Abstract
The aim of this mini review was to report the molybdenum compound intervention to control cancer disease. The intervention explains its roles and progress from inorganic molybdenum compounds via organomolybdenum complexes to its nanoparticles to control oesophageal cancer and breast cancer as case studies. Main contributions of molybdenum compounds as anticancer agents could be observed in their nanofibrous support with suitable physicochemical properties, combination therapy, and biosensors (biomarkers). Recent areas in anticancer drug design, which entail the uses of selected targets, were also surveyed and proposed.
1. Introduction
The increase in the population of those affected with cancer globally warrants a swift attention [1–6]. The increase might be due to aging, world population growth, and cancer-causing behaviours (smoking) [6]. From Jemal et al.'s study, they predicted more in the increase of all-cancer cases from 12.7 million emergent cases in 2008 to 22.2 million by 2030 [6].
Drugs used to control the increasing cancer are either cytotoxic (cell killing) or cytostatic (cell stabilizing) [1]. Both drugs lead to decrease in the tumour size due to the reason that cancer cells have a high mortality rate which stops them from splitting up, thereby resulting in a decrease in their populace [1]. In order to further bring decrease in the populace, the global research is focusing on the development of existing agents and the innovation of novel biological objectives. Medicinal application of metals can be dated back to five thousand years ago [1]. Metalloelements in trace amounts execute important activities in the living system. Among these metalloenzymes are transition metals, which represent the d block elements between Groups 3 and 12 in the periodic table [1]. The d block transition metals in the periodic table have partially filled electrons (d orbitals), which influence remarkable electronic properties when examined for the development and design of anticancer agents. This property of transition metals leads to the foundation of coordination compounds (metal complexes) [1]. The transition metal ions play important roles in appropriate functioning of various enzymes. The ligation of different bioligands to biometals enhances the metals' activities. The ability of ligands to coordinate metals in a three-dimensional arrangement permits groups' functionalization which can be designed to distinct molecular targets in the development of novel medicinal agents. The mode of biological action for coordination compounds relies on the thermodynamic and kinetic properties. The drug's lipophilicity is improved through chelates' formation, and drug action is extensively enhanced because of efficient drug permeability into the site of action. Additionally, coordination compounds implement important activities in agriculture and pharmaceutical industries.
In 1960, an antitumour action of an inorganic compound of cis-diammine-dichloroplatinum(III) (cisplatin) was discovered [1]. Today, in the clinics, cisplatin (platinum metal ammine) is a global cytotoxic drug for cancer treatment [1]. Further development of cisplatin had made it the most efficient drug for solid carcinomas' treatment.
In order to improve the global anticancer study, comes the question, what impact does molybdenum play?
Molybdenum has been known to exist in history. Carl Wilhelm Scheele discovered the element in 1778, while Peter Jacob Hjelm first isolated it in 1781 [7]. Molybdenum is the least abundant element in Group VI. It is extensively distributed in nature. The natural occurrence in the combined state most often occurs as ores of molybdenite (MoS2) and wulfenite (PbMoO4). It is silvery white in appearance and belongs to the chromium group.
Molybdenum is a second-row transition element [8, 9]. It has a symbol of Mo, atomic number of 42, mass number of 95.94, and electron configuration of [Kr] 4d55s1. It has a range of oxidation states from +2 to +6, that is, has five valances (+2, +3, +4, +5, and +6), where oxidation states from +2 to +5 are air sensitive. The key isotopes are 95Mo, 96Mo, and 98Mo.
Salts of molybdenum with oxidation states ranging from +3 to +6 can be formed with the exception of +5. Mo(VI) salts are the most stable. It forms stable and water-soluble compounds in trivalent and hexavalent states.
The hardness, durability, and toughness make them essential alloys and steels. Apart from the use of molybdenum as alloys and steels, other industrial uses include the use of molybdenum sulfide as a lubricant, colorant for ceramic and textiles, building aircraft and missile parts, application in nuclear energy, filaments in electrical devices, building filament supports in incandescent lamps, and electrodes for electrically heated glass furnaces. It is used industrially as a catalyst to refine petroleum. On the other hand, Mo can also be found in different concentrations in water.
Molybdenum is a vital trace element for humans, animals, and plants. It serves as an essential trace element in the nutrition of plants. Molybdenum in trace concentration can be found in plant-derived foods like cereal grains, cheese, leafy vegetables, legumes, milk, nuts, and organ meats. This depends on the concentration of molybdenum present in the soil of the growing region. In the human body, molybdenum is stored in the bones, glands, liver, and kidneys. It can also be located in the lungs, muscles, skin, and spleen, but almost 90% of molybdenum eaten from foods is eradicated from digested foods through the urine. Medical applications of molybdenum are numerous including avoidance of dental caries, cure of anaemia, enhancement of immunological reactions, as anticancer and antidiabetic agents. Molybdenum has an antagonistic action against copper; that is, high concentrations of molybdenum can decrease copper absorption and afterwards cause copper deficiency [7].
Molybdenum atoms go through transition between oxidation states of IV and VI, during enzymatic reactions [10]. Molybdenum, as a constituent of molybdoprotein, participates to form active sites for numerous enzymes. The three main molybdenum-containing enzymes are aldehyde oxidase, dehydrogenase/oxidase, and sulphite oxidase. Molybdenum containing enzymes perform three functions, namely, purine catabolism, protein synthesis stimulation, and body growth [7].
Fisher et al. reported the ambiguous impact of molybdenum in xanthine oxidase (XOD (flavoprotein enzyme)), while Hille et al. stated that XOD was the first evidence of the biological relevance of molybdenum in molybdenum-consisting metalloenzymes [11, 12].
Healthwise, Chan et al. [13] and Dmedley et al. [14] explained that exposure to the element can be detrimental, with scarce indication for signs in humans. Komada et al. reported that low molybdenum content in South African and China soils resulted in esophageal cancer [15]. Nouri et al.'s works were in line with those of Komada et al. when they reported low and moderate occurrence of esophageal cancer in Iran soils was due to low molybdenum content [16]. Researchers had reported the biological application of molybdenum as antibacterial, anticancer, antifungal, and antiulcer agents [17–20]. The motivation for opting for molybdenum among several metals was due to its wide labile chemistry and low toxicity [21, 22]. This review aimed to report on the advances in the use of molybdenum compounds as anticancer agents against esophageal cancer and breast cancer. Esophageal cancer and breast cancer were looked into among other types of cancer diseases because food has to pass through the esophageal (gullet) for it to be digested and provide energy, while babies feed on milk from women's breast for the first few months of the growth.
2. Molybdenum Compounds and Molybdenum Complexes as Anticancer Agents in Chemotherapy
The current treatments for cancer are surgery, radiation, and chemotherapy.
In chemotherapy, certain classifications of significant inorganic compounds (molybdenum halides (molybdenum(II) chloride and molybdenum(III) chloride), molybdenum oxides (molybdenum(IV) oxide (MoO2), and molybdenum(VI) oxide (MoO3)), iso- and hetero-polyoxomolybdates), molybdenum hexacarbonyl and hybrid inorganic-organic materials, and molybdenum oxides (MonW1−nO3), with chemical structures are shown in Figure 1. They are used vastly for medicinal applications [23, 24].
