Abstract
Introduction:
A previous Minnesota SimSmoke tobacco control policy model is extended to more recent years and to include smokeless tobacco (SLT) use.
Methods:
Using data from the 1993 Tobacco Use Supplement and information on state policies, the Minnesota SimSmoke model was updated and extended to incorporate SLT (both exclusive and dual use) and SLT-attributable deaths. The model was then validated against the 2002, 2006/2007, and 2014/2015 Tobacco Use Supplement and the 1999, 2007, 2014, and 2018 Minnesota Adult Tobacco Survey, and used to estimate the impact of policies implemented between 1993 and 2018. Analysis was conducted in April 2019.
Results:
The model validated well for cigarette and earlier SLT use, but predicted SLT use less well in recent years. The model projected that male (female) smoking prevalence was 35% (36%) lower in relative terms by 2018 and 43% (44%) lower by 2040 owing to policies, with lesser reductions projected for male SLT use. Tobacco-attributable deaths were reduced by 7,800 by 2018 and 46,900 by 2040. Price increases, primarily through taxes, were projected to have had the greatest impact on cigarette use followed by smoke-free air laws, cessation treatment policies, tobacco control campaign expenditures, and youth access enforcement. Similar effects were projected for SLT use, except that smoke-free air laws had smaller effects.
Conclusions:
As cigarettes remain the dominant form of nicotine delivery product, cigarette-oriented policies may be an effective means of reducing the use of all nicotine delivery products. However, non–cigarette oriented policies may also play an important role.
INTRODUCTION
Since the 1964 Surgeon General’s Report, U.S. smoking prevalence has declined by more than 50%. Much of that decline has been attributed to tobacco control policies,1–3 including smoke-free air laws, media campaigns, and tax increases. Whereas early policies were implemented at the federal level, recent policies have mostly been implemented by states.3 Simulation models have been used to show the effect of state-level policies.4–11 As one of the more active tobacco control states, a previous SimSmoke7 policy simulation model for Minnesota attributed a 25% reduction in smoking prevalence to policies implemented between 1993 and 2011.
Although cigarette use has fallen rapidly in Minnesota, smokeless tobacco (SLT) use has increased. After a period of relatively constant prevalence from 2000 through 2007, SLT use increased from 3.1% in 2007 to 4.3% in 2010, with SLT use by smokers increasing from 4.4% in 2007 to 9.6% in 2010.12 Since 2010, Minnesota passed policies that updated tobacco product definitions,13 implemented a large SLT tax increase,14 and expanded SLT treatment coverage. A better understanding of how policies impact SLT use is needed to develop effective strategies to minimize cigarette and SLT use harms.
In this paper, Minnesota SimSmoke is extended and further validated to 2018, and, based on a U.S. model,15 expanded to consider SLT use. The effect of policies implemented between 1993 and 2018 on cigarette and SLT use and deaths attributable to their use is estimated. Methods and Results are summarized below and discussed in greater detail in the Appendix.
METHODS
The model begins with the 1993 population distinguished by never tobacco users and current and former exclusive cigarette, exclusive SLT, and dual users. Changes over time in tobacco use occur from changes in the population, previous use patterns, and new policies.
Study Population
Population by single age and gender were obtained from the Census Bureau’s Population Estimates Program for 1993–201516–18 and the Minnesota State Demographic Center for 2016–2067.19 The population evolves using birth, mortality, and immigration rates.20
Measures
Individuals evolve from never tobacco users to current tobacco users through smoking and SLT initiation, become former users through quit rates, and may return to their prior tobacco use state through relapse. These transitions follow a discrete time, first-order Markov process.
Baseline estimates of exclusive smoking, exclusive SLT, and dual use status by age and gender were obtained from the state-representative 1992/1993 Tobacco Use Supplement of the Current Population Survey (CPS-TUS).21 Current smokers included those who smoked ≥100 cigarettes and currently smoke either daily or nondaily. A question on “regular” SLT use was used to distinguish dual and exclusive SLT users. Former users were defined as those who met the respective definitions for use, but reported no current use, and were distinguished by years quit. Former exclusive smokers and dual users were split from all former smokers using age-specific percentages of exclusive smokers and dual users. As former SLT use was not available, former exclusive SLT prevalence was estimated using the ratio of former to current smokers, assuming the same initial profile by years quit as smokers. Female exclusive and dual SLT use was <0.2% for all years, and thus not considered.
Because evidence on initiation and early transitions to SLT use is mixed22–26 and the CPS-TUS does not provide sufficient information to distinguish information on early initiation, cessation, and product switching, transitions at young ages are modeled using net initiation rates. Measured as the difference between the 1993 prevalence at the current age and previous age for each category of tobacco user, this method incorporates initiation, cessation, and switching between tobacco products, and helps ensure model stability and internal consistency. Net initiation occurs through age 30 years for males and age 27 years for females, the respective ages when net initiation for all three user groups began to decline.
To simplify the model, all product initiation and switching is assumed to occur until the final age of net initiation, and only cessation occurs after that age. Smoker quit rates were obtained from the 1993 CPS-TUS, measured as those who quit in the last year, but not the last 3 months.27 Data to distinguish exclusive SLT and dual users quit rates were not available, but previous literature28–30 indicates quit rates at least as high among SLT as cigarette users, and similar quit rates for dual users and exclusive smokers.30–32 Consequently, smoker quit rates and relapse rates33–36 were applied to dual and exclusive SLT users. Because studies indicate limited switching between SLT use and smoking except at younger ages,28–30 switching only occurs at young ages via net initiation.
Relative mortality risk estimates by age and gender for current and former smokers from the Cancer Prevention Study II35,37,38 were assigned to exclusive cigarette and dual users with risks declining for former smokers by years quit.35,37,38 Current exclusive SLT RR of 1.15 was based on a large-scale U.S. study.39 Tobacco user mortality rates were differentiated using prevalence rates and RRs, with excess risks measured as the difference between tobacco user and never tobacco user mortality rates. Tobacco-attributable deaths were estimated as the number of users in each of the current and former use categories multiplied by their excess mortality risks.
Policy descriptions and best estimates and credible ranges of effect sizes are shown in Table 1. Policies have immediate effects on prevalence rates and ongoing effects on initiation and cessation rates. When more than one policy is implemented, their effects are applied multiplicatively. Beginning with 1993, the model incorporates policy changes occurring between 1993 and 2018. Policy levels are based on consultation with Clearway Minnesota staff.
Table 1.
