Abstract
Context:
Prioritizing amongst potentially conflicting end-of-life values may help patients discriminate amongst treatments and allow clinicians to align treatments with values.
Objectives:
To investigate end-of-life values that patients prioritize when facing explicit trade-offs and identify predictors of patients whose values and treatment preferences seem inconsistent.
Methods:
Analysis of surveys from a multi-center cluster-randomized trial of patients with serious illness. Respondents prioritized end-of-life values and identified cardiopulmonary resuscitation (CPR) preferences in two health states.
Results:
Of 535 patients, 60% prioritized relief of discomfort over extending life, 17% prioritized extending life over relief of discomfort, and 23% were unsure. Patients prioritizing extending life were most likely to prefer CPR, with 93% preferring CPR in current health and 67% preferring CPR if dependent on others, compared to 69% and 21% respectively for patients prioritizing relief of discomfort, and 78% and 33% respectively for patients unsure of their prioritized value (p<0.001 for all comparisons). Among patients prioritizing relief of discomfort, preference for CPR in current health was less likely among older patients (OR 0.958 per year; 95%CI 0.935,0.981) and more likely with better self-perceived health (OR 1.402 per level of health; 95%CI 1.090,1.804).
Conclusion:
Clinicians face challenges as they clarify patient values and align treatments with values. Patients’ values predicted CPR preferences, but a substantial proportion of patients expressed CPR preferences that appeared potentially inconsistent with their primary value. Clinicians should question assumptions about relationships between values and CPR preferences. Further research is needed to identify ways to use values to guide treatment decisions.
Keywords: goals-of-care, palliative care, end-of-life, values, preferences, advance care planning (ACP), cardiopulmonary resuscitation (CPR)
INTRODUCTION
The primary focus of advance care planning (ACP) is shifting from asking patients to make decisions about treatment choices in advance of serious illness to helping prepare patients and their families to make medical decisions “in-the-moment” that are consistent with their values and goals at that time.[1–3] This shift is being prompted by a recognition that: clinical scenarios in advance directives (ADs) may not reflect the complexity of decision-making in nuanced and sometimes unforeseen clinical circumstances facing patients and families;[1–2,4] patients typically make decisions by weighing likely outcomes against burdens of treatment which is a context generally not provided in ADs;[5–7] treatment preferences can change over time;[8] and diminished health outcomes often become more acceptable as health declines.[9] To help prepare patients and families to make “in-the-moment” decisions, consensus expert opinion suggests ACP should begin with discussions of patient values, defined as “expressions of a person’s overarching philosophies and priorities in life”.[10] Patients and families also support the approach of eliciting values to help prepare them for decision-making when facing serious illness.[4] Ideally, by linking patient values to the most consistent treatments within a particular clinical situation, clinicians can ensure patients receive care aligned with their values and goals.[1–3]
Investigations into the application of this approach to ACP are limited but raise several challenges. First, clarifying patient values is often difficult for patients, families, and clinicians. No single strategy to clarify patient values has been widely adopted or successful, although a variety have been proposed.[3,7,11–22] One challenge is that patients commonly endorse multiple priorities that may conflict in guiding treatment decisions near the end of life.[3,11] For example, patients may value extending life as long as possible, but simultaneously value independence, being home with family, and freedom from discomfort near the end of life. In this situation, values may fail to provide reliable guidance on treatment decisions. Second, patients may prefer treatments that are seemingly inconsistent with their end-of-life values. For example, in a study in which patients were asked to independently rate the importance of relief of discomfort and extending life, rather than prioritizing one over the other, researchers found patients who valued freedom from discomfort also commonly requested cardiopulmonary resuscitation (CPR).[3]
Asking patients to prioritize amongst potentially conflicting values may help address these challenges. When patients’ priorities are defined, values may more effectively serve as the basis by which patients discriminate amongst treatment options “in-the-moment”, and clinicians may be better able to align treatment plans with patients’ values. The objective of the current study was to investigate the end-of-life values patients prioritize when facing explicit descriptions of trade-offs and factors associated with these value choices. In addition, we identified predictors of patients whose values and treatment preferences seem potentially inconsistent, specifically patients who prioritized relief of discomfort over extending life and yet also reported preference for CPR.
METHODS
Study Design
We conducted a secondary analysis of baseline surveys from a multi-center cluster-randomized trial designed to improve goals-of-care communication in seriously ill outpatients.[23–26] Data were obtained from patient questionnaires completed at enrollment (prior to the intervention) and from the electronic health record (EHR). Institutional review boards at all sites approved the study, and all participants provided written informed consent.
Population and Setting
Eligible patients were 18 years of age or older and had one or more qualifying condition. Qualifying conditions were chosen to identify patients with a median survival of approximately 2 years or for whom a goals-of-care discussion would be indicated, including those with: metastatic cancer or inoperable lung cancer; COPD with FEV1 <35% predicted or oxygen dependence, restrictive lung disease with TLC <50% predicted, or cystic fibrosis with FEV1 <30% predicted; NYHA Class III or IV heart failure, pulmonary arterial hypertension with six minute walk distance of <250 meters, LVAD, or ICD implant; Child’s Class C cirrhosis or MELD score >17; dialysis-dependent renal failure and diabetes; age 75 years or older and at least one life-limiting chronic illness; age 90 years or older; hospitalization in the prior 18 months with a life-limiting chronic illness; and Charlson comorbidity score of 6 or higher.[27–31] Life-limiting chronic illnesses were defined as any qualifying diagnosis listed above that was not severe enough for outright eligibility. Patients were recruited by mail or phone and then enrolled in person or by mail between March 2014 and May 2016.
Outcomes
Participants were asked to prioritize their end-of-life values with a survey item adapted from the SUPPORT study.[32] They were asked: “If you had to make a choice at this time, would you prefer a plan of medical care that focuses on extending life as much as possible, even if it means having more pain and discomfort, or would you want a plan of medical care that focuses on relieving pain and discomfort as much as possible, even if that means not living as long?” Participants chose either option or “I’m not sure which I would choose”. The “forced choice” structure was used to identify respondents’ top priority.[21–22]
We assessed CPR preferences with two survey questions. The first asked participants their preference in their current health: “In your current health, would you want CPR if your heart were to stop beating?” The second asked their preference in a hypothetical state of dependency: “If you were confined to bed and dependent on others for all your care, would you want CPR if your heart were to stop?” Response options were “Definitely No”, “Probably No”, “Probably Yes”, or “Definitely Yes”. For each question, “definitely” and “probably” responses were collapsed into a dichotomous variable for analyses. Because misperceptions about CPR are common,[18, 33–34] respondents were informed of likely outcomes and burdens of CPR prior to indicating their preferences (Appendix).
