Abstract
Objective
To review systematically the evidence on the costs and cost-effectiveness of deinstitutionalisation for adults with intellectual disabilities.
Design
Systematic review.
Population
Adults (aged 18 years and over) with intellectual disabilities.
Intervention
Deinstitutionalisation, that is, the move from institutional to community settings.
Primary and secondary outcome measures
Studies were eligible if evaluating within any cost-consequence framework (eg, cost-effectiveness analysis, cost–utility analysis) or resource use typically considered to fall within the societal viewpoint (eg, cost to payers, service-users, families and informal care costs).
Search
We searched MEDLINE, PsycINFO, CENTRAL, CINAHL, EconLit, Embase and Scopus to September 2017 and supplemented this with grey literature searches and handsearching of the references of the eligible studies. We assessed study quality using the Critical Appraisals Skills Programme suite of tools, excluding those judged to be of poor methodological quality.
Results
Two studies were included; both were cohort studies from the payer perspective of people leaving long-stay National Health Service hospitals in the UK between 1984 and 1992. One study found that deinstitutionalisation reduced costs, one study found an increase in costs.
Conclusion
A wide-ranging literature review found limited evidence on costs associated with deinstitutionalisation for people with intellectual disabilities. From two studies included in the review, the results were conflicting. Significant gaps in the evidence base were observable, particularly with respect to priority populations in contemporary policy: older people with intellectual disabilities and serious medical illness, and younger people with very complex needs and challenging behaviours.
PROSPERO registration number
CRD42018077406
Keywords: Economics, intellectual disabilities, deinstitutionalisation
Strengths and limitations of this study.
Examining a topic that was not previously the subject of a systematic review, we searched seven databases of peer-reviewed literature evaluating returned studies using two independent reviewers.
Identified evidence, therefore, represents state of the science on a pressing policy question for an underserved population.
We did not search books or monographs.
Commissioned by policy-makers to examine specifically the process of deinstitutionalisation, we did not include cross-sectional studies comparing outcomes for different populations in different settings.
Introduction
Background/rationale
The 2006 United Nations Convention on the Rights of Persons with Disabilities emphasises the right to live independently in a place of one’s own choosing.1 The promotion of autonomous decision-making and full participation in society for people with disabilities and mental health problems through deinstitutionalisation—movement from living in institutional settings to community settings—has variously occurred in Scandinavia, the UK, USA, Canada and Australia since the 1960s.2
While significant numbers of people have moved out of institutional settings over the last half century, substantial numbers with disabilities, including intellectual disabilities, are still prevented from living in a place of their own choosing, instead being restricted to institutions or inadequate community-based services.3 This is the case even in those countries where the process of deinstitutionalisation is quite advanced.4
In Ireland, a first wave of deinstitutionalisation included movement to smaller living units on what are called campus settings.5 A more decisive break from institutional to community arrangements for people with intellectual disability is now the stated policy priority.5 The Irish government, wishing to benefit from the experience of others and the best available and most rigorous evidence, commissioned through the Health Research Board, a systematic review of the evidence on the effect of deinstitutionalisation on economic outcomes and on quality of life (QoL) for people with intellectual disabilities. Their interest was specifically in analysis of those moving residence, rather than in cross-sectional analysis of different people living in the different settings. In this paper, we report the search strategy for the whole systematic review, and the results for the economics studies. QoL results have been published previously.6
Economic evaluations comparing the costs and outcomes of different options may inform decisions on which of the available choices represents the best use of the resources available.7 The accurate estimation of resource use in providing services can inform budgeting, workforce planning and organisation of services in the short and long term when groups of interest, in this case people with intellectual disabilities, are growing in number and complexity of need, and account disproportionately for overall expenditures.8
The population of people with intellectual disabilities is changing in important ways that must be accounted for in planning and provision of services.9 Life expectancy for children born with high levels of disability has increased markedly, meaning that supports must be provided to a growing number of people with very high needs, and increased life expectancy among the population of people with intellectual disabilities means rising prevalence of old age, multimorbidity and dementia.9–12 Taken together, these trends mean that, in the 21st century, societies worldwide face never-before-seen populations of people with intellectual disabilities and high support needs, and a limited evidence base on which to base funding decisions and budget projections. An historic reliance on informal care from unpaid family and friends may not be sustainable as age and mobility burdens increase among the carers themselves.13
Objectives
To review systematically the evidence on the costs and cost-effectiveness of deinstitutionalisation for adults with intellectual disabilities.
