Abstract
Background
The aim of this study was to analyze the efficacy of vacuum sealing drainage combined with Ilizarov bone transport technique in the treatment of tibial traumatic osteomyelitis and risk factors for postoperative pin infection.
Material/Methods
We enrolled 78 patients with tibial traumatic osteomyelitis admitted at the First People’s Hospital of Kashgar from January 2015 to September 2017 and treated with vacuum sealing drainage combined with Ilizarov bone transport technique.
Results
After combined treatment, SAS and SDS scores decreased significantly, while SF-36 scores increased significantly. Comparisons showed that there were significant differences in the scores of patients after treatment (P<0.05). Univariate analysis showed that there were no significant differences in gender, BMI, hypertension, diabetes mellitus, COPD, smoking index, alcohol abuse history, or residence (P>0.05). There were significant differences in age, fracture type, fixation type, pin loosening, and indwelling time between the 2 groups (P<0.05). Multivariate logistic analysis showed that age, fracture type, fixation type, pin loosening, and indwelling time were independent risk factors for pin infection. Age, fracture type, fixation type, pin loosening, and indwelling time are independent risk factors for pin infection in patients with tibial traumatic osteomyelitis.
Conclusions
Combination of vacuum sealing drainage with Ilizarov bone transport technique can effectively improve the condition of tibial traumatic osteomyelitis, improve the quality of life of patients, and reduce the occurrence of adverse emotions of patients. Age, fracture type, fixation type, pin loosening, and indwelling time are independent risk factors for pin infection in patients with tibial traumatic osteomyelitis.
MeSH Keywords: Negative-Pressure Wound Therapy; Tissue Expansion Devices; Vacuum Extraction, Obstetrical
Background
With the gradual development of society and the acceleration of industrial modernization, there are more and more cases of high-energy injuries, and limb fractures are the most common clinically [1]. Because patients are prone to wound infection, skin necrosis, and long-term wound healing after fracture, it is very easy for patients to develop traumatic osteomyelitis without effective treatment. As a chronic disease, traumatic osteomyelitis is mainly caused by wound, operation or tissue infection around the wound. and the patient is often accompanied by repeated infection and low fever. If the patient does not undergo timely debridement treatment, the pathogens existing in the lesion tissue for a long time can also cause low reactive inflammation, dead bone and sinus tract [2,3]. Research shows that [4], tibia is the most common site of traumatic osteomyelitis, and patients with tibial osteomyelitis not only have fractures, but also will be accompanied by bone infection and bone exposure. Bone infection is not conducive to fracture healing, and bone exposure can affect infection control and even aggravate the infection of patients. Therefore, clinical workers urgently need to find an effective treatment to improve the patient’s condition.
Surgery is the main clinical treatment of tibial traumatic osteomyelitis. Its principle is to promote bone healing by killing the necrotic joint cavity and clearing the lesions. However, the traditional treatment is to prevent active infection by antibiotics and surgical removal of the wound, then to close the wound by skin flap transplantation, and finally to repair the bone defect by free bone transplantation. It not only takes a lot of time and money, but also increases patients’ negative emotions and reduces patients’ healing and recovery [5,6]. With the continuous improvement of medical level, more and more treatment schemes have been applied in clinic. Vacuum sealing drainage and Ilizarov technology have been favored by clinicians in the treatment of tibial traumatic osteomyelitis. Vacuum sealing drainage can completely seal the wound and reduce the probability of cross infection in the surrounding tissues of patients. And continuous negative pressure suction can effectively remove the exudate and necrotic tissue of the wound, improve microcirculation of the wound and eliminate tissue edema [7,8]. Ilizarov technique can completely remove the necrotic bone segments without re-repair of bone and soft tissue. It can effectively control infection and shorten the treatment time of patients [9].
However, Ilizarov technology is likely to appear pin infection in the clinical treatment process, which may prolong the treatment time of patients and have a certain impact on the quality of life of patients [10]. However, Ilizarov technology is likely to cause pin infection in the clinical treatment process, which may prolong the treatment time of patients and affect the quality of life of patients [10]. Therefore, in this study, we explored the efficacy of vacuum sealing drainage combined with Ilizarov bone transport technique in the treatment of tibial traumatic osteomyelitis, and analyzed the risk factors of pin infection in patients, so as to provide reference for clinicians.
