Abstract
Background
The evolution of an undergraduate medical student into an adept physician is perpetual, demanding, and stressful. Several studies have indicated medical students have a higher predominance of mental health problems than other student groups of the same age, where medical education acts as a stressor and may lead to unfavorable consequences such as depression, burnout, somatic complaints, decrease in empathy, dismal thoughts about quitting medical school, self harm and suicidal ideation, and poor academic performance. It is imperative to determine the association between important psychoeducational variables and academic performance in the context of medical education to comprehend the response to academic stress.
Objective
The aim of this proof-of-concept study is to determine the relationship between resilience, learning approaches, and stress-coping strategies and how they can collectively predict achievement in undergraduate medical students. The following research questions will be addressed: What is the correlation between the psychoeducational variables resilience, learning approaches, and stress-coping strategies? Can academic performance of undergraduate medical students be predicted through the construction of linear relationships between defined variables employing the principles of empirical modeling?
Methods
Study population will consist of 234 students registered for the MBBS (Bachelor of Medicine, Bachelor of Surgery) at Mohammed Bin Rashid University of Medicine and Health Sciences distributed over 4 cohorts. Newly registered MBBS students will be excluded from the study. Various psychoeducational variables will be assessed using prevalidated questionnaires. For learning approaches assessment, the Approaches and Study Skills Inventory for Students questionnaire will be employed. Resilience and stress-coping strategies will be evaluated using the Wagnild-Young resilience scale and a coping strategies scale derived from Holahan and Moos’s Coping Strategies Scale, respectively. Independent variables (resilience, stress-coping strategies, and learning approaches) will be calculated. Scores will be tested for normality by using the Shapiro-Wilk test. An interitem correlational matrix of the dependent and independent variables to test pairwise correlation will be formed using Pearson bivariate correlation coefficients. Regression models will be used to answer our questions with type II analyses of variance in tests involving multiple predictors. Regression analyses will be checked for homogeneity of variance (Levine test) and normality of residuals and multicollinearity (variance inflation factor). Statistical significance will be set at 5% (alpha=.05). Effect sizes will be estimated with 95% CIs.
Results
Psychoeducational instruments in the form of validated questionnaire have been identified in relation to the objectives. These questionnaires have been formatted for integration into Google forms such that they can be electronically distributed to the consenting participants. We submitted the proposal to MBRU institutional review board (IRB) for which exemption has been awarded (application ID: MBRU-IRB-2019-013). There is no funding in place for this study and no anticipated start date. Total duration of the proposed research is 12 months.
Conclusions
Psychoeducational instruments used in this study will correlate resilience, stress-coping strategies, and learning approaches to academic performance of undergradudate medical students. To the best of our knowledge, no study exploring the multidimensional association of key psychoeducational variables and academic performance in undergraduate medical students has been pursued. Investigated variables, resilience, learning approaches, and stress-coping strategies, are individual traits, however; students’ learning history before they joined MBRU is unknown, so our research will not be able to address this specific aspect.
International Registered Report Identifier (IRRID)
PRR1-10.2196/14677
Keywords: medical education, undergraduate medical education, psychological resilience, resilience, learning, coping behavior, psychological stress
Introduction
Background
The evolution of an undergraduate medical student into a safe and competent physician is interminable, demanding, and stressful [1]. This journey involves combatting what Smith [2] defined as the “swampy lowlands where situations are confusing ‘messes’ incapable of technical solutions” coping with hidden insecurities of clinical practice. In fact, medical students have a higher predominance of mental health problems than other student groups of the same age [3]. This indicates that medical education itself contributes as a key stressor, an observation corroborated by other studies [4,5]. Academic stress is defined as the body’s response to academic-related strains and tensions that exceed adaptive potentials of students. Medical students experience high degrees of academic stress, where the most commonly reported stressors in the academic environment are related to oral presentations, academic overload, scarcity of time to meet commitments, and taking examinations. [6]. While some academic stress may boost academic performance [7], elevated stress levels in medical students may lead to detrimental consequences such as depression [8], burnout [9], somatic complaints [10], decrease in empathy [11], dismal thoughts about quitting medical school [12], suicidal ideation [5], and poor academic performance [13,14]. Therefore, it is imperative to determine the association between important psychoeducational variables and academic performance in the context of medical education to define the role of each psychoeducational variable in the response to academic stress.
Aim
The aim of this proof-of-concept study is to determine the relationship between meta-motivational skills for handling stress (resilience), meta-cognitive skills for study (learning approaches), and meta-emotional skills for managing stress (stress-coping strategies) and how they can collectively predict achievement in undergraduate medical students, founded on the competence of learning, studying, and performing under stress (CLSPS) model [15] (Textbox 1).
The competence of learning, studying, and performing under stress model of de la Fuente [15].
Knows (knowledge):
Facts: knowledge about the characteristics of the class subject or professional exam (career opportunities, percentage of candidates who pass, requirements)
Concepts: competitive exam system, requirements, type of examination, scoring, prior merits/credits, type of class subject
Principles: beliefs about the professional exam or selection process
Knows how (skills):
Principles: beliefs about the professional exam or selection process
Instrumental skills: written and oral skills
Learning and study skills: study skills and techniques
Meta-cognitive skills for study: learning approaches
Meta-emotional skills for managing stress: coping strategies
Meta-motivational skills for managing stress: resilience
Meta-behavioral skills for managing stress: self-regulation strategies
Knows how to be (attitudes):
Attitudes and values: behavioral confidence, achievement motivation, mindset
Study habits (time management, persistence, discipline)
Research Questions
The following research questions will be addressed:
What is the correlation between the psychoeducational variables resilience, learning approaches, and stress-coping strategies in an undergraduate entry medical program?
