Abstract
Objective
Ultrasound-guided regional anaesthesia using transversus abdominis plane (TAP) block is a newer and safer method that can be used in patients undergoing liver transplant surgeries. This systematic review and meta-analysis was done to quantify the analgesic potential and opioid-sparing capability of TAP block in these patients.
Methods
The studies comparing TAP-block to conventional analgesic regimens for liver transplant were searched. The studies evaluating the comparative 24-h morphine consumption during postoperative period in patients undergoing liver transplant surgeries were searched and included as the primary outcome in the analysis.
Results
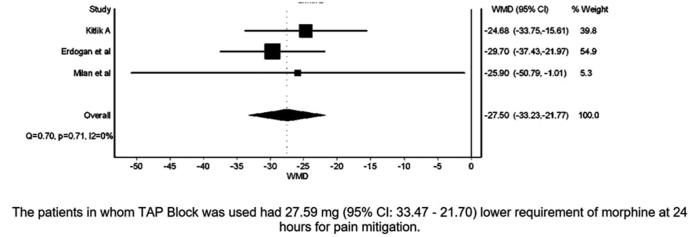
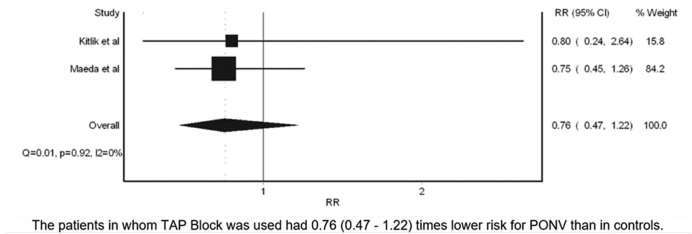
We found two randomised controlled trials and two retrospective studies that on meta-analysis showed that TAP block group had significantly lower requirement of morphine (WMD=27.59 mg; 95% CI: 33.47–21.70) at 24 h for pain mitigation. Also, postoperative nausea and vomiting was lower (RR=0.76; 95% CI: 0.47–1.22) but not statistically significant.
Conclusion
Ultrasound-guided TAP block provides postoperative analgesic efficacy in patients undergoing liver transplant surgeries. This study was registered in International prospective register of systematic reviews [PROSPERO: CRD42018094595].
Keywords: 24-h morphine, transversus abdominis plane (TAP) block, postoperative nausea and vomiting
Introduction
For patients undergoing liver transplant surgeries, adequate analgesia can often be challenging for the transplant teams. Prescriptions of analgesic drugs need consideration for deranged pharmacokinetics of drugs and higher chances of associated adverse effects (1). Perioperative care teams rely on opioids or different forms of regional analgesia. The use of epidural analgesia is considered as a gold standard for major abdominal surgeries, but it also has limitations in this population because of altered coagulation profile (2). Evidence suggests against the use of central neuraxial block in patients with chronic liver failure due to associated coagulation disorders (3).
Many trials have studied different regimens that can have opioid-sparing effect for patients undergoing organ transplantation (4). Recently, ultrasound-guided peripheral nerve blockade has been used for management of acute postoperative pain. These blocks can be executed with low risk of complications (5). Transversus abdominis plane (TAP) block is one of them. It requires anaesthesia to the sensory nerve supply of the anterior abdominal wall. Blockade of sensory nerves is achieved in the neurofascial plane between the internal oblique and transversus abdominis muscles either through landmarks technique or by use of ultrasound (6).
Ultrasound-guided regional anaesthesia using TAP block is a relatively newer and safer method in patients undergoing open abdominal surgeries like liver transplant donors and recipients for perioperative analgesia and opioid-sparing potential (7). This systematic review and meta-analysis was done to review the existing evidence and quantify the analgesic potential and opioid-sparing capability of TAP block in patients undergoing liver transplant surgeries.
Methods
This study was registered in International prospective register of systematic reviews [PROSPERO: CRD42018094595]. For the present analysis, Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines were followed. A population, intervention, control, and outcome study (PICOS) format was used to identify the potential trials that could be included in the present meta-analysis. After literature search, trials were abstracted into a standardised PICOS format (Table 1), and two independent reviewers assessed relevance to our research question. The studies evaluating the comparative 24-h morphine consumption during postoperative period in patients undergoing liver transplant surgeries were included as the primary outcome in the analysis. The salient features of trials included in the final analysis are shown in Table 2.
