Abstract
In the field of orthopedic surgery, distraction osteogenesis (DO) is well known for limb lengthening procedures or secondary corrective surgery in the fracture treatment of the extremities. The principle of gradual expansion of bone and surrounding soft tissues as originally described by G.A. Ilizarov is also applicable to the craniofacial skeleton when growth deficiency is present, and the patients affected by craniofacial or dentofacial anomalies may require distraction procedures. The surgical management is comparable. After osteotomy and the mounting of a specific craniomaxillofacial distraction device, active distraction is started after a latency phase of several days, with a distraction rate of up to 1 mm/day until the desired amount of distraction has been achieved. Subsequently, distractors are locked to provide appropriate stability within the distraction zone for callus mineralization during the consolidation phase of 3–6 months, which is followed by a further remodeling of the bony regenerate. After 14 years of clinical application, the role and significance of craniomaxillofacial DO are discussed after reviewing the files of all patients who were treated by craniomaxillofacial distraction procedures.
Keywords: dentofacial anomaly, gradual expansion, Ilizarov method
Introduction
In 1904/1905, the Italian Codivilla already reported about the possibility of lengthening the lower limb by continuous traction [1]. However, the first successful callus distraction of a human femur after bilateral diaphyseal fractures was performed in 1923 by August Bier in Berlin [2]. Within the field of maxillofacial surgery, distraction approaches were already described between 1920 and 1930. In 1926, Wassmund reported about the possibility of closing an open-bite situation by applying elastic traction to the upper jaw after its subtotal surgical mobilization. Almost at the same time, Rosenthal in Leipzig managed to reconstruct the lower face of a female patient affected by mandibular hypoplasia by applying a tooth-borne expansion device to the anterior lower jaw after bony separation. Probably due to the politic situation during the following period of time, these observations have not been further investigated by these authors [3]. The principle of distraction osteogenesis (DO) and its application to the extremities has been initially described in detail by the Russian surgeon G.A. Ilizarov who was working in Kurgan, Siberia, after World War II. There he was engaged in the treatment of complicated fractures and pseudarthroses of the lower limbs. For that purpose, he was using simple external fixation devices with threads to apply compression to the fracture zones. However, one of his patients occasionally failed to activate the threads correctly and “distracted” the bony segments instead of compressing them. Ilizarov observed ongoing callus formation and mineralization in the former fracture zone and continued to investigate this observation systematically. Subsequently, he developed his method – the “Ilizarov technique” – for fracture treatment, management of bony defect situations, and limb lengthening using the “tension stress effect”: metabolic tissue activation and improved vascularization by the application of gradual traction [4], [5], [6]. Within the field of craniomaxillofacial surgery, experimental work about mandibular DO was published by Snyder and Michieli in the 1970s [7], [8]. However, the clinical application of DO to the craniomaxillofacial skeleton has been emphasized by the U.S. plastic surgeon Joseph G. McCarthy who initially reported about the successful reconstruction of the lower face in children affected by craniofacial microsomia in the late 1980s and subsequently extended the indications of the method [9], [10]. Twenty-five years after an initial “hype” for the method, the application of craniomaxillofacial distraction nowadays is more restricted. According to web-based surveys, there seems to be a lack of evidence for the indication of craniomaxillofacial distraction procedures [11]. Nevertheless, the method can be regarded as an established treatment option in selected patients who are affected by obvious growth restriction or deficiency of the craniomaxillofacial skeleton. Based on 14 years of personal experience, the role and significance of craniomaxillofacial DO are discussed with regard to the corresponding literature and illustrated by three typical patient cases. Accordingly, craniomaxillofacial DO plays a minor role with regard to overall surgical procedures within the field; however, if severe growth restriction is present or has to be expected, the principle of gradual tissue expansion should be regarded as an additional reconstructive option for patients affected by craniofacial or dentofacial anomalies within an staged individual treatment plan.
Materials and methods
After the preceding experimental research work [12], [13], [14], craniomaxillofacial DO has been implemented in 2003 at the Charité Universitätsmedizin Berlin, Campus Virchow-Klinikum (CVK), for the reconstruction of patients affected by craniofacial or dentofacial deformities or comparable skeletal deficiencies due to trauma or tumor. Specific “distraction files” of these patients have been documented from the very beginning by the senior author, including parameters of distraction, corresponding X-rays, and photodocumentation. These distraction files have been reviewed and analyzed to assess the role and significance of craniomaxillofacial DO. In addition, after the end of the therapy, qualitative assessment was performed by a simple questionnaire: Would the patient undergo distraction again? Would distraction be recommended again? Informed consent has been obtained from all patients who were treated by craniomaxillofacial distraction procedures.
Results
Within 14 years, 152 distraction procedures of the craniomaxillofacial skeleton have been performed representing less than 1% of all patients (>30,000) who received craniomaxillofacial therapy during the period of time. A detailed overview of the type, localization, and results of distraction is given in Table 1.
