Abstract
Large population-based surveys by the Government of India and several other regional studies have reconfirmed the coexisting burden of over- and undernutrition. While time trends from the 2nd, 3rd and 4th rounds of the National Family Health Survey show declining trends in the prevalence of the underweight, it also highlights increasing rates in the overweight/obesity. Dose-response relationships with different micro- and macronutrient consumption with overweight/obesity prevalence have been established. In this context, it was attempted to identify the specific diet pattern and socio-behavioural determinants of overnutrition along with its combat strategies. This review highlights that while the proportion of chronic energy deficiency is decreasing in India, the intake of micronutrients and food groups continues to be below the recommended dietary allowance set by the Indian Council of Medical Research. Distal factors that determine the nutritional imbalance among Indians are presented under (i) household contextual factors, (ii) peer and socio-cultural influencers, and (iii) business and neighbourhood environment. Accumulation of such factors increases the density of obesogenic environment around individuals. Further, the review offers action points at individual, society and policy levels, presented in a 'logframe matrix' for bringing convergence actions across sectors in consultation with programme managers from different ministries/departments.
Keywords: Childhood obesity, convergence, dietary pattern, dual burden, non-communicable diseases, nutritional imbalance, whole of society
Introduction
Overnutrition is a form of malnutrition (imbalanced nutrition) arising from excessive intake of nutrients, leading to accumulation of body fat that impairs health (i.e., overweight/obesity)1. The crisis of overnutrition has increasingly been reported from countries where hunger is still endemic, referred to as coexisting double burden of nutritional imbalance2. Studies confirmed that the double burden of nutrition does not affect disproportionately on any population sub-group; however, the relative risk varies with economic development, food security, urbanization and living conditions. Among those living in countries undergoing economic transitioning, children are at higher risk of undernutrition while higher rates of overweight/obesity are observed among adults3.
Since 1972, the National Nutrition Monitoring Bureau (NNMB) in India has been monitoring nutrition transition at households and individual levels in 10 States4. So far, baseline (1975-1979) and four rounds of repeated cross-sectional surveys (1988-1990, 1996-1997, 2011-2012 and 2016-2017) have been conducted. Coexisting nutritional problems (both under- and overnutrition) along with associated cardiometabolic risk conditions such as diabetes and hypertension have already been confirmed from these studies5,6. Among children, concurrent with severe maternal malnutrition, the problem of undernutrition starts in much earlier ages in India. This was confirmed in the National Family Health Survey (NFHS, 4th round, 2015-2016)7, reporting stunting, wasting and underweight prevalence as 38, 21 and 36 per cent, respectively, among children below five years. Concomitantly, overweight and obesity rates among children also increased to 19.3 per cent (cumulative), highlighting coexisting nutritional imbalance8. Among adults, around 20 and 23 per cent of men and women were classified as thin while 19 and 21 per cent of men and women as overweight/obese, respectively (NFHS, 4th round)7. The prevalence rate ranged between 4.3 and 40.9 per cent in different States. The 4th round of the NNMB (2016-2017) survey also highlighted that one-third of men and half of women in urban areas suffered ill effects of overweight/obesity9. In rural areas, around 33 and 36 per cent of men and women were reported as undernourished while 10 and 13 per cent of men and women as overweight/obese, respectively10. In short, the 2nd, 3rd and 4th rounds of the NFHS showed decreasing proportion of men and women in normal weight categories (body mass index ≥18 to ≤25 kg/m2)11. In about two decades, a two- to three-fold increase in the cumulative prevalence of overweight/obesity was reported from the national population surveys in India12.
Overnutrition has several implications on cardiometabolic conditions, leading to chronic non-communicable diseases. India stood second in the list of countries affected with type 2 diabetes (from 5.9% in 2000 to 10.4% in 2017) - presently around 72 million people are affected (as per Diabetes Atlas)12. In addition, around 3.3 per cent of people (around 24 million) are pre-diabetic13. ICMR-INDIAB study conducted in four regions of India highlighted that the ratio of newly diagnosed cases to known diabetes cases were more than 1:114. Concomitantly, hypertension also increased to 29.2 per cent in 201415. Thus, as compared to three decades ago, people of all age groups across all geographic regions in India are at higher risk of such cardiometabolic conditions conditions16. Without addressing the issues associated with overnutrition in India, it will be difficult to prevent the rising burden of chronic disease epidemics, especially because overnutrition is the prime reason for fat accumulation in human body. Although reduction in the intake of sugar, salty and fatty foods is recommended widely, there is no clarity on how to achieve this.
Objectives
This narrative review was conceptualized to describe: (i) specific dietary pattern among overnourished individuals in India; (ii) socio-behavioural and environmental determinants of nutrition imbalance; and (iii) combating strategies to contain this epidemic at population level. This was achieved in two steps:
Step 1 - Literature search was done to identify determinants of nutrition imbalance in India with special emphasis on national-level population-based surveys. Search was conducted in PubMed and Google Scholar. Search strategy used MESH terms and key words (dual burden, nutritional balance, overweight, obesity, underweight, malnutrition along with determinants, drivers, proximal factors or enablers) and free-text articles between 2000 and 2018. Retrieved articles were scrutinized to reduce the heterogeneity in methodology. Determinants of overnutrition in India were then listed and narrated in three sub-heads.