Methods
Eligibility criteria
We used the participants, interventions, comparators, outcomes and study types)/participants, exposure, outcomes and study types) frameworks to define review eligibility as follows:
Types of participants
Adults (aged 18 years and over) with intellectual disabilities. No predetermined operational definition of intellectual disability was used; we followed author definition in the first instance and planned to resolve ambiguities through discussion and author contact if necessary.
Types of intervention/exposure/comparators
The intervention of interest in this review was deinstitutionalisation, that is, the move from institutional to community settings. We chose not define these ex ante, for example, according to the number of residents per unit, since no widely accepted cut-offs exist and any such cut-offs risked arbitrarily excluding studies of relevance. Moreover, deinstitutionalisation has occurred at different speeds in different countries over the last half century, in some cases incorporating phases of reinstitutionalisation (the residential move back from the community to an institution) and transinstitutionalisation (a residential move between institutions).14
We, therefore, defined our intervention/exposure variable broadly so as to avoid arbitrary exclusion of relevant studies, and we assessed the characteristics of settings on a study-by-study basis on the information provided.
Types of outcomes
Our prespecified primary outcome of interest was economic effects. For purposes of the review, economic effects were defined broadly as any cost-consequence framework (eg, cost-effectiveness analysis, cost–utility analysis) or resource use quantified as costs. We did not require that resource use which reflects the literal cost of provision for the study to be included, but also considered eligibility based on other approaches to calculating expenditures, such as insurance programme charges, frequency utilisation combined with unit cost data. We considered eligible any perspective typically considered to fall within the societal viewpoint (eg, cost to payers, service-users, families and informal care costs).
Types of studies/reports
Prospective/retrospective before and after studies, randomised trials, qualitative/descriptive and exploratory studies that reported on economic evaluations were eligible for inclusion. To be consistent with the desire to understand the likelihood of increases in QoL and in cost consequences over time, we excluded studies that did not evaluate economic effects following a move, and cross-sectional studies comparing community-living and institutional arrangements for two different groups at a single point in time.
Search strategy
Database search
Our search methodology encompassed both published and grey (eg, policy reports, national/international guideline documents, etc) literature using multiple sources. We restricted inclusion of studies to English language publications, but noted potentially eligible non-English language papers to determine whether this might present as a possible source of language bias.
Electronic databases were searched from their date of inception to September 2017. Using search terms and Medical Subject Headings, developed by an information specialist (GS) following ‘scoping’ and pilot searches, and confirmed with the review team, the databases of MEDLINE, PsycINFO, CENTRAL, CINAHL, EconLit, Embase and Scopus were searched (see online supplementary appendix 1 for full details).
bmjopen-2018-025736supp001.pdf (365.3KB, pdf)
Other sources
Grey literature searching focused on non-academic publications, readily available online. Documents of interest included government, statutory organisation, non-statutory organisation (eg, national disability organisations and university-based centres of disability studies), guideline or policy documents or reports of clinical audit with available primary or secondary analytical data (see online supplementary appendix 1 for details).
Study selection and quality assessment
Screening citations
Titles and abstracts of retrieved citations were assessed independently by two reviewers (RLV and EM); full-text papers forwarded from title and abstract screening were assessed independently by two reviewers (RLV and PM). Any differences of opinion on inclusion/exclusion at both stages were resolved between the reviewers based on discussion and consensus. A review manager software package, COVIDENCE (https://www.covidence.org/) supported screening and selecting relevant studies.
Assessment of methodological quality/risk of bias
The methodological quality of each included studies was assessed using the Critical Appraisal Skills Programme (CASP, http://www.casp-uk.net/casp-tools-checklists) standardised assessment tool appropriate to the included study’s design, that is, CASP Case Control Checklist, CASP Economic Evaluation Checklist or CASP Qualitative Checklist. All CASP checklists cover the three main areas of validity, results and clinical relevance. The CASP tool offers a set of 10 questions to which the reviewer assigns yes, no or can’t tell judgements (online supplementary appendix 1). Those studies that receive all (or mostly) yes assessments were judged to be of high quality (low risk of bias) and similarly, those receiving majority ‘no’ or ‘can’t tell’ assessments were considered of moderate or low quality. In a list with 11 categories, six ‘yes’ verdicts were, therefore, sufficient for inclusion.
One reviewer (PM) assessed the studies’ methodological quality and a second reviewer (CN) performed a rapid assessment to confirm judgements on quality. Conflicts were resolved through discussion and consensus. To limit bias and/or overestimates of effects that may arise from poorly designed, conducted and reported studies, studies were determined to meet a minimum of moderate to high quality of rigour to be included in the review (see online supplementary appendix 1).
