Abstract
Dysregulations of the mevalonate pathway (MVA) have been previously identified. Our previous study demonstrated that 3-hydroxy-3-methylglutaryl-coenzyme A reductase (HMGCR), the rate-limiting enzyme of the MVA pathway, was upregulated in esophageal squamous cell carcinoma (ESCC) and statin-inhibited ESCC tumorigenesis. However, the underlying mechanism of HMGCR regulation in ESCC remains unknown. In the present study, western blotting and immunohistochemistry analysis demonstrated that sterol regulatory element-binding protein 2 (SREBP2), the master regulator for HMGCR, was upregulated in ESCC clinical samples. Overexpression of SREBP2 expression in ESCC cell lines promoted the growth, migration and colony formation of cancer cells in the MTT, Boyden chamber and soft agar assays, respectively, which was inhibited by lovastatin. Downregulation of SREBP2 expression in ESCC cell lines inhibited the viability, and migration and colony formation abilities of cancer cells. Assessment of the molecular mechanism demonstrated that SREBP2 interacted with c-Myc and cooperated with c-Myc to activate HMGCR expression. Collectively, the present study identified SREBP2 as an oncogene associated with the tumorigenesis of ESCC and further demonstrated the therapeutic effects of statins in ESCC.
Keywords: sterol regulatory element-binding protein 2, esophageal squamous cell carcinoma, c-Myc, statin
Introduction
Esophageal squamous cell carcinoma (ESCC) is one of the most common types of malignancies in China (1). Significant advances in the diagnosis of ESCC have been made; however, the outcome of ESCC remains poor (1). Dysregulations in metabolism are one of the hallmarks of cancer cells (2,3). An improved understanding of the molecular mechanisms underlying the dysregulated metabolism in cancer cells may aid developments in the treatment of ESCC.
The mevalonate (MVA) pathway is responsible for the de novo synthesis of cholesterol (4,5). The 3-hydroxy 3-methylglutaryl (HMG)-coenzyme A reductase (HMGCR) is the rate-limiting enzyme of cholesterol synthesis and is regulated via a negative feedback mechanism mediated by sterols and non-sterol metabolites derived from MVA (6,7). Statins inhibit the activity of HMGCR, which is regulated by sterol regulatory element-binding protein 2 (SREBP2) (8,9). A lack of intracellular sterols leads to the translocation of SREBP2 from the endoplasmic reticulum to the Golgi; SREBP2 is cleaved by proteases in the Golgi membrane (10,11). The N-terminal of SREBP2 serves as a transcription factor and enters the nucleus to activate the transcription of enzymes involved in cholesterol biosynthesis (10,11).
In our previous study, it was demonstrated that the expression of enzymes involved in the MVA pathway was upregulated in ESCC clinical tissues, and treatment with statin inhibited the growth and tumorigenesis of ESCC cells (12). Additionally, it was demonstrated that HMGCR promoted the growth, migration and colony formation of ESCC cells (13); however, whether SREBP2 associates with other factors to regulate HMGCR expression in ESCC cells remains unknown.
In the present study, the expression profile and biological functions of SREBP2 in ESCC cells were investigated and an SREBP2-binding protein was identified. In addition, the underlying molecular mechanisms of SREBP2 in ESCC were examined.
Materials and methods
Cell culture and clinical samples
A normal human esophageal cell line (Het-1A) was obtained from the American Type Culture Collection (Manassas, VA, USA). 293T, Eca109 and KYSE150 cells were obtained from the cell bank (the Chinese Academy of Science, Shanghai, China). The Caes17 and KYSE180 cells were gifts from Professor Xu (Shantou Medical University, Shantou, China) (14). Cells were cultured in Dulbecco's modified Eagle's medium (DMEM; Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA, USA) supplemented with 10% fetal bovine serum (Thermo Fisher Scientific, Inc.), penicillin (100 U/ml) and streptomycin (100 µg/ml). Cell cultures were maintained in a humidified incubator with 5% CO2 at 37°C.
Patient sample collection (esophageal cancer and adjacent non-tumor samples) was approved by the Institutional Ethics Committee of Shanghai Chest Hospital (Shanghai, China), and all patients provided written informed consent. A total of 52 patients (32 males and 20 females, 45–78 years old with middle and lower esophageal cancer) between May 1 2010 and June 24 2014 who had not undergone radiotherapy and/or chemotherapy were recruited for the present study.
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
Total RNA was extracted from tissue or cell samples with TRIzol® (Thermo Fisher Scientific, Inc.) and cDNA was synthesized using an MMLV Reverse Transcription kit (Promega Corporation, Madison, WI, USA) at 37°C for 1 h. qPCR was performed with 2X SYBR Green mixture (Takara Biotechnology Co., Ltd., Dalian, China) in triplicate. The thermocycling conditions were: 95°C for 2 min; then 45 cycles of 94°C for 15 sec, 55°C for 15 sec and 68°C for 30 sec. The relative expression levels of target genes were normalized to 18S rRNA (Applied Biosystems; Thermo Fisher Scientific, Inc.) and were calculated using 2−∆∆Cq (15). The primer sequences for SREBP2 were: F, 5′-TGACTTGTTTTCAGAACAGC-3′ and R, 5′-AACTCTGCAAGTCAAGGTT-3′.