Can academic performance of undergraduate medical students be predicted through the construction of linear relationships between the defined variables employing the principles of empirical modeling?
Hypotheses
The research questions are founded on the following hypotheses regarding undergraduate medical students:
Resilience is correlated positively with strategic and deep learning approaches and negatively with surface learning approaches.
Resilience is correlated positively with problem-focused stress-coping strategies and negatively with emotion-focused stress-coping strategies.
Emotion-focused stress-coping strategies are correlated positively with surface learning approaches and negatively with strategic and deep learning approaches.
Resilience is a positive predictor of strategic and deep learning approaches and a negative predictor of surface learning approaches; in addition, it is a positive predictor of problem-focused stress-coping strategies and a negative predictor of emotion-focused stress-coping strategies. Moreover, resilience together with strategic and deep learning approaches and problem-focused stress-coping strategies will have a positive and a linear relationship with academic performance.
Literature Review
Search Strategy
Relevant publications were searched in PubMed using the keywords resilience, learning approaches, stress-coping strategies, academic performance, and combinations and variations of these words in conjunction with PubMed-accepted Boolean operators employing the strategy of Jadad et al [16]. Further, this proposal has drawn from the references listed in the research of de la Fuente et al [17] and Garzon-Umerenkova et al [18].
Meta-Motivational Variable: Resilience
Resilience is “a dynamic process wherein individuals display positive adaptation despite experiences of significant adversity or trauma” [19]. In medical education, resilience has a key role as a motivational-affective variable, where it not only acts as a key impetus for the comprehension of scholastic and individual objectives, it also provides one with suitable strategies to tackle adverse conditions of stress and anxiety [20]. Erudition directed to superior academic performance in medical students not only requires motivation, effectively tackling rhythms, modular stresses, and responses of different types but also the capability to self-motivate to effectively counter taxing and traumatic situations, concurrently avoiding circumstances of exacerbation or poignant distress such as vulnerability, apathy, dejection, or anguish [21-23]. Although considerable research has focused on investigating the factors for resilience in medical education, little research has been conducted to investigate the relationship of resilience with other confounding psychoeducational elements such as stress-coping strategies and learning approaches.
Meta-Emotional Variable: Stress-Coping Strategies
Folkman and Moscowitz [24] define coping as “continually changing cognitive and behavioral practices that are developed to handle specific external and/or internal demands that are valued as beyond the individual’s resources.” Individuals cope with different traumatic and taxing circumstances in a manner that surpasses the effect of the situational and chronological context, a phenomenon often referred to as coping styles [25]. Intrinsic to these styles is the involvement of a defined thought process and actions defined by Soucy as stress-coping strategies [26]. These can be broadly classified into three types of strategies [27]: problem-focused, emotion-focused, and avoidance-focused.
Although considerable research has been pursued to characterize the coping strategies of medical students, including a 10-year longitudinal study to predict how coping strategies inform styles of success in medical careers [28], there is a dearth of studies investigating how stress-coping strategies can predict academic performance in a multidimensional milieu (in association with resilience and learning approaches).
Meta-Cognitive Variable: Learning Approaches
Biggs defines learning approaches as “learning processes that emerge from students’ perceptions of academic tasks influenced by their personal characteristics” [29]. Entwistle et al [30] describe 3 learning approaches: deep, surface, and strategic [30] (Figure 1). The deep approach characterizes students who intend to seek meaning for themselves as well as relating ideas and using evidence. The strategic approach involves students who intend to excel academically by organized studying in order to achieve the highest possible grades. The surface apathetic approach has the intention of coping with the minimum course requirements and is linked to rote memorizing and a fear of failure [31].
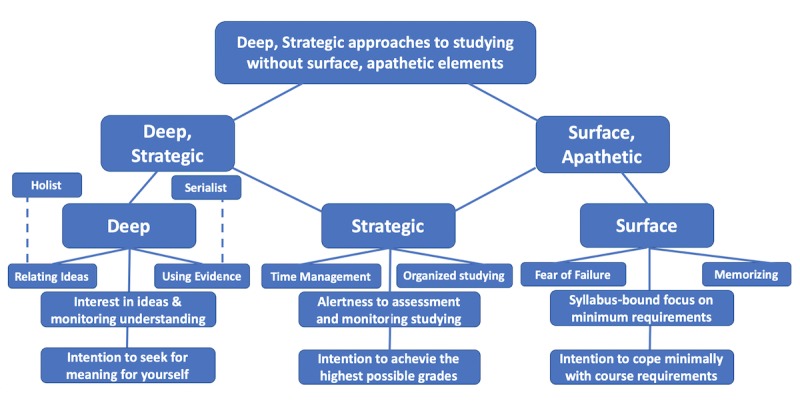
Classification of learning approaches as defined by Entwistle [30].
