Abstract
Objective
To evaluate the appropriateness of the initial prescribed daily dose of non-vitamin K antagonist oral anticoagulants (NOACs) according to label in patients with non-valvular atrial fibrillation (NVAF) in the UK.
Design
Population-based cross-sectional study.
Setting
UK primary care.
Population
30 467 patients with NVAF and a first prescription for apixaban, dabigatran or rivaroxaban between January 2011 and December 2016.
Main outcome measures
Percentage of patients prescribed a NOAC dose according to the European Union (EU) labels (appropriately dosed), and not according to the EU labels (inappropriately dosed—including both underdosed and overdosed patients); percentage of patients prescribed an initial NOAC dose according to renal function status.
Results
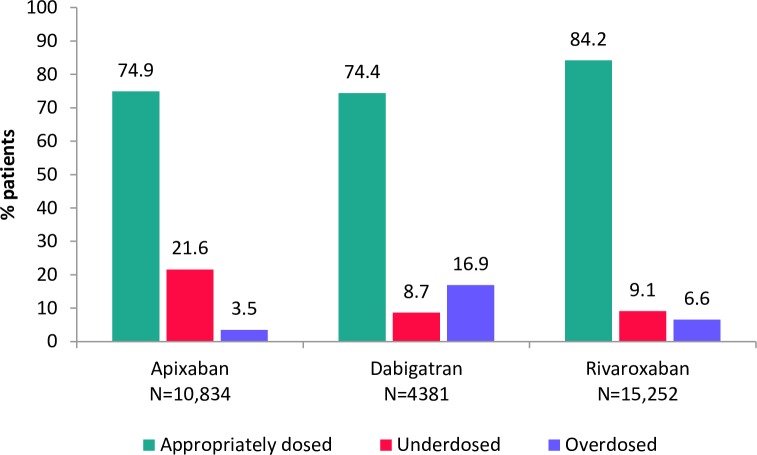
A total of 15 252 (50.1%) patients started NOAC therapy on rivaroxaban, 10 834 (35.6%) on apixaban and 4381 (14.4%) on dabigatran. Among patients starting NOAC therapy on rivaroxaban, 17.3% were eligible to receive a reduced dose compared with 12.8% of patients starting on apixaban and 53.8% of patients starting on dabigatran. The majority of patients were prescribed an appropriate dose according to the EU labels: apixaban 74.9 %, dabigatran, 74.4%; rivaroxaban, 84.2%. Underdosing occurred in 21.6% (apixaban), 8.7% (dabigatran), 9.1% (rivaroxaban). Overdosing was more frequent for dabigatran (16.9%) than for rivaroxaban (6.6%) or apixaban (3.5%). There was a trend towards dose reduction with increasing renal impairment. Among patients with severe renal impairment, the majority received a reduced dose NOAC: apixaban, 91.1%, dabigatran, 80.0%, rivaroxaban, 83.0%.
Conclusion
Between 2011 and 2016, the majority of patients starting NOAC therapy in UK primary care were prescribed a daily dose in line with the approved EU drug label. Underdosing was more than twice as common among patients starting on apixaban than those starting on dabigatran or rivaroxaban. Research into the patient characteristics that may influence inappropriate underdosing of NOACs in UK primary care is warranted.
Keywords: Thromboembolism, Cardiac Epidemiology, EPIDEMIOLOGY
Strengths and limitations of this study.
Our study is the first to comprehensively evaluate the appropriateness of the initial prescribed daily dose of non-vitamin K antagonist oral anticoagulant to patients with non-valvular atrial fibrillation in the UK according to the approved European Union drug labels, and the largest of its kind worldwide.
Our large sample size was derived from two population-based data sources representative of the UK general population, both of which contained data on bodyweight.
A potential limitation of study is that a small degree of misclassification for renal function and bodyweight may have occurred due to inaccuracies in data recording, which may have affected our findings for a small proportion of patients.
Potential overdosing may have been overestimated because patients may have split a prescribed standard dose over >1 day.
Introduction
Recent years have seen a rapid increase in the proportion of patients with atrial fibrillation (AF) starting anticoagulant therapy with a non-vitamin K antagonist oral anticoagulant (NOAC), replacing use of vitamin K antagonists (VKAs) as leading oral anticoagulant (OAC) therapy, both in the UK,1–3 and elsewhere in Europe.4–7 Decisions to prescribe standard or reduced dose NOACs are made on the basis of specific considerations such as age, weight, renal function and use of specific concomitant medications. Descriptive data show that a high proportion of patients with AF initiating anticoagulant therapy with a NOAC are prescribed a reduced dose,4 8–10 particularly in Europe,8 9 with evidence to suggest that many of these patients do not satisfy the necessary dose reduction criteria as specified on the drug labels.10–15 In Europe, studies describing the appropriate dosing of prescribed NOACs have been conducted in smaller cohorts8 12–14 and/or limited to a particular drug,8 14 and we are unaware of any conducted in patients with non-valvular atrial fibrillation (NVAF) in the UK. Therefore, using routinely collected primary care electronic health records (EHRs), we conducted a large population-based study with the aim of evaluating the level of appropriate prescribing (consistency with the approved drug label) of standard and reduced dose NOACs in over 30 000 patients with NVAF initiating therapy with a NOAC between 2011 and 2016. To our knowledge, our study is the largest of its kind among patients with AF in routine clinical practice worldwide.
Methods
Data sources
We used data from The Heath Improvement Network (THIN) and the Clinical Practice Research Datalink (CPRD)-GOLD in the UK—two similarly structured validated databases of anonymised primary care EHRs representative of the UK demographic.16–19 The databases hold clinical and prescribing information entered by general practitioners (GPs) as part of routine patient care, and cover ~5% and 7% of the UK population, respectively. The study protocol was approved by independent Scientific Research Committees (reference SRC 17THIN014 for THIN, and ISAC 17_020R for CPRD). Data collection for THIN was approved by the South East Multicentre Research Ethics Committee in 2003 and individual studies using THIN data do not require separate ethical approval if only anonymised THIN data are used. Similarly, the CPRD has been granted generic ethics approval for individual studies that make use of only anonymised data.
