TO THE EDITOR:
Psoriasis is a chronic inflammatory skin disease affecting about 3 percent of the population (Rachakonda et al., 2014). Over the past decade, more evidence has been published suggesting psoriasis is not just a disease of the skin but a disease of systemic inflammation predisposing patients to other medical comorbidities. Previous large, population-based studies have found that patients with psoriasis have higher rates of serious infections requiring hospitalization compared to adults without psoriasis, with lower respiratory tract infections, including pneumonia, being most common (Kao et al., 2014; Takeshita et al., 2018; Wakkee et al., 2011). Some respiratory infections are preventable through vaccination, but little is known about vaccination rates in psoriatic patients in the United States. Therefore, the objective of this study is to measure the rate of seasonal influenza vaccination in psoriasis patients in the United States and compare it to the rate of influenza vaccination in patients with other chronic diseases: rheumatoid arthritis and hypertension. Additionally, in psoriasis patients only, we sought to examine patient factors associated with receipt of a vaccination.
We performed a cohort study using U.S. based administrative and commercial claims data from OptumInsight Clinformatics DataMart, including all adults (≥18 years of age) with a diagnosis of psoriasis, rheumatoid arthritis or chronic hypertension requiring oral anti-hypertensive therapy and continuous enrollment during the 2010-2011 influenza season and 24 months prior (September 2008 – March 2011). Because this was an analysis of de-identified data, the study was granted an exempt status by the institutional review board at the University of Pennsylvania. The primary outcome was an inpatient, outpatient or pharmacy claim for an influenza vaccine during the 2010-2011 flu season: September 2010 – March 2011. This flu season was selected because it was considered “typical”, by the Centers for Disease Control (CDC, 2011). Measured covariates were age, gender, region of residency, and a history of any of the following medical comorbidities considered to confer higher risk for developing complications of influenza: asthma, congestive heart failure, chronic kidney disease, chronic liver disease, chronic obstructive pulmonary disease, human immunodeficiency virus (HIV), smoking, history of solid organ transplant and history of malignancy. A previously validated algorithm designed to identify smoking history in medical claims data was used (Chen et al., 2013). For patients with psoriasis and rheumatoid arthritis, information about treatments (including phototherapy) in the three months prior to the start of flu season (6/1/2010 – 8/31/2010) was also collected. Logistic regression was used to estimate the odds of vaccination in patients with chronic hypertension and rheumatoid arthritis compared to those with psoriasis, controlling for age, sex and treatment (RA only). Finally, in psoriasis patients only, patient factors associated with receipt of a vaccine were identified using multivariable logistic regression.
There were 17,078 patients with psoriasis, 21,832 with rheumatoid arthritis and 496,972 with chronic hypertension requiring oral therapy (Table). Patients with psoriasis were younger than those with rheumatoid arthritis and chronic hypertension. As expected, 73% of patients with rheumatoid arthritis were female compared to 49.8% and 50.6% of patients with psoriasis and chronic hypertension, respectively. A history of psoriatic arthritis was present in 11% of psoriasis patients, and the prevalence of comorbidities was similar to what has been reported in the literature previously (Shah et al., 2017).