Preliminary Data From Initial Study
An initial cross-sectional study was pursued at MBRU. The ASSIST questionnaire [30] was circulated to 84 students in the college of medicine. Of the 84 students, 64 responded to the questionnaire. Of the 64 responses, 4 responses were excluded as they were either incomplete or ambiguous. Statistical analysis was conducted on the data obtained from 60 responses. Of these students, 57% (34/60) used a deep learning approach, 16% (10/60) used a strategic learning approach, and 27% (16/60) used a surface learning approach.
Next, we investigated the association of learning approaches with teaching approaches in the 60 responses using logistic regression. In this analysis, responses of 5 students were excluded, as they had equivalent scores in teaching approaches. Among the 55 included students, 71% (39/55) preferred the surface teaching approach and 29% (16/35) preferred the deep teaching approach. Furthermore, strategic learners had a significant positive correlation with perceived academic performance compared with other learners (Figure 2).

Preliminary data showing the frequency of predominant learning approaches classified by predominant teaching approaches.
This initial study indicated that while the predominant learning approach was deep learning (seeking meaning and critical thinking), the preferred teaching approach was surface teaching. Also, strategic learners perceive themselves to perform better academically (Tables 1 and 2) [32].
Table 1.
Correlation of average learning approach scores and academic performance.
| Correlation variable | Strategic score | Surface score | Deep score | Academic performance |
| Strategic score | —a | — | — | — |
| Surface score | –.08 | — | — | — |
| Deep score | .38 | –.32 | — | — |
| Academic performance | .54 | –.25 | .23 | — |
aNot applicable.
Table 2.
P valuesa of correlation of average learning approach scores and academic performance.
| Correlation variable | Strategic score | Surface score | Deep score | Academic performance |
| Strategic score | >.99 | —b | — | — |
| Surface score | .56 | >.99 | — | — |
| Deep score | .003 | .01 | >.99 | — |
| Academic performance | <.001 | .06 | .08 | >.99 |
aSpearman correlation.
bNot applicable.
However, what happens in a multidimensional milieu, when resilience and stress-coping strategies of students are also included, is currently unknown and will be investigated in this study.
Rationale for Proposed Research
In the demanding academic milieu of medical education, the psychoeducational variables resilience, learning approaches, and stress-coping strategies act in concert; it is imperative to investigate the relationships between these variables and their collective effect on the academic performance of undergraduate medical students. To our knowledge this has not been studied, and the proposed research would address this gap.
Methods
Study Landscape
Mohammed Bin Rashid University of Medicine and Health Sciences (MBRU) is a new medical school located in Dubai Health Care City, the health care hub of United Arab Emirates, with a 6-year MBBS (Bachelor of Medicine, Bachelor of Surgery, or Medicinae Baccalaureus Baccalaureus Chirurgiae) undergraduate entry medical program where the curriculum is founded on a competency-based educational model. The MBRU curriculum is divided into 3 phases (Figure 3). Each phase of the curriculum includes integrated courses and builds on the preceding one such that the curriculum is a spiral: the students repeat the study of a subject, each time at a higher level of difficulty and in greater depth. The school has a diverse student population, drawing students from more than 19 countries across the globe. Approximately 75% of the students are women.
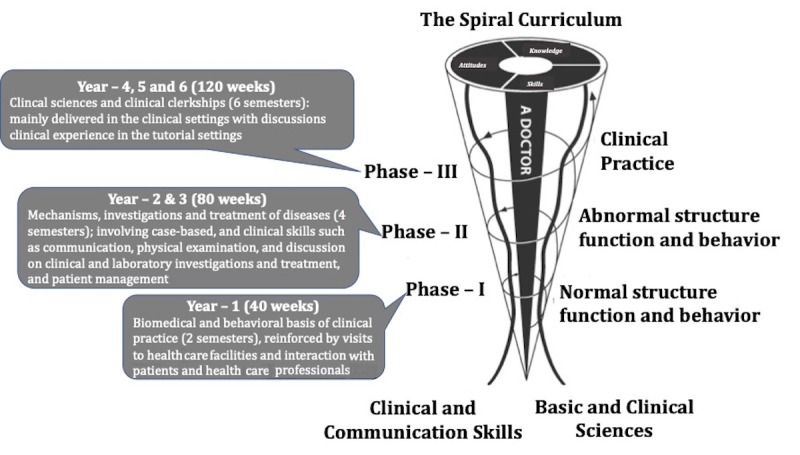
The 6-year undergraduate medical curriculum at Mohammed Bin Rashid University of Medicine and Health Sciences is divided into three phases. Each phase of the curriculum includes integrated courses and builds on the preceding one such that the curriculum is a spiral: the students repeat the study of a subject, each time at a higher level of difficulty and in greater depth.
Participants
As indicated earlier, MBRU is a new medical school in its fourth year of operation. The study population will consist of 234 MBBS students (students in the dental program are not eligible) distributed over four cohorts. Purposive sampling will be used. Newly registered MBBS students will be excluded from the study because their brief period in the program is not adequate to evaluate their academic performance and psychoeducational variables.
Mapping of the correlation coefficient values (over a defined range from .20 to .80) for association of resilience to academic performance with a range of power values (0.60 to 0.90; Table 3) indicates that the number of participants will be suitable for the statistical correlations performed in the study. To detect a simple correlation between resilence and academic performance, where correlation coefficient r=.20 of N observations using a 2-sided test of 5% significance level (alpha=.05) with 80% power (β=0.20), the required sample size is approximately 194.
Table 3.