Figure 1.
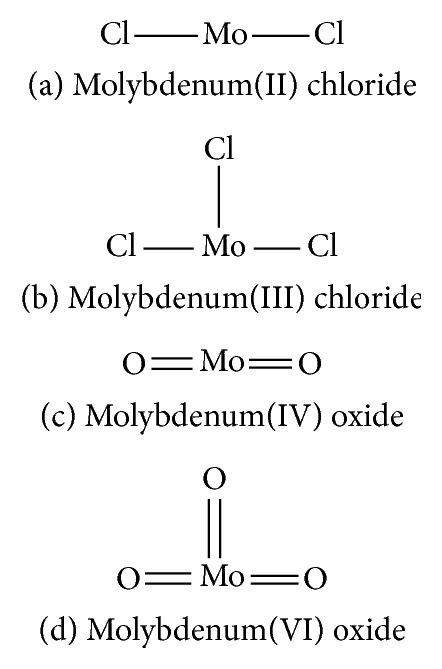
Inorganic molybdenum compounds. (a) Molybdenum(II) chloride. (b) Molybdenum(III) chloride. (c) Molybdenum(IV) oxide. (d) Molybdenum(VI) oxide.
Organomolybdenum compounds can be referred to coordinated molybdenum compounds in various oxidation states. They are potent anticancer and antimicrobial agents [8, 9, 17–19, 24–26]. According to Nair et al., biological applications of molybdenum complexes were due to the ability of incorporated ligands to chelate with trace metal ion (molybdenum ion), their rare action mechanisms, and capability to produce a high amount of harmful reactive oxygen species (ROS) which can interrupt the redox balance of a system leading to increase in deoxyribonucleic acid (DNA) damage, DNA protein cross-linked formation, lipid peroxidation, cellular toxicity, and/or wrong initiation of cellular signaling paths [8]. Results from their findings confirmed that Mo(V) had more cytotoxic activities than Mo(VI). On another note, Meléndez indicated that metallocenes are target specific drugs for cancer treatment. A metallocene (Figure 2) is an organometallic compound, which usually consists of two cyclopentadienyl anions (C5H5−, with Cp abbreviation) bound to a central metal (M) in the oxidation state, to yield (C5H5)2M [27]. Ndagi et al. [28] and Martin et al. [29] stated the lower attention on metallocenes (molybdocene, niobocene, vanadocene, and zirconocene) in perspective of cytotoxic impacts on cancer cell lines as compared to metal-based compounds. Marin et al. suggested extra optimization of these metallocenes for them to be used as anticancer agents in chemotherapy [29]. Molybdocene is a metallocene with a molybdenum atom. Molybdocene dichloride is the organomolybdenum which has the formula of (η5-C5H5)2MoCl2 (Figure 3). The International Union of Pure and Applied Chemistry (IUPAC) name is dichlorobismolybdenum(IV). Molybdocene dichloride had been reported to display anticancer activities, but there was a challenge of no yield of valuable compounds at the clinical stage [20]. Other organomolybdenum compounds are molybdocene dihydride, (mesitylene)molybdenum tricarbonyl, and cycloheptatrienenmolybdenum tricarbonyl, as shown in Figures 4–6, respectively.
Figure 2.
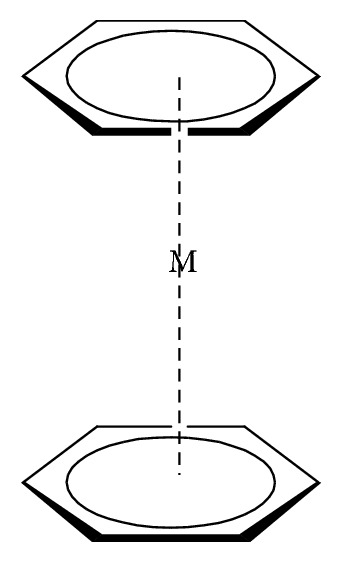
Metallocene.
Figure 3.
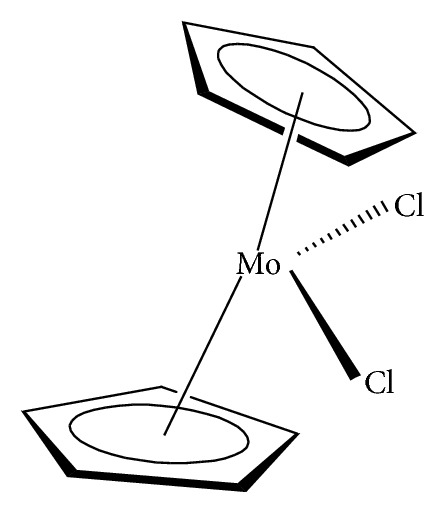
Dichlorobismolybdenum(IV) (molybdocene dichloride).
Figure 4.
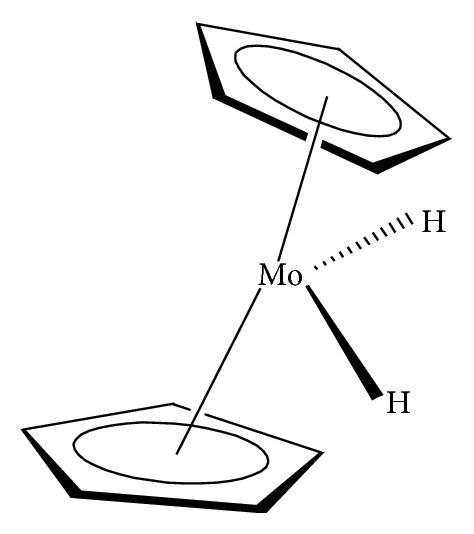
Molybdocene dihydride.
Figure 5.
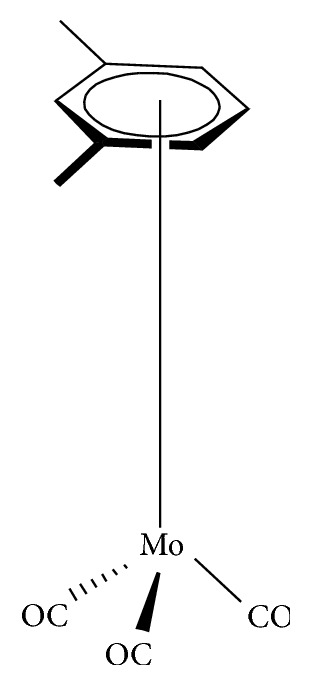
(Mesitylene)molybdenum tricarbonyl.
Figure 6.
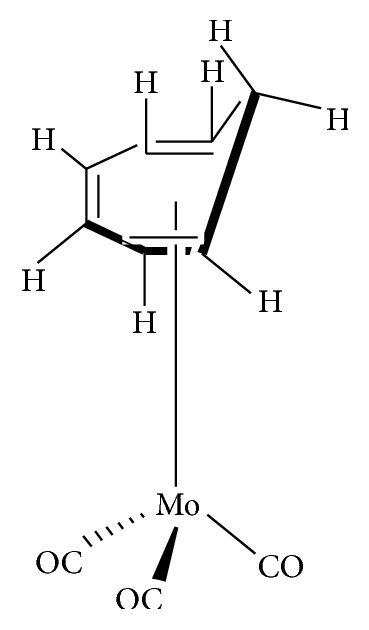
Cycloheptatrienenmolybdenum tricarbonyl.