Table 1.
Data extraction framework based on PICOS format
| Population |
|
| Interventions | Patients receiving local-anaesthetic-based transverse abdominis plane (TAP) block during the preoperative or imme diately after the surgery. The TAP block could be single shot or catheter-guided continuous block. TAP block could be ultrasound-guided, tactile-pop-based or surgeon-assisted catheter insertion during closure. |
| Controls | Donor and recipients undergoing liver transplant surgery and receiving perioperative multimodal intravenous anal gesia not based on TAP block. |
| Outcomes |
Primary outcome Comparison of first postoperative day opioids (in morphine equivalents) consumption in both the groups Secondary outcome Postoperative nausea vomiting incidence comparison |
| Study design | Comparative trials evaluating use of TAP block against conventional intravenous analgesics – including prospective, retrospective cohort and case series. |
Table 2.
Data extraction sheet
| Author/Year | County | Study Design | Participant Profile | Intervention Group Characteristics (USG-guided TAP + IV Opioid) Timing/USG-guided TAP | Control Group Characteristics (Only IV opioid used) | Measured Outcomes |
|---|---|---|---|---|---|---|
|
| ||||||
| Kitlik et al. (13) (2017) | Turkey | RCT-double blinded | 18 65 Yr, Living Liver Donors TAP (n=25) IV (n=25) |
Inj. 0.5% bupivacaine at the conclusion of surgery Single injection bilateral subcostal mL each side; total 40 mL) |
Intraoperative: - Remifentanil - Morphine Postoperative: - Morphine PCA - Acetaminophen |
- Postoperative Opioid (24-h morphine consumption) - Pain Intensity (VAS) at rest and movement - PONV |
| Erdogan et al. (14) (2017) | Turkey | RCT-double blinded | 18 65 Yr, Living Liver Donors TAP (n=22) IV (n=22) |
Inj. 0.5% bupivacaine before surgical incision Single injection bilateral subcostal (20 mL each side; total 40 mL) |
Intraoperative: - Fentanyl - Remifentanil - Morphine PCA - IV acetaminophen |
- Postoperative Opioid (24-h morphine consumption) - Perioperative remifentanil consumption - Mean BP - HR - Mean desflurane requirement - Anaesthesia recovery time, - Frequency of emergency vasopressor use - Length of hospital stay |
| Maeda et al. (15) (2015) | Japan | Retrospective | Adult (>16 Yr) Living Live donors TAP (n=16) IV (n=16) |
(>16 Yr) X levobupivacaine at the conclusion of surgery Single injection bilateral subcostal (10 mL each side; total 20 mL) AND Continuous subcostal infusion of 0.125% levobupivacaine for 48 h |
Intraoperative: - Fentanyl - Remifentanil - Flurbiprofen Postoperative (either of following): - Fentanyl - Flurbiprofen - Acetaminophen or - Oral loxoprofen |
- Cumulative postop fentanyl consumption for 48 h - Time to first supplemental analgesia - Total number of requests for supplemental analgesia - VRS scores at 3, 6, 12, 24 and 48 h postop - PONV in the first and second 24 h - PT-INR value - Number of meals missed postop - Duration of postop hospital stay |
| Milan et al. (16) (2011) | United Kingdom | Retrospective pilot study | Adult Liver Transplant Recipients TAP (n=17) IV (n=17) |
Inj. 0.5% levobupivacaine before surgical incision Single injection bilateral subcostal (20 ml each side; total 40 ml) |
Intraoperative: - Remifentanil Postoperative: - Morphine PCA - IV acetaminophen |
- Postoperative Opioid (24-h morphine consumption) - Pain scores - Time to extubation |
Search strategy
Two independent researchers performed the preliminary data search in Cochrane Central Register of Controlled Trials, Clinical trial registry, PubMed, Scopus and Google Scholar. Comparative trials published until April 2018 were included in the analysis. The following keywords were searched for in the above said databases – (“transversus abdominis plane block” OR “TAP Block”) AND (“Liver Transplantation”[Mesh] OR “Liver transplantation” OR “Liver transplant” OR “Hepatic transplantation” OR “OLT” OR “Liver donor” OR “Liver recipient”). In this analysis, comparative trials of both prospective and retrospective nature were included.