Data analyses
Data extraction
Predesigned and piloted data extraction forms captured year of study, study setting, type of study design, descriptions of the population/participants, interventions and comparator, ethical issues (eg, consent), cost outcome data (results) and authors’ conclusions. One reviewer (PM) extracted the data from the included papers, and a second reviewer (CN) performed a rapid assessment to confirm accuracy and comprehensiveness of the extracted data. As before, any differences were resolved by the discussion and consensus.
Data syntheses
Summary measures
The principal summary measure was the mean estimated effect of move in residential setting on costs or cost-effectiveness (from whatever perspective the study specified). Mean estimated effects on subcategories of costs, as well as drivers of costs, were the secondary measures of interest.
Analytical measures
A priori, our aim was to perform a meta-analysis of individual studies’ data so as to achieve an overall (higher level) effect estimate of cost outcomes following a move from an institutional setting to a different/community-based setting. Statistical pooling of data across studies proved neither feasible nor appropriate due to inadequate information on postdischarge residences and associated costs. We, therefore, present a narrative synthesis of the data using descriptive statistics and thematic analyses.
Patient and public involvement
There was no involvement of any person with an intellectual disability or the wider public in this systematic review. A representative from the National Disability Authority of Ireland,15 an independent state body providing expert advice on disability policy and practice to the government and the public sector, participated in the design of the systematic search strategy to maximise relevance to current policy and practice.
Results
Search and selection results
Database search
The database search, which was a combined search of studies reporting on both cost and QoL, returned 25 853 citations for consideration against the review’s eligibility criteria of which 6568 were duplicate citations across databases, and were excluded. A further 19 000 citations were excluded during title and abstract screening as they clearly did not meet the review’s prespecified eligibility criteria (figure 1). This left 285 papers for full-text review; of these a further 217 were excluded and 32 were unobtainable. Reasons for exclusion were: no examination of a change in residential setting (127 articles), no cost or author-defined QoL data (46), opinion or commentaries and reviews (18), not in English language (12), not an adult population with intellectual disability (8) and miscellaneous (6).
Figure 1.
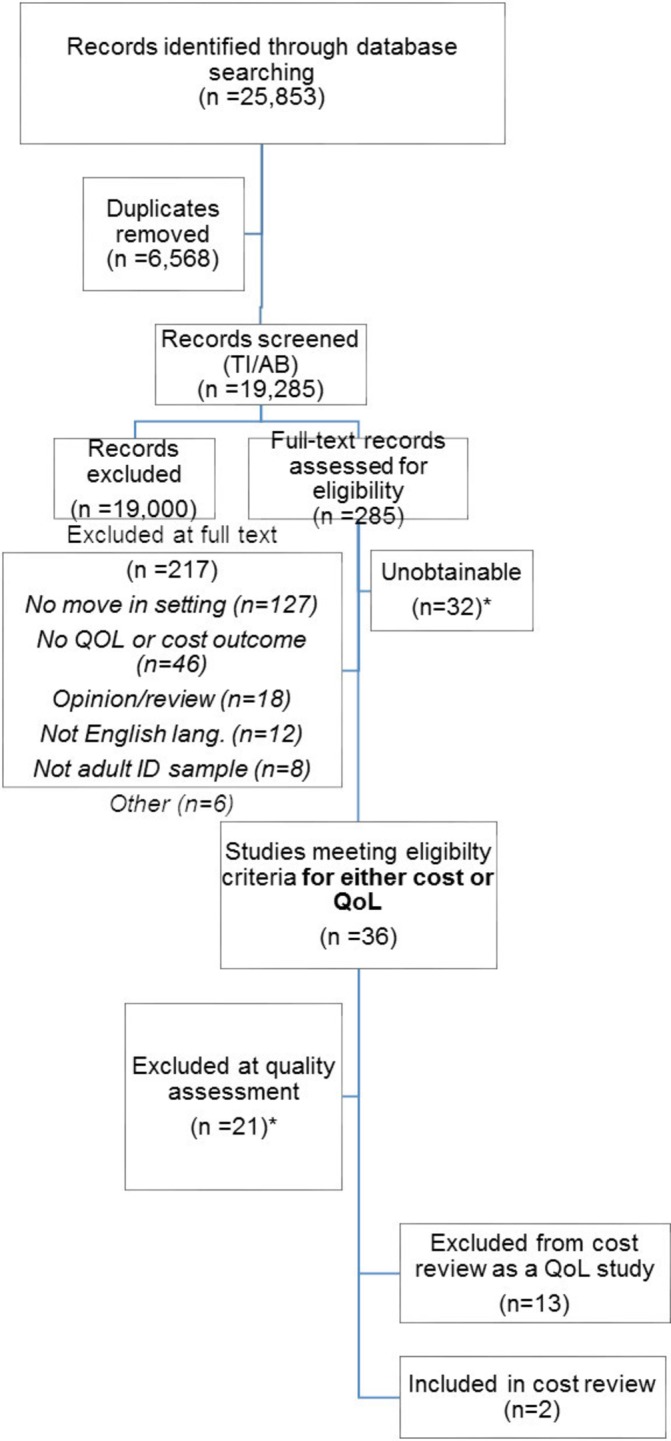
PRISMA for economics search. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; QoL, quality of life. *For details of unobtainable papers and those excluded at quality assessment, see online supplementary.
