Abstract
Purpose:
Sexual minorities are at heightened risk for substance use disorders (SUDs). Discrimination based on sexual orientation may be an important factor in this increased risk, but differences across age have not been systematically examined. We examined age-varying associations of sexual orientation discrimination with alcohol use disorder (AUD), tobacco use disorder (TUD), and drug use disorder (DUD).
Methods:
We used data from U.S. participants ages 18 to 50 who reported non-heterosexual identity, attraction, or behavior (N=2,375) in a nationally-representative survey. We examined the prevalence of sexual orientation discrimination across age and its salience as a risk factor for AUD, TUD, and DUD for gay/lesbian, bisexual, and heterosexual identifying individuals using time-varying effect modeling.
Results:
Sexual orientation discrimination was most prevalent in early young adulthood but was positively associated with greater odds of AUD, TUD, and DUD only at later ages. We found statistically significant associations at ages 24.5 to 40.0 for AUD, ages 32.5 to 42.9 for DUD, and ages 39.3 to 43.2 for TUD. For example, discrimination at age 30 was associated with 2.1 times greater odds of AUD (95% CI: 1.3, 3.3) compared to those who reported no discrimination at that age. Discrimination at age 35 was associated with 2.8 times greater odds of DUD (95% CI: 1.2, 6.6) relative to no discrimination.
Conclusions:
Sexual orientation discrimination is significantly associated with SUDs and risk varies across age. Thus, age should be considered in the development of prevention and treatment of AUD, TUD and DUD, particularly for sexual minorities.
Keywords: Sexual minorities, substance use disorders, discrimination, time-varying effect models
INTRODUCTION
Substance use disorders affect approximately 20 million adults in the U.S. (Substance Abuse and Mental Health Services Administration, 2018) and include alcohol use disorders (AUDs; Rehm et al., 2009; Conner et al., 2016), tobacco use disorders (TUDs; U.S. Department of Health and Human Services, 2014; World Health Organization, 2011), and other drug use disorders (DUDs; Reeves et al., 2011; Murray et al., 2013). These disorders are responsible for considerable morbidity and mortality in the U.S., as well as for substantial costs to families and the larger society (Whiteford et al., 2015). Sexual minorities (i.e., those who identify at lesbian, gay, or bisexual; report same-sex attraction; or engage in same-sex sexual behavior) suffer from substantially higher rates of AUDs, TUDs, and DUDs than their heterosexual counterparts. For example, a national study of U.S. adults found that sexual minorities were twice as likely to meet criteria for any substance use disorder (SUD) as heterosexuals (Kerridge et al., 2017). Specifically, adult sexual minorities are more likely to have an AUD (Allen & Mowbray, 2016; McCabe et al., 2009; Talley et al., 2015), a TUD (McCabe et al., 2018), and a marijuana or other DUD (McCabe et al., 2009; Schuler et al., 2018) diagnosis. These differences tend to be larger and more consistent across age for women than men (McCabe et al., 2009; Schuler et al., 2018).
Minority stress (Meyer, 2003) is among the most common explanations for increased SUD risk among sexual minorities. The Minority Stress Model posits that increased exposure to chronic stressors among sexual minorities is related to SUD and other negative mental health outcomes (Meyer, 2003). Chronic stressors include experiences of prejudice and discrimination, internalization of sexual minority related stigma, and the expectation of future discrimination. Sexual minorities face discrimination at both individual and institutional levels (Hatzenbueler et al., 2010; McCabe et al., 2010), in multiple domains including employment or school settings, health care settings, and public spaces (Slater et al., 2017). Further, a growing body of literature has demonstrated a link of discrimination with risk for substance use disorders and consequences cross-sectionally (Gilbert and Zemore, 2016; McCabe et al., 2010; Slater et al., 2017) and longitudinally (Hatzenbueler et al., 2010; Wilson et al., 2016).
Recent studies have also found that disparities by sexual identity in substance use disorders vary by age. Tobacco use disorder disparities are more pronounced among young adult than among older gay/lesbian individuals (McCabe et al., 2018). Another study found sexual minorities had most consistently elevated rates of AUD in mid-adulthood (ages 35–49) compared to younger ages, although rates among bisexual women were elevated across all adult age groups (i.e., 18–49; Schuler et al., 2018). Age differences in sexual identity disparities in other domains, including physical health, have also been documented (Branstrom et al., 2016). These differences may be due to differences in life stage development and to cohort differences. Both the experience of discrimination and its relationship to mental health likely vary both by developmental context and historical context. A younger individual may not have learned coping strategies for dealing with discrimination and may perceive and respond to discrimination in a different way than older individuals. Older individuals have had more time and life experience in which to develop coping strategies, but more social roles in which to experience discrimination and more exposure to discrimination, the effects of which can accumulate across the life course. Differences may also be related to social support structures at different stages of the life course (Umberson et al., 2010) and different accumulation of life stressors (Pearlin et al., 2005), both of which are hypothesized to mediate the association of discrimination and health (Meyer, 2003). Moreover, due to cohort differences in societal acceptance and structural discrimination in the U.S., the relationship of discrimination and its health effects, including the development of SUDs, may differ by cohort.
