Abstract
Objective
To assist sideline medical staff and to augment detection of concussion in National Football League (NFL) players during preseason and regular season games via the use of certified athletic trainer (ATC) spotters.
Background
Detecting concussive injuries in contact-sport athletes can be a challenging task for health care providers on the sideline. Over the past 8 years, professional sport leagues have begun to use additional sets of eyes (medical spotters along with video review) to help identify athletes with possible concussive injuries.
Description
The NFL first began a program using spotters in 2011, and the ATC Spotter Program has undergone systematic enhancements each year. This article describes the evolution of the ATC Spotter Program, the requirements and training of its participants, and the program data available to date. Directions for future improvement and research are addressed.
Clinical Advantages
The use of ATC spotters stationed in the broadcast booth has enhanced the real-time detection of concussed players in the NFL.
Keywords: sports, health and safety program, video review
Protecting athletes by making a timely and accurate diagnosis of sport-related concussion (SRC) has become a major goal of professional sports organizations.1 The Concussion in Sport Group, at its fifth meeting in Berlin, described SRC, in the acute phase, as an “evolving injury” with variable and “rapidly changing clinical signs and symptoms.”2Given the lack of a specific biomarker, neuroimaging technique, or biomechanical technology that can be used in real time for the unequivocal diagnosis of a concussion,3 SRC is “considered to be among the most complex injuries in sports medicine to diagnose, assess and manage.”1
The clinical diagnosis of SRC relies on an assessment of signs and symptoms and an evaluation of cognitive, neurologic, vestibular, and oculomotor functions.4 This is often complicated by the fast pace of the game, the multiple players involved, limited or obfuscated views of the field, and the availability of trained health care providers, leading to a risk of missed sideline detection of concussion.5
As described by attendees at the Dublin meeting, “television coverage and commentary of injuries in collision sport and the high profile of concussion as a public health issue, has placed medical management and return to sport decisions under increased scrutiny.”1 Both the Berlin consensus2 and Dublin statements1 have suggested that the use of spotters and video review could enhance concussion identification. The use of trained spotters as extra sets of eyes for detecting concussed athletes has been pioneered in the National Hockey League (NHL),6 in Major League Soccer, and in the National Football League (NFL).7 In addition to spotters, efforts have been advanced in the use of video review to identify possible on-field cases of SRC in the NHL,6 Australian Rules Football,5 NFL,7 and National Rugby League.8,9
Through the NFL's Head Neck and Spine Committee and in collaboration with the NFL Players Association (NFLPA), ongoing efforts have been made to enhance the detection of potential concussions and other neurologic injuries in players.7,10 The purpose of this paper is to describe the evolution of the NFL Athletic Trainer Certified (ATC) Spotter Program and to provide recent metrics of program detection efforts.
HISTORY OF ATC SPOTTERS IN THE NFL
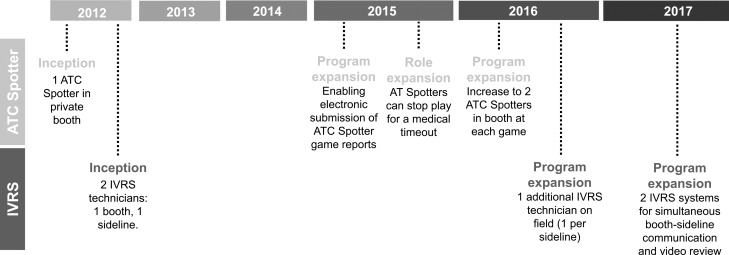
The ATC Spotter Program was launched on a pilot basis in December of the 2011 NFL regular season and introduced formally for the 2012 season. The use of video replay for detecting a possible concussion was initiated on January 7, 2012, during the 2011 NFL postseason. The program has undergone continuous enhancement (Figure 1) on a variety of levels to improve the spotters' ability to detect potentially injurious events. Although 1 ATC spotter was assigned to each game in the early seasons (2012–2015), the number was increased to 2 ATC spotters in 2016 after feedback from spotters that they could be more effective if 1 ATC could focus on the field at the same time that his or her counterpart was reviewing video with the team medical staff. In the 2015 season, ATC spotters were empowered to call a medical time-out (discussed later).
Figure 1.
Evolution of the National Football League ATC Spotter Program and injury video review system (IVRS).
