Abstract
Objectives
How advance care planning (ACP) is conceptualised in Australia including when, where and how ACP is best initiated, is unclear. It has been suggested that healthcare delivered in general practice provides an optimal setting for initiation of ACP discussions but uptake remains low. This systematic review and critical interpretive synthesis sought to answer two questions: (1) What are the barriers and enablers to uptake of ACP in general practice? (2) What initiatives have been used to increase uptake of ACP in general practice?
Design
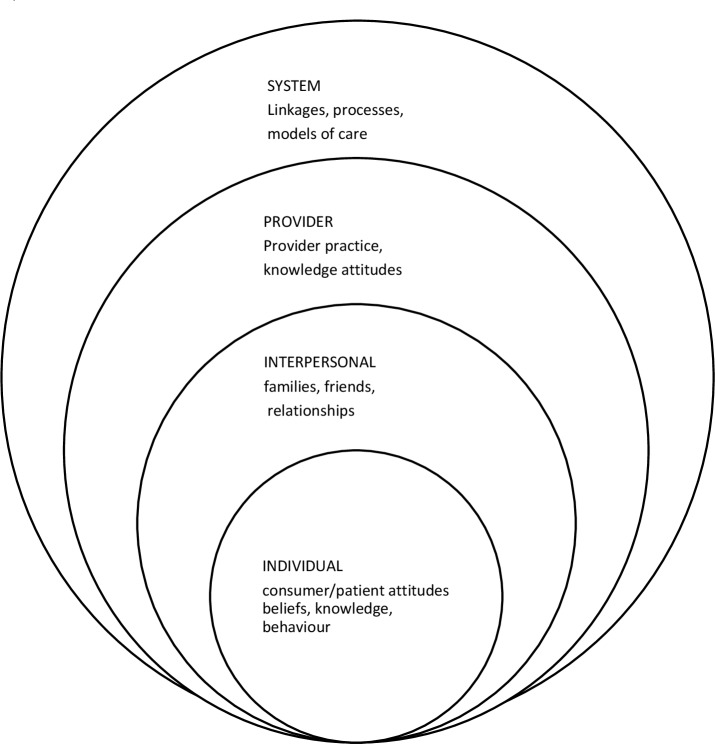
A systematic review and critical interpretive synthesis of the peer-reviewed literature was undertaken. A socioecological framework was used to interpret and map the literature across four contextual levels of influence including individual, interpersonal, provider and system levels within a general practice setting.
Setting
Primary care general practice settings
Data sources
Searches were undertaken from inception to July 2019 across Ovid Medline, Cumulative Index to Nursing and Allied Health Literature, Scopus, ProQuest and Cochrane Library of systematic reviews.
Results
The search yielded 4883 non-duplicate studies which were reduced to 54 studies for synthesis. Year of publication ranged from 1991 to 2019 and represented research from nine countries. Review findings identified a diverse and disaggregated body of ACP literature describing barriers and enablers to ACP in general practice, and interventions testing single or multiple mechanisms to improve ACP generally without explicit consideration for level of influence. There was a lack of cohesive guidance in shaping effective ACP interventions and some early indications of structured approaches emerging.
Conclusion
Findings from this review present an opportunity to strategically apply the ACP research evidence across targeted levels of influence, and with an understanding of mediators and moderators to inform the design of new and enhanced ACP models of care in general practice.
PROSPERO registration number
CRD42018088838
Keywords: advance care planning, advance directives, living will, general practice, family practice, primary care, interventions, socioecological perspective, causal mechanisms, knowledge, attitudes
Strengths and limitations of this study.
Use of the Joanna Briggs tools for quality assessment provided a rigorous quality assessment process tailored to study type.
Use of a conceptual framework provided a useful structure for critical synthesis of a complex body of literature and provides opportunity for future intervention design.
Studies identified with a focus on advance care planning interventions in general practice were limited.
Lack of consistent terminology may have resulted in not all relevant literature being surfaced.
The study is seeking transferability of international experience to the Australian context and this is uncertain.
Introduction
Within the Australian healthcare policy framework, advance care planning (ACP) is intended to ensure quality care according to individual wishes at end of life.1 An advance care plan, sometimes called a ‘living will’ or an advance care directive provides directions describing how an individual would prefer to be treated in the event of a loss of capacity to direct one’s own care.2 ACP emerged as a rights-based initiative in the USA in response to societal demand for the right to self-determination about medical care at end of life.1 This concern resonates internationally including in Australia where policies and/or laws have been enacted across all states and territories to support the uptake of ACP.1–4
Australia’s population profile is increasingly aged with an increasing life expectancy.5 For most Australians death will occur ‘at an advanced age following a period of chronic illness and decline’.6 Associated with increasing age, loss of cognition may limit an individual’s ability to make autonomous decisions at end of life.7 Advances in medical technology have resulted in the ability of practitioners to intervene and maintain life past what was previously possible, though quality of life resulting from the interventions is not assured.8 In these contexts, ACP is viewed as an important and emerging issue in the public health domain.6 7
Given Australia’s ageing demographic profile,5 and an identified societal concern about quality of life at the end of life,4 8 combined with a clearly stated policy position, it is difficult to explain why there has been limited uptake of ACP by consumers.9 10 A 2014 national study identified uptake of ACP in Australia as ~14%.10 There appear to be significant differences in how ACP is conceptualised in Australia,11 and uncertainty about where in the system responsibility lies for initiating an advance care plan. Many studies suggest primary care is optimal for initiation of discussions,12–15 though a 2019 multicentre audit determined ACP in general practice to be as low as 3%.16
This systematic review sought to synthesise the published literature to understand how the knowledge, attitudes and practices of clinicians and consumers in general practice are understood as barriers and or enablers to achieving uptake of ACP. Two specific questions guided the synthesis:
What are the barriers and enablers to uptake of ACP in general practice?
What initiatives have been used to increase uptake of ACP in general practice?
Method
Search strategy
Database searches were undertaken from inception to July 2019 across Ovid Medline, Cumulative Index to Nursing and Allied Health Literature, Scopus, ProQuest and Cochrane databases. The selected databases are considered the most useful to identify peer-reviewed articles relating to this topic. The search strategy was developed for Ovid Medline (see table 1) and was modified to suit the language requirements of other databases. It included subject headings and free text words. During the searches, wildcards and * truncation were used to ensure broad inclusion of related search terms. Boolean operators ‘OR’ and ‘AND’ were also used. Proximity searching was not used. The search strategy was developed with the expert assistance of a medical librarian. Search terms were determined with the intent of capturing a broad representation of the ACP literature, and then refined to focus on the specific context of interest, thus minimising the risk of incomplete data. Search terms included concepts of ACP, advance care directive or advance health directive or living will; AND concepts of knowledge, attitudes, practice AND concepts of behaviour, engagement, barriers, participation among both consumers, and healthcare providers AND general practice OR family practice or patient-centred medical homes. A review protocol was submitted to PROSPERO available at http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018088838.
Table 1.
Example of search strategy—Ovid Medline Search history
| # | Searches |
| 1 | Advance Care Planning/ |
| 2 | ((advance* adj3 (plan* or directive*)) or living will*) tw, kw. |
| 3 | 1 or 2 |
| 4 | Knowledge/ or Health Knowledge, Attitudes, Practice/ |
| 5 | (concept* or attitude* or belief* or practice* or experience* or knowledg*or uptake* or utilis* or implement*) tw, kf. |
| 6 | 4 or 5 |
| 7 | (Consumer Behavior or Consumer Participation or Consumer Health Information or consumer engag* or decision making or consumer uptake or barriers to uptake or consumer concepts or Primary health care* or general practice or family practice or GP or general practitioner or patient centred medical home or patient-centred medical home or health care home or practice nurse or community nurse) tw, kw. |
| 8 | Physicians, Family/ or General Practitioners/ or Family Practice/ |
| 9 | Primary Health Care/ |
| 10 | *Health Personnel/ |
| 11 | Consumer Behavior/ |
| 12 | Consumer Health Information/ |
| 13 | 7 or 8 or 9 or 10 or 11 or 12 |
| 14 | 3 and 6 and 13 |
Patient and public involvement
Patients and public involvement was not sought in the design or undertaking of this review.
Inclusion/exclusion criteria
Determining the most appropriate search terms and inclusion/exclusion criteria required consideration of nomenclature. Nationally and internationally, consistent terminology about research studies in ACP is lacking. It is variously characterised as ACP, an advance (care or health) directive or living will. The search strategy included all derivations.
To identify literature relating to low uptake of ACP required consideration of consumer and provider knowledge, attitudes and practices with regard to ACP. This included studies considering consumer and provider engagement, behaviour and participation.
The review was bound within general practice. General practice in Australia is described by one peak body as an entity that ‘provides person centred, continuing, comprehensive and coordinated whole person health care to individuals and families in their communities’.17 It was understood from preliminary searches that a substantial body of research about ACP had been generated in countries other than Australia, and within this, there were nuanced differences about how ‘general practice’ was described.
It was determined not to include or exclude studies based on geographical limits but to filter results based on the description of the healthcare provider and the setting. Studies from countries describing general practice, family medicine and primary care services sufficiently comparable to the definition of Australian general practice were included. Examples included Canadian family practice and Belgian family medicine each understood to be similar to Australian general practice. In the US general practice differed around type of organisational structure, professional roles and responsibilities, and service descriptors; however, US primary care clinics and family practice outpatient clinics have been described as analogous with Australian general practice.18
A further consideration and inclusion was the ‘patient centred medical home’ or ‘health care home’. This emerging model of primary care was thought to be changing the structure of general practice, both in Australia and internationally, and consideration of ACP in this context warranted inclusion in the review.
