Abstract
Knowledge of breast cancer genetics is critical for those at increased hereditary risk who must make decisions about breast cancer screening options. This descriptive study explored theory-based relationships among cognitive and emotional variables related to knowledge of breast cancer genetics in cancer families. Participants included first-degree relatives of women with breast cancer who had received genetic counseling and testing. Study participants themselves did not have breast cancer and had not received genetic counseling or testing. Data were collected by telephone interviews and surveys. Variables analyzed included numeracy, health literacy, cancer-related distress, age, education, and the reported amount of information shared by the participants’ family members about genetic counseling. The multiple regression model explained 13.9% of variance in knowledge of breast cancer genetics (p = 0.03). Best fit of the multiple regression model included all variables except education. Reported amount of information shared was the only independently significant factor associated with knowledge (β = 0.28, p = 0.01). Participants who reported higher levels of information shared by a family member about information learned during a genetic counseling session also demonstrated increased knowledge about breast cancer genetics.
Keywords: Knowledge, Breast cancer, Cancer genetics, Family communication, Genetic counseling, Precision medicine, Numeracy, Health literacy
Genetic conditions play a role in nine of the ten leading causes of death in the USA (National Human Genome Research Institute 2016) and affect an entire family, not just the individual presenting with disease. Thus, both patients and family members need information about genetics. Knowledge about a genetic condition and personal risk helps individuals make informed decisions about how to proceed with prevention, screening, and treatment options to minimize effects of disease.
When a disease is known to have a strong heritable component, individuals seek genetic counseling (as counselees) to gain further information, including personal and familial risk. For example, women with early-onset breast cancer may obtain genetic counseling to learn information to help them understand and manage their own risk for new primary cancer as well as their family members’ risk for developing cancer. Genetic counselors educate counselees about breast cancer genetics and encourage them to share information with family members who may have increased risk (Riley et al. 2012); however, family communication about genetic risk information may be difficult for a variety of reasons (Julian-Reynier et al. 2000; Sermijn et al. 2004).
Despite reasons for not disclosing and difficulties with sharing genetic results information with family members, sharing can affect whether at-risk family members understand their own risk and are prepared to make informed decisions about prevention and screening. Information shared about genetic counseling is associated with improved accuracy of risk perception of unaffected family members (Himes et al. 2016). Thus, family communication plays an important role in helping family members who have not had genetic counseling themselves (Riley et al. 2012).
Women’s screening and lifestyle choices are based on both risk perceptions and knowledge of breast cancer (Haas et al. 2005; Tilburt et al. 2011). Knowledge about breast cancer genetics is influenced by information obtained as well as an individual’s ability to comprehend that information, which is influenced by health literacy and numeracy. Health literacy is the ability to understand, use, and interpret basic health information necessary to make decisions (Institute of Medicine (U.S.) Committee on Health Literacy 2004). Research suggests that health literacy is an important skill in relation to communicating genetic information (Lea et al. 2011). Numeracy is defined as “the ability to access, use, interpret, and communicate mathematical information and ideas” (Centers for Disease Control and Prevention 2015). Low numeracy skills are associated with poor health outcomes, including a higher prevalence of comorbidities and a 20% increase in prescription medications (Garcia-Retamero et al. 2015). Conversely, strong numeracy skills influence one’s ability to interpret complex information related to cancer risk (Lea et al. 2011), which is essential to making decisions about prevention and treatment. Furthermore, genetic information is often conveyed in terms of probabilistic information that can be difficult to understand without solid numeracy skills.
Additionally, a person’s level of emotional distress is known to influence risk perception (Gibbons and Groarke 2016; van Dooren et al. 2004). Familial cancer involves strong emotions in both affected and non-affected family members. Receiving personalized genetic risk information can cause emotional reactions such as fear, worry, and distress (Marteau and Weinman 2006). Research has demonstrated that higher levels of distress correlate with higher and inaccurate levels of risk perception (Gibbons and Groarke 2016; van Dooren et al. 2004). If distress interferes with the cognitive task of accurately assessing risk, it is possible that higher levels of cancer-related distress may be related to the cognitive task of understanding breast cancer genetics.