Of the remaining 36 included studies, 21 of these were subsequently excluded based on methodological quality assessments using the CASP tool. Reasons for exclusion at this stage were failure to establish consent of study participants, and insufficient and negligible data on participants and/or outcomes (see online supplementary appendix 1). Of the 15 studies remaining, 13 addressed QoL outcomes only (reported separately16) and 2 reported on costs. No study was eligible for both the QoL review and this economics review. We reviewed references of two included studies and did not identify further eligible studies for inclusion.
Grey literature search
The grey literature search resulted in retrieval of 74 reports, of which 30 appeared relevant to deinstitutionalisation from a cost and/or QoL perspective, but on further review, only six provided premove and postmove measures. Following a quality assessment of these six reports, none met the minimum standards, and all six were excluded from the review (see online supplementary appendix 1 for details).
Main results
Description of included studies
Two studies evaluated the impact on economic outcomes for people with intellectual disabilities who experienced a move in residential setting. Both studies follow a single cohort of people moving from long-stay hospitals in the UK National Health Service (NHS) and are summarised in table 1. Beecham et al examine costs at 12 months for adults moving from what were then called ‘learning disabilities’ and psychiatric hospitals in Northern Ireland between 1990 and 1992;17 Hallam et al examine longitudinally costs after 1, 5 and 12 years for adults moving from 12 different sites in England between 1984 and 1987.18
Table 1.
Summary characteristics of included studies
| Lead author and year | Location (country); dates of study | Aim | Study design | Description of study sample | Description of congregated setting | Description of community setting |
| Beecham17 (1997) | Northern Ireland, 1990–1993 | To evaluate the effect on costs of discharging people with intellectual disabilities from long-stay hospitals to ‘community care’ | One cohort assessed prior to leaving hospital and 12 months after doing so | Adults with learning disabilities. Of 214 adults moving during study period, 22 were lost to follow-up leaving a sample of 192. 57% male* Median age 47 years* Median hospital stay prior to move 20 years* 7% low IQ score (<20), 52% medium IQ score (20–49), 33% high IQ score (50–69), and 8% not recorded* |
Three learning disabilities hospitals and four psychiatric hospitals | Residential facilities provided by statutory bodies (=30) Residential facilities provided by voluntary bodies (=20) Residential and nursing homes from private bodies (=141) Independent living arrangements (=1). |
| Hallam18 (2006) | England, 1984–1999 | Evaluation of ‘community care’ for people moving from learning disabilities hospitals | One cohort assessed prior to leaving hospital and at 1, 5 and 12 years postmove | Adults moving from learning disabilities hospitals. Of 397 recruited in hospital, 103 have cost data at all three outcome points. 47% male Mean age at move 44 Mean hospital length of stay premove 27 years |
12 long-stay hospitals across different regions | Residential/nursing home or hospice (=45)† Group home (=42)† Adult foster care or sheltered housing (=15)† Hospital (=1) Independent living (=0) |
*Data presented for 497 people moving 1987–1992; analytic cost sample of 192 are a subset of these for whom no specific data on characteristics are provided.
†All sample sizes for 12-year time point, some small divergence from these at 1 and 5 years. Categories grouped for this review according to number of residents: Residential/nursing home or hospice had six or more residents; Group homes had two to five residents; Adult foster care and sheltered housing do not specify sample size but are clients moving into established homes.
Both studies had a majority of ‘yes’ responses using the CASP assessment tool (table 2). Risk of bias within studies is considered low: each follows a single cohort of participants with each person effectively acting as their own control. Risk of bias across studies is difficult to ascertain: too little is known on both the populations and the interventions for strong conclusions to be drawn on representativeness of the study samples.
Table 2.