3. Nanotechnology
The cancer disease with its proliferation has limited current chemotherapy. Nanotechnology in the form of nanomaterials makes available a possible alternative for cancer treatment [30–39]. Tran et al. examined the cytotoxicity of molybdenum trioxide (MoO3) nanoplates to disturbing breast cancer IMCF-7 cells by evaluating morphological variations and executing Western blot and flow cytometry analyses [40]. Their results proposed that MoO3 introduction encouraged apoptosis and produces reactive oxygen species (ROS) in IMCF-7 cells, thereby revealing the use of MoO3 for treating metastatic cancer cells in order to promote cancer therapy.
Molybdenum trioxide (molybdenum(VI) oxide; MoO3) nanoparticles were reported to be one of the metal nanoparticles to possess least toxicity [40, 41]. Apart from the roles molybdenum trioxide plays as an essential trace element, other roles are fuel cells [42], antimicrobial paints [43], potent antimicrobial agents [44], and membrane stress creation for microorganisms. Nanotechnology has transformed therapeutic approaches by improving the bioavailability, biodistribution, pharmacokinetics, stability, and targeted delivery to the required site, thereby decreasing toxicity, as well as reducing side effects [45, 46]. On the other hand, the main challenge encountered with the nanoparticles therapeutics is to overcome the improved permeability, retention effect, and targeted delivery to take full advantage of the effectiveness [46–49]. Among the nanotechnology carrier systems, electrospun nanofibres are developing to be a beneficial drug delivery system since they have massive packing capacity and targeted drug delivery [50, 51]. Recognition of an appropriate carrier system for the NPs would lessen various challenges. In this way, MoO3 could be used to fabricate a nanofibrous support with appropriate physicochemical properties to purposefully target cancer cells in order to overcome the challenges and lessen dosage and side effects [52–54].
For the past ten years, there had been an improved interest in the direction of low-dimensional nanostructured materials. Several efforts have been made to synthesize and apply one-dimensional (1D) nanomaterials based on transition metals [40, 55–58]. In this perspective, the 1D morphologies (for example, nanoflakes, nanorods, nanosheets, nanotubes, and nanowires) have been anticipated to display improved characteristics, making them appropriate for a wide range of uses, such as biofuel cells, bioimaging, biosensors, drug delivery, electrochromic devices, field emitters, light-emitting diodes, nanobioelectronics, nanogenerators, and supercapacitors [40, 55–62]. Recently, 1D nanostructured metal oxides in the direction of biosensors for cancer diagnostics aroused abundant interest [63]. Biosensors are used as optional technique for the most prevalent cancer, breast cancer, because it offers affordable cost, high sensitivity, least sample volume condition, and point-of-precaution diagnostics [64, 65]. Biomarkers have been recognised to perform a noticeable role as they are linked with the diagnosis and prognosis of a certain disease for biosensors development as points-of-care strategies [66, 67]. Numerous traditional tissue biomarkers, such as estrogen receptor (ER), progesterone receptor (PR), and human epithelial growth factor receptor-2 (HER-2), can be linked with the presence of breast cancer [68–70]. Among the three mentioned receptors, HER-2 is the only hopeful biomarker for breast cancer diagnosis [71, 72]. Human epithelial growth factor receptor-2 is a tyrosine kinase receptor which encrypts between 185 and 210 kDa protein located on chromosome 17 and is made up of cytoplasmic domain (CD), transmembrane domain (TD), and extracellular domain (ECD) [73–76]. It discharges its ECD into the serum section on above manifestation during the occurrence of breast cancer [77–81]. The limit concentration of HER-2 in serum sample of a breast cancer patient can be >15 μg/mL [82–84]. As a result, monitoring HER-2 in serum can produce essential facts relating to tumour growth of a breast cancer patient. Recently, Gohring et al. established an optical-based biosensor based on optofluidic ring resonator for HER-2 detection [85].
Biomarkers perform important functions in the administration of patients with disturbing breast cancer [69, 86, 87]. Duffy et al. advocated that all laboratories assessing biomarkers for patient administration ought to use analytically and clinically certified assays, take part in external quality assurance programs, have recognized assay acceptance and rejection standards, implement regular audits, and be recognized by a suitable organization [69].
Weaver et al. stated that clinical breast care and breast cancer interrelated researches were influenced by imaging biomarkers [88]. They further stated that a previous incorporation of breast imaging with interrelated biomedical fields and the formation of large joint and shared databases of clinical, molecular, and imaging biomarkers would tolerate the field to continue controlling breast cancer care and research.
The aforementioned traditional biomarkers have various limitations, such as inability to arrest the spatial heterogeneity of breast cancer, and selected tissue cells during therapy might change the principal genotype and cause resistant treatment [89–91]. These can be overcome by molecular imaging biomarkers [86, 92].
The use of molybdenum-based compounds as anticancer agent against oesophageal and breast cancer diseases is shown in Figure 7.
Figure 7.
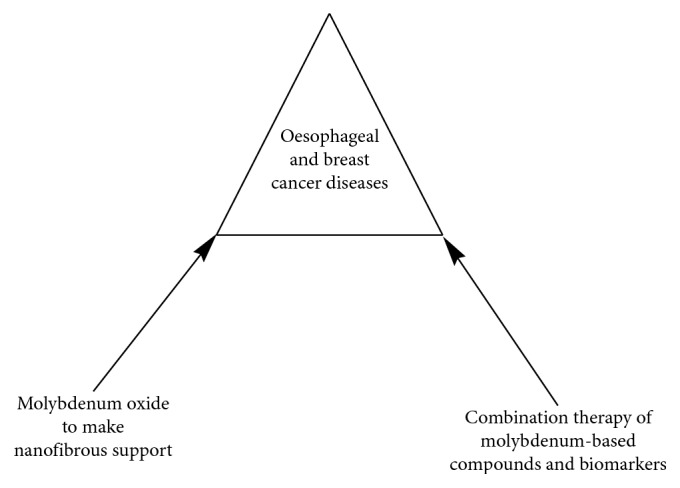
Use of molybdenum-based compounds as anticancer agent against oesophageal and breast cancer diseases.
3.1. Combination Therapy of Anticancer Agents and Biomarkers
According to Vivot et al., anticancer agents were progressively combined with a biomarker to decide if the prospective patient could benefit from the drug [93]. Two-thirds of Food and Drug Administration- (FDA-) endorsed anticancer agents require predictive biomarker testing to be based on clinical development restricted to biomarker-positive patients. From clinical evidence, they established that only limited cases of biomarker-negative patients would not benefit from treatment. They concluded that an absence of collective proof of clinical usefulness of biomarker testing for predictive biomarkers was identified as a challenge to precision medicine [93].
