Abstract
Purpose:
To assess whether girls with mothers who have had an eating disorder (ED) have greater odds of developing ED symptoms, and whether girls with ED symptoms have greater odds of receiving ED treatment if their mothers have an ED history.
Methods:
Data came from 3,649 females in the Growing Up Today Study. Data were collected via questionnaires that were mailed every 12-24 months from 1996-2013. Girls who reported on ED treatment in 2013 and whose mothers completed a questionnaire in 2004 about maternal and child EDs were included in main analyses. Generalized estimating equations were used.
Results:
Among complete cases, 28.3% of girls reported symptoms meeting criteria for an ED in at least one year and, of these, 12.4% reported receiving treatment. Girls with mothers with ED histories had nearly twice the odds of reporting symptoms of any ED (adjusted odds ratio [aOR]: 1.89; 95% confidence interval [CI]: 1.38-2.60). Girls who reported symptoms meeting criteria for any ED had more than twice the odds of reporting treatment if their mother had an ED history (aOR: 2.23; 95%CI: 1.25-3.99).
Conclusions:
Girls with mothers with an ED history had greater odds of both reporting ED symptoms and receiving ED treatment. Screening both girls and their mothers for current or previous disordered eating may be important for the prevention and detection of ED symptoms. More research is needed to examine reasons for the association between maternal ED history and ED treatment in girls.
Keywords: Eating disorders, treatment, cohort study, population-based, epidemiology
The majority of people with eating disorders (EDs) do not receive treatment for their disorders (1-3). In nationally representative studies, less than 30% of adolescents (3) and less than 50% of adults (1) with a history of an ED reported receiving treatment for their disorders. Low rates of receiving treatment are not unique to the United States. The WHO World Mental Health Survey Initiative, which surveyed over 24,000 adults from 14 countries, observed that fewer than 50% of people with histories of bulimia nervosa (BN) or binge eating disorder (BED) received ED treatment (2). Little is known about factors that are predictive of receiving ED treatment. Some research suggests that detection and treatment may depend on the level of severity (4). People with more severe forms of EDs may have more medical complications and outwardly visible signs of an ED, thus increasing the likelihood of detection and treatment for their disorders. Other research suggests that males, people from lower income backgrounds, and people from racial minority groups are less likely to receive ED or any mental health treatment compared with females, people from higher income backgrounds, or Whites, respectively (5-7).
Parental factors may influence the likelihood of a child both developing an ED and receiving ED treatment. Eating disorders are known to be heritable (8-13). Children with mothers with an ED history are at increased risk of developing an ED (14), and children are more likely to exhibit disordered eating behaviors if their parents exhibit any disordered eating symptoms or engage in negative weight-related talk (15-20). While previous research has found parental psychiatric history to be predictive of receiving mental health treatment for those with psychiatric disorders, including depression and substance use disorders (21-23), it is unknown whether a parental history of an ED influences the likelihood of receiving ED treatment. Because many studies on EDs use clinical samples of patients seeking treatment, it is important to know whether findings using such populations are applicable to all persons with EDs. Thus, the objectives of the current study were 1) to confirm, in a large population-based sample that includes a broad range ED symptoms, that girls with mothers with an ED history have greater odds of developing ED symptoms, and 2) to assess whether girls who develop ED symptoms have greater odds of receiving treatment if their mothers have an ED history.
METHODS
Sample
Data came from the Growing Up Today Study (GUTS). Detailed information on GUTS has been previously reported (24). Participants were recruited in 1996 from Nurses’ Health Study II participants who reported having at least one child between ages 9 and 14 years of age. Mothers were asked for consent for their children to be invited to participate in GUTS. Children were then mailed invitation letters and questionnaires; 9,033 females and 7,843 males returned completed questionnaires in 1996, thereby agreeing to participate in GUTS. Questionnaires were sent annually from 1996-2001, and then in 2003, 2005, 2007, 2010, and 2013. The Human Subjects Committee at Brigham and Women’s Hospital approved this study, and the Institutional Review Boards at Brigham and Women’s Hospital and Boston Children’s Hospital approved the present analyses.
The study sample for our main analysis was limited to females who responded to the 2013 questionnaire (n=4,293) and who answered questions about receiving ED treatment in this questionnaire (n=3,667), whose mothers also answered questions about past ED history in a 2004 questionnaire to the mothers (n=3,661), and who had complete information on demographic variables (n=3,649). Males were excluded because we had an insufficient number of cases for adequate statistical power.