Step 2 - Content analysis of policies and programmes was done based on the key determinants identified in step 1 and a desk review was conducted in policy documents, office memorandums, white papers, short communications and websites of the government departments. Schemes, policies and programmes across sectors were identified that could be tweaked to reduce the density of obesogenic environment at a societal level. Around 60 programmes/schemes attached to over 15 national-level policies, across ministries, were listed. Further, a framework was prepared, as per the step 1, for inclusion in the content analysis. Policies and programmes that may influence individual's food and physical activity behaviour were appraised. Identified options were discussed with 17 stakeholders (programme managers) across sectors to identify feasible action points. All responses were recorded verbatim and analyzed using qualitative methods. Themes emerged were grouped into action points at individuals, societies and policies and programme levels. Finally, the themes were organized in a 'log frame' matrix for adaptation.
Diet pattern specific to overnourished individuals in India (Proximal factors)
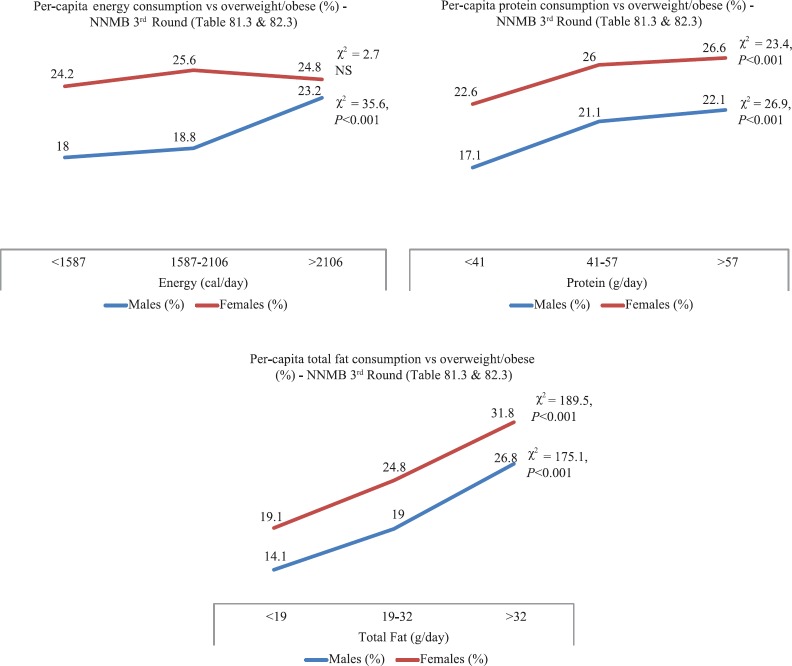
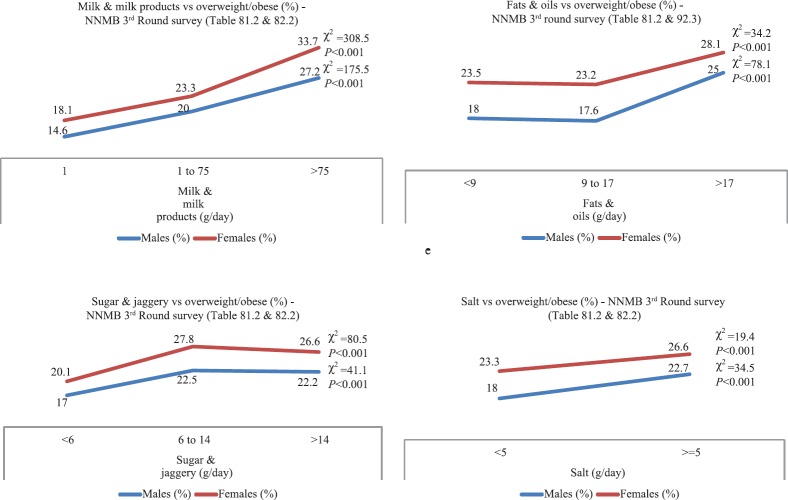
Data on macro- and micronutrient intake among overnourished individuals in urban settings in India were available from the 4th round of the NNMB survey (2016-17)9. For rural setting, the 3rd round of the NNMB survey has reported a significant dose–response relationship among overweight/obese men and women consuming total fat >32 g/day and protein >57 g/day (Fig. 1)17. Energy consumption >2106 cal/day was significantly higher among overweight/obese men; however, this was not significant among women17. Per-capita consumption of milk/milk products, fat/oils and sugar/jaggery and also salty foods was higher among overweight/obese men and women (Fig. 2). The amount of white sugar, trans fat and salt consumed by overweight/obese persons per day was not available. At population level, around 13.2 teaspoons of white sugar were consumed per person/day in India (~55.3 g/day), which was 22 g/day in 2000 - this was confirmed in the 66th round of the National Sample Survey Office (NSSO) report18. In addition, a considerable amount of sugar is consumed per person/day in invisible form, partly attributed to relatively lower price of sugar in Indian markets19. Around 54 g/day of total fat was consumed per person/day, which was 21.2 g/day in 200018. The mean salt intake was estimated around 10.9 g/day (95% CI: 8.57 to 13.40)20. Men consumed higher salt (9.6 to 13.3 g/day) as compared to women (6.6 to 11.3 g/day). Salt intake was not different in rural areas (9.6 to 12.7 g/day) as compared to urban areas (9.7 to 11.9 g/day). However, salt in invisible forms (savory snacks, condiments, etc) were not estimated20. Around 333 g/day of refined grains are consumed by Indians21.
Fig. 1.
Consumption of macronutrients and overnutrition; a dose-response relationship17.