Power calculation table.
| Power of the study (1-β) | Sample correlation (r) | ||||||
| .20 | .30 | .40 | .50 | .60 | .70 | .80 | |
| 0.90 | 259 | 113 | 62 | 38 | 25 | 17 | 12 |
| 0.80 | 194 | 85 | 47 | 29 | 19 | 13 | 10 |
| 0.70 | 153 | 67 | 37 | 23 | 16 | 11 | 8 |
| 0.60 | 122 | 54 | 30 | 19 | 13 | 10 | 7 |
Learning Approaches Evaluation
Our study will employ a modification of the Approaches and Study Skills Inventory for Students (ASSIST; Multimedia Appendix 1) questionnaire [33] to evaluate the predominant learning approaches of the students. This questionnaire was developed by Entwistle et al [30] to evaluate approaches to learning and has been refined and improved based on educational philosophies put forth by Martin and Saljo [34] and others [29].
The initially published ASSIST questionnaire consists of sections A, B, and C with questions rated on a Likert scale. As shown in Table 4, in the proposed research the 66 items have been reduced to 41 items (sections B and C). We modified the questionnaire to decrease the number of questions while maintaining an equal number of questions across the learning approaches. In the modified ASSIST, 4 items have been added to record the demographics of participants (age, gender, year of study in the MBBS program, and high school education). In modifying the ASSIST questionnaire, care has been taken such that overall validity of the tool is preserved. The original ASSIST questionnaire [30] has been amended instead of using an existing abridged version to make the tool as relevant as possible to the context of the proposed research. Modifications have been introduced to avoid survey fatigue among participants; specific items not relevant to the participants have been removed. Additionally, upon piloting the questionnaire we found that the language in a few items was ambiguous, and we amended these items.
Table 4.
Modified Approaches and Study Skills Inventory for Students questionnaire to be implemented in this study.
| Section | Content | Scale | Modifications |
| A | Conceptions of learning | Likert scale (1-5) | Removed a-f |
| B | Approaches to studying | Likert scale (1-5) | 33/52 questions included (11 per learning approach) |
| C | Preferences for different types of courses and teaching | Likert scale (1-5)a | No modifications (9 total questions) |
| Added | Demographics | Continuous | Age, gender, year of study, high school education |
aLast question: perceived academic performance rating (1-9).
Resilience Evaluation
The Connor-Davison [35] and Wagnild-Young [36] resilience scales were considered for our evaluation. We chose the Wagnild-Young scale (Multimedia Appendix 2) because it was developed using an oblimin rotation factor analysis (allowing correlatation) where the factor construction characterizes personal competence and acceptance of self and life [37]. The scale consists of 14 Likert-scale items grouped in five domains: self-reliance, meaning, equanimity, perseverance, and existential aloneness.
Coping Strategies Evaluation
A 13-item coping strategies questionnaire has been designed (Multimedia Appendix 3) that will assess participant cognitive, emotional, and behavioral approaches for tackling difficulties and problems. The cognitive and emotional approaches (items 2, 3, and 4) have been adapted from the Coping Strategies Scale of Holahan and Moos [38]. Additional items focusing on emotional and cognitive approaches (items 1, 5, 6, and 8) have been adapted from Hamby et al [39]. Other items in the questionnaire are from Spitzberg et al [40].
Data Collection Procedure
Students participating in the proposed research will receive identical information, disseminated through Google Forms, similar to previous research studies conducted in medical education at MBRU [41-43]. Participants will respond to the questionnaires during the self-study time between 11 am and 1 pm (after the morning teaching sessions). Gathering and processing of the collected data will be pursued with the informed consent of the participating students, in line with the ethical and deontological principles of psychology. Collected data will be analyzed in an anonymous and group format, and the data will be stored in an encrypted database and on a password-protected solid-state drive with the research team.
We submitted the proposal to MBRU institutional review board (IRB) for which exemption has been awarded (application ID: MBRU-IRB-2019-013). Further clarification with regard to the policies and terms of reference can be obtained from the IRB.
Data Analysis
The questionnaire response files from Google Forms will be converted to a spreadsheet, and the questions for each approach will be organized into adjacent columns with the value of each response in the respective row. All collected data will be cross-verified by two investigators from the research team. The average score for each questionnaire will be generated for each student. This will be done by taking the average of all responses recorded for a certain questionnaire for a particular student.
SPSS Statistics for Windows version 23.0 (IBM Corp) will be used for all statistical analyses. Cronbach alpha will be used to check internal consistency, and explanatory factor analysis will be used specifically for the questionnaire to confirm the evidence of its validity in the literature. Outliers will be identified by using a Bonferroni outlier test (P<.05). Scores of independent variables (resilience, stress-coping strategies, and learning approaches) will be calculated for independent variables. All scores will be tested for normality by using the Shapiro-Wilk test. An inter-item correlational matrix of the dependent and independent variables to test the pairwise correlation will be formed using Pearson bivariate correlation coefficients. Regression models will be used to answer questions with type II analyses of variance in tests involving multiple predictors. Regression analyses will be checked for homogeneity of variance (Levine test), normality of residuals, and multicollinearity (variance inflation factor). Statistical significance will be set at the conventional 5% threshold (alpha=.05). Effect sizes will be estimated with 95% CIs.
Ordered logistic regression will be used to analyze the effect of individual psychoacademic variables on academic performance controlling for age, gender, and cohort to which the student belongs.