Table 1:
Overview of craniomaxillofacial distraction procedures from 2003 to 2016.
| Region | Pathology | Type of DO (n=152) | Condition | Assessment |
|---|---|---|---|---|
| Craniofacial-midfacial DO (n=129) | Midfacial retrusion in craniofacial dysostosis | Frontofacial advancement (n=10) | Syndromal/cleft related | ++ |
| Anophtalmia Tessier 4 cleft | Orbital (n=4) | Syndromal/cleft related | ++ | |
| Median craniofacial cleft syndrome | Nasal dorsum (n=1) | Syndromal/cleft related | ++ | |
| Transverse maxillary deficiency | TPD bone-borne (n=93) | Dentofacial deformity | ++ | |
| Transverse maxillary deficiency | Hyrax tooth-borne (n=15) | Dentofacial deformity | ++ | |
| Midfacial retrusion (M. Crouzon) | Le-Fort III (n=1) | Syndromal/cleft related | ++ | |
| Maxillary retrusion (CLP) | Le Fort I (n=2) | Syndromal/cleft related | + – | |
| Deficiency of premaxilla (CLP) | Maxillary segment (n=2) | Syndromal/cleft related | + – | |
| Traumatic defect | Alveolar crest (n=1) | Trauma | – – | |
| Mandibular DO (n=23) | Postoperative defects after ablative surgery | Alveolar crest (n=6) | Oncologic | + + |
| Orthognathic (crowding) | Symphysis (n=5) | Dentofacial deformity | ++ | |
| Craniofacial microsomia | Ramus unilateral (n=6) | Syndromal/cleft related | + – | |
| Syndromal deficiency (TCS) | Ramus/corpus bilateral (n=5) | Syndromal/cleft related | ++ | |
| Neomandible | Alveolar crest (1) | Oncologic | ++ |
CLP, Cleft lip and palate; TCS, Treacher-Collins syndrome.
The grouping of the distraction procedures revealed that 114 distractions were applied to patients affected by dentofacial deformities (green). Thirty-one distraction procedures were performed in syndromal, syndrome-like, or cleft-related conditions (orange), 7 procedures were indicated after ablative oncologic surgery (blue), and only one alveolar ridge distraction was performed after maxillary trauma.
Transpalatal distraction (TPD) for the correction of transverse maxillary deficiency was the main distraction procedure. In 109 patients, gradual maxillary expansion with or without subsequent orthognathic surgery for the correction of an underlying dentofacial deformity was performed. In these patients, predominantly bone-borne distraction devices (n=94) were used as they offer different advantages when compared to tooth-borne orthodontic expansion appliances (Hyrax screws; n=15) [15]. TPD was also applied to a group of pediatric patients (n=8) improving the present deficiency before skeletal maturity [16].
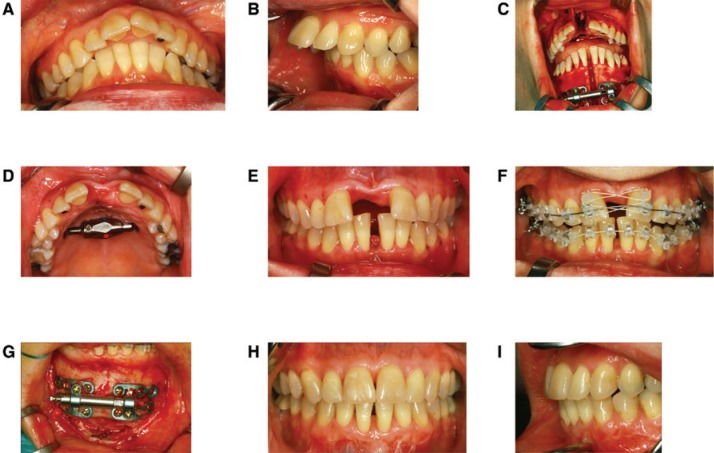
Figure 1A–I illustrates a case series of a 39-year-old female patient affected by a typical dentofacial deformity: transverse mandibulomaxillary deficiency and skeletal class II malocclusion. Skeletal deficiency was corrected by initial mandibulomaxillary (“two-jaw”) distraction followed by orthodontic treatment and subsequent orthognathic surgery.
Figure 1:
“Two-jaw distraction” for the correction of a transverse maxillary and mandibular deficiency (A) and corresponding skeletal class II malocclusion with increased overjet (B). Intraoperative situation after mounting two internal distraction devices to the upper and lower jaw. The desired amount of distraction is intraoperatively tested (C). Mandibulomaxillary expansion after the end of activation (D and E). The interdental gaps are closed by fixed orthodontic appliances during the consolidation phase (E and F). Complete bony consolidation in the symphyseal mandibular region at the time of device removal (G). Occlusal situation with physiologic overjet after additional orthognathic surgery 18 months after “two-jaw distraction” (H and I; orthodontic treatment by Dr. U. Jödecke, Fürstenwalde, Germany).