Immunohistochemistry
ESCC tissues and paired non-cancerous tissues were fixed with 4% PFA overnight at 4°C for 8 h and embed in paraffin wax. The paraffin-embed ESCC sections (5-µm-thick) were kept at 65°C for 30 min and then deparaffinized, washed in with xylene and rehydrated with descending ethanol series (100, 95, 75 and 50%). Endogenous peroxidase activity was blocked with 0.35% H2O2 solution. Antigen retrieval was performed using citrate solution (10 mM, pH 6.0) at 98°C for 20 min. Non-specific binding was blocked with 1% bovine serum albumin solution (Sangon Biotech Co., Ltd., Shanghai, China) at room temperature for 1 h. Sections were stained with an SREBP2 antibody (1:100; HPA031962; Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) at 4°C for 8 h. Then, the sections were washed with TBST and incubated with the secondary antibody [Gene Tech (Shanghai) Co., Ltd., Shanghai, China] for 2 h at room temperature. Following washing with TBST three times (5 min for each time), the sections were developed with 3,3′-diaminobenzidine (2 min at room temperature) and counterstained with hematoxylin (8 min at room temperature). The sections were examined under an inverted microscope and images acquired at the magnification, ×20.
Western blotting
Cellular proteins were harvested from tissues and cells with radioimmunoprecipitation assay buffer (Thermo Fisher Scientific, Inc.) containing a protease inhibitor (Sigma-Aldrich; Merck KGaA). Cell lysates were placed on ice for 30 min and were subsequently centrifuged at 12,000 × g for 10 min at 4°C. The Bradford method was used to determine the protein concentration. Equal amounts of proteins (20 µg/lane) were loaded to 10% SDS-PAGE and were transferred to a polyvinylidene difluoride membranes. Subsequently, the membranes were blocked (5% non-fat milk in 1X Tris-buffered saline with Tween-20) for 1 h at room temperature. The membranes were incubated with primary antibodies overnight at 4°C: SREBP2 (1:1,000; ab30682; Abcam, Cambridge, UK), c-Myc (1:1,000; 12189; Cell Signaling Technology, Inc., Danvers, MA, USA), HMGCR (1:1,000; HPA008338; Sigma-Aldrich; Merck KGaA) and GAPDH (1:5,000; EMD Millipore, Billerica, MA, USA). Secondary antibodies conjugated with peroxidase (1:1,000; 14708 and 4878; Cell Signaling Technology, Inc.) were applied to membranes for 1 h at room temperature. Following immunoblotting, the films were scanned with a Bio-Rad imaging system (Bio-Rad Laboratories, Inc., Hercules, CA, USA).
Mass spectrometry assay
The coding sequence for SREBP2 was inserted into pCMV14/3×FLAG-Pax3 (25427; Adgene, Watertown, MA, USA) using the restriction enzymes EcoR1 and EcoRV. Subsequently, the plasmids (Flag-SREBP2) were transfected into 293T cells (exogenous protein is highly expressed in this cell line) using Lipofectamine® 2000 (Invitrogen; Thermo Fisher Scientific, Inc.). The transfection efficiency was monitored by the co-transfecting GFP. After 48 h, the cells were harvested, and immunoprecipitation was performed as described below. The immunoprecipitates were subjected to SDS-PAGE and stained with silver solution at room temperature for 1 h. The differentially expressed bands were collected and digested with trypsin followed by mass spectrometry analysis (PTM Biolabs Inc., Hangzhou, China; http://www.ptm-biolab.com.cn).
Plasmids and cell transfection
The SREBP2 sequence was generated by PCR using KYSE180 cDNA and subcloned into the pCMVTag2B vector (11463; Adgene). KOD polymerase (Takara Biotechnology Co., Ltd.) was used. The primer sequences for SREBP2 were: F, 5′-ATGGACGACAGCGGCGAG-3′ and R, 5′-TCAGGAGGCGGCAATGGC-3′. The c-Myc sequence was generated by PCR and subcloned into the pcDNA3.1 vector (containing HA tag). Caes17 and KYSE180 cells were transfected with SREBP2 plasmids (1 µg) using Lipofectamine® 2000 (Invitrogen; Thermo Fisher Scientific, Inc.) according to the manufacturer's protocol. After 48 h, transfected cells were selected using G418 (600 µg/ml) for 2 weeks. After 2 weeks, G418-resistant cells were pooled.
