Abstract
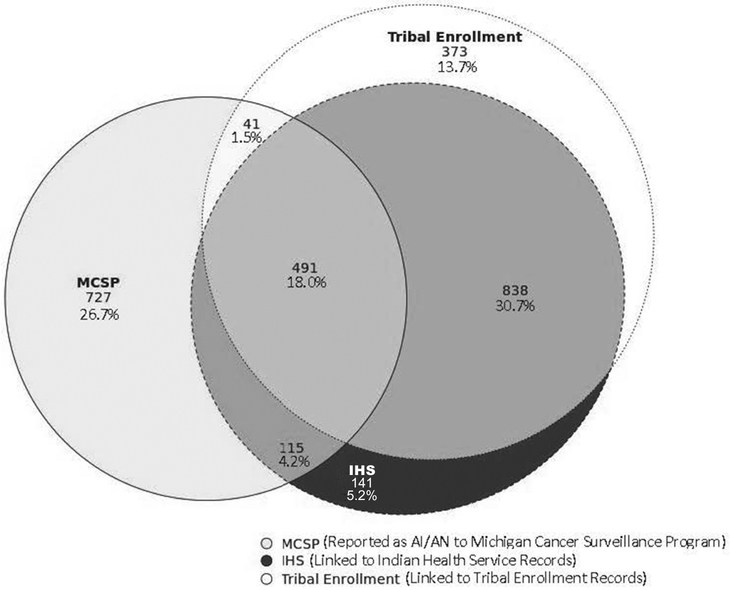
This study examines the extent to which data linkages between Indian Health Service, tribal data, and cancer registries affect cancer incidence rates among American Indians/Alaska Natives (AI/ANs) in Michigan. The incidence of tobacco- and alcohol-associated cancers for 1995–2012 was analyzed to compare rates of the Upper Peninsula (UP) and Lower Peninsula (LP) in Michigan and among AI/ANs and non-Hispanic Whites (NHWs). Complete linkage resulted in 1,352 additional AI/AN cases; 141 cases were linked via IHS records alone, while 373 were linked via tribal records alone; 838 were linked through both IHS and tribal records. Age-adjusted incidence rates for AI/ANs increased from 214.39 per 100,000 to 405.41 per 100,000, similar to that of NHWs after complete linkage (421.46 per 100,000). In the UP, AI/ANs had age-adjusted incidence rates 1.67 times higher than NHWs (596.69 per 100,000 vs. 356.32 per 100,000 respectively). This study indicates a substantial number of AI/AN cancer cases remain misclassified in Michigan.
Keywords: Data linkage, data quality, cancer incidence, American Indian, epidemiology, Michigan
Michigan is home to over 130,000 American Indians/Alaska Natives (AI/ANs), and the AI/AN population accounts for approximately 0.7% of Michigan’s total population.1 There are 12 federally recognized tribes in Michigan whose regions and territories branch throughout the state.2,3 According to the Inter-Tribal Council of Michigan, AI/ANs in Michigan suffer from disproportionately high rates of morbidity and mortality.2
Michigan belongs to the Northern Plains Indian Health Service (IHS) region, where higher rates of smoking and heavy drinking have been reported among AI/ANs compared with non-Hispanic Whites (NHWs).4 These prevalence estimates vary widely among geographically and culturally unique tribes.5 For example, current smoking prevalence among AI/ANs in Michigan ranges from 32% to 72%6 and heavy drinking prevalence has been found to be higher in the Upper Peninsula (UP) compared to the Lower Peninsula (LP).7 Furthermore, the Northern Plains region has substantial cancer disparities disfavoring AI/ANs.8-10 Cancer is the second leading cause of death among AI/AN males and the leading cause of death for AI/AN females in the Northern Plains.11
Racial/ethnic minorities are often undercounted in cancer registries due to racial misclassification from incorrect or missing demographic information in medical forms,8 resulting in underestimation of cancer rates. American Indians/Alaska Natives are more likely than members of other racial groups to be misclassified for race in cancer registries.12-18 Restricting AI/AN data to IHS Contract Health Service Delivery Area (CHSDA) counties has been identified as one way to address racial misclassification;19 however, nearly half of Michigan counties are non-CHSDA.20
Another option to examine cancer incidence more accurately in AI/AN populations is the linkage of records from cancer registries with records from IHS. This process aims to identify cancer patients directly within the IHS patient registration file in order to determine AI/AN race more accurately. The linkage is able to dramatically decrease misclassification of AI/ANs in cancer data but only captures AI/ANs who have accessed IHS services.10
The linkage between the Michigan Cancer Surveillance Program (MCSP) and IHS is conducted on an annual basis to address misclassification of AI/AN cancer cases. The MSCP has also been periodically linked with the tribal records from six of the 12 Michigan tribes to capture cases that may not have ever used IHS services.