Ethical Considerations
Distributive Justice
Distributive justice in medical education in line with the concept of egalitarianism [44] dictates that all subjects in the study population are provided with just and equal opportunity to participate in the study [45]. The principal investigator is the course director/instructor for several courses across different student cohorts and therefore has regular and extensive interactions with students. Due to this interaction with students, he may develop the preconceived notion that certain students in these cohorts, because of their personality traits, should not participate in the study. As a result, these students may be inadvertently left out if the recruitment of study participants is pursued by the principal investigator. To address this, participation of students from individual cohorts will be overseen by student representatives randomly assigned from each cohort.
Beneficience
Although studies pertaining to the “July phenomenon” (rise in the morbidity and mortality of patients with the inflow of new medical trainees) [46,47] have been unfounded, they have raised concerns regarding beneficence in medical education research. Keeping in mind the key aspects of beneficence, this study includes validated questionnaires and analytical tools and methodologies that have been used in other similar studies without any untoward physiological and psychological effect on the participants. Also, recruitment of participants will involve the use of smart applications (relying less on human involvement), which will minimize harm to the participants from relatively inexperienced researchers (students overseeing recruitment, etc).
Power Differential
The power differential under the five bases of power (coercive, reward, legitimate, referent, and expert [48]) must be considered because one of the principal investigators is both the primary researcher and the course director/instructor for several courses across different student cohorts in the study. To prevent such a power differential from compelling subjects to participate in the study, recruitment and associated processes will be carried out by a faculty member from the MBRU school of dentistry, who isn’t in a power relationship with the undergraduate medical students.
Respect for Participants
One of the key aspects of the Helsinki declaration on ethical guidance on research involving human subjects requires researchers to acknowledge autonomy of study participants and protect those with diminished autonomy [49]. Therefore, data will be obtained only from consenting participants. All study participants will be required to sign a consent form.
Confidentiality
Each participant will be assigned a unique study identifier. No participant names will be collected. Participant responses will be de-identified or anonymized and reported in aggregate. A repository will be created containing participant responses, which will be encrypted and password-protected.
Results
This study is at the protocol development stage only, and as such, no results are available. The psychoeducational instruments in the form of validated questionnaires have been identified in relation to the objectives. These questionnaires have been formatted for integration into Google Forms such that they can be electronically distributed to the consenting participants.
The MBRU IRB reviewed this study and provided an exempt status (MBRU-IRB-2019-013). Further clarification and information can be obtained from the MBRU IRB at irb@mbru.ac.ae. There is no funding in place for this study and no anticipated start date. The total duration of the proposed research is 12 months. Key project milestones and timeline are shown in Figure 4.

Important project milestones. IRB: institutional review board; MBRU: Mohammed Bin Rashid University of Medicine and Health Sciences.
Discussion
Summary
We have presented the data from an initial study, where we have correlated student learning approach to academic performance. Data from this initial study further encouraged us to investigate academic performance of medical students in a multidimensional setting; when resilience and stress-coping strategies are also included, the study protocol for this investigation is presented in this article.
Findings from this investigation will elaborate on the need for further research regarding resilience in medical students and how resilience can be improved in this population and emphasize that the concepts of stress, burnout, resilience, and coping appear to be very much related in the context of undergraduate medical education.
Limitations
The investigated variables, resilience, learning approaches, and stress-coping strategies, are individual traits; students’ learning history before they joined MBRU is unknown, so our research will not be able to address this specific aspect. Investigating this aspect would be difficult as the MBRU student pool draws from 19 different countries and 15 different high school curricula.
In addition, we cannot consider the gender variable in this study as more than 80% of our students are women, which has shown to have an effect on the investigated variables [50,51].
Conclusions
Results from the different psychoeducational instruments will institute the associative and extrapolative multidimensionality of the different variables in envisaging academic performance of medical students. To our knowledge, no study exploring the multidimensional association of learning approach, resilience, stress-coping strategies, and academic performance in undergraduate medical students has been pursued [52].
Additionally, this research will validate and expand on previous research on the importance of resilience and its association with academic stress and coping strategies in medical students [53,54]. Study results may initiate a framework for assessing psychoeducational variables while admitting students to medical school or during counseling as part of psychoeducational services.
Future studies from this research should investigate the associations of the studied psychoeducational variables with academic emotions or insufficient approaches of stress management, [55-57]. Study results can initiate strategies to integrate the studied variables in different models of medical curricula [58,59], adding to the understanding of the role of meta-motivational and meta-affective approaches during learning in medical school [60].
Abbreviations
- ASSIST
Approaches and Study Skills Inventory for Students
- CLSPS
competence of learning, studying, and performing under stress
- IRB
institutional review board
- MBBS
Bachelor of Medicine, Bachelor of Surgery
- MBRU
Mohammed Bin Rashid University of Medicine and Health Sciences
Appendix
Modified Approaches and Study Skills Inventory for Students [32] questionnaire.
The 25-item Resilience Scale of Wagnild and Young [35].