Quality assessment: included studies
| Study | Screening Q.1: Address clearly focused issue |
Screening Q.2: Cohort acceptably recruited |
Exposure accurately measured (min. bias) | Outcome accurately measured (min. bias) | Identified important confounding factors | Account for confounding factors in design/ analysis | Follow-up complete enough | Follow-up long enough | Believable results | Applicable to local population | Fit with available evidence | Total Yes | Total No | Total Can’t tell |
| Beecham17 (1997) | Yes | Yes | Can’t tell | Yes | No | No | Yes | Yes | Yes | Can’t tell | Can’t tell | 6 | 2 | 3 |
| Hallam18 (2006) | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Can’t tell | Can’t tell | 7 | 2 | 2 |
Both studies were parts of larger studies published in book form: Donnelly et al 19 is the companion to Beecham et al; Knapp et al 20 and Cambridge et al 21 present the main study for Hallam et al.
Review of both papers and books revealed limited information on the characteristics of the specific samples studied in the cost papers. Beecham et al do not report any sample characteristics although cost analyses are performed on a subset of the overall study’s analytic sample of 497 and indicative age, IQ level and time in hospital premove are provided for this larger group.19 Hallam et al report age and time in hospital premove, but no baseline information on level of disability or disease burden;18 in the supporting books the authors provide detailed baseline data (including gender, severity of intellectual disability, skills, behavioural issues, social interaction, depression, psychosocial function and life satisfaction) on the original recruited sample of people with intellectual disabilities (n=529) but it is not clear how representative is the subsample of 103 reported in the paper.20 21
An additional barrier to interpretation was the use of the term ‘community care’. In the Beecham et al study, only one person (total sample=192; 0.5%) is reported as moving to an independent living arrangement.17 Of the other settings, Beecham et al differentiate other categories according to provider (statutory, voluntary and private) but not setting characteristics such as specifying how many people lived in a single unit. A large majority of study participants (141; 73%) moved from hospital to ‘residential and nursing homes by private bodies’. It is, therefore, possible that a significant number of people ended up in community living,2 3 but it is not reported as such. In the Hallam et al, study settings are delineated more clearly by characteristics.18 At each time point postmove, approximately half were living in established homes via foster care or sheltered housing, or group homes with two to five residents per unit; 30%–40% of people were living in either nursing homes or hostels with six or more residents. Independent living was again highly unusual: two participants (2%) after 1 year; four (4%) after 5 years; 0 after 12 years
Key findings
Mean costs for hospital and ‘community’ care for each study are presented in table 3. In the Beecham et al study, mean costs are reported as lower for ‘community’ settings than hospital, but this difference is not tested for statistical significance (and none is possible ex post using the reported data). Differences within types of postmove residence are large and found to be statistically significant but comparisons of specific types of residence are not reported. As per table 1, ‘community’ settings are characterised by the sector of the provider but no other descriptive data, making it impossible to infer the characteristics of services that offer cost savings compared with hospital, beyond the fact that public facilities are more expensive and voluntary and private facilities are cheaper. These differences may reflect different levels of need among individuals and/or different levels and characteristics across provider (eg, the number of residents and environment) or they may reflect true differences in effect of provider type on cost of residential care for this population.
Table 3.
Key results from included studies sterling
| Author/ year | Mean (SD) weekly costs in pounds sterling,* by residential location | Evidence | |||||
| Beecham 17 (1997)† | Premove (No) | Postmove ‘community’ settings (No) | Mean costs are lower in ‘community’ settings than long-stay hospital, although no statistical analysis is reported and there is considerable variation is observable between different ‘community’ settings. | ||||
| Hospital (192) | Public (30) | Voluntary (20) | Private (141) | Ind. living(=1) | All (192) | ||
| 574 (−) | 517 (165) | 351 (72) | 323 (45) | 133 | 356 (106) | ||
| Hallam18 (2006)‡ | Premove (No=103) | Postmove all ‘community’ settings (No=103) | Mean costs are higher in ‘community’ settings than long-stay hospital at 1, 5 and 12 years; statistically significant in each case. No presentation or analysis of postdischarge costs by type of residence. | ||||
| Hospital | 1 Year | 5 Years | 12 Years | ||||
| 736 (136) | 899 (260) | 871 (301) | 765 (324) | ||||
| Paired t-test (df=102) | +163 (t=4.96, p<0.001) | +135 (t=35.04, p<0.001) | +29 (t=54.07, p< 0.001 | ||||
*In both cases, studies assessed formal costs per client (payer perspective) for hospital, community and accommodation services.
†Costs in £, 1994/1995 levels.
‡Costs in £, 2002/2003 levels.
In the Hallam et al study, mean costs are reported as higher for ‘community’ care than hospital care at 1, 5 and 12 years and these differences are statistically significant.18 In this comparison between hospital and ‘community’ costs, all ‘community’ costs were pooled meaning that no cost comparison of established home or small group home versus hospital was reported (and none is possible ex post using the reported data). Established home or small group home costs cannot be separated from nursing home and hostel costs. Secondary analysis by the study authors shows that accommodation accounts for 81%–86% of ‘community’ costs postmove. Summary cost data disaggregated by destination at 1 and 5 years were reported separately in prior books,20 21 but no formal evaluation of association between costs and specific destinations are reported.