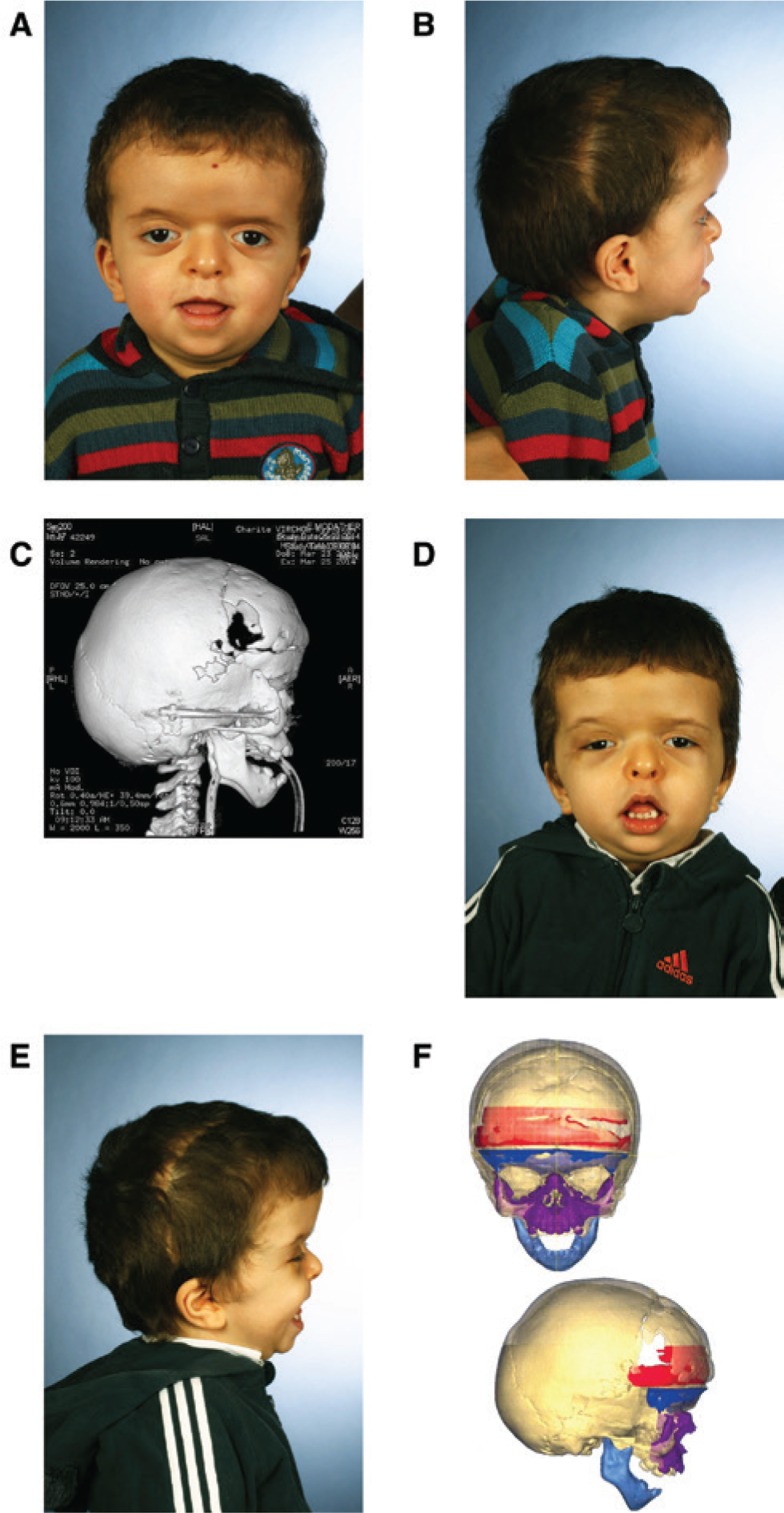
Patients affected by syndromal or cleft-related growth restrictions were the second group (n=31) having a clear benefit of corrective surgery by craniomaxillofacial DO as demonstrated in Figure 2A–F.
Figure 2:
3-year-old boy affected by craniofacial dysostosis (M. Apert) with midfacial retrusion.
Frontoorbital advancement with overcorrection had been performed in the first year of life (A and B). After computer-assisted frontofacial advancement of 17 mm by internal distraction devices (C), midfacial retrusion is improved (D and E). However, superimposition of predistraction and postdistraction data sets (DePuy Synthes ProPlan CMF; Materialise, Leuven, Belgium) reveals a lack of advancement in the central midface (F; violet zone), which is known to be one of the drawbacks of internal craniofacial distraction devices requiring additional corrective surgery.