Policy Inputs for Cigarette and Smokeless Tobacco Use in Minnesota SimSmoke
| Policy | Description | Cigarette effect sizea | Relative smoke-less tobacco effect sizeb | Sensitivity ranges cigarettes (smoke-less)c |
|---|---|---|---|---|
| Tax policy40–44 | −25%, 25% (50%, 50%) | |||
| Cigarette prices | The effect of taxes is directly incorporated through average price (including generics), with separate prices for cigarettes and SLT. The price elasticity is used to convert the % price changes into effect sizes. The dual price is computed as 3/4 of the cigarette price plus 1/4 SLT price | Elasticitiesd −0.4 ages 10‒17 years −0.3 ages 18‒24 years −0.2 ages 25‒34 years −0.1 ages 35‒64 years −0.2 ages ≥65 years |
same same same −0.2 same |
|
| Smoke-free air policies41,44,49 | −50%, +50% (−75%, +75%) | |||
| Worksite smoking ban, well-enforced | Ban in all indoor worksites, with strong public acceptance and enforcement of laws (reduced by 1/3 if allowed in ventilated areas and by 2/3 if allowed in common areas) | −6%e | 25% lower | |
| Restaurant smoking ban | Ban in all indoor restaurants (reduced by half if partial) | −2%e | 25% lower | |
| Bars smoking ban | Ban in all indoor bars (reduced by half if partial) | −1%e | 25% lower | |
| Other places bans | Ban in 3 out of 4 government buildings, retail stores, public transportation, and elevators | −1%e | 25% lower | |
| Enforcement | Government agency enforces the laws | Effects reduced 50% absent enforcement | 25% lower | |
| Tobacco control expenditures41,44,51 | −50%, +50% (−75%, +75%) | |||
| High level tobacco control campaign | Campaign heavily publicized, with per capita expenditures of at least $2.00 | −6.5% | 50% lower | |
| Mid-level tobacco control campaign | Campaign publicized, with per capita expenditures of at least $0.50 | −3.25% | 50% lower | |
| Low-level tobacco control campaign | Campaign sporadically publicized with per capita expenditures of at least $0.05 | −1.63% | 50% lower | |
| Health warnings41,44 | −50%, +50% (−75%, +75%) | |||
| Strong | Labels are large, bold and graphic, and cover at least 30% of pack | −4% prevalence, −6% initiation, +10% cessation | Same | |
| Moderate | Laws cover 1/3 of package, not bold or graphic | −2% prevalence and initiation, +4% cessation | Same | |
| Weak | Laws cover less than 1/3 of package, not bold or graphic | −1% prevalence and initiation, +2% cessation | Same | |
| Cessation treatment policy41,44,54 | −50%, +50% (−75%, +75%) | |||
| Availability of pharmacotherapies | Legality of nicotine replacement therapy, Bupropion and Varenicline | −1% prevalence, +4% cessationf | 50% lower | |
| Proactive quitline | A proactive quitline with publicity and no cost NRT | −1% prevalence, +6% cessationf | 50% lower | |
| Treatment coverage | Payments to cover pharmacotherapy and behavioral therapy | −2.25% prevalence, +8% cessationf | 50% lower | |
| Brief healthcare provider interventions | Advice by a healthcare provider to quit and methods provided | −1% prevalence, +4% cessationf | 50% lower | |
| All of the above | Complete availability and reimbursement of pharmaco- and behavioral treatments, quitlines, and brief interventions | −5.7% prevalence, +27.4% cessationf | 50% lower | |
| Youth access restrictions58–61 | −50%, +50% (−75%, +75%) |
|||
| Strongly enforced and publicized | Compliance rates of <5%, penalties are potent, enforced with heavy publicity | −16% initiation and prevalence for ages 16‒17 years and −24% for ages <16 years | 50% lower | |
| Well enforced | Compliance rates of <20% (and >5%), penalties are potent, and publicity and merchant training are included | −8% initiation and prevalence for ages 16‒17 years and −12% for ages <16 years | 50% lower | |
| Low enforcement | Compliance rates >20%, penalties are weak | −2% initiation and prevalence for ages 16‒17 years and −3% for ages <16 years | 50% lower | |
| Vending machine restrictions | Total ban | Enforcement effects increase by 8% | 50% lower | |
| Self-service restrictions | Total ban | Enforcement effects increase by 4% | 50% lower | |
| Publicity | Media campaigns directed at youth use | Enforcement effects increase by 10% | 50% lower |
Unless otherwise indicated, the effects are in terms of the reduction in prevalence during the first year, the reduction in initiation, and increase in first year quit rates during the years that the policy is in effect.
Effect sizes are relative to cigarette effect sizes and applied to exclusive smokeless tobacco use only unless otherwise indicated.
Same sensitivity ranges used for smokeless tobacco effect sizes, unless otherwise indicated.
Elasticities translate into effect sizes through percentage change in price.
Effect size differs for exclusive smokeless tobacco and dual use.
Effect size for dual use is assumed 1/4 that of exclusive cigarette.
SLT, smokeless tobacco; NRT, nicotine replacement therapy.
In the tax module,40 tax effects are modeled through price assuming constant proportional effects. Demand studies,41 including two recent studies,42,43 indicate that effects of price on SLT use are similar to those found for cigarette demand.44 Exclusive cigarette use depends upon Minnesota’s average cigarette retail prices (including generics).45 Because SLT prices were unavailable, they were estimated using data on manufacturer prices, state and federal taxes, and wholesale and retail markups.46 Weighted prices (75% cigarette, 25% SLT) were applied to dual users.47 Prices were adjusted for inflation using the Consumer Price Index.48 Minnesota taxes increased substantially in 2005, 2009, and 2013 for cigarettes and in 2005 and 2013 for SLT.
The existence and enforcement as well as publicity surrounding worksite, restaurant, bar, and other public place smoke-free air laws are incorporated in SimSmoke.49 Exclusive SLT and dual use effect sizes were set at 25% that of cigarette use.41 Minnesota implemented a state comprehensive smoke-free air law in 2007 after earlier local ordinances.50 Enforcement was set at 80% during 1993–2007 and 90% for 2008–2018.
SimSmoke distinguishes high, medium, and low levels of per-capita tobacco control expenditures,51 much of which are for media campaigns.52 Based on SLT-oriented media campaign evaluations,41 the exclusive SLT effect size was set at 50% that of smokers. Based on per-capita expenditures,53 Minnesota tobacco control expenditures were designated as low in 1993–1995, moderate in 1996–1999, and high since 2000.
Health warnings on packages are assumed to have similar effects on cigarette and SLT.41 They had been minimal since 1993, but text warnings covering ≥30% of two principal sides have been required on SLT packages since 2010 (moderate).
Cessation treatment policy includes pharmacotherapy availability, financial coverage of treatments, quitlines, and brief interventions.54 Reviews of randomized SLT trials find mixed effects for pharmacotherapies, but slightly stronger effects for behavioral interventions,41 but use has been low.55 Compared with exclusive smokers, cessation treatment policies were assigned 50% the effect on SLT users and 75% the effect on dual users. The patch was available by prescription in 1993 and became available without prescription in 1997. Bupropion became available in 1998 and Varenicline became available in 2007, both by prescription. Pharmacotherapy and behavioral therapy coverage were effectively available to 40% of smokers in 1993, increasing to 60% in 2003, 70% in 2007, 85% in 2011, and 90% in 2016. Minnesota was categorized as having an active, well-publicized quitline since 2001. The 2014 Minnesota Adult Tobacco Survey (MATS)56 indicates that about 67% of smokers visited a healthcare provider, of which about 79% received advice and 53% received a referral.57 Brief interventions were estimated at 40% coverage of smokers in 1993, increasing to 50% in 2004.
