Summary:
Targeted muscle reinnervation (TMR) has been shown to decrease neuroma pain after major limb loss; however, it has not previously been described for the treatment of symptomatic neuromas in the hand after digit amputations. This report describes the use of TMR in the hand for treatment of a patient with recurrent neuromas after ray amputation of the index and long fingers that were refractory to traditional treatments. TMR was performed first for the superficial branch of the radial nerve 6 years ago to treat the dorsal neuroma pain. Following this, there was complete resolution on the dorsal aspect of the hand, however, continued neuroma pain on the volar aspect of the hand. This was treated more recently with excision of the neuromas and TMR to motor branches of the intrinsic muscles of the hand. Outcomes were measured with a numerical rating scale and Patient-Reported Outcomes Measurement System assessments and revealed decreased pain postoperatively and less interference of her activities due to pain. This report demonstrates the ability to perform TMR within the hand with good results when used for the treatment of symptomatic neuromas.
At the time of digit amputations, digital nerves are traditionally treated with either traction neurectomy or transposition into muscle, fat, or bone. The proximal nerve stump attempts regeneration after transection; however, without a distal target or pathway for regeneration, disorganized growth occurs and a neuroma develops.1 Some neuromas will become symptomatic within 2–4 months and cause chronic pain in 10–25% of amputees.2,3 This pain is caused from irritation of the neuroma by scar tissue, intervention of soft tissue or bony structures, and pressure.4
Targeted muscle reinnervation (TMR) has emerged as a treatment for neuroma pain and prevention after major limb loss.5,6 This involves transfer of a transected sensory nerve to the motor nerve entry point for an expendable muscle (one that previously inserted on the amputated segment and, therefore, serves no meaningful function). TMR has been shown to reduce neuroma symptoms and may decrease opioid requirements.7 To date, there are no reports regarding the utility TMR in the hand. Here, we describe the use of TMR for the treatment of multiple, recalcitrant symptomatic neuromas in the hand after digital ray amputations.
METHODS
The patient is a 60-year-old woman with a complex 20-year history of right-hand pain that developed following index and long finger amputations. At the time of the amputations, the digital nerves underwent standard traction neurectomy. Subsequently, she developed multiple symptomatic neuromas (identified by positive Tinel sign) in the distributions of the transected nerves including the volar digital nerves and the dorsal superficial branch of the radial nerve (SBRN).
These neuromas were initially treated nonsurgically with desensitization therapy, steroid injections, gabapentin, opioids, repeated local anesthetic injections, nerve stimulation therapy, and even botox injections. After failing nonsurgical treatments, the first several neuromas were surgically resected with relocation of the proximal nerves into muscle. Following surgical treatment of one neuroma, she obtained relief for a few weeks followed by either return of pain at the same site or unmasking of neuroma pain at another site (Fig. 1). Once recurrence was noted, nonsurgical options were again attempted; all neuromas, however, required repeat surgical intervention.
Fig. 1.
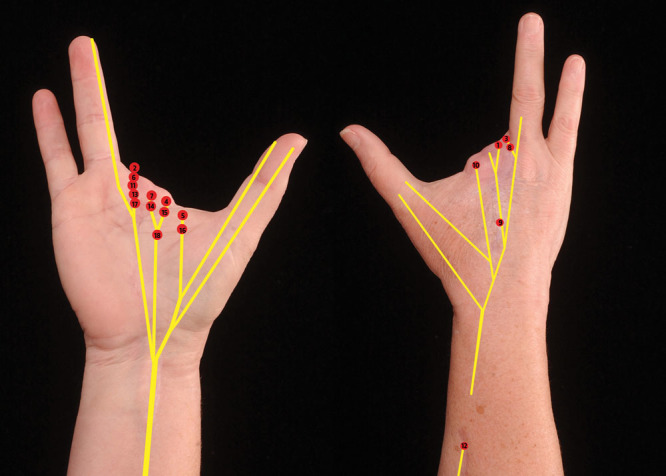
Patient’s hand showing the order neuromas that were excised over the 20-y course. Left: neuromas in the median nerve distribution; neuroma numbers 17 and 18 were treated with TMR to the intrinsic muscles. Right: neuromas treated in the distribution of the superficial branch of the radial nerve; neuroma number 12 was treated with TMR to the PIN.