Boyden chamber assays
Caes17 and KYSE180 cells (1×105 cells/well) were seeded on the top layer of the chamber. Medium supplemented with serum was used as a chemoattractant in the bottom chamber for the migration assay. The cells were incubated at 37°C for 8 h. The same protocol was used for the invasion assay; however, the membrane was pre-coated with 50 µg Matrigel. The non-migratory cells in the top chambers were removed with cotton swabs. The migrated and invaded cells on the lower membrane surface were fixed in 100% methanol for 5 min at room temperature, air-dried, stained with eosin for 5 min at room temperature and subsequently counted under an inverted microscope (magnification, ×20).
Cell viability assay
An MTT assay was performed to evaluate the viability of the cells. Cells were counted and placed in 96-well plates (1,000 cells/well) in triplicate and incubated with fresh medium. At 4 h prior to the analysis of cell viability at the indicated time points (day 2, 4, 6 and 8), cells were incubated with MTT (200 µl/ml medium) for 4 h. Following the MTT incubation, the formazan crystals were dissolved using DMSO. Subsequently, growth curves were generated by analyzing the optical density at 540 nm using a microplate reader.
Soft agar assay
Caes17 and KYSE180 cells (1×103 cells /well) were seeded in 1 ml 0.5% noble agar in complete DMEM overlaid with 2 ml 1% agar in the same medium. After 2 weeks of culture, cell colonies were examined under a microscope.
SREBP2, HMGCR and c-Myc knockdown in ESCC cell lines
SREBP2, HMGCR and c-Myc expression in ESCC cell lines was downregulated via lentiviral transduction. The lentivirus was purchased from Shanghai GeneChem Co., Ltd. (Shanghai, China). Cells were seeded in 6-well plates (5×105 cells/well) and incubated with the lentivirus for 24 h. The lentivirus expressed GFP independent of siRNA. GFP-positive cells were sorted by cytometry. The sequences for the siRNAs are: Si con: 5′-AATCTGAGTCCTTGCTTAATG-3′, Si SREBP2 1#: 5′-AATCAAGTGGGAGAGTTCCCT-3′, Si SREBP2 2#: 5′-AAGCTAAGACCAGCGCCCGGG-3′, Si HMGCR 1#: 5′-AAGTCATAGTGGGGACAGTGA-3′, SiHMGCR 2#: 5′-AACCAGAAATGTGATTCAGTA-3′, Si c-Myc 1#: 5′-AACGTTAGCTTCACCAACAGG-3′ and Si c-Myc 2#: 5′-AACCAGAGTTTCATCTGCGAC-3′.
Glutathione S-transferase (GST) pull-down assay
The GST-Myc fusion protein was purified using GST Protein Interaction Pull-Down kit (21516; Pierce; Thermo Fisher Scientific, Inc.). Caes17 cells were harvested using RIPA buffer. Then, the cell lysates were centrifugated (12,000 × g at 4°C for 20 min). Subsequently, 10 µg GST-Myc protein was incubated with the lysates of Caes17 cells at 4°C overnight. Sepharose 4B beads were added to the supernatant and incubated for 4 h at 4°C. Protein binding to GST-Myc was immunoprecipitated and analyzed by 8% SDS-PAGE with an anti-GST antibody (1:5,000, ab19256, Abcam). The blots were examined using a Bio-Rad imaging system.
HMGCR promoter assay
The promoter region (−2000bp-1bp) of HMGCR was cloned into pGL3 basic vectors using Mlu I and Bgl II. For the reporter assay, cells in each well were transfected with 0.05 µg HMGCR promoter, 0.01 µg TK as control, and 0.25 µg c-Myc expression vectors. After 24 h later, cells were harvested using the lysis buffer, and the reporter activity were measured using a dual-luciferase kit (Promega Corporation) according to the manufacturer's protocols.
Immunoprecipitation assay
Caes 17 cells (6×105) were seeded into a 10 cm dish. After 24 h, the cells were lysed with immunoprecipitation lysis buffer (9806; Cell Signaling Technology, Inc.). The cell lysates were incubated with Flag (1:1,000; ab205606; Abcam) and c-Myc (1:500; 12189; Cell Signaling Technology, Inc.) primary antibodies at 4°C overnight. Protein A Sepharose CL-4B antibody purification resin (GE Healthcare Life Sciences, Little Chalfont, UK) were added to the supernatant and incubated for 4 h at 4°C. The beads were washed three times using lysis buffer (0.05% Tween-20). The bound protein was immunoprecipitated and analyzed by 8% SDS-PAGE (Sangon, Shanghai). The blots were examined using Bio-Rad image system.