Previous research has found that substance use trajectories across the life course among sexual minorities differ from that of their heterosexual peers (Coulter et al., 2018; Dermody et al., 2014; Marshal et al., 2009) and other contextual factors associated with substance use may have different timing across the life course for sexual minorities compared to heterosexuals (Fish et al., 2018; Fredriksen-Goldsen et al., 2017). In terms of historical context, younger cohorts of sexual minority individual’s experiences of discrimination may be distinct form those experienced by older cohorts of sexual minority individuals (Hammack et al., 2018). Whether due to cohort or developmental age, these age-varying disparities in substance use highlight the need to understand how risk factors for substance use, particularly those relevant to minority stress, vary in their prominence across adulthood. Such information can be used to develop targeted substance use prevention and intervention strategies for sexual minorities of different ages. We examined the prevalence of sexual orientation discrimination across young and mid adulthood and examined how associations between sexual orientation discrimination and AUD, TUD, and DUD vary across young and mid adulthood.
METHODS
Study population
Data are from the National Epidemiologic Study on Alcohol and Related Conditions-III (NESARC III), collected in 2012–2013. NESARC-III is a U.S. nationally-representative survey of non-institutionalized civilian adults ages 18 years and older (N=36,309). Data were collected via in-person interviews. Individuals were sampled at the household level; young adults (ages 18–24) and Black and Hispanic individuals were oversampled (Grant et al., 2014). Survey weights were used to adjust for oversampling of these groups and to account for varying rates of nonresponse. Household, person-level, and overall response rates were 72%, 84%, and 60% respectively. Institutional Review Boards at both the National Institutes of Health and Westat approved the study protocol; the first author’s institution ruled the study exempt because it involved existing de-identified data.
The analytic sample included participants ages 18 to 50 who reported non-heterosexual sexual identity, attraction, or behavior (N=2,375). We restricted analysis to this age range due to the small number of older individuals who identified as a sexual minority and who met criteria for a past-year AUD, TUD, or DUD. Thus, the sample included those who identified as (1) heterosexual and reported same-sex attraction or behavior in the past year, (2) gay/lesbian, or (3) bisexual. Those who reported heterosexual identity, behavior, and attraction were not asked questions regarding sexual orientation discrimination and were excluded from the analyses.
Measures
Past-year sexual orientation discrimination.
All individuals who reported non-heterosexual sexual identity, attraction, or behavior were asked questions regarding discrimination related to minority sexual orientation. These items were drawn from the Experiences with Discrimination scale (Krieger & Sidney, 1997; Krieger et al., 2005). Six different domains of discrimination that a respondent may have experienced because they were assumed to be a sexual minority were assessed: (1) in ability to obtain health care or health insurance coverage; (2) health care treatment; (3) in public settings such as the street, in stores, or in restaurants; (4) in other situations such as obtaining a job or on the job, getting admitted to a school or training program, in the courts, or by police; (5) verbal aggression; (6) physical assault or threats of harm. For example, participants were asked: “During the last 12 months, about how often did you experience discrimination in your ability to obtain health care or health insurance coverage because you were assumed to be gay, lesbian or bisexual?” Response options ranged from “Never” to “Very often.” We dichotomized into those who reported any of these forms of discrimination in the past year to those who reported no discrimination in the past year.
Sexual identity.
Individuals were asked to report which category best described them: (1) heterosexual (straight), (2) gay or lesbian, (3) bisexual, or (4) not sure. We restricted our analysis to those who self-identified as either “heterosexual,” “gay or lesbian,” or “bisexual.” Only heterosexual identifying individuals who reported same-sex and/or attraction were asked questions regarding discrimination and thus included in the analytic sample.
Past-year substance use disorders.
The National Institute on Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5) was used to assess whether an individual met criteria for a past-year alcohol use disorder (AUD), tobacco use disorder (TUD), or other drug use disorder (DUD). The AUDADIS-5 is a structured diagnostic interview that assesses DSM-5 diagnostic criteria and can be administered by non-clinician interviewers (Grant et al., 2015). Questions about amphetamine, opioid, sedatives, tranquilizers, cannabis, cocaine, heroin, hallucinogen, inhalants/solvents, and other drugs were combined to create a measure of past-year DUD. Consistent with DSM-5 criteria for a SUD, the AUDADIS-5 uses a threshold of two symptoms to be consistent with a diagnosis of AUD, DUD, or TUD. Each disorder measure was dichotomized to compare those with and without a disorder in the past year.
Age.
Age was examined continuously to the nearest year (M=32.1, SD=9.4).
Covariates.
Analyses examining age-varying associations controlled for sex (male vs. female), race/ethnicity (White non-Hispanic, Black non-Hispanic, American Indian/Alaska Native non-Hispanic, Asian/Native Hawaiian/Other Pacific Islander non-Hispanic, and Hispanic), education (high school diploma or greater vs. less than high school diploma), income (<$25,000, $25,000-$59,999, $60,000+), urbanicity (urban vs. rural), region (Northeast, Midwest, South, and West), presence of a past year non-SUD mental health disorder ( i.e., dysthymia, bipolar disorder, specific phobia disorder, social phobia disorder, panic disorder, agoraphobia, generalized anxiety disorder, post-traumatic stress disorder, anorexia, bulimia nervosa, and binge-eating disorder), and any adverse childhood experience (e.g., physical, sexual, emotional abuse, exposure to family violence, parental incarceration).