Predictors
For analyses of factors associated with each end-of-life value as well as predictors of preference for CPR among patients whose top priority was relief of discomfort, we selected the following patient demographics a priori from self-reported questionnaires: age; gender; race/ethnicity; marital/partner status; level of education; and self-perceived health status (rating between “poor”, “fair”, “good”, “very good”, or “excellent”). A single item from the 8-item Patient Health Questionnaire (PHQ-8) was included as a measure of depression symptoms.[35–37] The item asked patients how often over the last two weeks they were bothered by “feeling down, depressed or hopeless”, with response options of “not at all”, “several days”, “more than half the days”, or “nearly every day”. Variables obtained from the EHR included hospitalization within 18 months prior to study enrollment and qualifying diagnosis of advanced cancer, defined as metastatic cancer or inoperable lung cancer. Demographic variables were chosen because of their associations with treatment preferences in prior studies.[8] We hypothesized that recent hospitalization would stimulate patient reflection on values and that patients with cancer would have unique perspectives given their distinct illness trajectory.[38–39]
Statistical Methods
To examine patient characteristics associated with each prioritized end-of-life value (relief of discomfort, extending life, unsure), we used multinomial multi-predictor logistic regression. Multinomial regression was chosen because there is no inherent ordering to the value options. To evaluate the association of prioritized values with preference for CPR in current health (or if dependent on others), we used the p-value from an omnibus test (based on Wald’s test of parameter constraints) from models without covariate adjustment. Models adjusted for potential confounders produced the same p-values as the unadjusted models. To evaluate whether the proportion of patients who preferred CPR in current health differed from the proportion that preferred CPR if dependent on others, within each value group, we used the Durkalski test, which adjusts the McNemar test for marginal homogeneity in the setting of clustered matched pair data.[40–41] To examine predictors of preference for CPR among patients whose top priority was relief of discomfort, we performed multi-predictor logistic regression estimated with restricted maximum likelihood. All models clustered patients under clinicians to adjust standard errors for lack of independence between patients treated by the same clinician. We accepted a 2-sided p<0.05 as evidence of statistical significance. We used IBM SPSS Version 19 for descriptive statistics, R Version 3.5.3 with clust.bin.pair package for Durkalski[41], Mplus Version 8 for clustered regression models, and HLM Version 7.03 for multi-level models.
RESULTS
There were 917 eligible patients identified for this study; 537 enrolled in the study with 535 answering the end-of-life value question and therefore included in these analyses (participation rate 58%). The average age was 76 years and a slight majority were men (53%). Most patients were non-Hispanic and white (79%), and 45% reported poor-to-fair health status (Table 1).
Table 1.
Patient Characteristics, by Prioritized End-of-Life Valuea
| Relief of Discomfort | Extending Life | Unsure | TOTAL | |
|---|---|---|---|---|
| TOTAL, n (%) | 323 (60.4) | 89 (16.6) | 123 (23.0) | 535 (100) |
| Characteristic | ||||
| Age, median (IQR) | 76.8 (17.0) | 69.2 (18.6) | 74.4 (19.9) | 76.0 (17.9) |
| Female | 166 (51.4) | 35 (39.3) | 53 (43.1) | 254 (47.5) |
| Racial/ethnic minority | 57 (17.6) | 34 (38.2) | 20 (16.3) | 111 (20.7) |
| Currently married or living with partnerb | 136 (42.1) | 42 (47.2) | 66 (54.1) | 244 (45.7) |
| Level of educationb | ||||
| 8th grade or less | 7 (2.2) | 2 (2.2) | 4 (3.3) | 13 (2.4) |
| Some high school | 20 (6.2) | 6 (6.7) | 6 (4.9) | 32 (6.0) |
| High school diploma or equivalent | 39 (12.1) | 15 (16.9) | 19 (15.6) | 73 (13.7) |
| Trade school or some college | 129 (39.9) | 45 (50.6) | 45 (36.9) | 219 (41.0) |
| 4-year college degree | 60 (18.6) | 11 (12.4) | 21 (17.2) | 92 (17.2) |
| Some graduate school | 14 (4.3) | 3 (3.4) | 6 (4.9) | 23 (4.3) |
| Graduate degree | 54 (16.7) | 7 (7.9) | 21 (17.2) | 82 (15.4) |
| Self-perceived health statusc | ||||
| Poor | 50 (15.5) | 13 (14.8) | 14 (11.5) | 77 (14.4) |
| Fair | 98 (30.3) | 24 (27.3) | 43 (35.2) | 165 (31.0) |
| Good | 108 (33.4) | 36 (40.9) | 43 (35.2) | 187 (35.1) |
| Very good | 52 (16.1) | 10 (11.4) | 17 (13.9) | 79 (14.8) |
| Excellent | 15 (4.6) | 5 (5.7) | 5 (4.1) | 25 (4.7) |
| Charlson comorbidity score, median (IQR)d | 7.0 (2.0) | 7.0 (3.0) | 7.0 (4.0) | 7.0 (3.0) |
| Any hospitalization in 18 months before study enrollmente | 149 (46.3) | 51 (57.3) | 50 (41.3) | 250 (47.0) |
| Qualifying conditions | ||||
| Diagnoses | ||||
| Advanced cancer | 50 (15.5) | 13 (14.6) | 34 (27.6) | 97 (18.1) |
| Chronic lung disease | 33 (10.2) | 8 (9.0) | 11 (8.9) | 52 (9.7) |
| Heart failure | 20 (6.2) | 9 (10.1) | 4 (3.3) | 33 (6.2) |
| Liver failure | 1 (0.3) | 1 (1.1) | 1 (0.8) | 3 (0.6) |
| Renal failure | 14 (4.3) | 5 (5.6) | 3 (2.4) | 22 (4.1) |
| Other conditions | ||||
| Age 75+ with chronic life-limiting condition | 128 (39.6) | 27 (30.3) | 43 (35.0) | 198 (37.0) |
| Age 90+ | 30 (9.3) | 2 (2.2) | 4 (3.3) | 36 (6.7) |
| Hospitalized w/serious condition in 18 mo before study enrollment | 52 (16.1) | 20 (22.5) | 18 (14.6) | 90 (16.8) |
| Charlson comorbidity score of 6+ | 266 (82.4) | 69 (77.5) | 105 (85.4) | 440 (82.2) |
| Depression symptoms | ||||
| PHQ2: feeling down/depressed/hopelessf | ||||
| Not at all | 200 (62.9) | 60 (68.2) | 84 (68.9) | 344 (65.2) |
| Several days | 77 (24.2) | 21 (23.9) | 32 (26.2) | 130 (24.6) |
| More than half the days | 26 (8.2) | 3 (3.4) | 4 (3.3) | 33 (6.3) |
| Nearly every day | 15 (4.7) | 4 (4.5) | 2 (1.6) | 21 (4.0) |
Except where otherwise noted, each cell contains the number (percentage of valid cases for the column) with the characteristic.