In a 3-year-old boy affected by craniofacial dysostosis (M. Apert), severe midfacial retrusion after frontoorbital advancement in his first year of life was improved by computer-assisted frontofacial advancement of 17 mm by internal distraction devices. However, superimposition of predistraction and postdistraction data sets reveals a lack of advancement in the central midface. This is known to be one of the drawbacks of internal craniofacial distraction devices requiring additional corrective surgery. Staged surgeries and interdisciplinary treatment may also be required in rare conditions of growth restriction as demonstrated in Figure 3A–E.
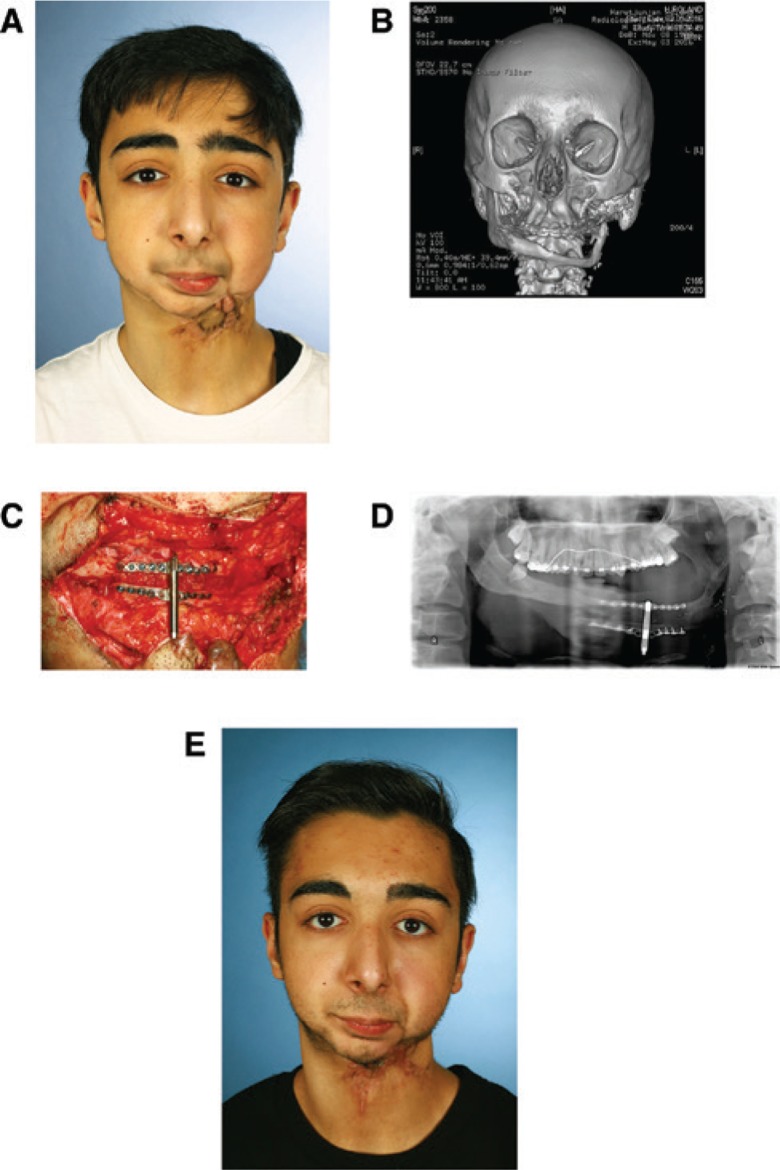
Figure 3:
17-year-old patient with a lower facial deformity after resection of a dermoid fibroma of the left mandible in early childhood followed by microvascular fibular reconstruction at age 9 years (A and B), “upside-down insertion” and intraoperative testing of an alveolar ridge distraction device for vertical augmentation of the “neomandible” (C), OPTG 8 weeks after the end of activation with ongoing mineralization in the distraction zone (D), dental implants can be placed at time of device removal, and corresponding clinical situation (E). Hypertrophic scars have been resected during device insertion. Gradual expansion was helpful in the management of submandibular soft tissues.
An improvement of the lower facial deformity after resection of a dermoid fibroma of the left mandible in early childhood followed by microvascular fibular reconstruction at age 9 years was achieved in a 17-year-old patient by “upside-down insertion” of an alveolar ridge distraction device. Vertical augmentation of the “neomandible” will be followed by the insertion of dental implants for a contemporary prosthodontic rehabilitation of the patient. Gradual expansion proved to be helpful in the management of the hypertrophic and scarred soft tissues.
Overall, in the majority of patients, intended skeletal and soft-tissue expansion could be realized with a low rate of distraction-related complications. Therefore, and overall assessment of the results was predominantly positive (++). The activation of the devices and regular controls during the activation phase was not a real burden even in pediatric patients. Minor complications such as the loosening of devices or activation-related pain were typically manageable in an outpatient setting. In the TPD group only in one mentally handicapped patient, relevant infection of the alveolar crest occurred leading to the failure of the procedure and permanent loss of teeth and bone. In another patient who underwent alveolar ridge augmentation after traumatic tooth loss, failure occurred due to the fact that interdisciplinary prosthodontic treatment could not be realized within the appropriate time frame (–). In the group of syndromal patients, no relevant distraction-related complications occurred. In the group of patients who underwent maxillary distraction and unilateral mandibular distraction, strain during activation and long-term stability were the issues (+–). However, the majority of patients indicated that they would undergo a craniomaxillofacial distraction procedure again.