Studies were included if they met the following criteria: written in English, published in a peer-reviewed journal, primary care research with scope limited to general practice, and adult participants. Studies that focused on acute care, inpatient care, aged care facilities, palliative care or clinical management at end of life were considered out of scope and excluded from the review. Other exclusion criteria included: legal focus, mental health focus or issues for minority groups.
Search results
An online search was conducted in July 2019. A total of 6703 online studies were identified as potentially relevant. At the completion of the database searches identified studies were catalogued in Endnote. Duplicate studies were removed and the remaining 4883 studies were screened by title for inclusion. Of these, 589 studies were considered potentially relevant and screened by abstract. Five hundred and thirty-seven studies were excluded by abstract and a further 18 studies were identified through targeted citation and reference list review resulting in a total of 70 studies for full text review. Year of publication ranged from 1991 to 2019 and represented research from nine countries. The earliest publications came from the USA where the antecedents of ACP originated, and the majority of publications also originated in the USA.
Study selection process
The search process was conducted by one researcher. Studies were reviewed and catalogued by the primary researcher using a template to identify key features of interest relevant to review. The template documented:
Type of study.
Year and country of publication.
Study setting.
Barriers identified,
Enablers identified.
Initiatives identified.
Outcomes/recommendations.
A barrier was understood to be ‘a circumstance or obstacle that keeps people or things apart or prevents communication or progress’.19 An enabler was understood as a moderating factor to be defined as ‘to make able; give power, means, competence, or ability to’.20 An initiative or intervention was defined as ‘a specified strategy or set of strategies designed to change the knowledge, perceptions, skills, and/or behavior of individuals, groups, or organizations, with the goal of improving health outcomes’,21 and specifically in this case ACP uptake. Studies were accepted when the primary focus of the study included all key search terms and aligned with inclusion and exclusion criteria. The resulting list of studies meeting the inclusion/exclusion criteria was subject to a quality review performed by two researchers.
Quality
The heterogeneity of approaches found within the search literature made it difficult to apply a standardised quality framework; however, the Joanna Briggs Institute provided a suite of critical appraisal tools considered suitable for quality assessment covering a range of methodological approaches.
As noted, a single researcher undertook the initial screening of search results with strict adherence to review protocol and inclusion and exclusion criteria.
Two researchers then independently reviewed all shortlisted papers using Joanna Briggs Critical Appraisal Checklists.22–26 Tools used included randomised control trial; systematic review and meta-analysis; cohort studies; analytical cross sectional studies; qualitative studies and quasi-experimental studies.
Results were compared and when reviewer findings differed, discussion ensued to reach a consensus understanding and search results were adjusted accordingly. This process was considered important to reduce reviewer bias. Following completion of this process, all studies agreed by both researchers were included in subsequent review and critical interpretive synthesis. The quality assessment resulted in the exclusion of 16 studies. There were quality concerns with three papers and on closer analysis 13 studies were identified as lacking relevance. At the completion of the quality review, a total of 54 studies were included in the critical interpretive synthesis. Results comprised of 8 systematic reviews, 8 randomised control trials, 14 analytical cross section studies, 3 cohort studies, 9 quasi-experimental studies and 12 qualitative studies.
Figure 1 outlines the Preferred Reporting Items for Systematic Reviews and Meta-Analyses framework used to summarise the search process.27
Figure 1.
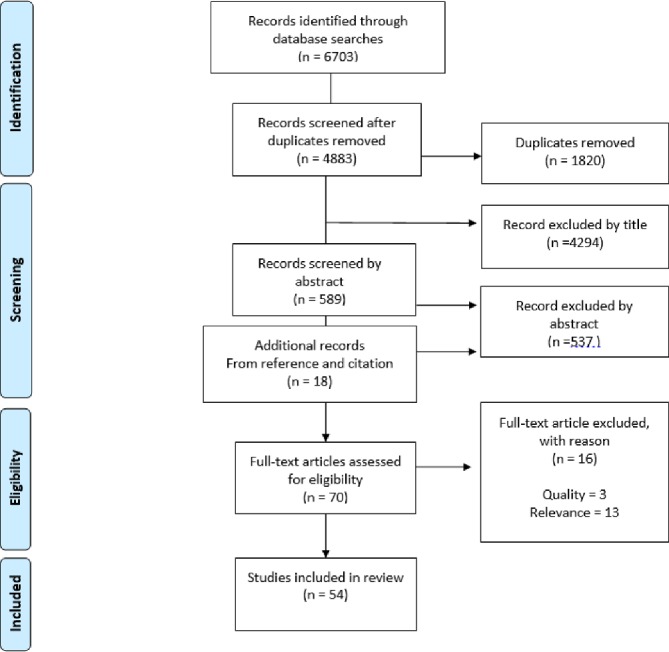
PRISMA flow diagram.27. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Conceptual framework
A socioecological conceptual framework was used to organise the literature. This framework has been frequently applied in health promotion research over the last years28 and has been found to have applicability to complex health systems.29 30 The multiple factors that influence health are attributable to levels of influence, often depicted as nested concentric circles representing contextual layers of increasing scope. McCormack (2017) applied this framework in considering the problem of low health literacy and patient engagement in health systems, presenting an argument in support of this theoretical approach. In a general practice setting, individuals as patients bring their own understanding and attitudes when engaging with providers to seek care. The provider is operating within their own frame of reference and within a broader system supported by processes and models of care. Figure 2, adapted from McCormack et al,29 outlines levels of influence depicted from a socioecological perspective appropriate to general practice as the functional system of interest.
Figure 2.
Socioecological perspective for general practice. Adapted from McCormack et al.29
Each study was reviewed and the barriers, enablers, stated aim and methodology was mapped into one or more of the contextual levels of influence across a socioecological perspective.
A decision matrix (online supplementary file 1) was developed to guide a consistent approach to categorisation of studies across the four contextual levels of influence. A summary of the distribution of studies across socioecological contextual levels of influence is presented in online supplementary file 2.
bmjopen-2019-030275supp001.pdf (49.5KB, pdf)
bmjopen-2019-030275supp002.pdf (100.7KB, pdf)
Results
Synthesising the diverse and disaggregated body of ACP literature was challenging. There was a lack of coherence in literature with regard to the nature and causality of barriers and enablers. Some studies inherently described barriers and enablers as linked and binary, for example—lack of knowledge as a barrier was frequently linked to provision of education as an enabler. Other studies described factors independent of each other in non-binary relationships. Cataloguing these variations was achieved by interpreting the barriers and enablers independently. This resulted in instances of apparent duplication but remained important to capture at each level and is explored further in the discussion. The results of the review are outlined in the following four sections:
Critical synthesis of systematic reviews.
Barriers to ACP in general practice.
Enablers of ACP in general practice.
Initiatives/strategies to increase ACP in general practice.
Critical synthesis of systematic reviews
Eight systematic reviews with relevance to ACP in general practice were included, generated from four countries and spanning publication dates from 2007 to 2019. In general, the reviews were quite heterogeneous with one focused on barriers and enablers to uptake of ACP in general practice,31 one focused on the attitudes of the public and GPs to ACP,32 and one focused on the effect of structured ACP communication tools.33 Four studies looked at the efficacy of a range of interventions,34–37 and the remaining study was a narrative review of other systematic reviews.38
In the 2009 review of reviews, Tamayo-Velasquez et al reported that most studies, though heterogeneous in approach, had reached very similar conclusions,38 and subsequent reviews have continued to have largely consistent findings. Common barriers were identified and attributed to lack of patient and provider knowledge; lack of provider skills and experience; patient, family and provider attitudes, and system issues related to time pressure, documentation challenges and mechanisms of information sharing.
A common theme was noted with a number of reviews categorising data across a combination of patient level, provider level and system level findings.31 32 34 One study,34 reported interventions at a patient and physician level, and another considered categories of individual autonomy, versus personal circumstance or health system effects.32 These levels were consistent with contextual levels of influence when viewed from a socioecological perspective, though none of the reviews explicitly linked the described levels to a theory, model or framework.
It was important to observe the described levels in order to understand if interventions described in the literature were targeting specific levels, to achieve their effect. Some studies reported targeting interventions across multiple levels, for example, patient, provider and system, whereas others were understood to be applying multiple interventions within a single level for example, mail outs, phone calls, websites aimed at the individual, which was a nuanced but important difference.
As suggested by Weiner et al,30 interventions where multiple level approaches were applied were more effective than single intervention approaches.34–37 When studies investigated the outcome of combinations of actions in achieving an effect, provision of information alone did not increase ACP completion rates above the background community level.34 The least successful interventions were mail outs without reinforcement, and one review reported inconsistent findings regarding all types of interventions.35 The most successful interventions exerted influence over multiple levels and involved direct and iterative patient–healthcare provider interaction over multiple visits. Studies reached similar conclusions in so far as person-to-person interaction was evidenced as a strong enabler when compared with more static approaches.34 36
There was some consensus across reviews about the need to better understand barriers to and enablers of ACP.31 34 37 Some reviews went further to suggest interventions needed to be based on these understandings.23 24 31 31 31 32 32 32 37 There was general consensus more research was required.