Different categorisation of ‘community care’ precludes meta-analysis. Both studies examine the same cost perspective: formal costs to the payer of a broad basket of hospital, community and accommodation services associated with each specific individual. This, therefore, implies the same limitations, and in particular an absence of informal care costs and out-of-pocket costs that may rise when people leave institutions for settings where on-site care is less comprehensive. While both overall studies to which the cost papers were attached did examine client outcomes, no cost–consequence analysis or ratio is reported in either study.
Discussion
Key findings
The two economic studies identified by our review report opposing headline findings: one concludes that ‘community care’ was more costly per individual at 1, 5 and 12 years than long-stay hospital care, and these differences are statistically significant. The other found that costs were lower for ‘community care’, although this association is not evaluated for statistical significance.
The greatest strength of the two included studies is the seriousness and detail with which costs were calculated for formal care services received by each specific participant. A comparable basket of health and community care services was assessed premove and postmove in each study. One of the two studies also examined patterns over a 12-year window, an approach with growing value as the population of people with intellectual disabilities is ageing and so understanding of changing needs becomes more important.
This review was originally commissioned by policy-makers to inform policy and cost projections in Ireland, which is in the relatively early stages of a comprehensive deinstitutionalisation compared with neighbouring countries. Unfortunately, the results have limited relevance for those commissioners. The headline results of the main two studies are at odds with one another, and there are three principal barriers to interpreting these results.
First, different types of destination are grouped in ways that are ill suited to our research question. Both studies group different destinations with different associated costs under the label ‘community care’, precluding identification of association between movement to specific accommodation types and costs. Second, some destination types (eg, nursing home and hostel) would today be widely classified as institutions themselves, meaning that the reported association of ‘deinstitutionalisation’ is questionable. Third, both studies analyse subsamples of larger parent studies. While the overall samples are detailed in book form, limited detail on the analytical cost subsamples is provided, making generalisability hard to ascertain.
In considering how the results of this cost literature may inform contemporary policy, there are additional limitations in the age of the studies. Priority populations for policy-makers are older people with intellectual disabilities and serious medical illness, and younger people with very complex needs and challenging behaviours.2 3 In the context of the United Nations Convention on the Rights of Persons with Disabilities and a growing emphasis on independent living,1 3 autonomous decision-making and full participation in society for people with disabilities that are prominent in ways that they were not when the original studies were conducted. A number of people living independently following a move were negligible in both studies. New studies that consider these changed circumstances have the potential to offer more useful findings.
The primary importance of our findings is that community care is not unambiguously less expensive than institutional care over time. Consistent with earlier non-systematic assessments of this issue, the data are inconclusive.22 23 Advocates sometimes argue that deinstitutionalisation is what economists call a dominant strategy, that is, one that both reduces costs and improves outcomes. However, well intentioned, this position is not supported by the best available evidence. This finding in no way undermines the position that all people should be supported to lead lives in places of their own choosing, and our QoL results suggest that deinstitutionalisation is associated with significant benefits.6 Nevertheless, these benefits will not be realised without substantial resource commitments from government and other funding bodies.
Strengths and limitations
This study has followed the best practice guidelines in systematic evidence reviews where possible, following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. The search strategy was developed by a team featuring subject experts, a systematic review specialist and an information specialist. The strategy’s thoroughness resulted in a very large number of returned titles and abstracts from databases. These and advanced full texts were reviewed independently by two researchers. Likewise, all full texts accessed were independently reviewed by two team members. Quality assessment for eligible studies and data extraction for included studies was performed by one reviewer with a second reviewer’s corroborating review.
Nevertheless, there are a number of important limitations to our work. In devising our search strategy, we were faced with profound challenges in defining our intervention. While every effort was made to include all potentially studies through broad search criteria and no ex ante definition of institutional or community settings, it is possible that we overlooked some terms that would have captured other relevant material.
This choice of intervention—the process of deinstitutionalisation, and not comparative analysis of outcomes living in one setting versus another—reflected the interests of the Irish Department of Health, who commissioned this work to inform ongoing policy reforms. Those countries where the process is at an advanced stage and the majority of people with intellectual disabilities already live in the community, might find such comparative analyses to be more useful in informing policy. However, a significant number of people in those countries continue to live in institutions, disproportionately those with the high support needs that are of particular policy interest.