Fig. 2.
Consumption of food groups and overnutrition in the 3rd Round of the National Nutrition Monitoring Bureau survey; a dose-response relationship17.
Four rounds of the NNMB survey reiterate that while chronic energy deficiency is decreasing, the intake of micronutrients and certain food groups continue to be below the recommended dietary allowance (RDA) set by the Indian Council of Medical Research (ICMR). While the median intake of protein, iron and thiamine has declined over time, the intake of calcium and vitamin C has improved. Over time, the consumption of cereals and millets is gradually decreasing at households while the consumption of vegetables and fruits is increasing slightly17. Fast foods, deep fried foods and processed foods are increasingly consumed at Indian households22,23. Concomitantly, per-capita consumption of coarse grains and pulses has decreased: in 2011-2012, per-capita consumption of pulses was around 26 g/day in rural areas and 29.6 g/day in urban areas, which was significantly lesser than the RDA of 40 g/day24. The 64th round of the NSSO on household consumer expenditure survey also confirmed such trends. Such population trends in food choices and declining physical activity levels necessitated ICMR to lower the RDA in 201725.
Determinants of nutritional imbalance in India (Distal factors)
Distal factors of nutritional imbalance begin with duration of breastfeeding of infants26,27, availability of calorie dense foods at home28, food and nutrition security, preference to and increased consumption of sweet and fatty/fried foods and salty snacks29,30, skipping meals, less physical activity (sedentary lifestyle) and overall stressful environment at home and neighbourhood. All such factors could be grouped under (i) household contextual factors, (ii) peer and socio-cultural influences, and (iii) business and neighbourhood environment.
Household contextual factors
With changes in family structure (nuclear families), time-constrained parents and children, access to disposable money and increased access and affordable ready-to-eat/cook foods and overall demand for convenience/comforts have catalyzed food preferences at household level. Thus, staple foods consumed by Indians now have a higher glycaemic index as compared to what they were consuming three decades ago. Animal-based foods shared in the diet increased exponentially31. The demand of high-value food items such as milk, egg and meat products and fruits/vegetables has increased in both urban and rural areas. The use of refined grains (polished rice and wheat) has replaced the whole grains32. Refined grains have only endosperms (starch) that elevate plasma glucose (glycaemic index), insulin, triglycerides and fatty acids33. Glycaemic load of refined grains exceeds far above the RDA. Refining process leads to the removal of outer bran and germ portions, resulting in the loss of many nutrients. The quantity of foods consumed (portion size) by Indians has also increased34. Processed, packaged and deep-fried foods are increasingly consumed at every household across social strata.
Peer influence & socio-cultural environment
Food habits of individuals are closely related to their social structure, urbanization, psychosocial stress35, increasing affluence (economic wellbeing)36, social capital and aggressive marketing37. Peers in the society/schools influence individual habits at large, specifically food and physical activity habits. For children, there is a societal pressure for academic performance and parental concerns (primarily safety concerns) that seriously affect their physical activities38. Overweight/obesity was found to be higher in children studying in English medium schools and in those children with father and/or mother working or involved in business39. Dose-response relationship between skipping breakfast (never, sometimes and daily) and overweight/obesity was observed40. Complexity increases with less physical activity due to motorized transportation41, increasing mechanization of day-to-day activities and less time in outdoor activities (<30 min). Decreased duration of sleep (<8.5 h/day) and increased television viewing (>3 h/day) were also found to be associated with obesity42.
Business & neighbourhood environment
The density of obesogenic environment is increasing at Indian neighbourhoods. Entrepreneurs and market research companies quickly identify and respond to changing household needs and devise products/services that meet convenience/comforts of families at affordable costs43. Affordability and consumption pattern, especially among Indian middle-class households, are non-homogenous. Purchasing power of middle-class families has been shifted to women, which has doubled in the past decade. Around 26 per cent of workforce in rural areas and 13.8 per cent in urban areas were women44. Media and advertisement agencies bridge consumers and producers through targeted approaches to facilitate large social changes. Television, mobile phones, internet and radio are used as the source of sharing information. Targeted marketing strategies, brand promotion through children and celebrity endorsements promote family-level changes. Studies have linked food advertisements with overnutrition at population level45. Reduction in healthy foods was observed with increased television viewing46,47. Peer influence and other driving forces of consumer behaviours will promote large social changes that increase the density of obesogenic environment in neighbourhood. Such a situation could be better understood by looking at market growth trends of selected products that are associated with overnutrition. Now, caloric beverages are easily available at neighbourhoods and have become a significant source of energy consumption at households. Around 13 per cent annual growth rates have been consistently reported since 2009 for canned sugar-sweetened beverages in India48. Condiments, bakery products, ready-to-eat/cook foods, frozen foods and other processed foods have also increased at Indian neighbourhoods. Availability and consumption of snacks, ice creams, chocolates, biscuits, probiotics and processed meats have increased. Studies have highlighted that the variety of food products and the packet sizes in neighbourhood promote overeating49,50. The number of food-processing industries has also increased and contributes significantly to the national GDP (Gross Domestic Product)51. Further, by 2020 India's food packaging industry is forecasted to become the 3rd largest in the world52. Artificial sweeteners/invisible sugar is heavily used in food-processing industries53. All such examples could be viewed as ecological indicators for increasing obesogenic environment in rapidly transitioning Indian societies, which needs to be graded and quantified.
What needs to be done?