Oczkowski et al 33 challenged the quality of available evidence in considering efficacy of documented approaches to ACP in primary care,33 describing it as low to very low in quality, echoing the findings of an earlier 2010 review.35
Analysis of the systematic reviews alone did not sufficiently answer the current review questions. A number of limitations diminished the value of review findings. The inclusion and exclusion criteria of individual reviews were very different, making direct comparison problematic. A number of studies included in the reviews were sourced from non-general practice contexts making more generalised findings not directly relevant.34–36 These reviews were conditionally included only where general practice findings were explicitly reported as discreet categories.
A number of papers referenced in one or more systematic reviews were also included for individual consideration in the current review because the questions posed were different to the reported aims of the systematic reviews in which the studies originally appeared. Table 2 provides a brief overview of the reported findings of the systematic reviews.
Table 2.
Summary of systematic reviews
| First author | Ref | Year | Country | Aim | Studies | Summary of outcomes | Recommendations |
| De Vleminck et al | 31 | 2013 | Belgium | To identify the perceived factors hindering or facilitating General Practitioners (GP) in engaging in ACP with their patients. | 16 | A range of barriers and facilitators were identified and attributed to GP characteristics, perceived patient characteristics and health system characteristics. | Understanding barriers and facilitators, and targeting GP and health system related barriers was considered important for development of interventions aimed at facilitating ACP in general practice. |
| Durbin et al | 35 | 2010 | USA | To systematically analyse evidence about the outcome and percent of newly completed AD, focusing on effectiveness of (1) types of educational interventions versus controls; and (2) one educational intervention over another. | 16 | After examining various combinations of intervention including single approaches, combined approaches and multiple combinations the authors determined the evidence base for effectiveness of specific interventions was weak, with the exception that combined approaches were more effective than single approaches in increasing the percentage of newly completed advance directives. | More research is needed to address the low number of studies looking at specific interventions. |
| Jezewski et al | 36 | 2007 | USA | To synthesise the state of the science regarding effectiveness of interventions to increase AD completion rates. | 25 | Interventions with repeated multiple contacts or stimuli were found to be most effective. Not all intervention designs may be effective across the life span and that ‘a single approach’ will likely not be effective because the same approach will probably not work for all people. |
A knowledgeable person who can answer questions should be an integral component of any intervention. Creative interventions need to be developed that are matched to the individual’s needs at a particular point in time. |
| Oczkowski et al | 33 | 2016 | USA | To determine the effect of structured communication tools for end-of-life decision making on completion of ACP. | 67 | Low quality evidence that structured communication tools assist with end-of-life decision making resulting in uncertainty about the magnitude of the effect. | Given the heterogeneity of populations, interventions and effects, more work is needed to guide the selection, adaptation and tailored implementation of tools in local settings and contexts. |
| Ramsaroop | 34 | 2007 | USA | To systematically review studies designed to increase advance directive completion in the primary care setting. | 18 | There was increased efficacy in achieving advance directive completion with direct patient to health professional contact with this being a consistent finding among studies. The more effective approaches used iterative interactions over multiple visits. Passive education of patients using written materials alone was relatively ineffective Uptake remains low. |
Barriers to completion of advance directives warrant attention in future intervention studies. |
| Sharp et al | 32 | 2013 | UK | To investigate attitudes of the public and healthcare professionals to ACP discussions with frail older people. | 26 | Many frail elderly people would welcome the opportunity to discuss ACP but a significant minority would not. There was no consensus for optimal timing of the conversation. Reluctance of family members to engage is a significant barrier. |
Categorised across three levels: health system issues —health providers require support and training to initiate discussions; individual autonomy—raised a number of questions about how to achieve this (inter)personal circumstance—raised a number of questions about how to achieve this |
| Solis | 37 | 2018 | USA | To evaluate strategies used in primary care settings to initiate ACP leading to completion of AD. | 12 | The use of multipronged approaches was most successful for initiating ACP discussion. Effective interventions included patient education materials, computer generated triggers for providers and multidisciplinary team involvement. | There is a gap in empirical knowledge and this opens an opportunity for more research. Providers should consider increasing ACP discussions with patients and create opportunities to do so more systematically. |
| Tamayo-Velazquez et al | 38 | 2009 | Spain | To identify, appraise and synthesise the results of systematic reviews of the literature that examine effectiveness of interventions to increase advance directive completion rate. | 7 | Determined that each of the systematic reviews reached very similar conclusions. Passive informative material in isolation does not significantly increase advance directive completion rates. Effectiveness is increased over multiple visits where patients are provided opportunity to interact with an expert in the field and are afforded an individual who will answer any queries. |
Further research is required to identify new strategies to increase ACP completion rates. |
ACP, advance care planning; AD, Advance Directive; GP, General Practitioner.
Barriers to ACP in general practice
A barrier is understood in the general practice context as something that limits uptake of ACP. A barrier can have effect at an individual level, at an interpersonal level, at a provider level or a system level. The same barrier can also occur across a number of levels. Table 3 catalogues barriers identified in the literature across four socioecological levels of influence.
Table 3.
Key barriers to ACP sorted by socioecological levels of influence and ranked by frequency
| Level identified | Barrier | No of studies | References |
| Individual level | Lack of (consumer) knowledge about ACP | 15 | 14 39 44–46 49 54 56 57 59 62 66 72 79 82 |
| Attitudes—perceived irrelevance | 7 | 13 14 39 40 44 50 76 | |
| Trust/questions of efficacy | 4 | 40 41 44 57 | |
| Denial/emotions/reluctance | 10 | 14 32 39 40 44 50 54 56 57 72 | |
| Interpersonal level | Role ambiguity—GP expectation patient will initiate discussion about ACP | 7 | 13 46 51 56 58 62 83 |
| Role ambiguity—patient expectation GP will initiate discussion about ACP | 5 | 41 42 49–51 83 | |
| GP—patient relationship | 5 | 44 49 55 57 62 | |
| Concern with family relationships | 6 | 13 14 32 39 44 74 | |
| Preference for informal discussion with family | 1 | 13 | |
| Provider level | Lack of (GP) knowledge/skills/confidence | 18 | 14 31 44 46 49 53–56 58–60 63 69 74 77–79 |
| Lack of time | 12 | 14 39 46 53–55 58 61 66 74 76 79 | |
| Misc concerns including legal uncertainty, prognosis, best time | 9 | 54 55 60 61 68 70 75 78 83 | |
| Doubts about efficacy of ACP | 3 | 44 58 | |
| System level | Lack of linkages and mechanism for sharing ACP | 5 | 31 44 54 58 60 80 |
| Lack of funding mechanisms | 2 | 56 60 | |
| Lack of standard templates, tools, documents, IT systems | 6 | 44 45 53 57–59 | |
| Accountability | 1 | 46 |
ACP, advance care planning; IT, Information technology.
Barriers at an individual level
When considering barriers to ACP in general practice from an individual perspective, there were very few general practice studies directly involving patients.14 39–43 A few studies described patient experience by proxy through opinions obtained from GPs. The most common barrier described at the individual level, largely attributed by clinicians, was patient lack of knowledge and awareness about ACP, including lack of knowledge about clinical considerations at end of life.44
Attitudes of individuals about ACP were reported to vary widely. Studies reported the perceived irrelevance of ACP was a barrier, with the relevance of ACP described with ambivalence when associated with an existing state of wellness or absence of terminal diagnoses.13 14
Further, an identified lack of trust in the health system with reported concern that an ACP would in some way limit care or negatively impact the individual was reported.40 The concepts of poor literacy,45 and poor health literacy,46 as contributing factors were also noted.
Barriers at an interpersonal level
Barriers identified across the interpersonal level involved the individual in relation with others. Very few general practice studies focused specifically on this interpersonal aspect.47 48 Many studies described confusion and role ambiguity about initiation of ACP. When considering the doctor–patient relationship a number of studies reported a difference in expectation about whose role it was to initiate the ACP discussion.
Described as a lack of role clarity, this uncertainty in the doctor–patient relationship was understood as a barrier to ACP.41 42 49–52 A number of studies cited GP concerns about initiating the ACP discussion, not doing so in order to avoid being a source of anxiety or loss of hope. Concern about jeopardising the doctor–patient relationship was a recurrent theme described by a number of studies.
Patient expectation that GPs should initiate ACP discussions,41 42 51 was understood as a barrier when the GP did not initiate the discussion. Studies found patients were willing to discuss ACP when asked. This contrasted with other findings that discussing ACP and end of life preferences was potentially distressing for some individuals who might prefer to avoid the topic as unpalatable or conversely trust in an absolute deity being cited as reason to not need ACP.39
One study explicitly studied interpersonal barriers,39 finding a range of relationship concerns. Poor family relationships were reported as a barrier for some. Not wanting family involved, or not wanting to burden family members was also a consideration.14 Difficulty conversing with family about ACP and the need for assistance to achieve these conversations was raised. Conversely, studies also identified family members not willing to support GPs in discussion about ACP with patients.32 44
Patient preference for informality, choosing to discuss end of life matters privately within the family was more common in more educated people and resulted in lack of formal documentation in the medical record.13
Barriers at a provider level
A number of studies focused on barriers to ACP at a provider level, with largely consistent findings, echoing those of the previously reported systematic reviews. GP lack of knowledge, skills and confidence in relation to ACP were most frequently cited. See table 3. Lack of GP knowledge was detailed in a number of studies variously outlining knowledge gaps relating to patient competence, legal considerations, documentation and processes.53 Time pressure to keep up with busy consultation schedules limited GP’s ability and willingness to initiate time consuming ACP discussions during consultations.
