editor. Encyclopedia of the Eye. Oxford: Academic Press; 2010. pp. 312–315. [Google Scholar]
- 15.Patil A, Singh S, Opere C, Dash A. Sustained-release delivery system of a slow hydrogen sulfide donor, GYY 4137, for potential application in glaucoma. AAPS PharmSciTech. 2017;18:2291–2302. doi: 10.1208/s12249-017-0712-6. [DOI] [PubMed] [Google Scholar]
- 16.New Medical Therapies for Glaucoma. https://www.glaucoma.org/news/blog/new-medical-therapies-offer-hope-for-glaucoma-patients.php. Published March 6, 2018. [Google Scholar]
- 17.Schehlein EM, Novack G, Robin AL. New pharmacotherapy for the treatment of glaucoma. Expert Opin Pharmacother. 2017;18:1939–1946. doi: 10.1080/14656566.2017.1408791. [DOI] [PubMed] [Google Scholar]
- 18.Twitchell W, Brown S, Mackie K. Cannabinoids inhibit N- and P/Q-type calcium channels in cultured rat hippocampal neurons. J Neurophysiol. 1997;78:43–50. doi: 10.1152/jn.1997.78.1.43. [DOI] [PubMed] [Google Scholar]
- 19.Malinowska B, Godlewski G, Bucher B, Schlicker E. Cannabinoid CB1 receptor-mediated inhibition of the neurogenic vasopressor response in the pithed rat. Naunyn Schmiedebergs Arch Pharmacol. 1997;356:197–202. doi: 10.1007/pl00005041. [DOI] [PubMed] [Google Scholar]
- 20.Sugrue MF. New approaches to antiglaucoma therapy. J Med Chem. 1997;40:2793–2809. doi: 10.1021/jm9608725. [DOI] [PubMed] [Google Scholar]
- 21.Allingham RR, de Kater AW, Ethier RC. Schlemm's canal and primary open angle glaucoma: correlation between Schlemm's canal dimensions and outflow facility. Exp Eye Res. 1996;62:101–110. doi: 10.1006/exer.1996.0012. [DOI] [PubMed] [Google Scholar]
- 22.Tomida I, Pertwee RG, Azuara-Blanco A. Cannabinoids and glaucoma. Br J Ophthalmol. 2004;88:708–713. doi: 10.1136/bjo.2003.032250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Panahi Y, Manayi A, Nikan M, Vazirian M. The arguments for and against cannabinoids application in glaucomatous retinopathy. Biomed Pharmacother. 2016;86:620–627. doi: 10.1016/j.biopha.2016.11.106. [DOI] [PubMed] [Google Scholar]
- 24.Porcella A, Maxia C, Gessa GL, Pani L. The human eye expresses high levels of CB1 cannabinoid receptor mRNA and protein. Eur J Neurosci. 2000;12:1123–1127. doi: 10.1046/j.1460-9568.2000.01027.x. [DOI] [PubMed] [Google Scholar]
- 25.Porcella A, Maxia C, Gessa GL, Pani L. The synthetic cannabinoid WIN55212-2 decreases the intraocular pressure in human glaucoma resistant to conventional therapies. Eur J Neurosci. 2001;13:409–412. doi: 10.1046/j.0953-816x.2000.01401.x. [DOI] [PubMed] [Google Scholar]
- 26.Morgan-Davies J, Taylor N, Hill AR, Aspinall P, O'Brien CJ, Azuara-Blanco A. Three dimensional analysis of the lamina cribrosa in glaucoma. Br J Ophthalmol. 2004;88:1299–1304. doi: 10.1136/bjo.2003.036020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Agarwal R, Gupta SK, Agarwal P, Saxena R, Agrawal SS. Current concepts in the pathophysiology of glaucoma. Indian J Ophthalmol. 2009;57:257–266. doi: 10.4103/0301-4738.53049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abe RY, Gracitelli CPB, Diniz-Filho A, Tatham AJ, Medeiros FA. Lamina cribrosa in glaucoma: diagnosis and monitoring. Curr Ophthalmol Rep. 2015;3:74–84. doi: 10.1007/s40135-015-0067-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Almasieh M, Wilson AM, Morquette B, Cueva Vargas JL, Di Polo A. The molecular basis of retinal ganglion cell death in glaucoma. Prog Retin Eye Res. 2012;31:152–181. doi: 10.1016/j.preteyeres.