Abstract
BACKGROUND:
Acute respiratory tract infections are the most common causes of both morbidity and mortality worldwid, and the management and prevention of acute respiratory infections is a global problem, especially in developing countries. This study sought to assess the community's compliance and practice of measures for the prevention of respiratory infections and discover their source of health information.
MATERIALS AND METHODS:
A cross-sectional study was carried out in the five biggest shopping malls in Riyadh city in July 2014. The required sample size was 980 persons aged 15 or older, with 196 from each of the five biggest shopping malls from each of the five geographic areas of Riyadh. Data was collected by face-to-face interview using standardised questionnaire, and analyzed using SPSS.
RESULTS:
Overall, 48.3% of the participants thought that they were susceptible to any of the respiratory infections of pandemic influenza; 59.7% always washed their hands with water and soap and 34.8% used antibacterial soap. About 29% reported avoiding touching their eyes, noses, and mouths directly with their hands; 63.5% covered their noses and mouths with tissue paper when sneezing or coughing. A substantial number said they “never” shared their personal stuff, including towels (70.5%) and utensils (49.0%) with others. Only 21.2% avoided crowded places or wore a mask (9.1%) in such a situation. A high proportion (62.8%) did not take the seasonal flu vaccine. The most common sources of health information included television/radio (47.9%), social media (29.4%), and friends/family (28.1%).
CONCLUSIONS:
Health authorities should seize every opportunity to prevent respiratory infections by adopting all evidence-based infection control measures to improve public awareness, attitude, and practice.
Keywords: Compliance, coronavirus, infection control, pandemic flu, respiratory infection
Introduction
Acute respiratory tract infections (ARTIs) are the most common causes of both morbidity and mortality worldwide, especially in developing countries.[1] In Saudi Arabia, viral pathogens are the most common of ARTIs with the highest detection rate in children.[2]
When large numbers of people come together for a social function, a huge public event or sports, there is a high risk of disseminating respiratory infections. Most respiratory infections are easily transmitted, but they have an incubation period of several days, during which they are most contagious.[3,4,5]
The world has learned from the recent emerging infectious diseases such as the severe acute respiratory syndrome in 2002, highly pathogenic influenza A virus subtype H5N1 (bird flu) in 2005, and H1N1 influenza (swine flu) in 2009; about the need to cooperate in developing better surveillance and control measures. Public health authorities should give priority to the improvement of the awareness of the public on infection control measures. The World Health Organization requires countries to report all new cases of emerging infectious diseases according to the International Health Regulations.[1] These global measures help countries to assess and increase their preparedness and readiness to the spread of infections.[6]
Nonpharmaceutical interventions (NPIs) routinely recommended for mitigating respiratory infections, include respiratory etiquette, hand hygiene, and routine cleaning of frequently touched surfaces and objects. Effective use of NPIs depends on the acceptance and participation of individuals who implement personal protective measures, and communities that implement communitywide measures.[7]
In a cross-sectional, probable multistage sampling study of patients over 18 years, 1600 participants (48.9% male) were interviewed in Mexico. The authors concluded that there was a higher acceptance rate for the pandemic influenza vaccine (with 90.6% willing to receive influenza A [H1N1] vaccine) compared to similar studies in other countries. The main reason given by 46.5% of participants for rejecting the vaccine was distrust; however, 34% had previously received the seasonal flu vaccine. Furthermore, 68% considered influenza A (H1N1) a risk to their families. The researchers reported that handwashing was the most common measure of infection prevention reported by 47.5%, followed by the influenza vaccine (28%). The level of education and age significantly influenced their objection to the vaccine.[8]
A descriptive analysis of a telephone survey was conducted in Spain on 1627 participants, (51.6% women, 66.5% aged between 18 and 55 years, 52.7% unskilled manual workers and 49.1% lived in cities larger than 50,000 inhabitants). Respondents perceptions, preventive measures, vaccination related to influenza (H1N1) were investigated. Only 15.7% felt that they were at risk of contracting influenza. However, in the second wave of this study, after the epidemic peak, the proportion of those who felt they were at risk of contracting influenza was much lower, at 3.9%. It was found that the main measures adopted were those recommended by the government.[9]
On the Mississippi Gulf Coast, when 216 residents were interviewed for the primary sources of their information during the 2009 influenza pandemic, most participants (98%) were aware of H1N1 influenza. The most frequent sources of information cited were television (TV, 69%), newspapers (19%), and the Internet (9%). The preventive measure most adopted was hand hygiene (41%); and that increased following the confirmation of the first influenza case.[10]
In a literature review based on the Health Belief Model, perceived susceptibility was the most significant factor that determined compliance. Moreover, perceived benefit of mask wearing was found to have a significant effect on compliance as well. Experience or perception of discomfort and sense of embarrassment were perceived barriers to the wearing of masks.[11]