We also manually searched the references for relevant studies in grey literature and peer-reviewed abstracts published in the proceedings of meetings. Once the abstracts were analysed by the authors and found appropriate, the full text of the articles were further studied. The decision to include a trial into final analysis was based on the independent assessment of the two authors. Any disagreements between the two were harmonised by consensus and arbitration by a third neutral author. Another independent researcher assessed for quality of evidence and possible methodological bias.
Data extraction
Data were abstracted into a standardised format for characteristics like study design, country of publication, year, sample size, primary and secondary outcomes, drug doses used in TAP block, use of ultrasound, catheter for continuous block, opioids needed in perioperative period, pain scores at various time intervals, incidence of postoperative nausea vomiting (PONV), and specific adverse effects (Table 2). Authors who had reported outcomes as median and interquartile range were contacted to provide values in mean and standard deviation. If authors did not reply, we estimated the mean using the validated formula: mean=(2m + a + b)/4 where m is the median and a and b are first and third quartiles, respectively (8). The SD was estimated by the formula given by the Higgins et al: interquartile range=1.35 SD (9, 10).
Statistical analysis
Data were pooled for meta-analysis using MetaXL plugin for Microsoft Excel (11). Fixed effect model and random effect model were used based on the absence or presence of significant heterogeneity, which was in turn assessed using the I2 statistic. I2 values of >90% were considered as high heterogeneity between studies; 40%–90% was considered as moderate heterogeneity and <40% as low heterogeneity (12). Continuous variables like 24-h morphine consumption between intervention and control groups were expressed as pooled mean differences. Dichotomous variables like presence of postoperative nausea and vomiting (PONV) were expressed as pooled relative risks. Sensitivity analysis was done for studies having extreme effect estimates. P value <0.05 was considered significant. Publication bias was assessed using Egger’s test and funnel plot.
Results
We searched Cochrane Central Register of Controlled Trials, Clinical trial registry, PubMed, Scopus and Google Scholar for eligible articles. Cross-references and manual searching was also performed. There were 627 articles regarding TAP Block in PubMed and 405 in Cochrane database of which 6 articles were about comparative assessment in patients with liver transplant. Two articles were in duplicate thus giving four eligible articles whose full texts were read for inclusion in systematic review. Of these, two were prospective randomised trials by Kitlik et al. (13) and Erdogan et al. (14). Other two by Maeda et al. (15) and Milan et al. (16) have performed retrospective comparisons between patients receiving TAP block and otherwise. Out of these four articles, three studies [Kitlik et al. (13), Erdogan al. (14) and Maeda et al. (15)] were on living liver donors, and one study [Milan et al. (16)] included liver transplant recipients. All the four studies were included for systematic review (Figure 1).
Figure 1.
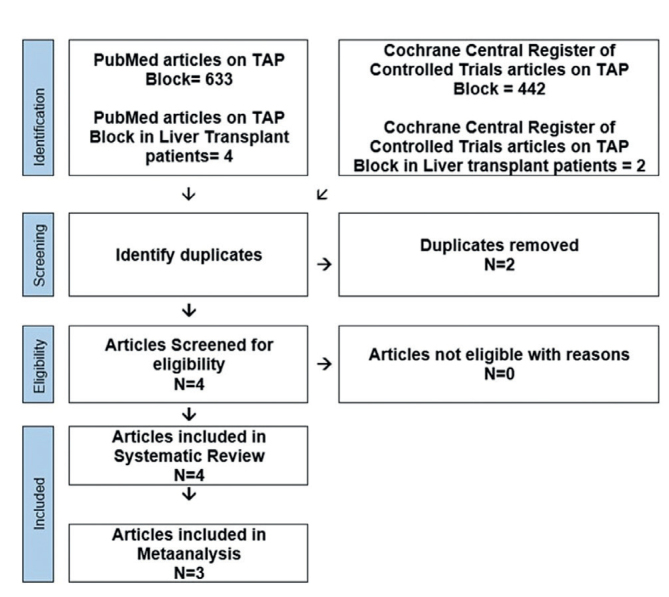
PRISMA flowchart
Kitlik et al. (13) in Turkey have compared 25 liver transplant donors receiving ultrasound-guided TAP block with another 25 donors who did not receive TAP block. The mean total morphine consumption values after 24 h were 40 mg and 65 mg, respectively. They found that the TAP block significantly reduced 24-h postoperative morphine consumption and postoperative visual analogue pain scores (VAS) both at rest and during movement till 24 hours.