The effect of minimum purchase age laws depends on enforcement levels, and on vending machines and self-service restrictions.58 Based on findings that youth access policies weakly affects SLT use,43,59–61 these policies were assigned 50% the effect for exclusive SLT compared with cigarette use. Based on Synar data,76 compliance rates were used to classify enforcement as low through 2000, moderate until 2010, and high since 2011. Bans were implemented on vending machines in 1996 and on self-service in 2009.
Modeling
The model was calibrated by comparing predicted prevalence rates by gender and age to 1996 and 1998 CPS-TUS prevalence rates. Based on the deviations, male initiation rates were increased for ages 18–30 years, and cessation rates were reduced for ages ≥35 years. Because female exclusive smoker prevalence rates for ages 18–27 years were higher than CPS-TUS rates, their initiation rates were reduced by 20%. SLT and dual use were not calibrated owing to the limited reliability of CPS-TUS estimates.
The model was validated by comparing model predictions of prevalence rates to those of 2002, 2006/2007, and 2014/2015 CPS-TUS surveys and 1999, 2007, 2014, and 2018 MATS.57,62 For the CPS-TUS, questions on SLT use changed in 1998 from asking about regular use to at least one time in the last month. Current SLT use was then defined to include those using ≥10 of the last 30 days in CPS-TUS.63 Two definitions were used from MATS, both based on any last 30-day use with one requiring ≥20 times in lifetime.
To estimate the effect of policies implemented between 1993 and 2018 on all (exclusive and dual) cigarette and SLT use, the model was programmed with all policies remaining at their 1993 levels (the counterfactual). The net reduction due to all policies was estimated by the relative difference between the counterfactual projection and that with all policies implemented. The contribution of an individual policy is estimated by programming the model to allow for the change in that policy while holding other policies constant. Because policy effects are not additive, the effect of an individual policy is measured relative to the summed effects of all individual policies.
RESULTS
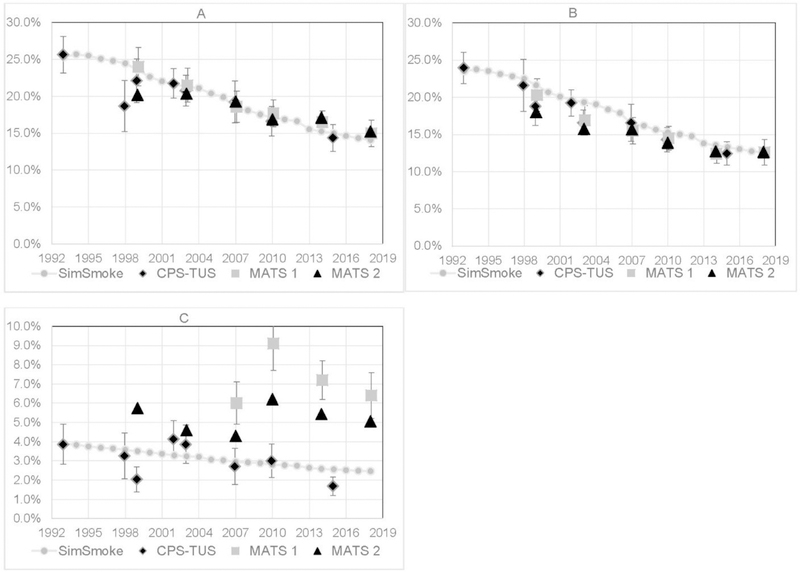
As shown in Figures 1A and 1B, SimSmoke predicted that male (female) age ≥18 years cigarette (exclusive plus dual) prevalence fell from 25.3% (23.5%) in 1993 to 15.0% (13.3%) in 2015, while the CPS-TUS was 14.4% (12.4%) in 2015. By 2018, smoking prevalence was projected to fall to 14.1% (12.5%) compared with 15.0% in MATS. For both 2015 and 2018 and earlier years, SimSmoke predicted well within the 95% CIs of estimates from the respective surveys, except for overestimating male smoking in 1998 and female smoking in 1999 and 2003. Analysis by age group (not shown) also generally yielded predictions within CPS-TUS and MATS CIs for each gender.
Figure 1.
Prevalence validation of all current smokers and all smokeless tobacco users, SimSmoke vs MATS and CPS-TUS with 95% CIs, 1993‒2018. (A) all male current smokers; (B) all female current smokers; (C) all male smokeless tobacco users.
CPS-TUS, Current Population Survey-Tobacco Use Supplement; MATS, Minnesota Adult Tobacco Survey.
As shown in Figure 1C, SimSmoke projected adult male SLT (exclusive and dual use) prevalence falling from 3.9% in 1993 to 2.6% in 2015, above the 1.7% estimate and CI from 2015 CPS-TUS. SimSmoke projected male SLT use at 2.5% in 2018, and in that year as well as in 2007, 2010, and 2014, SimSmoke projections were below the CIs from MATS estimates. The deviations from MATS since 2007 were especially large for young adults.
The effects of policies implemented between 1993 and 2018 are shown separately for male and female prevalence in Table 2 and total male and female tobacco-attributable deaths in Table 3.
Table 2.