The purpose of this study was to examine the extent to which data linkages affect cancer incidence rates among AI/ANs in Michigan, to compare these rates with those of NHWs, and to compare cancer rates between Michigan’s UP and LP. Analysis was limited to cancers associated with tobacco or alcohol21-24 due to the high prevalence of commercial tobacco and alcohol use among AI/ANs.6,7 Differences in cancer rates were expected between the UP and LP because of variations in tribal participation and cultural and lifestyle factors between tribes.
Methods
Classification of race.
Cancer cases were classified as AI/AN if they were identified as such in the medical record (the MCSP permits the reporting of up to five race fields in order to accurately represent people of multiple races), if they linked to IHS, or if they linked to tribal enrollment records. Tribal linkages using tribal enrollment records are carried out intermittently at the convenience and with the permission and cooperation of individual tribes.20 The data used in this analysis included the linkage results involving six of Michigan’s 12 recognized tribes that represent an estimated 85% of all registered tribal members in Michigan.
The tribal linkages are conducted with tribal members and MCSP staff present at all times. The state cancer data were brought to the working meeting by MCSP staff stored as an encrypted, compressed, and password-protected file on an external hard drive. The data linkages were conducted using Link Plus 2.0.25 Detailed description of the data sources and methods used for the IHS linkage are provided in previous publications.8,26
Upon completion of the linkage, two files were created. The first file contained de-identified data for all cancer cases that linked to the tribal records. This analytical file included specific cancer registry variables as previously determined to be necessary for analysis by the tribe, and was delivered to a representative from the tribe. The second file contained the cancer registry patient ID number for each case that linked to the tribe. This file was used to update the AI/AN status for the linked patients within the MCSP to improve the statewide AI/AN data. Note that no tribe-specific data were used in this analysis.
The output file of all true matches was merged with all linkage results maintained by MCSP and was used to build a de-identified dataset with predetermined variables and containing fields to identify AI/AN race: cancer cases that had been originally identified as AI/AN, those who had been linked with IHS, and those who had been linked to a Michigan tribe.
Cancer cases.
We analyzed tobacco- and alcohol-associated tumors for adults (18 years and older) diagnosed between 1995 and 2012 from the MCSP. We used registry classified tumor histology, tumor behavior, and primary cancer site according to the International Classification of Diseases for Oncology (ICD-O-3) edition in use at the time of diagnosis, converted to the 3rd edition coding.27 Incidence rates were calculated for cancers associated with alcohol (oral cavity and pharynx; esophagus; colon and rectum; liver; larynx; and female breast) and tobacco (oral cavity and pharynx; esophagus; stomach; colon and rectum; liver; pancreas; larynx; lung, bronchus, and trachea; cervix; kidney and renal pelvis; urinary bladder; and acute myeloid leukemia).21-24 The county of residence at the time of diagnosis was used to determine each case’s region as either UP or LP. The variables used for analysis included race (as reported in the medical record), an IHS link variable, a tribal link variable, sex, age at diagnosis, county of residence, year of diagnosis, primary cancer site, tumor behavior, histology, and SEER summary stage.
Population estimates.
All population estimates were retrieved from the Centers for Disease Control and Prevention WONDER bridged-race population estimates website.28
Statistical methods.
All rates, expressed per 100,000 population, were directly age adjusted to the 2000 United States standard population (19 age groups—Census P25-1130). Readers should avoid comparison of these data with published cancer rates that were adjusted using a different standard population.
