Abstract
The aim of the study is to explore whether monocyte–to-lymphocyte ratio (MLR) provides predictive value of the severity in patients with Klebsiella pneumonia infection (KPI).
Patients in a tertiary medical center with Klebsiella pneumonia infection from 2014 to 2017 were recruited in this study. Patients with Klebsiella pneumonia infection were stratified into two groups based on the National Early Warning Score (NEWS). MLR was calculated by dividing monocytes count by lymphocytes count obtained from routine blood examination. The area under the curve (AUC) values was determined using the receiver-operating characteristic (ROC) curve. The correlation between the variables was tested with Pearson or Spearman correlation analysis. Ordinal logistic regression analysis was used to assess the relationship between MLR and the severity of Klebsiella pneumonia infection.
One hundred fifty-two patients were finally enrolled for analysis. Among those, 43 (28.29%) cases had severe KPI. MLR was found to be an independent risk factor of the serious Klebsiella pneumonia infection (OR: 23.74, 95% CI: 5.41–104.11, P < .001). Besides, MLR was positively correlated with NEWS score (r = 0.57, P < .001). In the receiver-operating characteristic (ROC) curve analysis, MLR, with an optimal cut-off value of 0.665, predicted the severe coronary lesion with a sensitivity of 79.4% and specificity of 84.4%.
MLR was an independent predictor of the severe Klebsiella pneumonia infection. Compared with neutrophil-to-lymphocyte ratio (NLR), MLR has a better performance to evaluate the severity of Klebsiella pneumonia infection.
Keywords: Klebsiella pneumonia, monocyte-to-lymphocyte ratio (MLR), NEWS score
1. Introduction
The infection rate of Gram-negative bacteria has gradually increased in recent years. Together with Escherichia coli, Klebsiella pneumonia is the leading cause of serious infections in newborns, blood cancer patients, immunocompromised patients[1] and even healthy people nowadays. According to the result from China Antimicrobial Surveillance Network (CHINET) in 2017,[2] Klebsiella pneumonia is the leading cause of respiratory tract infections and the second most common cause of Gram-negative bacteremia and urinary tract infections.[1] As the mortality rate of Klebsiella bacteremia and pneumonia can exceed 50%,[1] it is important for clinical physicians to detect the severity of Klebsiella pneumonia as early as possible.
The biochemical markers, such as procalcitonin (PCT), C-reactive protein (CRP), tumor necrosis factor (TNF), and interleukin-6 (IL-6) help to specify patients at risk.[3,4] While, their sensitivity and specificity for prediction the severity of infection are variable and largely insufficient. Recently, some blood parameters, originated from routine complete blood count (CBC), such as neutrophil, lymphocyte, monocyte, neutrophil-to-lymphocyte ratio (NLR), and monocyte-to-lymphocyte ratio (MLR), have been investigated as potential biomarkers with mixed results. MLR has been proved to be a prognostic factor in patients with cancer and rheumatic diseases.[5–7] However, the role of MLR in Klebsiella pneumonia infection is still unknown. Therefore, this study retrospectively investigated whether MLR is an independent predictor of the serious Klebsiella pneumonia infection.
2. Methods
A total of 152 patients with Klebsiella pneumonia who were admitted in the emergency department of Renji Hospital were included between January 2014 and December 2017 prospectively. The exclusion criteria included younger than 18 years, use of antibiotics for more than 24 h at the time of enrollment, absence of monocyte or lymphocyte count records. The national early warning score (NEWS) proposed by the Royal College of Physicians of London was used as stratification standard among the included cases, and the NEWS score ≥7 were considered as with severe infection. Forty-three of the patients had a serious infection. The infection was confirmed by a positive pathogen test from various specimens such as blood, sputum, pus, urine, drainage, tracheal cannula stump, and so on. Monocyte and lymphocyte counts were collected at the first time of admission. MLR was defined as absolute monocyte count divided by absolute lymphocyte count. This inflammatory marker was compared between patients whose NEWS score ≥7 and those whose score <7.
We expressed continuous data as the mean ± standard deviation and categorical data as frequencies. Differences in continuous variables between groups were determined using in-dependent t test or the Mann–Whitney U test, with or without a normal distribution respectively. While the differences between categorical variables were analyzed using Pearson χ2 test. The use of MLR to accurately predict the severity of Klebsiella pneumonia infection was evaluated by receiver operating characteristics (ROC) analysis and maximum sensitivity and specificity were determined. Spearman and Pearson correlation was used to assess the correlation between disease severity marker and MLR. Binary and ordinal logistic regression analysis was used to assess the independent predictors of the severity of Klebsiella pneumonia respectively. A two side P value < .05 was considered statistically significant. All statistical analyses were performed using IBM SPSS 22.0 (SPSS Inc., Chicago, IL, USA).