Prevalence by Tobacco Use, Projected by Minnesota SimSmoke Under Multiple Scenarios, 1993‒2040
| Scenario/Use | 1993 % | 2018 Best (Lower, Upper),a % | 2040 Best (Lower, Upper),a % | Relative change 2018,b % | Relative change 2040,b % | Percent of total 2040c |
|---|---|---|---|---|---|---|
| Males | ||||||
| Counter-factual | ||||||
| Smokers | 25.3 | 21.6 (21.6, 21.6) | 19.1 (19.1, 19.1) | |||
| SLT use | 3.9 | 3.2 (3.2, 3.2) | 2.9 (2.9, 2.9) | |||
| All policies | ||||||
| Smokers | 25.3 | 14.1 (16.6, 11.8) | 10.9 (13.5, 8.6) | −35 (−23, −45) | −43 (−29, −55) | 100 |
| SLT use | 3.9 | 2.5 (2.8, 2.2) | 2.1 (2.4, 1.8) | −23 (−12, −32) | −27 (−15, −38) | 100 |
| Price alone | ||||||
| Smokers | 25.3 | 17.4 (18.4, 16.5) | 14.3 (15.4, 13.3) | −19 (−15, −24) | −25 (−20, −30) | 52 |
| SLT use | 3.9 | 2.8 (2.9, 2.6) | 2.5 (2.6, 2.3) | −14 (−9, −18) | −14 (−10, −19) | 54 |
| Smoke-free air laws alone | ||||||
| Smokers | 25.3 | 20.0 (20.8, 19.2) | 17.5 (18.3, 16.8) | −8 (−4, −11) | −8 (−4, −12) | 17 |
| SLT use | 3.9 | 3.2 (3.2, 3.1) | 2.8 (2.9, 2.8) | −1 (0, −1) | ‒1 (0, −1) | 3 |
| Tobacco control expenditures Alone | ||||||
| Smokers | 25.3 | 21.0 (21.3, 20.7) | 18.5 (18.8, 18.2) | −3 (−1, −4) | −3 (−2, −5) | 6 |
| SLT use | 3.9 | 3.1 (3.2, 3.1) | 2.8 (2.8, 2.8) | −2 (−1, −3) | −2 (−1, −3) | 8 |
| Cessation treatment alone | ||||||
| Smokers | 25.3 | 20.7 (21.1, 20.2) | 18.2 (18.7, 17.8) | −5 (−2, −7) | −5 (−3, −7) | 10 |
| SLT use | 3.9 | 3.1 (3.1, 3.0) | 2.8 (2.8, 2.7) | −3 (‒1, −5) | −3 (−1, −5) | 13 |
| Health warnings aloned | ||||||
| Smokers | 25.3 | 21.6 (21.6, 21.6) | 19.1 (19.1, 19.1) | ‒ | ‒ | ‒ |
| SLT use | 3.9 | 3.2 (3.2, 3.1) | 2.8 (2.9, 2.8) | −1 (0, −1) | −1 (0, −1) | 4 |
| Youth access alone | ||||||
| Smokers | 25.3 | 21.1 (21.4, 20.7) | 17.8 (18.6, 17.0) | −3 (−1, −5) | −7 (−3, −11) | 14 |
| SLT use | 3.9 | 3.1 (3.2, 3.1) | 2.7 (2.8, 2.6) | −2 (−1, −4) | −5 (−2, −9) | 18 |
| Females | ||||||
| Counter-factual | ||||||
| Smokers | 23.5 | 19.5 (19.5, 19.5) | 17.3 (17.3, 17.3) | |||
| SLT use | ‒ | ‒ | ‒ | |||
| All policies | ||||||
| Smokers | 23.5 | 12.6 (14.9, 10.5) | 9.7 (12.2, 7.6) | −36 (−23, −46) | −44 (−30, −56) | 100 |
| SLT use | ‒ | ‒ | ‒ | ‒ | ‒ | ‒ |
| Price alone | ||||||
| Smokers | 23.5 | 15.8 (16.7, 15.0) | 13.1 (14.0, 12.2) | −19 (−15, −23) | −24 (−19, −29) | 49 |
| SLT use | ‒ | ‒ | ‒ | ‒ | ‒ | ‒ |
| Smoke-free air laws alone | ||||||
| Smokers | 23.5 | 17.9 (18.7, 17.1) | 15.7 (16.5, 15.0) | −8 (−4, −12) | −9 (−5, −14) | 18 |
| SLT use | ‒ | ‒ | ‒ | ‒ | ‒ | ‒ |
| Tobacco control expenditures alone | ||||||
| Smokers | 23.5 | 18.9 (19.2, 18.6) | 16.7 (17.0, 16.4) | −3 (−2, −5) | −3 (−2, −5) | 7 |
| SLT use | ‒ | ‒ | ‒ | ‒ | ‒ | ‒ |
| Cessation treatment alone | ||||||
| Smokers | 23.5 | 18.5 (19.0, 18.0) | 16.2 (16.8, 15.8) | −5 (−3, −8) | −6 (−3, −9) | 12 |
| SLT use | ‒ | ‒ | ‒ | ‒ | ‒ | ‒ |
| Health warnings alone | ||||||
| Smokers | 23.5 | 19.5 (19.5, 19.5) | 17.3 (17.3, 17.3) | ‒ | ‒ | ‒ |
| SLT use | ‒ | ‒ | ‒ | ‒ | ‒ | ‒ |
| Youth access alone | ||||||
| Smokers | 23.5 | 19.0 (19.3, 18.6) | 16.2 (16.8, 15.4) | −3 (−1, −4) | −7 (−3, −11) | 13 |
| SLT use | ‒ | ‒ | ‒ | ‒ | ‒ | ‒ |
Estimates are given in terms of the best estimate and the upper and lower bounds based on the policy evaluation literature.
Relative changes are estimated for a particular policy or group of policies relative to the Counterfactual, i.e., (Policyp,t-Counterfactualp,t)/Counterfactualp,t for policy p and time period t.
Percent of total is measured as the relative change from the policy relative to the summed relative change effects of all policies.
Health warnings were changed for smokeless tobacco, but not cigarettes.
SLT, smokeless tobacco.
Table 3.
Tobacco-Attributable Deaths and Deaths Averted, Projected by Minnesota SimSmoke Under Multiple Scenarios, 1993‒2040
| Variable | 1993 | 2018 Best estimate (Lower, Upper)a | 2040 Best estimate (Lower, Upper)a | Summation by 2018 projected best (Lower, Upper)b | Summation by 2040 projected best (Lower, Upper)b |
|---|---|---|---|---|---|
| Tobacco-attributable deaths | |||||
| Counter-factual | |||||
| Cigarette | 5,279 | 7,152 (7,152, 7,152) | 7,965 (7,965, 7,965) | 157,176 (157,176, 157,176) | 330,846 (330,846, 330,846) |
| Dual | 17 | 119 (119, 119) | 242 (242, 242) | 1,523 (1,523, 1,523) | 5,688 (5,688, 5,688) |
| SLT | 71 | 69 (69, 69) | 77 (77, 77) | 1,964 (1,964, 1,964) | 3,543 (3,543, 3,543) |
| Total | 5,367 | 7,339 (7,339, 7,339) | 8,285 (8,285, 8,285) | 160,663 (160,663, 160,663) | 340,076 (340,076, 340,076) |
| Actual/ status quo | |||||
| Cigarette | 5,279 | 6,117 (6,507, 5,764) | 5,848 (6,581, 5,239) | 149,535 (152,389, 146,894) | 285,213 (301,765, 270,841) |
| Dual | 17 | 102 (108, 96) | 178 (199, 159) | 1,421 (1,459, 1,385) | 4,662 (5,021, 4,342) |
| SLT | 71 | 62 (66, 59) | 65 (72, 59) | 1,900 (1,935, 1,866) | 3,269 (3,423, 3,130) |
| Total | 5,367 | 6,281 (6,681, 5,920) | 6,090 (6,852, 5,457) | 152,855 (155,783, 150,145) | 293,144 (310,209, 278,313) |
| Tobacco-attributable deaths avertedc | |||||
| Actual/ status quo | |||||
| Cigarette | ‒ | 1,035 (644, 1,387) | 2,118 (1,385, 2,726) | 7,641 (4,787, 10,283) | 45,633 (29,080, 60,004) |
| Dual | ‒ | 17 (11, 23) | 65 (43, 84) | 102 (64, 138) | 1,025 (667, 1,346) |
| SLT | ‒ | 6 (3, 9) | 12 (5, 18) | 64 (29, 98) | 275 (120, 413) |
| Total | ‒ | 1,058 (658, 1,419) | 2,194 (1,433, 2,828) | 7,808 (4,880, 10,519) | 46,933 (29,867, 61,764) |
| Price alone | |||||
| Cigarette | ‒ | 441 (336, 542) | 1,010 (781, 1,225) | 3,457 (2,628, 4,264) | 20,570 (15,802, 25,117) |
| Dual | ‒ | 8 (6, 10) | 34 (27, 42) | 47 (35, 58) | 517 (397, 631) |
| SLT | ‒ | 4 (2, 6) | 7 (4, 10) | 48 (25, 71) | 177 (91, 258) |
| Total | ‒ | 453 (345, 558) | 1,051 (811, 1,276) | 3,551 (2,688, 4,392) | 21,264 (16,289, 26,006) |
| Smoke-free air laws alone | |||||
| Cigarette | ‒ | 267 (135, 397) | 529 (270, 778) | 1,396 (704, 2,079) | 11,232 (5,703, 16,592) |
| Dual | ‒ | 2 (1, 3) | 7 (3, 10) | 9 (4, 13) | 109 (55, 163) |
| SLT | ‒ | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) |