One case in the unsure group was missing data on this characteristic.
One case in the extending life group and one case in the unsure group were missing data on this characteristic.
Three cases in the relief of pain and discomfort group and three cases in the unsure group were missing data on this characteristic.
One case in the relief of pain and discomfort group and two cases in the unsure group were missing data on this characteristic.
Five cases in the relief of pain and discomfort group, one case in the extending life group, and one case in the unsure group were missing data on this characteristic.
Sixty percent of patients prioritized relief of discomfort, nearly 17% prioritized extending life, and 23% were unsure, prioritizing neither relief of discomfort nor extending life. Patient characteristics by prioritized value are shown in Table 1.
Predictors of Prioritized End-of-Life Value
As compared to patients who selected relief of discomfort, patients who chose extending life were less likely to be older (OR 0.962 per year; 95% CI 0.941, 0.983; Table 2) and more likely to be a member of a racial/ethnic minority (OR 2.749; 95% CI 1.564, 4.833). Compared to patients who were unsure, patients who selected relief of discomfort were more likely to be older (OR 1.020 per year; 95% CI 1.000, 1.040), less likely to have advanced cancer (OR 0.564; 95% CI 0.354, 0.898), and more likely to feel down, depressed or hopeless (OR 1.518 for each increase in level of the symptom; 95% CI 1.105, 2.087). Compared to patients who were unsure, patients who prioritized extending life were more likely to be a member of a racial/ethnic minority (OR 2.760; 95% CI 1.431, 5.279), less likely to have advanced cancer (OR 0.414; 95% CI 0.203, 0.759), and more likely to have been hospitalized in the prior 18 months (OR 1.805; 95% CI 1.040, 3.094).
Table 2.
Associations between Patient Characteristics and Prioritized End-of-Life Valuea
| Prioritized Value | Reference Group | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Extending Life | Relief of Discomfort | Relief of Discomfort | Unsure | Extending Life | Unsure | ||||||||||
| Predictor | b | p | OR | 95% CI | b | p | OR | 95% CI | b | p | OR | 95% CI |
| Age | −0.039 | 0.001 | 0.962 | 0.941, 0.983 | 0.020 | 0.046 | 1.020 | 1.000, 1.040 | −0.019 | 0.137 | 0.981 | 0.957, 1.005 |
| Female | −0.411 | 0.117 | 0.663 | 0.396, 1.109 | 0.332 | 0.104 | 1.394 | 0.934, 2.078 | −0.079 | 0.794 | 0.924 | 0.510, 1.698 |
| Racial/ethnic minority | 1.011 | <0.001 | 2.749 | 1.564, 4.833 | 0.004 | 0.989 | 1.004 | 0.584, 1.725 | 1.015 | 0.002 | 2.760 | 1.431, 5.279 |
| Currently married | 0.231 | 0.354 | 1.260 | 0.773, 2.053 | −0.170 | 0.497 | 0.844 | 0.517, 1.378 | 0.061 | 0.849 | 1.063 | 0.569, 2.024 |
| Level of education | −0.136 | 0.132 | 0.873 | 0.732, 1.041 | 0.054 | 0.528 | 1.056 | 0.893, 1.248 | −0.081 | 0.458 | 0.922 | 0.743, 1.154 |
| Self-perceived health status | 0.100 | 0.459 | 1.105 | 0.848, 1.441 | 0.085 | 0.433 | 1.088 | 0.881, 1.344 | 0.185 | 0.246 | 1.203 | 0.881, 1.649 |
| Advanced cancer | −0.309 | 0.412 | 0.734 | 0.344, 1.565 | −0.573 | 0.016 | 0.564 | 0.354, 0.898 | −0.882 | 0.015 | 0.414 | 0.203, 0.759 |
| Feeling down, depressed, or hopeless | −0.252 | 0.189 | 0.778 | 0.534, 1.132 | 0.418 | 0.010 | 1.518 | 1.105, 2.087 | 0.166 | 0.477 | 1.181 | 0.747, 1.869 |
| Hospitalized in previous 18 months | 0.352 | 0.189 | 1.422 | 0.841, 2.406 | 0.238 | 0.247 | 1.269 | 0.848, 1.900 | 0.591 | 0.036 | 1.805 | 1.040, 3.094 |
Results were based on two multinomial multi-predictor logistic regression models, each with nine predictors and estimated with restricted maximum likelihood. The first model used relief of pain and discomfort group as reference; the second the unsure group. The sample included 523 patients of 128 clinicians: 317 valuing relief of pain and discomfort, 87 valuing extending life, and 119 unsure.
CPR Preferences in Current Health and if Dependent on Others
The majority (518/535; 97%) of patients who answered the end-of-life values question also answered both CPR questions (Figure). Overall, 75% (n=389) of patients preferred CPR in their current health, but this percentage varied by patients’ prioritized values: the proportion preferring CPR in their current health was 69% (n=217) among patients who prioritized relief of discomfort, 78% (n=91) among patients who were unsure of their prioritized value, and 93% (n=81) among those who prioritized extending life (p-value <0.001). Overall, 31% (n=163) of patients preferred CPR in a potential state of dependency, and this percentage also varied by patients’ prioritized values: the proportion who preferred CPR if dependent on others was 21% (n=66) among patients who prioritized relief of discomfort, 33% (n=39) among patients who were unsure, and 67% (n=58) among patients who prioritized extending life (p-value <0.001). The proportion of patients who preferred CPR in current health was significantly greater than the proportion who preferred CPR in dependency within each prioritized value group (extending life chi-square 17.6, p-value <0.0001; relief of pain and discomfort chi-square 77.9, p-value <0.0001; unsure chi-square 34.4, p-value <0.0001).