The present study is a secondary analysis of data previously gathered. In prior research, we evaluated whether the amount of information shared by counselees, about their genetic counseling sessions, influenced the accuracy of risk perceptions held by their sisters or daughters. We found that women who had more accurate perceptions of personal risk had also received greater amounts of information about family members’ genetic counseling session (Himes et al. 2016). Both knowledge of breast cancer genetics as well as risk perception may influence decisions about prevention and screening behaviors (Marteau and Weinman 2006; Tilburt et al. 2011). Additionally, both breast cancer genetics as well as personal and family risk for breast cancer are discussed in genetic counseling sessions (Riley et al. 2012) Therefore, with the present analysis, we sought to explore factors that might influence knowledge of breast cancer genetics. Choice of factors was guided by theory (Marteau and Weinman 2006; Tilburt et al. 2011) and previous research (Ashida et al. 2011; Haga et al. 2013; Himes et al. 2016; Institute of Medicine (U.S.) Committee on Health Literacy 2004; Lea et al. 2011; Patenaude et al. 2013). We included information shared about genetic counseling as a factor in the present study both because it was found to be important in our prior work and because, in the setting of genetic counseling, counselees are encouraged to share information with family members that will help family members understand their risk for disease. Thus, the purpose of this study was to explore cognitive and emotional variables that influence knowledge of breast cancer genetics in women with a sister or mother who attended genetic counseling and received BRCA1/2 mutation testing.
Materials and methods
In this descriptive, exploratory secondary analysis, we analyzed theory-based relationships among variables related to knowledge of breast cancer genetics. Full details of study methods are published elsewhere (Himes et al. 2016); a brief summary of methods is presented below.
Study population
Participants were adult women who are sisters or daughters of women diagnosed with breast cancer. No participants were affected by breast cancer or received genetic counseling or testing themselves. All participants had a first-degree family member with cancer who received genetic counseling and testing with uninformative negative BRCA1/2 test results between 2010 and 2012. Counseling was administered via in-person or telephone by the same five board-certified genetic counselors. Participants were referred to the study by counselees (their sisters or mothers). After obtaining informed consent, data were collected via mailed survey and telephone interviews.
Measures
All variables were selected a priori. Variable measures are described below.
Knowledge about breast cancer genetics
Knowledge of breast cancer genetics, the outcome variable of interest, was measured using the 27-item Breast Cancer Genetic Counseling Knowledge Questionnaire (BGKQ) (Erblich et al. 2005). This measure was administered to participants in the survey packet. The BGKQ is an objective instrument developed to evaluate knowledge of information typically gained during genetic counseling. This measure has been used to assess knowledge about breast cancer genetics in daughters of women who had received genetic counseling for breast cancer (Patenaude et al., 2013).
Health literacy
Chew, Bradley, and Boyko’s Set of Brief Questions (2004) was used to assess self-reported health literacy. This measure was administered to participants in the survey packet. Each of the three items ask participants about their comprehending both written and verbal information in health care settings and was presented as a 5-point Likert scale ranging from “never” to “always.” Overall score of the three items combined can range from 0 to 15 with higher scores indicating higher self-reported levels of literacy.
Numeracy
The Rasch-based numeracy scale, an eight-item measure of objective numeracy, was used in this study and administered as part of the survey packet (Weller et al. 2012). This composite instrument asks participants to solve math equations to assess knowledge about principles necessary to interpret genetic knowledge. For example, “If the chance of getting a disease is 10%, how many people would be expected to get the disease out of 1000?” (Weller et al. 2012). Possible scores range from 0 to 8.
Cancer-related distress
Cancer-related distress was measured by an adaptation of the 15-item Impact of Events Scale (IES) with a stated stress-inducing scenario of having a known risk of heredity breast cancer. This measure was administered to participants in the survey packet. The scale asks participants to report the frequency of their psychological, physiological, and behavioral responses to an event as follows: not at all = 0, rarely = 1, sometimes = 3, and often = 5. Possible overall scores range from 0 to 75 points.