When elementary schools, household caregivers, students, and their teachers were asked to participate in a survey, the NPI measures appeared to be high (90%) among teachers and the caregivers. It is essential to communicate the necessary information to the household caregivers and teachers through trusted sources.[12]
In a cross-sectional study of 340 inhabitants in Florida Blanca, the best-known preventative actions were handwashing and use of surgical masks. Gender was associated with varying levels of knowledge, while the awareness of preventative action was associated with exposure to the media. Educational attainment was related to symptom control measures, and age was associated with the duration of handwashing and the use of quarantine.[13]
Another cross-sectional study involving face-to-face interviews of 221 respondents in Tampin, Negeri Sembilan reported that 88.9% and 85.8%, respectively, indicated that they covered their mouths when coughing and sneezing with tissue paper or handkerchief. When coughing or sneezing 91.2% and 88.9%, respectively turned their faces away. The previous respondents disposed of their used paper tissues properly in a waste bin, and 91.2% claimed that they did not spit in public areas. The vast majority used water and soap to wash their hands before eating (93.8%) and after using the lavatory (98.7%). However, 81.9% washed their hands if they covered their noses and mouths when they sneezed. Only 35.8% of the interviewees claimed to follow the handwashing steps given by the Ministry of Health. The use of face masks was moderate, with 76.5% of the respondents using face mask during a pandemic. Furthermore, 75.2% ensured that their face masks were properly fitted and covered their mouths and noses. About 74.3% wore the Ministry of Health recommended face masks during the pandemic. Slightly more than half of the respondents (54.0%) used face masks when they had influenza-like symptoms, and 40.3% admitted to reusing their face masks more than once. Respondents' practices on social distancing were appropriate. Those who avoided going to or taking their children unnecessarily to such crowded places as shopping areas were 88.9% and 83.2%, respectively. Only 64.6% practiced safety measures such as the wearing of face masks in crowded areas, and 30.1% used hand sanitizers when necessary. As for self-health care, the majority (79.2%) avoided sharing forks and spoons with friends during a meal. Only 37.2% of the respondents took the initiative to look for additional information on influenza A (H1N1) other than what was given by the government. About a third of the respondents took food supplements during the pandemic phase. A high percentage (68.6%) of the respondents did not wash their hands after shaking hands with other people. Ethnicity, education, income, and practice score predicted the knowledge score. Income and knowledge scores were predictors of practice score. There was a positive correlation between knowledge and practice scores.[14]
In Saudi Arabia, of the 1548 adult participants who were interviewed in various shopping malls in Riyadh and Jeddah; 54.3% were very concerned while 60.8% had taken minimal or no precautionary measures. Educational level was the only significant predictor of the degree of concern. Participants who were male, older, better educated, and more knowledgeable took more precautions than others. The Ministry of Health reports of the characteristics of the disease were not enough to convince 38.3% of participants, and only 16.1% of the participants reported receiving information from health providers. Frequent handwashing and face mask use in crowded areas were practiced by 57.7% and 56.2%, respectively. Moreover, 36.6% avoided touching their eyes, noses, or mouths; and 38.0% covered their mouths and noses when sneezing or coughing. Used tissues were disposed of in a bin after use by 26.9%, while 25.7% claimed that they avoided normal activities if they had flu-like symptoms.[15]
The objective of the present study was to measure the level of community compliance and practice of the measures for the prevention of respiratory infections and to identify the source of information of the measures for the prevention of respiratory infections.
Materials and Methods
An observational, quantitative, cross-sectional study was conducted in July 2014, in the five biggest shopping malls in each of the five geographic areas of Riyadh. The study participants were selected from these five malls. The inclusion criteria were persons older than 15 years and Arabic speakers.
The questionnaire which was prepared in Arabic by the authors had three main parts:
Sociodemographic, including age, gender, employment status, and the educational levels of participants
Assessment of the degree of public compliance and practice regarding preventive measures against respiratory infections.[1] was tested using a predesigned face-to-face interview questionnaire with close-ended answers (yes/no) to question on participants' perception of susceptibility to respiratory infections and the use of masks for preventing respiratory infection. The questions were Do you think you are susceptible to contracting any respiratory infection? Which type of mask do you wear in crowded places? Which type of mask do you wear in your daily life? Which type of mask do you wear around infected people?
Likert scale (always = 5, often = 4, sometimes = 3, rarely = 2, and never = 1) was used to illustrate the questions on participants' practices: Do you wash your hands with water and soap constantly?
Do you wash your hands with water and soap before eating? Are you keen on using antibacterial soap? Do you avoid touching your eyes, nose, and mouth directly with your hands?
Do you cover your nose and mouth when you sneeze or cough with tissue paper and dispose of it in the bin? If you do not have any tissue, do you use your elbow when you sneeze or cough?