3. Results
3.1. Basic characteristics of the study population
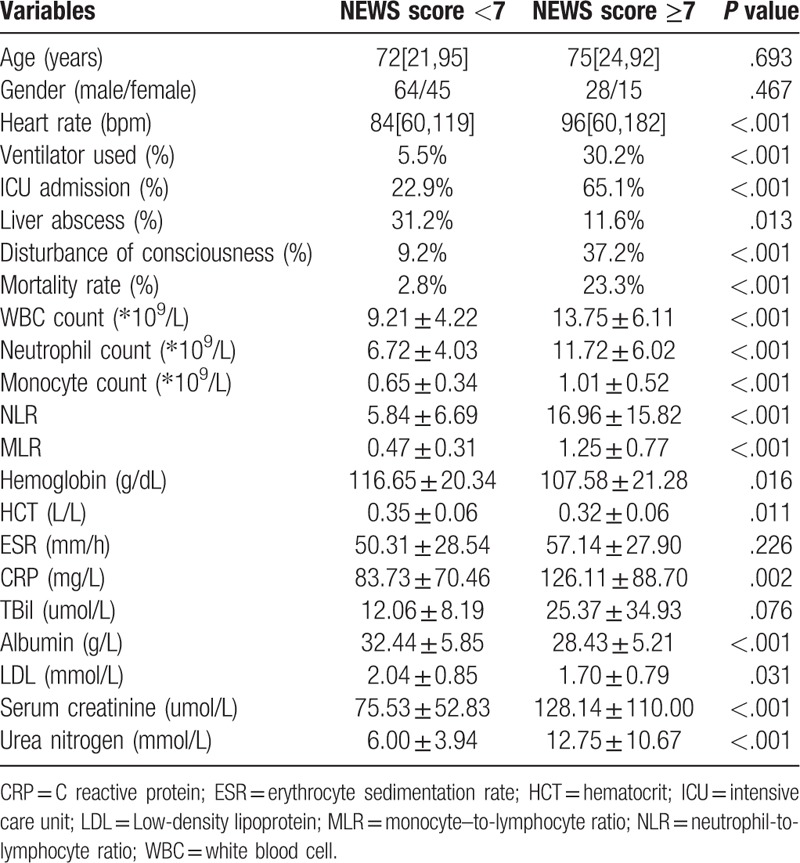
Basic demographic and biochemical characteristics of all 152 patients were outlined in Table 1. Our study included 43 patients whose NEWS score ≥7 (serious infection group, 65% of male) and 109 patients whose NEWS score <7 (normal infection group, 59% of male). Patients whose NEWS score ≥7 were a little bit older, and had more risk factors. WBC, neutrophil, monocyte, CRP, serum creatinine, and urea nitrogen levels in the serious infection group were higher than that of the normal infection group, whereas lymphocyte albumin, and low density lipoprotein level were lower (P < .05). The MLR and NLR values were 0.47 ± 0.31 and 5.84 ± 6.69 in the normal infection group, which were significantly lower than that in serious infection group patients (1.25 ± 0.77 and 16.96 ± 15.82, respectively; P < .05). The mortality rate of serious infection group was significantly higher (Table 1).
Table 1.
Basic demographic and biochemical characteristics of the study population.
3.2. MLR have high predictive value in the severe Klebsiella pneumonia infection patients
ROC curve analysis was applied to test the predictive value of MLR in severe Klebsiella pneumonia infection patients with an AUC of 0.888 (95% CI: 0.820–0.956), Figure 1. With a cut-off level of 0.665, MLR predicted serious infection with a sensitivity of 79.4% and specificity of 84.4% (Fig. 1, Table 2).
Figure 1.