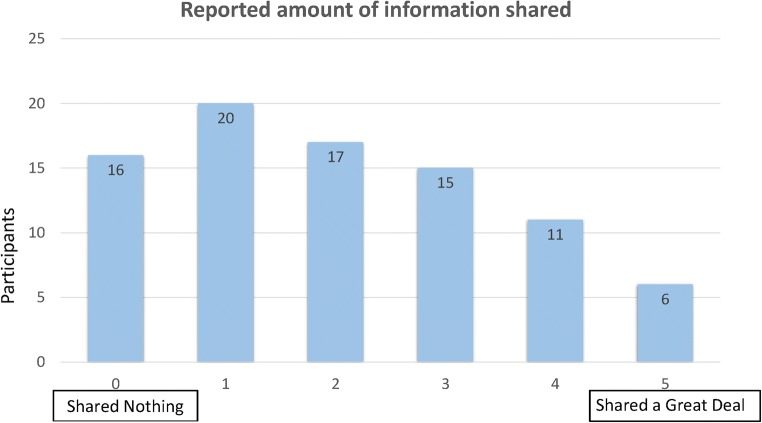
Reported amount of information shared
The variable “reported amount of information shared” was measured during a telephone interview with participants by asking, “Please rate on a scale of 0-5 how much information your sister/mother shared with you about what she learned in her genetic counseling session.” Answers ranged from “shared nothing” (0) to “shared a great deal” (5). This measure was developed for the parent study and was effective in describing amounts of information shared within families (Himes et al., 2016).
Data analysis
Data were analyzed using SPSS 22.0 (IBM Corp., Chicago, IL). Demographics and amount of information shared within families were explored using simple descriptive statistics. Independent associations between knowledge of breast cancer genetics and factors believed to influence knowledge were analyzed using multiple regression. Cancer-related distress and health literacy were transformed to normalize their distributions, which is a statistical requirement for multiple regression. Independent variables in the initial regression included age, education, cancer-related distress, numeracy, health literacy, and reported amount of information shared. All statistical assumptions were met.
Results
The study population included 85 women from the parent study who were mostly married (80.0%), non-Hispanic white (98.8%), and had received some college education (84.7%). The average participant age was 52.2 (SD = 8.9) years old (see Table 1). Most women reported low levels of cancer-related distress and high levels of self-reported health literacy. Instrument range of scores, means, standard deviations, and estimates of internal consistency reliability are presented in Table 2. Most women reported very little information from genetic counseling sessions was shared with them by their mother or sister who attended genetic counseling (see Fig. 1).
Table 1.
Demographics
| Category | Participants |
|---|---|
| n (%) | |
| Age | |
| 40–49 | 37 (43.5) |
| 50–59 | 29 (34.1) |
| 60–69 | 14 (16.4) |
| 70–74 | 5 (5.9) |
| Race/ethnicity | |
| Non-Hispanic White | 84 (98.8) |
| Asian | 1 (1.2) |
| Education | |
| High school/GED | 13 (15.3) |
| Some college/technical school | 32 (37.6) |
| College graduate and beyond | 40 (47.1) |
| Marital status | |
| Married or living as married | 68 (80.0) |
| Separated or divorced | 13 (15.3) |
| Widowed | 2 (2.4) |
| Never married | 2 (2.4) |
| Total | 85 (100.0) |
Table 2.
Results of multiple regression analysis
| Predictors | b [95% CI] | β | p |
|---|---|---|---|
| Age | − 0.10 [− 0.21–0.06] | − 0.13 | 0.25 |
| Distress | 0.18 [− 0.40–0.75] | 0.07 | 0.55 |
| Numeracy | 0.38 [− 0.37–1.12] | 0.11 | 0.31 |
| Health Literacy | − 1.07 [− 3.86–1.73] | − 0.08 | 0.45 |
| Amount of information shared* | 0.98 [0.22–1.74] | 0.28 | 0.01 |
Dependent variable: knowledge of breast cancer genetics. Overall model R2 = 0.139, p = 0.03
Fig. 1.