Among the final analytic sample, the majority (63.2%) participated in all 11 surveys from 1996-2013. There were 717 participants (19.7%) who missed one survey, 317 participants (8.7%) missed two surveys, and 141 participants (8.7%) missed 3 surveys. Less than 5% of the sample missed between 4-8 surveys. All girls participated in at least 3 surveys.
We compared baseline characteristics of females who were included in our main analytic sample to those who were not included, and there were no statistically significant differences in the baseline prevalence of overweight or obesity, White race, maternal report of an ED, or reporting some symptoms of anorexia nervosa (AN), BN, BED, or other specified feeding or eating disorder (OSFED). There were also no statistically significant differences in the distribution of baseline age or body mass index between those who were and were not included in the main analyses. Compared to participants not included in our main sample, those who were included were significantly more likely to have mothers report being in higher income brackets (p < .05). However, all participants were children of nurses, and report of only maternal income does not take into account other sources of family income.
Measurements
Eating Disorders
GUTS participants
GUTS questionnaires assessed disordered eating behaviors using validated questions on binge eating episodes and purging (25). Purging was defined as using vomiting or laxatives to keep from gaining weight in the past year. A two-part question assessed binge eating episodes. First, participants were asked about the frequency of eating a very large amount of food during the past year. Those who endorsed overeating were then asked whether they felt out of control during these episodes (that they could not stop eating even if they wanted to). Binge eating episodes were defined as eating a very large amount of food in a short amount of time, and also feeling out of control during the eating episodes. Questions on weight concerns came from the McKnight Risk Factor Survey (26), and responses ranged on a 5-point scale of: 1) “never/not at all”, 2) “a little”, 3) “sometimes/pretty much”, 4) “a lot”, or 5) “always/totally”. Scores for each weight concern question were averaged, and girls with a mean score of 4 or greater (corresponding to answering “a lot” or “always/totally” on average for these questions) were considered to have high levels of weight concerns (27).
Girls who reported engaging in weekly binge eating episodes and purging were considered to meet criteria for reporting symptoms of BN (RS-BN). Participants who reported weekly binge eating episodes, but no purging, were considered to meet criteria for reporting symptoms of BED (RS-BED). Those who reported engaging in monthly but not weekly binge eating episodes (with or without purging), and those who reported engaging in at least monthly purging without binge eating episodes (i.e. purging disorder), were classified as meeting criteria for reporting symptoms of OSFED (RS-OSFED).
Girls who were underweight (28) and reported high levels of concern with weight and shape were classified as meeting criteria for reporting symptoms of anorexia nervosa (RS-AN). Shape and weight concerns were not measured in later years, thus RS-AN pertains to only the years 1996-2007. Girls who were classified as RS-BN, RS-BED, RS-OSFED, or RS-AN at any point during the study were combined into a general “reporting symptoms of any eating disorder” group (RS-any ED). It should be noted that these classifications of EDs do not take into account all of the behavioral or cognitive symptoms of EDs (e.g. marked distress or impairment caused by an ED) (29). Girls could meet criteria for only one ED symptom category per survey, but could meet criteria for different ED symptom categories in different years (e.g., a girl could be classified as RS-BN in 2000 but RS-BED in 2001).
Mothers of GUTS participants
Mothers of GUTS participants were sent a brief questionnaire in 2004 that included a question asking whether anyone in the family currently had or previously had an ED. The mothers were then asked to identify who had an ED, and response options included the mother and the GUTS participants. Children of mothers who reported either currently or previously having an ED were classified as having a maternal ED history.
Professional diagnosis of an eating disorder
In 2013 participants were asked, “Since 2006, have you ever been told by a health care provider that you had any of the following illnesses.” The list of possible disorders included AN, BN, BED, or “other eating disorder”. Participants were classified as having a professional ED diagnosis reported if they self-reported one on the 2013 questionnaire, or if their mother reported the participant had an ED diagnosis on the 2004 mother’s questionnaire.