The individuals in Indian societies are under the influence of an obesogenic environment while relative risk varies with the density of such environment around the individuals. As the density increases, more and more individuals get susceptible to the adverse effect of overnutrition and cardiometabolic diseases. There is no consensus on which interventions are likely to be effective to reduce the density of obesogenic environment, especially in a rising economy like India. It is important to reduce this public health catastrophe without influencing the human development and economic reforms in India. As most components of obesogenic environment are driven by non-health sectors, it is important to engage different actors of society across sectors (from public and private) to devise strategies without hampering the economic interests of the nation. Therefore, convergence of health with non-health sectors including urban planning, education, agriculture, trade and market, food and nutrition, sports and recreation, and finances is recommended.
Defining and classifying societies (ranking) based on the density of obesogenic environment and population density correlated with the risk of cardiometabolic conditions are the logical first step to be accomplished. Further, concerted efforts must be implemented at policies and programmes, household and societal level, and individual habits, and choices that will contribute to the reduction of density of obesogenic environments are recommended. For this purpose, a 'whole-of-government-whole-of-society' engagement is recommended where the unit of intervention is not individual, but instead the aggregate society (at local self-governance level, district, State or nation). Through a desk review (by research teams at INCLEN Trust International, New Delhi) various opportunities existing within policies and programmes under nine different ministries (and 40 public programmes) were identified and presented to 17 stakeholders from different sectors. Most stakeholders interviewed were programme managers or department heads under different ministries. From stakeholders, responses, key action points were inductively derived that could potentially contribute in the reduction of obesogenic environment in India (Tables I–III). These were grouped under actions at:
Table I.
Policies and programme level actions suggested by stakeholders to contain childhood obesity in India
| Action point | Implementation plan |
|---|---|
| Working group for convergence | A working group is recommended for convergence between sectors and vertical programmes. Trained counsellors are available in NCD clinics, school health programmes and adolescent health clinics which can be integrated. This could become a stronger forum for behaviour change. Services of the National Mental Health Programme can also be integrated. |
| Integrated digital platform/programme databases across sectors | In India, infrastructure already exists under different programmes to identify and track vulnerable individuals. What is required is to bring convergence within vertical systems through integrating programme databases. This forms a digital platform developed and maintained at local panchayat/district/State or national level. It shall facilitate monitoring of individuals from birth till death. A life-course approach as recommended by World Health Organization54. |
| Integrated NCDs and nutrition activities under one roof | A few activities of nutrition promotion fall under the purview of Ministry of Women and Child Development while NCD monitoring programmes are under the purview of the Ministry of Health and Family Welfare. It was suggested that all nutrition and NCD prevention/management activities/programmes should be integrated under one-roof for better implementation and programme uptake. |
| Family-level risk factor monitoring | Under the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular diseases and Stroke (NPCDCS) programme, it is recommended to reduce the screening age from 30+ to all people above 18 yr. Further, this should be based on the risk factors for NCDs at household levels. NPCDCS activities can be extended to children and adolescents. |
| Nutrient profile model55 to classify and restrict high-fat, salt and sugar content in food packets | Recommends (i) Limit the contents of artificial sweeteners and sodium, etc. (ii) Revising labelling regulations - nutrient labelling to be mandated that include total sugar, added sugar, sodium, etc. (iii) Labels should be with appropriate size for better visibility and consider front-of-pack labelling (iv) Implement marketing restriction for HFSS foods to children (v) FSSAI to set up expert group for setting limits for salt, sugar and fat in food products in India |
| Pricing and subsidy schemes | Scientific guidelines on what to be subsidized and what should be incentivized based on the nutrient profile models (i) The government subsidizes palm oil due to which it is cheaper in market. This is why it is most commonly used oil in food industry. (ii) There should be guidelines for reuse of oils, sugar and sodium on packed foods. (iii) Heavy taxation for SSBs. (iv) Incentives to farmers on total grown crops/hectare or acre, organic farming and entertain use of certified seeds for farming. |
| Assessing physical fitness levels | Measuring physical fitness levels in all age groups is recommended through Ministry of Youth Affairs and Sports, Government of India. |
SSBs, sugar-sweetened beverages; NCDs, non-communicable diseases; FSSAI, Food Safety and Standards Authority of India; HFSS, high-fat, sugar and salt
Table III.
Individual level actions suggested by stakeholders to contain childhood obesity in India
| Action point | Implementation plan |
|---|---|
| Promote self-monitoring through nutrition education | Each individual should be empowered to monitor his/her anthropometry (BMI, height and weight) and calculate energy and nutrition intakes. They should be able to monitor their physical activity levels (i) NCD-related health education modules are prepared by NIHFW and this could be used for training and communications (ii) Education department should consider this to be formally included in the curriculum for training teachers (iii) Electronic formats of this module can be prepared |
| Training on parenting principles | Women at home intend to give value added foods to family and children. Therefore, it is important to educate women about optimum nutrition. Feeding practices of mother shall improve eating practices of entire home. Women should be specifically empowered for (i) Improving family culture and restrict eating-out habits (ii) Cooking practices in family |
| Low birth weight babies and underweight pregnant ladies to be monitored | Overfeeding and catch up growths among low birth weights can increase the risk for overweight/obesity in future. Under RBSK programme, low-birth-weight children are identified; however, it is important to follow them over time and monitor. This could be included under infant and young child feeding programme of the Government of India. |
NCD, non-communicable disease; BMI, body mass index; NIHFW, National Institute of Health and Family Welfare; RBSK, Rashtriya Bal Swasthya Karyakram
-
(i)
Policies and programme level;
-
(ii)
Household and societal level; and
-
(iii)
Individual habits and choices.
