Abstract
Background
Writer’s cramp (WC) is a form of focal hand dystonia, for which focal botulinum neurotoxin (BoNT) injections are the current best therapy. Past studies have shown that some types of rehabilitative therapy can be useful. We hypothesized that BoNT together with a specific type of occupational therapy would be better than BoNT alone for treating WC patients comparing the effects with a patient-rated subjective scale.
Methods
Twelve WC patients were randomized to two groups. Six received only BoNT therapy and 6 received BoNT & occupational therapy. The occupational therapy involved specific exercises of finger movements in the direction opposite to the dystonic movements during writing. BoNT was injected by movement disorders neurologists in the affected muscles under electromyography-guidance. The primary outcome was the patient-rated subjective scale at 20 weeks. Secondary exploratory outcomes included the writer’s cramp rating scale (WCRS), writer’s cramp impairment scale (WCIS), the writer’s cramp disability scale (WCDS), handgrip strength and kinetic parameters.
Results
The patient-rated subjective scale scores at 20 weeks were not significantly different between the two groups. Significant objective improvement was noted in the BoNT & occupational therapy group, as noted by the decrease (28%) in WCIS scores.
Conclusions
Improvement of the primary outcome measure, the patient-rated subjective scale, was not achieved. However, significant improvement was found in the BoNT & occupational therapy group in a secondary measure of impairment. Our hypothesis-driven study results are likely limited by small sample size, and further large-scale studies of occupational therapy methods to improve the efficacy of BoNT seems worthwhile.
Keywords: writer’s cramp, dystonia, focal, hand, botulinum, toxin, occupational, therapy
1. Introduction
Writer’s cramp (WC) is the most common type of task-specific dystonia involving the upper extremity(1). It is presumed to be triggered by repetitive writing, and affected individuals often report exposure to long periods of writing. Genetic factors are also thought to play a role. When the disorder worsens, the dystonia may no longer be task specific, and can occur with other manual tasks(1). As a result, writer’s cramp has been shown to have a negative impact on patients’ quality of life(2).
Various types of therapy have been introduced as treatment for WC, of which botulinum neurotoxin (BoNT) injections are considered to be the most beneficial at this time(3, 4). While focal BoNT injection of the dystonic muscles can be helpful, a limitation of BoNT is its temporary effects. Past studies have shown that some types of rehabilitative therapy can be useful. For example, sensory training has been attempted as treatment for focal hand dystonia, and appears to be helpful (5). Motor training has also been attempted as treatment, and both individualized finger training and non-specific finger training have been found to be useful(6–9).
In WC, abnormal posturing of the fingers, hand or forearm are seen and can have unique patterns in different individuals. Practicing movements in the direction opposite to the dystonia may not only be helpful symptomatically, but also help to reverse the altered brain excitability, which has been shown by previous studies(10). BoNT injections could also help to weaken the dystonic movements and allow for the patient to perform these movements. We hypothesized that motor training, specifically performing movements in opposite directions to the dystonia might lead to additional improvement in WC patients injected with BoNT.
In this study, we compared the effects of BoNT therapy alone with a combination of BoNT &occupational therapy (OT) in patients with writer’s cramp as measured by a patient-rated subjective scale. Other outcomes, including the writer’s cramp rating scale (WCRS), writer’s cramp impairment scale (WCIS), writer’s cramp disability scale (WCDS) and kinetic parameters were also studied.
2. Methods
2.1. Subjects
Twelve patients with confirmed diagnosis of writer’s cramp were recruited. All participants’ medical histories were reviewed and neurological examinations were performed per standard procedures in the Medical Neurology Branch of the National Institute of Neurological Disorders and Stroke (NINDS). Mean age of participants was 64 (range: 53 −73 years).