Reported amount of information shared
Because a small portion of participants were related to one another, intraclass correlation was run to assess the role of family membership among independent variables. Intraclass correlation of the average of all the independent variables was 0.001 indicating that family grouping was not a significant confounder and accounting for nesting was not necessary.
For the regression analysis, we used a process similar to backward elimination where, based on theory and previous research, we selected variables, determined a priori, to be relevant to the dependent variable of interest (knowledge of breast cancer genetics). We used backward elimination to remove variables until significance of the model was achieved. (p < 0.05). Unlike traditional backward elimination, having all predictors statistically significant was not a criteria. This is because variables can be non-significant individually yet still contribute to the overall model fit (R2).
The initial model included independent variables of reported amount of information shared, health literacy, numeracy, cancer-related distress, age, and education. This model explained 13.9% of the variance in the dependent variable (R2 = 0.139) but was non-significant (p = 0.06). Because education contributed the least to the model, it was the first one removed. The resulting regression model was significant (p = 0.03). Further elimination of variables resulted in a worse fitting model; therefore, the remaining variables were retained.
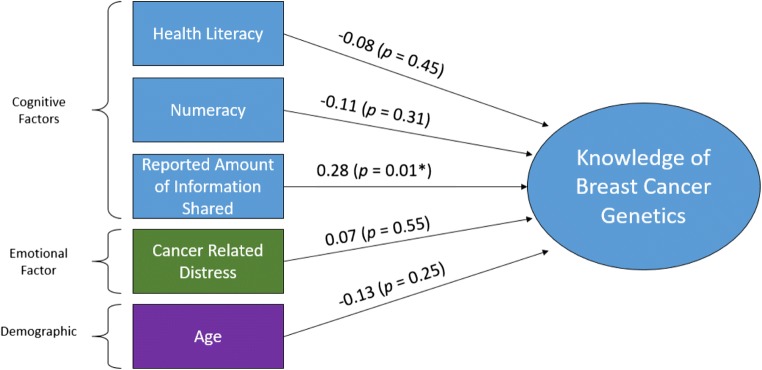
The final overall multiple regression model was significant (p = 0.03) and explained 13.9% of the variance in knowledge of breast cancer genetics (R2 = 0.139). The only predictor variable that was statistically significant was reported amount of information shared (p = 0.01). In practical terms, this result suggests that women of similar age with similar levels of health literacy, numeracy, and cancer distress are more likely to have increased levels of knowledge when probands have shared more information about their genetic counseling sessions. Although health literacy, numeracy, distress, and age were insignificant individually, as a whole, they were all necessary to explain overall variance in knowledge of breast cancer genetics and, thus, remained in the final regression model. Beta weights, a measure of the relative importance of each variable, and p values for each variable are shown in Table 2. The final model is presented in Fig. 2.
Fig. 2.
Final multiple regression model. Influence of cognitive, emotional, and demographic factors on knowledge of breast cancer genetics. Overall model fit: R-squared = 0.139, p < 0.05
Discussion
In order for genetic test results to best impact clinical management for family members, results must be communicated. Lack of knowledge can be a barrier to recommended cancer prevention and screening (Ashida et al. 2011; Patenaude et al. 2013; Schapira et al. 2011). Conversely, knowledge of breast cancer genetics is asserted to be a positive indicator of health (Haga et al. 2013). We found that the reported amount of information shared by a mother or sister about her genetic counseling experience explained a significant amount (β = 0.28, p = 0.01) of the variance in knowledge of breast cancer genetics among their first-degree relatives. In families where more information was shared about genetic counseling, family members (who had not attended counseling) had a greater understanding of breast cancer genetics. These findings underscore the importance of family communication in transferring knowledge about breast cancer genetics.