Eating disorder treatment
The 2013 GUTS questionnaire asked participants whether they had ever been treated for an ED by a doctor, nurse, or other health care provider. The three response options included: “no”, “yes, in the past”, and “yes, currently”. Mothers were asked in the 2004 questionnaire whether anyone in the family has been treated for an ED, and response options included their child in GUTS. Participants who reported ever receiving ED treatment in the 2013 questionnaire (either currently or in the past), or whose mothers reported that the participant received treatment in the 2004 questionnaire were classified as having received ED treatment.
Statistical analysis
Chi-square tests examined bivariate associations of maternal ED history with each ED symptom category, and also of maternal ED history with receiving ED treatment among participants in each ED symptom category. Fisher’s exact tests were used where expected cell counts were less than five. Generalized estimating equations, specifying a binary distribution, logit link function, independent working correlation, and robust standard errors, were used in main analyses, and adjusted for dependence due to multiple siblings per family. Maternal ED history was the primary predictor variable in each model. Outcomes were modeled as single binary variables (e.g., 1 = Met criteria for RS-BN in any survey from 1996-2013; 0 = Did not meet criteria for RS-BN in any survey from 1996-2013). Final models adjusted for demographic variables including participant’s age and race, and maternal income. In models examining predictors of receiving treatment for an ED, separate models were run conditional on each ED category (RS-BN, RS-BED, RS-OSFED, RS-any ED, and professional ED diagnosis). Due to the low prevalence of RS-AN in the sample, there was not enough statistical power to conduct models predicting ED treatment conditional on RS-AN. Models among those with RS-BED only adjusted for age because there were no participants in some of the race or income categories. Models among those with a professional diagnosis only adjusted for age and race because there were no participants in some of income categories. All main analyses were conducted in SAS version 9.4. Alpha levels of 0.05 were used to determine statistical significance.
Sensitivity analyses using multiple imputation for missing variables
By restricting the main analysis to participants with complete information on each variable, we excluded many participants from the baseline cohort (59.6%). A detailed table outlining the patterns of misssingness for variables used in analyses (that had missing data) can be found in Supplemental Table 3.
We repeated our main analyses with imputed values for missing variables, thereby allowing us to keep the original sample size. Missing data on all variables were imputed using multiple imputation by chained equations with 25 imputation sets using Stata12.1 (using the mi impute command). This procedure assumed missing at random (30). The imputation models included all predictor and outcome variables. The imputation method used “Rubin’s rules” to combine the repeated-imputation results and to calculate standard errors (31). Detailed steps for the procedures we used have been described elsewhere (32).
RESULTS
Among complete cases, the ages of participants ranged from 25-31 years in 2013 (Table 1). The majority of the sample was white (95.0%). Approximately 4.8% of mothers (n=174) reported that they currently or previously had an ED.
Table 1.
Characteristic of 3,649 females in the Growing Up Today Study
| Characteristic | Value |
|---|---|
| Age | |
| Baseline, mean (SD) | 11.6 (1.6) |
| Last follow up, mean (SD) | 27.9 (1.7) |
| White race, n (%) | 3465 (95.0) |
| Overweight or obesity | |
| Baseline, n (%) | 650 (18.1) |
| Ever between 1996 and 2013, n (%) | 1725 (47.3) |
| Mother had or has an eating disorder, n (%) | 174 (4.8) |
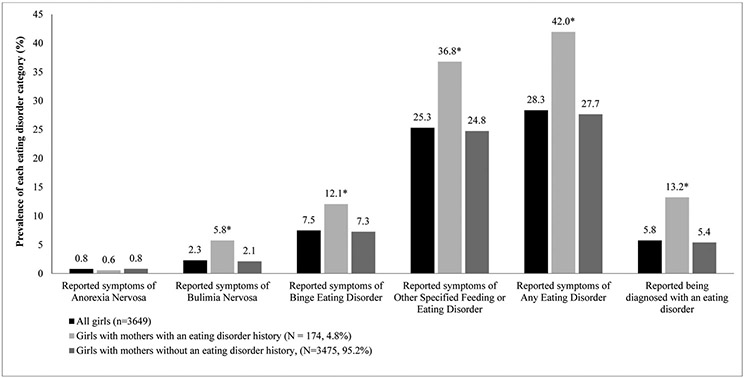
Between 1996-2013, 28.3% of girls met criteria for RS-AN, RS-BN, RS-BED or RS-OSFED in at least one year, and 4.8% had a maternal- or self-report of receiving a professional diagnosis (among complete cases). With the exception of RS-AN, the prevalence of each ED category was substantially higher among those whose mothers reported ever having an ED (Figure 1). Even after adjusting for age, race/ethnicity, and income, maternal self-reported ED history was positively associated with reported symptoms of EDs (Table 2). Compared with participants whose mothers did not have an ED history, those with mothers with an ED history had nearly three times the odds of meeting criteria for RS-BN (adjusted odds ratio (aOR): 2.82; 95% confidence interval (CI): 1.44-5.54) and 77% higher odds of meeting criteria for RS-BED or RS-OSFED (aORs: 1.77; 95% CIs: 1.10-2.83 and 1.28-2.46, respectively).