Chromatin immunoprecipitation (ChIP) assay
ChIP assays were performed according to the manufacturer's protocol (Cell Signaling Technology, Inc.). KYSE180 cells were cross-linked with 1% formaldehyde for 10 min at room temperature. Subsequently, 1.0 M glycine was added to a final concentration of 125 mM to terminate the cross-linking reaction via incubation for 5 min at room temperature. The cells were collected, resuspended and sonicated (100 Hz) six times for 5 sec with the 1 min interval between each sonication, to shear the chromatin into 200-to 1,000-bp fragments; one-third of the lysate was used as the input following cross-link reversal, phenol/chloroform extraction and ethanol precipitation. The remaining two-thirds of the lysate were subjected to immunoprecipitation with an anti-Myc antibody (1:1,000; 12189) or IgG (1:1,000; 14708; both Cell Signaling Technology, Inc.) at 4°C overnight. The immunoprecipitated complexes were collected using Protein G-Sepharose beads. The precipitates were sequentially subjected to cross-link reversal in 300 mM NaCl at 65°C for 8 h, phenol/chloroform (1:1 mixture) extraction to remove the protein by centrifugation at 12,000 × g and 4°C for 20 min and 75% ethanol precipitation on ice for 4 h. Following centrifugation (12,000 × g for 15 min), the supernatant was removed, and the DNA was resuspended in 40 µl double-distilled water for qPCR analysis (2X SYBR-Green mixture, Takara Biotechnology Co., Ltd.). The thermocycling conditions were: 95°C for 2 min; then 45 cycles of 94°C for 15 sec, 55°C for 15 sec and 68°C for 30 sec. The primers were: F, 5′-CAAGGTCGGGAGTGATGATG-3′ and R, 5′-TTCCTGTGCGAACCTTAC-3′. 18S was used as an internal control. The expression of SREBP2 was expressed as Ct (18S-SREBP2).
Statistical analysis
The results are presented as the mean ± standard deviation. The experiments were repeated three times. Differences between values were statistically analyzed using a Student's t-test or one-way analysis of variance (ANOVA) using SPSS 15.0 (SPSS, Inc., Chicago, IL, USA). Turkey was used as the post hoc test for ANOVA. P<0.05 was considered to indicate a statistically significant difference.
Results
SREBP2 expression is increased in ESCC
Our previous study demonstrated that HMGCR was upregulated in ESCC, and statins, inhibitors of HMGCR, inhibited the growth and migration of ESCC cells (13). SREBP2 is the master regulator of HMGCR. Therefore, the expression profile of SREBP2 in ESCC tissues was investigated in the present study. The mRNA expression levels of SREBP2 in 52 ESCC tissues and paired non-cancerous tissues were detected; as presented in Fig. 1A, significantly increased SREBP2 mRNA expression levels were identified in the ESCC tissues compared with the non-cancerous tissues. In addition, the protein expression levels of SREBP2 in ESCC tissues were analyzed via immunohistochemistry and western blotting. SREBP2 protein expression levels were markedly increased in ESCC tissues compared with normal samples (Fig. 1B and C). Furthermore, SREBP2 expression in normal esophageal epithelial cells (Het-1A) and ESCC cells (KYSE150, KYSE180, Eca109 and Caes17) was investigated. As presented in Fig. 1D, decreased SREBP2 expression was detected in the normal Het-1A cells. The N-terminus of SREBP2 [SREBP2(N)] serves as a transcriptional factor following cleavage (16). Therefore, the expression levels of the active form of SREBP2 in ESCC tissues and cell lines were additionally detected. As presented in Fig. 1C and D, SREBP2(N) was markedly upregulated in ESCC cell lines with the exception of the Eca109 cells; however, only a few ESCC tissue samples exhibited upregulated SREBP2(N) expression levels. These data suggested that SREBP2 is upregulated in ESCC.
Figure 1.
SREBP2 is upregulated in ESCC. (A) SREBP2 mRNA expression levels in ESCC tissues and paired non-cancerous tissues were examined by reverse transcription-quantitative polymerase chain reaction. 18S rRNA was used as an internal control. The Cq values (18S-SREBP2) were plotted. (B) SREBP2 protein expression levels in ESCC tissues and paired non-cancerous tissues were examined by immunohistochemistry. (C) Total SREBP2 and SREBP2(N) protein expression levels in ESCC tissues and paired non-cancerous tissues were examined by western blot analysis. (D) Total SREBP2 and SREBP2(N) protein expression levels in normal esophageal epithelial cells and ESCC cells were examined by western blot analysis. C, cancer; N, normal; SREBP2, sterol regulatory element-binding protein 2; SREBP2(N), N-terminal of SREBP2; ESCC, esophageal squamous cell carcinoma.