Although family communication seems to play an important role in knowledge transfer, unfortunately, few participants reported that their mother or sister shared a large amount of information about her genetic counseling (see Fig. 1). In our study, we found that many family members are not receiving personalized information. Sixteen women (nearly 19%) reported that their mother or sister shared nothing about their genetic counseling experience. Therefore, although family communication is encouraged by health professionals as a method of disseminating genetic information in a family (VandenBoom et al. 2017), our findings are consistent with other research indicating that a good portion of genetic test results are not shared among family members (Taber et al. 2015).
Additionally, although greater communication was associated with greater understanding of breast cancer genetics, women’s overall understanding of breast cancer genetics was low with women scoring an average of 10.26 (SD 5.5) items correct on the 27-item BGKQ. This instrument was designed to evaluate knowledge that might be gained through genetic counseling and has primarily been used to assess knowledge of people receiving genetic counseling. In a study of women who had agreed to receive genetic counseling themselves for possible BRCA1/2 testing, baseline scores prior to counseling on the BGKQ averaged 17.4 (SD 4.5); following genetic counseling, their mean scores rose approximately 2 points (Butrick et al. 2015). Thus, women in our study scored an average of 7 points lower on the BGKQ than other women who had not received counseling. However, to be part of the study by Butrick et al. (2015), women needed to have at least a 10% chance of carrying a BRCA1/2 mutation and many of them had breast cancer themselves. It is possible that a personal diagnosis of cancer raises one’s interest in breast cancer genetics to a greater degree than being a sister or daughter of a cancer survivor.
Women in our study had low levels of cancer-related distress with scores on the Impact of Events Scale falling into the subclinical or low range. Impact of event scores can be categorized as subclinical (0–8), mild (9–25), moderate (26–43), and severe (> 44) (Metcalfe et al. 2013). A study by Metcalfe et al. (2013) evaluated 205 sisters of women who were recently diagnosed with breast cancer and found their cancer-related distress to be in the mild to moderate range with an average of 25.6. It is notable that Metcalfe et al. (2013) studied sisters only. Other findings have indicated that sisters of women with breast cancer tend to have higher levels of cancer-related distress than daughters of women with breast cancer (van Dooren et al. 2005).
The Common Sense Model of Self-regulation of Health and Illness (Leventhal et al. 2003) suggests an interplay between emotional and cognitive factors when people contemplate health behaviors (coping actions). We suspected that higher levels of distress (an emotional factor) may interfere with knowledge of breast cancer genetics (a cognitive factor). However, no significant association was found between knowledge of breast cancer genetics and cancer-specific distress. This finding is similar to study results by Kelly et al. (2014), where no significant relationship was found between distress and a variety of cancer-related knowledge outcomes in women at risk for breast cancer. Therefore, distress related to cancer (or cancer risk) may interfere with some, but not all, cognitive factors related to disease. Further research is needed in this area.
Clinical significance
Although it seems logical that health literacy and numeracy might correlate with women’s knowledge of breast cancer genetics, the observation that these variables were not related may be important for healthcare providers. Some patients who perform well on literacy or numeracy evaluations may not understand complex genetic principles well enough to make informed decisions about prevention and screening. Indeed, our sample performed similarly on the Rasch-based Numeracy Scale to three separate samples of adult US citizens totaling 1970 participants [our sample average 4.48 (SD 1.5); combined average of other samples 4.13 (SD 1.87)] (Weller et al. 2012). Thus, clinicians should not assume individuals with high numeracy or self-reported health literacy understand complex genetic information. Clinicians should take care to assess genetic knowledge and help educate where knowledge deficits exist.