GP reluctance to engage patients in ACP discussions due to the complexity of diagnoses,54 55 doubting an individual’s ability to comprehend the issues involved was identified. GPs questioned the efficacy of ACP particularly about application at end of life, and one study described paternalistic views including a sense that the GP knew what the patient would prefer, so ACP was unnecessary.56
Barriers at a system level
System level barriers to ACP were commonly considered in the available literature. Common system level concerns included, for example, the suitability of ACP templates45 57; or uncertainty about the efficacy of one information kit versus another.53 Lack of consensus about what information was required in a written ACP including the relative importance of value statements, contributed to a lack of clarity.45 Difficulties associated with poor system linkages resulting in lack of availability of ACP at point of care were highlighted.58 Barriers associated with uptake of electronic medical record reminder prompts were identified.59 Context specific issues were described, for example, lack of suitable funding mechanisms was problematic in some jurisdictions.56 60 One study suggested that because there was no performance monitoring of providers’ ACP activity it was not important. If it was not measured at a system level—it was thought to be not important to the system outcomes.46 This lack of a reporting for providers was described as a barrier as there was no incentive to drive ACP activity.46
A recurrent barrier to ACP across the levels of influence was a lack of shared understanding by providers and patients about whose roles is was to initiate ACP discussions and when ACP was best initiated. Studies report conflicting views. A study by Tierney et al 51 sought to explore the perceived barrier about who (patient or provider) should initiate an ACP discussion identifying many arguments in support of broad ranging views.51 The following studies highlight widely contrasting views.
In a study reported by Emanuel et al 50 lack of physician initiative was the most frequently cited barrier to ACP according to patients.50 Physician reluctance to initiate the ACP discussion was compounded by patient expectation that it was the physician’s responsibility to do so,50 and this is somewhat consistent with findings in a (2015) UK study where 60% of respondents would only talk about ACP if the topic was raised with them.41 In other instances, patients were reported to have raised the issue themselves.61 A Canadian study found patients preferred to initiate the discussion themselves and often did so with family or friends in preference to their family physician.42
In contrast, Pfeifer et al 62 found physicians accepted responsibility to initiate discussions but retained a level of concern about the right time to do so,62 and this despite evidence that counselling by a clinician was the best catalyst for the completion of advance directives.59 In a UK study, for a patient, the most important predictor of having completed an ACP was having been asked.41 GP reported barriers to initiating ACP discussions included concern for causing the patient distress or triggering unwanted negative responses61 62; however, at least one study demonstrated significant improvement in patient satisfaction in primary care consultations when physicians initiated discussion about advance care directives. De Vleminck et al found GPs deliberated about actively initiating versus passively waiting to discuss ACP and this varied qualitatively according to GP knowledge, experience and communication skills.63
Other studies suggested there was a need to encourage more health professional involvement in ACP.56 Nurse care coordinators have been found to be well positioned to leverage opportunities to discuss ACP with patients in primary care,14 51 64 but Fletcher et al 58 explored the role of nurses and identified the majority of nurse participants looked to the doctor for leadership in ACP (p426) and pointed to lack of role clarity in this regard across providers generally.58
Studies described uncertainty about optimal timing for initiating ACP discussions.62 An emerging consensus was ACP discussion should occur in the community—prior to hospitalisation and before critical situations.48 60 Concepts about timing varied from routine inclusion of ACP discussion for all patients65; when illness became predominant65; to passively waiting for the patient to raise the topic directly or listening for patient triggers during consultation as a signal of readiness to participate in conversation.63
Barriers were often not considered in relation to their effect on each other. Some barriers were specific and applicable to a particular study modality. For example—studies requiring patients to receive an electronic message relied on the person being able to access the technology. An inability to do so would be reported as a barrier, the barrier being specific and limited to the mechanics of the particular intervention. Other barriers were more complex and multifaceted. In general, lack of patient and provider understanding of roles, lack of knowledge; lack of provider skills and experience; patient, family and provider attitudes, and system issues related to time pressure, documentation challenges and mechanisms of information sharing.
Enablers for ACP in general practice
An enabler was understood as a moderating factor defined as ‘to make able; give power, means, competence, or ability to’.19 An enabler can have effect at an individual level, at an interpersonal level, at a provider level or a system level. The same enabler can also occur across a number of levels. Table 4 provides a summary of literature analysed to identify enablers and locate their influence into one or more of the four levels across the socioecological perspective.
Table 4.
Key enablers mapped to socioecological levels of influence and frequency reported
| Level identified | Enabler | No of studies | References |
| Individual level | Demographic likelihood (increased age) | 3 | 41 66 67 |
| Education and public awareness | 7 | 31 43 56 67–70 | |
| Stage of change—readiness | 6 | 15 34 39 43 47 71 | |
| Timing | 6 | 13 31 61 65 67 69 | |
| Interpersonal level | Doctor–patient relationship (strength, length of, trust, familiarity) | 10 | 14 15 42 48 49 61–64 67 |
| Nurse–patient relationship | 5 | 14 64 72–74 | |
| Conversation and deliberation | 5 | 14 43 57 64 65 | |
| Group interaction | 2 | 66 73 | |
| Previous experience with ACP | 4 | 15 31 47 58 | |
| Provider level | GP and practice nurse education and communication training | 8 | 14 60 65 69 74–77 |
| GP or practice nurse initiating the ACP discussion | 6 | 14 46 50 52 63 74 | |
| GP with philosophical agreement to ACP | 8 | 40 42 43 49 55 57 58 63 | |
| GP engagement in team approach | 3 | 60 64 66 | |
| System level | IT systems—portals, prompts, decision aids | 8 | 44 46 54 59 63 64 71 80 |
| Templates | 6 | 57 63 67 70 75 78 | |
| Business as usual processes and protocols | 11 | 13 39 46 50 51 54 56 65 67 69 76 | |
| Models of care—group appointments, nurse led clinics, ACP facilitators | 10 | 14 49 60 64 66 72–74 76 79 |
ACP, advance care planning.
Enablers at an individual level
Studies explicitly outlining ACP enablers at an individual level were not common in the general practice literature. Understanding demographic profiles was suggested as an enabler by a number of studies in which people of an older age group were reported as most likely to engage in ACP discussions,41 66 67 and expanded by one study which reported people of all ages desired ACP discussion.50 Studies reported individuals initiating ACP discussion helped overcome GP reluctance to engage in the topic,63 and suggested that individuals should be encouraged to raise the subject68; however, the concept of individual autonomy and empowerment was largely silent in general practice literature.
Studies reported people with higher levels of education were more likely to have engaged in ACP,13 67 and tailoring ACP discussion and resources to an individual’s literacy level was effective.45 A number of studies reported the need for individuals to access education through public awareness raising activities.31 56 69 One randomised control trial (RCT) tested approaches to patient education and reported mixed results and ongoing challenges so while potentially useful, was not a panacea.70
An alternative approach described an individual’s readiness to engage in ACP viewed from the trans- theoretical stages of change approach.39 71 Described as an iterative process ACP was framed as a behaviour change process which involved the individual through discrete steps.34 43 Determining the individual’s readiness to engage prior to initiating ACP discussions was described as an important step.39 47 71
Studies considered if there was an optimal time to initiate ACP discussions referring to time in relation to disease timelines as opposed to chronological time—for example, during first consultation, at diagnosis, in advance disease stages or at end of life. A range of findings included at first appointment,67 while individuals were healthy,13 planting the seed for future discussions,61 and when chronically or terminally ill.69 In a binary relation, the anxiety of not knowing the best timing was a barrier so understanding the best timing would by contrast, provide clarity and be enabling.