2.2. Study design
The protocol was approved by the NIH Neuroscience IRB, and subjects gave informed consent. Participants were randomized to one of the two groups: BoNT alone or BoNT & OT group, by drawing a piece of paper that determined the assignment. The study was conducted at the National Institutes of Health Clinical Center outpatient clinic for nine visits over a 24-week period (See Table 1 for schedule of events). All visits consisted of responding to questions of the patient-rated subjective scale (a visual analogue scale shown as a 10 cm line, with 0 rated as no discomfort and 10 rated as maximal discomfort due to dystonia), and writer’s cramp disability scale (WCDS), videotaping of writer’s cramp rating scale (WCRS) and writer’s cramp impairment scale (WCIS) activities, handgrip measurements (using a commercially available dynamometer), and writing tasks using a pressure-sensitive digitizing tablet (WACOM Intuos; Wacom Europe, Neuss, Germany). Data obtained from the digitizing tablet were stored on a personal computer and analyzed using Neuroglyphics (developed by Camilo Toro, MD; available at http://www.neuroglyphics.org). Kinematic analyses were performed based on writing movements along the vertical axis (i.e., y-axis).
Table 1.
Schedule of Events.
| Visit # | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| Screening and history and physical | X | ||||||||
| Video-taping | X | X | X | X | |||||
| Rehab assess | X | X | |||||||
| Handgrip | X | X | X | X | X | X | X | X | X |
| BoNT Admin | X | X | |||||||
| Training | X | ||||||||
| Training assessment | X | X | X | X | X | X | X | X | |
| Log review | X | X | X | X | X | X | X | X | |
| WCRS | X | X | X | X | |||||
| WCIS/WCDS | X | X | X | X | |||||
| Tablet PC | X | X | X | X | |||||
| Subjective scale | X | X | X | X | X | X | X | X | X |
2.3. Clinical Assessment
Participants underwent a baseline history and neurological examination at their first visit by the examining neurologist. Participants were then asked to provide answers to questions of the patient-rated subjective scale and writer’s cramp disability scale (WCDS). The WCDS is composed of 24 questions related to problems that patients with WC typically experience with writing or other everyday activities. Baseline handgrip measurements were taken and the average of three trials was recorded. Patients were videotaped performing writing activities of the WCRS and WCIS, and scores were later given by video-raters blinded to the assignment. The video-raters were comprised of two movement disorders neurologists and a physiatrist who is a specialist in movement disorders. The WCIS (version 5.0) ratings were determined by the individual’s pen-grip posture and characteristics of dystonia (e.g., writing speed, number of breaks, and posture of the neck, shoulder, elbow, forearm, wrist, and fingers while writing, performance of writing continuous loops, mirror dystonia, spiral scores for tremor and accuracy and physician global rating). WCRS items included posture, latency of dystonia, tremor and writing speed.
Writing tasks included using the dominant hand to write a passage (“Mary had a little lamb, its fleece was white as snow, and everywhere that Mary went, the lamb was sure to go”), tracing spirals, making interconnected loops by drawing the letter ‘l’ serially. Patients were also asked to write the passage (‘Mary…”) with their non-dominant hand. These writing tasks were performed on paper (college-ruled paper for writing passages and loops, and blank paper for drawing spirals), and also on a digitizing tablet with and without paper.
2.4. Botulinum toxin injection
Following clinical assessment as detailed above, the patient’s dystonia was carefully examined by two neurologists blinded to the assignment of the patient and an occupational therapist. The pattern of the dystonia was closely observed by a panel of two to three movement disorders neurologists and muscles that appeared to be primarily affected based on the primary dystonic movements were injected with incobotulinumtoxin A (Xeomin®) under electromyography (EMG)-guidance, using standard dosing. When the direction of the primary dystonic movements was not clear, mirror movements were also observed and taken into account. Injections were performed by movement disorders neurologists twice during the study at visits 1 and 6, respectively, which were 12 weeks apart, and the same neurologist performed the injection at each visit for an individual patient. Details regarding the amount of injected BoNT and targeted muscles are shown in Table 2.
Table 2.