Because family communication is the most commonly used strategy for disseminating information about hereditary genetics, it is helpful to understand the relationship between amount of information shared within a family and knowledge outcomes as well as how knowledge impacts guideline-concordant care. Healthcare providers may mistakenly believe that if their patient has a family member with cancer who has received genetic counseling, then their patient will have adequate knowledge about hereditary breast cancer. As our study demonstrates, many counselees do not share information learned in genetic counseling with their close at-risk relatives (see Fig. 1). Additionally, overall knowledge scores were low. Thus, even in families where genetic counseling has been provided to at least one relative, non-counseled family members often need more information. For example, 47% of women in this study did not know there is more than one gene that can increase the risk of breast cancer and 90% did not realize that a father can pass a breast cancer gene mutation down to his daughters. These numbers are especially concerning in this population of women who come from families where no BRCA1/2 mutation was identified but whose family histories appear suspicious for familial or hereditary cancer. In these families, other gene mutations could account for the family history of breast cancer. Misperceptions about whether members of the family are still at risk despite uninformative negative BRCA1/2 test result could lead to sub-optimal screening and prevention measures.
This study illustrates a possible benefit of family communication following genetic counseling; when more information was shared by counselees, women who did not attend genetic counseling had greater knowledge about breast cancer genetics. Future research must be done to confirm this association and to explore causation. If sharing information obtained in genetic counseling with family members enhances knowledge, then interventions should focus on improving methods of sharing genetic information within families. Additionally, sharing family genetic information with healthcare providers is essential. Often, it is the role of the primary care provider to order screening tests and advise about risk reducing measures. Healthcare providers can assist at-risk women to make lifestyle changes (smoking cessation, increased activity, and improved nutrition) to decrease their likelihood of developing breast cancer and other significant health threats.
This study has several limitations worth noting. Counselees may have been biased in whom they referred to the study. It is possible that counselees might have been more likely to refer a family member with whom they had a better relationship and stronger communication. If this bias is present, then the perceived amount of information shared could be even lower in family members not included in the study. The study is also limited by a relatively small sample size and use of a single item to measure the amount of information shared. We did not assess the nature or accuracy of information shared. Because of the cross-sectional nature of this study, we are unable to determine causality in the relationship between information shared and knowledge. In other words, it is possible that because women received more information, they understood more about breast cancer genetics. It is equally plausible that women who understood more about breast cancer genetics sought out more information from their family member who attended genetic counseling. Further research including pre- and post-counseling family knowledge assessment is needed to determine the direction of this relationship. Finally, because our population was primarily composed of non-Hispanic white women, it may not be generalizable to other populations.
Conclusion
Our study found that when more information was shared with family members by counselees, family members had higher levels of knowledge; further research is needed to confirm this association. Unfortunately, few counselees shared a great deal of information about their genetic counseling sessions which contributed to lower levels of knowledge about hereditary breast cancer. More research is needed on developing and disseminating effective strategies to improve family communication. Healthcare providers should encourage women to share with family members what was learned in genetic counseling. Healthcare providers can also help women interpret and utilize personalized genetic information for informed decision-making related to prevention measures and guideline-concordant care.
Funding information
This study was funded by the Elaine Dyer Research Endowment, provided through the Brigham Young University College of Nursing and by a Graduate Research Fellowship, provided through the Office of Graduate Studies at Brigham Young University.
Previous research with first-degree relatives of current participants was supported by grants from the National Cancer Institute at the National Institutes of Health (1R01CA129142 to AYK and U01 CA152958, K05 CA096940, and U01 CA183081 to JSM) and the Huntsman Cancer Foundation. The project was also supported by the Shared Resources (P30 CA042014) at Huntsman Cancer Institute (Biostatistics and Research Design, Genetic Counseling, Research Informatics, and the Utah Population Database [UPDB]); the Utah Cancer Registry, which is funded by Contract No. HHSN261201000026C from the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) Program with additional support from the Utah State Department of Health and the University of Utah; the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 8UL1TR000105 (formerly UL1RR025764).
