Abstract
Purpose
The objective of the study was to explore breast cancer patients’ illness perception, its relationship to perceived sense of well-being, and the role of perceived social support.
Methods
Women with diagnosed breast cancer were recruited from the two university hospitals in South Korea between January and April 2018. The questionnaires included the Illness Perception Questionnaire-Revised (IPQ-R) and the Functional Assessment of Cancer Therapy for Breast cancer (FACT-B). A total of 321 participants’ data was analyzed using descriptive analyses, multiple regression, and structural equation modeling.
Results
Negative illness perception was greater in participants currently receiving chemotherapy (p=0.044) or had received chemotherapy in the past (p=0.006). Positive illness perception was lower in older participants (p=0.001) or those who had received chemotherapy (p=0.018). Negative illness perception had a direct effect on a low sense of well-being (p<0.001). Perceived social support had a significant mediation effect on the relationship between negative/positive illness perception and sense of well-being (p<0.001).
Conclusion
Significant relationships between illness perception and sense of well-being were observed in breast cancer patients. Strengthening patients’ perceived social support would be helpful in improving their sense of well-being.
Keywords: breast cancer, illness behavior, perception, social support, well-being
Introduction
Breast cancer is one of the most common cancers in women, as well as, the main cause of disability and deaths due to potential complications and late effects following the treatment.1 Improved screening rates and early detection have led to a broader selection of treatments, which has gradually decreased the overall morbidity and mortality rates of breast cancer.2 Given the increasing number of women who are experiencing or have survived breast cancer, studies have primarily focused on breast cancer patients’ quality of life.2
Being diagnosed with cancer is a burden due to the presence of multitude of symptoms as a result of the disease or the treatment.3,4 Breast cancer patients often report physical symptoms such as hot flashes, discomfort in the arm, vaginal dryness, pain, nausea, and vomiting.4 In addition, psychological symptoms are very common in this group; these include impaired sexuality, depression, anxiety, fear of recurrence.1,3 These symptoms not only affect breast cancer patients’ sense of well-being but also their perception of the illness.5
Studies have demonstrated how illness perception largely determines the sense of well-being in cancer patients, and breast cancer patients are no exception to this.1,6,7 The concept of illness perception has its foundation rooted in the self-regulation model by Leventhal and colleagues.8,9 According to this model, patients react to a disease based on a conceptualized idea, which is developed both cognitively and emotionally through a collection of personal experiences.10,11 Moreover, this model emphasized that the coping mechanisms depend on patients’ illness perception, which has a critical impact on their adherence to treatment and sense of well-being, both positive and negative.11,12 Previous studies have reported that breast cancer patients’ poor interpretation of their diagnosis, prognosis, and fear of progression is associated with poor physical (e.g., fatigue, pain) and poor mental health (e.g., helplessness, anxiety, depression),1,6 low medical compliance,12 and future sense of well-being prediction.7 Besides, illness perception in breast cancer patients has been a significant variable in determining the causes of psychological distress, coping strategies, and treatment outcomes.6,13 The perceived social support, locus of control, and self-efficacy have been frequently cited as correlated factors to illness perception.14,15 Especially, perceived social support has been described as a mediator in the relationship between illness perception and sense of well-being based on previous studies, which support its mediation role in the relationship between illness severity and depression15 and between stress and psychological morbidity and the quality of life.16
Despite the extended reports suggesting the influence of illness perceptions on the sense of well-being of cancer patients, to what extent and how these relationships are established, while considering other associated factors (e.g., demographic and breast cancer-related factors) have yet to be determined. Moreover, many studies on this topic have focused on White women.7,11,13 Therefore, it is critical to study the relationship between illness perception and the overall well-being of breast cancer patients across different cultural backgrounds, as the determinants of illness perception considerably differ between cultures.17 This study aimed to a) identify the demographic and disease factors influencing breast cancer patients’ illness perception, b) determine to what extent illness perception and the sense of well-being are related, and c) explore the role of perceived social support in the relationship between illness perception and sense of well-being based on the theoretical framework of Leventhal’s “Self-regulation Model of Illness Behavior.”
Materials and methods
Sample and setting
This study employed a descriptive, correlational study design. With a two-tailed power of 0.80, an alpha-level of 0.05, and an effect size of 0.30, we estimated the required sample size to be 298 using G*Power 3.1.9.2 analysis software.18,19 However, based on a study, which reported a dropout rate of 8% among cancer patients in the initial questionnaire after receiving informed consent,20 we recruited 330 participants (over sampled to 10%).
The study participants were recruited from Y University Hospital in Seoul and S University Hospital in Gyeong-gi province, Korea. A convenience sampling method was used to recruit participants who met the following criteria: a) female patients diagnosed with breast cancer; b) could read, speak, and understand the Korean language; and c) voluntarily agreed to participate in the study and provided informed consent. Breast cancer patients with brain metastasis or those diagnosed with a mental illness or cognitive impairments were excluded. We included all breast cancer stages and all types of cancer treatments to examine the differences.
Data collection
Data were collected between January and April 2018. Two research assistants with bachelor’s degrees in nursing assisted with the data collection process. The project investigator educated the two research assistants on the study design and special needs of breast cancer patients with various symptoms while they completed the questionnaires. Two collaborating surgeons from the two hospitals provided an orientation on the study sites and rooms that would be used to obtain the participants’ informed consents and completing the questionnaires. During the breast cancer patients’ office visits, their study participation eligibility was assessed twice, by both the surgeons and the project investigator. The study was explained to the eligible participants who were interested in the study. After signing their informed consent forms, the participants were asked to complete the 10 mins questionnaires and received a hand moisturizer worth US$ 1-2.