Figure.
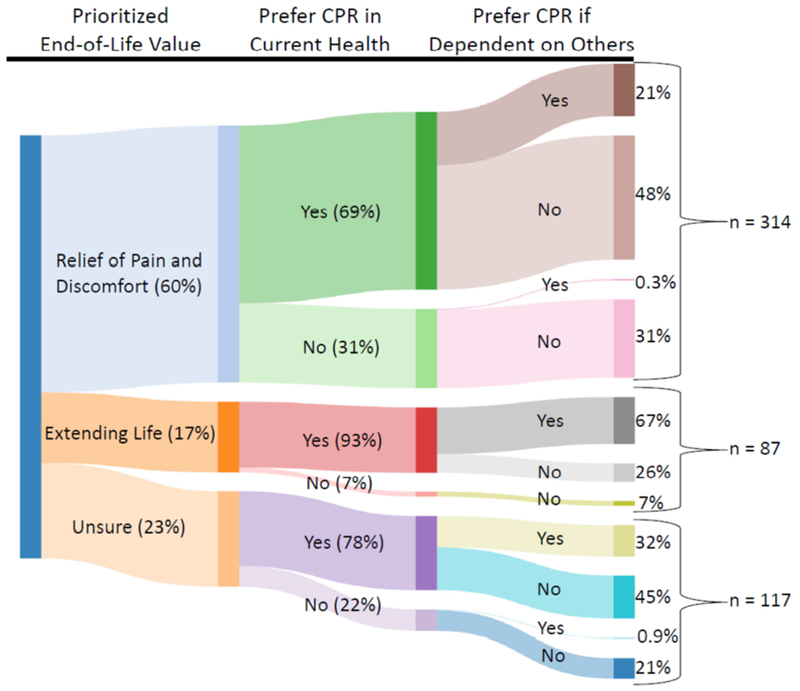
Patient CPR preference in current health and if dependent on others, by prioritized end-of-life valuea
a The sample includes 518 patients with responses to all three questions.
Predictors of Preference for CPR among Patients who Prioritized Relief of Discomfort
Among patients who prioritized relief of discomfort, patients who preferred CPR in their current health were less likely to be older (OR 0.958 per year; 95% CI 0.935, 0.981; Table 3) and more likely to have better self-perceived health status (OR 1.402 for each level of improvement in self-perceived health; 95% CI 1.090, 1.804) as compared to patients who did not prefer CPR.
Table 3.
Associations between Patient Characteristics and Preference for CPR in Current Health, among Patients Who Prioritized Relief of Discomfort
| Predictor | b | p | OR | 95% CI |
|---|---|---|---|---|
| Age | −0.043 | <0.001 | 0.958 | 0.935, 0.981 |
| Female | −0.276 | 0.296 | 0.759 | 0.452, 1.274 |
| Racial/ethnic minority | 0.687 | 0.087 | 1.988 | 0.906, 4.363 |
| Currently married | 0.511 | 0.077 | 1.668 | 0.947, 2.937 |
| Level of education | 0.024 | 0.764 | 1.024 | 0.878, 1.193 |
| Self-perceived health status | 0.338 | 0.009 | 1.402 | 1.090, 1.804 |
| Advanced cancer | −0.415 | 0.285 | 0.660 | 0.308, 1.414 |
| Feeling down, depressed, or hopeless | 0.234 | 0.209 | 1.264 | 0.877, 1.821 |
| Hospitalized in previous 18 months | −0.235 | 0.387 | 0.791 | 0.464, 1.347 |
The independent associations of the nine predictors with the outcome (0= definitely or probably not preferring CPR in current health, 1= definitely or probably preferring CPR in current health) were based on a multi-predictor logistic regression model estimated with restricted maximum likelihood and using data from 314 patients of 124 clinicians (94 not desiring CPR and 220 desiring CPR in their current health).
Among patients who prioritized relief of discomfort, patients who preferred CPR if dependent on others were less likely to be older (OR 0.969 per year; 95% CI 0.940, 0.999; Table 4) and more likely to be a member of a racial/ethnic minority (OR 3.618; 95% CI 1.878, 6.970) as compared to patients who did not prefer CPR.
Table 4.
Associations between Patient Characteristics and Preference for CPR if Dependent, among Patients Who Prioritized Relief of Discomfort
| Predictor | b | p | OR | 95% CI |
|---|---|---|---|---|
| Age | −0.032 | 0.040 | 0.969 | 0.940, 0.999 |
| Female | −0.191 | 0.564 | 0.826 | 0.432, 1.580 |
| Racial/ethnic minority | 1.286 | <0.001 | 3.618 | 1.878, 6.970 |
| Currently married | −0.045 | 0.884 | 0.956 | 0.520, 1.757 |
| Level of education | −0.145 | 0.140 | 0.865 | 0.713, 1.049 |
| Self-perceived health status | 0.104 | 0.521 | 1.109 | 0.808, 1.524 |
| Advanced cancer | −0.708 | 0.178 | 0.493 | 0.176, 1.379 |
| Feeling down, depressed, or hopeless | 0.378 | 0.055 | 1.459 | 0.992, 2.146 |
| Hospitalized in previous 18 months | −0.225 | 0.455 | 0.799 | 0.443, 1.441 |
The independent associations of the nine predictors with the outcome (0= definitely or probably not preferring CPR if dependent, 1= definitely or probably preferring CPR if dependent) were based on a multi-predictor logistic regression model estimated with restricted maximum likelihood and using data from 312 patients of 124 clinicians (247 not desiring CPR and 65 desiring CPR if dependent).