Figure 1.
Prevalence of self-reported symptoms of eating disorders§ and eating disorder diagnosis¶ among 3,649 females in the Growing Up Today Study overall, and by maternal eating disorder history.
§ Based on self-reported weight, height, and bulimic behaviors reported by the participants on questionnaires from 1996-2013
¶ History of a diagnosis of an eating disorder reported by the participant in 2013 or her mother in 2004.
* p < .05 in bivariate analyses
Table 2.
Odds ratios and 95% confidence intervals for maternal eating disorder history in unadjusted and adjusted models predicting symptomatic criteria for eating disorders and reported professional diagnosis of an eating disorder.
| Reported symptoms of anorexia nervosa, OR (95% CI) |
Reported symptoms of bulimia nervosa, OR (95% CI) |
Reported symptoms of binge eating disorder, OR (95% CI) |
Reported symptoms of other specified feeding or eating disorder, OR (95% CI) |
Reported symptoms of any eating disorder, OR (95% CI) |
Reported professional diagnosis of an eating disorder, OR (95% CI) |
|
|---|---|---|---|---|---|---|
| Unadjusted models | 0.71 (0.10-5.27) | 2.80 (1.43-5.51) | 1.76 (1.09-2.82) | 1.77 (1.28-2.45) | 1.89 (1.38-2.59) | 2.68 (1.70-4.23) |
| Adjusted modelsa | 0.71 (0.10-5.30) | 2.82 (1.44-5.54) | 1.77 (1.10-2.83) | 1.77 (1.28-2.46) | 1.89 (1.38-2.60) | 2.77 (1.75-4.36) |
Generalized estimating equations adjusted for age, race, and maternal income
Among the entire sample with complete information, 10.2% of those who reported having received ED treatment had mothers with an ED history compared with 4.5% of those who did not receive treatment (p < .001). Among those who met criteria for an ED, participants who received treatment had a higher prevalence of mothers with an ED history (12.4%) compared with those who did not receive ED treatment (6.3%) (p = .011).
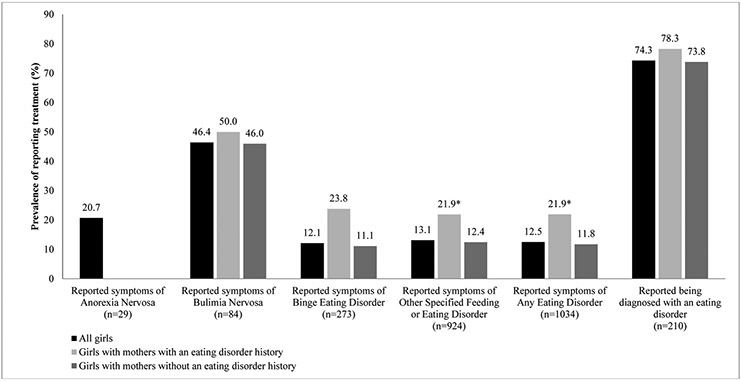
Only 5.7% of participants who met criteria for symptoms of an ED among complete cases were reported by the participant or mother to have received a professional diagnosis, and only 12.4% reported receiving ED treatment (Figures 1 and 2). Treatment rates were: 20.7% for RS-AN, 46.4% for RS-BN, 12.1% for RS-BED, and 13.1% for RS-OSFED. Nearly 75% of those who reported they had received a professional diagnosis reported receiving treatment. Among participants who met criteria for RS-OSFED or RS-any ED, those with mothers with an ED history had more than twice the odds of ED treatment reported compared with those whose mothers did not have an ED history (Table 3). Among those who reported a professional diagnosis, maternal ED history was not a significant predictor of receiving ED treatment
Figure 2.