Material and Methods
Clinical data of the patient
78 patients with tibial traumatic osteomyelitis admitted in The First People’s Hospital of Kashgar from January 2015 to September 2017 were selected as the study subjects (study group). Patients were treated with vacuum sealing drainage combined with Ilizarov bone transport technique. There were 52 male patients and 26 female patients, with an age range of 23 to 68 years and an average age of 44.5±10.5 years. Causes of injury: 54 cases of traffic accident, 12 cases of high-fall injury, 8 cases of crush injury and 4 cases of other injuries. According to the Gustilo-Anderson classification, there were 35 patients with type III and 43 patients with type IV (Table 1). The study was approved by the Medical Ethics Committee of The First People’s Hospital of Kashgar, and all family members and patients were informed and signed informed consent.
Table 1.
Clinical data of patients.
| Factor | Research group(n=78) |
|---|---|
| Sex | |
| Male | 52 (66.67) |
| Female | 26 (33.33) |
| Age (years) | |
| ≥50 | 24 (30.77) |
| <50 | 54 (69.23) |
| BMI (kg/m2) | 23.15±1.84 |
| Anamnesis | |
| Hypertension | 30 (38.46) |
| Diabetes mellitus | 25 (32.05) |
| COPD | 8 (10.26) |
| Smoking index (branch) | |
| ≥400 | 59 (75.64) |
| <400 | 19 (24.36) |
| History of alcoholism | |
| Yes | 13 (16.67) |
| No | 65 (83.33) |
| Domicile | |
| City | 70 (89.74) |
| Village | 8 (10.26) |
| Cause of injury in patients | |
| Traffic accident | 54 (69.23) |
| High fall injury | 12 (15.38) |
| Crush injury | 8 (10.26) |
| Other | 4 (5.13) |
| Gustilo-Anderson typing | |
| III type | 35 (44.87) |
| IV type | 43 (55.13) |
| Classification of fracture | |
| Open tibial fracture | 48 (61.54) |
| Closed tibial fracture | 30 (38.46) |
| Fixed type | |
| Plate internal fixation | 38 (48.72) |
| External fixator fixation | 40 (51.28) |
COPD – chronic obstructive pulmonary disease; BMI – body mass index.
Inclusion and exclusion criteria
Inclusion criteria: All patients were examined by X-ray and CT three-dimensional reconstruction. All patients met the diagnostic criteria of traumatic osteomyelitis. The patient’s lesion was located in the humerus. The patient’s condition was stable and surgery was possible. The patient’s clinical data was complete and can be combined with regular follow-up and treatment. Bone defect was more that 4 cm.
Exclusion criteria: patients with malignant tumors; patients with gestational or lactating gestational women; patients with lesions who had previous fractures before the current study and who had a history of related treatments; patients whose surgical risk exceeded the efficacy; patients who could not undergo surgery (All patients are treated conservatively).