Compliance with ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ashida S, Hadley DW, Goergen AF, Skapinsky KF, Devlin HC, Koehly LM. The importance of older family members in providing social resources and promoting cancer screening in families with a hereditary cancer syndrome. The Gerontologist. 2011;51:833–842. doi: 10.1093/geront/gnr049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butrick M, Kelly S, Peshkin BN, Luta G, Nusbaum R, Hooker GW, Graves K, Feeley L, Isaacs C, Valdimarsdottir HB, Jandorf L, DeMarco T, Wood M, McKinnon W, Garber J, McCormick SR, Schwartz MD. Disparities in uptake of BRCA1/2 genetic testing in a randomized trial of telephone counseling. Genet Med. 2015;17:467–475. doi: 10.1038/gim.2014.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2015) Understanding literacy and numeracy. https://www.cdc.gov/healthliteracy/learn/understandingliteracy.html. Accessed May 18, 2018
- Erblich J, Brown K, Kim Y, Valdimarsdottir HB, Livingston BE, and Bovbjerg DH (2005) Development and validation of a breast cancer genetic counseling knowledge questionnaire. Patient Education and Counseling 56(2):182–191. 10.1016/j.pec.2004.02.007 [DOI] [PubMed]
- van Dooren S, Rijnsburger AJ, Seynaeve C, Duivenvoorden HJ, Essink-Bot ML, Tilanus-Linthorst MMA, de Koning HJ, Tibben A. Psychological distress in women at increased risk for breast cancer: the role of risk perception. Eur J Cancer. 2004;40:2056–2063. doi: 10.1016/j.ejca.2004.05.004. [DOI] [PubMed] [Google Scholar]
- van Dooren S, et al. The impact of having relatives affected with breast cancer on psychological distress in women at increased risk for hereditary breast cancer. Breast Cancer Res Treat. 2005;89:75–80. doi: 10.1007/s10549-004-2623-y. [DOI] [PubMed] [Google Scholar]
- Garcia-Retamero R, Andrade A, Sharit J, Ruiz JG. Is patients’ numeracy related to physical and mental health? Med Decis Mak. 2015;35:501–511. doi: 10.1177/0272989X15578126. [DOI] [PubMed] [Google Scholar]
- Gibbons A, Groarke A. Can risk and illness perceptions predict breast cancer worry in healthy women? J Health Psychol. 2016;21:2052–2062. doi: 10.1177/1359105315570984. [DOI] [PubMed] [Google Scholar]
- Haas JS, Kaplan CP, Des Jarlais G, Gildengoin V, Perez-Stable EJ, Kerlikowske K. Perceived risk of breast cancer among women at average and increased risk. J Women's Health. 2005;14:845–851. doi: 10.1089/jwh.2005.14.845. [DOI] [PubMed] [Google Scholar]
- Haga SB, Barry WT, Mills R, Ginsburg GS, Svetkey L, Sullivan J, Willard HF. Public knowledge of and attitudes toward genetics and genetic testing. Genet Test Mol Biomarkers. 2013;17:327–335. doi: 10.1089/gtmb.2012.0350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himes DO, Clayton MF, Donaldson GW, Ellington L, Buys SS, Kinney AY. Breast cancer risk perceptions among relatives of women with uninformative negative BRCA1/2 test results: the moderating effect of the amount of shared information. J Genet Couns. 2016;25:258–269. doi: 10.1007/s10897-015-9866-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (U.S.) Committee on Health Literacy . Health literacy : a prescription to end confusion. Washington, D.C: National Academies Press; 2004. [PubMed] [Google Scholar]