Discussion
DO is an established method for the correction of skeletal deficiencies and is applicable to the whole skeleton [17], [18]. Almost 100 years after the first successful callus distraction in humans, the underlying physiology is better but not fully understood [19]. On the molecular level, there seems to be a complex differentiation of cells, which is mediated by mechanotransduction of the cytoskeleton corresponding to the “tension-stress effect” originally described by Ilizarov. As not only bone but also the surrounding soft tissues are expanded by gradual distraction, this principle can be regarded as an “in vivo bioreactor” and distraction histiogenesis seems to be a more appropriate term [20]. However, the successful application of this principle requires certain conditions. The stability in the distraction zone is crucial for the mineralization process during the consolidation phase as shown in experimental settings [12]. According to our personal experiences, the main factor for successful DO is stability; during the activation phase, there must be a characteristic haptic feedback of the tissues followed by stable conditions afterwards and then complete mineralization of the callus is likely to occur.
In orthognathic surgery, there seems to be a focus on classic osteotomies, as they provide fast and reliable results, and most of the skeletal discrepancies can be corrected by classic surgeries faster than by distraction procedures. In orthognathic patients, DO seems to be indicated if transverse maxillary deficiency is more than 6 mm and sagittal discrepancies exceed 12 mm. However, additional factors might have an influence when choosing the appropriate procedure (age, tissue conditions, patient’s compliance and comorbidities, and patient’s and surgeon’s preferences). In reconstructive surgery or syndromal patients when soft tissues should be addressed or growth impairment has to be managed, the principle of gradual expansion seems to be convincing; however, the decision is likely based on the individual situation [21], [22]. Due to the lack of appropriate studies, there is no evidence that one method is superior to the other so far.
Mandibular alveolar crest augmentation by vertical distraction was stopped after a small group of patients. The time frame for the prosthodontic rehabilitation was quite long, so the oncologic surgical protocol switched to primary microvascular reconstruction of ablative defects [23].
The role of mandibular DO in the management of craniofacial microsomia still remains unclear [24]. For the correction of dentofacial asymmetries, classic orthognathic procedures early after skeletal maturity seem to be more convenient for the patients compared to distraction procedures, which is in accordance to the personal experiences [25]. However, in craniofacial dysostosis syndromes, such as M. Crouzon or M. Apert, which are characterized by severe growth impairment of the craniofacial skeleton, gradual expansion procedures by DO are able to correct functional and psychosocial impairment already at an early age and seem to have advantages when compared to classic osteotomies [26], [27].
However, it has to be pointed out that craniofacial distraction procedures normally are not able to correct the complex underlying pathologies within one setting and secondary corrections are typically needed. Nevertheless, a clear improvement of the initial situation can be achieved by creating additional bone stock and preparing the surrounding soft tissues for further surgical procedures within staged individualized treatment concepts [28]. Appropriate distraction devices for almost all craniomaxillofacial indications are commercially available or can be manufactured. If internal or external devices are selected, it is best decided on the individual situation. Contemporary computer-assisted workflows support planning, transfer, and evaluation of craniofacial distraction procedures [29], [30].
According to these personal experiences, craniomaxillofacial DO is certainly an option if severe skeletal deficiency or growth restriction is present or has to be expected. TPD can be recommended for the correction of transverse maxillary deficiency. Gradual frontofacial advancement is a powerful tool for the correction of craniomaxillofacial growth restriction within the individually staged interdisciplinary management of patients affected by syndromal craniosynostosis or comparable craniofacial anomalies.
Conclusion
With regard to the overall number of patients who received craniomaxillofacial therapy in 14 years (n>30,000), craniomaxillofacial DO certainly plays a minor role (<1% of all patients). However, if severe growth restriction is present or has to be expected, craniomaxillofacial DO should be regarded as an additional reconstructive option for patients affected by craniofacial or dentofacial anomalies within an staged individual treatment plan.
Supporting Information
Acknowledgments
Special thanks to Prof. Dr. E.J. Haberl (Pediatric Neurosurgery, University Bonn, Germany), who was involved in the craniofacial correction of patient 2; Franz Hafner for his organizational skills in arranging the photodocumentation for this article; and Dr. Nadine Thieme (Charité Radiology Department/Head: Prof. Dr. B. Hamm) for providing DICOM datasets and CT scans in patients 2 and 3.
Supplemental Material
The article (DOI: iss-2016-0027) offers reviewer assessments as supplementary material.