Study variables and instruments
Participants’ illness perception was assessed using the Illness Perception Questionnaire-Revised (IPQ-R),21 which examines nine dimensions of illness perception: identity, timeline (acute/chronic), consequences, personal control, treatment control, illness coherence, timeline cyclical, emotional representation, and causes. The first dimension “identity” examines how an individual attributes 14 commonly experienced symptoms to the illness using yes/no responses. The second through eighth dimensions are examined using 38 items rated on a 5-point Likert scale. The last dimension “causes” is examined using 18 items indicating possible causes of one’s illness, which are rated on a 5-point Likert scale. Based on the scoring guidelines of the IPQ-R,1,22 “identity,” “timeline,” “consequences,” “time cyclical,” and “emotional representations” are grouped together, and higher scores on these dimensions indicate attributing more symptoms to the illness and perceiving chronicity and negative consequences of the illness. In this study, we labeled these dimensions as “negative illness perceptions.” On the other hand, “personal control,” “treatment control,” and “illness coherence” are grouped, and higher scores on these dimensions indicate positive beliefs and perceived controllability of the illness. In this study, we labeled these dimensions as “positive illness perceptions.” As the total achievable scores for “negative illness perceptions” and “positive illness perceptions” are different, it is not meaningful to compare the mean scores or the sum of scores on the two labels. The IPQ-R has been translated and used in over 17 different languages and among patients with various illness, including asthma, hemophilia, hypertension, and sexually transmitted diseases.22 The IPQ-R has been used among cancer patients, and it has demonstrated acceptable psychometric properties.23,24 For this study, the research team translated and back-translated the IPQ-R, and performed an expert review of the contents.25 The content validity indexing technique was used in the evaluation.25 The experts rated each questionnaire item on a 4-point Likert scale (1=inappropriate, 2=somewhat appropriate, 3=appropriate, and 4=very appropriate).25,26 Items that scored less than “2” by two experts were revised for clarity.26 The Cronbach’s alpha of the translated Korean version of the IPQ-R demonstrated was 0.87.
The participants’ perceived social support was assessed using the 12-item Multidimensional Scale of Perceived Social Support (MSPSS), which examines social support from three sources: family, friends, and important others. The items are rated on a 7-point Likert system. The reliability of the translated Korean version of MSPSS was tested in a previous study of Korean female college students and had a Cronbach’s alpha of 0.81.27 In this study, the Cronbach’s alpha was 0.95.
The Functional Assessment of Cancer Therapy for Breast Cancer (FACT-B) was used to assess participants’ sense of well-being on five domains: physical well-being, social/family well-being, emotional well-being, functional well-being, and breast-cancer-specific well-being.28,29 It is a 36-item questionnaire rated on a 5-point Likert scale. The Korean-translated version of the FACT-B was retrieved from the official website.30 The Korean version of the FACT-B has demonstrated acceptable reliability and validity in previous studies.31 In this study, the Cronbach’s alpha of the Korean-translated version of the FACT-B was 0.73.
Data analysis
Questionnaires with more than 10% missing data were excluded from the study to ensure the validity of the study.32 SPSS 25.0 was used to analyze the data. Descriptive analyses (frequencies, percentage, mean, and standard deviation) were used to characterize participants’ baseline information. Multiple regressions were performed on the entire sample to determine the demographic and disease factors influencing participants’ illness perception. Based on the findings of the study, additional analysis was conducted using Pearson’s correlation coefficient to further examine the relationships between age and other study variables. To examine the extent to which the illness perception and sense of well-being are related and to explore the role of perceived social support in the relationship, structural equation modeling (SEM) was performed using Mplus 7.4. The SEM was performed in two models: model 1 using the sum scores of the total IPQ-R and model 2 using the sum scores on the IPQ-R subscales: “negative illness perception” and “positive illness perception.” The criteria applied to evaluate the adequate model fit of this study were comparative fit index (CFI)>0.95, root mean square error of approximation (RMSEA)<0.60, and standardized root mean square residual (SRMR)<0.80.27,33 The study used sum scores of MSPSS and FACT-B because the model fit was inadequate when using the subscales of these instruments (X2=949.942, df=3, p<0.001, RMSEA=0.00, CFI=1.00, SRMR=0.00).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee (Catholic Medical Center of Korea; XC17QEDI0080) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The participants were informed that they are free to withdraw participation at any time or refuse to answer certain questions. To ensure participants’ rights are acknowledged, consent was obtained in a separate room without the presence of the participant’s surgeon.
Results
Characteristics of the study participants
A total of 330 breast cancer patients were assessed to be eligible for the study and agreed to participate. Only 321 of the participants’ responses were included in the data analysis, as nine participants did not complete over 10% of the survey questions. As shown in Table 1, most of the study participants were from Seoul and Gyeong-gi areas, and their mean age was 55.6±10.2 years. The mean age at breast cancer diagnosis was 52.1±10.0 years. About 50.2% of the study participants answered that they were diagnosed of breast cancer less than 3 years ago, 27.4% of the participants were diagnosed 3–5 years ago, 13.7% were diagnosed 6–10 years ago, and 8.7% diagnosed over 10 years ago. Regarding the cancer stage, 37.5% of the study participants were at stage 1 of breast cancer and 37.5% were at stage 2. While the majority of the patients answered that they do not know the specific type of their cancer, 26.4% answered that they have hormone-receptor-positive cancer and 12.1% answered that they have human epidermal growth factor receptor 2 (HER2) positive cancer. Most of the patients (55%) were currently on single breast cancer treatment, while 3.4% were on three different kinds of breast cancer treatments. The treatment types that patients were receiving were hormonal therapy (42.7%), chemotherapy (24.9%), and radiation therapy (11.8%). Regarding surgeries, 43.4% reported receiving partial-mastectomy, and 14.9% received mastectomy. Regarding other previous treatments for breast cancer, 21.5% of the participants answered receiving hormonal therapy, 40.2% answered receiving chemotherapy, and 44.5% answered receiving radiation therapy.