DISCUSSION
In this study of seriously ill adults asked to prioritize their end-of-life values and choose their CPR preferences, we report several findings relevant to clinicians’ use of patients’ values to determine treatment plans. Although the majority of patients were able to prioritize their values, nearly a quarter were unable to do so and identified themselves as “unsure”. We also found that treatment preferences depended on context—that is, how functional a patient might be prior to treatment—and we also failed to find important predictors that direct clinicians toward a patient’s primary value. Finally, although we found patients’ prioritized values were associated with their CPR preferences, a substantial proportion of patients expressed CPR preferences that appeared potentially inconsistent with their primary value.
We found nearly a quarter of patients were unable to select a primary value, endorsing “unsure” instead. This finding challenges the idea that all seriously ill patients have a clear and well-defined idea of what is most important to them when considering end-of-life care, and that they are able and ready to share these values when asked. Our findings instead suggest that, for some patients, end-of-life values are not necessarily well prioritized or able to be articulated even with a “forced choice” question. Identifying and ranking values is a context dependent process,[42–43] and while an explicit focus on the kinds of trade-offs patients are likely to face in the future given their particular conditions and prognosis may help them prioritize,[44] this process probably takes time for many patients. Helping patients move past uncertainty is an important part of preparing them to make decisions “in-the-moment”, as aligning treatments without a clear priority to guide care can be difficult. Clinicians should try to identify patients who have not prioritized their values early, as they may benefit from more frequent discussions and time to process. Moreover, clinicians should investigate possible reasons for uncertainty and choose varying approaches to address them. For some patients, uncertainty may result from psychological factors such as fear and anxiety, distrust in their clinician, or a limited support network. For others, uncertainty may result from cognitive factors such as lack of information about prognosis[45] and/or the kinds of trade-offs they are likely to face.
Another finding from our study suggests the importance of context on the relationship between values and treatment preferences. Among patients who prioritized extending life, over a quarter who selected the well aligned desire for CPR in their current health changed their CPR preference if in a dependent health state. This finding underscores the likely possibility that treatment preferences and the accompanying values on which they may be grounded may change over situation and time,[42–43] yet little investigation into the stability of end-of-life values has been performed in seriously ill patients.[19–20,46] Further work is needed to understand how patients prioritize values with changing contexts and over time, especially if values are to be the anchor that defines whether care is goal-concordant. One way to address this concern is to repeat discussions over time with a focus on reaffirming patients’ priorities or identifying changes in them.
We identified only a few and relatively weak predictors of prioritized value groups, providing clinicians with limited factors to consider when deciding who and how to approach for value discussions. We found the strongest predictor of the prioritized value of extending life was minority race/ethnicity. This finding is consistent with prior literature suggesting black and Hispanic patients often prefer more aggressive medical treatments at end of life than non-Hispanic whites, even after controlling for socioeconomic confounders.[47–49] One novel finding in need of further study was the increased endorsement of uncertainty about primary values amongst patients with advanced cancer. Although the illness trajectory of patients with advanced cancer is generally more predictable than for many other types of serious illness, patients’ experience of their illness may be uncertain and conflicting. For example, while oncologists frequently inform patients with advanced cancer that their disease is terminal, specific details such as survival estimates are often absent.[50] Patients with advanced cancer often fail to recognize the terminal nature of their condition and commonly overestimate their likelihood of survival, with medical care goals that reflect those optimistic estimates.[45, 51] Uncertainty about values in this population is further suggested by the recent finding that patients with advanced cancer who lacked understanding of the terminal nature of their illness were more likely to switch their top priority between relief of pain and discomfort and extending life in the absence of an unsure response option.[45]
Because of the critical role values are expected to play in treatment choices, we also examined CPR preferences and found potential misalignment between prioritized values and preference for CPR is common. Nearly 7 out of 10 patients who prioritized relief of discomfort also preferred to receive CPR in their current health, while 1 in 5 preferred to receive CPR in a hypothetical state of dependency on others for all their activities of daily living. One possible explanation for this finding may be lack of knowledge about CPR, including implications for quality of life. Prior studies suggest patients’ expectations about CPR are often overly optimistic, but when informed of the likely outcomes and associated burdens many choose to forgo CPR.[18,52–53] While we informed patients of the low likelihood of success of CPR and its associated burdens prior to surveying their CPR preference, it is possible some patients preferred CPR because they were optimistic about the outcome in their case, perhaps in part because of reliance on more than just medical estimates when forming perceptions of their prognosis.[54–55] Another potential explanation is that some patients may feel unwilling to choose to forgo CPR because it feels like “giving up” or a choice between life and death,[56] even if they fully acknowledge the likely poor outcomes. Alternatively, some patients may fear that forgoing CPR will limit their receipt of other desired medical care, a fear rooted in the symbolic power of CPR[57] and supported by empirical evidence.[58–61] Other patients may envision achievement of important life activities to be possible, even in a dependent state, and therefore successful CPR could prolong that acceptable quality of life.[14] Our description of a dependent state did not include decreased cognitive function, which is valued higher than physical function by many patients.[14]
Among patients more likely to report values seemingly inconsistent with preference for CPR were younger patients, those with better self-perceived health status, and members of racial/ethnic minorities. The particularly strong association amongst minority race/ethnicity warrants consideration of the role culture may play in values and treatment preferences. Values may be fundamentally different amongst patients with different backgrounds.[47–48] It is possible our survey question provides an incomplete picture of the values of these patients, and perhaps fuller understanding might reveal their preference for CPR is not, in fact, inconsistent with their value system. Alternatively, even when patients have identified relief of discomfort as their top priority, distrust of the healthcare system that may be rooted in historical and ongoing disparities may lead to more aggressive treatment choices.[47]
These findings raise several potential challenges for clinicians seeking to align treatments with end-of-life values. While clinicians might interpret the value of “relief of discomfort” as inconsistent with a preference for CPR, patients may not share this perception. It is important for clinicians to take time with patients to discuss and understand their perspectives. If it appears that the potential mismatch between values and treatment choice is due to lack of knowledge, clinicians might provide additional information on outcomes and burdens of CPR. For example, informing seriously ill patients that the most likely outcome of CPR, other than failure to revive them, is revival to a dependent state may provide information that will help patients align their CPR preferences with their values, as suggested by the significant drop in preference for CPR from 69% in current health to 21% if dependent among patients with a top priority of relief of pain and discomfort. However, when caring for patients whose preference for CPR stems from distrust or whose values are incompletely understood by clinicians perhaps because of difficulty communicating across cultures, clinicians may need to start by building trust or learning more about the patient’s culture. Similarly, while the values-first approach to ACP may encourage clinicians to make recommendations for treatments they perceive to align with patient values, recommendations given prematurely or with incomplete understanding of patient values or culture have potential for harm[62] while those built from trust may be quite helpful. Finally, in some cases clinicians may need to acknowledge their incomplete understanding of alternative value-preference frameworks and work to provide care that is mutually acceptable. While clinicians should explore values and preferences that sound potentially inconsistent, ultimately patients should define their own values. Further work is needed to better understand reasons for potentially inconsistent values and treatment preferences and develop strategies to navigate these situations.