Author Statement
Research Funding: Authors state no funding involved. Conflict of interest: Authors state no conflict of interest. Informed consent: Informed consent has been obtained from all individuals obtained in this study. Ethical approval: The research related to human use complied with all the relevant national regulations and institutional policies, was performed in accordance to the tenets of the Helsinki Declaration, and has been approved by the author’s institutional review board or equivalent committee.
Author Contributions
Nicole Ernst: Involved in most of the distraction procedures described in this review from 2007 on as surgical resident with regard to device insertion, device activation/removal and corresponding documentation. Retrospective evaluation of all patients who received transpalatal distraction procedures; concept of the manuscript and selection of illustrations.
Nicolai Adolphs: From 2006 as specialist, from 2009 on as consultant responsible for the treatment of patients affected by dentofacial and craniofacial anomalies; involved in the treatment of all patients that received distraction procedures; final revision of the manuscript before submission.
Publication Funding
The German Society of Surgery funded the article processing charges of this article.
References
- [1].Codivilla A. On the means of lengthening, in the lower limbs, the muscles and tissues which are shortened through deformity. Clin Orthop Relat Res 1994;4–9. [PubMed]; Codivilla A. On the means of lengthening, in the lower limbs, the muscles and tissues which are shortened through deformity. Clin Orthop Relat Res. 1994:4–9. [PubMed] [Google Scholar]
- [2].Wiedemann M. Callus distraction: a new method? A historical review of limb lengthening. Clin Orthop Relat Res 1996;291–304. [PubMed]; Wiedemann M. Callus distraction: a new method? A historical review of limb lengthening. Clin Orthop Relat Res. 1996:291–304. [PubMed] [Google Scholar]
- [3].Honig JF, Grohmann UA, Merten HA. Facial bone distraction osteogenesis for correction of malocclusion: a more than 70-year-old concept in craniofacial surgery. Plast Reconstr Surg 2002;109:41–44. [DOI] [PubMed]; Honig JF, Grohmann UA, Merten HA. Facial bone distraction osteogenesis for correction of malocclusion: a more than 70-year-old concept in craniofacial surgery. Plast Reconstr Surg. 2002;109:41–44. doi: 10.1097/00006534-200201000-00007. [DOI] [PubMed] [Google Scholar]
- [4].Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res 1989;263–285. [PubMed]; Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res. 1989:263–285. [PubMed] [Google Scholar]
- [5].Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res 1989;249–281. [PubMed]; Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989:249–281. [PubMed] [Google Scholar]
- [6].Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res 1990;8–26. [PubMed]; Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res. 1990:8–26. [PubMed] [Google Scholar]
- [7].Snyder CC, Levine GA, Swanson HM, Browne EZ Jr. Mandibular lengthening by gradual distraction. Preliminary report. Plast Reconstr Surg 1973;51:506–508. [DOI] [PubMed]; Snyder CC, Levine GA, Swanson HM, Browne EZ Jr.. Mandibular lengthening by gradual distraction. Preliminary report. Plast Reconstr Surg. 1973;51:506–508. doi: 10.1097/00006534-197305000-00003. [DOI] [PubMed] [Google Scholar]
- [8].Michieli S, Miotti B. Lengthening of mandibular body by gradual surgical-orthodontic distraction. J Oral Surg 1977;35:187–192. [PubMed]; Michieli S, Miotti B. Lengthening of mandibular body by gradual surgical-orthodontic distraction. J Oral Surg. 1977;35:187–192. [PubMed] [Google Scholar]
- [9].McCarthy JG, editor. Distraction of the Craniofacial Skeleton. 1st ed. New York: Springer, 1999.; McCarthy JG, editor. Distraction of the Craniofacial Skeleton. 1st ed. New York: Springer; 1999. [Google Scholar]
- [10].McCarthy JG, Schreiber J, Karp N, Thorne CH, Grayson BH. Lengthening the human mandible by gradual distraction. Plast Reconstr Surg 1992;89:1–8; discussion 9–10. [PubMed]; McCarthy JG, Schreiber J, Karp N, Thorne CH, Grayson BH. Lengthening the human mandible by gradual distraction. Plast Reconstr Surg. 1992;89:1–8. discussion 9–10. [PubMed] [Google Scholar]