Enablers at an interpersonal level
Studies explicitly focused on ACP enablers at an interpersonal level were least common in the general practice literature though the importance of relational aspects of ACP was evident. The majority of studies identifying interpersonal enablers referred specifically to the importance of the doctor–patient relationship. Enabling factors within this relationship were longevity of the association and high level of trust.14 42 48 49 61 62 64 67 72 A more recent trend is evidenced in the literature with five studies published since 2016 detailing the role of nurse–patient communication as an enabling factor in uptake of ACP. Other studies found individuals with lived experience of caring for someone else at end of life, or experience with ACP had increased uptake of ACP,47 58 and this also included GPs with personal experience of ACP.31 Two studies reported the process of discussion and reflection of values over multiple visits as enabling ACP to be most effective,14 34 supported by similar findings from others.43 57 64 65
Other interpersonal enablers involved participation in facilitated discussions in group settings where group dynamics and the ability to socialise were identified as effective levers.66 73 One study reported the value of socialisation around ACP discussion in group settings,66 and another described value in ‘learning from the experience and perspectives of others’ (p127).73
Enablers at a provider level
A number of suggested enablers at the provider level were inter-related. Strong communication skills, confidence, knowledge and positive GP attitudes were described as enablers and achieving this was variously described through provider education and training, skills development, deliberative discussion and the clarification of GP attitudes and roles. The emerging role of the broader healthcare team, with a particular focus on extended roles of the practice nurse was evident in most recent publications.14 64 72 74
A number of studies reported recommendations in support of provider training. Within these, the focus of studies varied with training recommendations ranging from the specific to the broad including legal considerations,75 professional mentorship and observed practice for providers engaged in ACP,46 60 communication skill training65 76 and professional development training about ACP.69 One study reported the efficacy of provider training which was reported to increase GP knowledge and confidence.77 Positive GP attitude to ACP was shown to increased engagement in ACP discussion.46 50 52 63
Enablers at a system level
Many studies included in the review were focused on describing and/or testing enablers at a system level. Among these, the most frequent recommendation was establishing various business as usual approaches to ACP seeking to normalise ACP in practice. Concepts ranged from a general theme,46 49 to including and specifically targeting all patients of a certain age13; to others describing monthly purpose specific clinics66; reminders in the medical record,59 and provision of ACP resources to patients and providers through portals in an automated way.54
Systematic prompting of patients and providers with technology reminders and information was found to have some effect. Studies explored timing the prompts preconsultation with mail out,46 during consultations as screen prompts for providers,59 and simultaneous prompts for both consumer and provider.46 68 Studies reported variable degrees of success.46 59 64 68 and those studies implementing a combination of approaches reported greater uptake of ACP than single step processes.68
The importance of ACP resources including templates and standardised documentation was a recurrent theme.61 A number of studies recommended the need for standardised and improved ACP templates and tools to support discussion in general practice,57 with testing and development of tools and fit for purpose approaches for target populations. This included one study with findings about efficacy of an ACP template designed for people with low health literacy,45 another study developed and tested a tool to assess stage of change71 and a study that found personalised ACPs increased uptake.70
Since 1992 when researchers noted the majority of participating physicians had never seen, used or discussed ACP with any patient,69 there have been many published studies internationally indicating growing physician support for ACP. More recently, most GPs felt ACP was important,61 citing ACP attributes as safe guarding patient autonomy and conferring peace of mind for the individual and the family.78 Positive GP attitudes are a known enabler. Practice nurses also reported ACP as beneficial to patients and understood a potential role for nurses in this context.14 60 Positive attitudes have also been reported in the community with one study describing a majority of patients and healthy people considering ACP as ‘meaningful and important’ (p1583).40
Leveraging enablers alone was not shown to be sufficient to systematically improve ACP. Many enablers were understood to share direct binary relationships with barriers and were described in the context of overcoming particular barriers. For example, if the barrier was lack of knowledge, the enabler was provision of education. If the barrier was lack of knowledge combined with an entrenched or cynical attitude, education alone would be ineffective. In considering the range of barriers, a number of studies explored a range of complex interventions and alternative models of care with a focus on changes to practice processes that enabled alternative ways of working, for example, by role delineation and delegation of responsibility. Alternative models of care were found to be complex enablers with implications across multiple levels of socioecological perspective. Examples included exploring attitudes to nurse led clinics,60 conducting group appointments66 73 79 and trialling ACP facilitators in practice.49
This section has catalogued a number of known enablers described across multiple contexts and each nuanced to the study environment. An overall observation in considering the body of literature was the need for flexible and place-based responsiveness in the design of interventions. Not understanding the range of barriers at play was understood to limit effectiveness of enablers. One size did not fit all and a single approach was unlikely to work for all.36
Initiatives to increase ACP in general practice
This section synthesises current knowledge from intervention studies with a summary provided in online supplementary file 3. Fourteen general practice intervention studies were identified in the review as outlined in online supplementary file 3. Of these, 12 studies were conducted in the USA, 1 in Australia and 1 study was reported from Belgium. Publications spanned a period from 1996 to 2019 with 6 of the 14 studies published after 2016. The studies consisted of six randomised control trials, two mixed-methods studies, a comparison study, a cross-sectional survey, a qualitative study and three studies described as complex interventions.
bmjopen-2019-030275supp003.pdf (126.3KB, pdf)
Intervention studies were only included if the research was undertaken in general practice. Interventions ranged in complexity from simple initiatives focused on one level of influence, to complex multilevel undertakings.
Each intervention aimed to increase ACP and the approaches used were different across the studies. A recent Canadian study (2018) found it was not clear that the assembled body of research had explicitly considered the known barriers and enablers when framing proposed interventions.44 Two exceptions were found. A study by Miller et al 14 explicitly described intervention activities based on and intending to overcome known barriers14 as did an earlier study by De Vleminck et al.72
Early research involved interventions with a common focus on prompting and reminding. Patients were prompted by mail outs,46 70 reminder letters46 and waiting room questionnaires.67 Physicians were prompted with scripts and various systems to trigger discussion during consultations.46 51 68 72 The efficacy of combining various combinations of prompting and reminding was explored in a three arm blinded randomised control trial which sought to test the efficacy of a combination of two simple interventions. Patients with upcoming appointments receiving a mail out of patient information and this was combined with the physician receiving a computer-generated reminder during consultation. Reported findings showed a substantial increase in completed ACPs in one of the three study arms supporting the efficacy of a mail out supported by a physician prompt, with no change between the control and the physician only prompt arms.68 Subsequent studies commonly included one or more prompts as components of more complex interventions. Another mixed-methods study compared the efficacy of two different conversation guides—based on a determination of the required literacy reading levels contained within the two documents. This was measured by patient and provider experience of use.53
Another early study by Tierney et al 51 hypothesised physicians feared initiating ACP discussion as it would cause a reduction in patient satisfaction with care. Tierney’s study used a physician computer prompt during consultation followed by a postconsultation patient satisfaction survey. Study findings reported patients were more satisfied with their provider when ACP was discussed, so the physician’s fears were found to be baseless.51
Weiner et al’s contention that ‘interventions that target determinants at multiple levels and mutually reinforce each other are likely to produce larger and longer lasting effects than interventions that target determinants at only one level’ (p34),30 remains to be seen. Of the one qualitative study14 and three complex interventions,46 72 73 only one study systematically and explicitly sought to address barriers and leverage enablers across multiple levels of influence.72 In this study, by understanding the key barriers and enablers, De Vleminck et al determined a structured response which identified four key components underpinning successful ACP interventions.72 The first key component was described as the involvement of trained and experienced facilitators. This approach was a common feature across complex studies, though the facilitation role varied with involvement of one or more of the patient’s physician, social worker, registered nurse or nurse practitioner. Face-to-face facilitation was a known enabler with influence at the interpersonal level. All but two interventions,54 80 involved discussion with knowledgeable health professionals. This interpersonal influence was further leveraged by Holland et al 64 who required individuals to discuss ACP with their families, prior to a second appointment; by Lum et al 73 who conducted group appointments to harness the dynamic interaction between participants in facilitated sessions. The importance of skilled facilitation was also noted by Miller et al 14 who provided training to the providers to enhance their facilitation skills.
The second key component identified in De Vleminck’s (2016) complex intervention, was a selection process to identify eligible patients, considered to be a key underpinning component of ACP interventions. The patient characteristics cited for inclusion on an ACP invitation register in De Vleminck’s study were those with poor health and poor prognosis.72 Demographic targeting of older people was identified as an enabler and advancing patient age was a primary consideration for recruitment in all but three interventions, ranging from 50 years for those with known chronic disease,51 68 to 65 years,73 80 70 years68 and 75 years.51 Only one study included all adults older than 21 years.14 67 Miller was unique in recruiting both opportunistically and by use of the surprise question—‘would I be surprised if this patient were to die in the next twelve months?’ If the answer was no, ACP discussion was considered indicated.14
The third key component suggested by De Vleminck was a structured and patient-centred ACP discussion which was addressed in the 2016 study design by development of a GP prompt, a conversation guide and template for ACP. Similarly, Duffield and Podzamsky67 employed waiting room questionnaires; Wissow et al 46 prepared physician scripts; Pearlman et al 70 employed a conversation guide as did Lum et al 73. Holland et al 64 sought to evaluate the feasibility of four different tools. Across all studies, a range of tools were suggested as suitable; however, the key point was the value of a structured approach,64 70 72 73 as a number of tools were reported as moderately effective. Miller et al 14 used an ACP workbook and an advance directive template to guide the discussion.14
The fourth key component cited by De Vleminck et al was the opportunity to complete ACP documents.72 The provision of an ACP form or template was evident in the majority of interventions.
The majority of intervention studies had a mitigating effect on one or more known barriers at various levels of influence, but no study was seen to mitigate the influence of all barriers, or leverage all enablers. There were examples of studies testing approaches in contexts in which other known barriers might be predictably problematic, but which were not factored into the proposed interventions. For example, testing a GP reminder prompt in the middle of a busy consultation without quarantining time to respond to the prompt, was not found to be an effective mechanism for change.68 Whereas some interventions had some impact and demonstrated a level of efficacy, to create a synergistic initiative required consideration of all key barriers operating at each level, with a design structured to maximise outcome. The findings of De Vleminck intervention are yet to be reported.72 The qualitative study by Miller et al 14 arguably addressed all four of De Vleminck’s key intervention components but reported outcomes as a pilot study suggesting further research was required.14
In keeping with complex approaches, a retrospective analysis by Dipko et al 66 explored the efficacy of a single face-to-face education session with a social worker in a primary care clinic versus a combination of multiple face-to-face sessions or participation in group education in an elderly population.66 In this study, the ACP completion rate was positively associated with participation in group education, and higher still in multiple face-to-face sessions. From an efficiency perspective, the study concluded group sessions provided the most efficacy with regard to time, resources and outcomes.66
A more recent study73 tested the feasibility of group medical visits in a patient-centred medical home environment and explicitly noted the importance of patient engagement through group interaction, ‘leveraging the group dynamic to transform the typical patient–clinician encounter’.73 Positive outcomes were reported from participants both in terms of individual uptake of advance directives but also in reported conversations with loved ones. Group appointments were suggested to be an effective forum for knowledge exchange creating an efficient and less stressful situation than one-on-one office visits,76 and overcoming a number of barriers related to process, time and role responsibilities. This study was one of two reported interventions from a patient-centred medical home perspective and warrants further consideration. This approach leveraged all of the key components identified by De Vleminck and in addition, compressed time demands by using the group approach. The authors recommended more research to understand the sustainable work flows required and to address ongoing barriers.