| Total | ‒ | 269 (136, 400) | 536 (273, 788) | 1,405 (708, 2,092) | 11,340 (5,758, 16,754) |
| Media campaigns alone | |||||
| Cigarette | ‒ | 145 (73, 216) | 212 (107, 316) | 1,403 (705, 2,095) | 5,528 (2,783, 8,237) |
| Dual | ‒ | 3 (1, 4) | 7 (4, 11) | 22 (11, 33) | 136 (69, 203) |
| SLT | ‒ | 1 (0, 1) | 1 (0, 2) | 9 (2, 15) | 28 (7, 50) |
| Total | ‒ | 149 (75, 222) | 220 (111, 328) | 1,434 (718, 2,143) | 5,693 (2,858, 8,490) |
| Cessation treatment alone | |||||
| Cigarette | ‒ | 224 (114, 330) | 483 (250, 699) | 1,649 (835, 2,443) | 10,381 (5,324, 15,187) |
| Dual | ‒ | 4 (2, 5) | 13 (7, 19) | 21 (11, 32) | 213 (109, 312) |
| SLT | ‒ | 1 (0, 2) | 3 (1, 5) | 10 (2, 17) | 55 (14, 95) |
| Total | ‒ | 228 (116, 337) | 498 (257, 723) | 1,680 (848, 2,492) | 10,649 (5,447, 15,595) |
| Health warnings aloned | |||||
| Cigarette | ‒ | ‒ | ‒ | ‒ | ‒ |
| Dual | ‒ | ‒ | ‒ | ‒ | ‒ |
| SLT | ‒ | 0 (0, 0) | 1 (1, 2) | 2 (1, 3) | 17 (9, 26) |
| Total | ‒ | 0 (0, 0) | 1 (0, 1) | 2 (1, 3) | 17 (8, 25) |
| Youth access alone | |||||
| Cigarette | ‒ | 0 (0, 0) | 56 (25, 94) | 0 (0, 1) | 447 (201, 743) |
| Dual | ‒ | 0 (0, 0) | 5 (2, 8) | 0 (0, 0) | 40 (18, 68) |
| SLT | ‒ | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 1) |
| Total | ‒ | 0 (0, 0) | 61 (27, 102) | 0 (0, 1) | 487 (219, 811) |
Estimates are given in terms of the best estimate and the upper and lower bounds based on the policy evaluation literature.
Summation is the summed deaths or deaths averted from 1993 through the current year.
Deaths averted is measured as the difference in deaths with a policy or group of policies implemented and deaths under the counterfactual.
Health warnings were changed for smokeless tobacco, but not cigarettes.
SLT, smokeless tobacco.
Compared with no new policies implemented after 1993, SimSmoke projected that male cigarette and SLT prevalence was reduced by 35% (23%–45%) and 23% (12%–32%) respectively in 2018, and by 43% (29%–55%) and 27% (15%–38%) respectively in 2040. Similar results were obtained for female users. In 1993, total tobacco-attributable deaths were 5,367 (5,279 exclusive cigarette, 17 dual, and 71 exclusive SLT users). With policies implemented, the number of deaths increased to 6,281 deaths (6,117 exclusive cigarette, 102 dual, and 62 exclusive SLT users) with a range of 6,681 to 5,920 in 2018. With policies implemented, SimSmoke projected that 7,808 (4,880–10,519) cumulative tobacco-attributable deaths would be averted by 2018, with 46,933 (29,867–61,764) premature deaths averted by 2040.
Among individual policies, price increases alone were estimated to have reduced male smoking rates by 19% (15%–24%) in 2018, increasing to 25% (20%–30%) by 2040, and reduced premature deaths by 21,264 (16,289–26,006) by 2040. Smoke-free air laws yielded a 7.7% (3.9%–11.5%) relative reduction in male smoking rate by 2018, increasing to 8.4% (4.2%–12.4%) by 2040, with 11,340 (5,758–16,754) fewer deaths by 2040. The relative reductions were 4.6% (2.3%–6.7%) in 2018 increasing to 4.9% (3.0%–7.2%) in 2040 for cessation treatments, 2.9% (1.5%–4.3%) increasing to 3.1% (1.6%–4.7%) for tobacco control expenditures, and 2.7% (1.2%–4.5%) increasing to 6.8% (3.0%–11.4%) for youth access enforcements. For male smokers in 2040, price increases represented 52% of total policy effects, followed by smoke-free air laws (17%), youth access enforcements (14%), cessation treatments (10%), and tobacco control expenditures (6%). For male SLT use in 2040, taxes represented 54% of total policy effects, followed by youth access enforcements (18%), cessation treatments (13%), tobacco control expenditures (5%), and health warnings (4%).
DISCUSSION
Minnesota SimSmoke predicted cigarette use close to that in the CPS-TUS and MATS surveys. Like previous U.S. literature,7,8 the present analyses indicate that overall Minnesota SLT rates fell at least up through 2007, especially for those aged <45 years. Indeed, the CPS-TUS SLT prevalence fell more rapidly than model predictions through 2007, suggesting that strong cigarette policies may have had a major impact on SLT use.
The model failed to predict the increased SLT use seen in MATS since 2007. Such increases occured primarily at younger ages and are consistent with recent studies for the U.S.6,9–12 These increases among young adults may reflect marketing by cigarette manufacturers.43,64 In particular, cigarette manufacturers acquired major SLT firms and soon dominated the industry.65 They also began promoting SLT as a way for smokers to satisfy nicotine cravings in places where smoking is banned,66,67 increased price promotions,68 and marketed flavored products.18,43
The model was also used to update estimated effects of tobacco control policies implemented in Minnesota since 1993. SimSmoke projected that smoking prevalence was about 35% lower in relative terms by 2018 and 43% lower by 2040. The increased impact compared with an earlier Minnesota SimSmoke analysis7 is due primarily to the growing effect of policies over time, and to a more limited extent to the implementation of additional policies. Price increases, primarily through taxes, were still projected to have had the greatest effect on cigarette use followed by smoke-free air laws, cessation treatment policies, and tobacco control expenditures. Substantial reductions were also projected for male dual use and SLT use, although the failure of the model to predict recent increases in SLT use warrants caution. These results are similar to those from SimSmoke models for other states,4–11 and suggest the importance of tax increases subject to its limitations.69–71 However, other policies also play an important role, in and of themselves, and through synergistic effects of the different policies (e.g., taxes and cessation treatment policies).72
In 2018, Minnesota SimSmoke estimated 62 SLT and 102 dual premature deaths, which paled in comparison with 6,117 exclusive cigarette deaths. However, the model also estimated that policies implemented between 1993 and 2018 reduced tobacco-attributable deaths by 7,808 by 2018 and 46,933 by 2040.