Prevalence of receiving treatment for an eating disorder among females reporting symptoms consistent with an eating disorder § in at least one year between 1996 and 2013 or an eating disorder diagnosis¶
§ Based on self-reported weight, height, and bulimic behaviors reported by the participants on questionnaires from 1996-2013
¶ History of a diagnosis of an eating disorder reported by the participant in 2013 or her mother in 2004.
* p < .05 in bivariate analyses
Table 3.
Odds ratios and 95% confidence intervals for maternal eating disorder history in unadjusted and adjusted models predicting receiving eating disorder treatment among those within each eating disorder symptom category
| Reported symptoms of anorexia nervosa (n=29), OR (95% CI) |
Reported symptoms of bulimia nervosa (n=84), OR (95% CI) |
Reported symptoms of binge eating disorder (n=273), OR (95% CI) |
Reported symptoms of other specified feeding or eating disorder (n=927), OR (95% CI) |
Reported symptoms of any eating disorder (n=1037), OR (95% CI) |
Reported a professional diagnosis of an eating disorder (n=210), OR (95% CI) |
|
|---|---|---|---|---|---|---|
| Unadjusted models | — | 1.18 (.31-4.41) | 2.50 (.85-7.35) | 1.97 (1.07-3.64) | 2.11 (1.18-3.76) | 1.28 (.45-3.63) |
| Adjusted models | — | 1.29 (.31-5.41)a | 2.57 (.87-7.61)b | 2.06 (1.11-3.83)a | 2.23 (1.25-3.99)a | 1.24 (.45-3.43)c |
Generalized estimating equations adjusted for age, race, and maternal income
Generalized estimating equations adjusted for age
Generalized estimating equations adjusted for age and race
In sensitivity analyses using multiple imputation, girls with mothers who reported ED histories had increased odds of reporting symptoms consistent with meeting criteria for RS-BN, RS-BED, RS-OSFED, or RS-any ED (Supplemental Table 1). These ORs were slightly attenuated from those in the main analyses, but confidence intervals excluded 1 (except for that of RS-BED in adjusted analyses). Among the entire multiply imputed sample (not conditional on any symptomatic ED category), girls had nearly twice the odds of reporting ED treatment if their mother had an ED history (OR: 1.92; 95% CI: 1.05-3.50). However, in analyses that were conditional on each ED symptom category, associations of maternal EDs were attenuated from those in the main analyses and 95% confidence intervals crossed 1.00 (Supplemental Table 2).
DISCUSSION
We found that, among complete cases, girls had nearly twice the odds of meeting criteria for RS-any ED if their mother reported an ED history, and nearly three times the odds of reporting having a professionally diagnosed ED if their mother had an ED history. These findings are consistent with previous research showing EDs and disordered eating behaviors to be more prevalent among those whose parents had or have an ED, engage in disordered eating, or talk about their weight (14-20). We also found that, among those with complete information, girls who reported they had received treatment for their EDs had greater odds of having a mother with an ED history. To our knowledge, this is the first study to find that girls with symptoms consistent with criteria for EDs have higher odds of reporting receiving ED treatment if their mothers had a reported an ED history. These findings extend previous research that has found parental psychiatric history to be positively associated with receiving mental health treatment. For example, using the National Epidemiologic Survey on Alcohol and Related Conditions, Prokofyeva and colleagues (2013) observed that, among adults with a lifetime history of major depressive disorder, those with a positive family history of depression were twice as likely to receive treatment for depression than those without such a family history (21). Studies using community-based samples of children and adolescents have also found that parental substance abuse history is associated with higher prevalence of psychiatric treatment utilization among adolescent boys with substance abuse issues, and that, among those with mental disorders, youth that received mental health treatment were more likely to have parents that have used mental health services themselves (22, 23).
There are several possible reasons for this observed association of maternal EDs with receiving ED treatment. Mothers with ED histories may be more knowledgeable or attuned to disordered eating behaviors, and may be more likely to detect EDs in their children, raise concerns about their child’s disordered eating to health providers, and have their children receive treatment. Further, stigmatization of EDs may be lower among mothers with an ED history, resulting in mothers feeling more comfortable talking with their children about their eating behaviors and having their children receive treatment. It is also possible that girls with a mother with an ED history may have more severe ED psychopathology, increasing the likelihood of detection and treatment. Further examination of reasons for this association may help inform ED prevention efforts.