Discussion
In seeking complementarity or synergy across levels of influence, McCormack et al reported that the socioecological model had demonstrated benefit.29 This was also described by Weiner et al 30 noting the potential synergies to be gained using a socioecological approach provided ‘compelling justification for multi-level intervention’. However, both acknowledged a lack of theoretical guidance with regard to the optimal design of multilevel interventions.
In seeking to understand optimal design of interventions, Pettigrew et al outlined two important considerations. The first was that complexity may be associated with the activities, singular or multiple, which comprise the actions of an intervention.81 The second consideration was that complexity may be associated with other mediators and moderators operating between the actions. Feedback loops occurring between the mediators and moderators have been described as mechanisms of action alternatively known as causal pathways. These pathways have been said to create or limit the effect of an intervention.81 Many studies in this literature review could be understood with regard to the first consideration—exploring activities, singular or multiple in various combinations. Studies concerned with the second consideration of looking at how or if the various interventions when combined together created or limit their effect were largely silent in the general practice ACP literature.
With regard to this second consideration, an approach to causal modelling was described by Weiner et al 30 in which five mechanisms of action were proposed. Each of the five mechanisms—accumulation, amplification, facilitation, cascade and convergence was observable but not explicitly described in the intervention literature. An accumulation strategy is at work when each intervention makes a discreet contribution to the outcome.29 30 The interventions occur at different levels of influence and produce an accumulative impact to achieve the desired outcome.30 It is accumulative because the effect of each intervention is not conditional on the other intervention. For example, in Heiman’s RCT, two separate interventions known to have positive impact individually were combined to determine if a greater impact was achievable. The first intervention was the sending of ACP information to individual patients prior to consultation with their GP. The second intervention involved sending a computer prompt to the patient’s GP during the consultation. Both actions were independent of the other, each targeting different levels of influence, but together had an accumulative effect resulting in a small but significant overall increase in ACP.68 Combining interventions in this manner was commonly described in the review literature. The implication for future intervention design is the explicit combination of known enablers across multiple levels will be more effective.
When considering amplification strategy, the effect of one intervention is conditional on another. One intervention increases the target audience’s receptivity to the other intervention.30 This mechanism was identifiable in a study by Amjad et al 47 where a patient’s previous experience of caring for someone at end of life (interpersonal level) was found to directly influence (or amplify) their likelihood of engaging with their own ACP (individual level).47 Understanding the conditional relationship or links between activities when planning interventions could be anticipated to enhance outcomes but was not observed in most studies.
Where an intervention clears the way or removes barriers for another intervention, it is facilitating the outcome. Facilitation strategy was commonly described in the body of general practice ACP literature.30 To illustrate, lack of GP knowledge about ACP was widely identified as a barrier to GP participation in ACP.30 43 51 53–55 63 67 68 73 74 78 81–83 By delivering GP education, one intervention77 sought to improve GP knowledge,77 which in turn would remove the lack of knowledge barrier, and arguably clear the way for improved GP engagement in ACP discussion. Interventions addressing known barriers were demonstrated in the literature but the complexity of association between barriers was often overlooked. For example a study facilitating access to knowledge and resources but failing to quarantine time overlooks a critical barrier. Facilitation alone was demonstrated to be insufficient.
The final two mechanisms were identified in more complex undertakings. In cascade strategy, an intervention at one level affects the desired outcome in and through one or more levels of influence.30 Generally this would occur from higher levels of influence to lower ones. In general practice ACP literature, a number of more complex interventions described a cascade like strategy. For example, Wissow et al 46 sought to increase ACP uptake through a multilevel intervention. To make ACP business as usual in clinic consultations the chief of staff provided opinion leader endorsement and introduced top down processes including allowance for structured ACP discussion time during consultation, and provision of ACP tools, templates and scripts. Combined with this, at the provider level, GP training in communication skills, was intended to increase GP likelihood of initiating ACP discussion with their patients. The combined actions cascading from the Director’s endorsement down constituted a test case for a multilevel intervention with cascading influence.46
Similarly, in convergence strategy, influence at different levels mutually reinforce each other by altering patterns of interaction.30 The extent to which convergence strategy applied in the literature can only be assumed as it was not explicitly noted. In a study by Lum et al, 73 the research explored ACP group medical appointments.73 Using this model of care, system levels changes around scheduling and provision of information was mutually reinforced by planning a multidisciplinary team approach. The doctor–patient–social worker communication at an interpersonal level was reinforced during the group interaction. In this example, there was presumably convergence across several levels including individual, interpersonal, provider and system levels of influence. Convergence strategy was implicit in a number of general practice ACP research studies.64 67 68 70 73 79
Future complex intervention design may benefit from consideration of the relationships between barriers and enablers operating at various levels of influence, and factor causal mechanisms into the intervention design. By doing so greater uptake of ACP in general practice may be achievable.
To note, the bulk of ACP literature was generated in the USA and as described in the Introduction section, was included based on criteria to assimilate models of care most consistent with Australian general practice. There were no Australian systematic reviews found and limited general practice literature. In considering the applicability of findings into the Australian healthcare setting the literature presented consistent themes regardless of geographical origin. The authors are satisfied that the findings are relatable.
Limitations
The volume of studies describing barriers and enablers to ACP in general practice was abundant; however, studies focused on interventions in general practice were quite limited.84 85 Study quality was variable and a number of small scale studies focused on singular aspects of ACP limiting broader applicability. Existing Australian research draws heavily on international evidence to support local findings and a number of authors identified the need for more Australian research to inform policy and implementation.86–89 The extent to which international ACP evidence is applicable and transferable to a population or place based context within Australia is uncertain.
Lack of consistent terminology was a challenge addressed initially in the formulation of search terms and inclusion criteria, though it is possible that all relevant literature was not surfaced due to complex terminology. By focusing on general practice literature only, it is possible that transferable knowledge from other sectors may have been excluded. The researcher sought to reduce bias by adhering to the study protocol and by using reflexivity to monitor adherence to methods described.
The Australian Medical Association (AMA) argue that as a distinct medical specialty, general practice requires its own specific body of research and that findings from other medical research cannot simply be transferred to general practice.90 More studies are required to contribute to the available body of general practice research, described by AMA as the missing link in the development of high-quality, evidence-based healthcare for populations. Limited general practice intervention research was available and opportunities to expand the body of ACP knowledge through effective design of complex interventions will make a useful contribution both to increasing general practice research literature and to increasing ACP uptake through general practice.
In this review, the ACP literature was categorised and considered across socioecological levels of influence distilled from the narrative. This approach provided an insight into distribution of research interest across levels of influence. Individual and interpersonal levels of influence were the least researched in general practice and provider and system aspects focused on GPs and processes were the most prevalent. This finding was unexpected when considering the central role of the individual in ACP, and in relationship with their family, in determining values and wishes for end of life care, and the perceived role of general practice in supporting this process.
Not only were research findings in relation to individual perspectives limited, the patient voice was more commonly presented through a provider as proxy. Future studies should seek to engage patients directly.
Conclusion
This review was set against a back drop in which uptake of ACP remained consistently low, despite widespread agreement that it was beneficial, and with general agreement it was best achieved in primary care settings. The review sought to understand known barriers and enablers to ACP, and based on these, to determine what initiatives had been described to increase uptake of ACP. In seeking to understand barriers, enablers and efficacy of interventions, it was useful to understand at which level of influence across the socioecological perspective the interaction was occurring, and in doing so, consider how interventions had been developed to mitigate barriers and leverage enablers targeted for greatest effect.
By stratifying barriers, enablers and interventions into levels of influence, the important relationship between activities operating across levels became evident. Within this complexity, it was understood that some interventions were more effective than others, and combinations of interventions were more effective again. There appeared to be a shift away from considering ACP as ‘a singular action’ to be achieved or documented, instead to view ACP as a set of discreet steps in a complex process.43 Interventions targeting multiple levels of influence were said to reinforce each other, and consequently were expected to yield greater and more sustainable effects than interventions targeting only one level of influence.30
Findings from this review have identified a gap between historical research approaches which involved asynchronous testing of multiple mechanisms for ACP across all levels of influence, versus the potential for strategically applying the evidence across targeted levels of influence, and with an understanding of mediators and moderators to inform the design of new and effective ACP models of care.
Supplementary Material
Footnotes
Contributors: JRi is the primary author responsible for all aspects of the preparation of this document. LM is the medical research librarian assisting with search strategy rigour, manuscript editing and final revision. JRh is coinvestigator assisting with manuscript preparation, editing and final revision. LW is coacademic supervisor assisting with manuscript preparation, editing and final revision and providing academic oversight. PRW is coacademic supervisor assisting with the design, quality review, manuscript editing, final revision and providing academic oversight.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1. Council AHMA A national framework for advance care directives, 2011. [Google Scholar]
- 2. Australia PC. Advance care planning position statement, 2013. [Google Scholar]
- 3. Australia ACP. Respecting your choices, 2014. [Google Scholar]
- 4. Swerissen HD, Dying Well S. Grattan Institute, 2014. [Google Scholar]
- 5. ABo S. Population projections. Australia 2013b;2012. [Google Scholar]
- 6. Rao JK, Anderson LA, Smith SM. End of life is a public health issue. Am J Prev Med 2002;23:215–20. 10.1016/S0749-3797(02)00500-7 [DOI] [PubMed] [Google Scholar]
- 7. Chapman DP, Marshall Williams S, Strine TW, et al. Dementia and its implications for public health. Preventing Chronic Disease 2006;3. [PMC free article] [PubMed] [Google Scholar]
- 8. Singer PAM, D.K.; Kelner M. Quality end of life care: patient perspectives. JAMA 1998;281:163–8. [DOI] [PubMed] [Google Scholar]
- 9. Senate select Committee into palliative care in Australia. in: health do, editor 2012.