Age-adjusted incidence rates were used to compare AI/AN cancer rates with NHW rates and to compare rates between the UP and LP in Michigan. Confidence intervals and rate ratios (RR) were also calculated, methods described by Tiwari et al.29 Calculations were performed using SAS 9.430 and Microsoft Excel 2013. Figure 1 was created using a shiny app based on an R package.31
Figure 1.
Number and percentage of American Indian/Alaska Native tobacco- and alcohol-associated cancer cases (N = 2,726) by linkage status: Michigan, 1995–2012.
Results
Cancer counts.
A total number of 496,418 cancer cases were included in this study (Table 1). After all subsequent linkages, 99.45% of cases were identified as NHW and 0.55% were AI/AN (493,692 and 2,726 respectively). A larger proportion of AI/AN cases than of NHW cases were located in the Upper Peninsula (28.43% vs. 3.80%, respectively). Nearly half (49.60%) of AI/AN cases were misclassified as NHW within MCSP. The MCSP identified 1,374 cases as AI/AN through normal case ascertainment. The linkage with IHS detected an additional 979 AI/AN cases that were misclassified by MCSP. The tribal record linkages detected an additional 373 AI/AN cases that were misclassified by MCSP or not detected through the IHS linkage (Figure 1). Females had lower percentages of case detection within MCSP than males (45.65% vs. 58.28%) (data not shown).
Table 1.
NUMBER AND PERCENTAGE OF TOBACCO- AND ALCOHOL-ASSOCIATED CANCERS AMONG NON-HISPANIC WHITES AND AMERICAN INDIANS/ALASKA NATIVES: MICHIGAN, 1995–2012
| Total (N = 496,418) |
NHW (n = 493,692, 99.45%) |
AI/AN Complete Link (n =2726, .55%) |
||||
|---|---|---|---|---|---|---|
| Number | % | Number | % | Number | % | |
| Upper Peninsula | 19,071 | 3.84 | 18,296 | 3.70 | 775 | 28.43 |
| Lower Peninsula | 477,347 | 96.16 | 475,396 | 96.30 | 1,951 | 71.57 |
Notes:
NHW = Non-Hispanic White
AI/AN = American Indian/Alaska Native
Age-adjusted rates.
Prior to any linkages, AI/ANs had significantly lower age-adjusted rates for tobacco- and alcohol-associated cancers compared with NHWs (214.39 per 100,000 and 422.65 per 100,000 respectively; RR = 0.51) (Table 2). However, the complete data linkage increased the age-adjusted rate among AI/ANs, making it statistically equivalent to that of NHWs (405.41 per 100,000 and 421.46 per 100,000 respectively; RR = 0.96).
Table 2.
AGE-ADJUSTED INCIDENCE RATES (PER 100,000) AND NUMBER OF CASES OF TOBACCO- AND ALCOHOL-ASSOCIATED CANCERS AMONG AMERICAN INDIANS/ALASKA NATIVES BY LINKAGE STATUS IN THE UPPER AND LOWER PENINSULAS COMPARED WITH NON-HISPANIC WHITES: MICHIGAN, 1995–2012
| NHW |
AI/AN |
AI/AN:NHW |
||||
|---|---|---|---|---|---|---|
| Count | Rate | Count | Rate | Rate Ratio | 95% CI | |
| Michigan Cancer Surveillance Program Only | ||||||
| Upper Peninsula | 18,756 | 366.18 | 315 | 242.16 | .66 | .50-.81 |
| Lower Peninsula | 476,288 | 425.08 | 1,059 | 208.35 | .49 | .42-.56 |
| Total | 495,044 | 422.65 | 1,374 | 214.39 | .51 | .44-.57 |
| Michigan Cancer Surveillance Program + IHS | ||||||
| Upper Peninsula | 18,329 | 357.00 | 742 | 570.47 | 1.60 | 1.36-1.82 |
| Lower Peninsula | 475,736 | 424.57 | 1,611 | 298.64 | .70 | .62-.78 |
| Total | 494,065 | 421.79 | 2,353 | 351.53 | .83 | .75-.91 |
| Michigan Cancer Surveillance Program + IHS + Tribal | ||||||
| Upper Peninsula | 18,296 | 356.32 | 775 | 596.69 | 1.67 | 1.43-1.90 |
| Lower Peninsula | 475,396 | 424.25 | 1,951 | 359.07 | .85 | .76-.93 |
| Total | 493,692 | 421.46 | 2,726 | 405.41 | .96 | .88-1.05 |
Notes:
NHW = Non-Hispanic White
AI/AN = American Indian/Alaska Native
CI = Confidence interval
HIS = Indian Health Service