Our study has several important limitations. First, discussing values with patients is different than responding to survey questions. While useful, survey questions likely oversimplify complex patient perspectives and decision-making. In this study, we did not explore how patients interpreted the values question, although it was developed and cognitively tested with patients for the SUPPORT study.[63] Although the wording of the values question was designed to address a current choice, it is possible some patients answered by projecting into the future, which could contribute to some of our findings. Second, we did not assess the importance of other possible end-of-life values, such as maintaining independence or preserving cognitive function. Perhaps some patients selected “unsure” because they prioritized an alternative value. While it may be possible to incorporate additional options into the values question, qualitative work is needed to ensure the question’s intent remains clear to patients. Third, patients in our study were seriously ill, but not terminally ill, as only 40 patients died during the study. It is possible the prioritized values, CPR preferences, and alignment between them for terminally ill patients may be different than for seriously ill patients. Fourth, our investigation into predictors of both prioritized end-of-life values and preferences for CPR among patients who prioritized relief of discomfort was limited to mostly non-modifiable factors based on the data available. Future work should focus on examination of more modifiable factors. Fifth, although our participation rate for patients was relatively high at 58%, some non-response bias could be present. Finally, although multi-centered, our study took place in one region of the US with mostly white, non-Hispanic patients and may not generalize to other regions or populations.
In this study, we assessed prioritized end-of-life values and CPR preferences among adults with serious illness. We identified challenges clinicians may face as they seek to align end-of-life care with their patients’ values. Further work is needed to better understand how patients prioritize potentially conflicting values and how patients with potentially inconsistent values and treatment preferences can best be supported by clinicians. To help manage these challenges, clinicians engaging in ACP should initiate discussions early, revisit them over time, and confirm the relationship between values and treatment preferences for each patient.
ACKNOWLEDGEMENTS
1. Contributors: none
2. Funders:
Patient-Centered Outcomes Research Institute® (PCORI®) Award (IH-12-11-4596)
Grant from the Cambia Health Foundation
University of Washington Pulmonary and Critical Care T32 # HL 007287-39
University of Washington Palliative Care T32 # HL 125195-04
3. Prior Presentation: none
Appendix:
Prior to answering the questions about CPR preferences, participants were asked to read the following:
“CPR consists of electric shocks to the heart, pumping on the chest, and help with breathing. Possible side effects of CPR include broken ribs and memory loss. It is important to realize that, for most people, CPR doesn’t work and they do not survive the attempt of CPR.”
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLAIMER
The statements presented in this work are solely the responsibility of the author(s) and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute® (PCORI®), its Board of Governors or Methodology Committee.
CONFLICTS OF INTEREST
There are no conflicts of interest from any of the authors.
Matthew E. Modes, MD, MPP = no conflicts of interest
Ruth A. Engelberg, PhD = no conflicts of interest
Lois Downey, MA = no conflicts of interest
Elizabeth L. Nielsen, MPH = no conflicts of interest
Robert Y. Lee, MD = no conflicts of interest
J. Randall Curtis, MD, MPH = no conflicts of interest
Erin K. Kross, MD = no conflicts of interest
REFERENCES
- [1].Sudore RL, Fried TR. Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Ann Intern Med. 2010. August 17;153(4):256–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Schenker Y, White DB, Arnold RM. What should be the goal of advance care planning? JAMA Intern Med. 2014. July;174(7):1093–4. [DOI] [PubMed] [Google Scholar]
- [3].Heyland DK, Heyland R, Dodek P, You JJ, Sinuff T, Hiebert T, Jiang X, Day AG, ACCEPT Study Team and the Canadian Researchers at the End of Life Network (CARENET). Discordance between patients’ stated values and treatment preferences for end-of-life care: results of a multicentre survey. BMJ Support Palliat Care. 2017. September;7(3):292–299. [DOI] [PubMed] [Google Scholar]
- [4].McMahan RD, Knight SJ, Fried TR, Sudore RL. Advance care planning beyond advance directives: perspectives from patients and surrogates. J Pain Symptom Manage. 2013. September;46(3):355–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Rosenfeld KE, Wenger NS, Kagawa-Singer M. End-of-life decision making: a qualitative study of elderly individuals. J Gen Intern Med. 2000. September;15(9):620–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002. April 4;346(14):1061–6. [DOI] [PubMed] [Google Scholar]
- [7].Fried TR, Bradley EH. What matters to seriously ill older persons making end-of-life treatment decisions?: a qualitative study. J Palliat Med. 2003. April;6(2):237–44. [DOI] [PubMed] [Google Scholar]
- [8].Auriemma CL, Nguyen CA, Bronheim R, Kent S, Nadiger S, Prado D, Halpern SD. Stability of end-of-life preferences: a systematic review of the evidence. JAMA Intern Med. 2014. July;174(7):1085–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Fried TR, Byers AL, Gallo WT, et al. Prospective study of health status preferences and changes in preferences over time in older adults. Arch Intern Med. 2006. April 24;166(8):890–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Sudore RL, Lum HD, You JJ, Hanson LC, Meier DE, Pantilat SZ, Matlock DD, Rietjens JAC, Korfage IJ, Ritchie CS, Kutner JS, Teno JM, Thomas J, McMahan RD, Heyland DK. Defining Advance Care Planning for Adults: A Consensus Definition From a Multidisciplinary Delphi Panel. J Pain Symptom Manage. 2017. May;53(5):821–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Howard M, Bansback N, Tan A, Klein D, Bernard C, Barwich D, Dodek P, Nijjar A, Heyland DK. Recognizing difficult trade-offs: values and treatment preferences for end-of-life care in a multi-site survey of adult patients in family practices. BMC Med Inform Decis Mak. 2017. December 6;17(1):164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Winter L Patient values and preferences for end-of-life treatments: are values better predictors than a living will? J Palliat Med. 2013. April;16(4):362–8. [DOI] [PubMed] [Google Scholar]