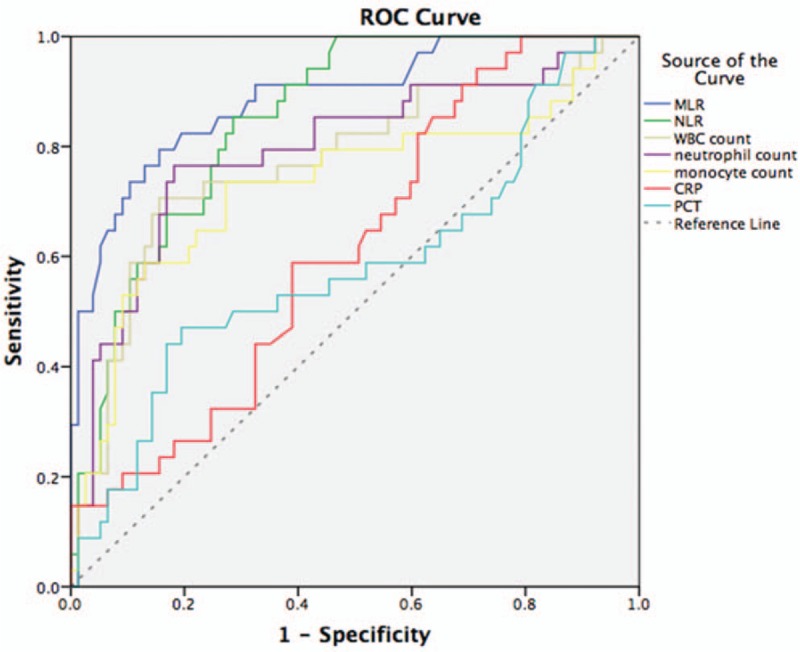
Receiver operating characteristic curves of seven infection markers for predicting the serious Klebsiella pneumonia infection. Receiver operating characteristic (ROC) curves of C-reactive protein (CRP), procalcitonin (PCT), white blood cell (WBC) count, neutrophil count, monocyte count neutrophil-to-lymphocyte ratio (NLR), and monocyte-to-lymphocyte ratio for predicting serious Klebsiella pneumonia. The area under the MLR ROC curve differed significantly from those for the NLR, CRP level, PCT level, WBC count neutrophil count, and monocyte count.
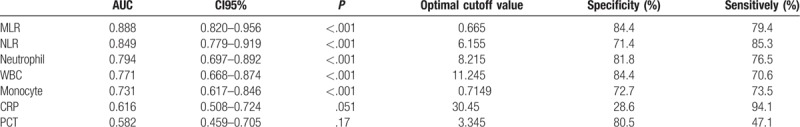
Table 2.
ROC curve was used to evaluate the predictive value of blood biomarkers for patients with severity Klebsiella pneumonia infection.
3.3. Correlation between the variables
As depicted in Figure 2, neutrophil count was positively correlated with CRP (r = 0.253, P = .002), serum creatinine (r = 0.318, P < .001), urea nitrogen (r = 0.358, P < .001), ICU admission (r = 0.309, P < .001), and mortality rate (r = 0.273, P = .001). Lymphocyte was negatively correlated with CRP (r = −0.303, P < .001), total biliburin (r = −0.240, P = .003), serum creatinine (r = −0.247, P = .002), urea nitrogen (r = −0.336, P < .001), ICU admission (r = −0.321, P < .001), and mortality rate (r = −0.234, P = .004). Monocyte was correlated with total biliburin (r = 0.196, P = .016), serum creatinine (r = 0.204, P = .012), and ICU admission (r = 0.166, P = .041). NLR was positively correlated with CRP (r = 0.260, P = .001), PCT (r = 0.197, P = .038), serum creatinine (r = 0.322, P < .001), urea nitrogen (r = 0.566, P < .001), ICU admission (r = 0.428, P < .001), and mortality rate (r = 0.313, P < .001). MLR was positively correlated with CRP (r = 0.226, P = .005), serum creatinine (r = 0.313, P < .001), urea nitrogen (r = 0.461, P < .001), ICU admission (r = 0.413, P < .001), and mortality rate (r = 0.203, P = .012) (Fig. 2).
Figure 2.
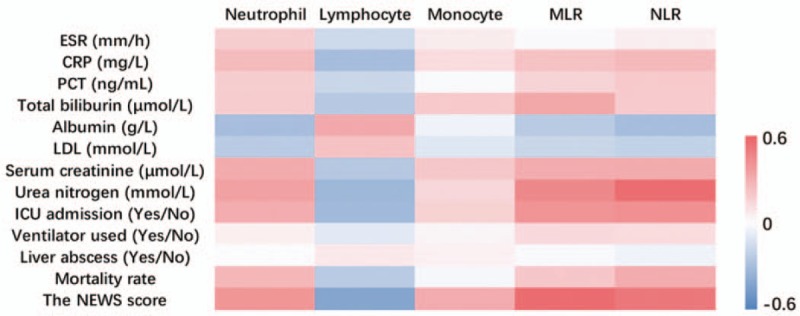
Correlation between variables.