Due to continued pain in the SBRN distribution despite excision of 5 neuromas, the nerve was transected more proximally in the forearm out of the zone of inflammation and the proximal end buried in muscle. Within weeks, the patient had return of pain on the dorsal hand. Later re-exploration revealed a large neuroma on the buried end of the SBRN. To try something different, this neuroma was removed and TMR was performed with transfer of the SBRN to a motor branch of the Posterior Interosseus Nerve through an epineurial window. Following this procedure, the patient has had no recurrence of neuroma pain in the SBRN distribution (6-y follow-up).
Improvement of the SBRN symptoms, however, led to unmasking of volar neuroma pain. Four additional volar neuromas were later excised followed by recurrence. The patient requested a hand amputation due to the chronic pain. A positive Tinel sign was present at 2 locations in the palm, and TMR was offered.
Intraoperatively, 2 neuromas were identified and excised: 1 on the ulnar digital nerve to the amputated long finger and the other on the common digital nerve to the second webspace (Fig. 2). Two recipient motor nerves were identified innervating intrinsic muscles for the amputated digits (second dorsal interossei and first palmar interossei, Fig. 2). These were confirmed as expendable with the nerve stimulator, transected, and coaptated to the sensory nerves with epineurial sutures.
Fig. 2.
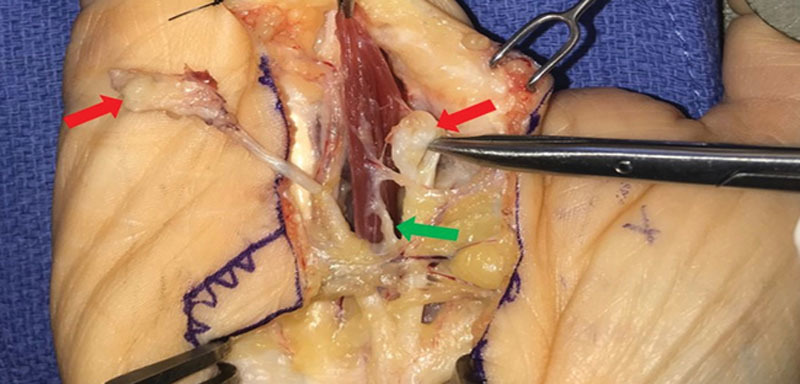
Intraoperative photograph during the second TMR procedure. Red arrows indicate the neuromas on the ulnar digital nerve to the amputated long finger and common digital nerve to second webspace. Green arrow indicates the motor branch to the first palmar interossei, which was utilized for coaptation to the proximal end of the ulnar digital nerve to the long finger. The motor branch to the second dorsal interossei not shown.
Preoperative and postoperative pain was evaluated using the 11-point (0–10) numerical rating scale and Patient-Reported Outcomes Measurement Information System assessments: Pain Intensity Short Form-3a, Neuropathic Pain Quality Short Form-5a, Nociceptive Pain Quality Short Form-5a, and Pain Interference Short Form-8a.
RESULTS
At 3 months postoperative, the patient subjectively reported a 75% improvement in symptoms. She noted that after her prior neuroma resections, the pain always returned within weeks; however, following TMR, the pain has remained diminished. She was back to doing activities that she had not been able to tolerate in several years. Use of narcotic pain medication was stopped by 2 weeks postoperatively.
Objectively, her pain decreased from 8/10 preoperatively to 2/10 at 3 months postoperatively on numerical rating scale (Fig. 3). Patient-Reported Outcomes Measurement Information System T-scores (Fig. 4) for neuropathic pain, nociceptive pain, and pain intensity decreased by 2 SDs. Pain interference (evaluates the degree of which pain interferes with daily activities) was classified as severe interference preoperatively and decreased to mild at 3 months.
Fig. 3.