Erdogan et al. (14) also compared 22 living liver donors who received subcostal TAP block in combination with 22 who received general anaesthesia alone. They concluded that combining subcostal TAP blocks with general anaesthesia significantly decreased opioid consumption and provided shorter anaesthesia recovery time and length of hospital stay in living liver donors. In this study, pain intensity was not compared between the two groups.
Maeda et al. (15) in their retrospective analysis compared 16 living liver donors receiving continuous subcostal TAP block with 16 donors who received only IV fentanyl-based analgesia. The result of this study showed that continuous subcostal TAP block provided an effective opioid-sparing analgesia, lower incidence of nausea and vomiting during 24–48 h postoperatively and fewer delays in the initiation of oral intake. In this study, pain intensity was assessed on a four-level verbal rating scale (VRS) scores, which were lower in the TAP group than in the control group at 3 h and 6 h.
Milan et al. (16) retrospectively compared 17 liver transplant recipients receiving TAP block with 17 patients who received only IV analgesia. The total amount of morphine consumption over 24 h was 45.9±33.9 mg in the TAP group and 71.8 ± 39.9 mg in the control group (p<0.005). Their study showed significant reduction in postoperative morphine consumption in recipients who received TAP block. In this study, pain scores (0 – no pain and 3 – worst pain imaginable) were lower in the TAP group, but there was no significant difference compared with the control group.
The pooled effect size by random effects model showed that TAP group had 27.59 mg (95% CI: 33.47–21.70) lower requirement of morphine at 24 h for pain mitigation (Figure 2 and Table 3). However, this measure is only from two studies from a single centre and are highly homogenous as shown by I2=0%. This may reduce the generalisability of findings. The patients in whom TAP block was used had 0.76 (0.47–1.22) times lower risk for PONV than in controls, but this was not statistically significant (Figure 3).
Figure 2.
Forest plot showing effect of TAP block on 24-h morphine use
Table 3.
Steps in calculation of pooled estimate
| Study | Intervention group | Control group | Mean difference (Xi −Xj) | Variance of mean difference | Weights=1/Var(D) | WiDi | Pooled estimate | S.E. of pooled estimate | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean (Xi) | SD | n | Mean (Xj) | SD | |||||||
|
| ||||||||||||
| a | b | c | d | e | f | g (=b−e) | h | i (=1/h) | j (=i × g) | k | l | |
|
| ||||||||||||
| Kitlik et al. (13)* | 25 | 40.96 | 14.80 | 25 | 65.64 | 17.79 | −24.68 | 21.42 | 0.047 | −1.152 | ||
| Erdogan et al. (14)* | 22 | 40.75 | 13.44 | 22 | 70.45 | 12.72 | −29.70 | 15.57 | 0.064 | −1.908 | ∑ WiDi/∑ Wi | |
| Milan et al. (16) | 17 | 45.90 | 33.9 | 17 | 71.80 | 39.90 | −25.90 | 161.25 | 0.006 | −0.161 | ||
| 0.117 | −3.221 | −27.50 | 2.922 | |||||||||
Data were reported as median in published article. Their mean and standard deviation were provided by authors
Figure 3.