3.2. Combination Therapy of Metal-Based Nanoparticles (NPs) and Biomarkers
Metal-based nanoparticles (NPs) of various forms and magnitudes had been studied for their functions in diagnosis and the drug delivery system [28]. Combination of large drug dose is permissible on metal-based NPs because of the large surface area to volume ratio [28]. In order to increase the exactness in the diagnosis of cancers, Ndagi et al. studied different types of very accurate and very sensitive NP-based imaging platforms because these platforms are more advantageous compared with other agents [28]. These NPs can be functionalized to target accurately cancer and tumour cells, allowing the imaging and healing agents to be accurately delivered into these cells. Nanoparticles can be multifunctional. They show magnetic, optical, and structural properties which are deficient in a single molecule [28]. Ndagi et al. further stated that information on tumour-specific receptors, homing proteins, enzymes, and biomarkers are essential because tumour-specific targeting is attained by combining the NPs' surface with a molecule or biomarker attached to the tumour-cell receptor [28]. Synergistic effect can be attained by combining multifunctional NPs with different biomarkers and loading them with multidrug regimens, thereby decreasing the drug portion in the combination [94–96].
The use of nanostructured metal oxides and nanostructured transition metal oxides (nTMOs) to the development of an effective biosensing transform has motivated much interest [57]. In the midst of the nTMOs, nanostructured nMoO3 has been anticipated to have exceptional features, such as electrochemical activity, effective electrical properties, optical clearness, photochemical stability, and surface charge properties.
Augustine et al. established the constriction of label-free immunosensor biocompatible 1D nMoO3 biosensor for breast cancer biomarker detection [57]. Their results from electrochemical studies gave a wide linear detection range and excellent sensitivity. They ascribed the improved sensitivity of the biosensor to the mesoporous performance and high electrocatalytic activity of 1D MoO3, which offered high aspect ratio for enhanced bimolecular loading.
3.3. Selected Targets in Anticancer Drug Design and Molybdenum-Based Compounds
The notion of selecting targets brings hope in designing therapeutics which would selectively target cancer cells, leaving healthy cells intact. Molybdenum-based compounds with different functionalities can be developed and designed to have higher anticancer activities than cisplatin (platinum-based compound). The recent areas in cytotoxic drug design are targeting of sugar, targeting of steroids, targeting of bile acid, targeting of related steroids, targeting of folate, and targeting of peptide (Figure 8).
Figure 8.
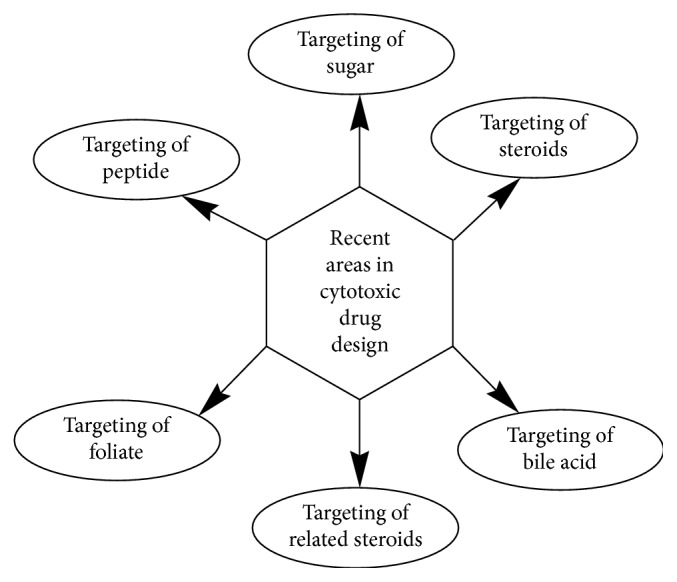
Selected targets in recent areas in cytotoxic drug design.
3.3.1. Targeting of Sugar
Cancer cells need sugar (glucose) to survive. With this fact, biosugar facet could be used for drug targeting due to improved uptake of glucose by cancer cells [28, 97]. According to Johnstone et al.'s example, 2αα, 3-diaminosugars coordination compounds equivalent to oxaliplatin (functionalized cisplatin) were studied and discovered to have potential activity [28, 98]. Other prospective platinum-based compounds coordinated with glucose were also studied and discovered to have hopeful outcomes.
3.3.2. Targeting for Steroid
Estrogen and testosterone are two of the several sex hormones which play important roles in drug targeting. They do this by combining steroidal units with nonliving group ligand. Ndagi et al. cited an example of estrogen receptor (ER), as a recognized drug target due to its extraordinary manifestation of protein on the faces of these cancer cells, which is predominantly, in breast cancer [28, 98]. Progress made in the research in this field led to the discovery of another conspicuous ER, labelled as ERα, while the previous ER was labelled as ERβ [99]. Similarly, as estrogen targets platinum to the cancer cells displaying ER receptors, testosterone could target platinum to cancer cells displaying androgen receptor (AR) in order to increase deoxyribonucleic acid (DNA) and enhance the anticancer activity [28, 98].
3.3.3. Targeting of Bile Acid
Bile acids are natural steroids and have been combined with platinum coordination compounds [28, 98]. For instance, a bile acid coordinated with dicarboxylate motif bound to a cisplatin piece was discovered to be an orally administered anticancer agent [28, 98].
3.3.4. Targeting of Related Steroids
The translocator protein (TSPO) generally known as peripheral benzodiazepine regulates cholesterol transport and steroid syntheses [28, 100]. The protein is an essential target in cancer treatment due to its overexpression in various tumour cells [28, 100]. Ligated platinum(II) coordination compounds with bidentate thiazolylimidazopyridine were reported to interact intensely with the receptor [28, 100].
3.3.5. Targeting of Folate
Folate is an essential carbon source for various cellular pathways, comprising DNA, ribonucleic acid (RNA), protein methylation, and DNA synthesis [101]. Improved folate uptake causes rapid cancer cell growth. This folate could be used as a baseline for drug targeting [101]. On another note, there is a control to the use of folate as a targeting agent of platinum complex. Previous study revealed that interaction of cisplatin with cellular folates would not be able to function as a cytosolic agent in a way similar to cisplatin [102]. In this regard, all researchers' hands are on deck to find the potential of folate in selecting drug targeting.
3.3.6. Targeting of Peptide
Combination of platinum(II) complexes with the peptide results in the platination of complexes with anticancer activity [28, 101, 103–105]. Several platinum complexes combined with peptides have been screened against cancer cell lines, and a realistic number of them showed promising anticancer activities.
4. Conclusion and Future Direction
The use of molybdenum-based compounds as anticancer agents has been enhanced with the introduction of nanotechnology in the areas of nanofibrous support, combination therapy, and biomarkers. Selected targets are potentials in recent areas of anticancer drug design.
Future direction will entail the use of molybdenum-based compounds to substitute platinum coordination compounds in selecting targets in cytotoxic drug design.
Acknowledgments
The authors appreciate Govan Mbeki Research and Development Centre (GMRDC) for the financial assistance.
Contributor Information
Ayodele T. Odularu, Email: 201106223@ufh.ac.za.