Table:
Characteristics of the Study Population and Mutually Adjusted Odds Ratios for the Association of Receipt of an Influenza Vaccination in Patients with Psoriasis
| Chronic HTN N = 496,972 |
RA N = 21,832 |
Psoriasis N = 17,078 |
OR (95% CI) *Psoriasis patients only* |
|
|---|---|---|---|---|
| Female, N (%) | 251,059 (50.6) | 16,053 (73.6) | 8500 (49.8) | 1.29 (1.20 – 1.38) |
| Mean age, in yrs (SD) | 60.8 (13.2) | 58.6 (14.3) | 52.7 (15.0) | 1.03 (1.02 – 1.03) |
| History of smoking, N (%) | 46,820 (9.4) | 2136 (9.8) | 1675 (9.8) | 1.10 (0.98 – 1.24) |
| Treatment with systemic agent, N (%) | N/A | 9618 (44.0) | 2684 (15.7) | 1.03 (0.98 – 1.24) |
| Medical Comorbidities | ||||
| Asthma | 46,071 (9.3) | 2950 (13.5) | 1598 (9.4) | 1.58 (1.40 – 1.77) |
| Chronic Kidney Disease | 41,159 (8.3) | 1634 (7.5) | 580 (3.4) | 0.97 (0.81 – 1.17) |
| Chronic Liver Disease | 15,868 (3.2) | 825 (3.8) | 623 (3.7) | 1.23 (1.03 – 1.47) |
| COPD | 23,048 (4.6) | 1481 (6.8) | 607 (3.6) | 1.04 (0.87 – 1.25) |
| CHF | 38,111 (7.7) | 1655 (7.6) | 575 (3.4) | 0.88 (0.73 – 1.07) |
| Diabetes | 152,430 (30.7) | 4830 (22.1) | 2851 (16.7) | 1.48 (1.36 – 1.63) |
| HIV | 1361 (0.3) | 82 (0.4) | 48 (0.3) | 3.68 (2.06 – 6.57) |
| History of Malignancy | 68,267 (13.7) | 3013 (13.8) | 2119 (12.4) | 1.21 (1.09 – 1.34) |
| Psoriatic Arthritis | - | - | 1872 (11.0) | 1.40 (1.25 – 1.58) |
| History of Organ Transplant | 3647 (0.7) | 100 (0.5) | 58 (0.3) | 1.47 (0.86 – 2.53) |
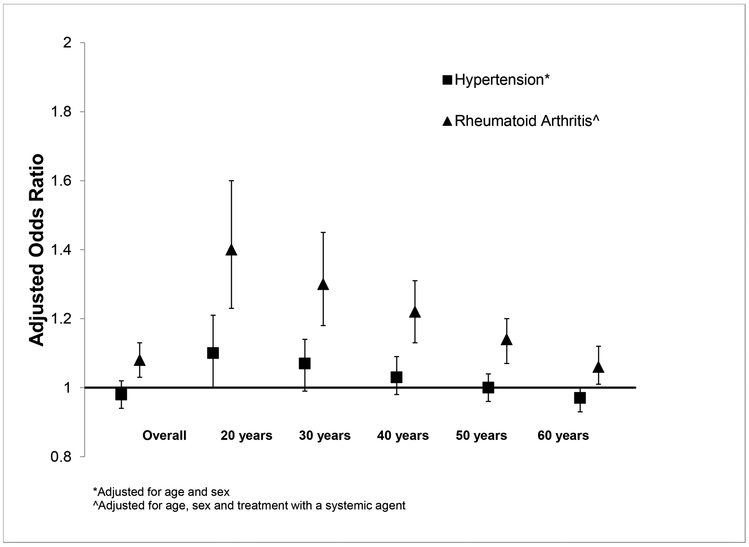
After controlling for age and sex, patients with chronic hypertension had similar odds of receiving an influenza vaccination as patients with psoriasis (OR: 0.98, 95% CI: 0.94 – 1.02). Adults with rheumatoid arthritis were approximately 10% more likely to receive a flu vaccination than psoriasis patients (OR: 1.08, 95% CI: 1.03 – 1.13), after controlling for age, sex and treatment with systemic therapy; however the likelihood of receiving a flu vaccination varied by age (Figure). For example, a 30-year-old patient with RA was 30% more likely to receive an influenza vaccine than a 30-year-old with psoriasis (OR: 1.30, 95% CI: 1.18 – 1.45), but a 70-year-old patient with rheumatoid arthritis had a similar likelihood of receiving a flu vaccination as a 70-year-old with psoriasis.
Figure: Likelihood of Receiving an Influenza Vaccination in Patients with Hypertension and Rheumatoid Arthritis Compared to Patients with Psoriasis, during the 2010-2011 influenza season.
Adjusted odds ratios for the likelihood of receiving an influenza vaccination in patients with hypertension (square) and rheumatoid arthritis (triangle) compared to psoriasis patients during the 2010-2011 influenza season.
In psoriasis patients, factors associated with the receipt of vaccine, including medical comorbidities identified by the Centers for Disease Control and Prevention as high risk for developing influenza related complications, were examined. In the multivariable model 8 factors were associated with an increased likelihood of receiving an influenza vaccine: age, female gender, and history of asthma, chronic liver disease, diabetes, human immunodeficiency virus (HIV), cancer, and psoriatic arthritis (Table). Treatment with a systemic agent (oral systemic agent or biologic therapy) was not associated with an increased likelihood of vaccination.