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 30.El-Remessy AB, Khalil IE, Matragoon S, et al. Neuroprotective effect of(−)Δ9-tetrahydrocannabinol and cannabidiol in N-methyl-d-aspartate-induced retinal neurotoxicity: involvement of peroxynitrite. Am J Pathol. 2003:1997–2008. doi: 10.1016/s0002-9440(10)63558-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ko ML, Hu DN, Ritch R, Sharma SC. The combined effect of brain-derived neurotrophic factor and a free radical scavenger in experimental glaucoma. Invest Ophthalmol Vis Sci. 2000;41:2967–2971. [PubMed] [Google Scholar]
- 32.Naveh N, Weissman C, Muchtar S, Benita S, Mechoulam R. A submicron emulsion of HU-211, a synthetic cannabinoid, reduces intraocular pressure in rabbits. Graefes Arch Clin Ophthalmol. 2000;238:334–338. doi: 10.1007/s004170050361. [DOI] [PubMed] [Google Scholar]
- 33.Shohami E, Gallily R, Mechoulam R, Bass R, Ben-Hur T. Cytokine production in the brain following closed head injury: dexanabinol (HU-211) is a novel TNF-α inhibitor and an effective neuroprotectant. J Neuroimmunol. 1997;72:169–177. doi: 10.1016/s0165-5728(96)00181-6. [DOI] [PubMed] [Google Scholar]
- 34.Crandall J, Matragoon S, Khalifa YM, et al. Neuroprotective and intraocular pressure-lowering effects of (–)δ9-tetrahydrocannabinol in a rat model of glaucoma. Ophthalmic Res. 2007;39:69–75. doi: 10.1159/000099240. [DOI] [PubMed] [Google Scholar]
- 35.Crandall J, Matragoon S, Khalifa YM, et al. Neuroprotective and intraocular pressure-lowering effects of (-)Delta9-tetrahydrocannabinol in a rat model of glaucoma. Ophthalmic Res. 2007;39:69–75. doi: 10.1159/000099240. [DOI] [PubMed] [Google Scholar]
- 36.Grotenhermen F, Russo E. New York: Haworth Integrative Healing Press; 2002. Cannabis and Cannabinoids: Pharmacology, Toxicology, and Therapeutic Potential. [Google Scholar]
- 37.Hepler RS, Frank IR. Marihuana smoking and intraocular pressure. JAMA. 1971;217:1392. [PubMed] [Google Scholar]
- 38.Green K. Marijuana smoking vs cannabinoids for glaucoma therapy. Arch Ophthalmol. 1998;116:1433–1437. doi: 10.1001/archopht.116.11.1433. [DOI] [PubMed] [Google Scholar]
- 39.Crawford WJ, Merritt JC. Effects of tetrahydrocannabinol on arterial and intraocular hypertension. Int J Clin Pharmacol Biopharm. 1979;17:191–196. [PubMed] [Google Scholar]
- 40.Merritt JC, Perry DD, Russell DN, Jones BF. Topical Δ9-tetrahydrocannabinol and aqueous dynamics in glaucoma. J Clin Pharmacol. 1981;21:467S–471S. doi: 10.1002/j.1552-4604.1981.tb02626.x. [DOI] [PubMed] [Google Scholar]
- 41.Elsohly MA, Harland E, Murphy JC, Wirth P, Waller CW. Cannabinoids in glaucoma: a primary screening procedure. J Clin Pharmacol. 1981;21:472S–478S. doi: 10.1002/j.1552-4604.1981.tb02627.x. [DOI] [PubMed] [Google Scholar]
- 42.Jay WM, Green K. Multiple-drop study of topically applied 1% δ9-tetrahydrocannabinol in human eyes. Arch Ophthalmol. 1983;101:591–593. doi: 10.1001/archopht.1983.01040010591012. [DOI] [PubMed] [Google Scholar]
- 43.Muchtar S, Almog S, Torracca MT, Saettone MF, Benita S. A submicron emulsion as ocular vehicle for delta-8-tetrahydrocannabinol: effect on intraocular pressure in rabbits. Ophthalmic Res. 1992;24:142–149. doi: 10.1159/000267160. [DOI] [PubMed] [Google Scholar]
- 44.Song Z-H, Slowey C-A. Involvement of cannabinoid receptors in the intraocular pressure-lowering effects of WIN55212-2. J PharmacolExp Ther. 2000;292:136–139. [PubMed] [Google Scholar]