Table II.
Household or societal level actions suggested by stakeholders to contain childhood obesity in India
| Action point | Implementation plan |
|---|---|
| Functional referral health systems | Referral systems exist within National Health Mission - There are over 7500 adolescent health clinics, RKSK clinics and RBSK clinics. Trained counsellors and health ambassadors for behavioural change already exist within these clinics. In addition, services of community workers (ASHA, ANM, AWW and VHNSCs) can be used to link vulnerable individuals and referral mechanism through anthropometric monitoring. These health workers can play a significant role in advocacy. |
| Shaping the eating and physical activity habits at schools | Every child should have an individual growth chart. This is possible through mandatory growth monitoring (BMI-for-age) charts at school/college admissions (transfer certificates). This could be integrated with annual health check-up and assess physical fitness in schools. (i) Two teachers per school to be trained as health ambassadors. NCERT teachers training curriculum should include optimal nutrition and growth monitoring concepts. (ii) Children in private schools also to be focused and mandated for annual physical fitness. (iii) PTA in schools (public and private) to improve diet and physical activity environment in (school canteens) and around schools. |
| Promotion of physical activity | Urban town planning departments and green tribunals shall mandate construction of park, walk-ways, safe play areas, grounds, cycling tracks, etc., in urban localities (i) Physical activity guidelines for workplaces to be issued based on regional contexts. (ii) Integrate physical activity with cultural beliefs - advocacy with religious leaders to include five minutes of exercise after prayers. |
| Social exclusion of HFSS foods | Strong advocacy campaigns to make HFSS foods socially unacceptable. Market will respond to healthy food demands. |
| VHNSC’s to track vulnerable individuals | Nutritional imbalance, substance abuse (smoking and alcohol) is common among migrants, labourers and out-of-school children. VHNSCs through ASHAs and ANMs can locally identify vulnerable individuals and integrate them with existing referral mechanism. (i) Family health cards were recommended under NHM. At present, BMI is not included in such cards. These could be made digital and integrated with national schemes. (ii) Promote VHND once in a month. |
| Grading of obesogenic environment at societies | Develop and implement scientific methods to grade and classify neighbourhoods based on the density of obesogenic environment. This shall be done according to population density and proportion of at-risk individuals in the locality which is correlated with access to HFSS foods. |
| Community Food and Nutrition Units (MoWCD) |
(i) There are 43 CFNEUs in 29 States which could be used to monitor micronutrient availability at village levels. (ii) Support of NCPCR, NCW, NIPCCD, CSWB and RMK can be used. |
RKSK, Rashtriya Kishor Swasthya Karyakram; RBSK, Rashtriya Bal Swasthya Karyakram; BMI, body mass index; PTA, Parent Teachers Association; VHND, Village Health and Nutrition Day; CFNEUs, Community Food and Nutrition Extension Units; NCPCR, National Commission for Protection of Child Rights; NCW, National Commission for Women; NIPCCD, National Institute of Public Cooperation and Child Development; CSWB, Central Social Welfare Board; RMK, Rashtriya Mahila Kosh; AWW, Anganwadi Worker; ANM, auxiliary nurse midwife; VHNSCs, Village Health Nutrition and Sanitation Committee; NCERT, National Council of Education Research and Training; HFSS, high-fat, sugar and salt; NHM; National Health Mission; MoWCD, Ministry of Women and Child Development
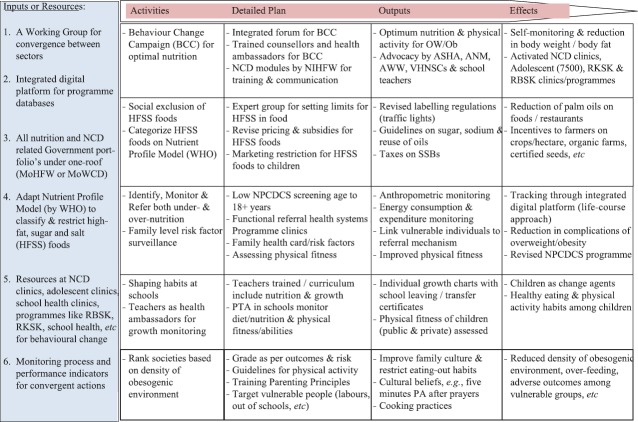
Emerging model on ‘path to convergence’
Through desk review policies and programmes spanning across nine ministries (health and non-health sectors), and potential opportunities for policy level improvisation have been identified56. Feasibility of such interventions was discussed with over 17 stakeholders having hands-on experience in implementing such national programmes in the field. Common themes emerged from the discussions were grouped to design a convergence model in the Indian context. Efforts were to identify potential strategies to bring different actors of existing vertical programmes across sectors without much additional resources. Such themes are presented in a 'logframe' matrix(Fig. 3) with activities, implementation plan, outputs and expected effects. This matrix can be used to design a public health programme at local self-government level, district and State or national level. The model requires adaptation to regional contexts and can add more specific inputs.
Fig. 3.