Do you avoid crowded places? Do you wear a mask in crowded places? Do you wear a mask in your daily life? Do you avoid people with respiratory infections?
If you are around infected people, do you wear mask? Do you take the seasonal flu vaccine?
Which type of mask do you wear in crowded places? Which type of mask do you wear in your daily life? Which type of mask do you wear around infected people?
This scoring system was reversed in the case of questions (Do you share your personal stuff with others [like towels]? Do you share your personal stuff with others [like utensils]?). The total score from the 14 statements on practice for preventing respiratory infections was categorized into two as good (median score and above) and bad (below median score) practices.
-
3.
Population's source of information about the measures for the prevention of respiratory infections
The study instrument was reviewed by two family physicians, one infectious disease consultant, one community professor, and one biostatistician. All the above reviewers were academic staff.
A pilot study was conducted on 50 patients to check the applicability, clarity and cultural appropriateness, and to estimate the time required to complete the questionnaire. The questionnaires took approximately 15–20 min to complete. Those who participated in the pilot study were excluded from the main study. Assumingt 50% of persons were compliant and practiced the measures of prevention of respiratory infections, with ± 7% precision and 95% confidence level, the required sample size was 980, and 196 persons to be included from each of the five malls.
Ethical approval was obtained from the Institutional Review Board, and informed written consent was obtained from all the participants. The participants provided their information in strictly anonymous and confidential manner.
Data were analyzed using SPSS Pc+ version 21.0 statistical software (IBM, NY, USA). Frequencies and percentages were used to describe categorical data and outcome variables. Pearson Chi-square test and odds ratios were used to determine the association between independent variables and outcome variables. Binary logistic regression analysis was used to identify independent factors associated with poor practice for the prevention of respiratory infection. P < 0.05 and 95% confidence intervals were used to report the statistical significance of the results.
Results
Out of 980 registered study participants, 869 (90.5%) participated in this survey. The age distribution indicated that 20.9% and 21.9% were in the 15–20 and 26–30 years age groups, respectively, while 5.4% were >45 years old. Overall, 63.2% participants were female, 46.7% had university level of education, and 53.6% were employed [Table 1]. About 48.3% of the participants thought that they were susceptible to any of the respiratory infections due to seasonal influenza (88%), coronavirus infection (20.2%), N1H1 (3.6%), and bird flu (5.4%).
Table 1.
Sociodemographic characteristics of the study participants (n=869)
| Variables | Number (%) |
|---|---|
| Age groups (n=851) | |
| 15-20 | 178 (20.9) |
| 21-25 | 204 (24.0) |
| 26-30 | 186 (21.9) |
| 31-35 | 127 (14.9) |
| 36-40 | 72 (8.5) |
| 41-45 | 38 (4.5) |
| ≥46 | 46 (5.4) |
| Gender (n=856) | |
| Male | 315 (36.8) |
| Female | 541 (63.2) |
| Educational level (n=861) | |
| Illiterate | 27 (3.1) |
| Intermediate | 95 (11.0) |
| Secondary school | 306 (35.5) |
| University | 402 (46.7) |
| Post graduate | 31 (3.6) |
| Occupation (n=857) | |
| Student | 230 (26.8) |
| Unemployed | 154 (18.0) |
| Employed | 459 (53.6) |
| Retired | 14 (1.6) |
With regard to the participants' practices, 59.7% participants responded always washing hands with water and soap, and 62.5% responded always washing of hands with water and soap before meals. Only 34.8% “always” used anti-bacterial soap, and 29.8% reported “always” avoiding touching eyes, nose and mouth with their hands. About 63.5% reported “always” covering their noses and mouths with a tissue when they sneezed or coughed and disposed of it in a bin. Only 35.8% of them responded positively with “always” to the statement on using their elbow while they sneezed or coughed if they did not have a tissue paper. About 71% and 49.0% reported “never” sharing their personal stuff (towels), and utensils with others, respectively. Only 21.2% “always” avoided crowded places and 9.1% used masks in crowded places. About 66.8% never wore masks in their daily lives. Moreover, 45% avoided persons with respiratory infections. Overall, only 38.6% “always” wore masks when in the presence of infected people, and 62.8% did not take the seasonal flu vaccine. Furthermore, a larger proportion of the participants used surgical masks or they do not know (IDK) what to do while in crowded places in their daily lives, and when infected persons were around [Table 2 and Figure 1].
Table 2.