3.4. MLR is the independent predictor of the severe Klebsiella pneumonia infection
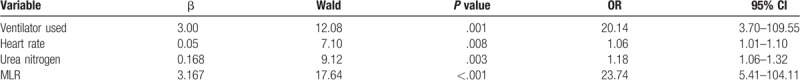
An binary logistic regression analysis was carried out to investigate which factors could be favorable for predicting the severity of the Klebsiella pneumonia infection. The regression analysis result in Table 3 demonstrated that ventilator used, heart rate, urea nitrogen and MLR were independent predictors for the severity of Klebsiella pneumonia infection. Additionally, MLR was an independent predictor for the risk of the severe Klebsiella pneumonia infection (OR: 23.74, 95%CI: 5.41–104.11, P < .001), while NLR was not. In the correlation analysis, MLR has significant association with the NEW score (r = 0.57, P < .001) (Table 3).
Table 3.
Result of ordinal logistic regression analysis.
4. Discussion
Klebsiella pneumonia is an important pathogen both in community and hospital settings. Recently, with the development of modern medical technology, especially the widely use of wide-spectrum antibiotics, endoscopy, mechanical ventilation, and catheter technology, currently with the aging of the social population, the rapid increase in tumor patients, Klebsiella pneumonia continues to cause a high rate of infection and mortality. New biomarkers are urgently required to assess disease severity. Currently, some easily, inexpensively available parameters, originated from routine complete blood count (CBC), including WBC, neutrophil, monocyte, lymphocyte, neutrophil-to-lymphocyte ratio (NLR), and monocyte-to-lymphocyte ratio (MLR) have been investigated as potential biomarkers. In our study, we found that MLR had a higher predictive value in severe Klebsiella pneumonia infection, while the MLR showed a significant correlation to the NEWS score, which is indicating the disease severity.
MLR is widely accepted to be useful in the prediction of survival in several clinical settings. The value of the MLR was previously reported in patients with laryngeal squamous cell carcinoma, patients with lung cancer, patients with advanced gastric cancer, and multiple myeloma patients with autologous transplantation.[8–11] Huang et al observed that in Guillain–Barré syndrome patients the MLR was significantly higher when compared with control, and it could be a desirable blood biomarkers in distinguishing the severe GBS from mild GBS.[12] The MLR was also gradually recognized as a predictor of prognosis in cardiovascular medicine. Fan et al reported that MLR was an independent risk factor of the presence of coronary artery disease.[13] Ji et al reported that MLR was a predictor of the lesion severity, and had better performance to reflect the severity of coronary lesion.[14] Literature regarding MLR in infection is scarce. One study reported that the MLR is a potentially valuable parameter in discriminating between different patient groups hospitalized for fever due to infection and those without infection. They concluded that MLR was a useful blood parameter to differentiate diagnosis of patients hospitalized for fever, rather than the commonly used parameters such as WBC, neutrophils counts, and CRP.[15] On the contrary, Huang et al found that MLR seemed not to be a good marker for community-acquired pneumonia (CAP) severity although MLR was elevated in CAP patients, having a higher diagnostic value for CAP.[16] Dragan explored the use of MLR in critically ill patients with secondary sepsis and/or trauma and suggested that patients with gram-negative blood culture had significantly higher MLR values in comparison with those who had gram-positive blood culture, and this was the first report which had demonstrated significant differences in MLR values regarding nature of bacteremia.[17]
To the best of our knowledge, no study investigating the predictive value of MLR in patients with Klebsiella pneumonia infection has been reported previously. This study is the first to demonstrate an association between MLR and severe Klebsiella pneumonia infection in these patients and provides a new option for predicting their severity. As mentioned, 152 patients were enrolled in our retrospective study, WBC, neutrophil, monocyte, NLR, MLR, and CRP levels in the severe Klebsiella pneumonia infection patients were higher, while the number of lymphocytes and HGB level were lower. The ROC curve showed that MLR yielded a higher AUC value, and the optimal cut-off value of MLR for serious Klebsiella pneumonia infection was 0.665, with a specificity of 84.4% and sensitivity of 79.4%. We also found that MLR showed a significant correlation to NEWS score, indicating the severity of Klebsiella pneumonia infection. However, the relationship between higher levels of MLR and serious Klebsiella pneumonia infection is not yet clear. It has been reported that monocyte were rapidly recruited to the side of inflammation upon infection, and in such situations they can develop into a wide range of terminally differentiated cells to perform versatile functions, enhancing microbicidal activities by producing cytokines and inflammatory or anti-inflammatory mediators,[18,19] and this may have an effect on increasing MLR.