Among participants with complete information, we also found that the majority of women who met criteria for RS-any ED did not report ever receiving ED treatment or a professional diagnosis. More than 85% of young women who met criteria for RS-any ED did not report receiving treatment. Treatment rates were highest for RS-BN and lowest for RS-BED. Previous research has likewise found that the majority of children and adults with EDs and other mental illnesses do not receive treatment; this has been shown in nationally representative and international samples (1-3, 33-37). Furthermore, while more than one in four participants in our complete case sample met criteria for RS-any ED from 1996-2013, only 5.7% had either a self- or maternal report of a professional diagnosis. Most people with symptoms of EDs therefore may not receive a diagnosis and may be unaware that they meet symptomatic criteria for an ED.
Among complete cases, treatment rates were highest for those with a professional diagnosis. While only 5.7% of our overall complete case sample reported a professional diagnosis, 74.3% of those who reported they had received a professional diagnosis also reported receiving ED treatment. This suggests that girls who have their symptoms of an ED identified by a health provider may be substantially more likely to receive treatment, underscoring the importance of screening efforts for ED symptoms. Although girls with mothers with an ED history had greater odds of reporting receiving a professional diagnosis, maternal ED history was not associated with report of receiving treatment among girls with a self-reported professional diagnosis.
There are some limitations to the present study. First, our sample only included females and was 95% White. Results may not be generalizable to males or non-White young adults. Second, questionnaires relied on self-report from participants and did not use structured psychiatric interviews to assess EDs. Although the questions have been validated, it is possible that participants under- or over-reported ED symptoms. Moreover, our classifications of EDs did not take into account many of the behavioral or cognitive symptoms of clinically significant EDs (29). As such, there may be false positive cases of EDs in our sample. This misclassification would likely be nondifferential and may bias results toward the null, since misclassification would most likely not depend on maternal report of ED history. Third, our main predictor of interest, maternal ED history, was self-reported by mothers in one survey in 2004. Some mothers could have developed an ED after 2004, although this is a minimal concern since it is rare for EDs to first onset in late adulthood (1). Because maternal ED history was self-reported, there may be misclassification of this variable. Since our measures of child ED symptoms and receiving ED treatment relied on child report, misclassification of maternal ED history would likely be independent and nondifferential, and potentially bias results towards the null. Moreover, we do not have the ability with our data to examine whether the type of maternal ED or timing of the maternal ED (e.g., before or during a child’s lifetime, and when) influenced the risk of the child developing an ED or receiving treatment; future research should explore this topic. Fourth, because AN is rare, GUTS was underpowered to study the disorder, thus few questions were included in GUTS surveys to identify AN cases and those questions were only included until 2007. Therefore, there may be unidentified cases of RS-AN in this sample. Lastly, because our main analyses included only participants with complete data, results from our study may be biased if those in our analytic sample were more or less likely to receive ED treatment compared to those not included in our study. However, we were unable to verify this information since most participants were excluded from our sample because they did not have information on that particular variable. In our sensitivity analyses predicting treatment using multiple imputation, some effect estimates were attenuated with confidence intervals that included 1.00. Despite these limitations, there are many strengths to this study as well. We used a large population-based sample with participants living across the United States, we included a broad range of ED symptoms, and we had repeated measures on ED symptoms, which increased the likelihood of detecting ED symptoms in our surveys.
Overall, our findings highlight that the majority of young women who meet symptomatic criteria for an ED do not receive treatment. Being aware of a patient’s family history of mental illness, especially of EDs, may help to increase detection and treatment. Providers should assess maternal history of weight concerns and disordered eating to help identify patients at increased risk of developing ED symptoms. Moreover, our study illuminates the fact that girls who receive treatment for EDs are likely not representative of all persons with EDs, and as such, studies using treatment-seeking samples may not be generalizable to all persons with EDs. Further research is needed to better understand reasons why girls whose mothers have an ED history are more likely to receive ED treatment and how to increase detection and treatment rates. Research into this area may help elucidate facilitating factors as well as barriers to receiving ED treatment.
Supplementary Material
IMPLICATIONS AND CONTRIBUTION.