Table 1.
Sociodemographic and baseline information of participants (N=321)
| Characteristics | Mean ± SD or N (%) | ||
|---|---|---|---|
| Region | Seoul | 112 (34.9) | |
| Gyeong-gi | 173 (53.9) | ||
| Others | 36 (11.2) | ||
| Age (years) | 55.6±10.2 | ||
| Age at diagnosis | 52.1±10.0 | ||
| Years since diagnosis | Less than 3 years | 161 (50.2) | |
| 3–5 years | 88 (27.4) | ||
| 6–10 years | 44 (13.7) | ||
| More than 10 years | 28 (8.7) | ||
| Breast cancer | Stage | 0 (DCIS) | 7 (2.4) |
| 1 | 127 (43.6) | ||
| 2 | 109 (37.5) | ||
| 3 | 40 (13.7) | ||
| 4 | 8 (2.7) | ||
| Type | HR (positive) | 75 (26.3) | |
| HER2 (positive) | 33 (12.1) | ||
| Current treatment | Numbers | Single | 178 (55.5) |
| Double | 23 (7.2) | ||
| Triple | 11 (3.4) | ||
| Type | Hormonal therapy | 137 (42.7) | |
| Chemotherapy | 80 (24.9) | ||
| Radiation therapy | 38 (11.8) | ||
| Past treatment | Surgery | Partial-mastectomy | 137 (43.4) |
| Mastectomy | 47 (14.9) | ||
| Hormonal therapy | 69 (21.5) | ||
| Chemotherapy | 129 (40.2) | ||
| Radiation therapy | 143 (44.5) | ||
| Illness perception | Negative | 68.94±15.11 | |
| Positive | 57.66±7.77 | ||
| Sense of well-being | Physical | 20.33±6.47 | |
| Social | 17.41±6.92 | ||
| Emotional | 15.59±5.31 | ||
| Functional | 16.41±6.23 | ||
| Breast cancer specific | 22.53±6.29 | ||
| Total | 92.28±21.61 | ||
| Perceived social support | Family | 20.63±4.80 | |
| Friends | 19.92±5.19 | ||
| Important Others | 20.86±4.61 | ||
| Total | 61.42±13.95 | ||
Abbreviations: DCIS, ductal carcinoma in situ; HR, hormone receptor; HER2, human epidermal growth factor receptor 2; SD, standard deviation.
The mean score of the negative illness perception was 68.94±15.11 and that of positive illness perception was 57.66±7.77. Participants scored the highest on breast-cancer-specific sense of well-being (22.53±6.29) and the lowest on emotional sense of well-being (15.59±5.31). Participants reported slightly higher perceived social support from family (20.63±4.80) and important others (20.86±4.61) than from friends (19.92±5.19).
Factors influencing illness perception
The sociodemographic and disease-related factors influencing illness perception were examined in the three models (Table 2). The descriptive power of the first model which examined the factors influencing negative illness perception was 10% (F=2.56, p=0.003). Participants who were currently receiving chemotherapy (β=0.14, p=0.044) and those who had received chemotherapy in the past (β=0.22, p=0.006) had more negative illness perception. The descriptive power of the second model which examined the factors influencing positive illness perception was 8% (F=2.10, p=0.017). Participants who were older (β=−0.21, p=0.001) and had received chemotherapy in the past (β=−0.19, p=0.018) reported low positive illness perception. The descriptive power of the third model which examined the factors influencing total illness perception was 9% (F=2.33, p=0.007). Participants who were older (β=−0.23, p<0.001) reported low total illness perception.
Table 2.
Demographics and disease factors influencing illness perceptions (N=321)
| Variables | Negative illness perception | Positive illness perception | Illness perception total | ||||
|---|---|---|---|---|---|---|---|
| β | t | β | t | β | t | ||
| Hospital | 0.08 | 1.16 | −0.14 | −1.87 | 0.01 | 0.18 | |
| Region | −0.10 | −1.49 | 0.06 | 0.87 | −0.07 | −1.03 | |
| Age | −0.12 | −1.86 | −0.21** | −3.34 | −0.23*** | −3.64 | |
| Years since diagnosis | 0.07 | 0.97 | 0.01 | 0.17 | 0.07 | 1.07 | |
| Breast cancer stage | 0.09 | 1.48 | 0 | −0.04 | 0.09 | 1.46 | |
| Current treatment | Hormonal therapy | −0.03 | −0.47 | 0.11 | 1.63 | 0.03 | 0.39 |
| Chemotherapy | 0.14* | 2.02 | −0.03 | −0.41 | 0.13 | 1.81 | |
| Radiation therapy | −0.06 | −0.96 | −0.03 | −0.56 | −0.08 | −1.26 | |
| Past treatment | Surgery | 0.12 | 1.43 | −0.02 | −0.25 | 0.11 | 1.30 |
| Hormonal therapy | −0.08 | −1.21 | 0.05 | 0.65 | −0.06 | −0.87 | |
| Chemotherapy | 0.22** | 2.75 | −0.19* | −2.37 | 0.12 | 1.51 | |
| Radiation therapy | 0.04 | 0.48 | 0.08 | 0.86 | 0.09 | 0.94 | |
| F (p) | 2.56 (0.003) | 2.10 (0.017) | 2.33 (0.007) | ||||
| R2 | 0.10 | 0.08 | 0.09 | ||||
Notes: ***p< 0.001, **p< 0.01, *p< 0.05.