Treatment programs
All patients in this study were treated with vacuum sealing drainage combined with Ilizarov bone transport technique. The treatment programs are as follows:
The patient was placed in a supine position and anesthetized with general anesthesia or continuous epidural anesthesia. The conventional drape is disinfected, and the affected limb is raised and treated with a disinfecting balloon tourniquet (the external fixed stent is taken out). Clean the patient’s wound, remove the scar, sinus and infected soft tissue, and remove the original internal fixation. The hardened and necrotic bone was resected and the medullary cavity was dredged. Loosen the tourniquet. After the blood is completely stopped, debridement is performed again until the wound edge and the bone end have fresh blood oozing out. The wound was subsequently cleaned (brine, 3% hydrogen peroxide solution, 5% povidone iodine solution). Tibial traumatic osteomyelitis was treated with vacuum sealing drainage combined with Ilizarov bone transport technique. The negative pressure closed drainage foam material was cut according to the size and shape of the patient’s wound surface. After cutting the material, fill it into the dead space and cover the wound. Then, the bio-permeable film was closed, sutured and fixed, and connected to the central negative pressure to ensure its airtight state. The Ilizarov external fixation stent (Taizhou Wuyan Medical Technology Development Co., Ltd. China) was selected for fixation according to the patient’s condition (the metaphysis was selected as the osteotomy site). The Ilizarov ring external fixation extension frame was placed on the patient’s leg, parallel to the upper and lower tibia rings (and across the osteotomy plane). Use 2 (1.5~2.0mm) Kirschner wire to drill into each ring at a constant speed (the angle of the same ring is 30~50°). It is then fixed (the removable bone mass can be fixed with a hydroxyapatite screw). Avoid contact with nerve vessels when entering the needle and ensure the integrity of the patient’s medullary cavity. If the patient needs to extend the limb, the tibia must be cut at the corresponding site. If the patient’s wound can be sutured directly, a negative pressure drainage tube is placed at the bone defect (the drainage tube is removed when the drainage fluid is <50 mL/d). If the patient’s wound cannot be directly closed, the negative pressure drainage material is used to cover the wound surface, and vacuum suction is performed until the patient’s wound is closed. The patients were treated with drug sensitive antibiotics according to the samples taken during the operation. After the patient’s white blood cell and central granulocyte count were normal, the drug was stopped. Continue negative pressure suction on the patient. Pay attention to whether there is a blockage in the pipeline. The pressure is adjusted according to the patient’s condition. The dressing is changed once a week, and the needle is disinfected daily with alcohol drip. During the process of bone transport, close attention is paid to the patient’s foot artery and posterior tibial artery pulse. Pay attention to the skin feeling of the patient’s calf and foot, and start transporting after 7 days, 1mm/d. It was performed in 4 times. When X-ray showed that the new callus bone was solid and well ossified, and the bone mineralization was basically mature, the limb could be loaded and removed from the external fixator.
Outcome measurement
Main observation index: The efficacy of patients was assessed according to Paley fracture evaluation criteria [11] (Table 2). The Self-rating depression scale (SDS) and Self-Rating Anxiety Scale (SAS) were observed before and after treatment. The quality of life of patients was assessed using a short form 36 questionnaire (SF-36). A higher score indicates a better quality of life. All patients were followed up by telephone.
Table 2.
Paley scoring criteria.
| Grade | Expression |
|---|---|
| Ample | The fracture healed completely, and there was no recurrent infection. The local malformation was less than 7°, and the limb length difference was <2.5 cm |
| Good people | The fracture healed completely, and there was no recurrent infection. The local malformation was less than 7°, and the limb length difference was less than 2.5 cm, which was consistent with any 2 of the 3 items |
| Centre | The fracture healed completely, and there was no recurrent infection. The local malformation was less than 7°, and the limb length was less than 2.5 cm, which was consistent with any one of the 3 items |
| Difference | The fracture healed completely, and there was no recurrent infection. The local malformation was less than 7°, and the limb length was less than 2.5 cm, which did not satisfy any of them |
Secondary observations: Observe the pin infection during the patient’s treatment. Patients were divided into infected and non-infected groups according to pin infection during treatment. Patient clinical data were collected for univariate analysis including gender, age, BMI, hypertension, diabetes, COPD, smoking index, alcohol history, place of residence, cause of injury, Gustilo-Anderson classification, fracture type, fixation type, pin loosening, indwelling time. Multivariate logistic was used to analyze independent factors in patient with pin infection.
Statistical methods
This study used the SPSS 20.0 software package to perform statistical analysis on the collected data. This data was drawn using GraphPad Prism 7. The K-S is used to test the normal distribution of the data. Rate (%) was used to indicate the count data, with chi-square test, which is represented by χ2. Measurement data were expressed using mean ± standard deviation (means ±SD). The measurement data between the 2 groups that conformed to the normal distribution were analyzed by t test and expressed as t. Logistic multivariate was used to analyze the risk factors for postoperative pin infection in patients. When P<0.05, there was a statistical difference.