ROLE OF ATC SPOTTERS
The primary duty of the ATC spotter is to alert the sideline medical staff about players with a potential injury who may need medical evaluation for concussion, musculoskeletal, or other injuries. For all preseason, regular season, and postseason games, 2 independent ATCs, or ATC spotters, observe play on the field and closely monitor the broadcast feed to identify possible player injuries. When an injury occurs, the ATC spotter places an electronic label on the specific time point in the game video at which the injury occurred; in this process, called tagging, the ATC is assisted by an injury video review system (IVRS) technician. Although ATC spotters look for and aim to tag all injuries, their emphasis is on ensuring capture of all concussions and other head and neck injuries. Tagged videos, inclusive of any injury observed during the game, are (1) provided to team physicians and sideline medical personnel for immediate use in assessment, evaluation, and possible diagnosis and (2) saved to a USB drive and provided to the club after the game, which allows the medical staff to review the play and ensure that the history is recorded accurately before entering it into the electronic medical record.
During a game, the ATC spotters use the IVRS to watch and review network footage of the game, while also monitoring play on the field. The spotters sit in a booth with 2 technicians who operate the IVRS and are responsible for tagging plays and replays at the direction of the ATC spotters. When an ATC spotter observes a possible injury, he or she will direct the IVRS technician to tag the appropriate play and associated replays in the network broadcast. The ATC spotters may also ask the IVRS technicians to rewind or slow down any video they would like to review.
If the ATC spotter observes an injury that requires immediate attention, he or she may call the sideline bench phone or use radios to speak with the team physician, head athletic trainer, or unaffiliated neurotrauma consultant (UNC; an independent neurotrauma specialist present on each sideline who is responsible for consulting on medical evaluations related to cases of possible neurologic injury) to alert and/or provide details of the injury. For purposes of potential injury review, a sideline injury video monitor is enclosed in a cart, which is opened only for use by the medical staff (Figure 2). The sideline video runs continuously and mirrors what is seen by the IVRS technicians and ATC spotter in the booth. When using the bench IVRS monitor, the sideline medical staff is able to communicate with the ATC spotter and IVRS technicians through headsets, and may ask them to rewind, slow down, or show any additional angles that may be available for the play (functions that, as of the 2018 season, were controllable on the field). The ATC spotter does not diagnose any injury or suggest treatment but simply alerts the team's sideline medical personnel to a possible injury and, when possible, describes how the injury may have occurred.
Figure 2.

Sideline video monitor and cart enclosure.
The ATC spotter must speak directly to the team physician, UNC, or head athletic trainer when reviewing a potential injury. The staff member assigned to answer the sideline bench phones is not allowed to relay the information to the team medical personnel.
QUALIFICATIONS AND TRAINING
All ATC spotters must meet the following criteria: (1) maintain a current certification by the Board of Certification for the Athletic Trainer, (2) hold an undergraduate degree from a 4-year bachelor's degree program, (3) have a minimum of 10 years' experience as an athletic trainer, (4) have significant college or professional sports experience, (5) have no prior employment as a head athletic trainer by an NFL team, and (6) have not been employed by an NFL team for the previous 10 years. These last qualifications exist to ensure that all ATC spotters are independent, which is defined as not having been recently affiliated with an NFL team in any way, including internships. Spotters are retained, assigned, and compensated by the NFL and not by the individual teams.
Since the program's inception, ATC spotters have received annual training on their role and responsibilities, including illustrative video cases. In 2017, the ATC spotters were invited to formal training sessions with other medical personnel involved in the game-day concussion care team, including NFL head athletic trainers, NFL head team physicians, and UNCs. Club neuropsychologists were added to the training sessions in 2018.
The annual medical training includes review and discussion of (1) the game-day concussion protocol, (2) the pregame medical meeting, (3) sideline medical tent usage, (4) locker room concussion evaluation, (5) video replay and game-day communications, and (6) educational sessions related to professionalism, how to work with game officials, and protocol enforcement, all directed by the NFL chief medical officer and with active input from the medical director of the NFLPA.
MEDICAL TIME-OUT
Starting in 2015, ATC spotters were empowered to call a medical time-out in cases of possible head injury to allow a player to be removed for medical examination.11 This change was initiated in response to a small number of situations in which an athlete experienced a possibly injurious event that was not immediately identified by game officials or medical staff on the field and sidelines. The ultimate goal of this added rule was to prevent possibly injured players from continuing to participate in game play, if in fact an injury had occurred, by leveraging the elevated view provided by the booth. Per the rule, an ATC spotter may initiate game stoppage and remove a player from the field if he or she has clear visual evidence that (1) a player displays obvious signs of concussion per the protocol or is clearly unstable from a suspected neurologic cause and (2) it becomes apparent that the player will remain in the game and not be attended to by the club's medical staff.