- 45.ElSohly MA, Gul W, Walker LA. Pharmacokinetics and tolerability of Δ9-THC-Hemisuccinate in a suppository formulation as an alternative to capsules for the systemic delivery of Δ9-THC. Med Cannabis Cannabinoids. 2018;1:44–53. doi: 10.1159/000489037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Taskar P, Adelli G, Patil A, et al. Analog derivatization of cannabidiol for improved ocular permeation. J Ocul Pharmacol Ther. 2019;35:301–310. doi: 10.1089/jop.2018.0141. [DOI] [PubMed] [Google Scholar]
- 47.Taskar P, Tatke A, Majumdar S. Advances in the use of prodrugs for drug delivery to the eye. Expert Opin Drug Deliv. 2017;14:49–63. doi: 10.1080/17425247.2016.1208649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Punyamurthula NS, Adelli GR, Gul W, Repka MA, ElSohly MA, Majumdar S. Ocular disposition of 8-tetrahydrocannabinol from various topical ophthalmic formulations. AAPS PharmSciTech. 2016;18:1936–1945. doi: 10.1208/s12249-016-0672-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.ElSohly MA, Gul W, Repka MA, Majumdar S. Compositions containing delta-9-THC-amino acid esters and process of preparation. Google Patents, US Patent number US8809261B2; 2011 [Google Scholar]
- 50.Schubert MA, Müller-Goymann CC. Characterisation of surface-modified solid lipid nanoparticles (SLN): influence of lecithin and nonionic emulsifier. Eur J Pharm Biopharm. 2005;61:77–86. doi: 10.1016/j.ejpb.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 51.Green K, Bigger JF, Kim K, Bowman K. Cannabinoid penetration and chronic effects in the eye. Exp Eye Res. 1977;24:197–205. doi: 10.1016/0014-4835(77)90260-3. [DOI] [PubMed] [Google Scholar]
- 52.Hingorani T, Adelli GR, Punyamurthula N, et al. Ocular disposition of the hemiglutarate ester prodrug of Δ9-tetrahydrocannabinol from various ophthalmic formulations. Pharm Res. 2013:30. doi: 10.1007/s11095-013-1072-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Maurice DM, Mishima S. Sears ML ed, Pharmacology of the Eye. Berlin Heidelberg: Springer; 1984. Ocular pharmacokinetics; pp. 19–116. [Google Scholar]
- 54.Balguri SP, Adelli GR, Majumdar S. Topical ophthalmic lipid nanoparticle formulations (SLN, NLC) of indomethacin for delivery to the posterior segment ocular tissues. Eur J Pharm Biopharm. 2016;109:224–235. doi: 10.1016/j.ejpb.2016.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hingorani T, Gul W, Elsohly M, Repka MA, Majumdar S. Effect of ion pairing on in vitro transcorneal permeability of a Delta(9) -tetrahydrocannabinol prodrug: potential in glaucoma therapy. J Pharm Sci. 2011;101:616–626. doi: 10.1002/jps.22791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thumma S, Majumdar S, ElSohly MA, Gul W, Repka MA. Preformulation studies of a prodrug of δ9-tetrahydrocannabinol. AAPS PharmSciTech. 2008;9:982–990. doi: 10.1208/s12249-008-9136-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Duvvuri S, Majumdar S, Mitra AK. Drug delivery to the retina: challenges and opportunities. Expert Opin Biol Ther. 2003;3:45–56. doi: 10.1517/14712598.3.1.45. [DOI] [PubMed] [Google Scholar]
- 58.Kaur IP, Kakkar S. Nanotherapy for posterior eye diseases. J Control Release. 2014;193:100–112. doi: 10.1016/j.jconrel.2014.05.031. [DOI] [PubMed] [Google Scholar]