- 10. White B, Tilse C, Wilson J, et al. Prevalence and predictors of advance directives in Australia. Intern Med J 2014;44:975–80. 10.1111/imj.12549 [DOI] [PubMed] [Google Scholar]
- 11. Rhee JJ, Zwar NA. How is advance care planning conceptualised in Australia? findings from key informant interviews. Australian Health Review 2011;35:197–203. 10.1071/AH10883 [DOI] [PubMed] [Google Scholar]
- 12. Scott IA, Mitchell GK, J Reymond E, et al. Difficult but necessary conversations — the case for advance care planning. Med J Aust 2013;199:662–6. 10.5694/mja13.10158 [DOI] [PubMed] [Google Scholar]
- 13. De Vleminck A, Batteauw D, Demeyere T, et al. Do non-terminally ill adults want to discuss the end of life with their family physician? an explorative mixed-method study on patients' preferences and family physicians' views in Belgium. Family Practice 2017:20. [DOI] [PubMed] [Google Scholar]
- 14. Miller H, Tan J, Clayton JM, et al. Patient experiences of nurse-facilitated advance care planning in a general practice setting: a qualitative study. BMC Palliat Care 2019;18:25 10.1186/s12904-019-0411-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hare D, Jerome-D'Emilia B. Using advance care planning to inform and improve practice. The Journal for Nurse Practitioners 2019;15:e61–3. 10.1016/j.nurpra.2018.09.020 [DOI] [Google Scholar]
- 16. Karen M, Detering KB, Ruseckaite R, et al. Prevalence and correlates of advance care directives among older Australians accessing health and residential aged care services: multicentre audit study. BMJ Open 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. RACGP Website, 2018. Available: https://www.racgp.org.au/becomingagp/what-is-a-gp/what-is-general-practice
- 18. Zwar N. The patient-centred medical home model: what does it mean for primary healthcare in NSW? : Sax Institute, 2016. Available: https://www.saxinstitute.org.au/news/the-patient-centred-medical-home-model-what-does-it-mean-for-primary-health-care-in-nsw/
- 19. 2018. Available: https://www.google.com.au/search?q=definition+barrier&rlz=1C1NHXL_en-gbAU769AU769&oq=definition+barrier&aqs=chrome.69i57j0l5.6345j0j7&sourceid=chrome&ie=UTF-8
- 20. Dictionary 2018.
- 21. Clauser SB, Taplin SH, Foster MK, et al. Multilevel intervention research: lessons learned and pathways forward. JNCI Monographs 2012;2012:127–33. 10.1093/jncimonographs/lgs019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Institute JB Critical appraisal Tool-cross sectional studies Adelaide: University of Adelaide, 2018. JBI Critical appraisal tools]. Available from Available: https://joannabriggs.org/research/critical-appraisal-tools.html
- 23. Institute JB Critical appraisal tool- qualitative research Adelaide: University of Adelaide, 2018. Available: https://joannabriggs.org/research/critical-appraisal-tools.html
- 24. Institute Jb Critical appraisal tool-quasi experimental Adelaide: University of Adelaide, 2018. Available: https://joannabriggs.org/research/critical-appraisal-tools.html
- 25. Institute JB Critical appraisal tool-RCT Adelaide: University of Adelaide, 2018. Available: https://joannabriggs.org/research/critical-appraisal-tools.html
- 26. Institute JB Critical appraisal tool-systematic review Adelaide: University of Adelaide, 2018. Available: https://joannabriggs.org/research/critical-appraisal-tools.html
- 27. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McLeroy KR, Bibeau D, Steckler A, et al. An ecological perspective on health promotion programs. Health Educ Q 1988;15:351–77. 10.1177/109019818801500401 [DOI] [PubMed] [Google Scholar]
- 29. McCormack L, Thomas V, Lewis MA, et al. Improving low health literacy and patient engagement: a social ecological approach. Patient Educ Couns 2017;100:8–13. 10.1016/j.pec.2016.07.007 [DOI] [PubMed] [Google Scholar]
- 30. Weiner BJ, Lewis MA, Clauser SB, et al. In search of synergy: strategies for combining interventions at multiple levels. JNCI Monographs 2012;2012:34–41. 10.1093/jncimonographs/lgs001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. De Vleminck A, Houttekier D, Pardon K, et al. Barriers and facilitators for general practitioners to engage in advance care planning: a systematic review. Scand J Prim Health Care 2013;31:215–26. 10.3109/02813432.2013.854590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sharp T, Moran E, Kuhn I, et al. Do the elderly have a voice? advance care planning discussions with frail and older individuals: a systematic literature review and narrative synthesis. British Journal of General Practice 2013;63:e657–68. 10.3399/bjgp13X673667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Oczkowski SJ, Chung H-O, Hanvey L, et al. Communication tools for end-of-life decision-making in ambulatory care settings: a systematic review and meta-analysis. PLoS One 2016;11:e0150671 10.1371/journal.pone.0150671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ramsaroop SD, Reid MC, Adelman RD. Completing an advance Directive in the primary care setting: what do we need for success? J Am Geriatr Soc 2007;55:277–83. 10.1111/j.1532-5415.2007.01065.x [DOI] [PubMed] [Google Scholar]
- 35. Durbin CR, Fish AF, Bachman JA, et al. Systematic review of educational interventions for improving advance Directive completion. Journal of Nursing Scholarship 2010;42:234–41. 10.1111/j.1547-5069.2010.01357.x [DOI] [PubMed] [Google Scholar]
- 36. Mary Ann J, Mary Ann M, Loralee S, et al. The effectiveness of interventions to increase advance Directive completion rates. Journal of Aging and Health 2007;19:519–36. [DOI] [PubMed] [Google Scholar]
- 37. Solis GR, Mancera BM, Shen MJ. Strategies used to facilitate the discussion of advance care planning with older adults in primary care settings. J Am Assoc Nurse Pract 2018;30:270–9. 10.1097/JXX.0000000000000025 [DOI] [PubMed] [Google Scholar]
- 38. Tamayo-Velázquez M-I, Simón-Lorda P, Villegas-Portero R, et al. Interventions to promote the use of advance directives: an overview of systematic reviews. Patient Educ Couns 2010;80:10–20. 10.1016/j.pec.2009.09.027 [DOI] [PubMed] [Google Scholar]
- 39. Schickedanz AD, Schillinger D, Landefeld CS, et al. A clinical framework for improving the advance care planning process: start with patients' self-identified barriers. J Am Geriatr Soc 2009;57:31–9. 10.1111/j.1532-5415.2008.02093.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Schröder L, Hommel G, Sahm S. Intricate decision making: ambivalences and barriers when fulfilling an advance Directive. Patient preference & adherence 2016;10:1583–9. 10.2147/PPA.S109040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Musa I, Seymour J, Narayanasamy MJ, et al. A survey of older peoples’ attitudes towards advance care planning. Age Ageing 2015;44:371–6. 10.1093/ageing/afv041 [DOI] [PubMed] [Google Scholar]
- 42. O'Sullivan R, Mailo K, Angeles R, et al. Advance directives: survey of primary care patients. Canadian Family Physician 2015;61:353–6. [PMC free article] [PubMed] [Google Scholar]
- 43. Sudore RL, Schickedanz AD, Landefeld CS, et al. Engagement in multiple steps of the advance care planning process: a descriptive study of diverse older adults. J Am Geriatr Soc 2008;56:1006–13. 10.1111/j.1532-5415.2008.01701.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Howard M, Day AG, Bernard C, et al. Development and psychometric properties of a survey to assess barriers to implementing advance care planning in primary care. J Pain Symptom Manage 2018;55:12–21. 10.1016/j.jpainsymman.2017.08.003 [DOI] [PubMed] [Google Scholar]
- 45. Sudore RL, Landefeld CS, Barnes DE, et al. An advance Directive redesigned to meet the literacy level of most adults: a randomized trial. Patient Educ Couns 2007;69:165–95. 10.1016/j.pec.2007.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wissow LS, Belote A, Kramer W, et al. Promoting advance directives among elderly primary care patients. J Gen Intern Med 2004;19:944–51. 10.1111/j.1525-1497.2004.30117.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Amjad H, Towle V, Fried T. Association of experience with illness and end-of-life care with advance care planning in older adults. J Am Geriatr Soc 2014;62:1304–9. 10.1111/jgs.12894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Aoki T, Miyashita J, Yamamoto Y, et al. Patient experience of primary care and advance care planning: a multicentre cross-sectional study in Japan. Fam Pract 2017;34:206–12. 10.1093/fampra/cmw126 [DOI] [PubMed] [Google Scholar]
- 49. Mann J, Gill SD, Mitchell L, et al. Locating advance care planning facilitators in general practice increases consumer participation. Australian family physician 2017;46:691. [PubMed] [Google Scholar]
- 50. Emanuel LL, Barry MJ, Stoeckle JD, et al. Advance directives for medical care — a case for greater use. New England Journal of Medicine 1991;324:889–95. 10.1056/NEJM199103283241305 [DOI] [PubMed] [Google Scholar]