Forest plot showing effect of TAP block on risk of PONV
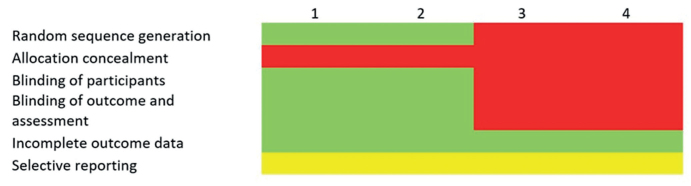
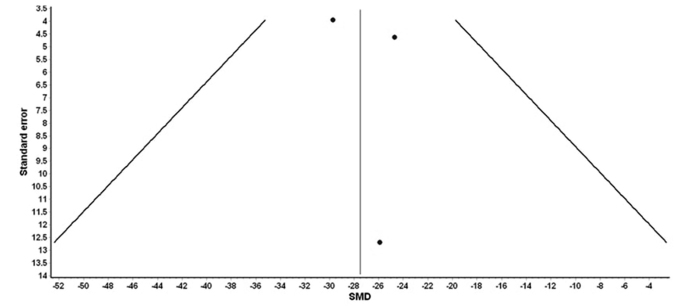
As per established guidelines of Cochrane collaboration, the quality assessment for bias in the included studies was performed as shown in Figure 4. Publication bias was examined for the primary outcome. There is a chance of publication bias in the included studies to report lesser morphine consumption with TAP block. Funnel plot distribution was skewed with studies results falling beyond expected neutral funnel boundary (towards positive side) (Figure 5). Egger’s regression test also confirmed the above finding.
Figure 4.
Assessment of risk of bias summary of all analysed studies as per Cochrane collaboration recommendations
Figure 5.
Funnel plot evaluating publication bias length of stay showing asymmetrical distribution of trials
Discussion
This meta-analysis and systematic review of the literature is the first to evaluate the postoperative analgesic efficacy of ultrasound-guided TAP block in liver transplant surgery recipients and donors. Here, we have reviewed two randomised controlled trials and two retrospective studies having 160 participants. Although the sample size is small, it reiterates the benefit of TAP block as shown by many other studies in other abdominal surgeries like renal transplantation (17), caesarean section (18), hernia surgery (19), laparoscopic cholecystectomy (20), laparoscopic gastric sleeve resection (21), radical cystectomy (22), abdominoplasty (23), colorectal surgery (24), and meta-analysis in various other surgeries (25–29). In this study, the patients in whom TAP block was used had 27.59 mg (95% CI: 33.47–21.70) lower morphine requirement at 24 h for pain mitigation. The patients in whom TAP block was used had 0.76 (0.47–1.22) times lower risk for PONV than in controls.
Epidural blockade is used most commonly for intraoperative and postoperative analgesia in living donor liver transplantation (LDLT) donors (30). These living liver donors are at risk of deranged coagulation profile after donor hepatectomy (31). Maeda et al. (15) in their study incidentally found two donors who had higher PT-INR than 1.5 even after two days after operation, which might have caused a delay in epidural catheter removal or a serious haematoma if they had received epidural analgesia. They emphasised that an alternative method that ensures safety against potential risk is desirable. TAP block is one of the options available in these patients as it can be administered in patients with coagulopathies. It will help in change of practice of putting the epidural in LDLT donors and then waiting for stopping of heparin dose to remove epidural catheters as we usually do at our centres.
Our meta-analysis shows a significant morphine-sparing effect of the TAP block in patients undergoing liver transplant surgery. Any reduction in intraoperative opioid analgesics that may also cause sedation would also improve recovery profile and eventually lower the sedation-related complications (32).
TAP block provides analgesia by blocking somatic component of pain sparing the visceral component. This limitation can be overcome by supplementing with NSAIDs, paracetamol, tramadol, gabapentin, N methyl D- aspartic acid antagonist and so on. TAP block can be included as a part of multimodal analgesia for open or laparoscopic abdominal surgeries. It can be used for the postoperative analgesia depending on the choice and skills of the anaesthesiologist supplementing intravenous (IV)/intramuscular (IM) analgesics for these surgeries (33). Various studies in the literature have established that additional analgesic requirements and related adverse effects can be reduced by supplementing a multimodal analgesic regimen with a TAP block (17, 18). Compared with the standard regimen alone, it also increases the duration of first analgesic request and provides better satisfaction with pain relief (33).
Opioids act on presynaptic receptors in the myenteric nerve plexuses that leads to more non-propulsive contraction of the bowel, by that decreasing forward peristalsis (34). In this way, TAP block can also reduce incidence of postoperative ileus caused by opioids and thus shortens the hospital stay.
There are massive fluids shifts after functioning of graft during immediate transplant period. If it does not function properly, it is difficult to predict fluid dynamics and the pharmacokinetics of systemically administered drugs (17). TAP block reduces opioid requirements and has a positive clinical impact by lowering the need for systemic analgesic drugs.