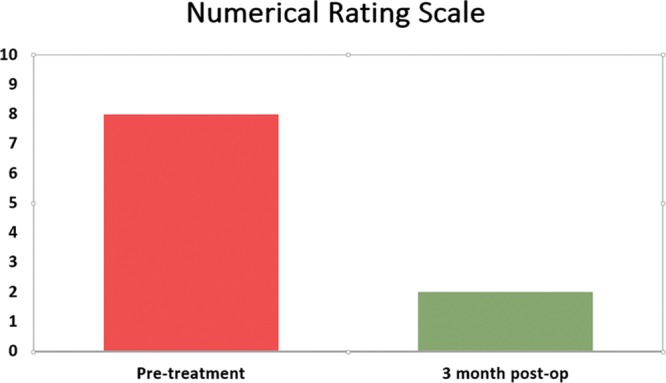
Comparison of patient’s pain based on a 11-point numerical rating scale. Pain decreased from 8/10 preoperatively to 2/10 at 3 mo post-TMR.
Fig. 4.
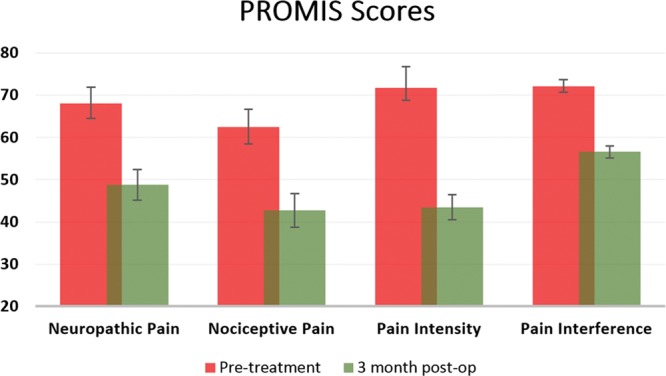
Comparison of patient’s pain based on PROMIS assessments showing T-scores pretreatment and 3 mo postoperative. Pain quality and intensity decreased by 2 SDs. Degree of pain interference decreased from severe to mild. PROMIS, Patient-Reported Outcomes Measurement Information System.
CONCLUSIONS
Neuromas in the hand can be particularly debilitating due to the hand’s importance for daily activities. Constant use may render the digital nerves more susceptible to the development of symptomatic neuromas after digit amputations. Neuroma treatment in the hand remains a challenge, as there are hundreds of described surgical and nonsurgical options.8–23
TMR offers a novel way to treat neuroma pain in the hand and provides the proximal sensory nerve the target and pathway needed to promote successful nerve regeneration without aberrant growth. These results show subjective and objective improvement in pain outcomes, adequate treatment of neuroma pain, and no recurrence in the SBRN distribution (6-y follow-up) or digital nerve distribution (3-mo follow-up) following TMR.
TMR indications could include (1) treatment of chronic symptomatic neuromas with or without digit amputations and (2) prevention of neuromas at the time of amputation. One of the potential concerns with TMR is functional deficit from muscle denervation; however, this does not occur when expendable muscles are utilized. If there is no digit amputation, the sensory nerve can be transferred end-to-side to a motor entry point, thus preserving muscle function. This patient had no deficits as TMR was performed to muscles that no longer serve a function.
Successful treatment of this patient’s recalcitrant neuroma pain suggests that TMR is successful when performed in the hand. The motor nerves to the intrinsic hand muscles are of adequate size to facilitate nerve coaptation to the digital sensory nerves. Further anatomic studies would be useful to map the locations of the motor nerve entry points for TMR in the hand.