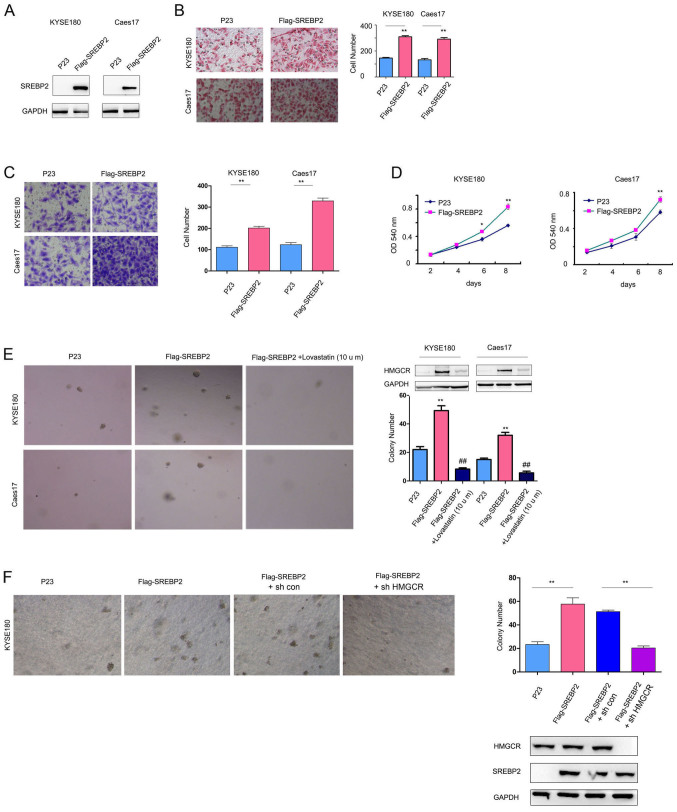
SREBP2 promotes ESCC cell viability, colony formation and migration
To study the biological functions of SREBP2 in ESCC, SREBP2 was overexpressed in KYSE180 and Caes17 cells, which had low expression levels of SREBP2 (Fig. 1D, Fig. 2A). SREBP2 overexpression significantly increased the KYSE180 and Caes17 cell migration and invasion in Boyden chamber assays and Transwell assays, respectively (Fig. 2B and C). Additionally, SREBP2 significantly promoted the growth and colony formation of KYSE180 and Caes17 cells in liquid culture and on the soft agar compared with the empty vector, P23 (Fig. 2D and E). Lovastatin (10 mg/l), an HMGCR inhibitor (17), significantly decreased the promoting effects of SREBP2 on the anchorage-independent growth of Caes17 and KYSE180 cells (Fig. 2E). Upregulated HMGCR expression levels were observed in Caes17 and KYSE180 cells overexpressing SREBP2; however, expression levels of HMGCR were decreased in cells treated with lovastatin (Fig. 2E). To investigate the effects of HMGCR expression on the malignant phenotype associated with SREBP2, HMGCR expression was downregulated in the present study. As presented in Fig. 2F, knockdown of HMGCR expression inhibited the anchorage-independent growth of KYSE180 cells compared with the control cells. These results suggested that SREBP2 promoted ESCC cell tumorigenesis by enhancing HMGCR activity.
Figure 2.
SREBP2 promotes ESCC cell viability, invasion and migration. (A) Constitutive SREBP2 expression in Caes17 and KYSE180 cells. Effects of SREBP2 on ESCC cell (B) migration and (C) invasion were evaluated using Boyden chamber and Transwell assays. Magnification, ×20. (D) Effects of SREBP2 on ESCC cell viability were evaluated via MTT assays. (E) Effects of SREBP2 on the anchorage-independent growth of ESCC cells were evaluated by a soft agar assay; treatment with lovastatin rescued the effects of SREBP2. Magnification, ×20. (F) Roles of HMGCR in the anchorage-independent growth of ESCC cells induced by SREBP2. Magnification, ×20. *P<0.05, **P<0.01 vs. respective P23; ##P<0.01 vs. respective Flag-SREBP2. sh, short hairpin RNA; SREBP2, sterol regulatory element-binding protein 2; ESCC, esophageal squamous cell carcinoma; HMGCR, 3-hydroxy 3-methylglutaryl coenzyme A reductase; OD, optical density.
To further examine the functions of endogenous SREBP2, the expression of SREBP2 was downregulated in Caes17 and KYSE180 cells (Fig. 3A). As presented in Fig. 3B and C, SREBP2 knockdown significantly inhibited the anchorage-independent growth and migration of ESCC cells compared with the control (Fig. 3B and C; P<0.01). Collectively, these results demonstrated that SREBP2 may promote ESCC cell growth and migration.
Figure 3.
Downregulation of SREBP2 inhibits ESCC cell growth and migration. (A) Knockdown of SREBP2 expression in ESCC cells. (B) Effects of SREBP2 knockdown on ESCC cell migration were evaluated using Boyden chamber assays. Magnification, ×20. (C) Effects of SREBP2 knockdown on the anchorage-independent growth of ESCC cells were evaluated by soft agar assays. Magnification, ×20. **P<0.01 vs. respective sh con. Con, control; sh, short hairpin RNA; SREBP2, sterol regulatory element-binding protein 2; ESCC, esophageal squamous cell carcinoma.
SREBP2 interacts with c-Myc in ESCC cells
The present study screened the binding partners of SREBP2 in ESCC cells via mass spectrometry (data not shown). c-Myc was identified as a potential binding partner for SREBP2. Therefore, the interaction between c-Myc and SREBP2 was investigated via GST pull-down assays. As presented in Fig. 4A, the fusion protein GST-Myc bound to SREBP2 in Caes17 cells. In addition, exogenously expressed c-Myc [hemagglutinin (HA)-Myc] and SREBP2 (Flag-SREBP2) co-transfected with Lipofectamine® 2000 (Invitrogen; Thermo Fisher Scientific, Inc.) formed a complex in Caes17 cells (Fig. 4B). Furthermore, endogenously expressed c-Myc and SREBP2 interacted with each other (Fig. 4C). Collectively, these data suggested that c-Myc and SREBP2 form a complex.