Patient satisfaction towards surgery is influenced by many intra and postoperative factors. Pain and PONV are the most common causes of dissatisfaction. Our analysis shows that not only analgesic requirements in TAP block are lower but the PONV incidence tends to be smaller. Meta-analyses of TAP block in renal transplant recipients by Singh et al. (17) revealed a decrease in the 24-h opioid consumption by 14.61±4.34 mg that was in accordance with the results of the present study. Similar to our study, the two larger meta-analyses using TAP block for analgesia showed a decrease of IV morphine consumption of 9.1 and 5.7 mg within the first 24 h postoperatively (35, 36).
The results of our meta-analysis have several limitations. Not many centres seem to have started using TAP block for liver transplantation. We could find only four studies of which only two were randomised control trials. More RCTs at different centres and setups will be required for more robust evidence in favour of TAP block in liver transplantation. None of the included studies specifically sought to assess the sensory blockade after the ultrasound-guided TAP block. Thus, the success rate of the technique is unknown and may therefore have affected our analysis. We could not compare pain scores as various studies used different pain scales. Finally, we could not pool time to discharge, because only one prospective trial and one retrospective study sought to capture this outcome. Consequently, the impact of the ultrasonography-guided TAP block on functional outcomes during postoperative recovery remains undetermined.
Conclusion
Ultrasonography-guided TAP block provides postoperative analgesic efficacy in patients undergoing liver transplant surgeries.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – A.S.; Design – A.S., A.D.G.; Supervision – V.V.; Resources – A.S., A.D.G.; Materials – A.S.; Data Collection and/or Processing – A.S., A.D.G.; Analysis and/or Interpretation – A.D.G., P.P.S., V.V.; Literature Search – S.P.A., V.V., A.S.; Writing Manuscript – A.S., A.D.G.; Critical Review – V.V., S.P.A.; Other – P.P.S., V.V.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Sladen RN. Perioperative care for the patient with renal or hepatic disease. Anaesthesia Analgesia. 2001;92(Suppl):99–103. doi: 10.1097/00000539-200103001-00016. [DOI] [Google Scholar]
- 2.Listing H, Pöpping D. Pro: Epidural Analgesia Remains the Gold Standard for Abdominal and Thoracic Surgery. Anasthesiol Intensivmed Notfallmed Schmerzther. 2018;53:237–44. doi: 10.1055/s-0043-104668. [DOI] [PubMed] [Google Scholar]
- 3.Torgeson M, Kileny J, Pfeifer C, Narkiewicz L, Obi S. Conventional Epidural vs Transversus Abdominis Plane Block with Liposomal Bupivacaine: A Randomized Trial in Colorectal Surgery. J Am Coll Surg. 2018;227:78–83. doi: 10.1016/j.jamcollsurg.2018.04.021. [DOI] [PubMed] [Google Scholar]
- 4.Zhang B, Liu GWX, Wang T, Chi P. The Opioid-Sparing Effect of Perioperative Dexmedetomidine Combined with Oxycodone Infusion during Open Hepatectomy: A Randomized Controlled Trial. Front Pharmacol. 2017;8:940. doi: 10.3389/fphar.2017.00940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martins LES, Ferraroa LHC, Takedaa A, Munechikaa M, Tardelli MA. Ultrasound-guided peripheral nerve blocks in anticoagulated patients - case series. Rev Bras Anestesiol. 2017;67:100–6. doi: 10.1016/j.bjan.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 6.Kadam RV, Field JB. Ultrasound-guided continuous transverse abdominis plane block for abdominal surgery. J Anaesthesiol Clin Pharmacol. 2011;27:333–6. doi: 10.4103/0970-9185.83676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Milan Z. Analgesia after liver transplantation. World J Hepatol. 2015;7:2331–5. doi: 10.4254/wjh.v7.i21.2331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hernandez AV, Guarnizo M, Miranda Y, Pasupuleti V, Deshpande A, Paico S, et al. Association between insulin resistance and breast carcinoma: A systematic review and meta-analysis. PLoS One. 2014;9:e99317. doi: 10.1371/journal.pone.0099317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi S, Rodseth R, McCartney CJ. Effects of dexamethasone as a local anaesthetic adjuvant for brachial plexus block: A systematic review and meta-analysis of randomized trials. Br J Anaesth. 2014;112:427–39. doi: 10.1093/bja/aet417. [DOI] [PubMed] [Google Scholar]