Results
Patient’s condition after treatment
We followed up 78 patients. The average follow-up time was 18.9 (12~36) months. The average defect length of the patient was 9.2cm (6~17 cm). The wound healing time was 35 days (22~78 days). The healing time of the new bone and bone segment was 7~18 months. The extension index averaged 40d/cm (25~60 d/cm).
Analysis of clinical efficacy and pin infection in patients
According to the Paley scoring criteria, the patient’s post-treatment efficacy was analyzed. The results showed that after combined treatment, 59 cases were excellent (75.64), 14 cases were good (17.95), and 5 cases were normal (6.41). The excellent and good rate was 93.59%. 78 patients who had been treated with post-intervention adjustments had recovered and recovered or returned to normal activities. When observing the occurrence of complications during the treatment of patients, 19 patients (24.36%) had pin infection.
Changes in SAS, SDS, and SF-36 before and after treatment
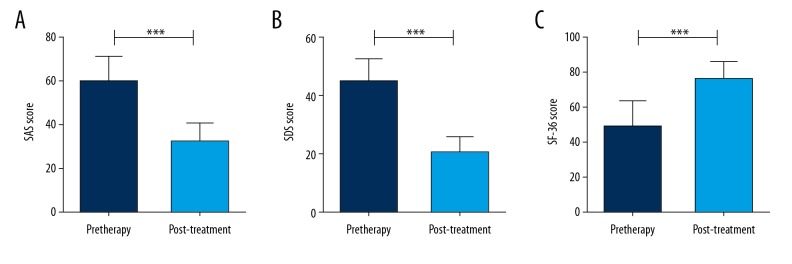
The SAS, SDS, and SF-36 scores of patients before treatment were first counted. The scores of patients before treatment were 59.62±11.65, 44.99±8.40, and 49.17±14.66, respectively. After the combination therapy, the SAS scores of the patients were significantly lower, and the SF-36 scores were significantly increased, which were 31.76±8.89, 20.86±5.08, and 75.60±10.57, respectively. It was found that there were significant differences in the scores after treatment (P<0.05) (Table 3, Figure 1).
Table 3.
Changes of SAS, SDS, SF-36 score before and after treatment.
| Grade | Pretherapy (n=78) | After treatment (nb78) | t value | P value |
|---|---|---|---|---|
| SAS score | 59.62±11.65 | 31.76±8.89 | 15.001 | <0.001 |
| SDS score | 44.99±8.40 | 20.86±5.08 | 20.937 | <0.001 |
| SF-36 score | 49.17±14.66 | 75.60±10.57 | −14.016 | <0.001 |
Figure 1.
Changes in scores of patients before and after treatment. (A) The SAS score of patients after treatment was significantly lower than that before treatment (P<0.05). (B) The SDS score of patients after treatment was significantly lower than that before treatment (P<0.05). (C) The SF-36 score of patients after treatment was significantly higher than that before treatment (P<0.05), *** indicated P<0.001.
Multi-factor analysis of pin infection
Patients were grouped according to the pin infection in the course of treatment. Patients with pin infection were divided into infected group (n=19), and patients without pin infection were divided into non-infected group (n=59). Univariate analysis showed that there were no significant differences in gender, BMI, hypertension, diabetes, COPD, smoking index, alcohol abuse history, place of residence, cause of injury, and Gustilo-Anderson classification between the 2 groups (P>0.05). There were significant differences in age, fracture type, fixation type, pin loosening, and indwelling time between the 2 groups (P<0.05) (Table 4).
Table 4.