Participants’ perception of susceptibility to respiratory infections and use of mask for the prevention of respiratory infections (n=869)
| Questions | Yes N (%) | No N (%) |
|---|---|---|
| Do you think you are susceptible to any respiratory infection? | 402 (46.2) | 467 (53.7) |
| If yes, which of the following? (n=402)* | ||
| Seasonal flu | 344 (85.5) | 58 (14.4) |
| Corona | 79 (19.6) | 323 (80.3) |
| N1H1 | 14 (3.6) | 388 (96.5) |
| Bird flu | 21 (5.2) | 381 (94.7) |
| Which type of mask do you wear in crowded places? (n=376) | ||
| Surgical mask | 145 (38.6) | 231 (61.4) |
| N95 mask | 19 (5.1) | 357 (94.9) |
| Don’t know | 212 (56.4) | 164 (43.6) |
| Which type of mask do you wear in your daily life? (n=316) | ||
| Surgical mask | 133 (42.1) | 183 (57.9) |
| N95 mask | 12 (3.8) | 304 (96.2) |
| Don’t know | 171 (54.1) | 145 (45.8) |
| Which type of mask do you wear around infected people? (n=452) | ||
| Surgical mask | 214 (47.3) | 238 (52.6) |
| N95 mask | 32 (7.1) | 420 (92.9) |
| Don’t know | 206 (45.6) | 246 (54.4) |
*Multiple responses allowed
Figure 1.
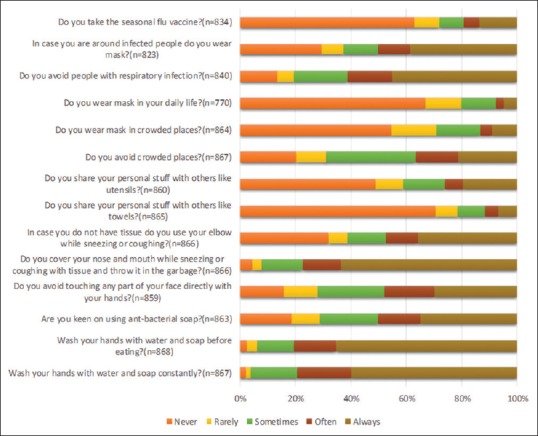
Participants practices toward preventing respiratory infection (n = 869). OR = Odds ratio, CI = Confidence interval. *Statistically significant
Of all participants, 49.7% had poor practices. There was significant association between age groups, gender, educational level, and occupation and the type of practice (bad and good). The unadjusted odds ratios for age groups (21–25, 26–30, 31–35, 36–40 and >46 years) gave significantly higher odds ratios (1.72, 1.96, 1.59, 1.81, and 2.76) compared with the younger age group (15–20 years) with poor practice. Moreover, being male showed a 1.40 times higher odds of having poor practice toward the prevention of respiratory infections compared with being female. Participants with no education had significantly higher odds of having poor practice compared with those with postgraduate education. Moreover, the odds of having poor practice were considerably higher among retired persons, employed, and unemployed participants (7.43, 2.58, and 2.13) compared with students. The binary multiple logistic regression analysis showed that only low educational level and occupation other than being a student were significantly associated with the poor practice of preventing respiratory infections. Participants with no education, intermediate education, and secondary school level education had higher odds of poor practice compared with those with postgraduate education. In comparison with being a student, all unemployed, employed, and retired participants had higher odds of having poor practice for the prevention of respiratory infections [Table 3].
Table 3.
Factors associated with poor practices for the prevention of respiratory infections among study participants
| Variables | Poor practice (n=432) N (%) | Good practice (n=437) N (%) | OR (95% CI) | AOR (95% CI) |
|---|---|---|---|---|
| Age groups (n=423; 428) | ||||
| 15-20 | 68 (16.1) | 110 (25.7) | 1.0 | 1.0 |
| 21-25 | 105 (24.8) | 99 (23.1) | 1.72 (1.14-2.58)* | 1.09 (0.64-1.84) |
| 26-30 | 102 (24.1) | 84 (19.6) | 1.96 (1.29-2.98)* | 0.97 (0.53-1.75) |
| 31-35 | 63 (14.9) | 64 (15.0) | 1.59 (1.0-2.52)* | 0.73 (0.38-1.37) |
| 36-40 | 38 (9.0) | 34 (7.9) | 1.81 (1.04-3.14)* | 0.75 (0.37-1.52) |
| 41-45 | 18 (4.3) | 20 (4.7) | 1.46 (0.72-2.95) | 0.54 (0.23-1.27) |
| ≥46 | 29 (6.9) | 17 (4.0) | 2.76 (1.41-5.40)* | 0.99 (0.42-2.30) |
| Gender (n=422;434) | ||||
| Male | 172 (40.8) | 143 (32.9) | 1.40 (1.06-1.85)* | 1.18 (0.83-1.66) |
| Female | 250 (59.2) | 291 (67.1) | 1.0 | 1.0 |
| Educational level (n=426; 435) | ||||
| Illiterate | 18 (4.2) | 9 (2.1) | 3.64 (1.23-10.78)* | 5.11 (1.52-17.18)* |
| Intermediate | 51 (12.0) | 44 (10.1) | 2.11 (0.91-4.88) | 3.22 (1.31-7.93)* |
| Secondary school | 158 (37.1) | 148 (34.0) | 1.94 (0.90-4.19) | 2.73 (1.20-6.24)* |
| University | 188 (44.1) | 214 (49.2) | 1.60 (0.75-3.42) | 2.01 (0.89-4.54) |
| Post graduate | 11 (2.6) | 20 (4.6) | 1.0 | 1.0 |
| Occupation (n=423; 434) | ||||