- [11].Nada RM, Sugar AW, Wijdeveld MG, et al. Current practice of distraction osteogenesis for craniofacial anomalies in Europe: a web based survey. J Craniomaxillofac Surg 2010;38:83–89. [DOI] [PubMed]; Nada RM, Sugar AW, Wijdeveld MG. et al. Current practice of distraction osteogenesis for craniofacial anomalies in Europe: a web based survey. J Craniomaxillofac Surg. 2010;38:83–89. doi: 10.1016/j.jcms.2009.03.014. [DOI] [PubMed] [Google Scholar]
- [12].Adolphs N, Kunz C, Pyk P, Hammer B, Rahn B. Callus mineralization following distraction osteogenesis of the mandible monitored by scanning acoustic microscopy (SAM). J Craniomaxillofac Surg 2005;33:314–317. [DOI] [PubMed]; Adolphs N, Kunz C, Pyk P, Hammer B, Rahn B. Callus mineralization following distraction osteogenesis of the mandible monitored by scanning acoustic microscopy (SAM) J Craniomaxillofac Surg. 2005;33:314–317. doi: 10.1016/j.jcms.2005.03.002. [DOI] [PubMed] [Google Scholar]
- [13].Kunz C, Adolphs N, Buescher P, Hammer B, Rahn B. Distraction osteogenesis of the canine mandible: the impact of acute callus manipulation on vascularization and early bone formation. J Oral Maxillofac Surg 2005;63:93–102. [DOI] [PubMed]; Kunz C, Adolphs N, Buescher P, Hammer B, Rahn B. Distraction osteogenesis of the canine mandible: the impact of acute callus manipulation on vascularization and early bone formation. J Oral Maxillofac Surg. 2005;63:93–102. doi: 10.1016/j.joms.2004.07.008. [DOI] [PubMed] [Google Scholar]
- [14].Kunz C, Adolphs N, Büscher P, Hammer B, Rahn B. Mineralization and mechanical properties of the canine mandible distraction wound following acute molding. Int J Oral Maxillofac Surg 2006;35:822–827. [DOI] [PubMed]; Kunz C, Adolphs N, Büscher P, Hammer B, Rahn B. Mineralization and mechanical properties of the canine mandible distraction wound following acute molding. Int J Oral Maxillofac Surg. 2006;35:822–827. doi: 10.1016/j.ijom.2006.03.018. [DOI] [PubMed] [Google Scholar]
- [15].Adolphs N, Ernst N, Menneking H, Hoffmeister B. Transpalatal distraction–state of the art for the individual management of transverse maxillary deficiency–a review of 50 consecutive cases. J Craniomaxillofac Surg 2014;42:1669–1674. [DOI] [PubMed]; Adolphs N, Ernst N, Menneking H, Hoffmeister B. Transpalatal distraction–state of the art for the individual management of transverse maxillary deficiency–a review of 50 consecutive cases. J Craniomaxillofac Surg. 2014;42:1669–1674. doi: 10.1016/j.jcms.2014.05.011. [DOI] [PubMed] [Google Scholar]
- [16].Adolphs N, Ernst N, Hoffmeister B, Raguse JD. Transpalatal distraction for the management of maxillary constriction in pediatric patients. Ann Maxillofac Surg 2015;5:44–48. [DOI] [PMC free article] [PubMed]; Adolphs N, Ernst N, Hoffmeister B, Raguse JD. Transpalatal distraction for the management of maxillary constriction in pediatric patients. Ann Maxillofac Surg. 2015;5:44–48. doi: 10.4103/2231-0746.161058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Hankemeier S, Bastian L, Gosling T, Krettek C. Principles of callus distraction. Unfallchirurg 2004;107:945–958. [DOI] [PubMed]; Hankemeier S, Bastian L, Gosling T, Krettek C. Principles of callus distraction. Unfallchirurg. 2004;107:945–958. doi: 10.1007/s00113-004-0842-7. [DOI] [PubMed] [Google Scholar]
- [18].Bell HW, Guerrero CA, editors. Distraction Osteogenesis of the Facial Skeleton. Hamilton, Ontario, Canada: BC Decker, Inc, 2007.; Bell HW, Guerrero CA, editors. Distraction Osteogenesis of the Facial Skeleton. Hamilton, Ontario, Canada: BC Decker, Inc; 2007. [Google Scholar]
- [19].Van Sickels JE. Distraction osteogenesis: advancements in the last 10 years. Oral Maxillofac Surg Clin North Am 2007;19:565–574, vii. [DOI] [PubMed]; Van Sickels JE. Distraction osteogenesis: advancements in the last 10 years. Oral Maxillofac Surg Clin North Am. 2007;19:565–574. doi: 10.1016/j.coms.2007.06.004. vii. [DOI] [PubMed] [Google Scholar]
- [20].Dhaliwal K, Kunchur R, Farhadieh R. Review of the cellular and biological principles of distraction osteogenesis: an in vivo bioreactor tissue engineering model. J Plast Reconstr Aesthet Surg 2016;69:e19–e26. [DOI] [PubMed]; Dhaliwal K, Kunchur R, Farhadieh R. Review of the cellular and biological principles of distraction osteogenesis: an in vivo bioreactor tissue engineering model. J Plast Reconstr Aesthet Surg. 2016;69:e19–e26. doi: 10.1016/j.bjps.2015.11.003. [DOI] [PubMed] [Google Scholar]