Study population
We identified patients aged ≥18 years with a first recorded prescription (index date) for apixaban, dabigatran or rivaroxaban between 01 January 2011 and 31 December 2016. Patients were required to have been registered with a GP for at least 1 year before their first NOAC prescription and to have at least 1 year prescription history. We subsequently identified patients with NVAF as those with a record of AF any time before the index date or in the 2 weeks after, and with no record of heart valve replacement or mitral stenosis during this time. We excluded patients with a record of deep vein thrombosis, pulmonary embolism or hip/knee replacement surgery in the 3 months before the index date because these could all have been alternative reasons for NOAC initiation. As some practices contribute data to both THIN and CPRD, we included all practices contributing to THIN and those exclusively contributing to CPRD. To identify and exclude duplicated practices, matching of anonymised patient characteristics was applied.20 21
NOAC study cohorts
Three mutually exclusive cohorts were identified based on the first prescribed NOAC (index NOAC) for stroke prevention in AF, either dabigatran (a direct thrombin inhibitor), apixaban or rivaroxaban (both direct factor Xa inhibitors). Edoxaban—another direct factor Xa inhibitor—was only relatively recently approved by the EMA and recommended by NICE (June and September 2015, respectively), therefore we anticipated prescribing levels would not be sufficiently high for robust analysis and thus excluded new users of edoxaban. Identification of the study cohorts is depicted in (online supplementary figure 1). Patients who were prescribed two different NOACs on the same day were excluded. Patients qualifying as a new user of more than one NOAC during the study period with different index dates (ie, switchers), were assigned to the cohort of the first prescribed NOAC. Patients were categorised as OAC non-naïve if they had a prescription for any OAC before their index NOAC (or a clinical entry implying previous use of any OAC, warfarin monitoring or international normalised ratio >2), otherwise they were considered to be OAC-naive.
bmjopen-2019-031341supp001.pdf (71.7KB, pdf)
Renal function and other patient characteristics
We calculated the daily dose of the index NOAC based on the product instructions (quantity, pack size, number of tablets and posology) for the first recorded NOAC prescription. We also extracted information on patients’ age, renal function and weight at the time of the index date, using the most recently recorded values. Patients’ renal function was ascertained using the closest valid serum creatinine value to the index date (within the year before) to calculate an estimated glomerular filtration rate (eGFR) expressed as mL/min/1.73 m2 applying the Chronic Kidney Disease Epidemiology Collaboration equation,22 but omitting ethnicity because this is not routinely recorded in UK primary care. Individuals with no valid serum creatinine measurement were assigned to a category ‘unknown’. Information on lifestyle variables (smoking status and body mass index) was collected using the most recently recorded value/status before the index date. CHA2DS2Vasc score for stroke risk was calculated according to patients’ recorded history of congestive heart failure, hypertension, age, diabetes mellitus and prior stroke/transient ischaemic attack (CHADS score was also calculated because this was assessed in the pivotal studies for the NOACs investigated in this study). HAS-BLED score for major bleeding risk was calculated using recorded history of hypertension, renal disease, liver disease, stroke history, major bleeding or predisposition to bleeding, age >65 years, medication use predisposing to bleeding and alcohol use. We also estimated frailty using an adaptation of a frailty index developed from data recorded in primary care databases,23 and categorised patients as fit, mildly frail, moderately frail or severely frail.
Recommendations for NOAC dosing
We categorised patients as eligible for standard or reduced dose NOAC therapy or ineligible for NOAC therapy (ie, contraindicated) based on all information in the approved European Union (EU) label for each respective NOAC, adapted to the information recorded in the databases (online supplementary table 1). For the prevention of stroke and systemic embolism in adults with NVAF, the recommended standard dosages according to the EU labels are 5 mg two times per day for apixaban, 150 mg two times per day for dabigatran and 20 mg once per day for rivaroxaban; the recommended reduced dosages are 2.5 mg two times per day for apixaban, 110 mg two times per day for dabigatran and 15 mg once per day for rivaroxaban. Hereafter, for simplicity, we refer to these dosages as ‘daily dose’. Dose reduction recommendations for rivaroxaban are based on renal function, while dose reduction for dabigatran considers renal function, age, concomitant medications and other comorbidities. For apixaban, at least two of the following criteria are to be met for dose reduction: ≥80 years, body weight ≤60 kg and serum creatinine ≥1.5 mg/dL. Also, patients with renal impairment creatinine clearance 15–29 mL/min patients are recommended to receive the reduced dose of apixaban. We therefore defined appropriate dosing as a patient being prescribed the correct recommended dose based on the approved EU label. Potential inappropriate dosing was defined as a patient being prescribed a dose not in line with the EU label—this included both underdosed patients (prescribing of a reduced dose NOAC to patients eligible for a standard dose) and overdosed patients (prescribing of a higher dose than recommended or any dose when contraindicated).
bmjopen-2019-031341supp003.pdf (103.5KB, pdf)
Statistical analysis
Patient characteristics were described according to the daily dose of the index NOAC (standard or reduced), using frequency counts and percentages for quantitative variables, and means with SD for continuous variables. For each NOAC cohort, we calculated the percentage of patients appropriately dosed, both overall and according to whether the daily dose of the index NOAC was a standard or reduced dose. For this calculation, patients with missing data on renal function were assumed to have normal renal function, and those with missing data on weight (when analysing apixaban dosing) were assumed to have a weight above 60 kg. To determine if NOAC prescription patterns were influenced by renal status alone, we further evaluated the initial daily dose prescribed according to renal function, categorised as normal (eGFR >50 mL/min/1.73 m2), mild-to-moderate impairment (eGFR 30–50 mL/min/1.73 m2) and severe impairment (eGFR <30 mL/min/1.73 m2). All analyses were undertaken using STATA V.12.0.