| Student | 76 (18.0) | 154 (35.5) | 1.0 | 1.0 |
| Unemployed | 79 (18.7) | 75 (17.3) | 2.13 (1.40-3.24)* | 2.03 (1.31-3.14)* |
| Employed | 257 (60.8) | 202 (46.5) | 2.58 (1.85-3.59)* | 2.90 (2.06-4.09)* |
| Retired | 11 (2.6) | 3 (0.7) | 7.43 (2.01-27.42)* | 14.34 (3.05-67.31)* |
*Statistically significant. OR=Odds ratio, AOR=Adjusted Odds ratio, CI=Confidence interval
The multiple responses to sources of information about respiratory infections included electronic media (TV/radio) from 47.9% of participants, followed by social media (WhatsApp and Twitter) among 29.4% and 28.1%, respectively; and the least with friends/family, doctors, magazine/newspaper, and campaigns [Figure 2].
Figure 2.
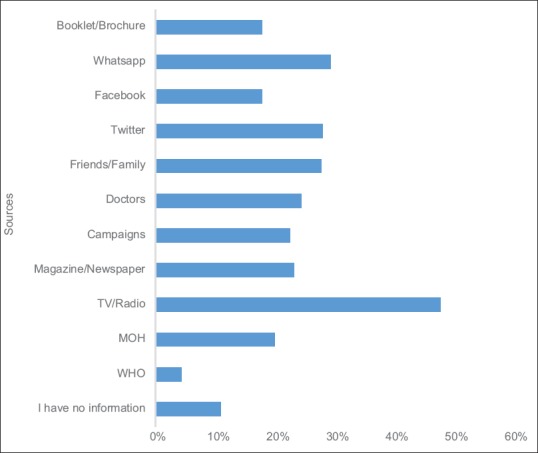
Sources of information about respiratory infection (n = 815). WHO = World Health Organization, MOH = Ministry of Health, TV = Television
Table 4 shows a comparison of the practices of those who considered themselves susceptible to respiratory infections and those who did not. The participants who perceived themselves susceptible to infections exhibit somewhat different preventive practices than their counterparts, but the differences were not statistically significant.
Table 4.
Comparison of the practices of those who consider themselves susceptible to respiratory infections and those who do not
| Susceptibility | Practice | P-Value | |||||
|---|---|---|---|---|---|---|---|
| Always N (%) | Often N (%) | Sometimes N (%) | Rarely N (%) | Never N (%) | |||
| Do you wash your hands with water and soap constantly? | Yes | 243 (60.8) | 74 (18.5) | 68 (17.0) | 6 (1.5) | 9 (2.3) | 0.85 |
| No | 275 (58.9) | 97 (20.8) | 76 (16.3) | 10 (2.1) | 9 (1.9) | ||
| Do you wash your hands with water and soap before eating? | Yes | 257 (63.9) | 63 (15.7) | 59 (14.7) | 15 (3.7) | 8 (2.0) | 0.68 |
| No | 309 (66.3) | 70 (15.0) | 56 (12.0) | 17 (3.6) | 14 (3.0) | ||
| Are you keen on using antibacterial soap? | Yes | 139 (34.8) | 63 (15.8) | 84 (21.0) | 33 (8.3) | 81 (20.3) | 0.52 |
| No | 161 (34.8) | 72 (15.6) | 97 (21.0) | 53 (11.4) | 80 (17.3) | ||
| Do you avoid touching your eyes, nose, and mouth directly with your hands? | Yes | 126 (31.7) | 76 (19.1) | 86 (21.7) | 46 (11.6) | 63 (15.9) | 0.45 |
| No | 130 (28.1) | 79 (17.1) | 122 (26.4) | 59 (12.8) | 72 (15.6) | ||
| Do you cover your nose and mouth when you sneeze or cough with a tissue and throw it in the bin? | Yes | 259 (64.6) | 58 (14.5) | 56 (14.0) | 11 (2.7) | 17 (4.2) | 0.76 |
| No | 291 (62.6) | 62 (13.3) | 72 (15.5) | 19 (4.1) | 21 (4.5) | ||
| If you have no tissue, do you use your elbow when you sneeze or cough? | Yes | 134 (33.3) | 49 (12.2) | 51 (12.7) | 26 (6.5) | 142 (35.3) | 0.25 |
| No | 176 (37.9) | 51 (11.0) | 69 (14.9) | 34 (7.3) | 134 (28.9) | ||
| Do you share your personal stuff with others (like towels)? | Yes | 22 (5.5) | 21 (5.3) | 35 (8.8) | 27 (6.8) | 294 (73.7) | 0.18 |
| No | 38 (8.2) | 19 (4.1) | 52 (11.2) | 41 (8.8) | 316 (67.8) | ||
| Do you share your personal stuff with others (like utensils)? | Yes | 81 (20.4) | 24 (6.0) | 68 (17.1) | 39 (9.8) | 186 (46.7) | 0.40 |
| No | 87 (18.8) | 34 (7.4) | 60 (13.0) | 46 (10.0) | 235 (50.9) | ||
| Do you avoid crowded places? | Yes | 85 (21.1) | 64 (15.9) | 122 (30.3) | 44 (10.9) | 87 (21.6) | 0.76 |
| No | 99 (21.3) | 69 (14.8) | 158 (34.0) | 51 (11.0) | 88 (18.9) | ||
| Do you wear a mask in crowded places? | Yes | 31 (7.7) | 12 (3.0) | 56 (14.0) | 66 (16.5) | 236 (58.9) | 0.08 |
| No | 48 (10.4) | 23 (5.0) | 82 (17.7) | 75 (16.2) | 235 (50.8) | ||
| Do you avoid people with respiratory infections? | Yes | 175 (45.0) | 72 (18.5) | 70 (18.0) | 21 (5.4) | 51 (13.1) | 0.47 |
| No | 203 (45.0) | 64 (14.2) | 93 (20.6) | 28 (6.2) | 63 (14.0) | ||
| If you are near infected people, do you wear a mask? | Yes | 149 (38.4) | 43 (11.1) | 53 (13.7) | 31 (8.0) | 112 (28.9) | 0.87 |
| No | 169 (38.9) | 53 (12.2) | 50 (11.5) | 32 (7.4) | 131 (30.1) | ||
| Do you take the seasonal flu vaccine? | Yes | 48 (12.1) | 27 (6.8) | 34 (8.6) | 37 (9.3) | 250 (63.1) | 0.49 |