Analyses
Analyses were conducted using time-varying effect models (TVEMs), a type of non-parametric spline regression that estimates how regression coefficients vary as a function of time (Hastie and Tibshirani, 1993; Tan et al., 2012). First, rates of past-year sexual orientation discrimination across age in a nationally representative sample, overall and stratified by sexual identity (heterosexual, gay/lesbian, bisexual), were estimated in the full sample using TVEM intercept-only models that did not include any covariates. These first results were converted to prevalence rates to facilitate interpretation of the age trends in reports of discrimination. Prevalence estimates are shown with solid lines and associated 95% confidence intervals with dashed lines. This allowed us to examine how prevalence of sexual orientation discrimination varied across age for the three sexual identity groups. We then examined the age-varying associations of past-year sexual orientation discrimination with AUD, DUD, and TUD in three separate TVEM models. These models included all control variables. This allowed us to examine variations in the associations of sexual orientation discrimination and AUD, DUD, and TUD across adulthood. In supplemental figures we show the age-varying sexual orientation discrimination × sex interaction illustrating the age-varying association of sexual orientation discrimination with AUD, DUD, and TUD among men and among women. Power limitations prohibited stratification by sexual identity when examining age-varying associations of sexual orientation discrimination with AUD, DUD, and TUD.
RESULTS
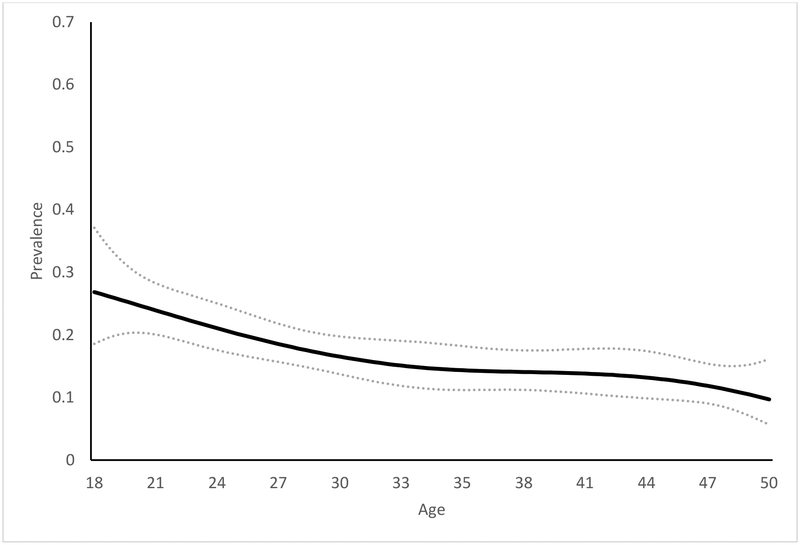
Prevalence of sexual orientation discrimination across age
Overall, the prevalence of sexual orientation discrimination was highest at age 18 and declined linearly with age. At age 18, 26.9% (95% CI: 18.6%, 37.1%) of individuals reported sexual orientation discrimination. At age 35, 14.4% (95% CI: 11.2%, 18.3%) reported any discrimination in the past year; prevalence was lowest at age 50 at 9.7% (95% CI: 5.6%, 16.2%).
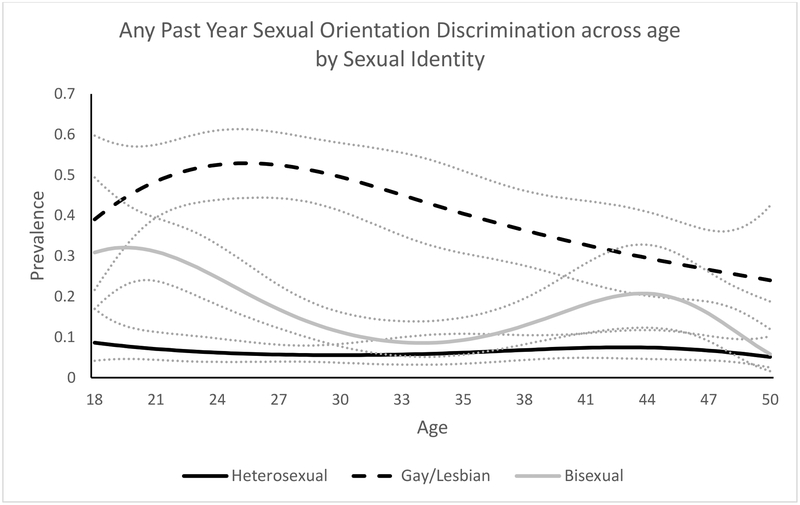
Prevalence of sexual orientation discrimination by sexual identity
Age trends in discrimination differed by sexual orientation. Prevalence of reported discrimination among Individuals who reported same-sex attraction or behavior but identified as heterosexual was consistently low across age groups. Prevalence of discrimination among bisexuals varied considerably across age, with two peaks. The first peak was at age 20 with almost one-third (32.1%, 95% CI: 23.3%, 42.5%) reporting experiencing discrimination in the past year. There was a subsequent decline in prevalence through age 34; 8.6% (95% CI: 5.2%, 13.9%) of individuals who were 34-years-old reported experiencing discrimination. There was another peak at age 44, with 20.8% (95% CI: 12.3%, 32.9%) reporting past-year discrimination. For gay men and lesbian women, prevalence of discrimination was higher than for bisexual or heterosexual men and women and varied across age. Reports of discrimination were highest among participants who were age 25, with more than one-half (52.9%, 95% CI: 44.4%, 61.3%) reporting experiencing sexual orientation discrimination. After age 25, there was a gradual decline in discrimination prevalence, although approximately one-fourth of gay/lesbian individuals reported discrimination at age 50.