‘Path to Convergence’ for grading and preventing obesogenic environment in India - a log frame approach based on common themes emerged from the discussion with different stakeholders (working groups, programmes and ministries). ASHA, Accredited Social Health Activist; AWW, Anganwadi Worker; ANM, auxiliary nurse midwife; SSBs, sugar-sweetened beverages; NCDs, non-communicable diseases; OW/Ob, overweight/obese; NPCDCS, National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular diseases and Stroke; NCW, National Commission for Women; RMK, Rashtriya Mahila Kosh; PA, physical activity; PTA, Parent Teachers Association; RKSK, Rashtriya Kishor Swasthya Karyakram; RBSK, Rashtriya Bal Swasthya Karyakram; VHNSCs, Village Health Nutrition and Sanitation Committee; MoWCD, Ministry of Women and Child Development.
Conclusion
The present review on determinants of double burden of nutrition reiterates that several recent changes in food environment and food culture have detrimental health effects. The NNMB surveys highlighted that overweight/obesity was specifically increased in men and women consuming energy above 1587 cal/day, protein above 41 to 57 g/day and fat above 19 to 32 g/day. Per-capita per day consumption of milk/milk products, fats and oils (including meat and meat products), sugars and jaggery (including condiments, biscuits etc.) and salts/sodium (savory snacks) showed a significant dose-response relationship with overweight/obesity prevalence. This review highlights that several determinants of obesogenic environment in India have linkages with non-health sectors. It is essential to devise mechanisms to grade obesogenic environment that correlates with the prevalence of overweight/obesity in corresponding locations. Finally, a model has been derived inductively based on the available documents and literature to bring convergence across sectors that are presented in a log frame matrix. Various components of a prospective programme to reduce overweight/obesity are listed in this matrix.
Acknowledgment
Authors acknowledge the contributions of all investigators and research staffs involved in the Indian Council of Medical Research Task Force project on childhood obesity in India.
Footnotes
Financial support & sponsorship: Stakeholder interviews were supported by WHO South East Asia Regional Office, New Delhi through 'scoping study for addressing obesity among children and adolescents in India'.
Conflicts of Interest: None.
References
- 1.The Partnership for Maternal, New Born and Child Health. Knowledge Summary: Women's & Children's Health, Nutrition. 2012. [accessed on August 10, 2018]. Available from: http://www.who.int/pmnch/topics/part_publications/KS18-high.pdf .
- 2.Chopra M, Galbraith S, Darnton-Hill I. A global response to a global problem: The epidemic of overnutrition. Bull World Health Organ. 2002;80:952–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Min J, Zhao Y, Slivka L, Wang Y. Double burden of diseases worldwide: Coexistence of undernutrition and overnutrition-related non-communicable chronic diseases. Obes Rev. 2018;19:49–61. doi: 10.1111/obr.12605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Nutrition Monitoring Bureau. Hyderabad: National Institute of Nutrition; [accessed on August 10, 2018]. Available from: http://www.nnmbindia.org/aboutus.html . [Google Scholar]
- 5.Kulkarni VS, Kulkarni VS, Gaiha R. “Double burden of malnutrition”: Reexamining the coexistence of undernutrition and overweight among women in India. Int J Health Serv. 2017;47:108–33. doi: 10.1177/0020731416664666. [DOI] [PubMed] [Google Scholar]
- 6.Paul K, Singh J. Emerging trends and patterns of self-reported morbidity in India: Evidence from three rounds of national sample survey. J Health Popul Nutr. 2017;36:32. doi: 10.1186/s41043-017-0109-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.International Institute of Population Science. National Family Health Survey, Round-4, (NFHS-4) 2015-16. [accessed on August 7, 2018]. Available from: http://www.rchiips.org/NFHS/NFHS-4Reports/India.pdf .
- 8.Ranjani H, Mehreen TS, Pradeepa R, Anjana RM, Garg R, Anand K, et al. Epidemiology of childhood overweight & obesity in India: A systematic review. Indian J Med Res. 2016;143:160–74. doi: 10.4103/0971-5916.180203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Nutrition Monitoring Bureau. Technical Report No. 27, Diet & nutritional status of urban population in India and prevalence of obesity, hypertension, diabetes and hyperlipidemia in urban men and women. A brief NNMB report on urban nutrition. Hyderabad: National Institution of Nutrition; 2017. [accessed on September 29, 2018]. Available from: http://www.ninindia.org/NNMB%20Urban%20Nutrition%20Report%20-Brief%20report.pdf . [Google Scholar]
- 10.Meshram II, Balakrishna N, Sreeramakrishna K, Rao KM, Kumar RH, Arlappa N, et al. Trends in nutritional status and nutrient intakes and correlates of overweight/obesity among rural adult women (≥18-60 years) in India: National Nutrition Monitoring Bureau (NNMB) National Surveys. Public Health Nutr. 2016;19:767–76. doi: 10.1017/S1368980015002268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.International Institute of Population Science. National Family Health Survey, Round-3, (NFHS-3) 2015-16 – fact sheets. [accessed on August 2, 2019]. Available from: http://rchiips.org/NFHS/pdf/India.pdf .
- 12.Swain S, Chowdhury S. Trends of nutritional status among rural adults in six states of India: Findings from national survey data. Clin Epidemiol Global Health. 2018;6:181–7. [Google Scholar]
- 13.International Diabetes Federation. Diabetes atlas. Prevalence of diabetes, South East Asia. International Diabetes Federation. [accessed on November 13, 2018]. Available from: http://reports.instantatlas.com/report/view/846e76122b5f476fa6ef09471965aedd/IND .