Figure 4.
SREBP2 interacts with c-Myc in ESCC cells. (A) A GST pull-down assay was performed to examine the interaction between c-Myc and SREBP2. (B) IP assays were performed to examine the interaction between exogenously expressed c-Myc and SREBP2. (C) Immunoprecipitation assays were performed to examine the interaction between endogenously expressed c-Myc and SREBP2. GST, glutathione S-transferase; HA, human influenza hemagglutinin; SREBP2, sterol regulatory element-binding protein 2; ESCC, esophageal squamous cell carcinoma; IP, immunoprecipitation.
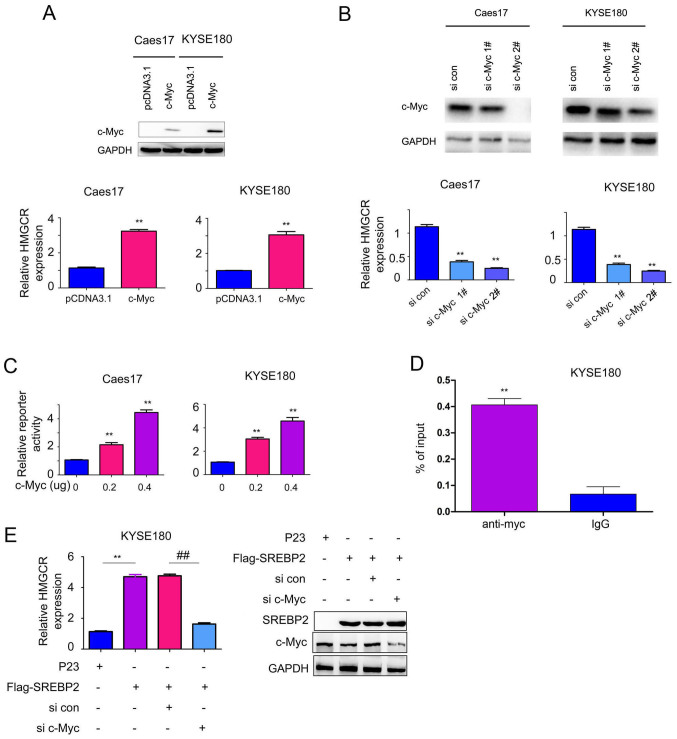
C-Myc is essential for SREBP2-induced HMGCR expression
To further investigate the function of the interaction between c-Myc and SREBP2, the effects of c-Myc on HMGCR expression were studied. Overexpression of c-Myc significantly increased the mRNA expression levels of HMGCR in Caes17 and KYSE180 cells compared with the control (Fig. 5A; P<0.01), whereas, knockdown of c-Myc expression significantly inhibited HMGCR expression compared with the control (Fig. 5B; P<0.01). Additionally, whether c-Myc activates HMGCR promoter activity was investigated in the present study. As presented in Fig. 5C, c-Myc significantly activated the HMGCR promoter in a dose-dependent manner compared with the control group (P<0.01) in KYSE180 cells. Additionally, c-Myc was determined to directly bind the HMGCR promoter via ChIP assays (Fig. 5D). Collectively, these data suggested that c-Myc induced HMGCR expression.
Figure 5.
C-Myc promotes HMGCR expression. (A) c-Myc overexpression upregulated HMGCR mRNA expression levels. **P<0.01 vs. respective c-Myc. (B) Knockdown of c-Myc downregulated HMGCR mRNA expression levels. **P<0.01 vs. respective si con. (C) c-Myc activated the HMGCR promoter. **P<0.01 vs. respective 0 µg c-Myc. (D) Chromatin immunoprecipitation assay reveals c-Myc binding to the HMGCR promoter. Quantitative polymerase chain reaction was performed. **P<0.01 vs. IgG. (E) c-Myc knockdown rescued the effects of SREBP2 on promoting HMGCR expression. **P<0.01; ##P<0.01. con, control; HMGCR, 3-hydroxy 3-methylglutaryl coenzyme A reductase; si, small interfering RNA; SREBP2, sterol regulatory element-binding protein 2; IgG, immunoglobulin G.
Based on the interaction between c-Myc and SREBP2, the present study subsequently investigated whether c-Myc and SREBP2 cooperate to regulate HMGCR expression. As presented in Fig. 5E, downregulation of c-Myc impaired the effects of SREBP2 in promoting HMGCR transcription. Collectively, these observations suggested that c-Myc is essential for SREBP2-induced HMGCR expression.