Supplemental figures show the prevalence of sexual orientation discrimination by sexual identity separately for men and women. Similar trends of higher prevalence among gay/lesbian individuals compared to bisexual and heterosexual identifying individuals hold for both men and women. However, the prevalence of discrimination for lesbian women peaks in the mid-20s and then remains stable at around 45% through the mid-40s. In contrast, the prevalence among gay men is greater in magnitude in the mid-20s (e.g., 59% at age 24), it declines sharply in the 30s and 40s.
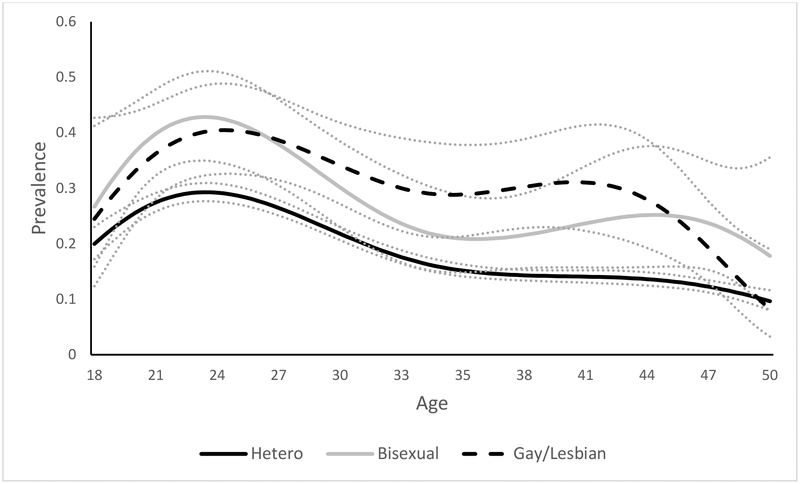
Prevalence of AUD, TUD, and DUD by sexual identity
Figure 3a shows the prevalence of AUD across ages 18 to 50 for heterosexual, gay/lesbian, and bisexual individuals. Patterns are somewhat similar for the three groups with an increase in prevalence through the mid-20s, but was lower for heterosexuals (29%) compared to bisexuals (43%) and gay/lesbians (40%) in the mid-20s.
Figure 3a.
Prevalence of past year AUD by sexual identity across ages 18 to 50
Figure 3b shows the prevalence of TUD across ages 18 to 50 by sexual identity. Prevalence for heterosexuals peaked at age 27 (28%) and for bisexual individuals at age 26 (43%). Gay/lesbian individuals had two peaks: the first at age 24 (37%) and the second at age 42 (36%).
Figure 3b.
Prevalence of past year TUD by sexual identity across ages 18 to 50.
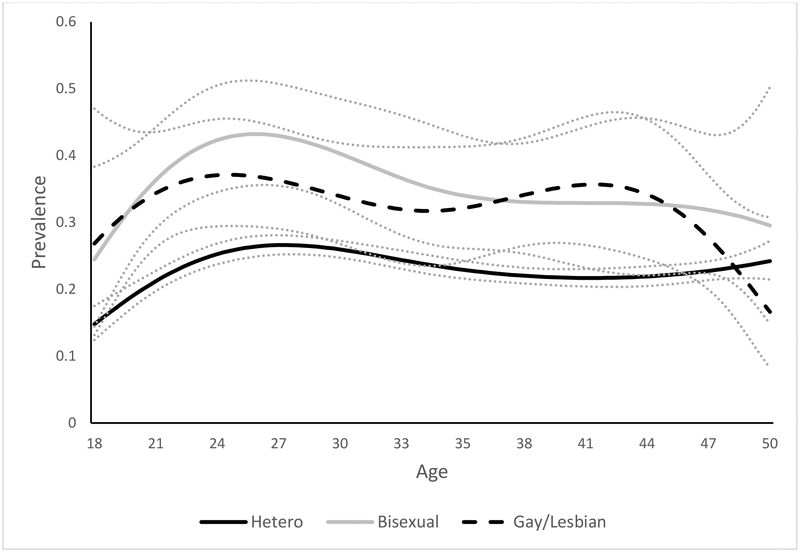
Figure 3c shows the prevalence of DUD across ages 18 to 50 for heterosexual, gay/lesbian, and bisexual individuals. Patterns across age are similar for the three sexual identity groups, with use decreasing across adulthood. Prevalence of DUD peaked at age 18 for heterosexuals, bisexuals, and gay/lesbians at 11%, 24% and 16% respectively. Among bisexual individuals, there was an increase in DUD prevalence from ages 45 to 50 (4% to 18%).
Figure 3c.
Prevalence of past year DUD by sexual identity across ages 18 to 50.