The 13-item Coping Scale.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Shoaib M, Afzal A, Aadil M. “Medical students” burn out: need of student mentor and support groups and emotional resilience skills training to be a part of medical school curriculum. Adv Med Educ Pract. 2017;8:179–180. doi: 10.2147/AMEP.S132809. doi: 10.2147/AMEP.S132809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith J. Reflecting in the swampy lowlands. BMJ. 2004 Aug 26;329(7464) doi: 10.1136/bmj.329.7464.0-f. [DOI] [Google Scholar]
- 3.Hill MR, Goicochea S, Merlo LJ. In their own words: stressors facing medical students in the millennial generation. Med Educ Online. 2018 Dec;23(1):1530558. doi: 10.1080/10872981.2018.1530558. http://europepmc.org/abstract/MED/30286698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosal MC, Ockene IS, Ockene JK, Barrett SV, Ma Y, Hebert JR. A longitudinal study of students' depression at one medical school. Acad Med. 1997 Jun;72(6):542–546. doi: 10.1097/00001888-199706000-00022. [DOI] [PubMed] [Google Scholar]
- 5.Compton MT, Carrera J, Frank E. Stress and depressive symptoms/dysphoria among US medical students: results from a large, nationally representative survey. J Nerv Ment Dis. 2008 Dec;196(12):891–897. doi: 10.1097/NMD.0b013e3181924d03. [DOI] [PubMed] [Google Scholar]
- 6.Kötter T, Wagner J, Brüheim L, Voltmer E. Perceived Medical School stress of undergraduate medical students predicts academic performance: an observational study. BMC Med Educ. 2017 Dec 16;17(1):256. doi: 10.1186/s12909-017-1091-0. https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-017-1091-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Toews JA, Lockyer JM, Dobson DJ, Simpson E, Brownell AK, Brenneis F, MacPherson KM, Cohen GS. Analysis of stress levels among medical students, residents, and graduate students at four Canadian schools of medicine. Acad Med. 1997 Nov;72(11):997–1002. doi: 10.1097/00001888-199711000-00019. [DOI] [PubMed] [Google Scholar]
- 8.Stecker T. Well-being in an academic environment. Med Educ. 2004 May;38(5):465–478. doi: 10.1046/j.1365-2929.2004.01812.x. [DOI] [PubMed] [Google Scholar]
- 9.Dyrbye LN, Power DV, Massie FS, Eacker A, Harper W, Thomas MR, Szydlo DW, Sloan JA, Shanafelt TD. Factors associated with resilience to and recovery from burnout: a prospective, multi-institutional study of US medical students. Med Educ. 2010 Oct;44(10):1016–1026. doi: 10.1111/j.1365-2923.2010.03754.x. [DOI] [PubMed] [Google Scholar]
- 10.Mosley TH, Perrin SG, Neral SM, Dubbert PM, Grothues CA, Pinto BM. Stress, coping, and well-being among third-year medical students. Acad Med. 1994 Sep;69(9):765–767. doi: 10.1097/00001888-199409000-00024. [DOI] [PubMed] [Google Scholar]
- 11.Neumann M, Edelhäuser F, Tauschel D, Fischer MR, Wirtz M, Woopen C, Haramati A, Scheffer C. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011 Aug;86(8):996–1009. doi: 10.1097/ACM.0b013e318221e615. [DOI] [PubMed] [Google Scholar]
- 12.Dyrbye LN, Harper W, Durning SJ, Moutier C, Thomas MR, Massie FS, Eacker A, Power DV, Szydlo DW, Sloan JA, Shanafelt TD. Patterns of distress in US medical students. Med Teach. 2011;33(10):834–839. doi: 10.3109/0142159X.2010.531158. [DOI] [PubMed] [Google Scholar]
- 13.Linn BS, Zeppa R. Stress in junior medical students: relationship to personality and performance. J Med Educ. 1984 Jan;59(1):7–12. [PubMed] [Google Scholar]
- 14.Hojat M, Robeson M, Damjanov I, Veloski JJ, Glaser K, Gonnella JS. Students' psychosocial characteristics as predictors of academic performance in medical school. Acad Med. 1993 Aug;68(8):635–637. doi: 10.1097/00001888-199308000-00015. [DOI] [PubMed] [Google Scholar]
- 15.de la Fuente-Arias J. Theory of self- vs. externally-regulated learning: fundamentals, evidence, and applicability. Front Psychol. 2017;8:1675. doi: 10.3389/fpsyg.2017.01675. doi: 10.3389/fpsyg.2017.01675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jadad AR, McQuay HJ. Searching the literature. Be systematic in your searching. BMJ. 1993 Jul 03;307(6895):66. doi: 10.1136/bmj.307.6895.66-a. http://europepmc.org/abstract/MED/8343701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de la Fuente J, Sander P, Martínez-Vicente JM, Vera M, Garzón A, Fadda S. Combined effect of levels in personal self-regulation and regulatory teaching on meta-cognitive, on meta-motivational, and on academic achievement variables in undergraduate students. Front Psychol. 2017;8:232. doi: 10.3389/fpsyg.2017.00232. doi: 10.3389/fpsyg.2017.00232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garzón-Umerenkova A, de la Fuente J, Amate J, Paoloni PV, Fadda S, Pérez JF. A linear empirical model of self-regulation on flourishing, health, procrastination, and achievement, among university students. Front Psychol. 2018;9:536. doi: 10.3389/fpsyg.2018.00536. doi: 10.3389/fpsyg.2018.00536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greenhill J, Fielke KR, Richards JN, Walker LJ, Walters LK. Towards an understanding of medical student resilience in longitudinal integrated clerkships. BMC Med Educ. 2015 Aug 21;15:137. doi: 10.1186/s12909-015-0404-4. https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-015-0404-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cicchetti D. Resilience under conditions of extreme stress: a multilevel perspective. World Psychiatry. 2010 Oct;9(3):145–154. doi: 10.1002/j.2051-5545.2010.tb00297.x. https://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=1723-8617&date=2010&volume=9&issue=3&spage=145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eley DS, Stallman H. Where does medical education stand in nurturing the 3Rs in medical students: responsibility, resilience and resolve? Med Teach. 2014 Oct;36(10):835–837. doi: 10.3109/0142159X.2014.917159. [DOI] [PubMed] [Google Scholar]