Discussion
Dysregulation of the MVA pathway has been demonstrated in numerous types of cancer (8,18,19). In our previous study, it was demonstrated that ESCC cells were very sensitive to treatment with statin (12). HMGCR, the target of statin, is upregulated in ESCC samples and promotes epithelial cell migration and transformation (13). In the present study, it was demonstrated that the expression of SREBP2, a regulator of HMGCR, was increased in ESCC. SREBP2 promoted the migration and invasive abilities, viability and anchorage-independent growth of ESCC. Additionally, the present study demonstrated that c-Myc is a binding partner of SREBP2 and cooperates with SREBP2 to enhance the expression of HMGCR. Collectively, these results suggested that the MVA pathway may be activated in ESCC, thus making ESCC sensitive to treatment with statin. These results potentially suggest a novel therapeutic target for ESCC.
A notable result of the present study is the identification of c-Myc as a binding protein of SREBP2. Recently, numerous transcriptional factors have been determined to be binding partners of the SREBP protein family (16). For example, mutant P53 interacts with SREBP and promotes the activation of the MVA pathway in breast cancer cells (20), suggesting that the MVA pathway is altered by oncogenes and tumor suppressors. A number of previous studies demonstrated the overexpression of c-Myc in ESCC (21–25). Therefore, it may be hypothesized that the upregulation of c-Myc cooperated with SREBP2 to activate the MVA pathway and promote tumorigenesis. In addition, numerous previous studies demonstrated the key roles of c-Myc in cancer metabolism (26–28). The results of the present study suggested that c-Myc regulates cholesterol synthesis by interacting with SREBP2.
In summary, the present study demonstrated the oncogenic roles of SREBP2 in ESCC-associated tumorigenesis, suggesting that SREBP2 may be a therapeutic target for ESCC.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National Science Foundation of China (grant no. 81401933) and Shanghai Science and Technology Committee (grant no. 13ZR1461300; Shanghai, China).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
CZ, LF, FY and HZ made substantial contributions to the design of the present study. CZ, LF, FY and ZL performed the experiments. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The present study was approved by the Institutional Ethics Committee of Shanghai Chest Hospital (Shanghai, China). All patients provided written informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67:7–30. doi: 10.3322/caac.21387. [DOI] [PubMed] [Google Scholar]
- 2.Schwartz L, Supuran CT, Alfarouk KO. The warburg effect and the hallmarks of cancer. Anticancer Agents Med Chem. 2017;17:164–170. doi: 10.2174/1871520616666161031143301. [DOI] [PubMed] [Google Scholar]
- 3.Munkley J, Elliott DJ. Hallmarks of glycosylation in cancer. Oncotarget. 2016;7:35478–35489. doi: 10.18632/oncotarget.8155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goldstein JL, Brown MS. Regulation of the mevalonate pathway. Nature. 1990;343:425–430. doi: 10.1038/343425a0. [DOI] [PubMed] [Google Scholar]
- 5.Landau BR, Brunengraber H. Shunt pathway of mevalonate metabolism. Methods Enzymol. 1985;110:100–114. doi: 10.1016/S0076-6879(85)10065-0. [DOI] [PubMed] [Google Scholar]
- 6.Weinberger C. A model for farnesoid feedback control in the mevalonate pathway. Trends Endocrinol Metab. 1996;7:1–6. doi: 10.1016/1043-2760(95)00180-8. [DOI] [PubMed] [Google Scholar]
- 7.Bathaie SZ, Ashrafi M, Azizian M, Tamanoi F. Mevalonate pathway and human cancers. Curr Mol Pharmacol. 2017;10:77–85. doi: 10.2174/1874467209666160112123205. [DOI] [PubMed] [Google Scholar]
- 8.Swanson KM, Hohl RJ. Anti-cancer therapy: Targeting the mevalonate pathway. Curr Cancer Drug Targets. 2006;6:15–37. doi: 10.2174/156800906775471743. [DOI] [PubMed] [Google Scholar]
- 9.Wang T, Seah S, Loh X, Chan CW, Hartman M, Goh BC, Lee SC. Simvastatin-induced breast cancer cell death and deactivation of PI3K/Akt and MAPK/ERK signalling are reversed by metabolic products of the mevalonate pathway. Oncotarget. 2016;7:2532–2544. doi: 10.18632/oncotarget.6304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Madison BB. Srebp2: A master regulator of sterol and fatty acid synthesis. J Lipid Res. 2016;57:333–335. doi: 10.1194/jlr.C066712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ma K, Malhotra P, Soni V, Hedroug O, Annaba F, Dudeja A, Shen L, Turner JR, Khramtsova EA, Saksena S, et al. Overactivation of intestinal SREBP2 in mice increases serum cholesterol. PLoS One. 2014;9:e84221. doi: 10.1371/journal.pone.0084221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shi J, Zhu J, Zhao H, Zhong C, Xu Z, Yao F. Mevalonate pathway is a therapeutic target in esophageal squamous cell carcinoma. Tumour Biol. 2013;34:429–435. doi: 10.1007/s13277-012-0567-0. [DOI] [PubMed] [Google Scholar]