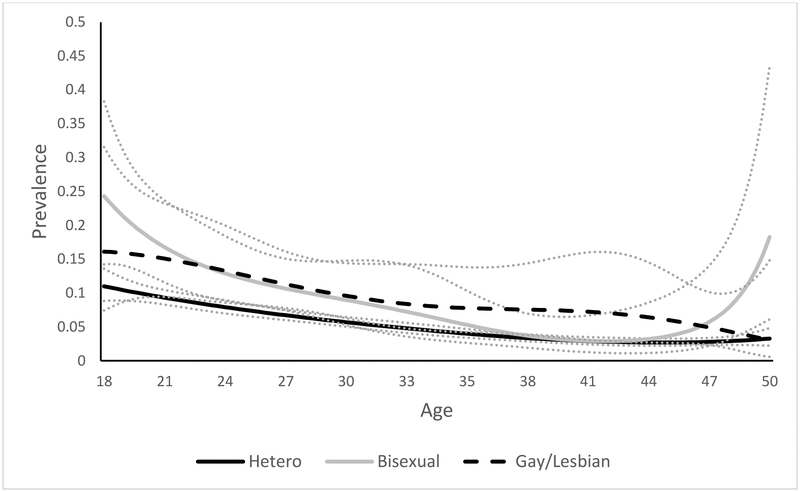
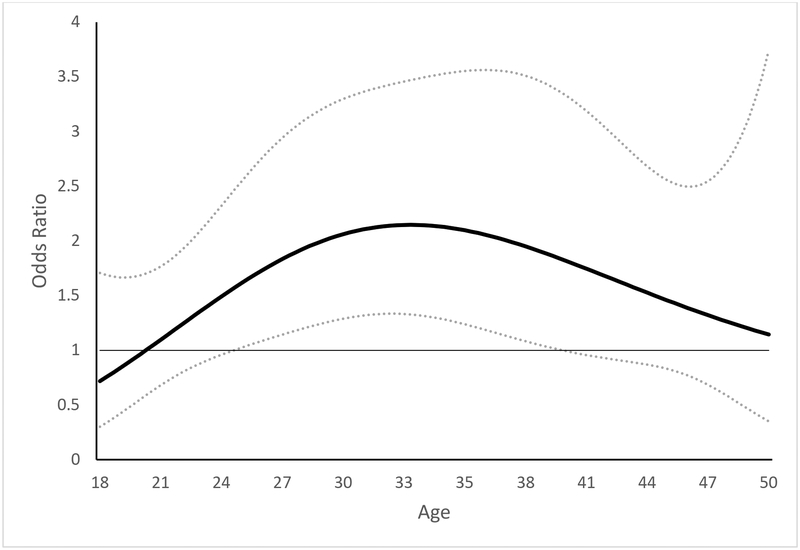
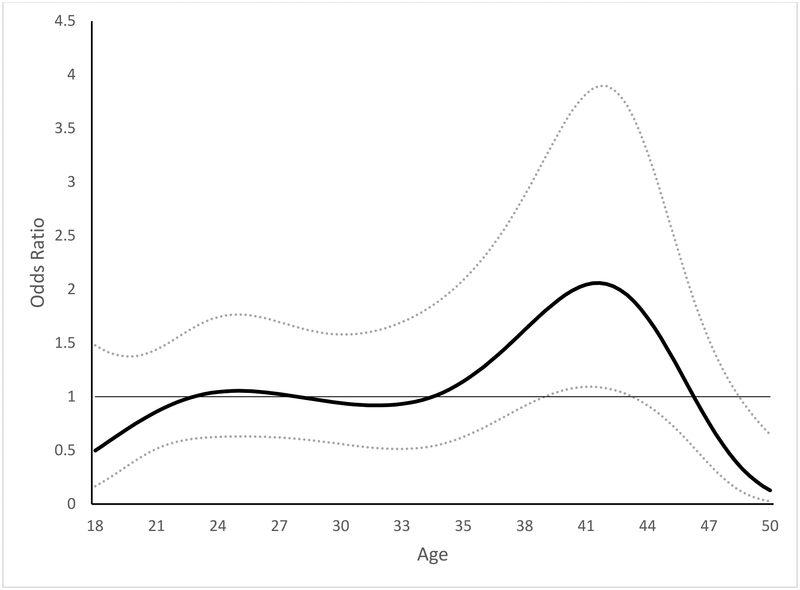
Age-varying association of sexual orientation discrimination with AUD
Figure 4a shows the age-varying association of past-year sexual orientation discrimination and past-year AUD, controlling for all covariates. Reports of any sexual orientation discrimination in the past year was associated with greater likelihood of having an AUD in the past year among individuals ages 24.5 to 40.0. For example, at age 30, those who reported sexual orientation discrimination had 2.1 times greater odds (95% CI: 1.3, 3.3) of having an AUD compared to those who reported no discrimination. The estimated magnitude of the association varied from an odds ratio of 1.6 to 2.1 across ages 24.5 to 40.0. Among participants younger than 24.5 years and older than 40.0 years there was no statistically significant association of sexual orientation discrimination and AUD. Figures showing the age-varying interaction of sexual orientation with sex for AUD, TUD, and DUD are presented in supplemental figures. The association of sexual orientation discrimination and AUD was significantly stronger for men at ages 36.1 to 42.9 compared to women at those ages.
Figure 4a.
Association of past year sexual orientation discrimination and past year AUD across ages 18 to 50
Age-varying association of sexual orientation discrimination with TUD
Figure 4b shows the age-varying association of past-year sexual orientation discrimination and past-year TUD, controlling for all covariates. Reporting sexual orientation discrimination in the past year was associated with greater likelihood of having a TUD in the past year only among individuals ages 39.3 to 43.2. For example, at age 40, those who reported discrimination had 1.9 times greater odds (95% CI: 1.0, 3.5) of having a TUD compared to those who reported no discrimination. At ages 48.7 to 50, there was a negative association with those reporting discrimination having decreased odds of TUD. The estimated magnitude of the association varied from an odds ratio of 1.8 to 2.1 across ages 39.3 to 43.2. Among participants younger than age 39.3 years and older than age 43.2 years there was no statistically significant association of sexual orientation discrimination and TUD. The association of sexual orientation discrimination and TUD was significantly stronger for men at ages 35.5 to 42.6.