Patient characteristics and details of BoNT-injected muscles
| Pt # | Group allocation | Age | Daily medications | Handedness | Disease duration | Total BoNT dose (units) | Injected side/muscles |
|---|---|---|---|---|---|---|---|
| 1 | BoNT | 73 | Amlodipine 5mg qday, Celebrex 200mg 1 T BID PRN for pain, oxybutynin 10mg QID, tramadol 50mg 1 T TID, acetaminophen 325mg 2 T prn for pain, hydrochlorothiazide 25mg qday, esomeprazole 40mg qday, cetirizine 10mg qday, magnesium 1 T qday, multivitamin 1T qday, omega-3 1200mg BID, calcium 500mg BID, biotin 2500 mg qday | Left | 23 years | 85 | L UE. FDP: 15, FDS: 10, FPB:5, Trapezius: 55 |
| 2 | BoNT | 61 | Atorvastatin 10 mg qhs, metformin 1000 mg qday, levothyroxine 25 mcg qday, carvedilol 3.125 mg qday | Right | 25 years | 26 | R UE. FPB: 5, FDS digit iv: 15, lumbrical ii: 3, lumbrical iii: 3. |
| 3 | BoNT | 66 | Omeprazole 20 mg qday, aspirin 81mg qday | Right | 4 years | 50 | R UE. Teres major: 20, ECR: 15, ECU: 15. |
| 4 | BoNT | 61 | Calcium and hormone supplements daily | Right | 30 years | 17 | R UE. FDS ii-v: 10, FPL: 7 |
| 5 | BoNT | 51 | None | Left | 13 years | 27.5 | L UE. FDS ii-iii: 15, FDS iv-v: 10, FPL: 2.5 |
| 6 | BoNT | 60 | None | Right | 16 years | 54 | R UE. ECU: 15, FDS iii,iv: 15, FPB: 4, Pronator:10, Trapezius: 10 |
| 7 | BoNT & OT | 63 | Levothyroxine 50 mcg qday, Alendronate 1 tablet qweek, melatonin prn for insomnia, calcium/vitamin D PRN | Right | 19 years | 32.5 | R UE. FDS: 10, FPL: 7.5, Pronator teres:15 |
| 8 | BoNT & OT | 72 | Valsartan/HCTZ 80/12.5mg qday, pantoprazole CR 20mg qday, multivitamin 1 tablet qday | Right | 42 years | 21 | R UE. FDS ii-v: 14, FPL: 7 |
| 9 | BoNT & OT | 56 | HCTZ 25mg qday, atorvastatin 20mg qhs, aspirin 81mg qday, multivitamin 1tablet qday | Right | 17 years | 32 | R UE. FDS ii-iii: 15, FDS iv-v: 12, FPL: 5 |
| 10 | BoNT & OT | 60 | levothyroxine 25 mcg qday | Right | 18 years | 49 | R UE. FDS ii, iii: 14, FPL: 5, Trapezius: 30 |
| 11 | BoNT & OT | 61 | Aspirin 81mg qday, atorvastatin 40mg qhs | Left | 30 years | 52 | L UE. FDS: 10, FPL: 7, Pronator teres:15, Trapezius: 20 |
| 12 | BoNT & OT | 65 | None | Right | 9 years | 32 | R UE. FDS ii-v: 15, FPL: 7, Pronator teres: 10 |
Abbreviations: Pt: patient, BoNT: Botulinum neurotoxin, OT: Occupational therapy, R: right, L: left, UE: upper extremity, FDP: flexor digitorum profundus, FDS: flexor digitorum superficialis, FPB: flexor pollicis brevis, FPL: flexor pollicis longus, ECU: extensor carpi ulnaris.
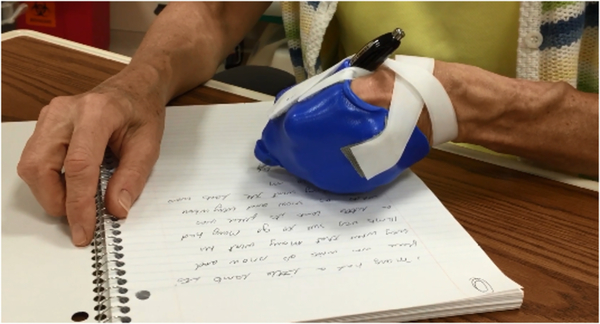
2.5. Motor Training
Subjects who were assigned to the BoNT & OT group underwent assessment by an occupational therapist (B.H.), and an isometric splint was fabricated to assist the patient to perform finger movements in the direction opposite to the patient’s own dystonic movements. (See Figure 1.) These subjects were instructed to wear this splint while performing daily 30-minute writing exercises for the entire study period. Journals were provided to perform the daily writing, and these were reviewed by the occupational therapist at subsequent visits to the clinical center in order to confirm compliance.