This study assessed whether an eating disorder history in mothers is associated with receipt of eating disorder treatment in daughters. Screening both girls and their mothers for current or previous disordered eating may be important for the prevention and detection of ED symptoms.
Acknowledgments:
The authors would like to thank the thousands of participants in the Growing Up Today Study and their mothers for completing multiple surveys, the Channing Laboratory of Network Medicine in the Department of Medicine, Brigham and Women’s Hospital, for the use of the data, and Dr. SonJa Swanson for her comments on preliminary analyses.
Funding: Data collection was supported by research grants from the National Institutes of Health (MH087786, DK59570, DK46200, HL68041, HD049889).
Abbreviations:
- (AN)
Anorexia nervosa
- (BED)
binge eating disorder
- (BN)
bulimia nervosa
- (ED)
eating disorder
- (GUTS)
Growing Up Today Study
- (OSFED)
other specified feeding or eating disorder
- (RS-AN)
reporting symptoms of anorexia nervosa
- (RS-Any ED)
reporting symptoms of any eating disorder
- (RS-BED)
reporting symptoms of binge eating disorder
- (RS-BN)
reporting symptoms of bulimia nervosa
- (RS-OSFED)
Reporting symptoms of other specified feeding or eating disorder
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Potential Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Hudson JI, Hiripi E, P HG Jr., et al. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry 2007;61:348–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Kessler RC, Berglund PA, Chiu WT, et al. The prevalence and correlates of binge eating disorder in the WHO World Mental Health Surveys. Biol Psychiatry 2013;73:904–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Swanson SA, Crow SJ, Grange DL, et al. Prevalence and correlates of eating disorders in adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. Arch Gen Psychiatry 2011;68:714–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Smink FRE, Hoeken Dv, Oldehinkel AJ, et al. Prevalence and severity of DSM-5 eating disorders in a community cohort of adolescents. Int J Eat Disord 2014;47:610–619. [DOI] [PubMed] [Google Scholar]
- [5].Marques L, Alegria M, Becker AE, et al. Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: implications for reducing ethnic disparities in health care access for eating disorders. Int J Eat Disord 2011;44:412–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Sonneville KR, Lipson SK. Disparities in eating disorder diagnosis and treatment according to weight status, race/ethnicity, socioeconomic background, and sex among college students. Int J Eat Disord 2018;51. [DOI] [PubMed] [Google Scholar]
- [7].Striegel-Moore RH, Dohm FA, Kraemer HC, et al. Eating disorders in white and black women. Am J Psychiatry 2003;160:1326–1331. [DOI] [PubMed] [Google Scholar]
- [8].Bulik CM, Sullivan PF, Kendler KS. Heritability of binge-eating and broadly defined bulimia nervosa. Biol Psychiatry 1998;44:1210–1218. [DOI] [PubMed] [Google Scholar]
- [9].Bulik CM, Sullivan PF, Tozzi F, et al. Prevalence, heritability, and prospective risk factors for anorexia nervosa. Arch Gen Psychiatry 2006;63:305–312. [DOI] [PubMed] [Google Scholar]
- [10].Javaras KN, Laird NM, Reichborn-Kjennerud T, et al. Familiality and heritability of binge eating disorder: results of a case-control family study and a twin study. Int J Eat Disord 2008;41:174. [DOI] [PubMed] [Google Scholar]
- [11].Klump KL, Miller KB, Keel PK, et al. Genetic and environmental influences on anorexia nervosa syndromes in a population–based twin sample. Psychol Med 2001;31:737–740. [DOI] [PubMed] [Google Scholar]
- [12].Mitchell KS, Neale MC, Bulik CM, et al. Binge eating disorder: a symptom-level investigation of genetic and environmental influences on liability. Psychol Med 2010;40:1899–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Kortegaard LS, Hoerder K, Joergensen J, et al. A preliminary population-based twin study of self-reported eating disorder. Psychol Med 2001;31:361–365. [DOI] [PubMed] [Google Scholar]
- [14].Bould H, Sovio U, Koupil I, et al. Do eating disorders in parents predict eating disorders in children? Evidence from a Swedish cohort. Acta Psychiat Scand 2015;132:51–59. [DOI] [PubMed] [Google Scholar]
- [15].Lydecker JA, Grilo CM. Fathers and mothers with eating-disorder psychopathology: Associations with child eating-disorder behaviors. J Psychosom Res 2016;86:63–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Easter A, Naumann U, Northstone K, et al. A longitudinal investigation of nutrition and dietary patterns in children of mothers with eating disorders. J Pediatr 2013;163:173–178. [DOI] [PubMed] [Google Scholar]