- 13.Zhong C, Fan L, Yao F, Shi J, Fang W, Zhao H. HMGCR is necessary for the tumorigenecity of esophageal squamous cell carcinoma and is regulated by Myc. Tumour Biol. 2014;35:4123–4129. doi: 10.1007/s13277-013-1539-8. [DOI] [PubMed] [Google Scholar]
- 14.Xie JJ, Xu LY, Wu JY, Shen ZY, Zhao Q, Du ZP, Lv Z, Gu W, Pan F, Xu XE, et al. Involvement of CYR61 and CTGF in the fascin-mediated proliferation and invasiveness of esophageal squamous cell carcinomas cells. Am J Pathol. 2010;176:939–951. doi: 10.2353/ajpath.2010.090118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 16.Mukherjee M, Basu Ball W, Das PK. Leishmania donovani activates SREBP2 to modulate macrophage membrane cholesterol and mitochondrial oxidants for establishment of infection. Int J Biochem Cell Biol. 2014;55:196–208. doi: 10.1016/j.biocel.2014.08.019. [DOI] [PubMed] [Google Scholar]
- 17.Kajinami K, Takekoshi N, Brousseau ME, Schaefer EJ. Pharmacogenetics of HMG-CoA reductase inhibitors: exploring the potential for genotype-based individualization of coronary heart disease management. Atherosclerosis. 2004;177:219–234. doi: 10.1016/j.atherosclerosis.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 18.Caruso MG, Notarnicola M. Biochemical changes of mevalonate pathway in human colorectal cancer. Anticancer Res. 2005;25:3393–3397. [PubMed] [Google Scholar]
- 19.Andela VB, Pirri M, Schwarz EM, Puzas EJ, O'Keefe RJ, Rosenblatt JD, Rosier RN. The mevalonate synthesis pathway as a therapeutic target in cancer. Clin Orthop Relat Res (415 Suppl) 2003:S59–S66. doi: 10.1097/01.blo.0000093846.72468.66. [DOI] [PubMed] [Google Scholar]
- 20.Freed-Pastor WA, Mizuno H, Zhao X, Langerød A, Moon SH, Rodriguez-Barrueco R, Barsotti A, Chicas A, Li W, Polotskaia A, et al. Mutant p53 disrupts mammary tissue architecture via the mevalonate pathway. Cell. 2012;148:244–258. doi: 10.1016/j.cell.2011.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gomes TS, Noguti J, Forones NM, Lima FO, Dobo C, Fernandes Junior JA, Oshima CT, Ribeiro DA. Correlation analysis of c-myc, p21(WAF/CIP1), p53, C-erbB-2 and COX-2 proteins in esophageal squamous cell carcinoma. Pathol Res Pract. 2013;209:6–9. doi: 10.1016/j.prp.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 22.Brown J, Bothma H, Veale R, Willem P. Genomic imbalances in esophageal carcinoma cell lines involve Wnt pathway genes. World J Gastroenterol. 2011;17:2909–2923. doi: 10.3748/wjg.v17.i24.2909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang W, Xue L, Wang P. Prognostic value of β-catenin, c-myc, and cyclin D1 expressions in patients with esophageal squamous cell carcinoma. Med Oncol. 2011;28:163–169. doi: 10.1007/s12032-010-9436-0. [DOI] [PubMed] [Google Scholar]
- 24.Ishizuka T, Tanabe C, Sakamoto H, Aoyagi K, Maekawa M, Matsukura N, Tokunaga A, Tajiri T, Yoshida T, Terada M, Sasaki H. Gene amplification profiling of esophageal squamous cell carcinomas by DNA array CGH. Biochem Biophys Res Commun. 2002;296:152–155. doi: 10.1016/S0006-291X(02)00836-7. [DOI] [PubMed] [Google Scholar]
- 25.Mandard AM, Hainaut P, Hollstein M. Genetic steps in the development of squamous cell carcinoma of the esophagus. Mutat Res. 2000;462:335–342. doi: 10.1016/S1383-5742(00)00019-3. [DOI] [PubMed] [Google Scholar]
- 26.Shukla SK, Gunda V, Abrego J, Haridas D, Mishra A, Souchek J, Chaika NV, Yu F, Sasson AR, Lazenby AJ, et al. MUC16-mediated activation of mTOR and c-Myc reprograms pancreatic cancer metabolism. Oncotarget. 2015;6:19118–19131. doi: 10.18632/oncotarget.4078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller DM, Thomas SD, Islam A, Muench D, Sedoris K. c-Myc and cancer metabolism. Clin Cancer Res. 2012;18:5546–5553. doi: 10.1158/1078-0432.CCR-12-0977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gordan JD, Thompson CB, Simon MC. HIF and c-Myc: Sibling rivals for control of cancer cell metabolism and proliferation. Cancer cell. 2007;12:108–113. doi: 10.1016/j.ccr.2007.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.