Patient and public involvement
This was a descriptive study using routinely collected primary care data in the UK. There was no public or patient involvement in the conception of the research question, the design and implementation of the study, or the writing of the manuscript.
Results
During the study period, there were a total of 30 467 new users of a NOAC with a record of NVAF and no other recent indication for anticoagulation; 10 834 (35.6%) started on apixaban, 4381 (14.4%) started on dabigatran and 15 252 (50.1%) started on rivaroxaban.
Patient characteristics by daily dose at index NOAC prescription
Characteristics of the study cohorts stratified by the total daily dose of the index NOAC prescription (standard or reduced) are shown in table 1, and the frequency distribution of the daily dose of the index NOAC prescription is shown in online supplementary table 2.
Table 1.
Baseline characteristics of the cohort of 30 467 new users of NOACs with NVAF and no other recent indication, stratified by dose of first NOAC prescription (standard or reduced dose)
| Apixaban (n=10 834) | Dabigatran (n=4381) | Rivaroxaban (n=15 252)* | ||||
| Standard dose (n=7061; 65.2%) |
Reduced dose (n=3773; 34.8%) |
Standard dose (n=2018; 46.1%) |
Reduced dose (n=2363; 53.9%) |
Standard dose (n=12 091; 79.3%) |
Reduced dose (n=3081; 20.2%) |
|
| Sex | ||||||
| Male | 4271 (60.5) | 1488 (39.4) | 1380 (68.4) | 1143 (48.4) | 7042 (58.2) | 1289 (41.8) |
| Female | 2790 (39.5) | 2285 (60.6) | 638 (31.6) | 1220 (51.6) | 5049 (41.8) | 1792 (58.2) |
| Age (years) | ||||||
| <60 | 833 (11.8) | 63 (1.7) | 380 (18.8) | 73 (3.1) | 1233 (10.2) | 66 (2.1) |
| 60–69 | 1903 (27.0) | 177 (4.7) | 726 (36.0) | 202 (8.5) | 2696 (22.3) | 199 (6.5) |
| 70–79 | 2860 (40.5) | 676 (17.9) | 842 (41.7) | 699 (29.6) | 4400 (36.4) | 715 (23.2) |
| ≥80 | 1465 (20.7) | 2857 (75.7) | 70 (3.5) | 1389 (58.8) | 3762 (31.1) | 2101 (68.2) |
| Mean age (SD) | 71.4 (10.2) | 82.8 (7.8) | 67.2 (9.1) | 79.7 (8.5) | 73.6 (10.6) | 81.8 (8.5) |
| OAC naïve status | ||||||
| Naïve | 3915 (55.4) | 1859 (49.3) | 909 (45.0) | 918 (38.8) | 5881 (48.6) | 1295 (42.0) |
| Non-naïve | 3146 (44.6) | 1914 (50.7) | 1109 (55.0) | 1445 (61.2) | 6210 (51.4) | 1786 (58.0) |
| Year of first NOAC prescription | ||||||
| 2011–2013 | 184 (2.6) | 107 (2.8) | 968 (48.0) | 1206 (51.0) | 1492 (12.3) | 479 (15.5) |
| 2014–2016 | 6877 (97.4) | 3666 (97.2) | 1050 (52.0) | 1157 (49.0) | 10 599 (87.7) | 2602 (84.5) |
| BMI | ||||||
| 10–19 (underweight) | 117 (1.7) | 331 (8.8) | 35 (1.7) | 139 (5.9) | 434 (3.6) | 212 (6.9) |
| 20–24 (healthy weight) | 1322 (18.7) | 1201 (31.8) | 343 (17.0) | 665 (28.1) | 2679 (22.2) | 875 (28.4) |
| 25–29 (overweight) | 2599 (36.8) | 1228 (32.5) | 735 (36.4) | 866 (36.6) | 4230 (35.0) | 1035 (33.6) |
| ≥30 (obese) | 2766 (39.2) | 836 (22.2) | 809 (40.1) | 593 (25.1) | 4291 (35.5) | 847 (27.5) |
| Unknown | 257 (3.6) | 177 (4.7) | 96 (4.8) | 100 (4.2) | 457 (3.8) | 112 (3.6) |
| Smoking | ||||||
| Non-smoker | 2851 (40.4) | 1683 (44.6) | 784 (38.9) | 1015 (43.0) | 4876 (40.3) | 1282 (41.6) |
| Smoker | 605 (8.6) | 221 (5.9) | 178 (8.8) | 126 (5.3) | 1015 (8.4) | 182 (5.9) |
| Ex-smoker | 3598 (51.0) | 1865 (49.4) | 1052 (52.1) | 1221 (51.7) | 6190 (51.2) | 1617 (52.5) |
| Unknown | 7 (0.1) | 4 (0.1) | 4 (0.2) | 1 (0.0) | 10 (0.1) | 0 (0.0) |
| Alcohol (units/week) | ||||||
| None | 1356 (19.2) | 1129 (29.9) | 244 (12.1) | 526 (22.3) | 2244 (18.6) | 827 (26.8) |
| 1–9 | 3044 (43.1) | 1663 (44.1) | 857 (42.5) | 1128 (47.7) | 5501 (45.5) | 1448 (47.0) |
| 10–20 | 1316 (18.6) | 390 (10.3) | 422 (20.9) | 315 (13.3) | 1975 (16.3) | 316 (10.3) |
| 21–41 | 470 (6.7) | 128 (3.4) | 219 (10.9) | 99 (4.2) | 821 (6.8) | 95 (3.1) |