| No | 66 (15.1) | 20 (4.6) | 40 (9.1) | 38 (8.7) | 274 (62.6) | ||
Discussion
The behavior of the public is vital in the prevention of respiratory infections.[16] The present study illustrates perceptions on the prevention of infections and safety practices with regard to respiratory infections in a sample of the urban population of Riyadh.
The research findings reveal a high awareness of susceptibility to seasonal flu (88%), but less susceptibility to coronavirus (20.2%), N1H1 (3.6%), and bird flu (5.4%) transmission. This finding might be reasonable since seasonal influenza is well known in the community while the other flu types seem to be newly emerging communicable diseases. The authorities recently initiated a public awareness campaign on the emerging flus as against the seasonal influenza which has existed for over a decade.
In our study, 75.1% of participants had heard about flu earlier, but this was lower than what had been reported in other studies. This finding may be due to a lack of awareness and interest in health issues in our study population. Similar to studies done in China, there were more female participants in the present study. This finding may be because women are usually keener about health issues than men.[17,18,19,20,21,22]
The majority of our participants were aware of the personal hygiene of hand washing following routine procedures and before eating; a measure that is very effective in preventing the transmission of respiratory diseases. However, only a third used antibacterial soap, which is less than found in previous studies. This provides an opportunity for the adoption of the religious teaching of handwashing after using the lavatory and before eating.[23]
Prophet Mohammed (peace be upon Him) always urged Muslims to wash their hands before and after meals; the lavatory; touching a cadaver, or one's shoes; and handling anything soiled or suspect in any way.[24]
In this study, 63.5% of the population always covered their noses and mouths when sneezing and coughing, two of the main modes of transmission of respiratory diseases. This finding is almost double what was reported in a previous study.[25]
In our study, only 40% of the population used masks as a preventive measure in crowded places, and only 20% used masks in daily lives, which is much less than what was reported in a previous study.[25] In our study, 32.1% of the participants avoided crowded places; this is comparatively lower than the findings of the other study.[26] This may be the result of the lack of awareness of the preventive measures to be taken against the transmission of pandemic respiratory diseases. In this survey, only 13.7% had received the seasonal flu vaccine. A large proportion (62.8%) of the participants did not intend to take the vaccine. Their primary reasons were that they were unsure of the benefits, and afraid of the adverse effects. This poor attitude emphasized the importance of conveying appropriate messages to the public to make them understand better the benefits of the vaccine and improve its uptake. Moreover, poor attitude has an impact on infection transmission. Therefore, attitudes should be improved to prevent the spread of an outbreak. This finding underpins the importance of awareness campaigns for frequenters of malls, sports stadium and Jummah prayers.[25,26]
In the present study, the majority knew about respiratory diseases. Similar to other studies, almost half of the participants agreed that TV and radio are the most common sources of information. The remaining participants obtained their information through WhatsApp, from the Ministry of Health, doctors, and through campaigns. Thus, the findings suggest the urgent need for educational programs that can explicitly improve knowledge and behavioral practices in this group.[27,28]
Conclusions
An intensive program should be planned periodically, executed, and monitored to improve awareness, attitude, and practice of the population for the prevention of respiratory virus infection.