- 14.Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: Phase I results of the Indian Council of Medical Research-India DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022–7. doi: 10.1007/s00125-011-2291-5. [DOI] [PubMed] [Google Scholar]
- 15.Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantonio E, et al. Hypertension in India: A systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32:1170–7. doi: 10.1097/HJH.0000000000000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leal C, Chaix B. The influence of geographic life environments on cardiometabolic risk factors: A systematic review, a methodological assessment and a research agenda. Obes Rev. 2011;12:217–30. doi: 10.1111/j.1467-789X.2010.00726.x. [DOI] [PubMed] [Google Scholar]
- 17.National Nutrition Monitoring Bureau. NNMB Technical Report No. 26. Diet and nutritional status of rural population. Prevalence of hypertension & diabetes among adults and infant & young child feeding practices: Report of third repeat survey. Hyderabad National Institute of Nutrition 2012. [accessed on August 7, 2018]. Available from: http://www.nnmbindia.org/1_NNMB_Third_Repeat_Rural_Survey___Technicl_Report_26.pdf .
- 18.National Sample Survey Office. Report No. 540, NSS 66th round. Nutritional Intake in India; 2009-10. [accessed on August 7, 2018]. Available from: http://www.indiaenvironmentportal.org.in/files/file/nutrition%20intake%20in%20india.pdf .
- 19.Balasaheb D. Indian sugar trade: A fresh look. Indira Gandhi Institute of Development Research; 2013. [accessed on September 28, 2018]. Available from: http://www.igidr.ac.in/pdf/publication/WP-2013-024.pdf . [Google Scholar]
- 20.Johnson C, Praveen D, Pope A, Raj TS, Pillai RN, Land MA, et al. Mean population salt consumption in India: A systematic review. J Hypertens. 2017;35:3–9. doi: 10.1097/HJH.0000000000001141. [DOI] [PubMed] [Google Scholar]
- 21.Radhika G, Van Dam RM, Sudha V, Ganesan A, Mohan V. Refined grain consumption and the metabolic syndrome in Urban Asian Indians (Chennai Urban Rural Epidemiology Study 57) Metabolism. 2009;58:675–81. doi: 10.1016/j.metabol.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 22.Keshari P, Mishra CP. Growing menace of fast food consumption in India: time to act. International Journal of Community Medicine And Public Health. 2017;5(3):1355–62. [Google Scholar]
- 23.Neal B, Sacks G, Swinburn B, Vandevijvere S, Dunford E, Snowdon W, et al. Monitoring the levels of important nutrients in the food supply. Obes Rev. 2013;14(Suppl 1):49–58. doi: 10.1111/obr.12075. [DOI] [PubMed] [Google Scholar]
- 24.Roy D, Joshi PK, Chandra R, editors. Pulses for nutrition in India: Changing patterns from farm to fork. Intl Food Policy Res Inst. 2017. Dec 26, DOI: https://doi.org/10.2499/9780896292567.
- 25.National Institute of Nutrition. Dietary guidelines for Indians; a manual. New Delhi: National Institute of Nutrition; 2017. [accessed on November 16, 2018]. Available from: http://www.ninindia.org/DietaryGuidelinesforNINwebsite.pdf . [Google Scholar]
- 26.Malhotra R, Noheria A, Amir O, Ackerson LK, Subramanian SV. Determinants of termination of breastfeeding within the first 2 years of life in India: evidence from the National Family Health Survey 2. Matern Child Nutri. 2008;4:181–93. doi: 10.1111/j.1740-8709.2007.00130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ahmad QI, Ahmad CB, Ahmad SM. Childhood obesity. Indian J Endocrinol Metab. 2010;14:19–25. [PMC free article] [PubMed] [Google Scholar]
- 28.Raj M, Kumar RK. Obesity in children & adolescents. Indian J Med Res. 2010;132:598–607. [PMC free article] [PubMed] [Google Scholar]
- 29.Kuriyan R, Bhat S, Thomas T, Vaz M, Kurpad AV. Television viewing and sleep are associated with overweight among urban and semi-urban South Indian children. Nutr J. 2007;6:25. doi: 10.1186/1475-2891-6-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sharma A, Hegde AM. Relationship between body mass index, caries experience and dietary preferences in children. J Clin Pediatr Dent. 2009;34:49–52. doi: 10.17796/jcpd.34.1.17364206hqm0477h. [DOI] [PubMed] [Google Scholar]
- 31.National Council of Applied and Economic Research. Agricultural outlook and situation analysis report. An analysis of changing food consumption pattern in India. National Council of Applied and Economic Research. 2015. [accessed on August 24, 2018]. Available from: http://www.nfsm.gov.in .
- 32.Mohan V, Radhika G, Vijayalakshmi P, Sudha V. Can the diabetes/cardiovascular disease epidemic in India be explained, at least in part, by excess refined grain (rice) intake? Indian J Med Res. 2010;131:369–72. [PubMed] [Google Scholar]
- 33.Rizkalla SW, Bellisle F, Slama G. Health benefits of low glycaemic index foods, such as pulses, in diabetic patients and healthy individuals. Br J Nutr. 2002;88(Suppl 3):S255–62. doi: 10.1079/BJN2002715. [DOI] [PubMed] [Google Scholar]
- 34.Mohan V, Radhika G, Sathya RM, Tamil SR, Ganesan A, Sudha V, et al. Dietary carbohydrates, glycaemic load, food groups and newly detected type 2 diabetes among urban Asian Indian population in Chennai, India (Chennai Urban Rural Epidemiology Study 59) Br J Nutr. 2009;102:1498–506. doi: 10.1017/S0007114509990468. [DOI] [PubMed] [Google Scholar]
- 35.Dasgupta P. In a weighty crisis. Health Environ Newsl. 2004;3:3. [Google Scholar]
- 36.Mahal A, Karan A, Engelgau M. The economic implications of non-communicable disease for India. HNP Discussion Paper. 2010. [accessed on September 16, 2018]. Available from: http://siteresources.worldbank.org/HEALTHNUTRITIONANDPOPULATION/Resources/281627-1095698140167/EconomicImplicationsofNCDforIndia.pdf .