| ≥42 | 227 (3.2) | 48 (1.3) | 92 (4.6) | 45 (1.9) | 354 (2.9) | 50 (1.6) |
| Unknown | 648 (9.2) | 415 (11.0) | 184 (9.1) | 250 (10.6) | 1196 (9.9) | 345 (11.2) |
| History of CVD | ||||||
| IHD | 1939 (27.5) | 1309 (34.7) | 416 (20.6) | 735 (31.1) | 3014 (24.9) | 1098 (35.6) |
| Heart failure | 1080 (15.3) | 847 (22.4) | 268 (13.3) | 469 (19.8) | 1709 (14.1) | 791 (25.7) |
| Hypertension | 4464 (63.2) | 2762 (73.2) | 1192 (59.1) | 1691 (71.6) | 7888 (65.2) | 2338 (75.9) |
| Ischaemic stroke | 990 (14.0) | 774 (20.5) | 254 (12.6) | 435 (18.4) | 1567 (13.0) | 553 (17.9) |
| History of bleeding disorders | ||||||
| Intracranial bleeding | 96 (1.4) | 108 (2.9) | 20 (1.0) | 51 (2.2) | 139 (1.1) | 52 (1.7) |
| GI bleeding | 957 (13.6) | 573 (15.2) | 232 (11.5) | 349 (14.8) | 1609 (13.3) | 440 (14.3) |
| Urogenital bleeding | 877 (12.4) | 517 (13.7) | 214 (10.6) | 309 (13.1) | 1629 (13.5) | 449 (14.6) |
| eGFR (CKD-EPI) /min/1.73 m2 | ||||||
| >50 | 5323 (75.4) | 1968 (52.2) | 1625 (80.5) | 1634 (69.1) | 9547 (79.0) | 1105 (35.9) |
| 30–50 | 694 (9.8) | 1125 (29.8) | 110 (5.5) | 464 (19.6) | 892 (7.4) | 1475 (47.9) |
| <30 | 25 (0.4) | 255 (6.8) | 4 (0.2) | 16 (0.7) | 46 (0.4) | 223 (7.2) |
| Unknown | 1019 (14.4) | 425 (11.3) | 279 (13.8) | 249 (10.5) | 1606 (13.3) | 278 (9.0) |
| Frailty index | ||||||
| Fit | 1306 (18.5) | 191 (5.1) | 517 (25.6) | 201 (8.5) | 2120 (17.5) | 133 (4.3) |
| Mild frailty | 2839 (40.2) | 933 (24.7) | 918 (45.5) | 706 (29.9) | 4624 (38.2) | 668 (21.7) |
| Moderate frailty | 1978 (28.0) | 1395 (37.0) | 448 (22.2) | 833 (35.3) | 3522 (29.1) | 1182 (38.4) |
| Severe frailty | 938 (13.3) | 1254 (33.2) | 135 (6.7) | 623 (26.4) | 1825 (15.1) | 1098 (35.6) |
| CHA2DS2VASc score | ||||||
| 0 | 42 (6.0) | 25 (0.7) | 220 (10.9) | 32 (1.4) | 608 (5.0) | 23 (0.7) |
| 1 | 675 (9.6) | 52 (1.4) | 260 (12.9) | 76 (3.2) | 1107 (9.2) | 68 (2.2) |
| 2 | 1425 (20.2) | 252 (6.7) | 517 (25.6) | 222 (9.4) | 2182 (18.0) | 199 (6.5) |
| 3 | 1564 (22.1) | 623 (16.5) | 418 (20.7) | 475 (20.1) | 2681 (22.2) | 507 (16.5) |
| ≥4 | 2971 (42.1) | 2821 (74.8) | 603 (29.9) | 1558 (65.9) | 5513 (45.6) | 2284 (74.1) |
| Mean (SD) | 3.2 (1.8) | 4.6 (1.6) | 2.7 (1.7) | 4.2 (1.7) | 3.4 (1.8) | 4.6 (1.6) |
| CHADS score | ||||||
| 0 | 1127 (16.0) | 103 (2.7) | 480 (23.8) | 114 (4.8) | 1696 (14.0) | 103 (3.3) |
| 1 | 2119 (30.0) | 595 (15.8) | 681 (33.7) | 448 (19.0) | 3440 (28.5) | 452 (14.7) |
| 2 | 1929 (27.3) | 1259 (33.4) | 468 (23.2) | 786 (33.3) | 3596 (29.7) | 1044 (33.9) |
| ≥3 | 1886 (26.7) | 1816 (48.1) | 389 (19.3) | 1015 (43.0) | 3359 (27.8) | 1482 (48.1) |
| Mean (SD) | 1.8 (1.3) | 2.6 (1.3) | 1.5 (1.2) | 1.9 (1.3) | 1.9 (1.3) | 2.6 (1.3) |
| HAS-BLED score | ||||||
| 0 | 814 (11.5) | 46 (1.2) | 312 (15.5) | 49 (2.1) | 1224 (10.1) | 54 (1.8) |
| 1 | 2437 (34.5) | 1163 (30.8) | 704 (34.9) | 721 (30.5) | 4460 (36.9) | 938 (30.4) |
| 2 | 2510 (35.5) | 1514 (40.1) | 699 (34.6) | 1005 (42.5) | 4467 (36.9) | 1305 (42.4) |
| 3 | 1089 (15.4) | 789 (20.9) | 263 (13.0) | 470 (19.9) | 1612 (13.3) | 596 (19.3) |
| ≥4 | 211 (3.0) | 261 (6.9) | 40 (2.0) | 118 (5.0) | 328 (2.7) | 188 (6.1) |
| Mean (SD) | 1.6 (1.0) | 2.0 (1.0) | 1.6 (0.9) | 2.0 (0.9) | 1.6 (0.9) | 2.0 (0.9) |
| Medications† | ||||||
| Antiplatelets | 3250 (46.0) | 1844 (48.9) | 993 (49.2) | 1285 (54.4) | 5299 (43.8) | 1519 (49.3) |
| Antiarrhythmics | 1074 (15.2) | 467 (12.4) | 403 (20.0) | 425 (18.0) | 1764 (14.6) | 403 (13.1) |
| Antihypertensives | 6114 (86.6) | 3400 (90.1) | 1743 (86.4) | 2147 (90.9) | 10 591 (87.6) | 2860 (92.8) |
*80 patients starting therapy on rivaroxaban were prescribed an initial daily dose higher than standard daily dose (>20 mg/day) and are not included in the table.