- [21].Labbe D, Nicolas J, Kaluzinski E, et al. Gunshot wounds: reconstruction of the lower face by osteogenic distraction. Plast Reconstr Surg 2005;116:1596–1603. [DOI] [PubMed]; Labbe D, Nicolas J, Kaluzinski E. et al. Gunshot wounds: reconstruction of the lower face by osteogenic distraction. Plast Reconstr Surg. 2005;116:1596–1603. doi: 10.1097/01.prs.0000187170.48370.76. [DOI] [PubMed] [Google Scholar]
- [22].Super S. Distraction osteogenesis in the treatment of dentofacial deformities. Alpha Omegan 2009;102:68–73. [DOI] [PubMed]; Super S. Distraction osteogenesis in the treatment of dentofacial deformities. Alpha Omegan. 2009;102:68–73. doi: 10.1016/j.aodf.2009.04.012. [DOI] [PubMed] [Google Scholar]
- [23].Adolphs N, Sproll C, Raguse JD, et al. Stable vertical distraction osteogenesis of highly atrophic mandibles after ablative tumour surgery of the oral cavity–a salvage pathway for mandibular reconstruction prior to oral rehabilitation with dental implants. J Craniomaxillofac Surg 2009;37:320–326. [DOI] [PubMed]; Adolphs N, Sproll C, Raguse JD. et al. Stable vertical distraction osteogenesis of highly atrophic mandibles after ablative tumour surgery of the oral cavity–a salvage pathway for mandibular reconstruction prior to oral rehabilitation with dental implants. J Craniomaxillofac Surg. 2009;37:320–326. doi: 10.1016/j.jcms.2009.01.003. [DOI] [PubMed] [Google Scholar]
- [24].Nagy K, Kuijpers-Jagtman AM, Mommaerts MY. No evidence for long-term effectiveness of early osteodistraction in hemifacial microsomia. Plast Reconstr Surg 2009;124:2061–2071. [DOI] [PubMed]; Nagy K, Kuijpers-Jagtman AM, Mommaerts MY. No evidence for long-term effectiveness of early osteodistraction in hemifacial microsomia. Plast Reconstr Surg. 2009;124:2061–2071. doi: 10.1097/PRS.0b013e3181bcf2a4. [DOI] [PubMed] [Google Scholar]
- [25].Posnick JC. Surgical correction of mandibular hypoplasia in hemifacial microsomia: a personal perspective. J Oral Maxillofac Surg 1998;56:639–650. [DOI] [PubMed]; Posnick JC. Surgical correction of mandibular hypoplasia in hemifacial microsomia: a personal perspective. J Oral Maxillofac Surg. 1998;56:639–650. doi: 10.1016/s0278-2391(98)90466-9. [DOI] [PubMed] [Google Scholar]
- [26].Adolphs N, Haberl EJ. Kraniofaziale Chirurgie: state of the art. Der MKG-Chirurg 2012;5:266–278.; Adolphs N, Haberl EJ. Kraniofaziale Chirurgie: state of the art. Der MKG-Chirurg. 2012;5:266–278. [Google Scholar]
- [27].Arnaud E, Marchac D, Renier D. The treatment of craniosynostosis: indications and techniques. Neurochirurgie 2006;52:264–291. [DOI] [PubMed]; Arnaud E, Marchac D, Renier D. The treatment of craniosynostosis: indications and techniques. Neurochirurgie. 2006;52:264–291. doi: 10.1016/s0028-3770(06)71221-8. [DOI] [PubMed] [Google Scholar]
- [28].Adolphs N, Ernst N, Menneking H, Hoffmeister B. Significance of distraction osteogenesis of the craniomaxillofacial skeleton–a clinical review after 10 years of experience with the technique. J Craniomaxillofac Surg 2014;42: 966–975. [DOI] [PubMed]; Adolphs N, Ernst N, Menneking H, Hoffmeister B. Significance of distraction osteogenesis of the craniomaxillofacial skeleton–a clinical review after 10 years of experience with the technique. J Craniomaxillofac Surg. 2014;42:966–975. doi: 10.1016/j.jcms.2014.01.018. [DOI] [PubMed] [Google Scholar]
- [29].Adolphs N, Schulz M, Haberl HJ, Hoffmeister B. Computer-assistierte kraniofaziale Chirurgie. Chirurg Praxis 2016;80:663–676.; Adolphs N, Schulz M, Haberl HJ, Hoffmeister B. Computer-assistierte kraniofaziale Chirurgie. Chirurg Praxis. 2016;80:663–676. [Google Scholar]
- [30].Adolphs N, Haberl EJ, Liu W, Keeve E, Menneking H, Hoffmeister B. Virtual planning for craniomaxillofacial surgery–7 years of experience. J Craniomaxillofac Surg 2014;42:e289–e295. [DOI] [PubMed]; Adolphs N, Haberl EJ, Liu W, Keeve E, Menneking H, Hoffmeister B. Virtual planning for craniomaxillofacial surgery–7 years of experience. J Craniomaxillofac Surg. 2014;42:e289–e295. doi: 10.1016/j.jcms.2013.10.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.