Our search strategy did turn up a larger body of cross-sectional comparisons, for example, of the cost of living in institutional settings versus community settings. Prior reviews have reported similarly mixed findings on the relative costs and there are additional concerns about the robustness of such comparisons and unobserved confounding, particularly with routinely collected data.23 A strength of the studies included in our review is that confounding concerns are minimised by the use of participants as their own controls.
In reviewing returned studies from the database search, we used two independent reviewers for title/abstract and full texts, but one reviewer at quality assessment and data extraction with a second reviewer providing a corroborating review. While corroboration by a second reviewer can be acceptable in the review process, the lack of independent second reviewer assessments does introduce the potential for bias in the quality assessment and data extraction phases of the review. Thirty-two (17%) of the studies that we identified as suitable for full-text review proved unobtainable and so are not included in our final analyses, thus, potentially introducing selection bias. These studies, however, are on average older than those we were able to access and are listed in online supplementary appendix 1.
The decision to require documentation of consent obtained from participants with intellectual disabilities and ethical considerations, a standard practice in systematic reviews, did mean that a number of older studies were excluded as well as all of the grey literature. Future studies may wish to revisit this issue.
We also included only English language studies in our review, excluding 12 studies on this basis, which is another potential source of bias. These studies are listed in online supplementary appendix 6 and were variously published in French (7), Croatian (2), German (2) and Japanese (1). It was, therefore, notable that no studies either included in the review or excluded due to language considerations originated in the Nordic countries with the longest history of deinstitutionalisation. It is possible that researchers and/or government agencies in these countries evaluated the impact of deinstitutionalisation prior to the mass uptake of online publishing, and that these evaluations exist somewhere purely offline.
The grey literature search was conducted by topic experts on the websites of research centres active in this field and those of governments in countries at the forefront of deinstitutionalisation in intellectual disability. This may have biassed reviewed studies against other nations and research groups. While much grey literature was excluded from the review for considerations including lack of comprehensive reporting on ethics, there may be findings of import within that literature that may warrant separate review or discussion.
Conclusion
A systematic review of the economic evidence of deinstitutionalisation for adults with intellectual disabilities identified two relevant studies, one of which found an increase in costs and one a decrease. Both were conducted on processes in the NHS in the 1980s and early 1990s, which limits relevance to 21st century international policy challenges. Economic studies of deinstitutionalisation for people with intellectual disabilities are, therefore, rare in the context of an ageing population with complex clinical and behavioural characteristics. Such research faces particular challenges in recruiting and retaining representative samples, defining and evaluating the causal effects of complex interventions often provided in multiple settings with multiple components, and maintaining study processes over long periods as people live months and years with serious illness and support needs. The growth in administrative datasets with the potential of standardised costs and shared definitions of key variables may offer an opportunity to better address these concerns. It is critical that more studies are conducted to understand both how to best support this growing population in leading independent lives of their choosing and the resources and resource allocations that will be needed to achieve this.
Supplementary Material
Footnotes
Contributors: MM and PhM codesigned the original review protocol, oversaw all phases of the review process and drafted and revised the paper. MM is guarantor. PeM codesigned the original review protocol, project-managed title/abstract and full-text review, performed the quality assessment and data extraction, and led writing of the paper. RLV and EM reviewed return studies for eligibility at title and abstract, and drafted and revised the paper. M-AO codesigned the original review protocol, led the grey literature search, advised and contributed throughout the review process as a topic expert, and drafted and revised the paper. NW conducted the grey literature search, and drafted and revised the paper. GS was the information specialist, codesigning and running the database searchers, and revising the paper. RS codesigned the original review protocol, advised and contributed throughout the review process as a topic expert and drafted and revised the paper. VS codesigned the original review protocol, advised and contributed throughout the review process as a systematic review expert, and drafted and revised the paper. CN codesigned the original review protocol, advised and contributed throughout the review process as an economics expert and drafted and revised the paper.
Funding: This work was funded by the Health Research Board (HRB). The study was funded by the Department of Health (Ireland), with commissioning assistance by the Health Research Board (Ireland).
Disclaimer: This work does not represent the opinions of the Department of Health in Ireland or the HRB, and any errors or omissions are the responsibility of the authors. All authors are independent of the study sponsors. All authors had full access to all of the data in the study and can take responsibility for the integrity of the data and the accuracy of the analysis.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: There are no data in this work. All data relevant to the study are included in the article or uploaded as online supplementary information.