The processes involved in a medical time-out are specific. When an on-field circumstance meets these narrowly defined circumstances and the player is not attended to medically, the ATC spotter will contact the game official over the official-to-official communication system to (1) identify the player by his team and jersey number and (2) advise the official to contact the medical staff of the involved player's team and inform them that the player appears to be in need of medical attention. The designated game official must immediately stop the game, go to the player in question, and await the arrival of the team's medical personnel to ensure that the player is attended to and escorted off the field.
If the ATC spotter cannot communicate with the designated game official, then the ATC spotter will radio the NFL's field communicator (wearing a teal hat on the sideline), who will relay the team and player's number to the nearest on-field game official.
According to NFL game-day rules,11 upon calling a medical time-out, the game and play clock will stop (if running) and remain frozen until the player is removed from the game. Both clocks will start again from the same point unless the play clock was stopped inside 10 seconds, in which case it will be reset to 10 seconds.
The player's team will have an opportunity to replace him with a substitute, and the opponent will be able to match up as necessary. No member of the coaching staff may enter the playing field, and no player other than the player receiving medical attention may go to the sideline unless he is being replaced by a substitute.
Once the player is removed from the field, the team medical staff will conduct an evaluation as required by the NFL concussion protocol7 before making any decision regarding the player's eligibility to return to play. The medical staff will make the return-to-play decision, again consistent with the established NFL concussion protocol.7
The NFL game-day rules11 also state that player evaluations must last at least 1 play unless (1) the team decides to take a time-out, (2) the period ends, (3) the 2-minute warning occurs, or (4) the injury was due to a foul by an opponent. An injury time-out will not be charged to a team that has a player removed during this process.
Any deliberate attempt by a team or player to (1) stop play unnecessarily, (2) prolong or delay the process, (3) improperly take advantage of a stoppage in play, or (4) influence the actions of the ATC spotter will be considered an unfair act and subject to discipline by the NFL.
REPORTING
After each game, the ATC spotters complete electronic reports to log injuries from both the home and visiting teams and submit them through the NFL's Game Management System. These reports (Figure 3) include a combination of single select questions and free text fields. These reports are reviewed and monitored for quality-assurance purposes by the NFL chief medical officer and the medical director of the NFLPA. Data from the reports are linkable with the NFL electronic medical record system.
Figure 3.
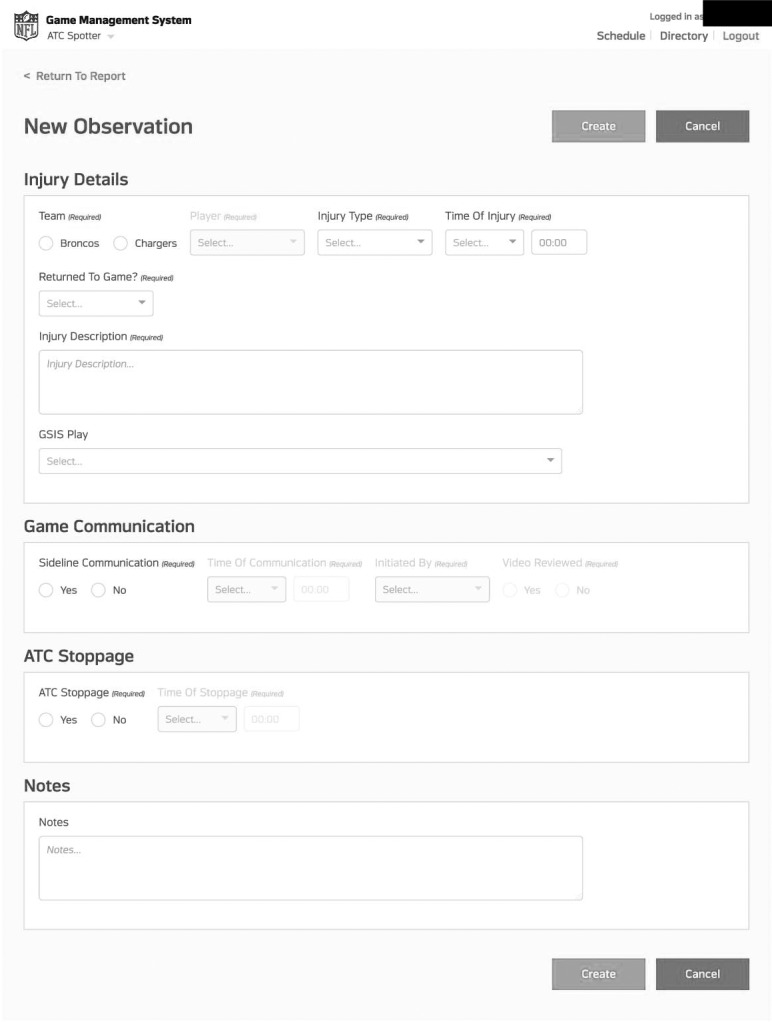
The ATC Spotter injury report.