Peter A. Ajibade, Email: ajibadep@ukzn.ac.za.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
- 1.Baile M. B., Kolhe N. S., Deotarse P. P., Jäin A. S., Kulkarni A. A. Metal ion complex-potential anticancer drug: a review. International Journal of Pharmaceutical Sciences Review and Research. 2015;4:59–66. [Google Scholar]
- 2.Bray F., Ferlay J., Soerjomataram I., Siegel R. L., Torre L. A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 3.Ferlay J., Colombet M., Soerjomataram I., et al. Cancer incidence and mortality patterns in europe: estimates for 40 countries and 25 major cancers in 2018. European Journal of Cancer. 2018;103:356–387. doi: 10.1016/j.ejca.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 4.Ferlay J., Colombet M., Soerjomataram I., et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. International Journal of Cancer. 2018;144 doi: 10.1002/ijc.31937. [DOI] [PubMed] [Google Scholar]
- 5.Bray F., Jemal A., Grey N., Ferlay J., Forman D. Global cancer transitions according to the human development index (2008–2030): a population-based study. The Lancet Oncology. 2012;13(8):790–801. doi: 10.1016/s1470-2045(12)70211-5. [DOI] [PubMed] [Google Scholar]
- 6.Jemal A., Bray F., Center M. M., Ferlay J., Ward E., Forman D. Global cancer statistics. CA: A Cancer Journal for Clinicians. 2011;61(2):69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 7.Bhattacharya P. T., Misra S. R., Hussain M. Nutritional aspects of essential trace elements in oral health and disease: an extensive review. Scientifica. 2016;2016:12. doi: 10.1155/2016/5464373.5464373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nair M. L. H., Thankamani D. Synthesis and characterization of oxomolybdenum (V) and dioxomolybdenum (VI) complexes with schiff base derived from isonicotinoylhydrazide. Indian Journal of Chemistry. 2009;48A:1212–1218. [Google Scholar]
- 9.Patil S. K., Naik V. M., Mallur N. B. Synthesis, spectral and antibacterial studies of oxomolybdenum(V) and dioxomolybdenum(VI) complexes with 2-imidazolylmercaptoacetohydrazone. Der Pharma Chemica. 2012;4:1812–1818. [Google Scholar]
- 10.Vrdolijak V., Prugovečki B., Matković-Ćalogović D., Novak P., Cindrić M. Synthesis and characterization of dinuclear oxomolybdenum(V) complexes with thienyl carboxylate ligands. Inorganica Chimica Acta. 2010;363:3516–3522. [Google Scholar]
- 11.Fisher B., Dubler E., Meienberger M., Hegetschweiler K. Molybdenum complexes of the anticancer drug 6-mercaptopurine. Inorganica Chimica Acta. 1998;279(2):136–143. doi: 10.1016/s0020-1693(98)00108-x. [DOI] [Google Scholar]
- 12.Hille R., Nishino T., Bittner F. Molybdenum enzymes in higher organisms. Coordination Chemistry Reviews. 2011;255(9-10):1179–1205. doi: 10.1016/j.ccr.2010.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chan P., Herbert R. A., Roycroft J. H., et al. Lung tumor induction by inhalation exposure to molybdenum trioxide in rats and mice. Toxicological Sciences. 1998;45(1):58–65. doi: 10.1006/toxs.1998.2497. [DOI] [PubMed] [Google Scholar]
- 14.Dmedley P. L., Kinniburgh D. G. Molybdenum in natural waters: a review of occurrence, distributions and controls. Applied Geochemistry. 2017;84:387–432. doi: 10.1016/j.apgeochem.2017.05.008. [DOI] [Google Scholar]
- 15.Komada H., Kise Y., Nakagawa M., Yamamura M., Hioki K., Yamamoto M. Effect of dietary molybdenum on esophageal carcinogenesis in rats induced by N-methyl-N-benzylnitrosamine. Cancer Research. 1990;50:2418–2422. [PubMed] [Google Scholar]
- 16.Nouri M., Chalian H., Bahman A., et al. Nail molybdenum and zinc contents in populations with low and moderate incidence of esophageal cancer. Archives of Iranian Medicine. 2008;11:392–396. [PubMed] [Google Scholar]
- 17.Saraswati K., Kant R. Synthesis, characterization and biological activity of some molybdenum (VI) complexes. Der Pharma Chemica. 2013;5:347–356. [Google Scholar]
- 18.Pereira C. C. L., Diogo C. V., Burgeiro A., et al. Complex Formation between Heptakis(2,6-di-O-methyl)-β-cyclodextrin and Cyclopentadienyl Molybdenum(II) Dicarbonyl Complexes: structural Studies and Cytotoxicity Evaluations. Organometallics. 2008;27(19):4948–4956. doi: 10.1021/om800413w. [DOI] [Google Scholar]
- 19.Köpf-Maier P., Köpf H. Organometallic titanium, vanadium, niobium, molybdenum and rhenium complexes—early transition metal antitumour drugs. In: Fricker S. P., editor. Metal Compounds in Cancer Therapy. Dordrecht, Netherlands: Springer; 1994. pp. 109–146. [DOI] [Google Scholar]
- 20.Waem J. B., Dillon C. T., Harding M. M. Organometallic anticancer agents: cellular uptake and cytotoxicity studies on thiol derivatives of the anticancer agent. Medicinal Chemistry. 2005;48:2093–2099. doi: 10.1021/jm049585o. [DOI] [PubMed] [Google Scholar]
- 21.Feng J., Lu X., Wang G., Du S., Cheng Y. The synthesis and characterizations of molybdenum(VI) complexes with catechol and 2, 3-dihydroxynaphthalene, and the structure-effect relationship in their in vitro anticancer activities. Dalton Trans. 2012;41:8657–8702. doi: 10.1039/c2dt30395g. [DOI] [PubMed] [Google Scholar]
- 22.Crichton R. R. Biological Inorganic Chemistry. Vol. 17. Oxford, UK: Elsevier; 2008. Molybdenum, tungsten, vanadium and chromium; pp. 279–296. [DOI] [Google Scholar]
- 23.Lunk H., Harti H. Discovery, properties and applications of molybdenum and its compounds. Chem Texts. 2017;3(3) doi: 10.1007/s40828-017-0048-6. [DOI] [Google Scholar]
- 24.Haddad S. F., Ali B. F., Al-Far R. H., Dawoud J. N., Alomari M. I. Density functional theory calculations of pentabromidooxomolybdate(V) anion with 2,2′-bipyridinium cation: comparison between the calculated geometry and the crystal structure determination at 293 and 90K. Polyhedron. 2010;29(3):1109–1115. doi: 10.1016/j.poly.2009.11.021. [DOI] [Google Scholar]
- 25.Quintal S., Matos J., Fonseca I., et al. Synthesis and properties of new trinuclear Mo(II) complexes containing imidazole and benzimidazole ferrocene units. Inorganica Chimica Acta. 2008;361(6):1584–1596. doi: 10.1016/j.ica.2007.05.039. [DOI] [Google Scholar]
- 26.Gretarsdóttir J. M., Bobersky S., Metzler-Nolte N., Suman S. G. Cytotoxicity studies of water soluble coordination compounds with a [Mo2O2S2]2+ core. Journal of Inorganic Biochemistry. 2016;160:166–171. doi: 10.1016/j.jinorgbio.2016.01.020. [DOI] [PubMed] [Google Scholar]