Figure 1.
Example of an isometric splint customized for a patient.
2.6. Data Acquisition and Analysis
Power analysis was conducted to determine the number of subjects. In previous studies, subjective improvement was used to assess responsiveness to therapy. Wissel et al noted that 80.6% had greater than 20% subjective benefit when analyzing the best ever recorded subjective responsed over the entire study period(18). Lungu et al reported a similar trend, where 55% of patients had 25–50% subjective benefit(15). Based on these results, we postulated that BoNT alone would provide 50% subjective benefit to the patient. We anticipated that combining occupational therapy and BoNT injections would result in 30% additional benefit, and assumed a common standard deviation of 15%. Power analysis was conducted based on two sample t-tests based on the assumption that a mean improvement of the BoNT only group is 50% and a mean improvement with BoNT & OT therapy is at least 80% (common standard deviation of 15%). With a significance level of 0.05, a total sample size of 12 (6 per each group) is required to obtain 80% power.
The primary outcome of the study was the relative change of the patient-rated subjective scale, which was calculated for each patient using the formula: 100*(V1-V8)/V1 (V1: baseline visit, V8: visit at 20 weeks). The patient-rated subjective scale was compared to baseline to assess for any continued benefit at 20 weeks. Secondary outcome measures included the WCRS, WCIS and kinematic parameters obtained via the new tablet PC-based writing analysis program. Scores (WCRS and WCIS) were given by blinded raters (two movement disorders neurologists and one physiatrist with expertise in movement disorders) based on videos of patients performing tasks including spiral drawing, writing passages (“Mary…”), and writing serial l’s (loops).
Statistical analyses were performed using SAS version 9.4. For the primary outcome, Wilcoxon rank sum test was used to evaluate the effect of occupational therapy by testing the difference in relative change, between the two groups. For secondary outcomes, repeated measures analysis of variance (RM-ANOVA) was applied to evaluate the effect of occupational therapy. The group (BoNT vs. OT) was a between-subject factor, and visit (baseline vs. 20 weeks, or V1 vs. V8) was a within-subject factor. The statistical model contained group, visit and the interaction between group and visit.
3. Results
All subjects (n=12, M:F=5:7) completed the study and remained compliant during the enrollment period. The mean age of participants was 62 years (range: 51 −73 years, standard deviation 6 years). The mean duration of illness was 21 years (range: 4 – 42 years, standard error 3 years); for each group, the mean duration of illness was 19 years (range: 4 – 25 years, standard error: 4 years) in the BoNT group and 23 years (range: 9 – 42 years, standard error: 5 years) in the BoNT & OT group. Table 2 shows the characteristics of patients. The pattern of dystonia was primarily flexion in both groups, as shown in Table 2; with some patients having mixed elements of extension, pronation or shoulder elevation (e.g., Patients # 3, 6, 7, 10, 11 and 12).
The relative change of the patient-rated subjective scale scores at 20 weeks was not significantly different between the two groups. RM-ANOVA showed the interaction between group and visit was significant (p=0.0327), which indicated that the change from baseline to 20 weeks in the BoNT group was different from that in the OT group. A significant (p=0.0174) decrease in WCIS (average score at visit 1, baseline: 24.6, average score at visit 8 (20 weeks): 18.1) in the BoNT & OT group and an increase in WCRS (average score at visit 1: 8, average score at visit 8: 12) in the BoNT group were found. This indicates improvement as indicated by WCIS in the BoNT & OT group and worsening as indicated by WCRS in the BoNT group, the latter finding which is questionable in significance. However, as the baseline scores of the two groups were found to be significantly different on our statistical analysis, this does not allow for a reliable comparison between the two groups. For other secondary outcome measures (WCDS, handgrip, and kinematic data including spiral error), no significant differences were found. Table 3 shows the scores at baseline and at visit 8 for the patient-rated subjective scale, WCDS, WCIS and WCRS.