These reports ensure that procedures are followed and enable the NFL to measure the effectiveness and volume of the ATC Spotter Program. Reporting started in 2014 and was upgraded to electronically submitted game reports in 2015.
RESULTS
Compliance with report submissions among ATC spotters has improved steadily over the years, from 89% in 2014 to 99% in 2015 and 100% in the 2016 and 2017 seasons. The results presented in this section are restricted to the 2015–2017 seasons, the strongest and most reliable years of reporting.
League wide and during the 2015–2017 seasons, between 1700 and 2300 events annually were video tagged for any possible injury. Across these 3 seasons, between 567 and 680 injuries were tagged as specifically related to the head or neck, an average of 2 per game (Table 1) and accounted for approximately 30% of all tagged injuries. The majority of tagged injuries did not result in a diagnosed concussion.
Table 1.
The ATC Spotter Reports of Possible Head or Neck Injuries per National Football League Game, 2015–2017
| Season |
Preseason |
Regular Season |
||||||
| N |
Mean ± SD |
Median |
Range |
N |
Mean ± SD |
Median |
Range |
|
| 2015 | 155 | 2.4 ± 2.0 | 2.0 | 0–9 | 518 | 2.0 ± 1.7 | 2.0 | 0–12 |
| 2016 | 133 | 2.1 ± 1.5 | 2.0 | 0–7 | 547 | 2.1 ± 1.8 | 2.0 | 0–11 |
| 2017 | 111 | 1.7 ± 1.2 | 2.0 | 0–7 | 456 | 1.8 ± 1.3 | 2.0 | 0–7 |
Sideline communications in each game, which are a metric of interaction between the ATC spotters and field personnel (eg, physicians and team ATCs) ranged from 509 to 568 per year and are detailed in Table 2. These numbers mirror trends in overall injury tagging; as the number of tagged injuries decreased, the number meriting sideline communications also decreased. The 2016 season, during which a second ATC spotter was added to the broadcast booth, had higher numbers of tagging injuries and athletic trainer-sideline communications.
Table 2.
The ATC Spotter Sideline Communications for Potential Head or Neck Injuries in National Football League Games, 2015–2017a
| Season |
Preseason |
Regular Season |
||||||
| N |
Mean ± SD |
Median |
Range |
N |
Mean ± SD |
Median |
Range |
|
| 2015 | 131 | 2.0 ± 1.7 | 2.00 | 0–8 | 419 | 1.6 ± 1.5 | 1.0 | 0–10 |
| 2016 | 107 | 1.7 ± 1.1 | 2.00 | 0–5 | 461 | 1.8 ± 1.4 | 1.5 | 0–7 |
| 2017 | 92 | 1.4 ± 0.9 | 1.00 | 0–4 | 417 | 1.6 ± 1.2 | 1.0 | 0–6 |
Includes all potential injuries where an ATC spotter in the booth called down to the sideline or where medical staff on the sideline called an ATC spotter in the booth.
Table 3 lists the number of medical time-outs called across the 2015–2017 seasons categorized by return-to-play decision. The number of medical time-outs called has ranged from 5 to 8 per season.
Table 3.
Medical Time-outs for ATC Spotter–Reported Potential Head or Neck Injuries and Subsequent Concussion Diagnosis in Preseason and Regular Season National Football League Games, 2015–2017
| Item |
2015 |
2016 |
2017 |
| Medical time-outs called by athletic trainers | 5 | 8 | 7 |
| Return-to-play decision after stoppagea | |||
| Examined, not cleared to return | 0 | 4 | 0 |
| Examined, cleared to return to play | 5 | 4 | 7 |
Player disposition after game stoppage, as indicated in the ATC Spotter report.