Limitations
Like all models, the current results depend on the underlying assumptions and data. In particular, cigarette prevalence projections were based on cessation rates from the 1993 CPS-TUS for Minnesota, but are subject to policy changes over time. Information on SLT cessation and product switching were not directly available. SLT prices had to be derived. The model also does not explicitly incorporate the role of the industry, which annually spends more than $100 million in Minnesota promoting their products.73 In addition, the model did not distinguish the risks to dual users compared with exclusive smokers, and treated SLT risks as a homogeneous category. Finally, several cities, including Minneapolis, St. Paul, and Duluth, recently implemented flavor restrictions, including menthol restrictions. Though not considered, previous analysis suggests that these policies may have additional effects on cigarette use.74
The estimated effect sizes of policies for SLT use in the model largely reflect studies conducted prior to 2007.15 The effect sizes may have changed in recent years with cigarette manufacturers coming to dominate the SLT firms industry.75 In addition, the model does not specifically consider interactive effects of cigarette policies on SLT use and SLT policies on smoking. In particular, cigarettes and SLT policy effects may have changed in recent years with increased multiproduct use,76 and the increased potential for substituting other products.
The model is limited to cigarette and SLT use, and does not incorporate the use of cigars, water pipes, and e-cigarettes. Since 2010, there has been a greater focus in Minnesota on regulating other tobacco products, such as cigars and e-cigarettes, in addition to SLT. The definition of a “cigarette” for excise tax purposes was amended in 2013 to include “little cigars,”77 and appears to have reduced their use to 2%–3% in Minnesota.57 E-cigarettes may play a role in recent years either to increase or reduce cigarette smoking, and the analysis here of SLT use may provide guidance.78
CONCLUSIONS
Although the landscape for nicotine delivery products has dramatically changed in the last 10 years, some lessons can be gleaned from the present modeling. With cigarettes still being the dominant form of nicotine delivery, cigarette-oriented policies may be an effective means, perhaps the most effective means, for reducing the use of all nicotine delivery products. Nevertheless, policies directed at other products, such as SLT and e-cigarettes, may also play a role.
Supplementary Material
ACKNOWLEDGMENTS
Funding was received from Clearway Minnesota and from the National Institute on Drug Abuse under grant R01DA036497–01.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Holford TR, Meza R, Warner KE, et al. Tobacco control and the reduction in smoking-related premature deaths in the United States, 1964–2012. JAMA 2014;311(2):164–171. 10.1016/j.jvs.2014.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levy DT, Meza R, Zhang Y, Holford TR. Gauging the effect of U.S. tobacco control policies from 1965 through 2014 using SimSmoke. Am J Prev Med 2016;50(4):535–542. 10.1016/j.amepre.2015.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.HHS. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General Atlanta, GA: HHS; 2014. [Google Scholar]
- 4.Lightwood J, Glantz S. Effect of the Arizona tobacco control program on cigarette consumption and healthcare expenditures. Soc Sci Med 2011;72(2):166–172. 10.1016/j.socscimed.2010.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lightwood J, Glantz SA. The effect of the California tobacco control program on smoking prevalence, cigarette consumption, and healthcare costs: 1989–2008. PLoS One 2013;8(2):e47145. 10.1371/journal.pone.0047145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levy D, Fergus C, Rudov L, McCormick-Ricket I, Carton T. Tobacco policies in Louisiana: recommendations for future tobacco control investment from SimSmoke, a policy simulation model. Prev Sci 2016;17(2):199–207. 10.1007/s11121-015-0587-2. [DOI] [PubMed] [Google Scholar]
- 7.Levy DT, Boyle RG, Abrams DB. The role of public policies in reducing smoking: the Minnesota SimSmoke tobacco policy model. Am J Prev Med 2012;43(5 suppl 3):S179–S186. 10.1016/j.amepre.2012.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levy DT, Huang AT, Havumaki JS, Meza R. The role of public policies in reducing smoking prevalence: results from the Michigan SimSmoke tobacco policy simulation model. Cancer Causes Control 2016;27(5):615–625. 10.1007/s10552-016-0735-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Levy DT, Hyland A, Higbee C, Remer L, Compton C. The role of public policies in reducing smoking prevalence in California: results from the California Tobacco Policy Simulation Model. Health Policy 2007;82(2):153–166. 10.1016/j.healthpol.2006.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levy DT, Ross H, Powell L, Bauer JE, Lee HR. The role of public policies in reducing smoking prevalence and deaths caused by smoking in Arizona: results from the Arizona tobacco policy simulation model. J Public Health Manag Pract 2007;13(1):59–67. 10.1097/00124784-200701000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Levy DT, Tworek C, Hahn EJ, Davis RE. The Kentucky SimSmoke tobacco policy simulation model: reaching Healthy People 2010 goals through policy change. South Med J 2008;101(5):503–507. 10.1097/smj.0b013e31816c013c. [DOI] [PubMed] [Google Scholar]
- 12.Boyle RG, St Claire AW, Kinney AM, D’Silva J, Carusi C. Concurrent use of cigarettes and smokeless tobacco in Minnesota. J Environ Public Health 2012;2012:493109 10.1155/2012/493109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freiberg M, Boyle RG, Moilanen M, St Claire AW, Weisman SR. The land of 10,000 tobacco products: how Minnesota led the way in regulating tobacco products. Am J Public Health 2014;104(2):e10–e12. 10.2105/ajph.2013.301747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brock B, Choi K, Boyle RG, Moilanen M, Schillo BA. Tobacco product prices before and after a statewide tobacco tax increase. Tob Control 2016;25(2):166–173. 10.1136/tobaccocontrol-2014-052018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levy DT, Yuan Z, Li Y. The U.S. SimSmoke tobacco control policy model of smokeless tobacco and cigarette use. BMC Public Health 2018;18:696 10.1186/s12889-018-5597-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.U.S. Census Bureau. Population Estimates 1993–1999 www2.census.gov/programs-surveys/popest/tables/1990-2000/state/asrh/. Accessed June 14, 2019.
- 17.U.S. Census Bureau. Population Estimates 2010–2015 http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk. Accessed June 14, 2019.
- 18.U.S. Census Bureau. Population Estimates 2000–2009 www2.census.gov/programs-surveys/popest/datasets/2000-2010/intercensal/state/st-est00int-agesex.csv. Accessed June 14, 2019.
- 19.Minnesota State Demographic Center. Population Projections for 2016–2067 https://mn.gov/admin/demography/data-by-topic/population-data/our-projections/. Accessed April 5, 2018.