Following all linkages, AI/ANs in the UP had tobacco- and alcohol-associated cancer age-adjusted rates 1.67 times higher than NHWs (596.69 per 100,000 vs. 356.32 per 100,000 respectively; Table 2). However, in the LP, AI/ANs had lower rates than NHWs (359.07 per 100,000 vs. 424.25 per 100,000 respectively, RR = 0.85). A comparison of AI/AN rates between the UP and LP revealed that AI/ANs in the UP had tobacco- and alcohol-associated age-adjusted rates 1.66 times higher than AI/ANs in the LP (596.69 per 100,000 vs. 359.07 per 100,000 respectively; 95% CI = 1.54–1.76; data not shown). However, the opposite was seen among NHWs (356.32 per 100,000 in the UP vs. 424.25 per 100,000 in the LP, RR = 0.84)
Discussion
The number of AI/AN cancer cases and rates increased drastically due to IHS and tribal linkages. These findings highlight the importance of data linkages to improving the quality of AI/AN cancer data. In routine MCSP data, AI/AN individuals were largely misclassified (at least 49.60% were incorrectly identified as non-AI/AN) resulting in problematic underestimation of the AI/AN cancer burden in Michigan. Age-adjusted incidence rates for all sites (tobacco- and alcohol-associated cancers) among AI/ANs were 1.89 times higher following linkage.
With each additional tribal linkage, the numbers of AI/AN cases increased and the quality of data improved. A majority of the cases (838, 30.7%) matched from the Michigan tribal rosters were also matched in IHS records. However, many AI/AN cases misclassified in MCSP were detected solely from the Michigan tribal rosters (373, 13.7%). This emphasizes the importance of performing tribal linkages to supplement the IHS linkage. Further action could be to continue engaging and collaborating with tribes who do not currently participate in linkages, and also to perform linkages routinely with the tribes who have participated in the past.
There are differences when comparing AI/ANs and NHWs between the UP and LP. In the UP, AI/ANs had higher incidence rates that NHW (RR=1.67). In the UP, AI/ANs also had much higher incidence rates than AI/ANs in the LP (RR = 1.66; 95% CI = 1.54–1.76; data not shown). The lower rates for the LP may be associated with variations in risk factor exposures. Tribes vary widely in culture and lifestyle. This is particularly so in the large differences of commercial tobacco and alcohol use among tribes.6,7 Smoking prevalence ranges from 43%–72% among AI/ANs in Michigan,6 and higher prevalence of heavy and binge drinking have been reported in the UP.7 However, it is difficult to infer that this is a true difference in incidence rates as it may simply be caused by variations in tribal participation among AI/ANs in the UP and LP.
The steep differential between the LP and UP is also likely associated with proportionately lower tribal membership and IHS participation by AI/AN in the LP, strictly limiting the ability to correct for racial misclassification through linkages. In addition, tribal participation in the linkage effort is lower in the LP. This suggests that AI/AN cancer incidence rates need to be interpreted cautiously, even following linkages, in order to improve the quality of the data.
While this paper focuses on regional differences of AI/AN misclassification within the MCSP, it is important to note that sex differences in linkage status were also observed in this dataset. Females had lower percentages of case detection within the MCSP compared with males (45.65% vs. 58.28% respectively; data not shown), and therefore age-adjusted incidence rates for females saw a larger increase following complete linkage compared with males (RR = 2.11 vs. 1.64 respectively, data not shown). While it is unclear if this is due to the types of cancers included in this study, or from sample size limitations, previous research has yielded similar results.32 Future research should examine sex differences in AI/AN misclassification and how these sex differences may affect the accuracy of cancer data.