DISCUSSION AND NEW DIRECTIONS
Neurologic and musculoskeletal injuries in football can occur out of the sight line of sideline medical staff or be obstructed. These few seconds of missed observation can be critical in the identification and management of injured athletes on the field, and the preliminary data indicate that the ATC Spotter Program, as an addition to other medical staff and interventions, offers a useful strategy for minimizing missed injuries and has added another layer of protection for professional football players.12 The data available to date have led the NFL Department of Health and Safety to continue the ATC Spotter Program. The program has undergone yearly enhancements, reflected in these data, including the increase in injury tagging and call-downs in 2016 when a second ATC spotter was added to the booth.
The NHL,6 Australian Football League,5 National Rugby League,8,9 and Major League Soccer have employed spotters of varying backgrounds to help identify in-game head, neck, and spine injuries. These programs are largely recent in origin, and given the limited data published in the literature, empirical comparisons related to program utility and effectiveness cannot be made at present. Though the notion of extra sets of eyes to help sideline health care personnel identify in-game head, neck, and spine injuries is intuitively useful, it will be incumbent on professional leagues to demonstrate the added value of such spotter programs. These programs may also be useful in other levels of sport when an elevated view is available, although resources may not allow this at collegiate and youth levels.
Further, the NHL,6,14 Australian Football League,6 and National Rugby League8,9 have delineated lists of visible signs (VSs) to identify potential in-game concussive injury. The heads-up checklist13 has served as the initial behavioral checklist of concussion symptoms that have been assessed via observers. Research from the NHL6,14 resulted in a list of 7 VSs that were noted in 47% of the concussions ultimately diagnosed clinically by NHL physicians. The NHL research has produced sensitivity, specificity, positive and negative predictive values, and positive and negative likelihood data for the 7 VSs, as well as an injury risk model incorporating mechanism of injury, which when added to the VSs, yielded sensitivity of 81%, specificity of 72%, and positive predictive value of 26%. Gardner et al8 used 6 VSs in assessing 20 randomly selected concussed rugby players and repeated the study on a second random sample of 25 concussed rugby players.9 Makdissi and Davis5 published a surveillance tool for concussion in Australian football and identified 8 VSs. These preliminary studies have identified similar VSs (eg, loss of consciousness, gait instability or ataxia) across sports but also indicate that sport-specific VS checklists are necessary. This is certainly an area of needed research as professional athletes will demand high rates of sensitivity and specificity for examinations that may preclude their game participation. The recent international effort led by Davis et al15 is certainly a valuable empirical step in this direction.
Although the ATC Spotter Program was designed initially to help identify concussion, an additional benefit of the program has been in the identification of other, non-neurologic injuries. The 2016 season had higher numbers of tagged injuries and athletic trainer or sideline communications. Records from 2014 and earlier are not reported, as in these early years of the ATC Spotter Program, emphasis was placed on program implementation rather than record standardization and compliance. Thus, statistics from the past 3 years are reported and viewed as more reliable.
Going forward for the 2018 season, the NFL's Head, Neck and Spine Committee has enhanced the ATC Spotter Program, adding a UNC to the team of ATC spotters in the broadcast booth. The main function of the booth UNC (as opposed to the UNCs located on the sidelines) is to provide additional monitoring to the network broadcast in real time, using their clinical expertise to evaluate signs of possible concussion. It is expected that this collaborative approach will enhance the ability of the ATC Spotter team to detect signs of concussion and other injury behaviors that may not be seen on the sideline video.
CONCLUSIONS
The NFL's ATC Spotter Program has provided a valuable extra layer of protection11 to game-day medical staff for the detection of possible neurologic injury not readily seen from the sideline perspective. From the launch of the program, evaluation and enhancements have occurred annually to strengthen the ability to detect injuries with an emphasis on hits to the head and neck. The utility of the NFL's ATC Spotter Program to medical staff, both through sideline communications during events and access to video review of injury events during and after a game, suggests that these programs add value to health and safety programs in sports where injury incidence can be high and when these often difficult-to-detect injuries are a primary concern. Evidence-based refinements and enhancements to the ATC Spotter Program are expected to continue.
ACKNOWLEDGMENTS
We extend appreciation to Rachel Sendor, MPH, for assistance with data analysis and editing and to David Gardi and the NFL ATC Spotter Program for history details.