Figure 4b.
Association of past year sexual orientation discrimination and past year TUD across ages 18 to 50
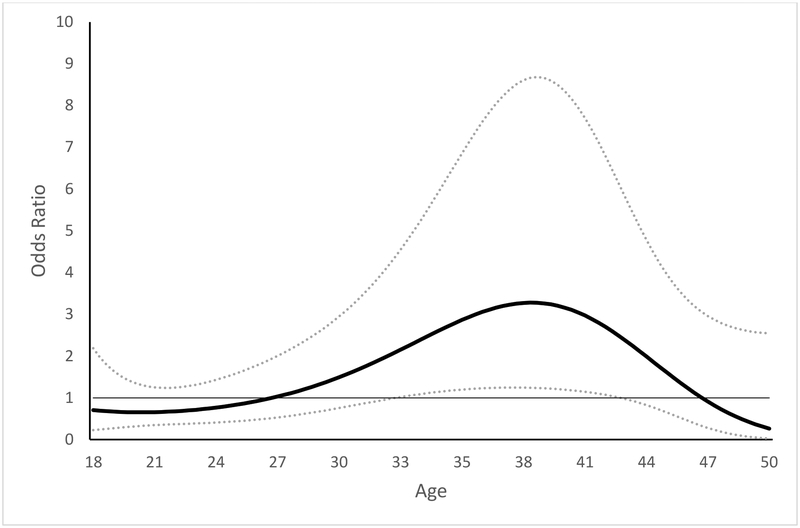
Age-varying association of sexual orientation discrimination with DUD
Figure 4c shows the age-varying association of past-year sexual orientation discrimination and past-year DUD controlling for all covariates. Reports of sexual orientation discrimination in the past year was associated with greater likelihood of having a DUD in the past year among individuals ages 32.5 to 42.9. For example, at age 35, those who reported discrimination had 2.8 times greater odds (95% CI: 1.2, 6.6) of having a DUD compared to those who reported no discrimination. The estimated magnitude of the association varied from an odds ratio of 2.2 to 3.3 across ages 32.5 to 42.9. Among participants younger than age 32.5 years and older than age 42.9 years there was no statistically significant association of sexual orientation discrimination and DUD. The association of sexual orientation discrimination and DUD was significantly stronger for men at ages 30.0 to 32.2.
Figure 4c.
Association of past year sexual orientation discrimination and past year DUD across ages 18 to 50
DISCUSSION
We examined sexual orientation discrimination prevalence across age and variations in the salience of this construct as a predictor of AUD, TUD, and DUD across age in a population based sample of adults. We demonstrated that: (1) sexual orientation discrimination varied across adulthood and (2) its salience as a risk factor for AUD, TUD, and DUD varied considerably across age. This is the first study to systematically examine how rates of sexual orientation discrimination differ across adulthood.
We found rates of sexual orientation discrimination varied across age among U.S. sexual minority adults. This is consistent with previous work that has found substantial developmental age differences in health behaviors (Fish et al., 2018) and work that has found cohort differences in lived experiences of sexual minority individuals (Fredrikson-Goldsen et al., 2017; Muraco et al., 2016). In particular, we found reports of past-year sexual orientation discrimination were greatest in young adulthood and then decreased in the 30s and 40s. This age trend appeared to be driven mostly by gay men. Lesbian women had consistently high rates of discrimination through the mid-40s and bisexual men and women had a resurgence in reported of discrimination in the 40s, after a drop in the 30s. This highlights the high risk for discrimination among young adult sexual minorities and the potential need for additional support during this developmental period. Bisexual men and women may also need these supports across all ages.
Consistent with previous research we found that sexual orientation discrimination was associated with AUD, TUD, and DUD. However, this association was limited to specific ages. While discrimination prevalence was generally greatest in young adulthood, its link with SUDs was not necessarily strongest at that age. The increased risk of AUD associated with discrimination spanned much of later young and mid-adulthood. However, the increased risk of TUD and DUD associated with discrimination was confined to the mid-30s to early-40s. This age-specific risk at older ages for TUD and DUD may be due to the cumulative stress of discrimination experiences across the life course. These findings emphasize the need to examine factors that may confer protection at certain ages (e.g., social support). Previous research suggests social support, identified as an important moderator in the Minority Stress Model (Meyer, 2003) may buffer the negative impact of discrimination (Bry et al., 2017; DePedro et al., 2017). Moreover, a better understanding of the mediating pathway from discrimination to SUDs across the life course is warranted. Previous research shows that the timing and chronicity of stressors has important implications for health (Pearlin et al., 2005). Further, understanding protective factors in mid-adulthood, an age period focused on less often in public health research, is particularly important and needed. We also found a puzzling negative association of discrimination and TUD for those ages 49 and 50. This again highlights the need to understand risk and protective factors in adults of older ages; it is possible that risk and protective factors may differ at this life stage. As sexual minority sample sizes grow and longitudinal data on this population increases, we will be able to better disentangle the extent to which findings represent age differences and cohort differences. In addition, our findings may have implications for substance use treatment by helping to identify ages at which it is particularly important to provide additional formal and informal support for sexual minorities. Future research is needed to understand what supports would be most helpful. Finally, the different findings for AUD compared to TUD and DUD emphasize the need to examine these disorders separately as risk factors and the ages at which they are relevant for each disorder may differ.