Although a data linkage was performed before this analysis, the AI/AN cancer burden may still be underestimated. While the IHS linkage is performed annually, not all AI/ANs use IHS services and those who do not would not be included in the IHS linkages. This is especially true of AI/ANs living in urban settings. Nationwide, only about 58% of AI/ANs use IHS services.33 The linkage with tribal data helps to address race misclassification in the 42% of the AI/AN population that has not used IHS. Tribal linkage is a unique form of data linkage in that it can only be performed with the authorization and collaboration of the tribe. To date, six of the 12 Michigan tribes have participated in a data linkage at least once.
Limitations.
Our interpretation of these results was subject to the following limitations. The method of linking records to further reduce AI/AN misclassification was based on tribal linkages only for those tribes that participated, and thus, did not address misclassification for Michigan tribes that did not participate in linking their tribal roster to the Michigan Department of Health and Human Services cancer registry. Furthermore, participation of individual tribes varied between the UP and LP, potentially biasing observed differences in incidence rates between these two geographic areas. Furthermore, note that roughly half of the cases originally reported as AI/AN to the MCSP were not detected in either the IHS or tribal links. This is likely due, primarily, to the Michigan AI/AN population not enrolled in any tribe. To a lesser degree this is connected to uncorrected misclassification of tribal members from tribes yet to participate in the linkage. The clear evidence of misclassification error in LP rates simply restates the continuing need to find ways to attribute AI/AN status accurately and to the need to interpret cancer incidence rates for the AI/AN population with considerable caution. Finally, the bridged intercensal population estimates significantly overestimated AI/AN individuals of Hispanic ethnicity.11 It is possible that by not restricting our analyses to non-Hispanic AI/AN our results may be underestimates of the true burden of cancer incidence in the Michigan AI/AN population.
Conclusions.
Cancer research among AI/AN populations is limited by small population sizes relative to other racial groups. Furthermore, racial misclassification of this group underestimates the cancer burden, resulting in misrepresentation of cancer incidence among AI/ANs. This study emphasizes the importance of supplementing routine IHS data linkages with tribal rosters. The results of this study also further our knowledge of cancer disparities among AI/ANs in Michigan. This information has allowed Michigan tribal leaders to formulate prevention and treatment strategies tailored specifically to their AI/AN community, which would lower the cancer burden of tribal members. Our findings reveal the importance of data linkages in order to improve cancer data among AI/AN populations, through IHS linkages and linkages with tribal records.
Acknowledgments
Tess Weber was funded in part by the Cancer Epidemiology Education in Special Populations (CEESP) Program, Grant R25 CA112383. The work of the Inter-Tribal Council of Michigan to accomplish the Linkage of the Michigan registry to Tribal rosters is supported by Cooperative Agreement Number 5, U58 DP003921, funded by the CDC.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Contributor Information
Tess L. Weber, Population Health, Sanford Research, Sioux Falls, South Dakota and the Department of Epidemiology, University of Nebraska Medical Center College of Public Health, Omaha, Nebraska..
Glenn Copeland, Michigan Cancer Surveillance System, Michigan Department of Health and Human Services, Lansing, Michigan..
Noel Pingatore, Health Education and Chronic Disease, Inter- Tribal Council of Michigan, Sault Ste. Marie, Michigan..
Kendra K. Schmid, Department of Biostatistics, University of Nebraska Medical Center College of Public Health, Omaha, Nebraska..
Melissa A. Jim, Division of Cancer Prevention and Control, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Albuquerque, New Mexico..
Shinobu Watanabe-Galloway, Department of Epidemiology, University of Nebraska Medical Center College of Public Health, Omaha, Nebraska..