All authors have received expense reimbursements from the NFL for participation in NFL-related activities. Emily Myers, BA, and Allen Sills, MD, are employees of the NFL. Ronnie Barnes, ATC, is employed by an NFL club. Gary Solomon, PhD, has received consulting fees from the NFL. Christina Mack, PhD is employed by IQVIA, which has contracts with the NFL to provide data-analytic services and scientific consulting to the NFL, the NFLPA, and their medical committees.
REFERENCES
- 1.Patricios JS, Ardern CL, Hislop MD, et al. Implementation of the 2017 Berlin Concussion in Sport Group Consensus Statement in contact and collision sports: a joint position statement from 11 national and international sports organisations. Br J Sports Med. 2018;52(10):635–641. doi: 10.1136/bjsports-2018-099079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCrory P, Meeuwisse W, Dvorak J, et al. Consensus statement on concussion in sport: the 5th International Conference on Concussion in Sport held in Berlin, October 2016. Br J Sports Med. 2018;51(11):838–847. doi: 10.1136/bjsports-2017-097699. [DOI] [PubMed] [Google Scholar]
- 3.McCrea M, Meier T, Huber D, et al. Role of advanced neuroimaging, fluid biomarkers and genetic testing in the assessment of sport-related concussion: a systematic review. Br J Sports Med. 2017;51(12):919–929. doi: 10.1136/bjsports-2016-097447. [DOI] [PubMed] [Google Scholar]
- 4.Feddermann-Demont N, Echemendia RJ, Schneider KJ, et al. What domains of clinical function should be assessed after sport-related concussion? A systematic review. Br J Sports Med. 2017;51(11):903–918. doi: 10.1136/bjsports-2016-097403. [DOI] [PubMed] [Google Scholar]
- 5.Makdissi M, Davis G. The reliability and validity of video analysis for the assessment of the clinical signs of concussion in Australian football. J Sci Med Sport. 2016;19(10):859–863. doi: 10.1016/j.jsams.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 6.Echemendia RJ, Bruce JM, Meeuwisse W, Hutchison MG, Comper P, Aubry M. Can visible signs predict concussion diagnosis in the National Hockey League? Br J Sports Med. 2018;52(17):1149–1154. doi: 10.1136/bjsports-2016-097090. [DOI] [PubMed] [Google Scholar]
- 7.Ellenbogen RG, Batjer H, Cardenas J, et al. National Football League Head, Neck and Spine Committee's concussion diagnosis and management protocol: 2017–18 season. Br J Sports Med. 2018;52(14):894–902. doi: 10.1136/bjsports-2018-099203. [DOI] [PubMed] [Google Scholar]
- 8.Gardner AJ, Iverson GL, Quinn TN, et al. A preliminary video analysis of concussion in the National Rugby League. Brain Inj. 2015;29(10):1182–1185. doi: 10.3109/02699052.2015.1034179. [DOI] [PubMed] [Google Scholar]
- 9.Gardner AJ, Howell DR, Levi CR, Iverson GL. Evidence of concussion signs in National Rugby League match play: a video review and validation study. Sports Med Open. 2017;3 doi: 10.1186/s40798-017-0097-9. (1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Football League. NFL Head, Neck and Spine Committee's Protocols Regarding Diagnosis and Management of Concussion. New York, NY: National Football League; 2013. [Google Scholar]
- 11.Goodell R. 2015 Official Playing Rules of the National Football League. New York, NY: National Football League; 2015. [Google Scholar]
- 12.Makdissi M, Patricios J. Concussion in sport: best from Berlin, direction from Dublin and gems from gridiron. Br J Sports Med. 2018;52(14):903–904. doi: 10.1136/bjsports-2018-099402. [DOI] [PubMed] [Google Scholar]
- 13.Hutchison MG, Comper P, Meeuwisse WH, Echemendia RJ. An observational method to code concussions in the National Hockey League (NHL): the heads-up checklist. Br J Sports Med. 2014;48(2):125–129. doi: 10.1136/bjsports-2012-092059. [DOI] [PubMed] [Google Scholar]
- 14.Bruce JM, Echemendia RJ, Meeuwisse W, Hutchison MG, Aubry M, Comper P. Development of a risk prediction model among professional hockey players with visible signs of concussion. Br J Sports Med. 2018;52(17):1143–1148. doi: 10.1136/bjsports-2016-097091. [DOI] [PubMed] [Google Scholar]
- 15.Davis GA, Makdissi M, Bloomfield P, et al. International study of video review of concussion in professional sports [epub ahead of print] Br J Sports Med. 2019 doi: 10.1136/bjsports-2018-099727. [DOI] [PubMed]