- 10.Higgins J, Deeks J. Cochrane Handbook for Systematic Reviews of Interventions Ver. The Cochrane Collaboration; 2011. Selecting studies and collecting data; p. 510. [Last updated on 2011 Mar]. Available from: http://www.cochrane-handbook.org. [Google Scholar]
- 11.Neyeloff JL, Fuchs SC, Moreira LB. Meta-analyses and Forest plots using a microsoft excel spreadsheet: step-by-step guide focusing on descriptive data analysis. BMC Res Notes. 2012;5:52. doi: 10.1186/1756-0500-5-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Loannidis JPA, Patsopoulos NA, Evangelou E. Uncertainty in heterogeneity estimates in meta-analyses. Br Med J. 2007;335:914–6. doi: 10.1136/bmj.39343.408449.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kıtlık A, Erdogan MA, Ozgul U, Aydogan MS, Ucar M, Toprak HI, et al. Ultrasound-guided transversus abdominis plane block for postoperative analgesia in living liver donors: A prospective, randomized, double-blinded clinical trial. J Clin Anaesth. 2017;37:103–7. doi: 10.1016/j.jclinane.2016.12.018. [DOI] [PubMed] [Google Scholar]
- 14.Erdogan MA, Ozgul U, Uçar M, Yalin MR, Colak YZ, Çolak C, et al. Effect of transversus abdominis plane block in combination with general anaesthesia on perioperative opioid consumption, hemodynamics, and recovery in living liver donors: The prospective, double-blinded, randomized study. Clin Transplant. 2017;31 doi: 10.1111/ctr.12931. doi: 10.1111/ctr.12931. [DOI] [PubMed] [Google Scholar]
- 15.Maeda A, Shibata SC, Wada H, Marubashi S, Kamibayashi T, Eguchi H, et al. The efficacy of continuous subcostal transversus abdominis plane block for analgesia after living liver donation: a retrospective study. J Anesth. 2016;30:39–46. doi: 10.1007/s00540-016-2144-y. [DOI] [PubMed] [Google Scholar]
- 16.Milan ZB, Duncan B, Rewari V, Kocarev M, Collin R. Subcostal transversus abdominis plane block for postoperative analgesia in liver transplant recipients. Transplant Proc. 2011;43:2687–90. doi: 10.1016/j.transproceed.2011.06.059. [DOI] [PubMed] [Google Scholar]
- 17.Singh PM, Borle A, Makkar JK, Trisha A, Sinha A. Evaluation of transversus abdominis plane block for renal transplant recipients – A meta-analysis and trial sequential analysis of published studies. Saudi J Anaesth. 2018;12:261–71. doi: 10.4103/sja.SJA_598_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mishriky BM, George RB, Habib AS. Transversus abdominis plane block for analgesia after Cesarean delivery: a systematic review and meta-analysis. Can J Anaesth. 2012;59:766–78. doi: 10.1007/s12630-012-9729-1. [DOI] [PubMed] [Google Scholar]
- 19.Gao T, Zhang JJ, Xi FC, Shi JL, Lu Y, Tan SJ, et al. Evaluation of Transversus Abdominis Plane (TAP) Block in Hernia Surgery: A Meta-analysis. Clin J Pain. 2017;33:369–75. doi: 10.1097/AJP.0000000000000412. [DOI] [PubMed] [Google Scholar]
- 20.Peng K, Ji FH, Liu HY, Wu SR. Ultrasound-Guided Transversus Abdominis Plane Block for Analgesia in Laparoscopic Cholecystectomy: A Systematic Review and Meta-Analysis. Med Princ Pract. 2016;25:237–46. doi: 10.1159/000444688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mittal T, Dey A, Siddhartha R, Nali A, Sharma B, Malik V. Efficacy of ultrasound-guided transversus abdominis plane (TAP) block for postoperative analgesia in laparoscopic gastric sleeve resection: a randomized single blinded case control study. Surg Endosc. 2018;32:4985–9. doi: 10.1007/s00464-018-6261-6. [DOI] [PubMed] [Google Scholar]