We found preliminary evidence for differences in both the prevalence of sexual minority-related risk factors across age and their salience with regard to alcohol, tobacco, and drug use disorders across adulthood. Our findings suggested that sexual orientation discrimination was a stronger risk factor for men in their 30s and 40s. Because of sample size limitations, we were unable to fully analyze sex differences, but findings suggest differences in risk factors for AUD, TUD, and DUD by sex. Thorough examination of sex differences was limited by sample size as even in the NESARC-III, one of the largest national studies to examine sexual identity and SUDs. The number of older sexual minority participants—particularly those with SUDs—was also limited. Thus, larger samples of sexual minorities, perhaps through oversampling of sexual minorities in large national studies, are greatly needed to understand SUD risk among this population.
It is important to note the limitations of this study. First, due to sample size limitations we combined DUD into one category. We were, however, able to examine cannabis, cocaine, and opioid use disorders separately. We found similar patterns among these disorders as for overall DUD--although confidence intervals were wider. Specific SUDs deserve attention in future research. Also, because of sample size limitations we could not fully examine important variations within the sexual minority population such as by sex and sexual identity, and we were unable to include participants who were older than 50. As stated above, power limitations of this study strongly point to the need to oversample sexual minorities in large national studies in order to understand risk for SUDs, including older sexual minority populations for whom risk and protective factors may differ. Second, the NESARC-III does not include a measure of gender identity and thus were not able to examine gender minority individuals even at a preliminary level. Finally, because this study used a cross-sectional design inferences about causality cannot be made.
Despite these limitations, this study utilized a large national sample to examine important age variations in sexual minority discrimination prevalence and risk. This provides important evidence regarding age-varying risks for substance use disorders among sexual minorities.
Supplementary Material
Figure 1. Prevalence of past-year sexual orientation discrimination across ages 18 to 50 (N=2375).
Note: Solid line represents prevalence estimates across age and dashed lines are 95% confidence intervals.
Figure 2.
Prevalence of past-year sexual orientation discrimination by sexual identity across ages 18 to 50
Note: Heterosexual includes those who report heterosexual identity and non-heterosexual identity and/or behavior. Solid lines are prevalence estimates and dashed lines represent 95% confidence intervals.
Acknowledgments.
This research was supported by grants R01AA025684 (PI: McCabe) and R01AA013328 (PI: Hughes) from the National Institute on Alcohol Abuse and Alcoholism, R01DA043696 (PI: Boyd) and R01DA036541 (PI: McCabe) from the National Institute on Drug Abuse, and R01CA212517 (PI: McCabe) from the National Cancer Institute.
Footnotes
Conflict of interest statement
On behalf of all authors, the corresponding author states that there is no conflict of interest.
REFERENCES
- Allen JL, Mowbray O (2016). Sexual orientation, treatment utilization, and barriers for alcohol related problems: findings from a nationally representative sample. Drug Alcohol Dependence, 161, 323–330. [DOI] [PubMed] [Google Scholar]
- Branstrom R, Hatzenbuehler ML, Pachankis JE (2016). Sexual orientation disparities in physical health: age and gender effects in a population-based study. Social Psychiatry and Psychiatric Epidemiology, 51, 289–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bry LJ, Mustanski B, Garofalo R, Burns MN (2017). Management of a Concealable Stigmatized Identity: A Qualitative Study of Concealment, Disclosure, and Role Flexing Among Young, Resilient Sexual and Gender Minority Individuals. Journal of Homosexuality, 64(6), 745–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor JP, Haber PS, & Hall WD (2016). Alcohol use disorders. The Lancet, 387(10022), 988–998. [DOI] [PubMed] [Google Scholar]
- Coulter RWS, Jun HJ, Calzo JP, Truong NL, Mair C, Markovic N, Charlton BM, Silvestre AJ, Stall R, Corliss HL (2018). Sexual-orientation differences in alcohol use trajectories and disorders in emerging adulthood: results from a longitudinal cohort study in the United States. Addiction, 113(9), 1619–1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Pedro KT, Esqueda MC, Gilreath TD (2017). School Protective Factors and Substance Use among Lesbian, Gay, and Bisexual Adolescents in California Public Schools. LGBT Health, 4(3), 210–216. [DOI] [PubMed] [Google Scholar]
- Dermody SS, Marshal MP, Cheong J, Burton C, Hughes T, Aranda F, Friedman MS (2014). Longitudinal disparities of hazardous drinking between sexual minority and heterosexual individuals from adolescence to young adulthood. Journal of Youth and Adolescence, 43, 30–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fish JN, Rice CE, Lanza ST, & Russell ST (2018). Is young adulthood a critical period for suicidal behavior among sexual minorities? Results from a US national sample. Prevention Science, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Bryan AE, Jen S, Goldsen J, Kim HJ, Muraco A, 2017. The unfolding of LGBT lives: key events associated with health and well-being in later life. Gerontologist 57, S15–S29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert PA, & Zemore SE (2016). Discrimination and drinking: A systematic review of the evidence. Social Science & Medicine, 161, 178–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Chu A, Sigman R, Amsbary M, Kali J, Sugawara Y, Goldstein R (2014). Source and Accuracy Statement: National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC III). National Institute on Alcohol Abuse and Alcoholism, Rockville, MD. [Google Scholar]