To further examine the correlations between the abovementioned factors (age, past and current history of receiving chemotherapy) and other study variables, a Pearson’s correlation coefficient was performed (Table 3). The participants’ age was positively correlated to age at diagnosis (r=0.940, p<0.001) and year since diagnosis (r=0.221, p<0.001). The negative correlations were observed with negative illness perception (r=−0.111, p=0.047), positive illness perception (r=−0.189, p=0.001), and perceived social support (r=−0.120, p=0.032). Participants’ past history of receiving chemotherapy was positively correlated to years since diagnosis (r=0.344, p<0.001) and negative illness perception (r=0.155, p=0.006), and negatively correlated to age at diagnosis (r=−0.123, p=0.028) and current history of receiving chemotherapy (r=−0.139, p=0.013). The participants’ current history of receiving chemotherapy was positively correlated to negative illness perception (r=0.127, p=0.023) and negatively correlated to years since diagnosis (r=−0.248, p<0.001), past history of receiving chemotherapy (r=−0.139, p=0.013), and sense of well-being (r=−0.162, p=0.004).
Table 3.
Correlations between study variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Pearson’s correlation coefficient (p-value) | ||||||||||
| 1.Age | – | |||||||||
| 2.Age at diagnosis | 0.940 (<0.001)*** | – | ||||||||
| 3.Year since diagnosis | 0.221 (<0.001)*** | −0.125 (0.025)* | – | |||||||
| 4.Advanced breast cancer (Stage 3 & 4) | −0.060 (0.306) | −0.055 (0.353) | −0.019 (0.741) | – | ||||||
| 5.Current treatment (chemotherapy) | −0.083 (0.137) | 0.002 (0.967) | −0.248 (<0.001)*** | 0.013 (0.832) | – | |||||
| 6.Past treatment (chemotherapy) | −0.002 (0.976) | −0.123 (0.028)* | 0.344 (<0.001)*** | −0.041 (0.492) | −0.139 (0.013)* | – | ||||
| 7.Negative illness perception | −0.111 (0.047)* | −0.119 (0.034)* | 0.017 (0.765) | 0.035 (0.554) | 0.127 (0.023)* | 0.155 (0.006)** | – | |||
| 8.Positive illness perception | −0.189 (0.001)** | −0.176 (0.002)** | −0.046 (0.412) | 0.046 (0.431) | −0.072 (0.195) | −0.089 (0.117) | −0.286 (<0.001)*** | – | ||
| 9.Sense of well-being | −0.080 (0.151) | −0.103 (0.066) | 0.060 (0.283) | 0.065 (0.271) | −0.162 (0.004)** | −0.074 (0.189) | −0.547 (<0.001)*** | 0.459 (<0.001)*** | – | |
| 10.Perceived social support | −0.120 (0.032)* | −0.107 (0.055) | −0.041 (0.460) | 0.009 (0.877) | −0.040 (0.475) | −0.043 (0.448) | −0.254 (<0.001)*** | 0.390 (<0.001)*** | 0.581 (<0.001)*** | – |
Notes: ***p< 0.001, **p< 0.01, *p< 0.05.
Relationships between illness perception and the sense of well-being
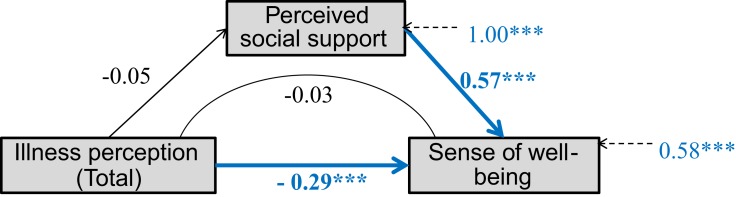
The relationships between illness perception and the sense of well-being were examined in two models. Total illness perception was considered to be an independent variable related to breast cancer patients’ sense of well-being in the first model (Figure 1). The overall model fit was acceptable (X2=174.91, df=3, p<0.001, RMSEA=0.00, CFI=1.00, SRMR=0.00). Total illness perception had a significant direct effect on the sense of well-being (β=−0.29, p<0.001); however, its effect on perceived social support was not significant (β=−0.05, p=0.336). Perceived social support did not have a mediation effect in the relationship between total illness perception and sense of well-being.
Figure 1.
Mediation modeling between total illness perception and sense of well-being. The bolded arrows and values indicate a statistically significant effect (***p<0.001).