- 37.James WP. The challenge of childhood obesity (Editorial) Int J Pediatr Obes. 2006;1:7–10. doi: 10.1080/17477160600630404. [DOI] [PubMed] [Google Scholar]
- 38.The drivers of body weight, shape and health: An Indian perspective of domestic and international influences. In: Das MK, Arora NK, editors; Dube L, Berchara A, Dagher A, Drewnowski A, LeBel J, James P, et al., editors. Obesity prevention: The role of brain and society on individual behavior. New York: Elsevier Inc; 2010. [Google Scholar]
- 39.Bharati DR, Deshmukh PR, Garg BS. Correlates of overweight & obesity among school going children of Wardha city, central India. Indian J Med Res. 2008;127:539–43. [PubMed] [Google Scholar]
- 40.Arora M, Nazar GP, Gupta VK, Perry CL, Reddy KS, Stigler MH, et al. Association of breakfast intake with obesity, dietary and physical activity behavior among urban school-aged adolescents in Delhi, India: Results of a cross-sectional study. BMC Public Health. 2012;12:881. doi: 10.1186/1471-2458-12-881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Singh SK. Review of urban transportation in India. J Public Transport. 2005;8:75–97. [Google Scholar]
- 42.Laxmaiah A, Nagalla B, Vijayaraghavan K, Nair M. Factors affecting prevalence of overweight among 12- to 17-year-old urban adolescents in Hyderabad, India. Obesity (Silver Spring) 2007;15:1384–90. doi: 10.1038/oby.2007.165. [DOI] [PubMed] [Google Scholar]
- 43.Pingali P, Khwaja Y. Inaugural key note address, 17th Annual Conference. Indian Society of Agricultural Marketing Hyderabad, February 5-7. Agricultural and Development Economics Division, The Food and Agriculture Organization; 2004. Globalisation of Indian diets and the transformation of food supply systems. [Google Scholar]
- 44.Olsen W, Mehta S. Female labour participation in rural and urban India: Does housewives' work count? Radic Stat. 2006;93:57–90. [Google Scholar]
- 45.Lobstein T, Dibb S. Evidence of a possible link between obesogenic food advertising and child overweight. Obes Rev. 2005;6:203–8. doi: 10.1111/j.1467-789X.2005.00191.x. [DOI] [PubMed] [Google Scholar]
- 46.Gable S, Chang Y, Krull JL. Television watching and frequency of family meals are predictive of overweight onset and persistence in a national sample of school-aged children. J Am Diet Assoc. 2007;107:53–61. doi: 10.1016/j.jada.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 47.Halford JC, Boyland EJ, Hughes G, Oliveira LP, Dovey TM. Beyond-brand effect of television (TV) food advertisements/commercials on caloric intake and food choice of 5-7-year-old children. Appetite. 2007;49:263–7. doi: 10.1016/j.appet.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 48.Bhaskar H. Indian beverage industry's double digit growth will continue, says IBA. Indian Beverage Association; [accessed on August 3, 2018]. Available from: http://www.fnbnews.com/article/detnews.asp?articleid=33532§ionid=1 . [Google Scholar]
- 49.Chandon P, Wansink B. Is food marketing making us fat? A multi-disciplinary review, Foundations and Trends® in Marketing. 2010;5(3):113–96. [Google Scholar]
- 50.Khare A, Inman JJ. Habitual behavior in American eating patterns: The role of meal occasions. J Consumer Res. 2006;32:567–75. [Google Scholar]
- 51.Rais M, Acharya S, Sharma N. Food processing industry in India: S & T capability, skills and employment opportunity. J Food Process Technol. 2013;4:260. [Google Scholar]
- 52.Bureau Report. India to be world's 3rd-biggest packaged food market: ASSOCHAM. [accessed on August 2, 2019]. Available from: http://www.fnbnews.com/Interview/india-to-be-worlds-3rdbiggest-packaged-foodmarket-43250 .
- 53.Chattopadhyay S, Raychaudhuri U, Chakraborty R. Artificial sweeteners–a review. JFST. 2014;51:611–21. doi: 10.1007/s13197-011-0571-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jacob C, Baird J, Barker M, Cooper C, Hanson M. The importance of a life course approach to health: chronic disease risk from preconception through adolescence and adulthood. Southampton: University of Southampton; 2015. [Google Scholar]
- 55.Scarborough P, Rayner M, Stockley L. Developing nutrient profile models: a systematic approach. Public Health Nutrition. 2007;10:330–6. doi: 10.1017/S1368980007223870. [DOI] [PubMed] [Google Scholar]
- 56.Kar SS, Kar SS. Prevention of childhood obesity in India: Way forward. J Nat Sc Biol Med. 2015;6:12. doi: 10.4103/0976-9668.149071. [DOI] [PMC free article] [PubMed] [Google Scholar]