†Prescription in the year before the first NOAC prescription.
BMI, body mass index; CKD-EPI, chronic kidney disease epidemiology; CVD, cardiovascular disease; eGFR, estimated glomerular filtration rate; GI, gastrointestinal; IHD, ischaemic heart disease; NOACs, non-vitamin K antagonist oral anticoagulants; NVAF, non-valvular atrial fibrillation.
bmjopen-2019-031341supp004.pdf (70KB, pdf)
A reduced NOAC dose was prescribed in the majority of patients with impaired renal function. Among patients receiving a standard dose, the apixaban cohort had the highest proportion of OAC-naïve patients (55.4% vs 45% for dabigatran and 48.6% for rivaroxaban). Most patients prescribed a standard dose had normal renal function. Among patients prescribed a reduced dose NOAC, the majority were aged 70 years or older and were moderately or severely frail. Bleeding risk (according to the HAS-BLED score) was similar between the three cohorts, and was higher among patients prescribed reduced NOAC doses (mean 2.0, SD 0.9) than among patients receiving standard doses (mean 1.6; SD 0.9). Approximately three-quarters of the patients in each cohort who were prescribed a reduced dose had a high stroke risk index (CHA2DS2VASc score of ≥4).
Overall appropriateness of index NOAC daily dose
Characteristics of patients appropriately or inappropriately dosed in accordance with the drug label can be found in online supplementary table 3. The percentage of patients appropriately dosed, underdosed and overdosed among all patients in each study cohort is shown in figure 1. The majority of patients (76.9%) starting NOAC therapy were prescribed an appropriate dose; 74.9% of patients on apixaban, 74.4% on dabigatran and 84.2% on rivaroxaban. Underdosing was more frequent in the apixaban cohort (21.6% of patients) than in the dabigatran (8.7% of patients) and rivaroxaban (9.1%) cohorts. Overdosing was more frequent in the dabigatran cohort (16.9%) than in the rivaroxaban (6.6%) or apixaban (3.5%) cohorts. Little difference was seen in the level of appropriate prescribing when analyses were stratified by whether patients had previously been prescribed a VKA (non-naïve) or not (naïve) (online supplementary table 4A–4D).
Figure 1.
Overall appropriateness of index NOAC daily dose (first prescribed NOAC). Overdosed includes patients who received a higher dose than recommended plus patients who were contraindicated. NOAC, non-vitamin K antagonist oral anticoagulant.
bmjopen-2019-031341supp005.pdf (94KB, pdf)
bmjopen-2019-031341supp006.pdf (63KB, pdf)
Appropriateness of NOAC prescription by eligibility to receive a standard or reduced dose
As shown in table 2, the majority of patients in the apixaban and rivaroxaban cohorts were eligible to receive the standard treatment dose, 84.9% (9194/10 834) for apixaban and 82.7% (12 608/15 252) for rivaroxaban, while in the dabigatran cohort less than half (40.9%; 1790/4381) were eligible for the standard dose. The percentage of users eligible to receive the reduced treatment dose was 12.8% for apixaban, 53.8% for dabigatran and 17.3% for rivaroxaban. Among all patients eligible to receive a standard dose NOAC (n=23 591), the majority received the correct standard dose (82.3%); this percentage was highest for rivaroxaban (88.5%) followed by dabigatran (78.7%) and apixaban (74.5%). However, a quarter of apixaban patients (25.5%, 2344/9194) eligible to receive the recommended standard daily dose were prescribed a reduced dose, compared with 21.3% (381/1790) in the dabigatran cohort and 11.0% (1390/12 608) in the rivaroxaban cohort. Among patients inappropriately prescribed a reduced dose of apixaban (n=2344), 73.1% met only one of the dose-reduction criteria with the remaining meeting no dose-reduction criteria. Among patients eligible for reduced dosing, the majority correctly received a reduced dose: apixaban (91.0%), dabigatran (78.4%) and rivaroxaban (63.9%).
Table 2.
Prescribing of recommended daily dose of index NOAC (first NOAC prescription) by eligibility according to the EU label
| Daily dose of index NOAC prescribed | Dosing eligibility | |||
| Standard dose | Reduced dose | Contraindicated | Total (overall eligibility) |
|
| Apixaban | n=9194 | n=1385 | n=255 | n=10 834 |
| Recommended | 6850 (74.5) | 1260 (91.0) | NA | 8110 (74.9) |
| Lower than recommended | 2344 (25.5) | 0 (0) | NA | 2344 (21.6) |
| Higher than recommended | 0 (0) | 125 (9.0) | NA | 125 (1.1) |
| Prescribed a NOAC when contraindicated | NA | NA | 255 (100) | 255 (2.4) |
| Dabigatran | n=1790 | n=2357 | n=234 | n=4381 |
| Recommended | 1409 (78.7) | 1849 (78.4) | NA | 3258 (74.4) |
| Lower than recommended | 381 (21.3) | 0 (0) | NA | 381 (8.7) |
| Higher than recommended | 0 (0) | 508 (21.6) | NA | 508 (11.6) |
| Prescribed a NOAC when contraindicated | NA | NA | 234 (100) | 234 (5.3) |
| Rivaroxaban | n=12 607 | n=2638 | n=7 | n=15 252 |
| Recommended | 11 162 (88.5) | 1687 (63.9) | NA | 12 849 (84.2) |
| Lower than recommended | 1389 (11.0) | 0 (0) | NA | 1389 (9.1) |
| Higher than recommended | 56 (0.40) | 951 (36.1) | NA | 1007 (6.6) |
| Prescribed a NOAC when contraindicated | NA | NA | 7 (100) | 7 (0.05) |
Data are n (column %).
EU, European Union; NOAC, non-vitamin K antagonist oral anticoagulant.