- 59.Patil A, Lakhani P, Taskar P, et al. Formulation development, optimization, and in-vitro characterization of natamycin-loaded PEGylated nano-lipid carriers for ocular applications. J Pharm Sci. 2018;107:2160–2171. doi: 10.1016/j.xphs.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 60.Lakhani P, Patil A, Taskar P, Ashour E, Majumdar S. Curcumin-loaded nanostructured lipid carriers for ocular drug delivery: design optimization and characterization. J Drug Deliv Sci Technol. 2018;47:159–166. doi: 10.1016/j.jddst.2018.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Thumma S, ElSohly MA, Zhang SQ, Gul W, Repka MA. Influence of plasticizers on the stability and release of a prodrug of Delta(9)-tetrahydrocannabinol incorporated in poly (ethylene oxide) matrices. Eur J Pharm Biopharm. 2008;70:605–614. doi: 10.1016/j.ejpb.2008.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Munjal M, ElSohly MA, Repka MA. Chemical stabilization of a Delta9-tetrahydrocannabinol prodrug in polymeric matrix systems produced by a hot-melt method: Role of microenvironment pH. AAPS PharmSciTech. 2006;7:E114–E125. doi: 10.1208/pt070371. [DOI] [PubMed] [Google Scholar]
- 63.Munjal M, Elsohly MA, Repka MA. Polymeric systems for amorphous δ9-tetrahydrocannabinol produced by a hot-melt method. Part II: Effect of oxidation mechanisms and chemical interactions on stability. J Pharm Sci. 2006;95:2473–2485. doi: 10.1002/jps.20711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Punyamurthula NS, Hingorani T, Adelli G, et al. Controlled release tablet formulation containing natural Delta(9)-tetrahydrocannabinol. Drug Dev Ind Pharm. 2015;42:1158–1164. doi: 10.3109/03639045.2015.1118490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lizunova AA, Loshkarev AA, Tokunov YM, Ivanov VV. Comparison of the results of measurements of the sizes of nanoparticles in stable colloidal solutions by the methods of acoustic spectroscopy, dynamic light scattering, and transmission electron microscopy. Meas Tech. 2017;59:1151–1155. [Google Scholar]
- 66.Anderson W, Kozak D, Coleman VA, Jämting ÅK, Trau M. A comparative study of submicron particle sizing platforms: accuracy, precision and resolution analysis of polydisperse particle size distributions. J Colloid Interface Sci. 2013;405:322–330. doi: 10.1016/j.jcis.2013.02.030. [DOI] [PubMed] [Google Scholar]
- 67.Freitas C, Müller RH. Effect of light and temperature on zeta potential and physical stability in solid lipid nanoparticle (SLN™) dispersions. Int J Pharm. 1998;168:221–229. [Google Scholar]
- 68.Goldman JN, Kuwabara T. Histopathology of corneal edema. Int Ophthalmol Clin. 1968;8:561–579. [PubMed] [Google Scholar]
- 69.Wang J, Xia Q. Alpha-lipoic acid-loaded nanostructured lipid carrier: sustained release and biocompatibility to HaCaT cells in vitro. Drug Deliv. 2014;21:328–341. doi: 10.3109/10717544.2013.846435. [DOI] [PubMed] [Google Scholar]
- 70.Montenegro L, Parenti C, Turnaturi R, Pasquinucci L. Resveratrol-loaded lipid nanocarriers: correlation between in vitro occlusion factor and in vivo skin hydrating effect. Pharmaceutics. 2017;9(58) doi: 10.3390/pharmaceutics9040058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wang J, Zhao F, Liu R, et al. Novel cationic lipid nanoparticles as an ophthalmic delivery system for multicomponent drugs: development, characterization, in vitro permeation, in vivo pharmacokinetic, and molecular dynamics studies. Int J Nanomedicine. 2017;12:8115–8127. doi: 10.2147/IJN.S139436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sarpotdar Pp, Zatz JL. Percutaneous Absorption enhancement by nonionic surfactants. Drug Dev Ind Pharm. 1986;12:1625–1647. [Google Scholar]