- 20.CDC. Fertility rates, mortality and birth rates by age and gender http://wonder.cdc.gov/cmf-icd10.html. Accessed August 15, 2015.
- 21.U.S. Census Bureau. Current Population Survey, September 1993: Tobacco Use Supplement File, Technical Documentation CPS-01 Washington, DC: U.S. Census Bureau; 2001. [Google Scholar]
- 22.Hatsukami DK, Henningfield JE, Kotlyar M. Harm reduction approaches to reducing tobacco-related mortality. Annu Rev Public Health 2004;25:377–395. 10.1146/annurev.publhealth.25.102802.124406. [DOI] [PubMed] [Google Scholar]
- 23.Hatsukami DK, Lemmonds C, Tomar SL. Smokeless tobacco use: harm reduction or induction approach? Prev Med 2004;38(3):309–317. 10.1016/j.ypmed.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 24.Phillips CV, Heavner KK. Smokeless tobacco: the epidemiology and politics of harm. Biomarkers 2009;14(suppl 1):79–84. 10.1080/13547500902965476. [DOI] [PubMed] [Google Scholar]
- 25.Tomar SL. Is use of smokeless tobacco a risk factor for cigarette smoking? The U.S. experience. Nicotine Tob Res 2003;5(4):561–569. 10.1080/1462220031000118667. [DOI] [PubMed] [Google Scholar]
- 26.Tomar SL. Epidemiologic perspectives on smokeless tobacco marketing and population harm. Am J Prev Med 2007;33(6 suppl):S387–S397. 10.1016/j.amepre.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 27.Burns DM, Anderson C, Major J, Vaughn J, Shanks T. Cessation and cessation measures among daily adult smokers: national- and state-specific data. In: Monograph 12: Population Based Smoking Cessation Proceedings of a Conference on What Works to Influence Cessation in the General Population Washington, DC: NIH, National Cancer Institute; 2000. [Google Scholar]
- 28.Zhu SH, Wang JB, Hartman A, et al. Quitting cigarettes completely or switching to smokeless tobacco: do U.S. data replicate the Swedish results? Tob Control 2009;18(2):82–87. 10.1136/tc.2008.028209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tam J, Day HR, Rostron BL, Apelberg BJ. A systematic review of transitions between cigarette and smokeless tobacco product use in the United States. BMC Public Health 2015;15:258 10.1186/s12889-015-1594-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chang JT, Levy DT, Meza R. Examining the transitions between cigarette and smokeless tobacco product use in the United States using the 2002–2003 and 2010–2011 longitudinal cohorts. Nicotine Tob Res 2018;20(11):1412–1416. 10.1093/ntr/ntx251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schauer GL, Pederson LL, Malarcher AM. Past year quit attempts and use of cessation resources among cigarette-only smokers and cigarette smokers who use other tobacco products. Nicotine Tob Res 2016;18(1):41–47. 10.1093/ntr/ntv038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Messer K, Vijayaraghavan M, White MM, et al. Cigarette smoking cessation attempts among current U.S. smokers who also use smokeless tobacco. Addict Behav 2015;51:113–119. 10.1016/j.addbeh.2015.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McWhorter WP, Boyd GM, Mattson ME. Predictors of quitting smoking: the NHANES I followup experience. J Clin Epidemiol 1990;43(12):1399–1405. 10.1016/0895-4356(90)90108-2. [DOI] [PubMed] [Google Scholar]
- 34.Gilpin EA, Pierce JP, Farkas AJ. Duration of smoking abstinence and success in quitting. J Natl Cancer Inst 1997;89(8):572–576. 10.1093/jnci/89.8.572. [DOI] [PubMed] [Google Scholar]
- 35.HHS. Reducing the health consequences of smoking: 25 years of progress: a report of the Surgeon General Atlanta, GA: CDC, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1989. [Google Scholar]
- 36.HHS. The Health Benefits of Smoking Cessation: a report of the Surgeon General Atlanta, GA: HHS, Public Health Service, CDC, Office on Smoking and Health;1990. [Google Scholar]
- 37.Thun MJ, Myers DG, Day-Lally C, et al. Age and the exposure-response relationships between cigarette smoking and premature death in Cancer Prevention Study II. In: Monograph 8: Changes in cigarette related disease risks and their implication for prevention and control Bethesda, MD: National Cancer Institute; 1997:383–475. [Google Scholar]
- 38.Burns D, Garfinkel L, Samet J, eds. Changes in Cigarette-Related Disease Risks and Their Implication for Prevention and Control Bethesda, MD: NIH, National Cancer Institute; 1997. [Google Scholar]
- 39.Henley SJ, Thun MJ, Connell C, Calle EE. Two large prospective studies of mortality among men who use snuff or chewing tobacco (United States). Cancer Causes Control 2005;16(4):347–358. 10.1007/s10552-004-5519-6. [DOI] [PubMed] [Google Scholar]
- 40.Levy DT, Cummings KM, Hyland A. Increasing taxes as a strategy to reduce cigarette use and deaths: results of a simulation model. Prev Med 2000;31(3):279–286. 10.1006/pmed.2000.0696. [DOI] [PubMed] [Google Scholar]
- 41.Levy DT, Mays D, Boyle RG, Tam J, Chaloupka FJ. The effect of tobacco control policies on U.S. smokeless tobacco use: a structured review. Nicotine Tob Res 2017;20(1):3–11. 10.1093/ntr/ntw291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huang J, Gwarnicki C, Xu X, Caraballo RS, Wada R, Chaloupka FJ. A comprehensive examination of own- and cross-price elasticities of tobacco and nicotine replacement products in the U.S. Prev Med 2018;117:107–114. 10.1016/j.ypmed.2018.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zheng Y, Zhen C, Dench D, Nonnemaker JM. U.S. demand for tobacco products in a system framework. Health Econ 2017;26(8):1067–1086. 10.1002/hec.3384. [DOI] [PubMed] [Google Scholar]
- 44.Levy DT, Tam J, Kuo C, Fong GT, Chaloupka F. The impact of implementing tobacco control policies: the 2017 Tobacco Control Policy Scorecard. J Public Health Manag Pract 2018;24(5):448–457. 10.1097/phh.0000000000000780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Orzechowski and Walker. The Tax Burden on Tobacco Volume 51, 1970–2016 Arlington, VA: Orzechowski and Walker; 2017. [Google Scholar]
- 46.Federal Trade Commission. Smokeless Tobacco Report for 2017 www.ftc.gov/system/files/documents/reports/federal-trade-commission-cigarette-report-2017-federal-trade-commission-smokeless-tobacco-report/ftc_smokeless_tobacco_report_2017.pdf. Accessed January 5, 2019.
- 47.Levy DT, Yuan Z. Prices and Taxes of Smokeless Tobacco, 2017. [working paper] Washington, DC: Georgetown University. [Google Scholar]
- 48.Bureau of Labor Statistics. Consumer Price Index www.bls.gov. Accessed January 5, 2019.