Appropriateness of NOAC prescription among patients prescribed a standard or reduced dose
Among patients starting NOAC therapy on a standard daily dose, the prescription was appropriate for the vast majority of those in the apixaban cohort (97.0%) and rivaroxaban cohort (92.3%), but for fewer patients in the dabigatran cohort (69.8%) (online supplementary figure 2). Among patients starting NOAC therapy on a reduced dose, this was appropriate in only 33.4% of patients in the apixaban cohort compared with 78.2% of the dabigatran cohort and 54.7% of the rivaroxaban cohort (online supplementary figure 2).
bmjopen-2019-031341supp002.pdf (72.1KB, pdf)
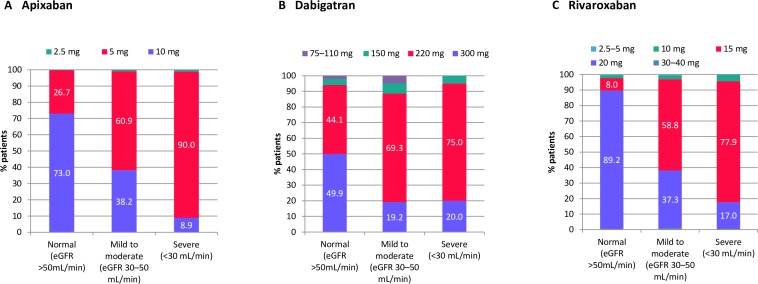
Dosing by degree of renal impairment
The daily dose of the index NOAC prescription according to renal function is shown in figure 2 (approximately one in eight patients in each cohort had unknown renal function). In all three cohorts, there was a trend towards dose reduction with increasing renal impairment. Among patients with severe renal impairment (eGFR <30 mL/min /1.73 m2), most were prescribed a reduced daily dose: apixaban (91.1%, ≤5 mg), dabigatran (80.0%, ≤200 mg) and rivaroxaban (83.0%, 15 mg). However, reduced doses were also prescribed to patients with no evidence of renal impairment, especially among the dabigatran cohort (50.1%, 1634/3259; mostly 220 mg/day) followed by apixaban (26.7% (1968/7291; nearly all 5 mg/day), and least frequently for rivaroxaban (10.3%, 1105/10 699; mostly 15 mg/day) users.
Figure 2.
Daily dose of the index NOAC prescription by degree of renal impairment* for (A) new users of apixaban, (B) new users of dabigatran and (C) new users of rivaroxaban, in patients with NVAF and no other recent indication. Renal function was unknown in 13.6% of the apixaban cohort, 12.3% of the dabigatran cohort and 13.0% of the rivaroxaban cohort. *Estimated using the chronic kidney disease epidemiology collaboration equation. eGFR, estimated glomerular filtration rate; NOAC, non-vitamin K antagonist oral anticoagulant; NVAF, non-valvular atrial fibrillation.
NOAC daily dose over time
As shown in online supplementary table 5, among patients with at least 6 months of follow-up and a continuous user of a NOAC at 6 months (ie, no gaps of >30 days between the end of supply of one prescription and the start of the next), the vast majority were prescribed the same dose of the index NOAC at 6 months (95.4% for apixaban, 93.7% for dabigatran and 94.5% for rivaroxaban). Among patients whose were underdosed at the index date and who also had at least 6 months of follow-up, the majority still received an underdosed prescription 6 months after their initial underdosed prescription: apixaban 90.2%, dabigatran 82.0% and rivaroxaban 84.6%. Baseline doses of the index NOAC among patients who were, or who were not, continuous users of a NOAC at 6 months are shown in online supplementary table 6.
bmjopen-2019-031341supp007.pdf (72.5KB, pdf)
bmjopen-2019-031341supp008.pdf (66.9KB, pdf)
Discussion
Between 2011 and 2016, the majority of patients with NVAF starting therapy with a NOAC in UK primary care were prescribed an appropriate daily dose based on the approved EU label, according to the information recorded in THIN and CPRD-GOLD. However, notable differences were seen in the level of underdosing between individual NOACs, being more than twice as frequent among patients starting treatment on apixaban compared with those starting on dabigatran or rivaroxaban.
Our study is the first to comprehensively evaluate the appropriateness of the initial prescribed daily dose of NOACs to patients with NVAF in the UK according to the approved EU drug labels, and the largest of its kind worldwide. Also, few other studies have compared levels of potential underdosing and overdosing between individual NOACs. The large sample from two population-based data sources representative of the UK general population is a key strength, as is the fact that all medications prescribed by the GP will have been captured because they are automatically recorded on issue. Another strength is that, unlike other healthcare databases, THIN and CPRD-GOLD contain data on all criteria, including bodyweight, required to make an accurate assessment of appropriate NOAC dosing. In terms of our study’s limitations, we evaluated the dose of the first NOAC prescription issued in primary care and not subsequent prescriptions; however, the majority of patients had continued on the same dose of the index NOAC 6 months after treatment initiation. Additionally, although the very first NOAC prescription may have been issued in secondary care and this will not have been captured in the primary care databases, we believe it is unlikely that the first NOAC prescription issued in primary care would be a different dose to that issued by a specialist with the relevant expertise. A small degree of misclassification for renal function and bodyweight may have occurred due to inaccuracies in data recording, which may have affected our findings for a small proportion of patients. Also, potential overdosing may have been overestimated because patients may have split a prescribed standard dose over >1 day, and likewise potential underdosing may have occurred if patients were instructed to spread out their prescribed medication, although we feel this is unlikely.