The National Early Warning Score (NEWS) was established by the Royal College of Physicians of London and is currently used in several countries.[20,21] Unlike The Acute Physiology and Chronic Health Evaluation (APACHE) and the Simplified Acute Physiology Score (SAPS), it is used as a quick bedside tool, and is also intended to provide reliable, timely, and effective indications of the clinical responses of acutely ill patients. Each score of the patient corresponds to the severity of the disease, the higher the score is, the more critical the patient's condition is.[22] A NEWS score ≥7 is a key threshold to assess the severity of disease. In our study, MLR level was positively related to the NEWS score (r = 0.570, P < .001), which reflected that patients with relatively higher MLR might have more severe Klebsiella pneumonia infection.
Our study also has some potential limitations. The major limitation of our study was the limited sample size, and a retrospective single-center study, it would be better to take further prospective plan to ensure our results. Besides, we only used spot parameters for the analysis, and no follow-up values were available. Therefore, further controlled studies comprising a greater number of patients from different centers are needed to validate the clinical value of MLR for Klebsiella pneumonia infection.
In conclusion, our study is the first report on the relationship between MLR and severity of Klebsiella pneumonia infection. We consider that MLR, a widely available, inexpensive inflammatory biomarker, could be helpful to predict the severity of Klebsiella pneumonia.
Author contributions
Conceptualization: Chang-qing Zhu.
Data curation: Jialu Wang, Xin-hui Xu, Zhu-ang Ni.
Formal analysis: Jialu Wang, Dan Lv.
Funding acquisition: Ke-ji Zhang.
Investigation: Jialu Wang, Hao Gong.
Methodology: Jialu Wang.
Project administration: Jialu Wang.
Resources: Jialu Wang.
Software: Jialu Wang.
Supervision: Xiao-ye Lu, Chang-qing Zhu.
Writing – original draft: Jialu Wang.
Writing – review & editing: Jialu Wang.
Jialu Wang orcid: 0000-0003-1013-2712.
Footnotes
Abbreviations: APACHE = Acute Physiology and Chronic Health Evaluation, CAP = community-acquired pneumonia, CBC = complete blood count, CHINET = China Antimicrobial Surveillance Network, KPI = Klebsiella pneumonia infection, MLR = monocyte–to-lymphocyte ratio, NEWS = National Early Warning Score, NLR = neutrophil-to-lymphocyte ratio, ROC = receiver operating characteristics, SAPS = Simplified Acute Physiology Score.
How to cite this article: Wang Jl, Lu Xy, Xu Xh, Zhang Kj, Gong H, Lv D, Ni Za, Zhu Cq. Predictive role of monocyte-to-lymphocyte ratio in patients with Klebsiella pneumonia infection. Medicine. 2019;98:38(e17215).
Contributors: Jia-lu Wang contributed to the study design and was involved in the data analysis. All authors contributed to the study implementation/data acquisition, manuscript preparation and revision.
Data sharing statement: No additional data available.
Funding: This study was supported by grants from Shanghai Municipal Commission of Health and Family Planning (no.201640220)
Competing interests: None declared.