- 27.Meléndez E. Metallocenes as target specific drugs for cancer treatment. Inorganica Chimica Acta. 2012;393:36–52. doi: 10.1016/j.ica.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ndagi U., Mhlongo N., Soliman M. Metal complexes in cancer therapy – an update from drug design perspective. Drug Design, Development and Therapy. 2017;11:599–616. doi: 10.2147/dddt.s119488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martin P., Marques M., Coito L., Pombeiro A. J., Fernandes A. R. Organometallic compounds in cancer therapy: past lessons and future decisions. Anticancer Agents Med. Chem. 2014;14(9):1199–1212. doi: 10.2174/1871520614666140829124925. [DOI] [PubMed] [Google Scholar]
- 30.Bae K. H., Chung H. J., Park T. G. Nanomaterials for cancer therapy and imaging. Molecules and Cells. 2011;31(4):295–302. doi: 10.1007/s10059-011-0051-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gmeiner W. H., Ghosh S. Nanotechnology for cancer treatment. Nanotechnology Reviews. 2015;3(2):111–122. doi: 10.1515/ntrev-2013-0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Markman J. L., Rekechenetskiy A., Holler E., Ljubimova J. Y. Nanomedicine therapeutic approaches to overcome cancer drug resistance. Advanced Drug Delivery Reviews. 2013;65(13-14):1866–1879. doi: 10.1016/j.addr.2013.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kirtane A. R., Kalscheuer S. M., Panyam J. Exploiting nanotechnology to overcome tumor drug resistance: challenges and opportunities. Advanced Drug Delivery Reviews. 2013;65(13-14):1731–1747. doi: 10.1016/j.addr.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hare J. I., Lammers T., Ashford M. B., Puri S., Storm G., Barry S. T. Challenges and strategies in anti-cancer nanomedicine development: an industry perspective. Advanced Drug Delivery Reviews. 2017;108:25–38. doi: 10.1016/j.addr.2016.04.025. [DOI] [PubMed] [Google Scholar]
- 35.Livney Y. D., Assaraf Y. G. Rationally designed nanovehicles to overcome cancer chemoresistance. Advanced Drug Delivery Reviews. 2013;65(13-14):1716–1730. doi: 10.1016/j.addr.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 36.Minko T. Nanotechnology and drug resistance. Advanced Drug Delivery Reviews. 2013;65(13-14):1665–1666. doi: 10.1016/j.addr.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 37.Zhao Y., Alakhova D. Y., Kabanov A. V. Can nanomedicines kill cancer stem cells? Advanced Drug Delivery Reviews. 2013;65(13-14):1763–1783. doi: 10.1016/j.addr.2013.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Iyer A. K., Singh A., Ganta S., Amiji M. M. Role of integrated cancer nanomedicine in overcoming drug resistance. Advanced Drug Delivery Reviews. 2013;65:1880–1895. doi: 10.1016/j.addr.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 39.Minko T., Rodriguez-Rodriguez L., Pozharov V. Nanotechnology approaches for personalized treatment of multiple resistant carriers. Advanced Drug Delivery Reviews. 2013;65(13-14):1784–1802. doi: 10.1016/j.addr.2013.09.017. [DOI] [PubMed] [Google Scholar]
- 40.Tran T. A., Krishnamoorthy K., Song Y. W., Cho S. K., Kim S. J. Toxicity of nano molybdenum trioxide toward invasive brest cancer cells. ACS Applied Materials & Interfaces. 2014;6(4):2980–2986. doi: 10.1021/am405586d. [DOI] [PubMed] [Google Scholar]
- 41.Braydich-Stolle L., Hussain S., Schlager J. J., Hofmann M.-C. In vitro cytotoxicity of nanoparticles in mammalian germline stem cells. Toxicological Sciences. 2005;88(2):412–419. doi: 10.1093/toxsci/kfi256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yamashita T., Yokoyama H. Molybdenum anode: a novel electrode for enhanced power generation in microbial fuel cells, identified via extensive screening of metal electrodes. Biotechnology for Biofuels. 2018;11(1):1–13. doi: 10.1186/s13068-018-1046-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Krishnamoorthy K., Premanathan M., Veerapandian M., Kim S. J. Nanostructured molybdenum oxide-based antibacterial paint: effective growth inhibition of various pathogenic bacteria. Nanotechnology. 2014;25(31) doi: 10.1088/0957-4484/25/31/315101. [DOI] [PubMed] [Google Scholar]
- 44.Perreault F., De Faria A. F., Nejati S., Elimelech M. Antimicrobial properties of graphene oxide nanosheets: why size matters. ACS Nano. 2015;9(7):7226–7236. doi: 10.1021/acsnano.5b02067. [DOI] [PubMed] [Google Scholar]
- 45.Gunasekaran T., Haile T., Nigusse T., Dhanaraju M. D. Nanotechnology: an effective tool for enhancing bioavailability and bioactivity of phytomedicine. Asian Pacific Journal of Tropical Biomedicine. 2014;4:51–57. doi: 10.12980/apjtb.4.2014c980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Din F. U., Aman W., Ullah I., et al. Effective use of nanocarriers as drug delivery systems for the treatment of selected tumors. International Journal of Nanomedicine. 2017;12:7291–7309. doi: 10.2147/ijn.s146315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nakamura Y., Mochida A., Choyke P. L., Kobayashi H. Nanodrug delivery: is the enhanced permeability and retention effect sufficient for curing cancer? Bioconjugate Chemistry. 2016;27(10):2225–2238. doi: 10.1021/acs.bioconjchem.6b00437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Babu A., Templeton A. K., Munshi A., Ramesh R. Nanoparticle-based drug delivery for therapy of lung cancer: progress and challenges. Journal of Nanomaterials. 2013;2013:11. doi: 10.1155/2013/863951.863951 [DOI] [Google Scholar]
- 49.Rahman M. A., Shin D. M. CCR 20th anniversary commentary: prospects and challenges of therapeutic nanoparticles in cancer. Clinical Cancer Research. 2015;21(20):4499–4501. doi: 10.1158/1078-0432.ccr-14-3126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Golberg M., Langer R., Jia X. Nanostructured materials for applications in drug delivery and tissue engineering. Biomaterials Science, Polymer Edition. 2007;18(3):241–268. doi: 10.1163/156856207779996931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Weng L., Xie J. Smart electrospun nanofibers for controlled drug release: recent advances and new perspectives. Current Pharmaceutical Design. 2015;21(15):1944–1959. doi: 10.2174/1381612821666150302151959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mondal K. Recent advances in the synthesis of metal oxide nanofibres and their environmental remediation applications. Invent. 2017;2(2):1–29. doi: 10.3390/inventions2020009. [DOI] [Google Scholar]
- 53.Li J., Zhang Q., Xu M., Wu C., Li P. Antimicrobial efficacy and cell adhesion inhibition of in situ synthesized ZnO nanoparticles/polyvinyl alcohol nanofibrous membranes. Advances in Condensed Matter Physics. 2016;2016:9. doi: 10.1155/2016/6394124.6394124 [DOI] [Google Scholar]
- 54.Janani I., Lakra R., Kiran M. S., Korrapati P. S. Selectivity and sensitivity of molybdenum oxide-polycaprolactone nanofiber composites on skin cancer: preliminary in-vitro and in-vivo implications. Journal of Trace Elements in Medicine and Biology. 2018;49:60–71. doi: 10.1016/j.jtemb.2018.04.033. [DOI] [PubMed] [Google Scholar]