Table 3.
Scores and handgrip strength obtained at baseline and follow-up visit.
| Pt # | Group allocation | Visual Analogue Scale (V1, V8) | WCDS (V1, V8) | WCIS (V1, V8) | WCRS (V1, V8) | Handgrip (kg) (V1, V8) |
|---|---|---|---|---|---|---|
| 1 | BoNT | 2.9, 4.2 | 19, 7 | 15.3, 17.8 | 10, 10.5 | 19.5, 13.8 |
| 2 | BoNT | M, M | M, 13 | 17.3, 17.3 | 4.8, 8 | M, 27.4 |
| 3 | BoNT | 7.7, 5.8 | 24, 10 | 20.8, 24.8 | 8.3, 14.5 | 40.1, 32.4 |
| 4 | BoNT | 8.8, 7.8 | 17, 7 | 18.0, 16.8 | 6, 8.5 | 28.7, 28.0 |
| 5 | BoNT | 6.3, 4.3 | 18, 14 | 22.3, 24.5 | 12.5, 12.5 | 31.0, 31.0 |
| 6 | BoNT | 8.8, 1.4 | 21, 20 | 22.0, 23.5 | 8, 15 | 9.3, 17.6 |
| Average | 6.9, 3.9 | 19.8, 11.8 | 19.3, 20.8 | 8.3, 11.5 | 25.7, 25.0 | |
| 7 | BoNT & OT | 8.7, 1.5 | 20, 9 | 23.8, 15.0 | 14.0, 11.5 | 19.3, 17.0 |
| 8 | BoNT & OT | 2.9, 3.2 | 20, 16 | 23.3, 21.5 | 10, 12.5 | 24.9, 25.1 |
| 9 | BoNT & OT | 5.3, 3.8 | 31, 21 | 24.3, 27.0 | 11.3, 11.0 | 35.4, 34.7 |
| 10 | BoNT & OT | 8.1, 3 | 19, 12 | 22.5, 21.3 | 10.5, 10.8 | 29.6, 22.0 |
| 11 | BoNT & OT | M, 4.1 | 19, 13 | 25.0, 12.3 | 5.3, 1.5 | 17.8, 23.2 |
| 12 | BoNT & OT | 5.3, 3.4 | 21, 13 | 28.8, 11.5 | 16.3, 7.0 | 21.0, 11.4 |
| Average | 6.1, 3.2 | 21.7, 14.0 | 24.6, 16.4 | 11.2, 9.0 | 24.7, 22.2 |
Abbreviations: Pt: patient, BoNT: Botulinum neurotoxin, OT: Occupational therapy, V1: Visit 1, V8: Visit 8, WCDS: Writer’s cramp Disability Scale, WCIS: Writer’s cramp Impairment Scale, WCRS: Writer’s cramp Rating Scale. M denotes missing values.
The following writing parameters obtained from the tablet PC were assessed for which no significant group differences were found: spiral accuracy measured by assessing deviation from ideal, expressed as a root mean deviation, time to perform the drawing or writing, tremor frequency, change in inclination of the pen as measured by degrees of deviation, change in inclination measured by ascertaining degrees of deviation from the original grip around the Azimuth (polar coordinates). Mean handgrip in each group were not found to be statistically different and were 24.7 kg (BoNT & OT therapy group) and 25.7 kg (BoNT group) at initial evaluation (visit 1) and 22.2 kg and 25 kg at visit 8, respectively (see Table 3).
4. Discussion
Our study results show that the patient-rated subjective scale scores at 20 weeks were not significantly different between the two groups; however, a trend for greater improvement in the BoNT & OT therapy group (40% decrease in Visual Analogue Scale[VAS] scores) was noted, compared to the BoNT therapy group (21% decrease in VAS scores). For WCIS, improvement was noted in the BoNT & OT group, suggesting that combining BoNT injections and occupational therapy may result in a beneficial effect, but as the baseline scores of the two groups were found to be significantly different, this does not allow for a reliable between-group comparison.