- 22.Matulewicz RS, Patel M, Jordan BJ, Morano J, Frainey B, Bhanji Y, et al. Transversus Abdominis Plane Blockade as Part of a Multimodal Postoperative Analgesia Plan in Patients Undergoing Radical Cystectomy. Bladder Cancer. 2018;4:161–7. doi: 10.3233/BLC-170157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fiala T. Tranversus abdominis plane block during abdominoplasty to improve postoperative patient comfort. Aesthet Surg J. 2015;35:72–80. doi: 10.1093/asj/sju019. [DOI] [PubMed] [Google Scholar]
- 24.Liu L, Xie YH, Zhang W, Chai XQ. Effect of Transversus Abdominis Plane Block on Postoperative Pain after Colorectal Surgery: A Meta-Analysis of Randomized Controlled Trials. Med Princ Pract. 2018;27:158–65. doi: 10.1159/000487323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brogi E, Kazan R, Cyr S, Giunta F, Hemmerling TM. Transversus abdominal plane block for postoperative analgesia: a systematic review and meta-analysis of randomized-controlled trials. Can J Anaesth. 2016;63:1184–96. doi: 10.1007/s12630-016-0679-x. [DOI] [PubMed] [Google Scholar]
- 26.Hamill JK, Rahiri JL, Liley A, Hill AG. Rectus sheath and transversus abdominis plane blocks in children: a systematic review and meta-analysis of randomized trials. Paediatr Anaesth. 2016;26:363–71. doi: 10.1111/pan.12855. [DOI] [PubMed] [Google Scholar]
- 27.Yu N, Long X, Lujan-Hernandez JR, Succar J, Xin X, Wang X. Transversus abdominis-plane block versus local anesthetic wound infiltration in lower abdominal surgery: a systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2014;14:121. doi: 10.1186/1471-2253-14-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abdallah FW, Laffey JG, Halpern SH, Brull R. Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: a meta-analysis. Br J Anaesth. 2013;111:721–35. doi: 10.1093/bja/aet214. [DOI] [PubMed] [Google Scholar]
- 29.Siddiqui MR, Sajid MS, Uncles DR, Cheek L, Baig MK. A meta-analysis on the clinical effectiveness of transversus abdominis plane block. J Clin Anaesth. 2011;23:7–14. doi: 10.1016/j.jclinane.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 30.Koul A, Pant D, Rudravaram S, Sood J. Thoracic epidural analgesia in donor hepatectomy: An analysis. Liver Transpl. 2018;24:214–21. doi: 10.1002/lt.24989. [DOI] [PubMed] [Google Scholar]
- 31.Singh SA, Vivekananthan P, Sharma A, Sharma S, Bharathy KGS. Retrospective analysis of post-operative coagulopathy after major hepatic resection at a tertiary care centre in Northern India. Indian J Anaesth. 2017;61:575–80. doi: 10.4103/ija.IJA_734_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Amornyotin S. Sedation-related complications in gastrointestinal endoscopy. World J Gastrointest Endosc. 2013;5:527–33. doi: 10.4253/wjge.v5.i2.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dwivedi D, Bhatnagar V, Goje HK, Ray A, Kumar P. Transversus abdominis plane block: A multimodal analgesia technique-Our experience. J Mar Med Soc. 2017;19:38–42. doi: 10.4103/jmms.jmms_9_17. [DOI] [Google Scholar]
- 34.Kehlet H, Holte K. Review of postoperative ileus. Am J Surg. 2001;182(Suppl 5A):3S–10S. doi: 10.1016/S0002-9610(01)00781-4. [DOI] [PubMed] [Google Scholar]
- 35.Abdallah FW, Laffey JG, Halpern SH, Brull R. Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: a meta-analysis. Br J Anaesth. 2013;111:721–35. doi: 10.1093/bja/aet214. [DOI] [PubMed] [Google Scholar]
- 36.De Oliveira GS, Jr, Castro-Alves LJ, Nader A, Kendall MC, McCarthy RJ. Transversus abdominis plane block to ameliorate postoperative pain outcomes after laparoscopic surgery: a meta-analysis of randomized controlled trials. Anaesthesia Analgesia. 2014;118:454–63. doi: 10.1213/ANE.0000000000000066. [DOI] [PubMed] [Google Scholar]