References
- 1.Norris T, Vines PL, Hoeffel EM. The American Indian and Alaska Native population: 2010. Washingon, DC: United States Census Bureau, 2012. Available at: https://www.census.gov/library/publications/2012/dec/c2010br-10.html. [Google Scholar]
- 2.Inter-Tribal Council of Michigan. Member tribes. Sault Sainte Marie, MI: Inter-Tribal Council of Michigan, 2012. Available at: http://www.itcmi.org/blog/category/member-tribes. [Google Scholar]
- 3.Michigan Department of Health and Human Services. Federally recognized tribes in Michigan. Lansing, MI: Michigan Department of Health and Human Services, 2019. Available at: http://www.michigan.gov/mdhhs/0,5885,7-339-73971_7209-216627—,00.html. [Google Scholar]
- 4.Cobb N, Espey D, King J. Health behaviors and risk factors among American Indians and Alaska Natives, 2000–2010. Am J Public Health. 2014. June;104 Suppl 3:S481–9. Epub 2014 Apr 22. 10.2105/AJPH.2014.301879, PMid:24754662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnes PM, Adams PF, Powell-Griner E. Health characteristics of the American Indian or Alaska Native adult population: United States, 2004–2008. Natl Health Stat Report. 2010. March 9;(20):1–22. 10.1037/e407192008-001 [DOI] [PubMed] [Google Scholar]
- 6.Ramsey F, Ussery-Hall A, Garcia D, et al. Prevalence of selected risk behaviors and chronic diseases—Behavioral Risk Factor Surveillance System (BRFSS), 39 steps communities, United States, 2005. MMWR Surveill Summ. 2008. October 31;57(11):1–20. PMid:18971922 [PubMed] [Google Scholar]
- 7.Western Upper Peninsula Health Department (WUPHD). U.P. community health needs assessment—2018 (2nd ed.). Hancock, MI: WUPHD, 2018. Available at http://wuphd.org/upchna/. [Google Scholar]
- 8.Espey DK, Wu XC, Swan J, et al. Annual report to the nation on the status of cancer, 1975–2004, featuring cancer in American Indians and Alaska Natives. Cancer. 2007. November 15;110(10):2119–52. 10.1002/cncr.23044 PMid:17939129 [DOI] [PubMed] [Google Scholar]
- 9.Wiggins CL, Espey DK, Wingo PA, et al. Cancer among American Indians and Alaska Natives in the United States, 1999–2004. Cancer. 2008. September 1;113(5 Suppl):1142–52. 10.1002/cncr.23734 PMid:18720375 [DOI] [PubMed] [Google Scholar]
- 10.White MC, Espey DK, Swan J, et al. Disparities in cancer mortality and incidence among American Indians and Alaska Natives in the United States. Am J Public Health. 2014. June;104 Suppl 3:S377–87. Epub 2014 Apr 22. 10.2105/AJPH.2013.301673 PMid:24754660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Espey DK, Jim MA, Cobb N, et al. Leading causes of death and all-cause mortality in American Indians and Alaska Natives. Am J Public Health. 2014. June;104 Suppl 3:S303–11. Epub 2014 Apr 22. 10.2105/AJPH.2013.301798 PMid:24754554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roen EL, Copeland GE, Pinagtore NL, et al. Disparities of cancer incidence in Michigan’s American Indians: spotlight on breast cancer. Cancer. 2014. June 15;120(12):1847–53. Epub 2014 Mar 26. 10.1002/cncr.28589 PMid:24676851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mettlin CJ, Menck HR, Winchester DP, et al. A comparison of breast, colorectal, lung, and prostate cancers reported to the National Cancer Data Base and the Surveillance, Epidemiology, and End Results Program. Cancer. 1997. May 15;79(10):2052–61. [DOI] [PubMed] [Google Scholar]
- 14.Frost F, Taylor V, Fries E. Racial misclassification of Native Americans in a surveillance, epidemiology, and end results cancer registry. J Natl Cancer Inst. 1992. June 17;84(12): 957–62. 10.1093/jnci/84.12.957 PMid:1629916 [DOI] [PubMed] [Google Scholar]
- 15.Partin MR, Rith-Najarian SJ, Slater JS, et al. Improving cancer incidence estimates for American Indians in Minnesota. Am J Public Health. 1999. November;89(11):1673–7. 10.2105/AJPH.89.11.1673 PMid:10553387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Swan J, Edwards BK. Cancer rates among American Indians and Alaska Natives: is there a national perspective. Cancer. 2003. September 15;98(6):1262–72. 10.1002/cncr.11633 PMid:12973851 [DOI] [PubMed] [Google Scholar]