Footnotes
Published online 5 August 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Lee SK, Wolfe SW. Peripheral nerve injury and repair. J Am Acad Orthop Surg. 1999;8:243e252. [DOI] [PubMed] [Google Scholar]
- 2.Vlot MA, Wilkens SC, Chen NC, et al. Symptomatic neuroma following initial amputation for traumatic digital amputation. J Hand Surg Am. 2018;43:86.e1–86.e8. [DOI] [PubMed] [Google Scholar]
- 3.Ducic I, Mesbahi AN, Attinger CE, et al. The role of peripheral nerve surgery in the treatment of chronic pain associated with amputation stumps. Plast Reconstr Surg. 2008;121:908–914; discussion 915. [DOI] [PubMed] [Google Scholar]
- 4.Watson J, Gonzalez M, Romero A, et al. Neuromas of the hand and upper extremity. J Hand Surg Am. 2010;35:499–510. [DOI] [PubMed] [Google Scholar]
- 5.Souza JM, Cheesborough JE, Ko JH, et al. Targeted muscle reinnervation: a novel approach to postamputation neuroma pain. Clin Orthop Relat Res. 2014;472:2984–2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dumanian GA, Potter BK, Mioton LM, et al. Targeted muscle reinnervation treats neuroma and phantom pain in major limb amputees. Annals of Surgery. 2018; Oct 26 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 7.Valerio IL, Dumanian GA, Jordan SW, et al. Preemptive treatment of phantom and residual limb pain with targeted muscle reinnervation at the time of major limb amputation. J Am Coll Surg. 2019;228:217–226. [DOI] [PubMed] [Google Scholar]
- 8.Dellon AL, Mackinnon SE. Treatment of the painful neuroma by neuroma resection and muscle implantation. Plast Reconstr Surg. 1986;77:427–438. [DOI] [PubMed] [Google Scholar]
- 9.Gorkisch K, Boese-Landgraf J, Vaubel E. Treatment and prevention of amputation neuromas in hand surgery. Plast Reconstr Surg. 1984;73:293–299. [DOI] [PubMed] [Google Scholar]
- 10.Atherton DD, Fabre J, Anand P, et al. Relocation of painful neuromas in zone III of the hand and forearm. J Hand Surg Eur Vol. 2008;33:155–162. [DOI] [PubMed] [Google Scholar]
- 11.Atherton DD, Leong JC, Anand P, et al. Relocation of painful end neuromas and scarred nerves from the zone II territory of the hand. J Hand Surg Eur Vol. 2007;32:38–44. [DOI] [PubMed] [Google Scholar]
- 12.Goldstein SA, Sturim HS. Intraosseous nerve transposition for treatment of painful neuromas. J Hand Surg Am. 1985;10:270–274. [DOI] [PubMed] [Google Scholar]
- 13.De Smet L. Preventing neuroma formation in finger amputation. Acta Orthop Belg. 1996;62:69–70. [PubMed] [Google Scholar]
- 14.Kakinoki R, Ikeguchi R, Matsumoto T, et al. Treatment of painful peripheral neuromas by vein implantation. Int Orthop. 2003;27:60–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karev A, Stahl S. Treatment of painful nerve lesions in the palm by “rerouting” of the digital nerve. J Hand Surg Am. 1986;11:539–542. [DOI] [PubMed] [Google Scholar]
- 16.Koch H, Haas F, Hubmer M, et al. Treatment of painful neuroma by resection and nerve stump transplantation into a vein. Ann Plast Surg. 2003;51:45–50. [DOI] [PubMed] [Google Scholar]
- 17.Herbert TJ, Filan SL. Vein implantation for treatment of painful cutaneous neuromas. a preliminary report. J Hand Surg Br. 1998;23:220–224. [DOI] [PubMed] [Google Scholar]
- 18.Kon M, Bloem JJ. The treatment of amputation neuromas in fingers with a centrocentral nerve union. Ann Plast Surg. 1987;18:506–510. [DOI] [PubMed] [Google Scholar]
- 19.Kumar N, Stevenson JH. Intractable digital neuroma pain; the ultimate solution? Br J Plast Surg. 1990;43:122–123. [DOI] [PubMed] [Google Scholar]
- 20.St-Laurent JY, Duclos L. Prevention of neuroma in elective digital amputations by utilization of neurovascular island flap. Ann Chir Main Memb Super. 1996;15:50–54. [DOI] [PubMed] [Google Scholar]
- 21.Mass DP, Ciano MC, Tortosa R, et al. Treatment of painful hand neuromas by their transfer into bone. Plast Reconstr Surg. 1984;74:182–185. [DOI] [PubMed] [Google Scholar]
- 22.Hazari A, Elliot D. Treatment of end-neuromas, neuromas-in-continuity and scarred nerves of the digits by proximal relocation. J Hand Surg Br. 2004;29:338–350. [DOI] [PubMed] [Google Scholar]
- 23.Guse DM, Moran SL. Outcomes of the surgical treatment of peripheral neuromas of the hand and forearm: a 25-year comparative outcome study. Ann Plast Surg. 2013;71:654–658. [DOI] [PubMed] [Google Scholar]