Single factor analysis of needle infections [n (%)].
| Factor | n | Infection group (n=19) | Non-infection group (n=59) | t/χ2 value | P value |
|---|---|---|---|---|---|
| Sex | 2.227 | 0.136 | |||
| Male | 52 (66.67) | 10 (52.63) | 42 (71.19) | ||
| Female | 26 (33.33) | 9 (47.37) | 17 (28.81) | ||
| Age (years) | 12.370 | 3.517 | |||
| ≥50 | 24 (30.77) | 12 (63.16) | 12 (20.34) | ||
| <50 | 54 (69.23) | 7 (38.84) | 47 (79.66) | ||
| BMI (kg/m2) | 22.55±1.82 | 22.97±1.88 | 0.853 | 0.396 | |
| Anamnesis | |||||
| Hypertension | 30 (38.46) | 8 (42.11) | 24 (40.68) | 0.012 | 0.912 |
| Diabetes mellitus | 25 (32.05) | 7 (3.684) | 18 (30.51) | 0.264 | 0.607 |
| COPD | 8 (10.26) | 3 (15.79) | 5 (8.47) | 0.835 | 0.361 |
| Smoking index (branch) | 0.711 | 0.399 | |||
| ≥400 | 59 (75.64) | 13 (68.42) | 46 (77.97) | ||
| <400 | 19 (24.36) | 6 (31.58) | 13 (22.03) | ||
| History of alcoholism | 0.348 | 0.555 | |||
| Yes | 13 (16.67) | 4 (21.05) | 9 (15.25) | ||
| No | 65 (83.33) | 15 (78.95) | 50 (84.75) | ||
| Domicile | 0.835 | 0.361 | |||
| City | 70 (89.74) | 16 (84.21) | 54 (91.53) | ||
| Village | 8 (10.26) | 3 (15.79) | 5 (8.47) | ||
| Cause of injury in patients | 2.043 | 0.564 | |||
| Traffic accident | 54 (69.23) | 13 (68.42) | 41 (69.50) | ||
| High fall injury | 12 (15.38) | 3 (15.79) | 9 (15.25) | ||
| Crush injury | 8 (10.26) | 3 (15.79) | 5 (8.47) | ||
| Other | 4 (5.13) | 0 (0.00) | 4 (6.78) | ||
| Gustilo-Anderson typing | 0.078 | 0.780 | |||
| III type | 35 (44.87) | 8 (42.11) | 27 (45.76) | ||
| IV type | 43 (55.13) | 11 (57.89) | 32 (54.24) | ||
| Classification of fracture | 5.455 | 0.020 | |||
| Open tibial fracture | 48 (61.54) | 16 (84.21) | 32 (54.24) | ||
| Closed tibial fracture | 30 (38.46) | 3 (15.79) | 27 (45.76) | ||
| Fixed type | 3.903 | 0.048 | |||
| Plate internal fixation | 38 (48.72) | 13 (68.42) | 25 (42.37) | ||
| External fixator fixation | 40 (51.28) | 6 (31.59) | 34 (57.63) | ||
| Needle loosening | 9.526 | 0.002 | |||
| Yes | 30 (38.46) | 13 (68.42) | 17 (28.81) | ||
| No | 48 (61.58) | 6 (31.59) | 42 (71.19) | ||
| Retention time (d) | 36.93±17.47 | 22.04±12.05 | 4.172 | <0.001 | |
COPD – chronic obstructive pulmonary disease; BMI – body mass index.
Multivariate analysis of pin infection
We incorporate and assign indexes with differences (Table 5). Then we choose Forward: LR multivariate logistic analysis showed that age (OR: 13.863, 95% CI: 2.112~91.000), fracture type (OR: 30.602, 95% CI: 2.625~356.784), fixation type (OR: 8.358, 95% CI: 1.239~56.400), pin loosening (OR: 42.709, 95% CI: 4.379~416.574), indwelling time (OR: 1.068, 95% CI: 1.017~1.122) was independent risk factors for pin infection (Table 6).
Table 5.
Assignment tables.
| Factor | Assignment |
|---|---|
| Age | 1=≥50 year, 0=<50 year |
| Classification of fracture | 1=open tibial fracture, 0=closed tibial fracture |
| Fixed type | 1=plate internal fixation, 0=external fixator fixation |
| Needle loosening | 1=yes, 0=no |
| Retention time | Analysis of continuous variables using raw data |
| Needle infection(Y) | 1=infect, 0=non-infection |
Table 6.