The health authority should seize every opportunity to prevent the transmission of respiratory infections by promoting such religious and cultural practices as the washing of hands and the covering of mouths and noses when sneezing and coughing.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank all the participants. We will also like to thank Bayan Alshahrani and Maram Bin-Dayel for their assistance with data collection and data entry. The study was approved by the College of Medicine Research Center, and the Chair of Health Education and Health Promotion; the Deanship of Scientific Research chairs, King Saud University, Riyadh, Saudi Arabia.
References
- 1.World Health Organization. Infection Prevention and Control of Epidemic-and Pandemic-Prone Acute Respiratory Infections in Health Care 2014. [Last accessed on 2019 Apr 04]. Available from: https://apps.who.int/iris/bitstream/handle/10665/112656/9789241507134_eng.pdf . [PubMed]
- 2.Albogami SS, Alotaibi MR, Alsahli SA, Masuadi E, Alshaalan M. Seasonal variations of respiratory viruses detected from children with respiratory tract infections in Riyadh, Saudi Arabia. J Infect Public Health. 2018;11:183–6. doi: 10.1016/j.jiph.2017.06.001. [DOI] [PubMed] [Google Scholar]
- 3.Schraufnagel D. The respiratory health risks of large crowds. Ann Am Thorac Soc. 2016;13:766. doi: 10.1513/AnnalsATS.201603-177ED. [DOI] [PubMed] [Google Scholar]
- 4.Al-Tawfiq JA, Gautret P, Benkouiten S, Memish ZA. Mass gatherings and the spread of respiratory infections: Lessons drawn from the Hajj. Ann Am Thorac Soc. 2016;13:759–65. doi: 10.1513/AnnalsATS.201511-772FR. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Communicable Disease Alert and Response for Mass Gatherings: key Considerations. World Health Organization; 2008. [Last accessed on 2019 Apr 04]. Available from: http://www.who.int/csr/Mass_gatherings2.pdf . [Google Scholar]
- 6.The Lancet Infectious Diseases. Need for global cooperation in control of MERS-coV. Lancet Infect Dis. 2013;13:639. doi: 10.1016/S1473-3099(13)70205-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qualls N, Levitt A, Kanade N, Wright-Jegede N, Dopson S, Biggerstaff M, et al. Community mitigation guidelines to prevent pandemic influenza-United States, 2017. MMWR Recomm Rep. 2017;66:1–34. doi: 10.15585/mmwr.rr6601a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jiménez-Corona ME, Aguilar-Díaz Fdel C, León-Solís LE, Morales-Virgen JJ, de León-Rosales SP. Knowledge, attitudes and practices about influenza A (H1N1) 2009, and influenza vaccine in Mexico: Results of a population survey. Salud Publica Mex. 2012;54:607–15. doi: 10.1590/s0036-36342012000600009. [DOI] [PubMed] [Google Scholar]
- 9.Agüero Santagelo F, Nebot Adell M, Pérez Giménez AA, López Medina MJ, García Continente X. Attitudes and preventive behaviours adopted during the (H1N1) 2009 influenza virus epidemic in Spain. Rev Esp Salud Publica. 2011;85:73–80. doi: 10.1590/S1135-57272011000100009. [DOI] [PubMed] [Google Scholar]
- 10.Freiman AJ, Montgomery JP, Green JJ, Thomas DL, Kleiner AM, Boulton ML. Did H1N1 influenza prevention messages reach the vulnerable population along the Mississippi gulf coast? J Public Health Manag Pract. 2011;17:52–8. doi: 10.1097/PHH.0b013e3181fb8002. [DOI] [PubMed] [Google Scholar]
- 11.Sim SW, Moey KS, Tan NC. The use of facemasks to prevent respiratory infection: A literature review in the context of the health belief model. Singapore Med J. 2014;55:160–7. doi: 10.11622/smedj.2014037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shi J, Njai R, Wells E, Collins J, Wilkins M, Dooyema C, et al. Knowledge, attitudes, and practices of nonpharmaceutical interventions following school dismissals during the 2009 influenza A H1N1 pandemic in Michigan, United States. PLoS One. 2014;9:e94290. doi: 10.1371/journal.pone.0094290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarmiento MP, Suárez O, Sanabria JA, Pérez CE, Cadena Ldel P, Niño ME. Knowledge and practices about the prevention and the control of the influenza A H1N1 in the community of Floridablanca, Santander. Biomedica. 2011;31:91–9. doi: 10.1590/S0120-41572011000100011. [DOI] [PubMed] [Google Scholar]