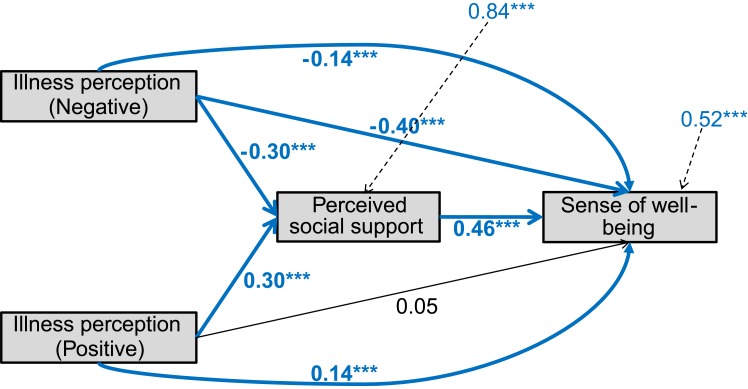
In the second model, negative and positive illness perceptions were considered to be independent variables (Figure 2). The overall fit of the data was acceptable (X2=265.61, df=5, p<0.001, RMSEA=0.00, CFI=1.00, SRMR=0.00). Negative illness perception had a significant direct effect on perceived social support (β=−0.30, p<0.001) and sense of well-being (β=−0.40, p<0.001). Positive illness perception had a significant direct effect on perceived social support (β=0.30, p<0.001); however, its effect on sense of well-being was not significant (β=0.05, p=0.211). Perceived social support had a partial mediation effect in the relationship between negative illness perception and sense of well-being (β=−0.14, p<0.001) and a full mediation effect in the relationship between positive illness perception and sense of well-being (β=0.14, p<0.001).
Figure 2.
Mediation modeling between negative/positive illness perception and sense of well-being. The bolded arrows and values indicate a statistically significant effect (***p<0.001).
Discussion
This study examined breast cancer patients’ illness perception, sense of well-being, and their related factors. The patients who were currently receiving chemotherapy and those with a history of having received chemotherapy both had more negative illness perception. In addition, patients who were currently receiving chemotherapy had less positive illness perception. Previous studies have reported that how a patient perceives the treatment side effects and their disease experience contribute to a sense of well-being.34 Chemotherapy for breast cancer patients often accompanies multiple unfavorable side-effects, which are often described as cancer-related stressors.35 Along with having a more invasive type of cancer, having more cancer-related stressors are shown to contribute to negative illness perception.35 Moreover, past experience of severe stress contributes to one’s susceptibility to psychological problems, impairs one’s ability to cope, and contributes to the negative illness perception.36 On the other hand, some studies have reported that perceived successful chemotherapy predicts a positive illness perception.35 Some cancer patients tend to adjust to the emotional upset related to the cancer diagnosis after chemotherapy.37
In this study, participants’ older age was related to both positive and total illness perception. Older patients tend to perceive less negative changes as a result of the cancer experience.35 Moreover, they report more sense of control of cancer treatment.38 However, other study has reported that younger cancer patients perform better on role functioning, and thus have less negative illness perception.39 Older cancer patients were reported to feel more hopeless and psychologically distressed compared to their younger counterparts.40 The additional analysis showed negative correlations between age and perceived social support. Perceived social support was positively correlated to negative illness perception and negatively correlated to positive illness perception. It is possible that older participants’ perception of having less social support contributed to their negative illness perception.
The participants who reported more negative illness perception had a lower sense of well-being, in this study. When negative and positive illness perceptions were examined separately, only negative illness perception was significantly related to the women’s sense of well-being. In this study, participants with more negative illness perception reported a lower sense of well-being. Previous studies also support this relationship. Negative illness perceptions, including expectance of negative consequences of the disease and fear of recurrence were associated with a low sense of well-being.34,41
Perceived social support was a significant mediator in the relationship between negative illness perception and sense of well-being, as well as between positive illness perception and sense of well-being. The importance of perceived social support has been indicated in previous studies. While the stage of breast cancer did not have any relation to illness perception, functional social support was a significant factor of illness perception, which is consistent with the findings of a previous study.1 Similarly, patients with greater perceived social support and sense of coherence with caregiver showed better illness acceptance.42 With enough social support, the patients showed better treatment adherence and quality of life.43,44
Limitations
This study has some limitations. First, we could not include all the variables related to illness perception mentioned in previous studies. Considering that the study participants were cancer patients, we sought to minimize the fatigue from completing the questionnaires.6 Some other variables which could be included in future studies of illness perception are previous illness history, experience of breast cancer in the past (including serving as a caregiver for a family member or an important other with breast cancer), cultural aspects,36 disease knowledge,38 social socioeconomic status,35 and general life stress.34 Additionally, to explore the differences of disease experience by age, examining women’s sense of control or role functioning would be helpful. Second, the descriptive power of the models, which examined the factors influencing negative, positive, and total illness perception, was small. This can be improved by adding the aforementioned variables in the model. Third, the cross-sectional study design of this study precludes a causal inference. Although the path coefficients were significant in the hypothesized relationships, a longitudinal study would better describe their causal relationships. Fourth, the generalizability of the study is limited as the study only included Korean breast cancer patients from two university hospitals. Careful interpretation is necessary when applying the findings of the study to patients from other cultural backgrounds.
Conclusion
Several conclusions can be drawn from this study. First, breast cancer patients who are receiving or have received chemotherapy in the past should be particularly given attention, as they are reported to have more negative illness perception. Treatment satisfaction is associated with illness perception and quality of life in the previous study.10 Therefore, enhancing patients’ treatment experience and satisfaction will contribute to a better illness perception, adherence to the treatment, and disease outcomes.10
Second, when examining illness perception, the patients’ age should be considered. Older breast cancer patients reported less positive illness perception and total illness perception. Efforts to improve illness perception are especially needed for this population. Older age is related to a higher level of psychological distress, limited physical functioning, and multiple chronic illnesses other than cancer.45 The additional discomfort as a result of aging should not be neglected while managing breast cancer.