Multi-factor logistic analysis.
| Factor | β | S.E. | Wals | Sig. | Exp (β) | EXP(β) 95% CI | |
|---|---|---|---|---|---|---|---|
| Lower limit | Superior limit | ||||||
| Age | 2.629 | 0.96 | 7.5 | 0.006 | 13.863 | 2.112 | 91.000 |
| Classification of fracture | 3.421 | 1.253 | 7.453 | 0.006 | 30.602 | 2.625 | 356.784 |
| Fixed type | 2.123 | 0.974 | 4.751 | 0.029 | 8.358 | 1.239 | 56.400 |
| Needle loosening | 3.754 | 1.162 | 10.438 | 0.001 | 42.709 | 4.379 | 416.574 |
| Retention time | 0.066 | 0.025 | 6.944 | 0.008 | 1.068 | 1.017 | 1.122 |
Discussion
The main cause of traumatic osteomyelitis is occult infection caused by traumatic trauma or improper treatment during acute infection treatment. And the disease mostly occurs in the tibia. Tibial traumatic osteomyelitis is difficult to treat and easy to recur in clinic. To a certain extent, this has increased the family financial burden and psychological pressure of patients [6]. At present, the main clinical treatment of osteomyelitis is through the thorough removal of inactivated bone and related soft tissue to improve the patient’s condition. However, debridement can cause bone defects in patients, especially the reconstruction of large bone defects, which is the most difficult problem at present.
Ilizarov technique is an important method in clinical orthopedics for the treatment of bone malformation, bone disconnection and tibial fracture. In particular, tibial traumatic osteomyelitis caused by bone resection has relatively ideal therapeutic effect [12]. Biofilm bacteria multiply on the dead bone and internal fixation surface of patients, leading to repeated inflammation and further extending the treatment time of patients. Vacuum sealing drainage is a technology introduced by Qiu et al. in 1994. It has played a significant role in improving various chronic wound diseases in recent years. Therefore, in this study, we explored the improvement of vacuum sealing drainage combined with Ilizarov bone transport technique in patients with tibial osteomyelitis, to provide references for clinicians.
In this study, 78 patients with tibial traumatic osteomyelitis were treated with vacuum sealing drainage combined with Ilizarov technique. The results showed that the average time of wound healing was 35 days, the average length of defect was 9.2 cm, the healing time of new bone and bone segment was 7–18 months, and the prolongation index was 40 d/cm. This is basically the same as that of Jiang et al. [13,14]. We then evaluated the efficacy of all patients in accordance with the Paley fracture evaluation criteria. Paley fracture evaluation standard is an important clinical standard to evaluate the clinical efficacy of tibial osteomyelitis after treatment, and its effect has been confirmed in several clinical trials [15,16].
We evaluated the patients in this study group and found that 59 cases were excellent, 14 cases were good and 5 cases were normal, and the excellent and good rate was 93.59%. In the study of Jian et al. [7], 15 patients with tibial traumatic osteomyelitis were treated with Ilizarov technique. According to the evaluation criteria of Paley fracture, 12 cases were excellent, 1 case was good, 1 case was normal, and 1 case was poor. The excellent and good rate was 87.3%. The excellent rate of treatment by combination therapy is significantly higher than its research. This shows that the combination of Illirov technique with negative pressure drainage can significantly improve the patient’s condition. The main reason is that the Ilizarov technology is strongly stable through three-dimensional fixation. In addition, 1.5–2.0mm Kirschner wire has good elasticity, which can increase the strength of fixation, provide excellent axial stress stimulation to patients’ limbs, accelerate the formation of new blood vessels at the fracture end of patients, and promote fracture healing [17,18]. Compared with traditional closed lavage drainage, vacuum sealing drainage has good airtightness and is characterized by sufficient, thorough and efficient drainage. It prevents the drainage fluid from communicating with the outside world to prevent poor infection, thus reducing the chance of infection [18,19]. And we analyzed the SAS, SDS, and SF-36 scores before and after treatment. It was found that the patients’ scores were significantly improved after treatment, which improved the quality of life of patients and prevented patients from adverse emotions from affecting patients’ treatment effects.