Potential underdosing of NOACs has been reported in moderate-to-large studies from the USA,10 11 as well as in smaller studies from Europe, North America12–14 and Israel,15 with findings indicative of variation in the level of inappropriate NOAC dosing between countries. Using data from 7925 patients with AF in the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation II (ORBIT-AF-II) registry, Steinberg et al,10 reported that 57% (734/1289) of patients prescribed a reduced dose NOAC did not fulfil the Food and Drug Administration’s (FDAs) recommended criteria for dose reduction. A larger administrative claims database study of 14 865 patients with AF initiating NOAC treatment reported a much lower level of underdosing with 13.3% (1781/13 392) of patients with no renal indication for dose reduction receiving a reduced dose11; although other criteria for dose reduction were not assessed. A large administrative healthcare database study in Israel reported very high levels of inappropriate prescribing of low-dose NOACs, occurring in 84% of patients prescribed reduced dose dabigatran, 68% of those prescribed reduced dosed apixaban and 78.5% of those prescribed reduced dose rivaroxaban. It is unclear what factors might underlie the marked difference in findings between studies yet it is clear that inappropriate underdosing is not uncommon. In our analyses, the percentage of patients receiving a reduced dose differed between the individual NOACs, occurring more than twice as frequently among patients prescribed apixaban or dabigatran than those prescribed rivaroxaban. One can speculate that this finding may reflect the criteria for dose reduction for the former two NOACs with respect to apixaban and dabigatran, although it was not possible to substantiate this with the current study design. Studies from Europe have been small but also suggest that underdosing may be more prevalent for apixaban than rivaroxaban. In Germany, Bucholtz et al 8 found that among 268 patients with NVAF starting reduced dose apixaban therapy in 2016, 60.8% did not meet labelling criteria for dose reduction, while in a study of 899 patients with NVAF starting rivaroxaban therapy in the Netherlands, Pisters et al 14 reported that 3.1% received a label-discordant dose. In the USA, Yao et al 11 found that 43% of patients with a renal indication for NOAC dose reduction did not receive a reduced dose, while Steinberg et al 10 found that 32% of NVAF patients eligible for dose reduction according to the FDA approved drug labels received a standard dose NOAC. This is similar to the level of potential rivaroxaban overdosing in our study. Whether differences in levels of inappropriate prescribing between studies relates to differences between study populations or completeness of data in the information sources is unclear, but patients in our study were on average 4 years older than those in the ORBIT-AF-II registry (75 vs 71 years) and previous gastrointestinal bleeding was more frequent (14% vs 4%).
Inappropriate dosing of NOACs has concerning clinical implications because patients may not receive the benefits of the recommended NOAC dose in protecting against stroke and systemic embolism. Data from the ORBIT-AF-II registry suggest that patients receiving an inappropriately reduced NOAC dose have less favourable outcomes in terms of thromboembolic events and death.10 Yao et al 11 found that among apixaban-treated patients with no renal justification for dose reduction, those receiving the reduced dose had a significantly higher risk of stroke with no significant change in the risk of bleeding when compared with those receiving the standard dose. Reasons why GPs prescribe reduced NOAC doses to patients with no justification for dose reduction are unclear. It is possible that NOAC-related bleeding may be more concerning to physicians than reduced stroke prophylaxis. Although, contrary to expectations, Steinberg et al 10 found that patients inappropriately prescribed a reduced dose of a NOAC were significantly younger and had lower bleeding scores than those appropriately dose reduced. In our study, we saw a trend of dose reduction with worsening renal function. In addition, the majority of patients started on a reduced dose NOAC were moderately or severely frail. It is therefore possible that some GPs are exercising caution among patients with renal function values close to the qualifying cut-offs and/or among frail individuals. For apixaban, being close to the cut-offs for age and bodyweight could also influence prescribing In the study by Bucholtz et al 8 there were 163 apixaban patients who received a reduced dose despite being eligible for the higher dose, and among these a substantial percentage met either only one (57.1%) or no (42.9%) dose-reduction criteria, with these patients more often having ages, weights and serum creatinine levels close to the cut-off values compared with patients prescribed an appropriate dose. In our study, the majority (73.1%) of patients inappropriately prescribed a reduced dose of apixaban met only one dose reduction criteria. Our findings also pointed to some potential overdosing of NOACs, which has been shown by others to increase bleeding risk.11 Notwithstanding our study’s limitation in assessing overdosing, the possibility of overdosing prescribing habits among some UK GPs cannot be excluded.
Our findings underscore the importance of monitoring the prescribing of NOACs in the postmarketing period. Research is warranted into reasons for the inappropriate prescribing of reduced and standard dose NOACs in UK primary care, and the patient characteristics that may influence this. Additionally, research is needed into the impact that inappropriate dosing of NOACs has on risks of clinical outcomes, including stroke, systemic embolism and major bleeding in this setting, and ways to improve levels of correct dosing to ensure patients receive maximum benefit from treatment.
Supplementary Material
Acknowledgments
We thank Susan Bromley, EpiMed Communications Ltd (Oxford, UK) for medical writing assistance funded by Bayer AG.
Footnotes
Contributors: LR and SF developed the concept for the research study. LR, SF, LAGR, AR, GB, PV, KS-W and YB planned the study. AR, MM-P and LAGR conducted the study. All authors (LAGR, AR, MM-P, LR, SF, GB, PV, KS-W, YB and BS) interpreted the data, reviewed drafts of the manuscript and approved the final version of the article for publication.
Funding: This work was supported by BAG.
Competing interests: PV, YB, KS-W and BS are employees of Bayer AG (Germany), the funder of the study. GB is an employee of Bayer AB (Stockholm, Sweden). LR and SF are employees of Bayer PLC (Reading, UK). KS-W declares Bayer stocks. LR and SF declare shares in Bayer. LAGR, MM-P and AR work for the Spanish Centre for Pharmacoepidemiologic Research (Madrid, Spain), which has received research funding from Bayer AG. LAGR also declares honoraria for serving on advisory boards for Bayer AG.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available from the corresponding author following reasonable request.