- 22.McKenna KM, Hashimoto DA, Maguire MS, Bynum WE. The missing link: connection is the key to resilience in medical education. Acad Med. 2016 Dec;91(9):1197–1199. doi: 10.1097/ACM.0000000000001311. [DOI] [PubMed] [Google Scholar]
- 23.Olson K, Kemper KJ, Mahan JD. What factors promote resilience and protect against burnout in first-year pediatric and medicine-pediatric residents? J Evid Based Complementary Altern Med. 2015 Jul;20(3):192–198. doi: 10.1177/2156587214568894. [DOI] [PubMed] [Google Scholar]
- 24.Folkman S, Moskowitz JT. Coping: pitfalls and promise. Annu Rev Psychol. 2004;55:745–774. doi: 10.1146/annurev.psych.55.090902.141456. [DOI] [PubMed] [Google Scholar]
- 25.Hamaideh SH. Stressors and reactions to stressors among university students. Int J Soc Psychiatry. 2011 Jan;57(1):69–80. doi: 10.1177/0020764009348442. [DOI] [PubMed] [Google Scholar]
- 26.Soucy Chartier I, Gaudreau P, Fecteau M. From dispositional affect to academic goal attainment: the mediating role of coping. Anxiety Stress Coping. 2011 Jan;24(1):43–58. doi: 10.1080/10615801003725360. [DOI] [PubMed] [Google Scholar]
- 27.Nakano K. Coping strategies and psychological symptoms in a Japanese sample. J Clin Psychol. 1991 May;47(3):346–350. doi: 10.1002/1097-4679(199105)47:3<346::aid-jclp2270470304>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 28.Tartas M, Walkiewicz M, Budziński W, Majkowicz M, Wójcikiewicz K, Zdun-Ryżewska A. The coping strategies during medical education predict style of success in medical career: a 10-year longitudinal study. BMC Med Educ. 2016 Jul 22;16:186. doi: 10.1186/s12909-016-0706-1. https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-016-0706-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Biggs J. Learning Strategies and Learning Styles. New York: Springer; 1988. Approaches to learning and to essay writing. [Google Scholar]
- 30.Entwistle N, Tait H, McCune V. Patterns of response to an approaches to studying inventory across contrasting groups and contexts. Eur J Psychol Educ. 2000 Mar;15(1):33–48. doi: 10.1007/BF03173165. [DOI] [Google Scholar]
- 31.Dolmans D, Loyens S, Marcq H, Gijbels D. Deep and surface learning in problem-based learning: a review of the literature. Adv Health Sci Educ Theory Pract. 2016 Dec;21(5):1087–1112. doi: 10.1007/s10459-015-9645-6. http://europepmc.org/abstract/MED/26563722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Akhras A. A Single Center Cross-Sectional Study Investigating the Learning Approaches in Undergraduate Medical Education [student research project] Dubai: Basic Medical Sciences, Mohammed Bin Rasheed University of Medicine and Health Sciences; 2018. Jun, [Google Scholar]
- 33.Reid WA, Evans P, Duvall E. Medical students' approaches to learning over a full degree programme. Med Educ Online. 2012;17 doi: 10.3402/meo.v17i0.17205. http://europepmc.org/abstract/MED/22927717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nakamura A, Osonoi T, Terauchi Y. Relationship between urinary sodium excretion and pioglitazone-induced edema. J Diabetes Investig. 2010 Oct 19;1(5):208–211. doi: 10.1111/j.2040-1124.2010.00046.x. doi: 10.1111/j.2040-1124.2010.00046.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 36.Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. J Nurs Meas. 1993;1(2):165–178. [PubMed] [Google Scholar]
- 37.Wagnild G. A review of the Resilience Scale. J Nurs Meas. 2009;17(2):105–113. doi: 10.1891/1061-3749.17.2.105. [DOI] [PubMed] [Google Scholar]
- 38.Holahan CJ, Moos RH. Personal and contextual determinants of coping strategies. J Pers Soc Psychol. 1987 May;52(5):946–955. doi: 10.1037//0022-3514.52.5.946. [DOI] [PubMed] [Google Scholar]
- 39.Hamby S, Grych J, Banyard V. Life Paths measurement packet: finalized scales. Sewanee: Life Paths Research Program; 2015. [2019-07-05]. https://www.lifepathsresearch.org/wp-content/uploads/Life-Paths-Measurement-Packet-finalized-scales-Aug-2015.pdf. [Google Scholar]
- 40.Spitzberg B, Cupach W. Studies in Applied Interpersonal Communication. First Edition. Thousand Oaks: Sage; 2008. [Google Scholar]