At the end of the study, we analyzed the risk factors of patients with pin infection. Compared with the advantages of Ilizarov technology, the shortcomings are obvious. The most common complication is pin infection [20]. patients with pin infection are grouped for risk factor analysis. Univariate analysis showed that there were statistical differences in age, fracture type, fixation type, pin loosening, and indwelling time between the 2 groups. Multivariate analysis found that age, fracture type, fixation type, pin loosening, and indwelling time were independent risk factors for pin infection in patients. This increases the likelihood of infection, but can be completely cured with prompt antimicrobial therapy. Compared with closed fracture patients, patients with open fractures are subject to high mechanical damage. As a result, the local skin resistance of patients with needle passage is low, which easily leads to the breeding of bacteria. This suggested that we need to closely observe the skin around the needle during the nursing process to prevent the occurrence of oozing and seepage in the skin around the needle. In contrast to the internal fixation, the external fixation pin is usually only subjected to traction in one direction. This increases the possibility of slipping or loosening of the pin track. Therefore, it is necessary to pay close attention to the situation of needle passage in the nursing process to avoid loosening and slippage. Since the steel needle is in contact with the skin for a long time during the treatment of the patient, a new wound may be caused when the skin around the bone puncture needle is excessively pulled. Combined with the growth of secretions around the needle tract, repeated infections may occur. Therefore, timely nursing after clinical treatment is particularly important.
However, there are still some limitations in this time. First of all, our study was not included in the corresponding control group. The difference between the traditional treatment regimen and the Ilizarov technique combined with vacuum sealing drainage was not compared. Secondly, during the multivariate analysis, the confidence intervals of the fracture type and pin loosening were wider, which may be due to the small number of samples. Finally, we did not have long-term follow-up of patients, and the long-term efficacy of patients after treatment is still unclear. Therefore, in future research, we hope to increase the corresponding group, expand the number of samples with multi-centers, and conduct long-term follow-up to verify the correctness of the results.
Conclusions
Age, fracture type, fixation type, pin loosening, and indwelling time are independent risk factors for pin infection in patients with tibial traumatic osteomyelitis. Combination of vacuum sealing drainage with Ilizarov bone transport technique can effectively improve the condition of tibial traumatic osteomyelitis, improve the quality of life of patients, and reduce the occurrence of adverse emotions of patients, which is expected to be popularized in clinical.
Footnotes
Source of support: Departmental sources
Conflict of interests
None.
References
- 1.Winkler D, Goudie ST, Court-Brown CM. The changing epidemiology of open fractures in vehicle occupants, pedestrians, motorcyclists and cyclists. Injury. 2018;49:208–12. doi: 10.1016/j.injury.2017.11.009. [DOI] [PubMed] [Google Scholar]
- 2.Hake ME, Oh JK, Kim JW, et al. Difficulties and challenges to diagnose and treat post-traumatic long bone osteomyelitis. Eur J Orthop Surg Traumatol. 2015;25:1–3. doi: 10.1007/s00590-014-1576-z. [DOI] [PubMed] [Google Scholar]