Third, more studies are needed to examine ways to improve negative illness perception in breast cancer patients. In previous studies, interventions aimed at clarifying distorted illness perception were shown to enhance patients’ illness perception.34 In addition, interventions to alleviate symptoms,46 enhance coping strategies, and those involving psychoeducation47 have been shown to be effective. As studies have suggested that caregivers’ illness perceptions could affect cancer patients’ illness perception, future studies may consider including caregivers in the intervention programs to improve the negative illness perception in breast cancer patients.48,49
Lastly, patients’ perceived social support needs to be considered in their breast cancer management. Perceived social support was a significant mediator in the relationship between both negative/positive illness perception and sense of well-being. Previous studies of cancer patients have extensively explored the roles of perceived social support, which include helping the patient adjust to a cancer diagnosis,50 and adherence to treatment,43 helping the patient overcome negative emotions, reducing psychological distress in the patient, and improving the patient’s quality of life.51 Health care providers should consider patients’ perceived social support in their care plans and provide more support.
Breast cancer patients are reported to have more negative illness perceptions than do patients with other chronic illnesses.11 We believe that this study provides a better understanding of breast cancer patients’ illness perception, sense of well-being, and related factors. Especially, the study has its significance in exploring these topics among non-White breast cancer patients who have been relatively less studied.
Acknowledgments
The authors would like to thank the nurses of the breast cancer outpatient units of the two university hospitals for their assistance in data collection. This research was funded by Chung-Ang University Research Grants in 2018. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
- 1.Kus T, Aktas G, Ekici H, Elboga G, Djamgoz S. Illness perception is a strong parameter on anxiety and depression scores in early-stage breast cancer survivors: a single-center cross-sectional study of Turkish patients. Support Care Cancer. 2017;25(11):3347–3355. doi: 10.1007/s00520-017-3753-1 [DOI] [PubMed] [Google Scholar]
- 2.Houssami N, Ciatto S, Martinelli F, Bonardi R, Duffy SW. Early detection of second breast cancers improves prognosis in breast cancer survivors. Ann Oncol. 2009;20(9):1505–1510. doi: 10.1093/annonc/mdp037 [DOI] [PubMed] [Google Scholar]
- 3.Fanakidou I, Zyga S, Alikari V, Tsironi M, Stathoulis J, Theofilou P. Mental health, loneliness, and illness perception outcomes in quality of life among young breast cancer patients after mastectomy: the role of breast reconstruction. Qual Life Res. 2018;27(2):539–543. doi: 10.1007/s11136-017-1735-x [DOI] [PubMed] [Google Scholar]
- 4.Yoon J, Malin JL, Tao ML, et al. Symptoms after breast cancer treatment: are they influenced by patient characteristics? Breast Cancer Res Treat. 2008;108(2):153–165. doi: 10.1007/s10549-007-9599-3 [DOI] [PubMed] [Google Scholar]
- 5.Leonhart R, Tang L, Pang Y, et al. Physical and psychological correlates of high somatic symptom severity in Chinese breast cancer patients. Psycho-Oncology. 2017;26(5):656–663. doi: 10.1002/pon.4203 [DOI] [PubMed] [Google Scholar]
- 6.Ma C, Yan J, Wu Y, Huang W. Illness perceptions of Chinese women with breast cancer and relationships with socio-demographic and clinical characteristics. Int J Nurs Pract. 2018. doi: 10.1111/ijn.12677 [DOI] [PubMed] [Google Scholar]
- 7.Ashley L, Marti J, Jones H, Velikova G, Wright P. Illness perceptions within 6 months of cancer diagnosis are an independent prospective predictor of health-related quality of life 15 months post-diagnosis. Psycho-Oncology. 2015;24(11):1463–1470. doi: 10.1002/pon.3812 [DOI] [PubMed] [Google Scholar]
- 8.Leventhal H, Nerenz DR, Steele DS. Illness Representations and Coping with Health Threats. Vol. IV Hillsdale, NJ: Erlbaum; 1984. [Google Scholar]
- 9.Leventhal H, Benyamini Y, Brownlee S, et al. Illness Representations: Theoretical Foundations. Amsterdam: Harwood Academic Publishers; 1997. [Google Scholar]
- 10.Iskandarsyah A, De Klerk C, Suardi DR, Soemitro MP, Sadarjoen SS, Passchier J. Satisfaction with information and its association with illness perception and quality of life in Indonesian breast cancer patients. Support Care Cancer. 2013;21(11):2999–3007. doi: 10.1007/s00520-013-1877-5 [DOI] [PubMed] [Google Scholar]