- [13].Pearlman RA, Cain KC, Patrick DL, Appelbaum-Maizel M, Starks HE, Jecker NS, Uhlmann RF. Insights pertaining to patient assessments of states worse than death. J Clin Ethics. 1993. Spring;4(1):33–41. [PubMed] [Google Scholar]
- [14].Ditto PH, Druley JA, Moore KA, Danks JH, Smucker WD. Fates worse than death: the role of valued life activities in health-state evaluations. Health Psychol. 1996. September;15(5):332–343. [DOI] [PubMed] [Google Scholar]
- [15].Fried TR, McGaw S, Agostini JV, Tinetti ME. Views of older persons with multiple morbidities on competing outcomes and clinical decision-making. J Am Geriatr Soc. 2008. October;56(10):1839–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Fried TR, Tinetti M, Agostini J, lannone L, Towle V. Health outcome prioritization to elicit preferences of older persons with multiple health conditions. Patient Educ Couns. 2011. May;83(2):278–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Fried TR, Tinetti ME, Iannone L, O’Leary JR, Towle V, Van Ness PH. Health outcome prioritization as a tool for decision making among older persons with multiple chronic conditions. Arch Intern Med. 2011. November 14;171(20):1854–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Kaldjian LC, Erekson ZD, Haberle TH, Curtis AE, Shinkunas LA, Cannon KT, Forman-Hoffman VL. Code status discussions and goals of care among hospitalised adults. J Med Ethics. 2009. June;35(6):338–42. [DOI] [PubMed] [Google Scholar]
- [19].Tsevat J, Cook EF, Green ML, Matchar DB, Dawson NV, Broste SK, Wu AW, Phillips RS, Oye RK, Goldman L. Health values of the seriously ill. SUPPORT investigators. Ann Intern Med. 1995. April 1;122(7):514–20. [DOI] [PubMed] [Google Scholar]
- [20].Tsevat J, Dawson NV, Wu AW, Lynn J, Soukup JR, Cook EF, Vidaillet H, Phillips RS. Health values of hospitalized patients 80 years or older. HELP Investigators. Hospitalized Elderly Longitudinal Project. JAMA. 1998. February 4;279(5):371–5. [DOI] [PubMed] [Google Scholar]
- [21].Finkelstein EA, Bilger M, Flynn TN, Malhotra C. Preferences for end-of-life care among community-dwelling older adults and patients with advanced cancer: a discrete choice experiment. Health Policy. 2015;119(11):1482–1489. [DOI] [PubMed] [Google Scholar]
- [22].Flynn TN, Bilger M, Malhotra C, Finkelstein EA. Are efficient designs used in discrete choice experiments too difficult for some respondents? A case study eliciting preferences for end-of-life care. Pharmacoeconomics. 2016;34(3):273–284. [DOI] [PubMed] [Google Scholar]
- [23].Curtis JR, Downey L, Back AL, et al. Effect of a patient and clinician communication-priming intervention on patient-reported goals-of-care discussions between patients with serious illness and clinicians: a randomized clinical trial. JAMA Intern Med. 2018. July 1;178(7):930–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Fakhri S, Engelberg RA, Downey L, Nielsen EL, Paul S, Lahdya AZ, Treece PD, Curtis JR. Factors affecting patients preferences for and actual discussions about end-of-life care. J Pain Symptom Manage. 2016. September;52(3):386–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Coats H, Downey L, Sharma RK, Curtis JR, Engelberg RA. Quality of Communication and Trust in Patients With Serious Illness: An Exploratory Study of the Relationships of Race/Ethnicity, Socioeconomic Status, and Religiosity. J Pain Symptom Manage. 2018. October;56(4):530–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Modes ME, Engelberg RA, Downey L, Nielsen EL, Curtis JR, Kross EK. Did a Goals-of-Care Discussion Happen? Differences in the Occurrence of Goals-of-Care Discussions as Reported by Patients, Clinicians, and in the Electronic Health Record. J Pain Symptom Manage. 2019. February;57(2):251–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].McMurray JJ, Pfeffer MA. Heart failure. Lancet. 2005;365(9474):1877–1889. [DOI] [PubMed] [Google Scholar]
- [28].Connors AF Jr, Dawson NV, Thomas C, et al. Outcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments). Am J Respir Crit Care Med. 1996;154(4, pt 1):959–967. [DOI] [PubMed] [Google Scholar]
- [29].Steinhauser KE, Clipp EC, Hays JC, et al. Identifying, recruiting, and retaining seriously-ill patients and their caregivers in longitudinal research. Palliat Med. 2006;20(8):745–754. [DOI] [PubMed] [Google Scholar]
- [30].Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62(1):10–29. [DOI] [PubMed] [Google Scholar]
- [31].Cholongitas E, Papatheodoridis GV, Vangeli M, Terreni N, Patch D, Burroughs AK. Systematic review: the model for end-stage liver disease – should it replace Child-Pugh’s classification for assessing prognosis in cirrhosis? Aliment Pharmacol Ther. 2005;22(11-12):1079–1089. [DOI] [PubMed] [Google Scholar]
- [32].The SUPPORT Principal Investigators. A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). JAMA. 1995. November 22-29;274(20):1591–8. [PubMed] [Google Scholar]
- [33].Heyland DK, Frank C, Groll D, Pichora D, Dodek P, Rocker G, Gafni A. Understanding cardiopulmonary resuscitation decision making: perspectives of seriously ill hospitalized patients and family members. Chest. 2006. August;130(2):419–28. [DOI] [PubMed] [Google Scholar]
- [34].Gehlbach TG, Shinkunas LA, Forman-Hoffman VL, Thomas KW, Schmidt GA, Kaldjian LC. Code status orders and goals of care in the medical ICU. Chest. 2011. April;139(4):802–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Martin A, Rief W, Klaiberg A, Braehler E. Validity of the brief patient health questionnaire mood scale (PHQ-9) in the general population. Gen Hosp Psychiatry. 2006;28(1):71–77. [DOI] [PubMed] [Google Scholar]