- 3.Govaert GA, IJpma FF, McNally M, et al. Accuracy of diagnostic imaging modalities for peripheral post-traumatic osteomyelitis – a systematic review of the recent literature. Eur J Nucl Med Mol Imaging. 2017;44:1393–407. doi: 10.1007/s00259-017-3683-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yilihamu Y, Keremu A, Abulaiti A, et al. Outcomes of post-traumatic tibial osteomyelitis treated with an Orthofix LRS versus an Ilizarov external fixator. Injury. 2017;48:1636–43. doi: 10.1016/j.injury.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 5.Letchmanan K, Shen SC, Ng WK, et al. Mechanical properties and antibiotic release characteristics of poly(methyl methacrylate)-based bone cement formulated with mesoporous silica nanoparticles. J Mech Behav Biomed Mater. 2017;72:163–70. doi: 10.1016/j.jmbbm.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 6.Wang X, Luo F, Huang K, Xie Z. Induced membrane technique for the treatment of bone defects due to post-traumatic osteomyelitis. Bone Joint Res. 2016;5:101–5. doi: 10.1302/2046-3758.53.2000487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abulaiti A, Yilihamu Y, Yasheng T, et al. The psychological impact of external fixation using the Ilizarov or Orthofix LRS method to treat tibial osteomyelitis with a bone defect. Injury. 2017;48:2842–46. doi: 10.1016/j.injury.2017.10.036. [DOI] [PubMed] [Google Scholar]
- 8.Skrinjar E, Duschek N, Bayer GS, et al. Randomized controlled trial comparing the combination of a polymeric membrane dressing plus negative pressure wound therapy against negative pressure wound therapy alone: The WICVAC study. Wound Repair Regen. 2016;24:928–35. doi: 10.1111/wrr.12457. [DOI] [PubMed] [Google Scholar]
- 9.Onyekwelu I, Hasan S, Chapman CB. Ilizarov external fixator for length salvage in infected amputated nonunions. Bull Hosp Jt Dis (2013) 2014;72:176–80. [PubMed] [Google Scholar]
- 10.Radunovic A, Kosutic M, Vulovic M, et al. Ilizarov method as limb salvage in treatment of massive femoral defect after unsuccessful tumor arthroplasty. Vojnosanit Pregl. 2016;73:779–82. doi: 10.2298/VSP150419039R. [DOI] [PubMed] [Google Scholar]
- 11.Paley D, Maar DC. Ilizarov bone transport treatment for tibial defects. J Orthop Trauma. 2000;14:76–85. doi: 10.1097/00005131-200002000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Bibbo C. Reverse sural flap with bifocal Ilizarov technique for tibial osteomyelitis with bone and soft tissue defects. J Foot Ankle Surg. 2014;53:344–49. doi: 10.1053/j.jfas.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 13.Xiao K, Li T, Jiang Y, et al. Ilizarov technique in an adolescent patient with progressive pseudorheumatoid dysplasia: A case report. Medicine (Baltimore) 2018;97:e11375. doi: 10.1097/MD.0000000000011375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tetsworth K, Paley D, Sen C, et al. Bone transport versus acute shortening for the management of infected tibial non-unions with bone defects. Injury. 2017;48:2276–84. doi: 10.1016/j.injury.2017.07.018. [DOI] [PubMed] [Google Scholar]
- 15.Kadhim M, Holmes L, Jr, Gesheff MG, Conway JD. Treatment options for nonunion with segmental bone defects: Systematic review and quantitative evidence synthesis. J Orthop Trauma. 2017;31:111–19. doi: 10.1097/BOT.0000000000000700. [DOI] [PubMed] [Google Scholar]
- 16.Herring MJ, Rud CT, Macalena JA. Autologous chondrocyte implantation using a bilayer collagen membrane with bone graft and anteromedialization of the tibial tubercle for the treatment of a large osteochondral defect in the lateral knee trochlea: A case report. JBJS Case Connect. 2016;6:e35. doi: 10.2106/JBJS.CC.14.00154. [DOI] [PubMed] [Google Scholar]
- 17.Eralp L, Kocaoglu M, Celiktas M, Gulsen M. Is acute compression and distraction superior to segmental bone transport techniques in chronic tibial osteomyelitis? Comparison of distraction osteogenesis techniques. Acta Orthop Belg. 2016;82:599–609. [PubMed] [Google Scholar]
- 18.Chen X, Liu L, Nie W, et al. Vacuum sealing drainage therapy for refractory infectious wound on 16 renal transplant recipients. Transplant Proc. 2018;50:2479–84. doi: 10.1016/j.transproceed.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 19.Yang SC, Chen WJ, Chen HS, et al. Extended indications of percutaneous endoscopic lavage and drainage for the treatment of lumbar infectious spondylitis. Eur Spine J. 2014;23:846–53. doi: 10.1007/s00586-013-3157-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kao HK, Chen MC, Lee WC, et al. Seasonal temperature and pin site care regimen affect the incidence of pin site infection in pediatric supracondylar humeral fractures. Biomed Res Int. 2015;2015 doi: 10.1155/2015/838913. 838913. [DOI] [PMC free article] [PubMed] [Google Scholar]