- 14.Zairina AR, Nooriah MS, Yunus AM. Knowledge and practices towards influenza A (H1N1) among adults in three residential areas in Tampin Negeri Sembilan: A cross sectional survey. Med J Malaysia. 2011;66:207–13. [PubMed] [Google Scholar]
- 15.Balkhy HH, Abolfotouh MA, Al-Hathlool RH, Al-Jumah MA. Awareness, attitudes, and practices related to the swine influenza pandemic among the Saudi public. BMC Infect Dis. 2010;10:42. doi: 10.1186/1471-2334-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dawes MG, Kaczorowski J, Swanson G, Hickey J, Karwalajtys T. The effect of a patient education booklet and BP 'tracker' on knowledge about hypertension. A randomized controlled trial. Fam Pract. 2010;27:472–8. doi: 10.1093/fampra/cmq048. [DOI] [PubMed] [Google Scholar]
- 17.Singh S, Kaur P, Singh G. Study to assess the awareness, perception and myths regarding swine flu among educated common public in Patiala district. Int J Res Dev Health. 2013;12:54–60. [Google Scholar]
- 18.Rathi S, Gandhi H, Francis M. Knowledge and awareness about H1N1 flu in urban adult population of Vadodara, India. Electron Phys. 2011;3:392–5. [Google Scholar]
- 19.Chaudhary V, Singh RK, Agrawal VK, Agarwal A, Kumar R, Sharma M. Awareness, perception and myths towards swine flu in school children of Bareilly, Uttar Pradesh. Indian J Public Health. 2010;54:161–4. doi: 10.4103/0019-557X.75741. [DOI] [PubMed] [Google Scholar]
- 20.Farahat T, Al-Kot M, Al-Fath A, Noh A, Diab N. Promotion of knowledge, attitude and practice towards swine flu A/H1N1: An intervention study on secondary school children of Menofia Governorate, Egypt. Menofia Med J. 2010;23:83–94. [Google Scholar]
- 21.Latiff LA, Parhizkar S, Zainuddin H, Chun GM, Rahiman MA, Ramli NL, et al. Pandemic influenza A (H1N1) and its prevention: A cross sectional study on patients' knowledge, attitude and practice among patients attending primary health care clinic in Kuala Lumpur, Malaysia. Glob J Health Sci. 2012;4:95–102. doi: 10.5539/gjhs.v4n2p95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin Y, Huang L, Nie S, Liu Z, Yu H, Yan W, et al. Knowledge, attitudes and practices (KAP) related to the pandemic (H1N1) 2009 among Chinese general population: A telephone survey. BMC Infect Dis. 2011;11:128. doi: 10.1186/1471-2334-11-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rubin GJ, Potts HW, Michie S. The impact of communications about swine flu (influenza A H1N1v) on public responses to the outbreak: Results from 36 national telephone surveys in the UK. Health Technol Assess. 2010;14:183–266. doi: 10.3310/hta14340-03. [DOI] [PubMed] [Google Scholar]
- 24.Mishra S, Sarkar D, Srivastava S, Deepthi S, Chetan N, Mishra S. Hand hygiene–religious, cultural and behavioral aspects. Univ J Educ Gen Stud. 2013;2:184–8. [Google Scholar]
- 25.Shilpa K, Kumar BP, Kumar SY, Ugargol AR, Naik VA, Mallapur M. A study on awareness regarding swine flu (influenza A H1N1) pandemic in an urban community of Karnataka. Med J Dr DY Patil Univ. 2014;7:732. [Google Scholar]
- 26.Kamate SK, Agrawal A, Chaudhary H, Singh K, Mishra P, Asawa K. Public knowledge, attitude and behavioural changes in an Indian population during the influenza A (H1N1) outbreak. J Infect Dev Ctries. 2009;4:7–14. doi: 10.3855/jidc.501. [DOI] [PubMed] [Google Scholar]
- 27.Sedighi I, Nouri S, Sadrosadat T, Nemati R, Shahbazi M. Can children enhance their family's health knowledge. An infectious disease prevention program? Iran J Pediatr. 2012;22:493–8. [PMC free article] [PubMed] [Google Scholar]
- 28.Evans D, Clark NM, Levison MJ, Levin B, Mellins RB. Can children teach their parents about asthma? Health Educ Behav. 2001;28:500–11. doi: 10.1177/109019810102800409. [DOI] [PubMed] [Google Scholar]