In this study, we also conducted kinematic analysis of pen-tip position data obtained during writing tasks (writing passages, drawing loops, and spirals) performed on a pressure-sensitive digitizing tablet. This type of device has been used as an objective tool to analyze various writing parameters(11, 12). A previous study found that mean stroke frequency was reduced in patients with dystonia when drawing circles, and increased variability of mean vertical peak velocity relative to control subjects. No statistical differences in kinematic parameters were found between the two treatment groups, which we interpret as the two groups having similar severity.
Writer’s cramp is the most common type of focal hand dystonia, for which BoNT injections are the most efficacious treatment to date(3, 13). While the administration of BoNT is generally safe and effective for symptoms in this patient group, treatment effects vary and the benefit is also only temporary, usually lasting around 12 weeks(14, 15). Other types of treatment have been attempted for a permanent effect, involving mostly invasive interventions such as deep brain stimulation or stereotactic thalamotomy(16, 17).
In our study, we attempted to use physical therapy to possibly amplify the beneficial effects of BoNT injection. Occupational therapy in this study involved subjects performing daily writing exercises while wearing a splint that was custom-made to counteract the dystonic movements. Previous studies have shown that motor training can help with writer’s cramp, and by delivering BoNT to weaken the dystonic muscles and using customized splints while writing, we hypothesized that this would ultimately result in lesser severity of dystonia(7).
Our study has several potential limitations. A major limitation of the study is its relatively small sample size. This is associated with other limitations, such as the presence of different patterns of dystonia within our small sample that may result in varying degrees of clinical severity, impairment and disability. While we also aimed to compare several secondary outcome measures between the two groups, our statistical analysis showed that the two groups had different baseline scores that did not allow for a reliable comparison (e.g., different baseline scores of WCIS).
Our study is the first to assess the effects of combining BoNT injections with OT to only BoNT injections on WC patients in a randomized, double-blinded fashion. While we did not find a statistically significant difference of patient-rated subjective scale scores between the two groups, a trend for improvement was seen and. future larger-scale studies are necessary to further establish the additive effect of customized occupational therapy on chemo-denervation achieved by BoNT injection.
5. Conclusions
The study was powered on the expected effect size of the primary outcome measure of subjective improvement; this was not achieved. While comparison of secondary measures between the two treatmeant groups was limited due to differences in baseline disease severity between the two groups, our study results suggest that objective impairment was improved in the BoNT & OT therapy group. Therefore, our results indicate a limitation of sample size, and a future large-scale study using occupational therapy methods to improve the efficacy of BoNT seems worthwhile.
Writer’s cramp is a type of focal hand dystonia for which focal botulinum toxin injections are the current best therapy
We conducted a randomized, double-blinded study to study the additive effects of occupational therapy on focal hand dystonia
No significant improvement was found between the two groups; however, significant objective benefit in the group that also received occupational therapy was found.
Our study results were drawn from a relatively small sample size and have limited significance; future large-scale study using occupational therapy methods to improve the efficacy of botulinum toxin injections seems worthwhile.
Acknowledgements
The research was done in the Intramural Program of NINDS. The authors are grateful to our study participants who were generous with their time and effort that made it possible to complete the study.
Conflicts of interest
The authors have no relevant conflicts of interest other than research support from Merz North America.
Funding
This study was funded by Merz North America and the National Institute of Neurological Disorders and Stroke (NINDS).
Ethical Statement
This study was approved by the NIH Neuroscience IRB, and subjects gave informed consent.