- 55.Song G., Shen J., Jiang F., et al. Hydrophilic molybdenum oxide nanomaterials with controlled morphology and strong plasmonic absorption for photothermal ablation of cancer cells. ACS Applied Materials & Interfaces. 2014;6(6):3915–3922. doi: 10.1021/am4050184. [DOI] [PubMed] [Google Scholar]
- 56.Hanhua Z., Andrew J. B., Andrey V. P., Dunbar R. K. One-dimensional square-and ladder-type architectures incorporating octacyanometallates of molybdenum(V) and tungsten(V) Polyhedron. 2013;64:321–327. doi: 10.1016/j.poly.2013.06.006. [DOI] [Google Scholar]
- 57.Augustine S., Joshi A. G., Yadav B. K., et al. An emerging nanostructured molybdenum trioxide-based biocompatible sensor platform for breast cancer biomarker detection. MRS Communications. 2018;8(3):668–679. doi: 10.1557/mrc.2018.182. [DOI] [Google Scholar]
- 58.Pandey S., Sharma K. H., Sharma A. K., Nerthigan Y., Wu H. Comparative photothermal performance among various sub-stoichiometric 2D oxygen-deficient molybdenum oxide nanoflakes and in vivo toxicity. Chemistry—A European Journal. 2018;24(29):7417–7427. doi: 10.1002/chem.201705734. [DOI] [PubMed] [Google Scholar]
- 59.Liu W., Li X., Li W., et al. Highly stable molybdenum dioxide nanoparticles with strong plasmon resonance are promising in photothermal cancer therapy. Biomaterials. 2018;163:43–54. doi: 10.1016/j.biomaterials.2018.02.021. [DOI] [PubMed] [Google Scholar]
- 60.Bao T., Yin W., Zheng X., et al. One-pot synthesis of PEGylated plasmonic MoO3−x hollow nanospheres for photoacoustic imaging guided chemo-photothermal combinational therapy of cancer. Biomaterials. 2016;76:11–24. doi: 10.1016/j.biomaterials.2015.10.048. [DOI] [PubMed] [Google Scholar]
- 61.Pultz B. D-A., Da Luz F. A. C., De Faria P. R., Oliveira A. P. L., De Araújo R. A., Silver M. J. R. Far beyond the usual biomarkers in breast cancer: a review. Journal of Cancer. 2014;5(7):559–571. doi: 10.7150/jca.8925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Besutti G., Iotti V., Giorgi Rossi P. Molecular imaging biomarkers for breast cancer risk and personalized screening. Translational Cancer Research. 2018;7(5):1319–1325. doi: 10.21037/tcr.2018.09.04. [DOI] [Google Scholar]
- 63.Hahm J.-I. Biomedical detection via macro- and nano-sensors fabricated with metallic and semiconducting oxides. Journal of Biomedical Nanotechnology. 2013;9(1):1–25. doi: 10.1166/jbn.2013.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bohunicky B., Mousa S. A. Biosensors: the new wave in cancer diagnosis. Nanotechnology, Science and Applications. 2011;4:1–10. doi: 10.2147/NSA.S13465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Choi Y.-E., Kwak J.-W., Park J. W. Nanotechnology for early cancer detection. Sensors. 2010;10(1):428–455. doi: 10.3390/s100100428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Liu X., Jiang H. Constructions and potential applications of biosensors for protein in clinical laboratory diagnosis. Sensors. 2017;17(12):1–23. doi: 10.3390/s17122805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Doria G., Conde J., Veigas B., et al. Noble metal nanoparticles for biosensing applications. Sensors. 2012;12(2):1657–1687. doi: 10.3390/s120201657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Finn R. S., Press M. F., Dering J., et al. Estrogen receptor, progesterone receptor, human epidermal growth factor receptor 2 (HER2), and epidermal growth factor receptor expression and benefit from lapatinib in a randomized trial of paclitaxel with lapatinib or placebo as first-line treatment in HER2-negative or unknown metastatic breast cancer. Journal of Clinical Oncology. 2009;27(24):3908–3915. doi: 10.1200/jco.2008.18.1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Duffy M. J., Harbeck N., Nap M., et al. Clinical use of biomarkers in breast cancer: updated guidelines from the European group on tumor markers (EGTM) European Journal of Cancer. 2017;75:284–298. doi: 10.1016/j.ejca.2017.01.017. [DOI] [PubMed] [Google Scholar]
- 70.Vohra P., Buelow B., Chen Y.-Y., et al. Estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 expression in breast cancer FNA cell blocks and paired histologic specimens: a large retrospective study. Cancer Cytopathology. 2016;124(11):828–835. doi: 10.1002/cncy.21745. [DOI] [PubMed] [Google Scholar]
- 71.Hicks D. G., Kulkarni S. HER2+ breast cancer. American Journal of Clinical Pathology. 2008;129(2):263–273. doi: 10.1309/99ae032r9fm8wnd1. [DOI] [PubMed] [Google Scholar]
- 72.Barron J. J., Cziraky M. J., Weisman T., Hicks D. G. HERS testing and subsequent trastuzumab treatment for breast cancer in a managed care environment. The Oncologist. 2009;14:760–768. doi: 10.1634/theoncologist.2008-0288. [DOI] [PubMed] [Google Scholar]
- 73.Wieduwilt M. J., Moasser M. M. The epidermal growth factor receptor family: biology driving targeted therapeutics. Cellular and Molecular Life Sciences. 2008;65(10):1566–1584. doi: 10.1007/s00018-008-7440-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Manash K. P., Anup K. M. Tyrosine kinase-role and significance in cancer. International Journal of Medical Sciences. 2004;1:101–115. doi: 10.7150/ijms.1.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tai W., Mahato R., Cheng K. The role of HER2 in cancer therapy and targeted drug delivery. Journal of Controlled Release. 2010;146(3):264–275. doi: 10.1016/j.jconrel.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Iqbal N., Iqbal N. Human epidermal growth factor receptor 2 (her2) in cancers: overexpression and therapeutic implications. Molecular Biology International. 2014;2014:9. doi: 10.1155/2014/852748.852748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shukla S., Singh R. K., Pathania O. P., Jain M. Evaluation of HER2/neu oncoprotein in serum & tissue samples of women with breast cancer. Indian Journal of Medical Research. 2016;143(7):S52–S58. doi: 10.4103/0971-5916.191769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fehm T., Becker S., Duerr-Stoerzer S., et al. Determination of HERS status using both serum hers levels and circulating tumor cells in patients with recurrent breast cancer whose primary tumor was hers negative or of unknown hers status. Breast Cancer Research. 2007;9(5):1–8. doi: 10.1186/bcr1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wulfing P., Borchard J., Buerger H., et al. HER2-positive circulating tumor cells indicate poor clinical outcome in stage i to iii breast cancer patients. Clinical Cancer Research. 2006;12(6):1715–1720. doi: 10.1158/1078-0432.ccr-05-2087. [DOI] [PubMed] [Google Scholar]