References
- 1. United Nations Convention on the rights of persons with disabilities. New York: United Nations, 2006. [Google Scholar]
- 2. Mansell J, Beadle-Brown J. Deinstitutionalisation and community living: position statement of the comparative policy and practice special interest Research group of the International association for the scientific study of intellectual disabilities. J Intellect Disabil Res 2010;54:104–12. 10.1111/j.1365-2788.2009.01239.x [DOI] [PubMed] [Google Scholar]
- 3. Bigby C, Fyffe C, Mansell J. From ideology to reality: current issu es in implementation of intellectual disability policy. Roundtable on intellectual disability policy. Bundoora, Victoria: School of Social Work and Social Policy, La Trobe University, 2006. [Google Scholar]
- 4. NHS England Building the right support 2015.
- 5. Health Service Executive Time to move on from Congregated settings: a strategy for community inclusion 2011.
- 6. McCarron M, Lombard-Vance R, Murphy E, et al. . Effect of deinstitutionalisation on quality of life for adults with intellectual disabilities: a systematic review. BMJ Open 2019;9:e025735 10.1136/bmjopen-2018-025735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Drummond M, Sculpher MJ, Claxton K, et al. . Methods for the economic evaluation of health care programmes : Drummond MF, Sculpher MJ, Claxton K, et al., 4th edn OUP, 2015. [Google Scholar]
- 8. European Commission Ageing report economic and budgetary projections for the 28 EU member states (2013-2060). Luxembourg, 2015. [Google Scholar]
- 9. McCarron M, McCallion P, Carroll R, et al. . Health, wellbeing and social inclusion: ageing with an intellectual disability in Ireland Dublin 2017.
- 10. Patja K, Iivanainen M, Vesala H, et al. . Life expectancy of people with intellectual disability: a 35-year follow-up study. J Intellect Disabil Res 2000;44:591–9. 10.1046/j.1365-2788.2000.00280.x [DOI] [PubMed] [Google Scholar]
- 11. Bittles AH, Petterson BA, Sullivan SG, et al. . The influence of intellectual disability on life expectancy. J Gerontol A Biol Sci Med Sci 2002;57:M470–2. 10.1093/gerona/57.7.M470 [DOI] [PubMed] [Google Scholar]
- 12. McCarron M, McCallion P, Reilly E, et al. . A prospective 14-year longitudinal follow-up of dementia in persons with Down syndrome. J Intellect Disabil Res 2014;58:61–70. 10.1111/jir.12074 [DOI] [PubMed] [Google Scholar]
- 13. Broese van Groenou MI, De Boer A. Providing informal care in a changing society. Eur J Ageing 2016;13:271–9. 10.1007/s10433-016-0370-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wiesel I, Bigby C. Movement on shifting sands: deinstitutionalisation and people with intellectual disability in Australia, 1974–2014. Urban Policy Res 2015;33:178–94. 10.1080/08111146.2014.980902 [DOI] [Google Scholar]
- 15. National Disability Authority of Ireland Secondary, 2018. Available: http://nda.ie/
- 16. McCarron M, Lombard-Vance R, Murphy E, et al. . The effect of deinstitutionalisation for adults with intellectual disabilities on quality of life: a systematic review 2018. [DOI] [PMC free article] [PubMed]
- 17. Beecham J, Knapp M, McGilloway S, et al. . The cost-effectiveness of community care for adults with learning disabilities leaving long-stay hospital in Northern Ireland. J Intellect Disabil Res 1997;41:30–41. 10.1111/j.1365-2788.1997.tb00674.x [DOI] [PubMed] [Google Scholar]
- 18. Hallam A, Beecham J, Knapp M, et al. . Service use and costs of support 12 years after leaving hospital. J Appl Res Intellect Disabil 2006;19:296–308. 10.1111/j.1468-3148.2006.00278.x [DOI] [Google Scholar]
- 19. Donnelly M, McGilloway S, Perry S, et al. . Opening new doors: an evaluation of community care for people discharged from psychiatric and mental handicap hospitals. Belfast: Her Majesty's Stationery Office, 1994. [Google Scholar]
- 20. Knapp M, Cambridge P, Thomason C, et al. . Care in the community: challenge and demonstration. Aldershot: Ashgate, 1992. [Google Scholar]
- 21. Cambridge P, Hayes L, Knapp M, et al. . Care in the community: five years on. Aldershot: Ashgate, 1994. [Google Scholar]
- 22. Taylor SJ. The editor's perspective on institutional and community costs. Ment Retard 2003;41:125–6. [DOI] [PubMed] [Google Scholar]
- 23. Felce D. Community living for adults with intellectual disabilities: unravelling the cost effectiveness discourse. J Policy Pract Intellect Disabil 2017;14:187–97. 10.1111/jppi.12180 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-025736supp001.pdf (365.3KB, pdf)