- [17].Bauer KW, Bucchianeri MM, Neumark-Sztainer D. Mother-reported parental weight talk and adolescent girls’ emotional health, weight control attempts, and disordered eating behaviors. J Eat Disord 2013;1:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Stein A, Woolley H, Cooper S, et al. Eating habits and attitudes among 10-year-old children of mothers with eating disorders. Br J Psychiatry 2006;189:324–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Neumark-Sztainer D, Bauer KW, Friend S, et al. Family weight talk and dieting: how much do they matter for body dissatisfaction and disordered eating behaviors in adolescent girls? J Adolesc Health 2010;47:270–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Berge JM, MacLehose R, Loth KA, et al. Parent conversations about healthful eating and weight: associations with adolescent disordered eating behaviors. JAMA Pediatr 2013;167:746–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Prokofyeva E, Martins SS, Younès N, et al. The role of family history in mental health service utilization for major depression. J Affect Disord 2013;151:461–466. [DOI] [PubMed] [Google Scholar]
- [22].Goodman SH, Lahey BB, Fielding B, et al. Representativeness of clinical samples of youths with mental disorders: A preliminary population-based study. J Abnorm Psychol 1997;106:3. [DOI] [PubMed] [Google Scholar]
- [23].Cornelius JR, Pringle J, Jernigan J, et al. Correlates of mental health service utilization and unmet need among a sample of male adolescents. Addict Behav 2001;26:11–19. [DOI] [PubMed] [Google Scholar]
- [24].Solomon CG, Willett WC, Carey VJ, et al. A prospective study of pregravid determinants of gestational diabetes mellitus. JAMA 1997;278:1078–1083. [PubMed] [Google Scholar]
- [25].Field AE, Taylor CB, Celio A, et al. Comparison of self-report to interview assessment of bulimic behaviors among preadolescent and adolescent girls and boys. Int J Eat Disord 2004;35:86–92. [DOI] [PubMed] [Google Scholar]
- [26].Shisslak CM, Renger R, Sharpe T, et al. Development and evaluation of the McKnight Risk Factor Survey for assessing potential risk and protective factors for disordered eating in preadolescent and adolescent girls. Int J Eat Disord 1999;25:195–214. [DOI] [PubMed] [Google Scholar]
- [27].Field AE, Austin SB, Frazier AL, et al. Smoking, getting drunk, and engaging in bulimic behaviors: in which order are the behaviors adopted? J Am Acad Child Adolesc Psychiatry 2002;41:846–853. [DOI] [PubMed] [Google Scholar]
- [28].Cole TJ, Flegal KM, Nicholls D, et al. Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ 2007;335:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, D.C.: American Psychiatric Association, 2013. [Google Scholar]
- [30].Horton NJ, Kleinman KP. Much ado about nothing: A comparison of missing data methods and software to fit incomplete data regression models. Am Stat 2007;61:79–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Little RJ, Rubin DB. Statistical analysis with missing data. 2 'edition'. New York: Wiley, 2002. [Google Scholar]
- [32].Aloisio KM, Micali N, Swanson SA, et al. Analysis of partially observed clustered data using generalized estimating equations and multiple imputation. Stata J 2014;14:863–883. [PMC free article] [PubMed] [Google Scholar]
- [33].Merikangas KR, He JP, Brody D, et al. Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics 2010;125:75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Wang PS, Demler O, Kessler RC. Adequacy of treatment for serious mental illness in the United States. Am J Public Health 2002;92:92–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Wang PS, Aguilar-Gaxiola SA,J, et al. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet 2007;370:841–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Micali N, Martini MG, Thomas JJ, et al. Lifetime and 12-month prevalence of eating disorders amongst women in mid-life: a population-based study of diagnoses and risk factors. BMC Med 2017;15:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Solmi F, Hotopf M, Hatch SL, et al. Eating disorders in a multi-ethnic inner-city UK sample: prevalence, comorbidity and service use. Soc Psychiatry Psychiatr Epidemiol 2016;51:369–381. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.