References
- 1. Loo SY, Dell’Aniello S, Huiart L, et al. . Trends in the prescription of novel oral anticoagulants in UK primary care. Br J Clin Pharmacol 2017;83:2096–106. 10.1111/bcp.13299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ruigomez A, Brobert G, Vora P, et al. . Trends in use of rivaroxaban for prophylaxis and treatment in general practice in the United Kingdom between 2012 and 2015. Pharmacoepidemiol Drug Saf 2018;27. [Google Scholar]
- 3. Vinogradova Y, Coupland C, Hill T, et al. . Risks and benefits of direct oral anticoagulants versus warfarin in a real world setting: cohort study in primary care. BMJ 2018;362 10.1136/bmj.k2505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fay MR, Martins JL, Czekay B. Oral anticoagulant prescribing patterns for stroke prevention in atrial fibrillation among general practitioners and cardiologists in three European countries. Eur Heart J 2016;37(Abstract Supplement):510.26726043 [Google Scholar]
- 5. Schuh T, Reichardt B, Finsterer J, et al. . Age-dependency of prescribing patterns of oral anticoagulant drugs in Austria during 2011-2014. J Thromb Thrombolysis 2016;42:447–51. 10.1007/s11239-016-1380-1 [DOI] [PubMed] [Google Scholar]
- 6. Olesen JB, Sørensen R, Hansen ML, et al. . Non-vitamin K antagonist oral anticoagulation agents in anticoagulant naïve atrial fibrillation patients: Danish nationwide descriptive data 2011-2013. Europace 2015;17:187–93. 10.1093/europace/euu225 [DOI] [PubMed] [Google Scholar]
- 7. Kjerpeseth LJ, Ellekjær H, Selmer R, et al. . Trends in use of warfarin and direct oral anticoagulants in atrial fibrillation in Norway, 2010 to 2015. Eur J Clin Pharmacol 2017;73:1417–25. 10.1007/s00228-017-2296-1 [DOI] [PubMed] [Google Scholar]
- 8. Buchholz A, Ueberham L, Gorczynska K, et al. . Initial apixaban dosing in patients with atrial fibrillation. Clin Cardiol 2018;41:671–6. 10.1002/clc.22949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Staerk L, Gerds TA, Lip GYH, et al. . Standard and reduced doses of dabigatran, rivaroxaban and apixaban for stroke prevention in atrial fibrillation: a nationwide cohort study. J Intern Med 2018;283:45–55. 10.1111/joim.12683 [DOI] [PubMed] [Google Scholar]
- 10. Steinberg BA, Shrader P, Pieper K, et al. . Frequency and outcomes of reduced dose non-vitamin K antagonist anticoagulants: results from ORBIT-AF II (the outcomes Registry for better informed treatment of atrial fibrillation II). J Am Heart Assoc 2018;7 10.1161/JAHA.117.007633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yao X, Shah ND, Sangaralingham LR, et al. . Non-Vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction. J Am Coll Cardiol 2017;69:2779–90. 10.1016/j.jacc.2017.03.600 [DOI] [PubMed] [Google Scholar]
- 12. Barra ME, Fanikos J, Connors JM, et al. . Evaluation of Dose-Reduced direct oral anticoagulant therapy. Am J Med 2016;129:1198–204. 10.1016/j.amjmed.2016.05.041 [DOI] [PubMed] [Google Scholar]
- 13. Lavoie K, Turgeon M-H, Brais C, et al. . Inappropriate dosing of direct oral anticoagulants in patients with atrial fibrillation. J Atr Fibrillation 2016;9:1478 10.4022/jafib.1478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pisters R, van Vugt SPG, Brouwer MA, et al. . Real-life use of Rivaroxaban in the Netherlands: data from the Xarelto for Prevention of Stroke in Patients with Atrial Fibrillation (XANTUS) registry. Neth Heart J 2017;25:551–8. 10.1007/s12471-017-1009-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ellis MH, Dotan SG, Hammerman A, et al. . Appropriateness of non-vitamin K antagonist oral anticoagulant dose in patients with atrial fibrillation in Israel: a population-based study. Thromb Res 2018;169:140–2. 10.1016/j.thromres.2018.07.024 [DOI] [PubMed] [Google Scholar]
- 16. Blak BT, Thompson M, Dattani H, et al. . Generalisability of the health improvement network (thin) database: demographics, chronic disease prevalence and mortality rates. Inform Prim Care 2011;19:251–5. 10.14236/jhi.v19i4.820 [DOI] [PubMed] [Google Scholar]
- 17. Herrett E, Gallagher AM, Bhaskaran K, et al. . Data resource profile: clinical practice research Datalink (CPRD). Int J Epidemiol 2015;44:827–36. 10.1093/ije/dyv098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Herrett E, Thomas SL, Schoonen WM, et al. . Validation and validity of diagnoses in the general practice research database: a systematic review. Br J Clin Pharmacol 2010;69:4–14. 10.1111/j.1365-2125.2009.03537.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lewis JD, Schinnar R, Bilker WB, et al. . Validation studies of the health improvement network (thin) database for pharmacoepidemiology research. Pharmacoepidemiol Drug Saf 2007;16:393–401. 10.1002/pds.1335 [DOI] [PubMed] [Google Scholar]
- 20. Cai B, Xu W, Bortnichak E, et al. . An algorithm to identify medical practices common to both the general practice research database and the health improvement network database. Pharmacoepidemiol Drug Saf 2012;21:770–4. 10.1002/pds.3277 [DOI] [PubMed] [Google Scholar]
- 21. Plana E, McGrath LJ, Fortuny J, et al. . An algorithm to identify duplicate patients when pooling aggregate data from two primary care databases in the United Kingdom. Pharmacoepidemiol Drug Saf 2016;25(Suppl 3):58–9. [Google Scholar]
- 22. Levey AS, Stevens LA, Schmid CH, et al. . A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150:604–12. 10.7326/0003-4819-150-9-200905050-00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Clegg A, Bates C, Young J, et al. . Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing 2016;45:353–60. 10.1093/ageing/afw039 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-031341supp001.pdf (71.7KB, pdf)
bmjopen-2019-031341supp003.pdf (103.5KB, pdf)
bmjopen-2019-031341supp004.pdf (70KB, pdf)
bmjopen-2019-031341supp005.pdf (94KB, pdf)
bmjopen-2019-031341supp006.pdf (63KB, pdf)
bmjopen-2019-031341supp002.pdf (72.1KB, pdf)
bmjopen-2019-031341supp007.pdf (72.5KB, pdf)
bmjopen-2019-031341supp008.pdf (66.9KB, pdf)