- 11.Kaptein AA, Yamaoka K, Snoei L, et al. Illness perceptions and quality of life in Japanese and Dutch women with breast cancer. J Psychosoc Oncol. 2013;31(1):83–102. doi: 10.1080/07347332.2012.741092 [DOI] [PubMed] [Google Scholar]
- 12.Ross S, Walker A, MacLeod MJ. Patient compliance in hypertension: role of illness perceptions and treatment beliefs. J Hum Hypertens. 2004;18(9):607–613. doi: 10.1038/sj.jhh.1001721 [DOI] [PubMed] [Google Scholar]
- 13.McCorry NK, Dempster M, Quinn J, et al. Illness perception clusters at diagnosis predict psychological distress among women with breast cancer at 6 months post diagnosis. Psycho-Oncology. 2013;22(3):692–698. doi: 10.1002/pon.3054 [DOI] [PubMed] [Google Scholar]
- 14.Shiri M, Bagherian R, Maracy M, Saenei HM. The relationship of perceived social support and locus of control subscales with illness perception in myocardial infarction patients, using structural equation modeling. Arch Psychiatry Psychotherapy. 2019;21(12):36–44. doi: 10.12740/APP/99945 [DOI] [Google Scholar]
- 15.Greco A, Steca P, Pozzi R, et al. Predicting depression from illness severity in cardiovascular disease patients: self-efficacy beliefs, illness perception, and perceived social support as mediators. Int J Behav Med. 2014;21(2):221–229. doi: 10.1007/s12529-013-9290-5 [DOI] [PubMed] [Google Scholar]
- 16.Pereira MG, Ponte M, Ferreira G, Machado JC. Quality of life in patients with skin tumors: the mediator role of body image and social support. Psycho-Oncology. 2017;26(6):815–821. doi: 10.1002/pon.4236 [DOI] [PubMed] [Google Scholar]
- 17.Van Der Kloot WA, Uchida Y, Inoue K, et al. The effects of illness beliefs and chemotherapy impact on quality of life in Japanese and Dutch patients with breast or lung cancer. Chin Clin Oncol. 2016;5(1):1-12. [DOI] [PubMed] [Google Scholar]
- 18.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ.: Lawrence Erlbaum; 1988. [Google Scholar]
- 19.Cohen J. A power primer. Psychol Bull. 1992;112(1):155–159. [DOI] [PubMed] [Google Scholar]
- 20.Mathibe LJ. Drop-out rates of cancer patients participating in longitudinal RCTs. Contemp Clin Trials. 2007;28(4):340–342. doi: 10.1016/j.cct.2007.03.006 [DOI] [PubMed] [Google Scholar]
- 21.Moss-Morris R, Weinman J, Petrie K, Horne R, Cameron L, Buick D. The revised Illness Perception Questionnaire (IPQ-R). Psychol Health. 2002;17(1):1–16. doi: 10.1080/08870440290001494 [DOI] [Google Scholar]
- 22.Moss-Morris R, Weinman J, Petrie KJ, Horne R, Cameron LD, Buick D Using and Scoring the IPQ-R; n.d.; Available from: https://www.uib.no/ipq/. Accessed February9, 2019.
- 23.Dempster M, McCorry NK. The factor structure of the revised illness perception questionnaire in a population of oesophageal cancer survivors. Psycho-Oncology. 2012;21(5):524–530. doi: 10.1002/pon.1927 [DOI] [PubMed] [Google Scholar]
- 24.Zhang N, Fielding R, Soong I, et al. Psychometric assessment of the Chinese version of the brief illness perception questionnaire in breast cancer survivors. PLoS One. 2017;12(3):e0174093. doi: 10.1371/journal.pone.0174093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Squires A, Aiken LH, van den Heede K, et al. A systematic survey instrument translation process for multi-country, comparative health workforce studies. Int J Nurs Stud. 2013;50(2):264–273. doi: 10.1016/j.ijnurstu.2012.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu DSF. Insomnia severity index: psychometric properties with Chinese community-dwelling older people. J Adv Nurs. 2010;66(10):2350–2359. doi: 10.1111/j.1365-2648.2010.05394.x [DOI] [PubMed] [Google Scholar]
- 27.Lee Y, Im EO. A path analysis of stress and premenstrual symptoms in Korean international and Korean domestic students. J Adv Nurs. 2016;72(12):3045–3059. doi: 10.1111/jan.13061 [DOI] [PubMed] [Google Scholar]
- 28.Cella DF, Tulsky DS, Gray G, et al. The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11(3):570–579. doi: 10.1200/JCO.1993.11.3.570 [DOI] [PubMed] [Google Scholar]
- 29.Brady MJ, Cella DF, Mo F, et al. Reliability and validity of the functional assessment of cancer therapy-breast quality-of-life instrument. J Clin Oncol. 1997;15(3):974–986. doi: 10.1200/JCO.1997.15.3.974 [DOI] [PubMed] [Google Scholar]
- 30.FACIT. FACT-B: for patients with breast cancer; 2013. Available from: http://www.facit.org/FACITOrg/Questionnaires. Accessed February9, 2019.