- [36].Lowe B, Grafe K, Kroenke K, et al. Predictors of psychiatric comorbidity in medical outpatients. Psychosom Med. 2003;65(5):764–770. [DOI] [PubMed] [Google Scholar]
- [37].Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry TJ, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Discord. 2009. April;114(1–3):163–73. [DOI] [PubMed] [Google Scholar]
- [38].Lunney JR, Lynn J, Foley DJ, Lipson S, Guralnik JM. Patterns of functional decline at the end of life. JAMA. 2003. May 14;289(18):2387–92. [DOI] [PubMed] [Google Scholar]
- [39].Lunney JR, Albert SM, Boudreau R, Ives D, Satterfield S, Newman AB, Harris T; Health Aging and Body Composition Study. Mobility Trajectories at the End of Life: Comparing Clinical Condition and Latent Class Approaches. J Am Geriatr Soc. 2018. March;66(3):503–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Durkalski VL, Palesch YY, Lipsitz SR, Rust PF. Analysis of clustered matched-pair data. Statistics in medicine. 2003;22(15), 2417–2428. [DOI] [PubMed] [Google Scholar]
- [41].Gopstein D Statistical methods for analyzing clustered matched pair data. 2018. February 15 Available at: https://cran.r-project.org/web/packages/clust.bin.pair/clust.bin.pair.pdf
- [42].Slovic P The Construction of Preference. American Psychologist. 1995. May;50(5):364–371. [Google Scholar]
- [43].Dickert S, Slovic P. Unstable values in lifesaving decisions. Front Psychol. 2011. November 15;2:294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Abhyankar P, Bekker HL, Summers BA, Velikova G. Why values elicitation techniques enable people to make informed decisions about cancer trial participation. Health Expectations. 2010;14(1):20–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Jabbarian LJ, Maciejewski RC, Maciejewski PK, Rietjens JA, Korfage IJ, van der Heide A, van Delden JJ, Prigerson HG. The Stability of Treatment Preferences among Patients with Advanced Cancer. J Pain Symptom Manage. 2019. June;57(6):1071–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Lockhart LK, Ditto PH, Danks JH, Coppola KM, Smucker WD. The stability of older adults’ judgments of fates better or worse than death. Death Stud. 2001. June;25(4):299–317. [DOI] [PubMed] [Google Scholar]
- [47].Kagawa-Singer M, Blackhall LJ. Negotiating cross-cultural issues at the end of life: “You got to go where he lives”. JAMA. 2001. December 19;286(23):2993–3001. [DOI] [PubMed] [Google Scholar]
- [48].Cain CL, Surbone A, Elk R, Kagawa-Singer M. Culture and Palliative Care: Preferences, Communication, Meaning, and Mutual Decision Making. J Pain Symptom Manage. 2018. May;55(5):1408–1419. [DOI] [PubMed] [Google Scholar]
- [49].Barnato AE, Anthony DL, Skinner J, Gallagher PM, Fisher ES. Racial and ethnic differences in preferences for end-of-life treatment. J Gen Intern Med. 2009. June;24(6):695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Daugherty CK, Hlubocky EJ. What are terminally ill cancer patients told about their expected deaths? A study of cancer physicians’ self-reports of prognosis disclosure. J Clin Oncol. 2008. December 20;26(36):5988–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Weeks JC, Cook EF, O’Day SJ, et al. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA. 1998. June 3;279(21):1709–14. [DOI] [PubMed] [Google Scholar]
- [52].Schonwetter RS, Walker RM, Kramer DR, Robinson BE. Resuscitation decision making in the elderly: the value of outcome data. J Gen Intern Med. 1993. June;8(6):295–300. [DOI] [PubMed] [Google Scholar]
- [53].Murphy DJ, Burrows D, Santilli S, Kemp AW, Tenner S, Kreling B, Teno J. The influence of the probability of survival on patients’ preferences regarding cardiopulmonary resuscitation. N Engl J Med. 1994. February 24;330(8):545–9. [DOI] [PubMed] [Google Scholar]
- [54].Fried TR, Bradley EH, O’Leary J. Prognosis communication in serious illness: perceptions of older patients, caregivers, and clinicians. J Am Geriatr Soc. 2003. October;51(10):1398–403. [DOI] [PubMed] [Google Scholar]
- [55].Ahalt C, Walter LC, Yourman L, Eng C, Perez-Stable EJ, Smith AK. “Knowing is better”: preferences of diverse older adults for discussing prognosis. J Gen Intern Med. 2012. May;27(5):568–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Eliott J, Olver I. Choosing between life and death: patient and family perceptions of the decision not to resuscitate the terminally ill cancer patient. Bioethics. 2008. March;22(3):179–89. [DOI] [PubMed] [Google Scholar]
- [57].Brauner DJ. Later than sooner: a proposal for ending the stigma of premature do-not-resuscitate orders. J Am Geriatr Soc. 2011. December;59(12):2366–8. [DOI] [PubMed] [Google Scholar]
- [58].Breu AC, Herzig SJ. Differentiating DNI from DNR: combating code status conflation. J Hosp Med. 2014. October;9(10):669–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Beach MC, Morrison RS. The effect of do-not-resuscitate orders on physician decision-making. J Am Geriatr Soc. 2002. December;50(12):2057–61. [DOI] [PubMed] [Google Scholar]
- [60].Stevenson EK, Mehter HM, Walkey AJ, Wiener RS. Association between Do Not Resuscitate/Do Not Intubate Status and Resident Physician Decision-making. A National Survey. Ann Am Thorac Soc. 2017. April;14(4):536–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Fuchs L, Anstey M, Feng M, Toledano R, Kogan S, Howell MD, Clardy P, Celi L, Talmor D, Novack V. Quantifying the Mortality Impact of Do-Not-Resuscitate Orders in the ICU. Crit Care Med. 2017. June;45(6):1019–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Luth EA, Prigerson HG. Unintended Harm? Race Differences in the Relationship Between Advance Care Planning and Psychological Distress at the End of Life. J Pain Symptom Manage. 2018. November;56(5):752–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Kreling B, Robinson DK, Bergner M. Data collection strategies in SUPPORT. J Clin Epidemiol. 1990;43 Suppl:5S–9S. [DOI] [PubMed] [Google Scholar]