In conclusion, patients with rheumatoid arthritis are more likely to receive a flu vaccine than patients with psoriasis and this difference is magnified in people younger than 50 year of age. In patients with psoriasis, increasing age, female gender and having other chronic medical conditions was associated with receipt of a flu vaccine. Additional research is necessary to better understand psoriasis-specific vaccination beliefs and behaviors. In this study, psoriasis patients were younger and had lower rates of certain chronic diseases, including chronic kidney disease, chronic obstructive pulmonary disease, congestive heart failure, and diabetes, which may lead to a lower perception of flu risk. Patient with psoriasis may also have concerns about the safety of receiving vaccinations, especially while on systemic therapies. Additionally, psoriasis patients may not receive adequate counseling from physicians. A survey of American households found the majority of adults who received a vaccination during the 2009-2010 influence season reported that healthcare providers were the most influential information source regarding the flu vaccine (Maurer et al., 2010), suggesting dermatologists can potentially be an important resource for psoriasis patients. For younger psoriasis patients, a dermatologist may be the only healthcare provider they see regularly, making it important for dermatologist to provide counseling about recommended vaccinations. While this is a large, population-based study examining influenza vaccination rates in patients with psoriasis, there are some limitations to the use of administrative claims data to study vaccination rates including misclassification and lack of generalizability to patients with other types of insurance or without insurance. Further research understanding why adults with psoriasis do not receive recommended vaccinations will help to create targeted interventions to improve vaccination rates and decrease hospitalizations in adults with psoriasis.
ACKNOWLEDGEMENTS:
This work was supported by an early career research grant from the National Psoriasis Foundation (MHN), NIH Training Grant T32-GM075766 (MHN), a career development award from the Dermatology Foundation (MHN) and K24-AR064310 36 (JMG) from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (JMG).
Abbreviations:
- DMARD
disease modifying antirheumatic drug
- HIV
human immunodeficiency virus
- RA
rheumatoid arthritis
Footnotes
CONFLICTS OF INTEREST: Dr. Gelfand served as a consultant for BMS, Boehringer Ingelheim, GSK, Janssen Biologics, Novartis Corp, UCB (DSMB), and Pfizer Inc., receiving honoraria; and receives research grants (to the Trustees of the University of Pennsylvania) from Abbvie, Janssen, Novartis Corp, Celgene, Ortho Dermatologics, and Pfizer Inc.; and received payment for continuing medical education work related to psoriasis that was supported indirectly by Lilly and Ortho Dermatologics. Dr Gelfand is a Deputy Editor for the Journal of Investigative Dermatology receiving honoraria from the Society for Investigative Dermatology. The other authors state no conflicts of interest.
REFERENCES:
- CDC (2011) Final state-level influenza vaccination coverage estimates for the 2010-11 season - United States, National Immunication Survey and Behavorial Risk Factor Surveillance System, August 2010 through May 2011. Accessed April 17, 2016. [Google Scholar]
- Chen LH, Quinn V, Xu L, Gould MK, Jacobsen SJ, Koebnick C, et al. The accuracy and trends of smoking history documentation in electronic medical records in a large managed care organization. Subst Use Misuse 2013;48:731–42. [DOI] [PubMed] [Google Scholar]
- Kao LT, Lee CZ, Liu SP, Tsai MC, Lin HC Psoriasis and the risk of pneumonia: a population-based study. PLoS One 2014;9:e116077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maurer J, Uscher-Pines L, Harris KM Perceived seriousness of seasonal and A(H1N1) influenzas, attitudes toward vaccination, and vaccine uptake among U.S. adults: does the source of information matter? Prev Med 2010;51:185–7. [DOI] [PubMed] [Google Scholar]
- Rachakonda TD, Schupp CW, Armstrong AW Psoriasis prevalence among adults in the United States. J Am Acad Dermatol 2014;70:512–6. [DOI] [PubMed] [Google Scholar]
- Shah K, Mellars L, Changolkar A, Feldman SR Real-world burden of comorbidities in US patients with psoriasis. J Am Acad Dermatol 2017;77:287–92 e4. [DOI] [PubMed] [Google Scholar]
- Takeshita J, Shin DB, Ogdie A, Gelfand JM Risk of serious infection, opportunistic infection and herpes zoster among patients with psoriasis in the United Kingdom. J Invest Dermatol 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakkee M, de Vries E, van den Haak P, Nijsten T Increased risk of infectious disease requiring hospitalization among patients with psoriasis: a population-based cohort. J Am Acad Dermatol 2011;65:1135–44. [DOI] [PubMed] [Google Scholar]