- 31.Park H, Yoon HG. Menopausal symptoms, sexual function, depression, and quality of life in Korean patients with breast cancer receiving chemotherapy. Support Care Cancer. 2013;21(9):2499–2507. doi: 10.1007/s00520-013-1815-6 [DOI] [PubMed] [Google Scholar]
- 32.Dong Y, Peng CYJ. Principled missing data methods for researchers. SpringerPlus. 2013;2(1):1–17. doi: 10.1186/2193-1801-2-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Elavsky S, Gold CH. Depressed mood but not fatigue mediate the relationship between physical activity and perceived stress in middle-aged women. Maturitas. 2009;64(4):235–240. doi: 10.1016/j.maturitas.2009.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Traeger L, Penedo FJ, Gonzalez JS, et al. Illness perceptions and emotional well-being in men treated for localized prostate cancer. J Psychosom Res. 2009;67(5):389–397. doi: 10.1016/j.jpsychores.2009.03.013 [DOI] [PubMed] [Google Scholar]
- 35.Pinquart M, Fröhlich C, Silbereisen RK. Cancer patients’ perceptions of positive and negative illness-related changes. J Health Psychol. 2007;12(6):907–921. doi: 10.1177/1359105307082454 [DOI] [PubMed] [Google Scholar]
- 36.Popov N, Heruti I, Levy S, Lulav-Grinwald D, Bar-Sela G. Illness perception differences between Russian- and Hebrew-speaking Israeli oncology patients. J Clin Psychol Med Settings. 2014;21(1):33–40. doi: 10.1007/s10880-013-9384-x [DOI] [PubMed] [Google Scholar]
- 37.Kaptein AA, Yamaoka K, Snoei L, et al. Illness perceptions and quality of life in Japanese and Dutch patients with non-small-cell lung cancer. Lung Cancer. 2011;72(3):384–390. doi: 10.1016/j.lungcan.2010.09.010 [DOI] [PubMed] [Google Scholar]
- 38.Husson O, Thong MSY, Mols F, Oerlemans S, Kaptein AA, Van De Poll-Franse LV. Illness perceptions in cancer survivors: what is the role of information provision? Psycho-Oncology. 2013;22(3):490–498. doi: 10.1002/pon.3042 [DOI] [PubMed] [Google Scholar]
- 39.Scharloo M, De Jong RJB, Langeveld TPM, Van Velzen-Verkaik E, Den Akker MMDO, Kaptein AA. Quality of life and illness perceptions in patients with recently diagnosed head and neck cancer. Head Neck. 2005;27(10):857–863. doi: 10.1002/hed.20251 [DOI] [PubMed] [Google Scholar]
- 40.Palgi Y, Ben-Ezra M, Hamama-Raz Y, Shacham Shmueli E, Shrira A. The effect of age on illness cognition, subjective well-being and psychological distress among gastric cancer patients. Stress Health. 2014;30(4):280–286. doi: 10.1002/smi.2521 [DOI] [PubMed] [Google Scholar]
- 41.Dempster M, McCorry NK, Brennan E, Donnelly M, Murray LJ, Johnston BT. Illness perceptions among carer-survivor dyads are related to psychological distress among oesophageal cancer survivors. J Psychosom Res. 2011;70(5):432–439. doi: 10.1016/j.jpsychores.2010.07.007 [DOI] [PubMed] [Google Scholar]
- 42.Pasek M, Dębska G, Wojtyna E. Perceived social support and the sense of coherence in patient–caregiver dyad versus acceptance of illness in cancer patients. J Clin Nurs. 2017;26(23–24):4985–4993. doi: 10.1111/jocn.13997 [DOI] [PubMed] [Google Scholar]
- 43.Saffari M, Lin CY, Chen H, Pakpour AH. The role of religious coping and social support on medication adherence and quality of life among the elderly with type 2 diabetes. Qual Life Res. 2019;28(8):2183–2193. doi: 10.1007/s11136-019-02183-z [DOI] [PubMed] [Google Scholar]
- 44.Varghese SA. Social support: an important factor for treatment adherence and health-related quality of life of patients with end-stage renal disease. J Soc Serv Res. 2018;44(1):1–18. doi: 10.1080/01488376.2017.1374315 [DOI] [Google Scholar]
- 45.Han J. Chronic illnesses and depressive symptoms among older people: functional limitations as a mediator and self-perceptions of aging as a moderator. J Aging Health. 2018;30(8):1188–1204. doi: 10.1177/0898264317711609 [DOI] [PubMed] [Google Scholar]
- 46.Fischer MJ, Krol-Warmerdam EMM, Ranke GMC, et al. Stick together: a Nordic walking group intervention for breast cancer survivors. J Psychosoc Oncol. 2015;33(3):278–296. doi: 10.1080/07347332.2015.1020465 [DOI] [PubMed] [Google Scholar]
- 47.Fischer MJ, Wiesenhaan ME, Heijer ADD, Kleijn WC, Nortier JWR, Kaptein AA. From despair to hope: a longitudinal study of illness perceptions and coping in a psycho-educational group intervention for women with breast cancer. Br J Health Psychol. 2013;18(3):526–545. doi: 10.1111/j.2044-8287.2012.02100.x [DOI] [PubMed] [Google Scholar]
- 48.Richardson AE, Morton R, Broadbent E. Caregivers’ illness perceptions contribute to quality of life in head and neck cancer patients at diagnosis. J Psychosoc Oncol. 2015;33(4):414–432. doi: 10.1080/07347332.2015.1046011 [DOI] [PubMed] [Google Scholar]
- 49.Bassi M, Falautano M, Cilia S, et al. Illness perception and well-being among persons with multiple sclerosis and their caregivers. J Clin Psychol Med Settings. 2016;23(1):33–52. doi: 10.1007/s10880-015-9425-8 [DOI] [PubMed] [Google Scholar]
- 50.Mishra VS, Saranath D. Association between demographic features and perceived social support in the mental adjustment to breast cancer. Psycho-Oncology. 2019;28(3):629–634. doi: 10.1002/pon.5001 [DOI] [PubMed] [Google Scholar]
- 51.Ng CG, Mohamed S, See MH, et al. Anxiety, depression, perceived social support and quality of life in Malaysian breast cancer patients: a 1-year prospective study. Health Qual Life Outcomes. 2015;13(1):205. doi: 10.1186/s12955-015-0401-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Moss-Morris R, Weinman J, Petrie KJ, Horne R, Cameron LD, Buick D Using and Scoring the IPQ-R; n.d.; Available from: https://www.uib.no/ipq/. Accessed February9, 2019.