- Julian-Reynier C, Sobol H, Sevilla C, Nogues C, Bourret P, French Cancer Genetic N. Uptake of hereditary breast/ovarian cancer genetic testing in a French national sample of BRCA1 families. French Cancer Genet Netw Psychooncol. 2000;9:504–510. doi: 10.1002/1099-1611(200011/12)9:6<504::aid-pon491>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Kelly KM, Ellington L, Schoenberg N, Agarwal P, Jackson T, Dickinson S, Abraham J, Paskett ED, Leventhal H, Andrykowski M. Linking genetic counseling content to short-term outcomes in individuals at elevated breast cancer risk. J Genet Couns. 2014;23:838–848. doi: 10.1007/s10897-014-9705-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lea DH, Kaphingst KA, Bowen D, Lipkus I, Hadley DW. Communicating genetic and genomic information: health literacy and numeracy considerations. Public Health Genomics. 2011;14:279–289. doi: 10.1159/000294191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal H, Brissette I, Leventhal EA. The common-sense model of self-regulation of health and illness. In: Cameron LD, Leventhal H, editors. The self-regulation of health and illness behaviour. New York: Routledge; 2003. pp. 42–65. [Google Scholar]
- Marteau TM, Weinman J. Self-regulation and the behavioural response to DNA risk information: a theoretical analysis and framework for future research. Soc Sci Med. 2006;62:1360–1368. doi: 10.1016/j.socscimed.2005.08.005. [DOI] [PubMed] [Google Scholar]
- Metcalfe KA, Quan ML, Eisen A, Cil T, Sun P, Narod SA. The impact of having a sister diagnosed with breast cancer on cancer-related distress and breast cancer risk perception. Cancer. 2013;119:1722–1728. doi: 10.1002/cncr.27924. [DOI] [PubMed] [Google Scholar]
- National Human Genome Research Institute (2016) Frequently asked questions about genetic and genomic science. https://www.genome.gov/19016904/faq-about-genetic-and-genomic-science/ Accessed May 18, 2018
- Patenaude AF, Tung N, Ryan PD, Ellisen LW, Hewitt L, Schneider KA, Tercyak KP, Aldridge J, Garber JE. Young adult daughters of BRCA1/2 positive mothers: what do they know about hereditary cancer and how much do they worry? Psycho-Oncology. 2013;22:2024–2031. doi: 10.1002/pon.3257. [DOI] [PubMed] [Google Scholar]
- Riley BD, Culver JO, Skrzynia C, Senter LA, Peters JA, Costalas JW, Callif-Daley F, Grumet SC, Hunt KS, Nagy RS, McKinnon WC, Petrucelli NM, Bennett RL, Trepanier AM. Essential elements of genetic cancer risk assessment, counseling, and testing: updated recommendations of the National Society of Genetic Counselors. J Genet Couns. 2012;21:151–161. doi: 10.1007/s10897-011-9462-x. [DOI] [PubMed] [Google Scholar]
- Schapira MM, Neuner J, Fletcher KE, Gilligan MA, Hayes E, Laud P. The relationship of health numeracy to cancer screening. J Cancer Educ. 2011;26:103–110. doi: 10.1007/s13187-010-0133-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sermijn E et al (2004) The impact of proband mediated information dissemination in families with a BRCA1/2 gene mutation. J Med Genet 41:23e–223e. 10.1136/jmg.2003.011353 [DOI] [PMC free article] [PubMed]
- Taber JM, Chang CQ, Lam TK, Gillanders EM, Hamilton JG, Schully SD. Prevalence and correlates of receiving and sharing high-penetrance cancer genetic test results: findings from the Health Information National Trends Survey. Public Health Genomics. 2015;18:67–77. doi: 10.1159/000368745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilburt JC, James KM, Sinicrope PS, Eton DT, Costello BA, Carey J, Lane MA, Ehlers SL, Erwin PJ, Nowakowski KE, Murad MH. Factors influencing cancer risk perception in high risk populations: a systematic review. Hered Cancer Clin Pr. 2011;9:2. doi: 10.1186/1897-4287-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VandenBoom E, Trepanier AM, Carmany EP. Assessment of current genetic counselor practices in post-visit written communications to patients. J Genet Couns. 2017;27:681–688. doi: 10.1007/s10897-017-0163-y. [DOI] [PubMed] [Google Scholar]
- Weller JA, Dieckmann NF, Tusler M, Mertz CK, Burns WJ, Peters E. Development and testing of an abbreviated numeracy scale: a Rasch analysis approach. J Behav Decis Mak. 2012;26:198–212. doi: 10.1002/bdm.1751. [DOI] [PMC free article] [PubMed] [Google Scholar]