- 49.Levy DT, Friend K, Polishchuk E. Effect of clean indoor air laws on smokers: the clean air module of the SimSmoke computer simulation model. Tob Control 2001;10(4):345–351. 10.1136/tc.10.4.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.American Nonsmokers’ Rights Foundation. Summary of 100% Smokefree State Laws and Population Protected by 100% U.S. Smokefree Laws https://no-smoke.org/wp-content/uploads/pdf/EffectivePopulationList.pdf. Accessed March 2,2019.
- 51.Levy DT, Friend K. A computer simulation model of mass media interventions directed at tobacco use. PrevMed 2001;32(3):284–294. 10.1006/pmed.2000.0808. [DOI] [PubMed] [Google Scholar]
- 52.Huang J, Walton K, Gerzoff RB, et al. State tobacco control program spending – United States, 2011. MMWR Morb Mortal Wkly Rep 2015;64(24):673–678. [PMC free article] [PubMed] [Google Scholar]
- 53.Tobacco Free-Kids. Factsheet: State Tobacco Control Expenditures, 2000–2016 www.tobaccofreekids.org/research/factsheets/pdf/0209.pdf. Accessed September 2, 2017.
- 54.Levy DT, Graham AL, Mabry PL, Abrams DB, Orleans CT. Modeling the impact of smoking cessation treatment policies on quit rates. Am J Prev Med 2010;38(3 suppl):S364–S372. 10.1016/j.amepre.2009.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.North American Quitline Consortium. Quitline Stats www.naquitline.org/?page=800QUITNOWstats. Accessed August 30, 2015.
- 56.ClearWay MinnesotaSM, Minnesota Department of Health. Tobacco use in Minnesota: 2014 Update. Minneapolis, MN: ClearWay MinnesotaSM, Minnesota Department of Health; January 2015. [Google Scholar]
- 57.Clearway Minnesota. Minnesota Adult Tobacco Survey (MATS) 2014 http://clearwaymn.org/minnesota-adult-tobacco-survey-mats-2014/. Accessed May 15, 2018.
- 58.Levy DT, Friend K, Holder H, et al. Effect of policies directed at youth access to smoking: results from the SimSmoke computer simulation model. Tob Control 2001;10(2):108–116. 10.1136/tc.10.2.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chaloupka FJ, Tauras JA, Grossman M. Public policy and youth smokeless tobacco use. South Econ J 1997;64(2):503–516. 10.2307/1060863. [DOI] [Google Scholar]
- 60.Tauras J, Powell L, Chaloupka F, Ross H. The demand for smokeless tobacco among male high school students in the United States: the impact of taxes, prices and policies. Appl Econ 2007;39(1):31–41. 10.1080/00036840500427940. [DOI] [Google Scholar]
- 61.Choi K, Fabian LE, Brock B, Engman KH, Jansen J, Forster JL. Availability of snus and its sale to minors in a large Minnesota city. Tob Control 2014;23(5):449–451. 10.1136/tobaccocontrol-2012-050719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.ClearWay Minnesota, Minnesota Department of Health. Tobacco Use in Minnesota: 2010 Update. Minneapolis, MN: ClearWay Minnesota, Minnesota Department of Health; 2011. [Google Scholar]
- 63.Mumford EA, Levy DT, Gitchell JG, Blackman KO. Smokeless tobacco use 1992–2002: trends and measurement in the Current Population Survey-Tobacco Use Supplements. Tob Control 2006;15(3):166–171. 10.1136/tc.2005.012807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.McClave-Regan AK, Berkowitz J. Smokers who are also using smokeless tobacco products in the U.S.: a national assessment of characteristics, behaviours and beliefs of „dual users’. Tob Control 2011;20(3):239–242. 10.1136/tc.2010.039115. [DOI] [PubMed] [Google Scholar]
- 65.National Cancer Instute, CDC. Report on Smokeless Tobacco and Public Health: A Global Perspective Washington, DC: National Cancer Instute, CDC; 2014. [Google Scholar]
- 66.Mejia AB, Ling PM. Tobacco industry consumer research on smokeless tobacco users and product development. Am J Public Health 2010;100(1):78–87. 10.2105/ajph.2008.152603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Carpenter CM, Connolly GN, Ayo-Yusuf OA, Wayne GF. Developing smokeless tobacco products for smokers: an examination of tobacco industry documents. Tob Control 2009;18(1):54–59. 10.1136/tc.2008.026583. [DOI] [PubMed] [Google Scholar]
- 68.Richardson A, Ganz O, Stalgaitis C, Abrams D, Vallone D. Noncombustible tobacco product advertising: how companies are selling the new face of tobacco. Nicotine Tob Res 2014;16(5):606–614. 10.1093/ntr/ntt200. [DOI] [PubMed] [Google Scholar]
- 69.Koch SF. Quasi-experimental evidence on tobacco tax regressivity. Soc Sci Med 2018;196:19–28. 10.1016/j.socscimed.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 70.Pesko MF, Licht AS, Kruger JM. Cigarette price minimization strategies in the United States: price reductions and responsiveness to excise taxes. Nicotine Tob Res 2013;15(11):1858–1866. 10.1093/ntr/ntt068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pesko MF, Xu X, Tynan MA, Gerzoff RB, Malarcher AM, Pechacek TF. Per-pack price reductions available from different cigarette purchasing strategies: United States, 2009–2010. Prev Med 2014;63:13–19. 10.1016/j.ypmed.2014.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Levy DT, Mabry PL, Graham AL, Orleans CT, Abrams DB. Reaching healthy people 2010 by 2013: a SimSmoke simulation. Am J Prev Med 2010;38(3 suppl):S373–S381. 10.1016/j.amepre.2009.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Campaign for Tobacco-Free Kids. Broken Promises to our Children www.tobaccofreekids.org/problem/toll-us/minnesota. Accessed June 6, 2019.
- 74.Levy DT, Pearson JL, Villanti AC, et al. Modeling the future effects of a menthol ban on smoking prevalence and smoking-attributable deaths in the United States. Am J Public Health 2011;101(7):1236–1240. 10.2105/ajph.2011.300179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.National Cancer Institute, CDC. Report on Smokeless Tobacco and Public Health: A Global Perspective Washington, DC: National Cancer Institute, CDC; 2014. [Google Scholar]
- 76.Lee YO, Hebert CJ, Nonnemaker JM, Kim AE. Multiple tobacco product use among adults in the United States: cigarettes, cigars, electronic cigarettes, hookah, smokeless tobacco, and snus. Prev Med 2014;62:14–19. 10.1016/j.ypmed.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 77.Office of the Revisor of Statutes State of Minnesota. Minnesota Session Laws - 2013, Regular Session, Chapter 143, Article 5 (HF 677) 2013; www.revisor.mn.gov/data/revisor/law/2013/0/2013-143.pdf. Published 2013. Accessed August 14, 2017.
- 78.Levy DT, Cummings KM, Villanti AC, et al. A framework for evaluating the public health impact of e-cigarettes and other vaporized nicotine products. Addiction 2017;112(1):8–17. 10.1111/add.13394. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.