- 80.Pestrin M., Bessi S., Galardi F., et al. Correlation of HER2 status between primary tumors and corresponding circulating tumor cells in advanced breast cancer patients. Breast Cancer Research and Treatment. 2009;118(3):523–530. doi: 10.1007/s10549-009-0461-7. [DOI] [PubMed] [Google Scholar]
- 81.Carney W. P., Leitzel K., Ali S., Neumann R., Lipton A. HER-2/neu diagnostics in breast cancer. Breast Cancer Research. 2007;9(3):1–11. doi: 10.1186/bcr1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Esteva F. J., Cheli C. D., Fritsche H., et al. Clinical utility of serum HER2/neu in monitoring and prediction of progression-free survival in metastatic breast cancer patients treated with trastuzumab-based therapies. Breast Cancer Research. 2005;7(4):R436–R443. doi: 10.1186/bcr1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Qian T., Xinyi W., Qingyuan L., et al. Portable detection of serum HER-2 in breast cancer by a pressure-based platform. Analytical and Bioanalytical Chemistry. 2018;410(28):7489–7498. doi: 10.1007/s00216-018-1364-4. [DOI] [PubMed] [Google Scholar]
- 84.Lee M. H., Jung S., Kang S. H., et al. The significance of serum HER2 levels at diagnosis on intrinsic subtype-specific outcome of operable breast cancer patients. PLos One. 2016;11(10):1–11. doi: 10.1371/journal.pone.0163370.e0163370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gohring J. T., Dale P. S., Dale P. S., Fan X. Detection of HER2 breast cancer biomarker using the opto-fluidic ring resonator biosensor. Sensors and Actuators B: Chemical. 2010;146(1):226–230. doi: 10.1016/j.snb.2010.01.067. [DOI] [Google Scholar]
- 86.Ulaner G. A., Riedl C. C., Dickler M. N., Jhaveri K., Pandit-Taskar N., Weber W. Molecular imaging of biomarkers in breast cancer. Journal of Nuclear Medicine. 2016;57(1):53S–59S. doi: 10.2967/jnumed.115.157909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Patel S. K., Wong A. L., Wong F. L., et al. Inflammatory biomarkers, comorbidity, and neurocognition in women with newly diagnosed breast cancer. JNCI: Journal of the National Cancer Institute. 2015;107(8):1–7. doi: 10.1093/jnci/djv131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Weaver O., Leung J. W. T. Biomarkers and imaging of breast cancer. American Journal of Roentgenology. 2018;210(8):271–278. doi: 10.2214/ajr.17.18708. [DOI] [PubMed] [Google Scholar]
- 89.Rybinski B., Yun K. Addressing intra-tumoral heterogeneity and therapy resistance. Oncotarget. 2016;7(44):72322–72342. doi: 10.18632/oncotarget.11875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Diaz-Cano S. J. Tumor heterogeneity: mechanisms and bases for a reliable application of molecular marker design. International Journal of Molecular Sciences. 2012;13(2):1951–2011. doi: 10.3390/ijms13021951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Feng Y., Spezia M., Huang S., et al. Breast cancer development and progression: risk factors, cancer stem cells, signaling pathways, genomics, and molecular pathogenesis. Genes & Diseases. 2018;5(2):77–106. doi: 10.1016/j.gendis.2018.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.O’Connor C. J. P. B., Aboagye E. O., Waterton J. C. Imaging biomarker roadmap for cancer studies. Nature Reviews Clinical Oncology. 2017;14:169–186. doi: 10.1038/nrclinonc.2016.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Vivot A., Boutron I., Béraud-Chaulet G., Zeitoun J., Ravaud P., Porcher R. Evidence for treatment-by biomarker interaction for FDA approved oncology drugs with required pharmacogenomic biomarker testing. Scientific Reports. 2017;7(1):1–9. doi: 10.1038/s41598-017-07358-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kydd J., Jadia R., Velpurisiva P., Gad A., Paliwal S., Rai P. Targeting strategies for the contribution of cancer using drug delivery systems. Pharm. 2017;9(4):1–26. doi: 10.3390/pharmaceutics9040046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gurunathan S., Kang M. H., Qasim M., Kim J. Nanoparticle-mediated combination therapy: two-in-one approach for cancer. International Journal of Molecular Sciences. 2018;19:1–37. doi: 10.3390/ijms19103264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ventola C. L. The nanomedicine revolution: part 2: current and future clinical applications. P & T: A Peer-Reviewed Journal for Formulary Management. 2012;37(10):582–91. [PMC free article] [PubMed] [Google Scholar]
- 97.Coller H. A. Is cancer a metabolic disease? American Journal of Pathology. 2014;184(1):4–17. doi: 10.1016/j.ajpath.2013.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Johnstone T. C., Suntharalingam K., Lippard S. J. The next generation of platinum drugs: targeted Pt(II) agents, nanoparticle delivery, and Pt(IV) prodrugs. Chemical Reviews. 2016;116(5):3436–3486. doi: 10.1021/acs.chemrev.5b00597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Capper C. P., Rae J. M., Auchus R. J. The metabolism, analysis, and targeting of steroid hormones in breast and prostate cancer. Hormones and Cancer. 2016;7(3):149–164. doi: 10.1007/s12672-016-0259-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Joo H. K., Lee Y. R., Kang G., Choi S., Kim C., Ryoo S. The 18-kDa trans-locator protein inhibits vascular cell adhesion molecule-1 expression via inhibition of mitochondrial reactive oxygen species. Molecules and Cells. 2015;38(12):1064–1070. doi: 10.14348/molcells.2015.0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Crider K. S., Yang T. P., Berry R. J., Bailey L. B. Folate and DNA methylation: a review of molecular mechanisms and the evidence for folate’s role. Advances in Nutrition. 2012;3(1):21–38. doi: 10.3945/an.111.000992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zwicke G. L., Mansoori G. A., Jeffery C. L. Targeting cancer nanotherapeutics. Nanotechnology Reviews. 2012;1:1–11. doi: 10.3402/nano.v3i0.18496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Xiao Y.-F., Jie M.-M., Li B.-S., et al. Peptide-based treatment: a promising cancer therapy. Journal of Immunology Research. 2015;2015:13. doi: 10.1155/2015/761820.761820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Butler J. S., Sadler P. J. Targeted delivery of platinum-based anticancer complexes. Current Opinion in Chemical Biology. 2013;17(2):175–188. doi: 10.1016/j.cbpa.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 105.Wooton C. A., Sanchez-Cano C., Lopez-Clavijo A. F., et al. Sequence-dependent attack on peptides by photoactivated platinum anticancer complexes. Chemical Science. 2018;9(10):2733–2739. doi: 10.1039/c7sc05135b. [DOI] [PMC free article] [PubMed] [Google Scholar]