- 51. Tierney WM, Dexter PR, Gramelspacher GP, et al. The effect of discussions about advance directives on patients' satisfaction with primary care. Journal of General Internal Medicine 2001;16:32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Doukas DJ, Gorenflo DW, Coughlin SS. The living will: a national survey. Family Medicine 1991;23:354–6. [PubMed] [Google Scholar]
- 53. Wickersham E, Gowin M, Deen MH, Nagykaldi Z. Improving the Adoption of Advance Directives in Primary Care Practices. Journal of the American Board of Family Medicine. 2019;32(2):168‐79. [DOI] [PMC free article] [PubMed]
- 54. Bose-Brill SMD, Kretovics M, Ballenger TMD, et al. Testing of a tethered personal health record framework for early end-of-life discussions. The American Journal of Managed Care 2016;22:258. [PubMed] [Google Scholar]
- 55. Sinclair C, Gates K, Evans S, et al. Factors influencing Australian general practitioners' clinical decisions regarding advance care planning: a factorial survey. J Pain Symptom Manage 2016;51:718–27. 10.1016/j.jpainsymman.2015.11.014 [DOI] [PubMed] [Google Scholar]
- 56. Rhee JJ, Zwar NA, Kemp LA. Uptake and implementation of advance care planning in Australia: findings of key informant interviews. Australian Health Review 2012;36:98–104. 10.1071/AH11019 [DOI] [PubMed] [Google Scholar]
- 57. Otte IC, Elger B, Jung C, et al. The utility of standardized advance directives: the general practitioners’ perspective. Med Health Care Philos 2016;19:199–206. 10.1007/s11019-016-9688-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Fletcher S, Sinclair C, Rhee J, et al. Rural health professionals‘ experiences in implementing advance care planning: a focus group study. Aust J Prim Health 2016;22:423–7. 10.1071/PY15004 [DOI] [PubMed] [Google Scholar]
- 59. Dexter PR, et al. Effectiveness of computer-generated reminders for increasing discussions about advance directives and completion of advance Directive forms. Ann Intern Med 1998;128:102–10. 10.7326/0003-4819-128-2-199801150-00005 [DOI] [PubMed] [Google Scholar]
- 60. Fan E, Rhee JJ. A self-reported survey on the confidence levels and motivation of new South Wales practice nurses on conducting advance-care planning (ACP) initiatives in the general-practice setting. Aust J Prim Health 2017;23:80–6. 10.1071/PY15174 [DOI] [PubMed] [Google Scholar]
- 61. Sharp T, Malyon A, Barclay S. GPs’ perceptions of advance care planning with frail and older people: a qualitative study. British Journal of General Practice 2018;68:e44–53. 10.3399/bjgp17X694145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Pfeifer MP, Sidorov JE, Smith AC, et al. The discussion of end-of-life medical care by primary care patients and physicians: a multicenter study using structured qualitative interviews. The EOL Study Group. Journal of General Internal Medicine 1994;9:82–8. [DOI] [PubMed] [Google Scholar]
- 63. De Vleminck A, Pardon K, Beernaert K, et al. How do general practitioners Conceptualise advance care planning in their practice? A qualitative study. PLoS One 2016;11:e0153747 10.1371/journal.pone.0153747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Holland DE, Vanderboom CE, Dose AM, et al. Nurse-Led patient-centered advance care planning in primary care. Journal of Hospice & Palliative Nursing 2017;19:368–75. 10.1097/NJH.0000000000000358 [DOI] [Google Scholar]
- 65. Otte IC, Jung C, Elger BS, et al. Advance directives and the impact of timing. Swiss Medical Weekly 2014;144. [DOI] [PubMed] [Google Scholar]
- 66. Dipko LR, Xavier K, Kohlwes RJ. Advance Directive group education in a Va outpatient clinic. Soc Work Health Care 2004;38:93–106. 10.1300/J010v38n02_05 [DOI] [PubMed] [Google Scholar]
- 67. Duffield P, Podzamsky JE. The completion of advance directives in primary care. Journal of Family Practice 1996;42:378–84. [PubMed] [Google Scholar]
- 68. Heiman H, Bates DW, Fairchild D, et al. Improving completion of advance directives in the primary care setting: a randomized controlled trial. Am J Med 2004;117:318–24. 10.1016/j.amjmed.2004.03.027 [DOI] [PubMed] [Google Scholar]
- 69. Hughes DL, Singer PA. Family physicians' attitudes toward advance directives. CMAJ Canadian Medical Association Journal 1992;146:1937–44. [PMC free article] [PubMed] [Google Scholar]
- 70. Pearlman RA, Starks H, Cain KC, et al. Improvements in advance care planning in the Veterans Affairs system: results of a multifaceted intervention. Archives of Internal Medicine 2005;165:667–74. [DOI] [PubMed] [Google Scholar]
- 71. Fried TR, Redding CA, Robbins ML, et al. Stages of change for the component behaviors of advance care planning. J Am Geriatr Soc 2010;58:2329–36. 10.1111/j.1532-5415.2010.03184.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. De Vleminck A, Houttekier D, Deliens L, et al. Development of a complex intervention to support the initiation of advance care planning by general practitioners in patients at risk of deteriorating or dying: a phase 0-1 study. BMC Palliat Care 2016;15 10.1186/s12904-016-0091-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Lum HD, Jones J, Matlock DD, et al. Advance care planning meets group medical visits: the feasibility of promoting conversations. The Annals of Family Medicine 2016;14:125–32. 10.1370/afm.1906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Rose BL, Leung S, Gustin J, et al. Initiating advance care planning in primary care: a model for success. J Palliat Med 2019;22:427–31. 10.1089/jpm.2018.0380 [DOI] [PubMed] [Google Scholar]
- 75. Cartwright C, Montgomery J, Rhee J, et al. Medical practitioners' knowledge and self-reported practices of substitute decision making and implementation of advance care plans. Intern Med J 2014;44:234–9. 10.1111/imj.12354 [DOI] [PubMed] [Google Scholar]
- 76. Gordon NP, Shade SB. Advance directives are more likely among seniors asked about end-of-life care preferences. Arch Intern Med 1999;159:701–4. 10.1001/archinte.159.7.701 [DOI] [PubMed] [Google Scholar]
- 77. Detering K, Silvester W, Corke C, et al. Teaching general practitioners and doctors-in-training to discuss advance care planning: evaluation of a brief multimodality education programme. BMJ Support Palliat Care 2014;4:313–21. bmjspcare-2013-000450 10.1136/bmjspcare-2013-000450 [DOI] [PubMed] [Google Scholar]
- 78. Thompson TDB, Barbour RS, Schwartz L. Health professionals' views on advance directives: a qualitative interdisciplinary study. Palliat Med 2003;17:403–9. 10.1191/0269216303pm784oa [DOI] [PubMed] [Google Scholar]
- 79. Splendore E, Grant C. A nurse practitioner–led community workshop: increasing adult participation in advance care planning. Journal of the American Association of Nurse Practitioners 2017;29:535–42. [DOI] [PubMed] [Google Scholar]
- 80. Tieu C, Chaudhry R, Schroeder DR, et al. Utilization of patient electronic messaging to promote advance care planning in the primary care setting. Am J Hosp Palliat Care 2017;34:665–70. 10.1177/1049909116650237 [DOI] [PubMed] [Google Scholar]
- 81. Petticrew M, Anderson L, Elder R, et al. Complex interventions and their implications for systematic reviews: a pragmatic approach. Int J Nurs Stud 2015;52:1211–6. 10.1016/j.ijnurstu.2015.01.004 [DOI] [PubMed] [Google Scholar]
- 82. Brown J. Practical methods to increase use of advance medical directives. Journal of Internal medicine 1999;14:21–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Doukas DJ, McCullough LB. The values history: the evaluation of the patient's values and advance directives. Journal of Family Practice 1991;32:145–53. [PubMed] [Google Scholar]
- 84. Jeong SY-S, Higgins I, McMillan M. Experiences with advance care planning: older people and family members’ perspective. Int J Older People Nurs 2011;6:176–86. 10.1111/j.1748-3743.2009.00201.x [DOI] [PubMed] [Google Scholar]
- 85. Nair B, Kerridgey I, Dobson A, et al. Advance care planning in residential care. Aust N Z J Med 2000;30:339–43. 10.1111/j.1445-5994.2000.tb00835.x [DOI] [PubMed] [Google Scholar]
- 86. Bloomer M, Tan H, Lee S. End of life care-the importance of advance care planning. Australian Family Physician;39:734–7. [PubMed] [Google Scholar]
- 87. Boddy J, Chenoweth L, McLennan V, et al. It’s just too hard! Australian health care practitioner perspectives on barriers to advance care planning. Aust J Prim Health 2013;19:38–45. 10.1071/PY11070 [DOI] [PubMed] [Google Scholar]
- 88. Michael N, O’Callaghan C, Clayton J, et al. Understanding how cancer patients actualise, relinquish, and reject advance care planning: implications for practice. Supportive Care in Cancer 2013;21:2195–205. 10.1007/s00520-013-1779-6 [DOI] [PubMed] [Google Scholar]
- 89. Lovell A, Yates P. Advance care planning in palliative care: a systematic literature review of the contextual factors influencing its uptake 2008–2012. Palliat Med 2014;28:1026–35. 10.1177/0269216314531313 [DOI] [PubMed] [Google Scholar]
- 90. Rosser WW. Research in Family/General practice is essential for improving health globally. The Annals of Family Medicine 2004;2(suppl_2):S2–4. 10.1370/afm.145 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-030275supp001.pdf (49.5KB, pdf)
bmjopen-2019-030275supp002.pdf (100.7KB, pdf)
bmjopen-2019-030275supp003.pdf (126.3KB, pdf)