Patient consent: All patients gave written informed consent before participation in this study
Ethics approval: Ethics committee of Renji Hospital afflicted to School of Medicine, Shanghai Jiaotong University
References
- [1].Ahmad TA, El-Sayed LH, Haroun M, et al. Development of immunization trials against Klebsiella pneumoniae[J]. Vaccine 2012;30:2411–20. [DOI] [PubMed] [Google Scholar]
- [2].CHINET 2017 surveillance of bacterial resistance in China. Chinese Journal of Infection and Chemotherapy, 2018. [Google Scholar]
- [3].Korkmaz MF, Güzel A, Açikgöz M, et al. Reliability of pro-adrenomedullin and Interleukin 1(in predicting severity of community-acquired pneumonia in pediatric patients[J]. Ann Clin Lab Sci 2018;48:81. [PubMed] [Google Scholar]
- [4].Wang X, Jiao J, Wei R, et al. A new method to predict hospital mortality in severe community acquired pneumonia[J]. Eur J Intern Med 2017;40:56. [DOI] [PubMed] [Google Scholar]
- [5].Conrad K, Wu P, Sieper J, et al. In vivo pre-activation of monocytes in patients with axial spondyloarthritis. Arthritis Res Ther 2015;17:179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Xiang J, Zhou L, Li X, et al. Preoperative monocyte-to-lymphocyte ratio in peripheral blood predicts stages, metastasis, and histological grades in patients with ovarian cancer. Transl Oncol 2017;10:33–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Song S, Li C, Li S, et al. Derived neutrophil to lymphocyte ratio and monocyte to lymphocyte ratio may be better biomarkers for predicting overall survival of patients with advanced gastric cancer. Onco Targets Ther 2017;10:3145–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Chen L, Zeng H, Yang J, et al. Survival and prognostic analysis of preoperative inflammatory markers in patients undergoing surgical resection for laryngeal squamous cell carcinoma[J]. BMC Cancer 2018;18:816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Chen X, Wu J, Ying L, et al. Prognostic significance of pre-operative monocyte-to-lymphocyte ratio in lung cancer patients undergoing radical surgery[J]. Lab Med 2018;49:e29–39. [DOI] [PubMed] [Google Scholar]
- [10].Chen L, Hao Y, Zhu L, et al. Monocyte to lymphocyte ratio predicts survival in patients with advanced gastric cancer undergoing neoadjuvant chemotherapy[J]. Oncotargets Ther 2017;10:4007–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Solmaz Medeni S, Acar C, Olgun A, et al. Can neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio, and platelet-to-lymphocyte ratio at day +100 be used as a prognostic marker in Multiple Myeloma patients with autologous transplantation?[J]. Clin Transplant 2018;32:e13359. [DOI] [PubMed] [Google Scholar]
- [12].Huang Y, Ying Z, Quan W, et al. The clinical significance of neutrophil-to-lymphocyte ratio and monocyte-to-lymphocyte ratio in Guillain-Barré syndrome [J]. Int J Neurosci 2018;128:729–35. [DOI] [PubMed] [Google Scholar]
- [13].Fan Z, Ji H, Li Y, et al. Relationship between monocyte-to-lymphocyte ratio and coronary plaque vulnerability in patients with stable angina[J]. Biomark Med 2017;11:979. [DOI] [PubMed] [Google Scholar]
- [14].Ji H, Li Y, Fan Z, et al. Monocyte/lymphocyte ratio predicts the severity of coronary artery disease: a syntax score assessment [J]. BMC Cardiovasc Disord 2017;17:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Naess A, Nilssen SS, Mo R, et al. Role of neutrophil to lymphocyte and monocyte to lymphocyte ratios in the diagnosis of bacterial infection in patients with fever[J]. Infection 2016;45:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Huang Y, Liu A, Liang L, et al. Diagnostic value of blood parameters for community-acquired pneumonia[J]. Int Immunopharmacol 2018;64:10–5. [DOI] [PubMed] [Google Scholar]
- [17].Djordjevic D, Rondovic G, Surbatovic M, et al. Neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and mean platelet volume-to-platelet count ratio as biomarkers in critically ill and injured patients: which ratio to choose to predict outcome and nature of bacteremia?[J]. Mediators Inflamm 2018;2018:3758068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Bieber K, Autenrieth SE. Insights how monocytes and dendritic cells contribute and regulate immune defense against microbial pathogens[J]. Immunobiology 2015;220:215–26. [DOI] [PubMed] [Google Scholar]
- [19].Tsuchimoto Y, Asai A, Tsuda Y, et al. M2b monocytes provoke bacterial pneumonia and gut bacteria-associated sepsis in alcoholics. J Immunol 2015;195:5169–77. [DOI] [PubMed] [Google Scholar]
- [20].Smith GB, Prytherch DR, Meredith P, et al. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death[J]. Resuscitation 2013;84:465–70. [DOI] [PubMed] [Google Scholar]
- [21].Williams B, Alberti G, Ball C, et al. National Early Warning Score (NEWS): standardising the assessment of acute-illness severity in the NHS. London: The Royal College of Physicians; 2012. [Google Scholar]
- [22].Lee YS, Choi JW, Park YH, et al. Evaluation of the efficacy of the National Early Warning Score in predicting in-hospital mortality via the risk stratification[J]. J Crit Care 2018;47:222. [DOI] [PubMed] [Google Scholar]