- Grant BF, Goldstein RB, Smith SM, Jung J, Zhang H, Chou SP, Pickering RP,Ruan WJ, Huang B, Saha TD, Aivadyan C, Greenstein E, Hasin DS (2015). The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5(AUDADIS-5): reliability of substance use and psychiatric disorder modules in a general population sample. Drug Alcohol Dependence, 148, 27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammack PL, Frost DM, Meyer IH, Pletta DR (2018). Gay men’s health and identity: social change and the life-course. Archives of Sexual Behavior, 47, 59–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hastie T, Tibshirani R (1993). Varying-coefficient models. Journal of the Royal Statistical Society Series B (Methodological), 55, 757–779. [Google Scholar]
- Hatzenbuehler ML, McLaughlin KA, Keyes KM, & Hasin DS (2010). The impact of institutional discrimination on psychiatric disorders in lesbian, gay, and bisexual populations: A prospective study. American Journal of Public Health, 100(3), 452–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JH, Gamarel KE, Bryant KJ, Zaller ND, & Operario D (2016). Discrimination, mental health, and substance use disorders among sexual minority populations. LGBT Health, 3(4), 258–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li R, Dziak JD, Tan X, Huang L, Wagner AT, Yang J (2015). TVEM (Time-varying Effect Model) SAS Macro Users’ Guide (Version 3.1.0). University Park, PA, pp.2, Retrieved from http://methodology.psu.edu. [Google Scholar]
- Marshal MP, Friedman MS, Stall R, Thompson AL (2009). Individual trajectories of substance use in lesbian, gay and bisexual youth and heterosexual youth. Addiction, 104, 974–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Hughes TL, Bostwick WB, West BT, & Boyd CJ (2009). Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction, 104(8), 1333–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Bostwick WB, Hughes TL, West BT, & Boyd CJ (2010). The relationship between discrimination and substance use disorders among lesbian, gay, and bisexual adults in the United States. American Journal of Public Health, 100(10), 1946–1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Matthews AK, Lee JG, Veliz P, Hughes TL, & Boyd CJ (2018). Tobacco Use and Sexual Orientation in a National Cross-sectional Study: Age, Race/Ethnicity, and Sexual Identity–Attraction Differences. American Journal of Preventive Medicine, 54(6), 736–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological Bulletin, 129, 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muraco A, & Fredriksen-Goldsen KI (2016). Turning points in the lives of lesbian and gay adults age 50 and over. Advances in Life Course Research, 30, 124–132. doi: 10.1016/j.alcr.2016.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CJL, & Lopez AD (2013). Measuring the global burden of disease. New England Journal of Medicine, 369, 448–457. 10.1056/nejmra1201534 [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Schieman S, Fazio EM, & Meersman SC (2005). Stress, health, and the life course: Some conceptual perspectives. Journal of Health and Social Behavior, 46(2), 205–219. [DOI] [PubMed] [Google Scholar]
- Reeves WC, Strine TW, Pratt LA, Thompson W, Ahluwalia I, Dhingra SS, McKnight-Eily LR, Harrison L, D’Angelo DV, Williams L, Morrow B, Gould D, & Safran MA (2011). Mental illness surveillance among adults in the United States. Morbidity and Mortality Weekly Report CDC Surveillance Summaries, 60(Suppl. 3), 1–29. Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/su6003a1.htm [PubMed] [Google Scholar]
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, & Patra J (2009). Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. The Lancet, 373(9682), 2223–2233. [DOI] [PubMed] [Google Scholar]
- Schuler MS, Rice CE, Evans-Polce RJ, & Collins RL (2018). Disparities in substance use behaviors and disorders among adult sexual minorities by age, gender, and sexual identity. Drug and Alcohol Dependence, 189, 139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slater ME, Godette D, Huang B, Ruan WJ, & Kerridge BT (2017). Sexual orientation-based discrimination, excessive alcohol use, and substance use disorders among sexual minority adults. LGBT Health, 4(5), 337–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2018). Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18–5068, NSDUH Series H-53). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; Retrieved from https://www. samhsa.gov/data/ [Google Scholar]
- Talley AE, Aranda F, Hughes TL, Everett B, & Johnson TP (2015). Longitudinal associations among discordant sexual orientation dimensions and hazardous drinking in a cohort of sexual minority women. Journal of Health and Social Behavior, 56(2), 225–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan X, Shiyko MP, Li R, Li Y, Dierker L (2012). A time-varying effect model for intensive longitudinal data. Psychological Methods, 17, 61–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D, Crosnoe R, & Reczek C (2010). Social relationships and health behavior across the life course. Annual Review of Sociology, 36, 139–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2014). The health consequences of smoking—50 years of progress: a report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. [Google Scholar]
- Whiteford HA, Ferrari AJ, Degenhardt L, Feigin V, & Vos T (2015). The global burden of mental, neurological and substance use disorders: an analysis from the Global Burden of Disease Study 2010. PloS One, 10(2), e0116820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson SM, Gilmore AK, Rhew IC, Hodge KA, & Kaysen DL (2016). Minority stress is longitudinally associated with alcohol-related problems among sexual minority women. Addictive Behaviors, 61, 80–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2011). WHO Report on the Global Tobacco Epidemic. Geneva: World Health Organization. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.