- 17.Ioannou GN, Chapko MK, Dominitz JA. Predictors of colorectal cancer screening participation in the United States. Am J Gastroenterol. 2003. September;98(9):2082–91. PMid:14499792 [DOI] [PubMed] [Google Scholar]
- 18.Kwong S, Perkins C, Snipes K, et al. Improving American Indian cancer data in the California Central Registry by linkage with the Indian Health Service. J Registry Manage. 1998;25:17–20. [Google Scholar]
- 19.Jim MA, Arias E, Seneca DS, et al. Racial misclassification of American Indians and Alaska Natives by Indian Health Service Contract Health Service Delivery Area. Am J Public Health. 2014. June;104 Suppl 3:S295–302. Epub 2014 Apr 22. 10.2105/AJPH.2014.301933 PMid:24754617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johnson JC, Soliman AS, Tadgerson D, et al. Tribal linkage and race data quality for American Indians in a state cancer registry. Am J Prev Med. 2009. June;36(6):549–54. Epub 2009 Apr 8. 10.1016/j.amepre.2009.01.035 PMid:19356888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.International Agency for Research on Cancer (IARC). IARC monographs on the evaluation of carcinogenic risks to humans: Volume 96: Alcohol consumption and ethyl carbamate. Lyon, France: IARC, 2010. Available at: http://monographs.iarc.fr/ENG/Monographs/vol96/index.php. [PMC free article] [PubMed] [Google Scholar]
- 22.International Agency for Research on Cancer. Consumption of alcoholic beverages. Lyon, France: IARC, 2018. Available at: http://monographs.iarc.fr/ENG/Monographs/vol100E/mono100E-11.pdf. [Google Scholar]
- 23.National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. The health consequences of smoking—50 years of progress: a report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention, 2014. [Google Scholar]
- 24.Henley SJ, Singh SD, King J, et al. Invasive cancer incidence and survival—United States, 2013. MMWR Morb Mortal Wkly Rep. 2017. January 27;66(3):69–75. 10.15585/mmwr.mm6603a1 PMid:28125576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Division of Cancer Prevention and Control. Registry Plus: a suite of publicly available software programs for collecting and processing cancer registry data. Atlanta, GA: Centers for Disease Control and Prevention, 2015. Available at: https://www.cdc.gov/cancer/npcr/index.htm. [Google Scholar]
- 26.Espey DK, Wiggins CL, Jim MA, et al. Methods for improving cancer surveillance data in American Indian and Alaska Native populations. Cancer. 2008. September 1;113(5 Suppl):1120–30. 10.1002/cncr.23724 PMid:18720372 [DOI] [PubMed] [Google Scholar]
- 27.Fritz A, Percy C, Jack A, et al. eds. International classification of diseases for oncology. Geneva, Switzerland: World Health Organization, 2013. [Google Scholar]
- 28.Centers for Disease Control and Prevention (CDC). Bridged-Race Population Estimates, United States July 1st resident population by state, county, age, sex, bridged-race, and Hispanic origin. Atlanta, GA: CDC, 2016. Available at: http://wonder.cdc.gov/bridged-race-v2015.html. [Google Scholar]
- 29.Tiwari RC, Li Y, Zou Z. Interval estimation for ratios of correlated age-adjusted rates. J Data Sci. 2010. July;8:471–82. PMid:22347884 [PMC free article] [PubMed] [Google Scholar]
- 30.SAS software. Cary, NC: SAS Institute Inc., 2012:SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc. [Google Scholar]
- 31.Larsson J. Area-Proportional Euler and Venn Diagrams with Ellipses. R package version 4.1. 2018. Available at: https://cran.r-project.org/package=eulerr, 2018. [Google Scholar]
- 32.Arias E, Schauman WS, Eschbach K, et al. The validity of race and Hispanic origin reporting on death certificates in the United States. Vital Health Stat 2. 2008. October;(148): 1–23. PMid:19024798 [PubMed] [Google Scholar]
- 33.Burwell S MR, Frazier F, Greenway K. Trends in Indian Health 2014 Edition. Rockville, MD: Indian Health Service, 2015. Available at: https://www.ihs.gov/dps/includes/themes/responsive2017/display_objects/documents/Trends2014Book508.pdf. [Google Scholar]