- 41.Banerjee Y, Tambi R, Gholami M, Alsheikh-Ali A, Bayoumi R, Lansberg P. Augmenting flexnerism via twitterism: need for integrating social media application in blueprinting pedagogical strategies for undergraduate medical education. JMIR Med Educ. 2019 Mar 25;5(1):e12403. doi: 10.2196/12403. http://mededu.jmir.org/2019/1/e12403/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Banerjee Y, Azar AJ, Tuffnell C, Lansberg PJ, Bayoumi R, Davis D. A novel 6D-approach to radically transform undergraduate medical education: preliminary reflections from MBRU. BMC Med Educ. 2018 Dec 12;18(1):304. doi: 10.1186/s12909-018-1402-0. https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-018-1402-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tambi R, Bayoumi R, Lansberg P, Banerjee Y. Blending Gagne's instructional model with Peyton's approach to design an introductory bioinformatics lesson plan for medical students: proof-of-concept study. JMIR Med Educ. 2018 Oct 25;4(2):e11122. doi: 10.2196/11122. http://mededu.jmir.org/2018/2/e11122/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Abásolo I, Tsuchiya A. Egalitarianism and altruism in health: some evidence of their relationship. Int J Equity Health. 2014 Feb 06;13:13. doi: 10.1186/1475-9276-13-13. https://equityhealthj.biomedcentral.com/articles/10.1186/1475-9276-13-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Capp S, Savage S, Clarke V. Exploring distributive justice in health care. Aust Health Rev. 2001;24(2):40–44. doi: 10.1071/ah010040. [DOI] [PubMed] [Google Scholar]
- 46.Rich EC, Gifford G, Luxenberg M, Dowd B. The relationship of house staff experience to the cost and quality of inpatient care. JAMA. 1990 Feb 16;263(7):953–957. [PubMed] [Google Scholar]
- 47.Perry RP. It's ok to get sick in July. JAMA. 1990 Feb 16;263(7):994. [PubMed] [Google Scholar]
- 48.Milgram S. Behavioral Study of Obedience. J Abnorm Psychol. 1963 Oct;67:371–378. doi: 10.1037/h0040525. [DOI] [PubMed] [Google Scholar]
- 49.World Medical Association World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013 Nov 27;310(20):2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 50.Stöber J. Dimensions of test anxiety: relations to ways of coping with pre-exam anxiety and uncertainty. Anxiety Stress Coping. 2004 Sep;17(3):213–226. doi: 10.1080/10615800412331292615. [DOI] [Google Scholar]
- 51.Rubin M, Scevak J, Southgate E, Macqueen S, Williams P, Douglas H. Older women, deeper learning, and greater satisfaction at university: age and gender predict university students’ learning approach and degree satisfaction. J Diversity Higher Educ. 2018 Mar;11(1):82–96. doi: 10.1037/dhe0000042. [DOI] [Google Scholar]
- 52.Erschens R, Loda T, Herrmann-Werner A, Keifenheim KE, Stuber F, Nikendei C, Zipfel S, Junne F. Behaviour-based functional and dysfunctional strategies of medical students to cope with burnout. Med Educ Online. 2018 Dec;23(1):1535738. doi: 10.1080/10872981.2018.1535738. http://europepmc.org/abstract/MED/30371222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yoo HH, Park KH. [Relationships among emotional intelligence, ego-resilience, coping efficacy, and academic stress in medical students] Korean J Med Educ. 2015 Sep;27(3):187–193. doi: 10.3946/kjme.2015.27.3.187. doi: 10.3946/kjme.2015.27.3.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Slavin SJ, Schindler DL, Chibnall JT. Medical student mental health 3.0: improving student wellness through curricular changes. Acad Med. 2014 Apr;89(4):573–577. doi: 10.1097/ACM.0000000000000166. http://Insights.ovid.com/pubmed?pmid=24556765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ayala EE, Roseman D, Winseman JS, Mason HRC. Prevalence, perceptions, and consequences of substance use in medical students. Med Educ Online. 2017;22(1):1392824. doi: 10.1080/10872981.2017.1392824. http://europepmc.org/abstract/MED/29072119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Talih F, Daher M, Daou D, Ajaltouni J. Examining burnout, depression, and attitudes regarding drug use among lebanese medical students during the 4 years of medical school. Acad Psychiatry. 2018 Apr;42(2):288–296. doi: 10.1007/s40596-017-0879-x. [DOI] [PubMed] [Google Scholar]
- 57.Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, Sen S, Mata DA. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016 Dec 06;316(21):2214–2236. doi: 10.1001/jama.2016.17324. http://europepmc.org/abstract/MED/27923088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bird A, Martinchek M, Pincavage AT. A curriculum to enhance resilience in internal medicine interns. J Grad Med Educ. 2017 Oct;9(5):600–604. doi: 10.4300/JGME-D-16-00554.1. http://europepmc.org/abstract/MED/29075380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Passi V. Developing resilience throughout the continuum of medical education. Perspect Med Educ. 2014 Nov;3(5):329–331. doi: 10.1007/s40037-014-0140-1. http://europepmc.org/abstract/MED/25395227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Whitcomb ME. More on competency-based education. Acad Med. 2004 Jun;79(6):493–494. doi: 10.1097/00001888-200406000-00001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Modified Approaches and Study Skills Inventory for Students [32] questionnaire.
The 25-item Resilience Scale of Wagnild and Young [35].
The 13-item Coping Scale.