Abbreviations
- WC
Writer’s cramp
- BoNT
Botulinum neurotoxin
- OT
Occupational therapy
- WCRS
Writer’s cramp Rating Scale
- WCIS
Writer’s cramp Impairment Scale
- WCDS
Writer’s cramp Disability Scale
- EMG
Electromyography
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hallett M Pathophysiology of writer’s cramp. Hum Mov Sci. 2006;25(4–5):454–63. [DOI] [PubMed] [Google Scholar]
- 2.Pekmezovic T, Svetel M, Ivanovic N, Dragasevic N, Petrovic I, Tepavcevic DK, et al. Quality of life in patients with focal dystonia. Clin Neurol Neurosurg. 2009;111(2):161–4. [DOI] [PubMed] [Google Scholar]
- 3.Hallett M, Benecke R, Blitzer A, Comella CL. Treatment of focal dystonias with botulinum neurotoxin. Toxicon. 2009;54(5):628–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karp BI. Botulinum toxin physiology in focal hand and cranial dystonia. Toxins (Basel). 2012;4(11):1404–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeuner KE, Bara-Jimenez W, Noguchi PS, Goldstein SR, Dambrosia JM, Hallett M. Sensory training for patients with focal hand dystonia. Ann Neurol. 2002;51(5):593–8. [DOI] [PubMed] [Google Scholar]
- 6.Zeuner KE, Shill HA, Sohn YH, Molloy FM, Thornton BC, Dambrosia JM, et al. Motor training as treatment in focal hand dystonia. Mov Disord. 2005;20(3):335–41. [DOI] [PubMed] [Google Scholar]
- 7.Zeuner KE, Peller M, Knutzen A, Hallett M, Deuschl G, Siebner HR. Motor re-training does not need to be task specific to improve writer’s cramp. Mov Disord. 2008;23(16):2319–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baur B, Furholzer W, Jasper I, Marquardt C, Hermsdorfer J. Effects of modified pen grip and handwriting training on writer’s cramp. Arch Phys Med Rehabil. 2009;90(5):867–75. [DOI] [PubMed] [Google Scholar]
- 9.Berger HJ, van der Werf SP, Horstink CA, Cools AR, Oyen WJ, Horstink MW. Writer’s cramp: restoration of striatal D2-binding after successful biofeedback-based sensorimotor training. Parkinsonism Relat Disord. 2007;13(3):170–3. [DOI] [PubMed] [Google Scholar]
- 10.Classen J, Liepert J, Wise SP, Hallett M, Cohen LG. Rapid plasticity of human cortical movement representation induced by practice. J Neurophysiol. 1998;79(2):1117–23. [DOI] [PubMed] [Google Scholar]
- 11.Zeuner KE, Peller M, Knutzen A, Holler I, Munchau A, Hallett M, et al. How to assess motor impairment in writer’s cramp. Mov Disord. 2007;22(8):1102–9. [DOI] [PubMed] [Google Scholar]
- 12.Schneider AS, Furholzer W, Marquardt C, Hermsdorfer J. Task specific grip force control in writer’s cramp. Clin Neurophysiol. 2014;125(4):786–97. [DOI] [PubMed] [Google Scholar]
- 13.Das CP, Dressler D, Hallett M. Botulinum toxin therapy of writer’s cramp. Eur J Neurol. 2006;13 Suppl 1:55–9. [DOI] [PubMed] [Google Scholar]
- 14.Comella CL. Dystonia: Then and now. Parkinsonism Relat Disord. 2018;46 Suppl 1:S66–S9. [DOI] [PubMed] [Google Scholar]
- 15.Lungu C, Karp BI, Alter K, Zolbrod R, Hallett M. Long-term follow-up of botulinum toxin therapy for focal hand dystonia: outcome at 10 years or more. Mov Disord. 2011;26(4):750–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Horisawa S, Taira T, Goto S, Ochiai T, Nakajima T. Long-term improvement of musician’s dystonia after stereotactic ventro-oral thalamotomy. Ann Neurol. 2013;74(5):648–54. [DOI] [PubMed] [Google Scholar]
- 17.Hedera P, Phibbs FT, Dolhun R, Charles PD, Konrad PE, Neimat JS, et al. Surgical targets for dystonic tremor: considerations between the globus pallidus and ventral intermediate thalamic nucleus. Parkinsonism Relat Disord. 2013;19(7):684–6. [DOI] [PubMed] [Google Scholar]
- 18.Wissel J, et al. (1996). Botulinum toxin in writer’s cramp: objective response evaluation in 31 patients. J Neurol Neurosurg Psychiatry 61(2): 172–175. [DOI] [PMC free article] [PubMed] [Google Scholar]